Abstract
The effects of deep brain stimulation (DBS) on balance in people with Parkinson's disease (PD) are not well established. This study examined whether DBS randomized to the subthalamic nucleus (STN; n = 11) or globus pallidus interna (GPi; n = 10) improved compensatory stepping to recover balance after a perturbation. The standing surface translated backward, forcing subjects to take compensatory steps forward. Kinematic and kinetic responses were recorded. PD-DBS subjects were tested off and on their levodopa medication before bilateral DBS surgery and retested 6 mo later off and on DBS, combined with off and on levodopa medication. Responses were compared with PD-control subjects (n = 8) tested over the same timescale and 17 healthy control subjects. Neither DBS nor levodopa improved the stepping response. Compensatory stepping in the best-treated state after surgery (DBS+DOPA) was similar to the best-treated state before surgery (DOPA) for the PD-GPi group and the PD-control group. For the PD-STN group, there were more lateral weight shifts, a delayed foot-off, and a greater number of steps required to recover balance in DBS+DOPA after surgery compared with DOPA before surgery. Within the STN group five subjects who did not fall during the experiment before surgery fell at least once after surgery, whereas the number of falls in the GPi and PD-control groups were unchanged. DBS did not improve the compensatory step response needed to recover from balance perturbations in the GPi group and caused delays in the preparation phase of the step in the STN group.
Keywords: deep brain stimulation, Parkinson's disease, balance, compensatory stepping
the large number of falls experienced by people with Parkinson's disease (PD) (Pickering et al. 2007) is thought to be related to inadequate postural responses (Bloem et al. 2001; Horak et al. 1996, 2005). The ability to generate a step quickly and accurately after a loss of balance is disrupted in PD, and levodopa medication seems to offer no benefit (King et al. 2008, 2010). This study investigated whether deep brain stimulation (DBS) randomized to either the globus pallidus interna (GPi) or subthalamic nuclei (STN) could improve the compensatory stepping response of people with PD.
DBS has been shown to have significant antiparkinsonian effects that are superior to best medical therapy by reducing the cardinal PD symptoms including tremor, bradykinesia, and rigidity (Weaver et al. 2009, 2012). However, there have been mixed results on whether quantitatively measured balance is also improved. Some aspects of balance control, such as postural sway when standing, show improvement when DBS is turned on (Rocchi et al. 2002). In-place postural responses also improve when DBS is turned on compared with off DBS; however, compared with presurgery function there is no overall improvement, with STN-DBS showing worsening compared with GPi-DBS (St George et al. 2012). Voluntary step initiation does not improve with DBS, and there is an overall impairment in step preparation after surgery compared with before surgery in both STN and GPi sites (Rocchi et al. 2012).
When taking a voluntary step forward, a lateral weight shift toward the stance foot (sometimes called an anticipatory postural adjustment or APA) is required to maintain lateral balance when the stepping foot is off the ground. When a predictable external perturbation pushes a standing person just beyond the threshold of an in-place response, an APA is generally observed just prior to the compensatory step. However, as the perturbation increases in strength or becomes unpredictable, the APA is increasingly absent in healthy control subjects (McIlroy and Maki 1993). The sideways instability induced by taking one foot off the ground is given less priority than the forward instability imposed by the perturbation, and so the lateral APA is inhibited in order to expedite the compensatory step to preserve balance. When subjects with PD are exposed to large, unpredictable perturbations they exhibit APAs far more frequently than control subjects, which delays the time to lift the stepping foot (King et al. 2010). Furthermore, PD subjects sometimes make multiple APAs before a compensatory step, as though they are preparing to lift a particular foot off the ground only to abort and switch to the other foot. This behavior is associated with festination and freezing of gait (Jacobs et al. 2009), and freezing of gait in PD is associated with falls (Kerr et al. 2010).
The execution phase of the compensatory step is also affected in PD (King et al. 2010). A step that is too short may be insufficient to arrest the falling center of mass (CoM) of the body, so subsequent steps may be required to recover balance. Similarly, a step that is too slow may allow the CoM to fall further in the time before the foot contacts the floor; again, subsequent steps may be required.
