Abstract
Objective(s):
Human cytomegalovirus (CMV), a double-strand DNA herpesvirus, can be transmitted via blood transfusion which is especially important for immunocompromised recipients and can cause a fatal infection. CMV seroprevalence in Iran was studied on blood donors, healthy subjects, and some patients. Highly variable rates were detected. The purpose of this study was to review CMV seroprevalence in blood donors and apparently healthy individuals, in Iran.
Materials and Methods:
One hundred and fifty-eight electronic and paper-based resources and databases including published articles in internal and external journals, seminars, dissertations, and theses available in the database and different websites were used to be systematically reviewed as a meta-analysis. Less related articles to the issue, papers of specific high risk population, and articles with not enough information, were excluded. Eventually 22 articles that satisfied our selection criteria were systematically reviewed and analyzed. To explore heterogeneity between studies the I square (I2) index was used. Data were analyzed using the statistical software package (STATA) 11.
Results:
The heterogeneity between selected studies was 97% with an I2 statistic. In this study a random effects model was used for meta-analysis. The prevalence of CMV IgG and CMV IgM antibodies in the country were estimated to be 92% (95% CI: 90-94) and 2.6% (95% CI: 1.7-3.6), respectively.
Conclusion:
Given high rate of CMV seropositivity in Iran, it seems that CMVAbs screening would not be a reasonable and affordable approach to prevent CMV infection via transfusion especially for immune compromised recipients, so alternative strategies should be considered.
Keywords: Blood donors, CMV antibodies, CMV IgG, CMV IgM, CMV infection, CMV seroprevalence, Iran, Meta-analysis
Introduction
Cytomegalovirus (CMV) a double-strand DNA herpes virus (1) is very common infection and can lead to major disability and mortality for an immune compromised host. Transfusion of infected blood is one of human cytomegalovirus (HCMV) transmission routes. Primary infection in immunocompetent hosts usually is asymptomatic and mostly occurs in childhood and adolescence but can also be seen in adults. CMV causes severe disease with high mortality in immunocompromised individuals including solid organ transplant recipients, hematopoietic cell transplant recipients, HIV-infected patients, and patients treated with immunomodulating drugs.
The virus may hide in white cells and have a latent status after primary infection and reactivation of infection may occur whenever immune status changes, in immunocompromised and immunocompetent patients. Clinical manifestations often mimic infectious mononucleosis or severe influenza. CMV disease can be identified by finding the evidence of CMV infection with attributable symptoms or signs that may be manifest either as a viral syndrome such as fever, malaise, leukopenia, thrombocytopenia or as evidence of tissue invasion such as neurological, pulmonary, gastrointestinal, ocular, cardiovascular, and hepatic manifestations (2-5). Transmission of CMV during pregnancy can be as high as 40% and in first trimester of gestation and may lead to severe fetal developmental abnormalities (1, 4-6).
The diagnosis of CMV infection can be relied on different techniques including: electron microscopic detection of typical CMV virion, histologic or cytologic detection of typical CMV cytopathology, isolation of virus, detection of CMV antigen in blood and tissues, detection of CMV genome in tissues, DNA amplification, and serology techniques based on CMV antibodies detection. The diagnosis of CMV infection in immunocompromised patients can be difficult as it requires virus detection and determination of CMV as the cause of the disease. Several other tests are available including: DNA probe techniques, polymerase chain reaction (PCR), and immunofluorescence technique for detection of CMV early antigen (pp65) in circulating leucocytes (7). One of the most common available serologic tests to detect CMV IgG and CMV IgM antibodies is based on enzyme-linked immunosorbent assay (ELISA). IgG positive result is indicative of a person infected by CMV during his or her life. This test is not able to determine the exact time of infection. CMV IgM presence could be interpreted as new infection, acute infection or re-activation of CMV. It has been reported that CMV infection rate increases with blood donor age (3, 4). There are many articles on CMV antibody prevalence in blood donors, healthy people, pregnant women, HIV positive subjects, and patients’ candidate for renal transplantation in Iran (8-33), which reflect highly variable rates among different populations in different provinces.
The purpose of this study was to conduct a meta-analysis in order to define the rate of CMV seropositivity among the blood donors and healthy subjects and suggest a better way to limit transfusion transmission CMV, especially for immunocompromised recipients.
