Abstract
The oroantral fistula (OAF) is an epithelialized communication between the oral cavity and the maxillary sinus. In most of the cases, this communication occurs after molars and premolars extractions, but other factors may be cause of the communication, such as trauma. This article demonstrates an alternative surgical technique illustrated with a case report in which we perform the surgical treatment of OAF with palatal flap rotation combined with the use of titanium mesh in a victim of gunshot projectile wound in oral cavity.
Keywords: Maxillary antrum, oroantral fistula, surgical flap, surgical mesh
INTRODUCTION
The oroantral fistula (OAF) comprises the epithelialization of a communication between the oral cavity and the maxillary sinus, where it forms a pathologic tract between the squamous epithelium and pseudo stratified columnar ciliated, respectively.[1] OAF occurs most commonly due to complications after molars and premolars extraction because of the close proximity between their roots and the maxillary sinus floor.[2] Physiologic pneumatization of maxillary sinus increases the risk of communication. However, other etiological factors described in the literature may improve this occurrence as implant surgeries, cysts and tumors enucleation, Le Fort I osteotomy in orthognathic surgery, osteomyelitis, and trauma.[3]
Maxillofacial trauma caused by firearms and its high rate of morbidity are considered public health problems. Immediate and mediate treatment must be carried out aiming recovering patient's satisfactory masticatory function, phonetic and aesthetic, making it possible to return to social intercourse. In addition to the emergency problems as airway obstruction and neurovascular compromise, the great challenge to the Oral and Maxillofacial Surgeon to perform adequate bone and soft tissue reconstruction is extensively discussed in the literature.[4]
Several surgical techniques have been used for OAF closure, mainly with the use of local rotations as buccal and palatal flaps, the distance flaps as the temporal muscle and tongue, and the use of buccal pedicled fat pad graft (Bichat ball). It has been also described the usage of materials such as autogenous bone graft from the iliac crest, metal plates such as tantalum and gold, and synthetic materials as hydroxyapatite and resorbable membranes.[5]
The purpose of this study is to describe an alternative surgical technique illustrated with a case report using a titanium mesh combined with a palatal rotation flap for OAF closure due to trauma caused by firearms.
CASE REPORT
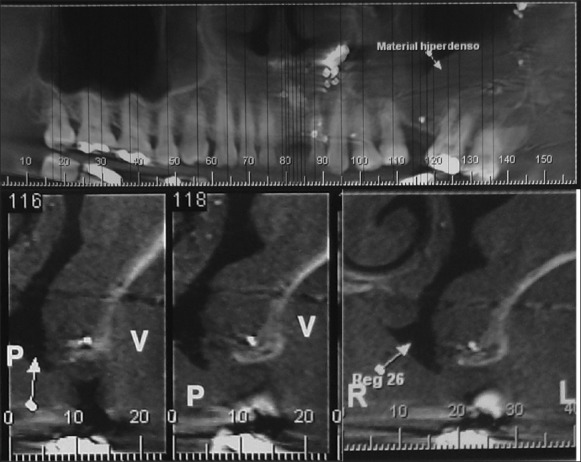
A 41-year-old male patient attended the service of Oral and Maxillofacial Surgery, Hospital Regional Agreste Caruaru/PE, victim of firearm projectile wound, with perforation entrance on the palate and accommodation bullet fragmented in the midface [Figure 1]. Primary care showed no airway compromise and/or neurovascular damage. The patient was conscious, oriented, normal respiration, acyanotic and in good condition. The extraoral examination showed mild face edema, bruising and mild mouth opening limitation. Intraoral examination presented extensive oroantral communication with soft tissue laceration, traces of gray material on irregular wound borders similar to gunpowder, minor bleeding at the site and heightened mobility of left superior molars and premolars.
Figure 1.

Radiographic aspect immediately after firearm accident
During initial treatment, a computed tomography scan was requested to evaluate the extent of the injury, as well as assisting in the treatment planning. Immediate treatment was done with copious cleaning with saline, teeth fixation with stainless steel wire no. 0, review of hemostasis, suturing of wounds and use of a nasogastric tube for patient's nutrition because an extensive oroantral communication was present. During 3 months, the patient used an occlusal splint to temporarily occlude the fistula and had orientations for wound cleaning and irrigation with 0.12% chlorhexidine. After that, definitive surgical procedure was performed to treat persistent OAF [Figures 2 and 3].
Figure 2.

Oroantral fistula
Figure 3.
Cone beam computed tomography – Note bone defect in left maxilla
Technique
Patient under general anesthesia, was infiltrated lidocaine 2% + epinephrine 1:200,000 and conducted probing around the fistula to demarcate the bone defect. The pathological tract and polypoid antral tissue were soon removed and copious irrigation with saline was performed. An intrasulcular and paramedian subperiosteal incisions were made on palate, thus forming a full-thickness palatal flap and possible full view of the bone defect of approximately 2 cm in diameter [Figure 4]. A titanium mesh measuring 3 cm × 3 cm, 0.1 mm thick with four screws 1.5 mm × 5 mm was installed in the place [Figure 5], covered with palatine flap and sutured with 4-0 polyglactin 910. The denudated place was covered with surgical cement (PerioBond - Dentsply®- Petrópolis/RJ - Brasil) and removed after 2 weeks. Postoperatively, patient received antibiotics, anti-inflammatory, analgesic and nasal decongestant. We observed proper surgical site healing after the surgical cement was removed, without infection and/or dehiscence. The patient remained under follow-up of 06 months, when complete closure of OAF and tissue repair was noted [Figures 6 and 7].