The primary aim of this study was to determine whether the DBS procedure in either STN or GPi could improve the stepping responses of PD subjects to fast, unexpected postural perturbations. Step preparation and execution phases were studied in PD subjects before and 6 mo after DBS surgery. Both off- and on-levodopa medication and off- and on-DBS states were tested to determine interaction effects between the therapies. A PD-control group was tested to compare any changes to the natural progression of PD over the 6-mo time frame.
MATERIALS AND METHODS
Subjects
Seventeen healthy control subjects and 29 subjects with idiopathic PD were included in this study. The healthy control group included 14 men and 3 women with an average age of 65.7 (SD 7.7) yr. Twenty-one of the PD subjects underwent DBS surgery. Target DBS sites were randomized to either the STN (n = 11) or the GPi (n = 10) as part of a VA/NINDS multicenter, double-blind clinical trial (Follett et al. 2010). The eight remaining PD-control subjects met the criteria for DBS surgery but chose not to undergo the procedure. There were no significant demographic differences between the groups (Table 1). All subjects gave informed written consent for protocols approved by the Institutional Review Board of Oregon Health and Science University.
Table 1.
Demographics of PD groups and clinical characteristics
| GPi (n = 10) | STN (n = 11) | PD-Control (n = 8) | |
|---|---|---|---|
| Sex | 9 M, 1 F | 9 M, 2 F | 7 M, 1 F |
| Age, yr | 62.8 ± 8.2 | 62.0 ± 5.7 | 60.0 ± 8.5 |
| PD duration, yr | 15.4 ± 8.7 | 13.3 ± 5.0 | 12.1 ± 6.0 |
| UPDRS III | |||
| Baseline off | 51.3 ± 20.0 | 46.4 ± 10.2 | 47.0 ± 16.5 |
| Baseline DOPA | 30.5 ± 15.0 | 22.6 ± 10.9 | 23.3 ± 9.5 |
| 6 mo off | 50.0 ± 17.3 | 53.1 ± 16.7 | 44.6 ± 13.0 |
| 6 mo DOPA | 33.8 ± 13.0 | 32.7 ± 15.3 | 23.6 ± 10.1 |
| 6 mo DBS | 37 ± 19.0 | 31.6 ± 12.5 | |
| 6 mo DBS+DOPA | 22.4 ± 14.4 | 20.5 ± 9.5 | |
| LEDD: baseline | 1,412 ± 887 | 1,349 ± 668 | 1,253 ± 477 |
| LEDD: 6 mo | 1,122.6 ± 348 | 908.4 ± 538 | 1,149 ± 345 |
All errors are SDs.
PD, Parkinson's disease; GPi, globus pallidus interna; STN, subthalamic nucleus; UPDRS III, Total Unified Parkinson's Disease Rating Scale III; DBS, deep brain stimulation; LEDD, Levodopa Equivalent Daily Dose (Nutt et al. 2003).
Surgical Procedure
Bilateral surgical implantation of DBS electrodes (Medtronic, 3387) was performed by an experienced neurosurgeon (K. J. Burchiel) using a Leksell stereotactic frame and MRI guidance (STEALTH FrameLink). With the NeuroTrek system (Alpha-Omega, Atlanta, GA) two microelectrodes were advanced simultaneously and recordings made for the purposes of target verification, and corrections to the implant site were made if needed. For further details see St George et al. (2012). DBS subjects visited a movement disorders neurologist on at least three occasions over 90 days for DBS and medication optimization. The mean amplitude of the DBS was 3.29 V (range 1.4–5 V), with 80% of the subjects having a 90-μm pulse width (4 subjects at 60 μm), and at a rate of 185 Hz for 70% of the subjects (the others ranged between 130 and 150 Hz).