Materials and Methods
This study is a meta-analysis to define the seroprevalence of CMV infection in Iran among apparently healthy people and blood donors based on review of all published papers and theses documents from January1992 up to December 2013. Electronic and paper-based resources and databases were used, including published articles in internal and external journals, seminars, dissertations, and theses available in the databases and different websites (e.g: Index Copenicus, PubMed, academic journals database, free medical journals, Google scholar, SID, Magiran, Iran Docs, Medlib, Google, Bing, webcrawler, scientific journal of Iranian blood organization (IBTO) and IBTO research information booklet, dissertations) or theses in the above databases and the ones that were available in the libraries of Medical Faculty of the Universities of Tehran, Iran, Shahid Beheshti, and Tarbiat Modarres in Tehran. The literature search was performed using the dedicated keywords including CMV IgG, CMV IgM, blood donors, Iran, CMV infection, blood donors, CMV seroprevalence, meta-analysis, in reports published in both English and Persian.
To limit the different articles and records in different data bases, a combination of keywords was used in the different electronic resources or search engines (e.g: CMV + Iran + blood donors + IgG + IgM, in Google Scholar and Iran + CMV + IgG in PubMed). The registered cases about CMV in the libraries were studied. Totally nearly 800 different sources or records (including published articles in internal and external journals, seminars, and dissertations) were found, most relevant records were saved in Endnote software and duplicated (or repeated) papers or records were deleted.
Selection criteria
Initially all articles and dissertations that reported CMV were reviewed separately. Only those that specifically referred to the estimated prevalence of CMV antibodies in Iranian population were enrolled and unrelated reviews and studies with no reports of prevalence or insufficient data were excluded from the study, after critical evaluation by the authors. Based on the above steps a total of 158 records were found about CMV infection on groups of post kidney/liver, and hematopoietic stem cell transplantation (HSCT), pregnant women and their neonates after exchange blood transfusion, thalassemic patients, neurological patients, Iranian blood donors of some provinces, patients with heart diseases, HIV positive patients, healthy subjects as control groups of different ages, and army force pilots. Initially 45 articles were selected. Subsequently, 12 less relevant articles, 6 papers about high risk population, and 5 articles without enough informative data were excluded. Eventually 22 articles that satisfied our selection criteria were systematically analyzed.
Data extraction
The 22 statistically analyzed. The percentage of IgG and IgM positivity, were transcribed into a table that included place of study, study time, sample size, percentage of CMV IgG and CMV IgM antibodies positivity, and general characteristics of the samples (Table 1).
Table 1.
Characteristics of selected studies (including: year/population/detection method/sample size/results). -: Not reported
| % IgM positivity | % IgG positivity | Detection method | N | Population | Year | Place | Reference |
|---|---|---|---|---|---|---|---|
| - | 96 | ELISA | 180 | Blood bags | 1991 | Tehran | 18 |
| (as controls) | |||||||
| 0.4 | 89.6 | ELISA | 1040 | Blood donors | 2004 | Tehran | 7 |
| (as controls) | |||||||
| 3.4 | 89.2 | ELISA | 500 | Blood donors | 2004 | Zanjan | 11 |
| 2.3 | - | ELISA | 600 | Blood donors | 2004 | Kashan | 14 |
| 0 | 100 | ELISA | 30 | Blood donors | 2004 | Tehran | 9 |
| (as controls) | |||||||
| - | 94 | ELISA | 250 | Urmia residents | 2005 | Urmia | 24 |
| 2.8 | 100 | ELISA | 180 | Blood donors | 2006 | Urmia | 21 |
| (as controls) | |||||||
| - | 92.8 | ELISA | 1754 | Bushehr residents | 2007 | Bushehr | 25 |
| 4.9 | - | ELISA | 225 | Healthy subjects | 2007 | Ardebil/Tehran | 27 |
| <15Y | |||||||
| 4.4 | 98.9 | ELISA | 364 | Blood donors | 2007 | Shiraz | 17 |
| 13.5 | 88.6 | ELISA | 37 | Blood donors | 2008 | Urmia | 10 |
| (as controls) | |||||||
| - | 100 | ELISA | 925 | Kidney donors | 2009 | Tehran | 28 |
| (as controls) | |||||||
| - | 96.7 | ELISA | 96 | Healthy subjects | 2009 | Ahvaz | 29 |
| 1.1 | 94.4 | ELISA | 360 | Female university | 2009 | Kazeroon | 30 |
| students | |||||||
| 6.2 | 95.4 | ELISA | 65 | Healthy subjects | 2010 | Tehran | 19 |
| 0 | 75 | ELISA | 200 | Healthy Women | 2010 | Jahrom | 31 |
| (as controls) | Hormozgan | ||||||
| 6.5 | 49 | Minineph | 123 | Blood donors | 2011 | Zabol | 20 |
| (as controls) | |||||||
| - | 98.2 | ELISA | 595 | Province residents | 2011 | Isfahan | 16 |
| 0.4 | 55 | ELISA | 270 | Blood donors | 2012 | Khoramabad | 12 |
| (as controls) | |||||||
| 0.28 | 69.6 | ELISA | 20 | Healthy Men | 2013 | Tehran | 32 |
| - | 93 | ELISA | 100 | Healthy people | 2013 | Tehran | 22 |
| 1.6 | 99.2 | ELISA | 1008 | Blood donors | 2013 | Mashhad | 13 |
The antibodies were tested by ELISA method (based on colorimetry) using different kits prepared from different manufactures like: Dia-Pro (Italy), Diagnostica EIA-Gen (Italy), Biochem (Germany), Pishtaz-reb (Iran), Trinity Biotech Captia™ (USA), Radim SPA (Italy), Euroimmune (Germany), Sigma Diagnostica, IBL International, Biotest (Germany). CMV antibodies were evaluated with Minineph kit based on nephelometry in one study (20).