Figure 4.
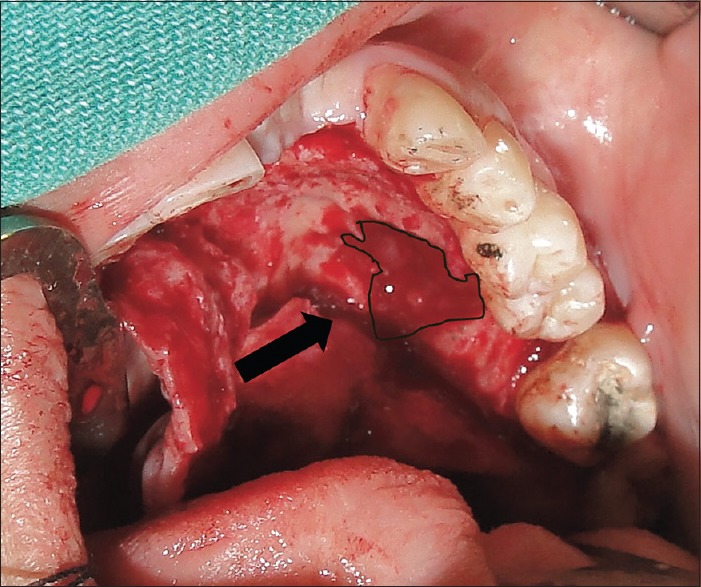
Bone defect – Compare with clinical aspect
Figure 5.
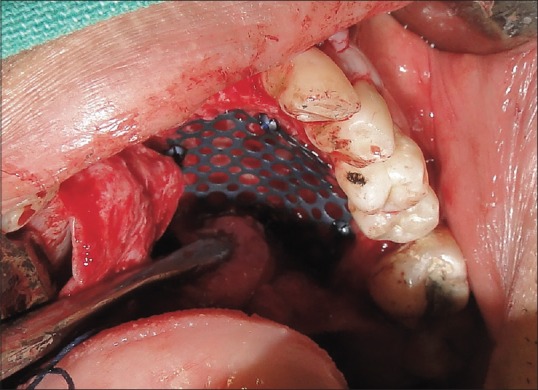
Titanium mesh
Figure 6.

Healing status of oroantral fistula on 40th postclosure day
Figure 7.

Complete closure of oroantral fistula and epithelization – after 18 months
DISCUSSION
The maxillary sinus, also called Highmore Antrum, is an air cavity which is part of the paranasal sinuses, internally revested by a membrane (Schneiderian membrane). Originally described as a useless structure, it is known that these structures are responsible for heating inspired air and drainage of secretions into the nasal cavity through the maxillary ostium. Due to its close relationship with upper posterior teeth's roots, this site is often associated with oroantral communications due to accidents during oral/dental surgery.[6]
In most cases of OAF, communication occurs after superior molars and premolars extractions.[2] When these bone defects are under 5 mm, spontaneous closure is possible. However, the largest communications as described in this article require surgical intervention. The untreated communications may cause speech and feeding problems, facial pain and chronic sinusitis.[7]
Imaging study should be always performed with high accurate methods as cone beam computed tomography (CBCT), which may accurately analyze the size of bone defect. Bone defects are generally higher than soft tissue defects observed clinically and it is an important variable to determine adequate surgical option. This kind of imaging method is also capable to analyze maxillary sinus health and possible donor sites of autogenous bone.[8]
The OAF treatment is a challenge for the Maxillofacial Surgeon. Various techniques are described as autografts,[9] allografts (dura mater, fascia lata), synthetic materials (metal plates, gold foils),[2,5] absorbable material (polyglactin, polydioxanon)[10,11] and the usage of soft tissue advancement or rotation flaps.[11] In this case, the choice for this specific technique was based on the size and location of the communication, the absence of sinus infection and the availability of soft tissues, in which buccal flaps would be difficult surgical positioning by extension of the lesion.[12] With using unique flap rotation, only soft tissue closure is achieved and techniques was developed for this occasions like guided tissue regeneration with resorbable membrane and bone substitute on sandwich technique.[13] The usage of a supporting material (titanium mesh) for palatal flap was selected to avoid a possible surgical wound dehiscence. Titanium mesh is nonresorbable, easily manipulated and feasible, biocompatible, noncarcinogenic, available in our hospital and will avoid the morbidity of a donor site as in the use of autogenous graft.[3,14]
One of the essential factors in the treatment of fistulas is the absence of sinusitis, which are the main causes of failure. Based on the multivariate analysis, the presence of maxillary sinusitis at the follow-up appointment was associated with a 15 times higher risk of recurrent OAF.[15] In this case, based on clinical signs of absence of sinusitis and CBCT it was seen that the defect in the sinus membrane was reduced, probably due to the use of the occlusal splint. Based on these facts, maxillary antrum was not operated thus decreasing comorbidity. The authors agree not to indicate this kind of technique when the OAF occurs on alveolar ridge area. Masticatory forces are higher on these sites favoring local trauma; there is lack of soft tissue availability for complete closure of a titanium mesh; also, it would be difficult for dental implant placement in these sites.