Experimental Protocol
Subjects stood on dual-force plates of a movable platform looking straight ahead (Fig. 1). Arms were folded across the chest to ensure consistency between subjects and to allow visibility of the motion analysis markers on the greater trochanter. Trials took place after a series of slower-velocity forward and backward platform translations. Three trials began with foot width parallel and 5 cm apart, another three trials at 26 cm apart, and a final trial at a self-selected comfortable width. Initial analysis revealed no significant effect of these three foot displacements between treatment conditions, so responses were averaged across the seven trials. A harness attached to the ceiling was worn, which did not provide support in upright stance but would catch the subject midway through a fall. An assistant stood behind the subject and only intervened when it was clear the subject could not regain standing equilibrium independently. The location of the center of pressure was monitored prior to each trial on an oscilloscope, and the perturbation only began when the center of pressure was in the subject's quiet stance range. Subjects were instructed to keep their balance as best they could. Platform translation was backward at a velocity that pilot testing had revealed was above stepping threshold of young control subjects (step velocity profile of 56 cm/s for 0.5 s). Therefore the only way to recover equilibrium without assistance was to initiate a compensatory stepping response.
Fig. 1.
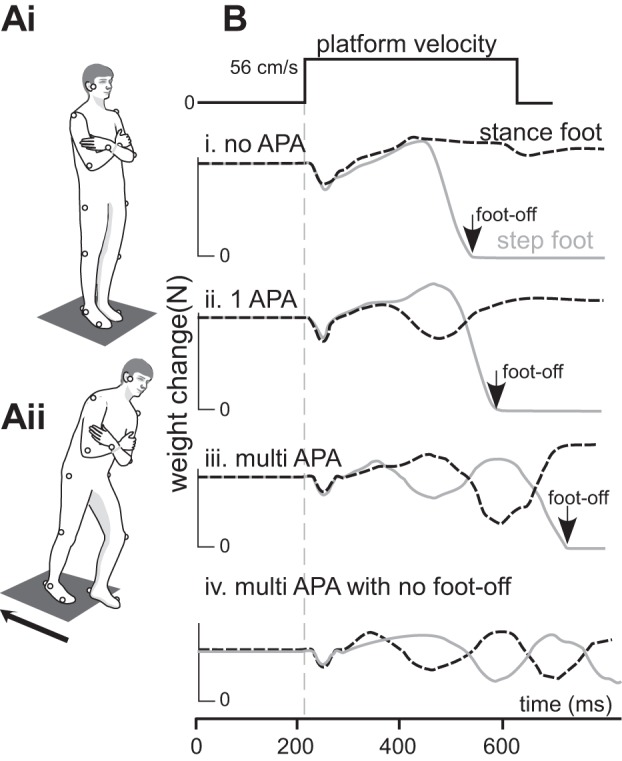
A: the subject stood quietly with arms folded (Ai) when the standing surface unexpectedly moved backward with a step velocity that forced the subject to make a compensatory step forward (Aii). B: examples of vertical force distribution changes under the feet during the perturbation and the categorization of anticipatory postural adjustments (APAs).
Experimental Conditions
Baseline.
Compensatory stepping responses of PD-DBS and PD-control subjects were tested in the morning in the “practical” OFF state—at least 12 h since taking any dopaminergic medication. Later the same day they were retested when they reported feeling “ON” medication after waiting between 45 and 75 min after taking their usual dose of dopaminergic medication.
Six months.
PD-DBS subjects were retested 6 mo after DBS surgery to allow the effects of surgery to stabilize (Burchiel et al. 1999). These subjects again arrived at the laboratory in the practical OFF medication state with their DBS on. After testing in the DBS-only condition the stimulator was turned off, and after 45–60 min subjects were retested in the OFF/OFF condition. Subjects then took their usual antiparkinsonian medication dose and were retested approximately an hour later on medication (DOPA). In the final condition, the stimulator was turned on and ∼30 min later testing was performed in the DBS+DOPA condition. The PD-control subjects were retested 6 mo later with the baseline test protocol.
Before each condition, PD subjects were tested on the motor subsection of the Unified Parkinson's Disease Rating Scale (UPDRS III) (Fahn and Elton 1987; St George et al. 2014). Plenty of rest and refreshment breaks were offered throughout the testing session.