Statistical analysis
The prevalence rate of CMV antibodies (IgG and IgM) was collected from descriptive studies in this field. In this review a random effects model was used for meta-analysis, the heterogeneity between selected studies was tested using I square (I2) statistic. The test significance level was set at 0.05. Data were analyzed using the statistical software package (STATA) 11.
Results
Twenty two articles estimated the prevalence of CMV IgG and 15 articles evaluated the prevalence of CMV IgM antibodies were analyzed (Table 1). The studies were conducted in the time period of 1992 to 2013.
Total number of subjects in all articles was 8913, in average 405 people. In these studies, the highest rate of CMV IgG prevalence was reported as high as 100% in 180 blood donors of Urmia in 2006 (21), 30 blood donors of Tehran in 2004 (9), and 925 kidney donors of Tehran in 2009 (28). The lowest prevalence of CMV IgG was found as 49% among 123 blood donors in Zabol (20) and 55% (95% CI: 49-60) in 2012 among 270 blood donors from Khoramabad (12).
As the purpose of this study was to estimate the pooled prevalence of CMV IgG and CMV IgM antibodies in the Iranian blood donors and healthy subjects, based on the heterogeneity test (I square=%97) a random effects model was considered.
The prevalence of CMV IgG using the random effects model in Iranian blood donors and healthy individuals was 92% (95% CI: 90-94) (Figure 1).
Figure 1.
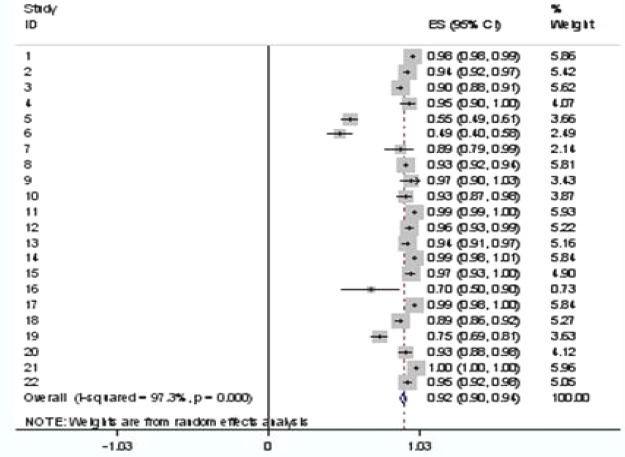
Forest plot of cytomegalovirus IgG antibody prevalence for random effects meta-analysis. Confidence interval (CI)
In some articles listed in Table 1, IgM prevalence was not studied so the sample size for meta-analysis
of IgM prevalence was 15 out of 22 articles. The heterogeneity between these 15 reviewed studies was tested using I square (I2) statistic. Based on the heterogeneity test (I2=%83) a random effect model was considered.
The prevalence of CMV IgM using the random effect model in Iranian population was 2.6% (95%CI: 1.7-3.6) (Figure 2).
Figure 2.