Palatal rotation flap technique consists of full thickness flap release, which includes the greater palatine artery, the one responsible for the adequate blood supply of the flap. The flap will fully cover the exposed communication, avoiding the edges of the flap being kept near the bone defect boundaries. Denudated area of the palate will repair by secondary intention, being suggested to cover it with some kind of dressing. The palatine flap has some advantage over buccal flap as not reducing the vestibulolabial depth, consequently there is no need for a second surgical procedure as a vestibuloplasty, which would allow the use of prosthesis, besides these flaps have a greater thickness, favoring the success of the technique. Its main disadvantage is the need to leave a palate denudated area in the donor site.[3]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hassan O, Shoukry T, Raouf AA, Wahba H. Combined palatal and buccal flaps in oroantral fistula repais. Egypt J Ear Nose Throat Allied Sci. 2012;13:77–81. [Google Scholar]
- 2.Güven O. A clinical study on oroantral fistulae. J Craniomaxillofac Surg. 1998;26:267–71. doi: 10.1016/s1010-5182(98)80024-3. [DOI] [PubMed] [Google Scholar]
- 3.Dym H, Wolf JC. Oroantral communication. Oral Maxillofac Surg Clin North Am. 2012;24:239–47. doi: 10.1016/j.coms.2012.01.015. viii. [DOI] [PubMed] [Google Scholar]
- 4.Majid OW. Persistent oronasal fistula after primary management of facial gunshot injuries. Br J Oral Maxillofac Surg. 2008;46:50–2. doi: 10.1016/j.bjoms.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Steiner M, Gould AR, Madion DC, Abraham MS, Loeser JG. Metal plates and foils for closure of oroantral fistulae. J Oral Maxillofac Surg. 2008;66:1551–5. doi: 10.1016/j.joms.2007.08.043. [DOI] [PubMed] [Google Scholar]
- 6.Whaites E. Porto Alegre: Artmed; 2003. Essentials of Dental Radiography and Radiology - 3rd ed; pp. 208–24. [Google Scholar]
- 7.Bureau S, Penko M, McFadden L. Speech outcome after closure of oronasal fistulas with bone grafts. J Oral Maxillofac Surg. 2001;59:1408–13. doi: 10.1053/joms.2001.28270. [DOI] [PubMed] [Google Scholar]
- 8.Watzak G, Tepper G, Zechner W, Monov G, Busenlechner D, Watzek G. Bony press-fit closure of oro-antral fistulas: A technique for pre-sinus lift repair and secondary closure. J Oral Maxillofac Surg. 2005;63:1288–94. doi: 10.1016/j.joms.2005.05.299. [DOI] [PubMed] [Google Scholar]
- 9.Er N, Tuncer HY, Karaca C, Copuroglu S. Treatment of oroantral fistulas using bony press-fit technique. J Oral Maxillofac Surg. 2013;71:659–66. doi: 10.1016/j.joms.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Buric N, Jovanovic G, Krasic D, Tijanic M, Buric M, Tarana S, et al. The use of absorbable polyglactin/polydioxanon implant (Ethisorb®) in non-surgical closure of oro-antral communication. J Craniomaxillofac Surg. 2012;40:71–7. doi: 10.1016/j.jcms.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 11.Visscher SH, van Minnen B, Bos RR. Closure of oroantral communications: A review of the literature. J Oral Maxillofac Surg. 2010;68:1384–91. doi: 10.1016/j.joms.2009.07.044. [DOI] [PubMed] [Google Scholar]
- 12.Poeschl PW, Baumann A, Russmueller G, Poeschl E, Klug C, Ewers R. Closure of oroantral communications with Bichat's buccal fat pad. J Oral Maxillofac Surg. 2009;67:1460–6. doi: 10.1016/j.joms.2009.03.049. [DOI] [PubMed] [Google Scholar]
- 13.Ogunsalu C. A new surgical management for oro-antral communication: The resorbable guided tissue regeneration membrane – bone substitute sandwich technique. West Indian Med J. 2005;54:261–3. doi: 10.1590/s0043-31442005000400011. [DOI] [PubMed] [Google Scholar]
- 14.Chacko JP, Joseph C, James H. Turn over flap for longstanding oroantral fistula closure. J Oral Maxillofac Surg Med Pathol. 2013;25:24–7. [Google Scholar]
- 15.Visscher SH, van Roon MR, Sluiter WJ, van Minnen B, Bos RR. Retrospective study on the treatment outcome of surgical closure of oroantral communications. J Oral Maxillofac Surg. 2011;69:2956–61. doi: 10.1016/j.joms.2011.02.102. [DOI] [PubMed] [Google Scholar]