Data Collection and Analysis
A three-dimensional representation of body motion was measured with the Motion Analysis system (Santa Rosa, CA) with 8 video cameras recording 23 reflective markers placed on body landmarks at 60 Hz. Step latency was determined from the time of surface translation to the time the weight on the stepping foot dropped to below 2% of body weight. The vertical forces under the feet were assessed for the presence of APAs prior to stepping. An APA was only identified if a mediolateral force shift toward the stepping foot and away from the stance foot occurred before foot liftoff and at least 50 ms after the perturbation onset (Fig. 1B) (King et al. 2010). Center of body mass (CoM) was calculated from joint positions and anthropomorphic measurements (Vaughan et al. 1982). The number of steps required to arrest the falling CoM was recorded.
Statistical Analysis
The number of APAs before foot-off were compared between groups and conditions with nonparametric statistics. The normally distributed foot-off latency, CoM position at foot-off, mean number of steps, and length and velocity of the first step were compared between groups and conditions with multivariate repeated-measures analysis of variance. The statistical tests were implemented according to the specific comparisons of interest.
Disease effect.
Comparisons between the healthy control subjects and PD subjects at baseline were performed using group (healthy control/PD-control/PD-GPi/PD-STN) as a between-subjects factor.
Procedural effect.
Comparisons were performed between baseline and the 6-mo assessment when off and on medication for the three PD groups (PD-control, PD-STN, PD-GPi).
Stimulation and therapy interaction effects.
After DBS surgery the effects of DBS (on/off) and medication (on/off) on the stepping variables for the STN and GPi groups were compared.
Therapeutic effect.
The best-treated state at baseline (DOPA) was compared to the best-treated state at the 6-mo retest (DOPA for the PD-control subjects and DOPA+DBS for the PD-DBS subjects).
Spearman correlations were calculated to determine the association between the number of APAs prior to foot-off and the other step parameters.
RESULTS
Disease Effect
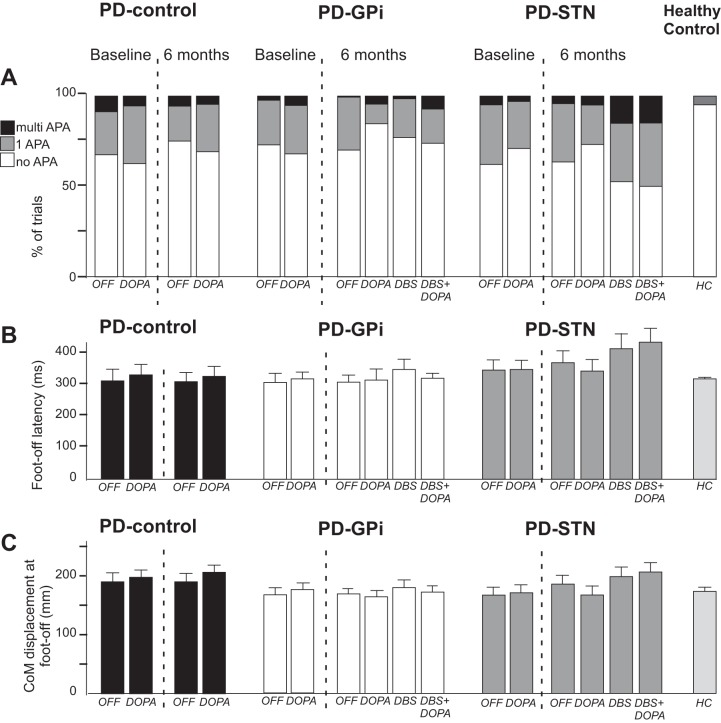
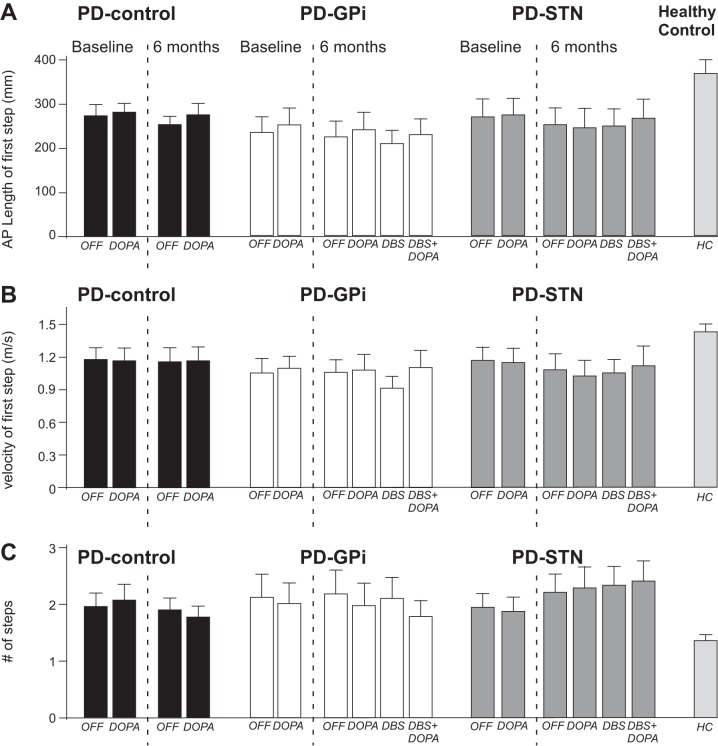
At baseline assessment, there was no difference in any of the stepping variables between the PD-control, PD-STN, and PD-GPi groups (P > 0.05 for each post hoc comparison). Figure 2A shows that lateral APAs before foot-off occurred more frequently in subjects with PD compared with control subjects (P < 0.01). In 90% of trials healthy control subjects had no APA prior to foot-off, whereas PD subjects at baseline had one or more APAs on approximately one-third of trials. The time to take the stepping foot off the ground and the displacement of the CoM were similar between control and PD groups at baseline (Fig. 2, B and C). The first compensatory step was longer (P < 0.01) and faster (P = 0.045) for healthy control subjects compared with subjects with PD (Fig. 3, A and B). In addition, subjects with PD required a greater number of total steps to regain balance compared with the healthy control subjects (P < 0.01; Fig. 3C).