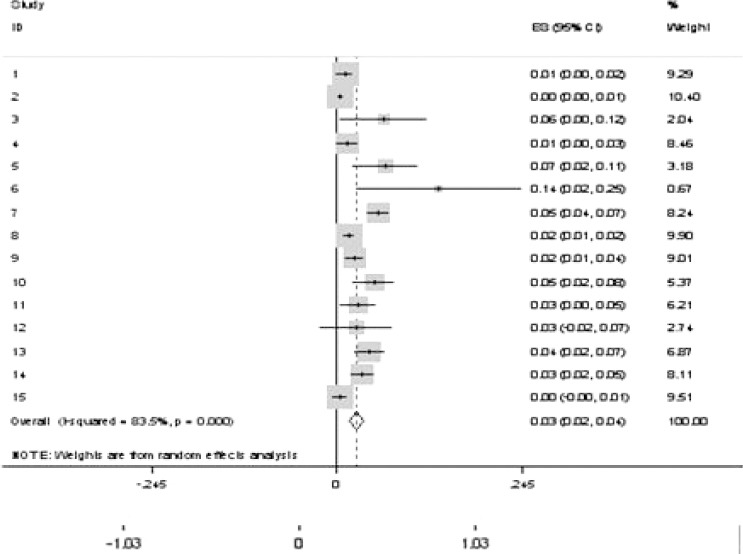
Forest plot of cytomegalovirus IgM antibody prevalence for random effects meta-analysis. Confidence interval (CI)
The highest rate of CMV IgM prevalence was eported 13.5% in 37 blood donors of Urmia in 2008 (10), and the lowest prevalence of CMV IgM was reported as 0.28% and 0.4% among healthy and blood donors individuals in Tehran (7, 32) and blood donors in Khoramabad (12), respectively.
Discussion
Using our criteria and analysis the prevalence of CMV IgG and CMV IgM antibodies in blood donors and healthy subjects were found to be 92% and 2.6%, respectively. The high seroprevalence of CMV IgG reflects the endemic state of CMV infection in Iran.
There are many studies about the prevalence of CMV antibody in adult population who live in different parts of the world; however the results may not be comparable because of different diagnostic methods, tools, and sample sizes. The results of several articles with available abstracts or full texts focused on CMV antibodies prevalence in blood donors or healthy subjects from different countries are summarized in Table 2. Articles with no information about method of antibody detection were excluded. The highest CMV IgG prevalence (97.2%) was reported in Turkey (39), while the lowest rate (64%) was reported in Brazil (35). The highest CMV IgM prevalence (19.5%) was reported in Lagos (41), while the lowest rate (0.071%) was reported in India (49).
Table 2.
Characteristics and results of studies reporting cytomegalovirus IgG and IgM antibodies prevalence
| Country | Year | N | population | % IgG positivity | % IgM positivity | References |
|---|---|---|---|---|---|---|
| India | 2002 | 200 | Blood donors | 95 | 4.5 | 36 |
| Thailand | 2001 | 441 | Blood donors | 52.23 | 9.52 | 37 |
| Germany | 2004 | 24,260 | Blood donors | 45.8 | 38 | |
| USA | 2006 | 16,040 >20Y | Normal USA Population | 68 | - | 2 |
| Turkey | 2008 | 1,264 | Blood donors | 97.2 | - | 39 |
| India | 2008 | 5,600 | Blood donors | - | 0.071 | 40 |
| Lagos | 2009 | 122 | Blood donors | 96 | 19.5 | 41 |
| Sudan | 2009 | 150 | Blood donors | 77 | - | 42 |
| Bangladesh | 2010 | 100 | donors, staffs | 94 | 2 | 43 |
| Brazil | 2010 | 1,045 | Blood donors | 64 | 2.3 | 35 |
| Iraq | 2011 | 90 | Blood donors | - | 3 | 44 |
| Nigeria | 2012 | 200 | Blood donors | 92 | - | 45 |
| Nigeria | 2012 | 192 | Blood donors | 95.8 | 3.1 | 46 |
| Saudi Arabia | 2012 | 316 | Female students | 76 | - | 47 |
| Jordan | 2012 | 2,000 | Blood donors | 90 | - | 48 |
| Japan | 2013 | 2,400 | Blood donors | 76.6 | - | 49 |
Previous systematic review and meta-analysis regarding CMV seroprevalence in healthy or blood donors has not been conducted in Iran, therefore we were not able to compare the results with another similar study in the country. Blood donation is voluntary and unpaid in Iran, with age range between 18 to 65 years old. More than 90% of donors are men. Blood donors are selected as test group in some studies, or as control group in a couple of studied articles (34, 38). According to information written in some articles (Table 1) healthy controls were selected from healthy relatives of patients included in the studies, female students, province population. (22, 24, 27, 28, 30).
The seropositivity rate of CMV in people over 40 years of age in the world is 60 to 100%, due to different factors and spreading through contacts in public places (34). Nearly 90% of population more
than 6 years of age in developing countries are infected to CMV (30). It is suggested that CMV antibodies presence is related to different factors such as socioeconomic level, and environmental and climatic factors. Souza et al (35) and Staras et al (2) declared there was no correlation between the presence of CMV antibodies and the socioeconomic characteristics of donors in the USA and Brazil. In one of the included studies (7), that serum samples were collected in spring and summer time, there was not any significance difference according to age, socioeconomical, and gender of blood donors (unpublished results).