Fig. 2.
Preparation for compensatory stepping. A: % of trials categorized by their APA behavior for each of the groups. B and C: mean ± SE of the latency to foot-off (B) and forward displacement of center of mass (CoM) at the time of foot-off (C) for each condition. In B and C, the Parkinson's disease (PD) control group is shown in black, the PD-globus pallidus interna (GPi) group is white, the PD-subthalamic nucleus (STN) group is dark gray, and the healthy control (HC) group is light gray.
Fig. 3.
Execution phase of compensatory stepping: mean ± SE anterior-posterior (AP) length of the first step (A), average velocity of the first step (B), and total number of steps required to regain balance for the PD-control subjects (C). The PD-control group is shown in black, the PD-GPi group is white, the PD-STN group is dark gray, and the HC group is light gray.
Procedural Effect
When comparing baseline OFF and DOPA conditions with 6-mo OFF and DOPA conditions across PD groups, there was no significant change in the number of APAs prior to stepping, the foot-off latency, the displacement of the CoM at foot-off, or the velocity of the step. Step length of the first step was shorter at the 6-mo assessment compared with baseline assessment (P = 0.04), but there was no session × PD group interaction (P = 0.913), suggesting that natural progression of disease was the cause. There was a significant session × PD group interaction (P = 0.037) for the total number of steps, as the STN group required more steps to recover balance than they did before surgery (P = 0.029), whereas the GPi and PD-control groups had no change (P > 0.05 for each). Medication did not affect any of the stepping variables, with no significant main or interaction effects.
Stimulation and Therapy Interaction Effects
When the four conditions at 6-mo assessment in the DBS groups were compared, the preparation phase of the step appeared to be negatively affected by turning the stimulator on in the STN group but not the GPi group. The number of APAs prior to foot-off increased from about one-third to half of all trials when the DBS was turned on compared with off (Fig. 2A) for the STN-DBS subjects (P = 0.021). In contrast, the number of trials with APAs remained unchanged for the GPi-DBS group when DBS was turned on. There was a significant stimulation (DBS off, DBS on) × group interaction for stepping latency (P = 0.05), with the DBS stimulation increasing stepping latency more in the STN than in the GPi. The length and speed of the first step and the number of total steps were not changed by turning the stimulator on, and there were no length or speed interaction effects with DBS group.
Therapeutic Effect
The number of APAs prior to the step increased in the best-treated state after surgery (DBS+DOPA) compared with the best-treated state (DOPA) at baseline for the STN group (P = 0.017) but not the GPi or PD-control group (Fig. 2A). There was a significant best therapy (baseline, 6 mo) × group interaction for step latency (P = 0.041) and CoM displacement at foot-off (P = 0.043) and the number of steps (0.017). This interaction was because the STN group had longer step latencies, a further CoM displacement at foot-off, and a greater number of average steps required to recover balance at the 6-mo assessment than they did at baseline.
APA Correlations
A greater number of APAs prior to foot-off was associated with delayed step latency (R = 0.39, P < 0.001), an increased CoM displacement at foot-off (R = 0.37, P < 0.001), reduced step length (R = −0.1, P = 0.001), reduced step velocity (R = −0.11, P < 0.001), and an increase in the total number of steps required to recover balance (R = 0.23, P < 0.001).
Falls
When subjects failed to independently recover balance, the trial was classified as a fall (always caught by the harness or researcher). Within the STN group five subjects who did not fall before surgery experienced at least one fall after surgery, whereas the number of falls in the GPi group was either unchanged or improved (Table 2).
Table 2.
Percentage of trials in which subject fell
| Baseline |
6 mo |
||||||
|---|---|---|---|---|---|---|---|
| Site | OFF % | DOPA % | OFF % | DOPA % | DBS % | DOPA+DBS % | Stimulation |
| STN | 0 | 0 | 43 | 0 | 0 | 0 | 150 Hz, 4.2 V |
| STN | 0 | 0 | 0 | 14 | 0 | 0 | 180 Hz, 1.8 V |
| STN | 0 | 0 | 0 | 57 | 0 | 50 | 185 Hz, 2.6 V |
| STN | NA | 0 | 0 | 0 | 0 | 43 | 185 Hz, 2.6 V |
| STN | 0 | 0 | 0 | 14 | 0 | 0 | 185 Hz, 3 V |
| GPi | NA | 43 | NA | 43 | 43 | 43 | 185 Hz, 5 V |
| GPi | 0 | 14 | 0 | 0 | 0 | 0 | 150 Hz, 3.8 V |
Only subjects who fell are shown. All other subjects did not fall for any trials. NA, the subject did not complete the condition.
DISCUSSION
DBS in either the STN or GPi did not improve stepping responses to external perturbations. The results showed that step latency, step speed, step length, and the total number of steps did not improve for either group 6 mo after DBS surgery. In fact, DBS in the STN disrupted the postural preparation phase, with more lateral weight shifts prior to foot-off, which led to delays in executing the step.
Perturbations to the body during standing may be overcome with a feet-in-place response for small perturbation forces; however, as the perturbation force increases a protective step must be executed to prevent a fall. Previously we showed that turning lateral APA prior to the compensatory forward step occurred infrequently for control subjects, whereas subjects with PD had difficulty inhibiting the APA. The occurrence of APAs prior to a step indicates that a decision to step had been made. More frequent lateral weight shifts prior to foot-off may indicate a deficit in coupling the postural preparation for the step and the execution of the step itself. An emerging concept from this work is that the delay to initiate a compensatory step in PD could be due to a failure to inhibit the lateral APA, compounded with impairment in transitioning from the APA to the leg lift. The failure to switch quickly to the most appropriate motor program for large perturbations may be due to a response inhibition problem in people with PD.