Mostafavi et al in his study on the residents of Isfahan province showed high prevalence of CMV infection (nearly 96%) in children under 9 years old and reported that there were no difference or no relationship between CMV prevalence and age groups of 6-9, 10-19, and above 19 years of age; this reflects the fact that most infections in Iran may acquire at early ages. With regard to the reported high rate of CMV seropositivity in children under five years of age, Mostafavi et al concluded that the role of congenital, perinatal, and breast feeding transmission of CMV may have a greater effect than childhood contact in kindergartens and schools (16).
Safabakhsh (13) did not report any relationship between CMV seropositivity with gender and age.
The rate of CMV IgG and IgM positivity is reported in range between 52.23% in Thailand (37) to 97.2% in Turkey (39) and 0.071% in India (40) to 19.5% in Lagos (41), respectively (Table 2). The ranges of IgG and IgM seropositivity in Iran look as the same as other developing countries.
Although CMV infection in healthy subjects is mostly asymptomatic, transfusion transmitted CMV infection might be risky in immunocompromised patients (38) such as pregnant women, newborns and such as pregnant women, newborns and immunocompromised patients. Seronegative subjects and infants acquire CMV through infected blood products or direct contact with infected people (39). Although CMV transmission by non-leukoreduced blood products from seropositive donors occurs undoubtedly, detection rate of viable CMV is very low. It is reported that blood donation from small groups of donors can cause transmission of CMV. There are no data about the infectious dose of CMV, however low concentrations might be assumed infectious for immunocompromised patients. Low concentration of CMV in peripheral blood of immunocompetent subjects causes limitation to detect the virus in their sera (50). Several different strategies have been suggested to reduce the risk of transfusion transmitted CMV.
A possible strategy for immunocompromised patients is to remove leukocytes to decrease latent virus, but due to window period of CMV infections and seroconversion, some apparently seronegative donors with transient viremia (increasing CMV DNA in plasma) may be able to transfer CMV (38).
Providing seronegative blood units is another strategy, but because of high prevalence of CMV (>90%) in some countries, and the need for screening of a great number of blood donations (39), providing of seronegative donors strategy may not be practically affordable. Bowden reported that “the incidence rate of CMV transmission in patients receiving seronegative blood products is 1.3% while it is 2.4% in patients receiving leukodepleted blood products”. In this regard using leukodepleted blood products will not be able to significantly reduce CMV transmission. NAT testing may be a useful option, however it is challenging and there are limitations in identifying infected donors during seroconversion; it is reported that CMV DNA is rarely detectable in donors with long term CMV infection. Other strategies to identify infectious donors including testing of urine due to higher viral load in the urine and testing for rising IgM antibody titres are also suggested (50). The rate of CMV DNA positivity is reported as 75-80% in seroconverting individuals (38). Wu and colleagues reported probable transmission of CMV in seronegative patients during transfusion of leukoreduced, CMV-untested cellular blood products (50). Amini et al reported CMVDNA positivity in 6 out of 450 blood donors in Tehran blood center, in 2009, who all were CMV IgG positive and CMV IgM negative (51).
Ziemann and Hennig proposed that investigation of the interval between blood donation and transfusion might be useful because CMV stability could be affected by the conditions and duration of blood products storage prior to transfusion (50).
Due to high rate of CMV seropositivity in our country (nearly 92%) CMV antibody screening is not an efficient practical and financial option to identify CMV seronegative blood donors. CMV seronegative blood units should be made available for neonates and immunosuppressed patients or chronic users of blood products. There is no evidence of neonatal transfusion transmitted infection in Iran which might be due to high seroprevalence rate of mothers and passive IgG transfer to newborns.
In brief due to high rate of CMV seropositivity in Iran, it seems that CMV antibody screening is not an efficient or affordable strategy to prevent transfusion transmitted CMV of susceptible recipients, so alternative strategies, (e.g: leukoreduction filtration, saline-washed RBCs, and irradiation) might be helpful to minimize the transmission of CMV through transfusion.