Impulsive behavior and motor inhibition are generally worse in people with PD compared with healthy control subjects (Cohen et al. 2014; Obeso et al. 2011), and levodopa medication does not improve these problems (Obeso et al. 2011). The STN is well placed for a role in suppressing thalamocortical output, via the hyperdirect pathway, in order to inhibit unwanted motor responses (Aron and Poldrack 2006). DBS of the STN does appear to affect inhibitory motor control, but the literature disagrees on whether STN DBS is detrimental or beneficial. When DBS is turned “on” response inhibition is worse compared with DBS “off”, as assessed by the Stroop test (Witt et al. 2004) and go/no-go tasks (Ballanger et al. 2009; Hershey et al. 2004). In the stop-signal task (SST), where the movement response must be halted during preparation or execution phases, some studies have shown that STN DBS enhances inhibitory control by shortening the SST reaction time of arm (Mirabella et al. 2012) and finger (Swann et al. 2011; van den Wildenberg et al. 2006) movements. Other studies demonstrate more complex interactions. Ray et al. (2009) show that STN DBS improves inhibitory control in patients with initially worse SST compared with control subjects; however, when SST was initially in the range of control subjects, inhibitory responses are impaired by STN DBS (Ray et al. 2009). Furthermore, while proactive inhibition is reported to be enhanced by STN DBS (Mirabella et al. 2013; Obeso et al. 2013), reactive inhibition is worsened (Obeso et al. 2013). Together, the literature suggests that the STN affects motor inhibition through parallel pathways, which may have positive or negative effects depending on the context and the nature of the motor task.
The results of this study showed that turning the STN DBS on prolonged the initial in-place postural response before switching to the more appropriate stepping response. This delay was not evident in GPi DBS. Unfortunately, there are no studies of the effect of GPi DBS on inhibition of upper limb movements to compare with our findings. Our results indicate that there may be differential effects of STN and GPi stimulation on response inhibition in postural tasks.
Turning the stimulator on in the STN group seemed to affect the preparation phase of the step more than the execution phase, as the number of APAs increased, which in turn delayed stepping time and resulted in greater CoM displacement. In contrast, the length and speed of the first step in the STN DBS group were similar whether DBS was on or off. This suggests that DBS may be more involved in coordinating the timing between the postural and stepping programs than with the step execution itself. Although the step length and speed were not changed by DBS in STN, given that the CoM was further forward when the step was made, the step size and speed should have been scaled up to make an appropriate compensatory response. The initial step was not sufficient to halt the body's forward motion, and this explains the need for a greater number of steps. The failure to scale the postural response appropriately may be more related to the PD than the DBS. It is known that people with PD have difficulty scaling motor output according to postural feedback (Kim et al. 2009).
Five (45%) of the STN group fell more after surgery than before, whereas there was no change in the fall incidence in the GPi group. This result may help explain the higher incidence of more serious falls in the STN DBS group than the GPi DBS group in the larger multicenter trial of which these subjects were a subset (Follett et al. 2010).
A limitation of the study was the fixed sequence of conditions: DBS, OFF, DOPA, DBS+DOPA. This sequence was chosen to allow PD DBS subjects to be tested over a single day; however, it is possible that stepping responses improved with practice. However, as the final condition (DBS+DOPA) showed worsening in the STN group, it suggests that the DBS was detrimental over and above any practice effect that may have occurred.
STN DBS is often associated with a reduction in levodopa medication dose, but in the present study there was no significant reduction. The clinician who consulted with the subjects for treatment optimization may have had a cautious medication reduction approach. Although medication dose was routinely reduced if medication-induced dyskinesias were problematic, dyskinesia cannot be ruled out as a potential confounder. On the other hand, because medication dose remained similar across PD groups and between baseline and 6-mo assessments, confounding effects of medication dose variability were minimized.
Conclusions
The human balance system needs to be flexible and continuously adaptable to new conditions. The ability to inhibit and switch between motor responses quickly and to scale the motor output appropriately is affected in PD. The results of this study show that neither levodopa medication nor DBS treatments were able to improve the flexibility of the balance system in PD. In fact, there was evidence that DBS stimulation in the STN prolonged inhibition of the in-place response, thereby delaying the transition to the compensatory stepping response.
GRANTS
This research was supported by National Institute on Aging Grants AG-19706 and AG-006457 and The Parkinson Alliance.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: R.J.S.G., P.C.-K., and K.J.B. performed experiments; R.J.S.G. analyzed data; R.J.S.G., L.A.K., and F.B.H. interpreted results of experiments; R.J.S.G. prepared figures; R.J.S.G. drafted manuscript; R.J.S.G., P.C.-K., L.A.K., and F.B.H. edited and revised manuscript; R.J.S.G., P.C.-K., L.A.K., K.J.B., and F.B.H. approved final version of manuscript; P.C.-K., K.J.B., and F.B.H. conception and design of research.