References
- 1.Piri S. Cytomegalovirus infection in pregnancy. J Iran Obs Gynec. 2011;6:1–7. [Google Scholar]
- 2.Staras SA, Dollard SC, Radford KW, Flanders WD, Pass RF, Cannon MJ. Seroprevalence of cytomegalovirus infection in the United States 1988-1994. Clin Infect Dis. 2006;43:1143–1151. doi: 10.1086/508173. [DOI] [PubMed] [Google Scholar]
- 3.Bate SL, Dollard SC, Cannon MJ. Cytomegalovirus seroprevalence in the United States: the national health and nutrition examination surveys 1988-2004. Clin Infect Dis. 2010;50:1439. doi: 10.1086/652438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain M, Duggal S, Das Chugh T. Cytomegalovirus infection in non-immunosuppressed critically ill patients. J Infect Dev Ctries. 2011;5:571–579. doi: 10.3855/jidc.1487. [DOI] [PubMed] [Google Scholar]
- 5.Lopo S, Vinagre E, Palminha P, Paixao MT, Nogueira P, Freitas MG. Seroprevalence to cytomegalovirus in the Portuguese population 2002-2003. Eurosurvivelance. 2011;16:1–6. [PubMed] [Google Scholar]
- 6.Munro SC, Hall B, Whybin LR, Leader L, Robertson P, et al. Diagnosis of and screening for cytomegalovirus infection in pregnant women. J Clin Microbiol. 2005;43:4713–4718. doi: 10.1128/JCM.43.9.4713-4718.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aghaeipour M, Tarabadi FA, Shaeigan M, Babaei GR. Detection of serologic prevalence of anti-CMV antibodies in thalassemia major patients and blood donors. Sci J Iran Blood Transfus Organ. 2004;1:37–42. [Google Scholar]
- 8.Tarabadi F, Ghaledi J, Shaeigan M, Babaei GR. Comparison of prevalence of anti-CMV antibodies (IgM &IgG) and CMV Ag in renal transplant recipients. Sci J Iran Blood Transfusion Organization. 2005;2:145–150. [Google Scholar]
- 9.Tarabadi F, Aghaeipour M, Shaiegan M, Babaei GR. Correlation between anti-cytomegalovirus IgM antibody and HIV Positivity in HIV+ Subjects (S93). 28th International ISBT Congress - Edinburgh Scotland-2004. Vox Sang. 2004:104. A 3.29. [Google Scholar]
- 10.Khameneh ZR. Occurrence of cytomegalovirus infection and factors causing reactivation of the infection among renal transplant recipients: a single center study. Saudi J Kidney Dis Transplant. 2008;19:41. [PubMed] [Google Scholar]
- 11.Asadi MH, Esmaeilzadeh AR. Frequency of cytomegalovirus antibodies (IgG and IgM) in blood donors in Zanjan province during 2004. J Zanjan Univ Med Sci. 2004;13:43–48. [Google Scholar]
- 12.Delfan-Beiranvand M, Sheikhian A, Birjandi M, Fazeli Ml. Seroprevalence of cytomegalovirus infection in pregnant women referred to health care center of Khorramabad. Iran J Virol. 2012;5:11–16. [Google Scholar]
- 13.Safabakhsh H, Tehranian F, Tehranian B, Hatami H, Karimi G, Shahabi M. Prevalence of anti-CMV antibodies in blood donors in Mashhad, Iran. Iran J Epidemiol. 2013;9:52–57. [Google Scholar]
- 14.Moniri R, Mosayebii Z, Mossavi GA. Seroprevalence of cytomegalovirus, hepatitis B, hepatitis C and human immunodeficiency virus antibodies among volunteer blood donors. Iran J Pub Health. 2004;33:38–42. [Google Scholar]
- 15.Mostafavi SN, Ataei B, Nokhodian Z, Yaran B, Babak A, Salehi A, et al. Seroprevalence of Cytomegalovirus infection and estimate of congenital Cytomegalovirus infection in Isfahan state, Iran:A population based study. Pak J Med Sci. 2013;29:418–422. [Google Scholar]
- 16.Mostafavi SN, Ataei B, Salehi A, Nokhodian Z, Yaran M, Babak A. Seroprevalence of human cytomegalovirus diseases in Isfahan, Iran. J Isfahan Univ Med Sci. 2011;29:2475–2483. [Google Scholar]
- 17.Hashemzadeh Z, Motamedifar M. The comparison of ELISA test and nested- PCR for detection of human Cytomegalovirus (HCMV) infection. Armaghan Danesh. 2007;12:89–97. [Google Scholar]
- 18.Zandieh T, Kavian S, Rakhshan M. The evaluation of cytomegalovirus in infants following transfusion in children medical historical. Sci J Iran Blood Transfus Organ. 2:83–89. [Google Scholar]
- 19.Noorbakhsh S, Farhadi M, Tabatabaei A. Cytomegalovirus, a common cause of intrauterine infection: a case-control study in Tehran, Iran. J Comprehensive Pediatr. 2010;1:31–36. [Google Scholar]
- 20.Sanadgol N, Ramroodi N, Ahmadi GA, Komijani M, Moghtaderi A, et al. Prevalence of cytomegalovirus infection and its role in total immunoglobulin pattern in Iranian patients with different subtypes of multiple sclerosis. New Microbiologica. 2011;34:263–274. [PubMed] [Google Scholar]
- 21.Hejazi S, Molla-Abaszadeh A, Karamiyar M. Prevalence of anti-CMV antibodies in blood donors in Urmia. Sci J Iran Blood Transfus Organ. 2006;3:427–435. [Google Scholar]
- 22.Abdollahi A, Shoar S, Sheikhbahaei S, Jafari S. Sero-prevalence of cytomegalovirus and toxoplasma infections among newly diagnosed HIV patients in Iran;assessing the correlation with CD4+Cell Counts. Iran J Pathol. 2013;2:81–88. [Google Scholar]
- 23.Tarabadi F, Babaei G R, Hashemi E, Broumand B, Shaiegan M. Comparison of anti-CMV (IgG-IgM) serologic prevalence among Controls and patients under maintanance hemodialysis candidate for renal transplantation. Hakim J. 2001;4:243–247. [Google Scholar]
- 24.Hamkar R, Azarian B, Saadatmand Z. Sero-epidemiology of CMV in people under 45 years in the city of Urmia, Iran. Iran J Infect Dis Trop Med. 2005;10:29–33. [Google Scholar]
- 25.Vahdat K, Jafari SM, Pazoki R, Nabipour I. Current sensitivity C-Resactice Protein and chronic infections are associated with coronary artery disease:A population based study. Ind J Med Soc. 2007;61:135–143. [PubMed] [Google Scholar]
- 26.Arabpour M, Kaviyanee K, Jankhah A, Yaghobi R. Human cytomegalovirus infection in women of childbearing age throughout Fars Province - Iran: a population-based cohort study. Malays J Microbiol 2007. 2007:23–28. [Google Scholar]
- 27.Choobineh H, Alizadeh SH, Sharifi-Yazdi MK, Vaezzadeh F, Dargahi H, Pourfatholah AA. Serologic evaluation of Major Beta Thalassemia below 15 for cytomegalovirus infection in Iran. Res J Biomed Sci. 2007;2:584–589. [Google Scholar]
- 28.Saghafi H, Qorashi M, Heidar A. Is screening for IgG antibody to cytomegalovirus and epstein-barr virus infections mandatory in potential renal transplant recipients and donors in Iran? Transplant Proc. 2009;41:2761–2763. doi: 10.1016/j.transproceed.2009.07.057. [DOI] [PubMed] [Google Scholar]
- 29.Alavi SM, Hasan –Adel SM, Rajabzadeh AR. An Evidence against the effect of chronic cytomegalovirus infection in unstable angina pectoris. Acta Medica Iranica. 2011;49:78–80. [PubMed] [Google Scholar]
- 30.Taiebi D, Tabatabaei M, Rahsaz M, Sharifi S, Shariati M, Sohrabi I. Seroepidemiology of CMV among femal students of Azad University in Kazeroon. Iran J Epidemiol. 2009;5:55–60. [Google Scholar]
- 31.Sotoodeh-Jahromi A, Makiani MJ, Farjam MR, Madani A, Amirian M, et al. Cytomegalovirus immunity in pregnancy in South of Iran. Am J Infect Dis. 2010;6:8–12. [Google Scholar]
- 32.Abdolmohammadi K, Ghorban K, Dormanesh B, Dadmanesh M, Zarei S. Cellular and humoral immunity investigation in the Air Force Pilots of Islamic Republic of Iran. J Med Ebnesina. 2013;15:19–27. [Google Scholar]
- 33.Barazesh A, Zandi K, Hadavand F, Mootamed N, Hafzollah F, et al. Seroepidemiology of rubella, Cytomegalovirus, Herpes simplex & Varicella zoster virus in college women of Bushehr. Iran South Med J. 2014;16:459–466. [Google Scholar]
- 34.Adjei A, Armah H, Narter-Olaga E. Seroprevalence of cytomegalovirus among some voluntary blood donors at the 37 military hospital, Accra, Ghana. Ghana Med J. 2006;40:99–104. doi: 10.4314/gmj.v40i3.55261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Souza MA, Passos AM, Treitinger A, Spada C. Seroprevalence of cytomegalovirus antibodies in blood donors in southern, Brazil. Rev Soc Bras Med Trop. 2010;43:359–361. doi: 10.1590/s0037-86822010000400004. [DOI] [PubMed] [Google Scholar]
- 36.Kothari1 A, Ramachandran VG, Gupta P, Singh B, Talwar V. Seroprevalence of Cytomegalovirus among Voluntary Blood Donors in Delhi, India. J Health Popul Nutr. 2002;20:348–351. [PubMed] [Google Scholar]
- 37.Amarapal p, Tantivanich S, Balachandra K. Prevalence of Cytomegalovirus in Thai Blood donors by monoclonal staining of blood leukocytes. Southeast Asian J Trop Med Public Health. 2001;32:148–153. [PubMed] [Google Scholar]
- 38.Hecker M, Qiu D, Marquardt K, Bein G, Hackstein H. Continuous cytomegalovirus seroconversion in a large group of healthy blood donors. Vox Sang. 2004;86:41–44. doi: 10.1111/j.0042-9007.2004.00388.x. [DOI] [PubMed] [Google Scholar]
- 39.Mutlu B, Günlemez A, Türker G, Gokalp AS, Willke A. Is serologic screening necessary in the donor bloods for cytomegalovirus seronegative blood transfusion to risky patients? Mikrobiyol Bul. 2008;42:337–341. [PubMed] [Google Scholar]
- 40.Kumar H, Gupta PK, Kumar S, Sarkar RS. Is seroprevalence of anti-IGM CMV among blood donors relevant in India. Indian J Pathol Microbiol. 2008;51:351–352. doi: 10.4103/0377-4929.42509. [DOI] [PubMed] [Google Scholar]
- 41.Akinbami AA, Akanmu AS, Adeyemo TA, Wright KO, Dada MO, Dosunmu A. Cytomegalovirus antibodies amongst healthy blood donors at Lagos University Teaching Hospital (Luth) South Afr Med J. 2009;99:528. [Google Scholar]
- 42.Kafi S, Eldouma E, Saeed S, Musa H. Seroprevalence of Cytomegalovirus among blood donors and antenatal women attending two hospitals in Khartoum State. Sudan J Med Sci. 2009;4:48–52. [Google Scholar]
- 43.Jahan M, Tabassum S, Aziz A, Ahmed M, Islam N. Transfusion associated CMV infection:Transfusion strategies for high risk patients. Bangladesh J Med Microbiol. 2010;04:24–27. [Google Scholar]
- 44.Al-Dabbagh KA. Detection of toxoplasma gondii IgM and cytomegalovirus IgM antibodies among blood donors in Mosul. Irq J Pharm. 2011;11:86–91. [Google Scholar]
- 45.Alao O, Mamman A, Araoye MO, Joseph E. Effect of demographic variables on cytomegalovirus antibody seropositivity among prospective blood donors in Jos, Nigeria. Niger Postgrad Med J. 2009;16:139–142. [PubMed] [Google Scholar]
- 46.Ojide CK, Ophori EA, Eghafona N, Omoti C. Seroprevalence of cytomegalovirus (CMV)amongst voluntary blood donors in University of Benin Teaching Hospital (UBTH), Edo State, Nigeria. Br J Med Med Res. 2012;2:15–20. [Google Scholar]
- 47.Barah F. Prevalence of herpes simplex types 1 and 2, varicella zoster virus, cytomegalovirus, and immunoglobulin G antibodies among female university students in Syria. Saudi Med J. 2012;33:990–994. [PubMed] [Google Scholar]
- 48.Hani A. Seroprevalence of cytomegalovirus in healthy voluntary blood donors in renowned Jordanian Hospital. Int J Biol Med Res. 2012;3:2193. [Google Scholar]
- 49.Furui Y, Satake M, Hoshi Y, Uchida S, Suzuki K, Tadokoro K. Cytomegalovirus (CMV) seroprevalence in Japanese blood donors and high detection frequency of CMV DNA in elderly donors. Transfusion. 2013;53:2190–2197. doi: 10.1111/trf.12390. [DOI] [PubMed] [Google Scholar]
- 50.Ziemann M, Hennig H. Prevention of transfusion-transmitted cytomegalovirus infections: which is the optimal strategy? Transfus Med Hemother. 2014;41:40–44. doi: 10.1159/000357102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amini Kafi-abad S, Ranjbar-Kermani F, Ferdowsian F, Sobhani M, Samie S. Assessing the frequency of cytomegalovirus viremia in Iranian (Tehran) blood donors by polymerase Chain reaction method. Hakim Res J. 2009;12:61–67. [Google Scholar]