ACKNOWLEDGMENTS
We thank Drs. Penelope Hogarth and Ali Saami for referring subjects from the Oregon Health and Science University and Seattle, respectively, and Triana Nagel for assisting with data acquisition.
REFERENCES
- Aron AR, Poldrack RA. Cortical and subcortical contributions to Stop signal response inhibition: role of the subthalamic nucleus. J Neurosci 26: 2424–2433, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballanger B, Eimeren TV, Moro E, Lozano AM, Hamani C, Boulinguez P, Pellecchia G, Houle S, Poon YY, Lang A, Strafella A. Stimulation of the subthalamic nucleus and impulsivity: release your horses. Ann Neurol 66: 817–824, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH. Prospective assessment of falls in Parkinson's disease. J Neurol 248: 950–958, 2001. [DOI] [PubMed] [Google Scholar]
- Burchiel K, Anderson V, Favre J, Hammerstad F. Comparison of pallidal and subthalamic nucleus deep brain stimulation for advanced Parkinson's disease: results of a randomized, blinded pilot study. Neurosurgery 45: 1375–1384, 1999. [DOI] [PubMed] [Google Scholar]
- Cohen RG, Klein KA, Nomura M, Fleming M, Mancini M, Giladi N, Nutt JG, Horak FB. Inhibition, executive function, and freezing of gait. J Parkinsons Dis 4: 111–122, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahn S, Elton R. Unified Parkinson's Disease Rating Scale. Florham Park, NJ: Macmillan Healthcare Information, 1987. [Google Scholar]
- Follett K, Weaver F, Stern M, Hur K, Harris C, Luo P, Marks W, Rothlind J, Sagher O, Moy C, Pahwa R, Burchiel K, Hogarth P, Lai E, Duda J, Holloway K, Samii A, Horn S, Bronstein J, Stoner G, Starr P, Simpson R, Baltuch G, Salles AD, Huang G, Reda D. Pallidal versus subthalamic deep-brain stimulation for Parkinson's disease. N Engl J Med 362: 2077–2091, 2010. [DOI] [PubMed] [Google Scholar]
- Hershey T, Revilla FJ, Wernle A, Gibson PS, Dowling JL, Perlmutter JS. Stimulation of STN impairs aspects of cognitive control in PD. Neurology 62: 1110–1114, 2004. [DOI] [PubMed] [Google Scholar]
- Horak FB, Dimitrova D, Nutt JG. Direction-specific postural instability in subjects with Parkinson's disease. Exp Neurol 193: 504–521, 2005. [DOI] [PubMed] [Google Scholar]
- Horak FB, Frank JS, Nutt J. Effects of dopamine on postural control in Parkinsonian subjects: scaling, set and tone. J Neurophysiol 75: 2380–2396, 1996. [DOI] [PubMed] [Google Scholar]
- Jacobs JV, Horak FB. Cortical control of postural responses. J Neural Transm 114: 1339–1348, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs JV, Nutt JG, Carlson-Kuhta P, Stephens M, Horak FB. Knee trembling during freezing of gait represents multiple anticipatory postural adjustments. Exp Neurol 215: 334–341, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr GK, Worringham CJ, Cole MH, Lacherez PF, Wood JM, Silburn PA. Predictors of future falls in Parkinson disease. Neurology 75: 116–124, 2010. [DOI] [PubMed] [Google Scholar]
- Kim S, Horak FB, Carlson-Kuhta P, Park S. Postural feedback scaling deficits in Parkinson's disease. J Neurophysiol 102: 2910–2920, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, Horak FB. Lateral stepping for postural correction in Parkinson's disease. Arch Phys Med Rehabil 89: 492–499, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, St George RJ, Carlson-Kuhta P, Nutt JG, Horak FB. Preparation for compensatory forward stepping in Parkinson's disease. Arch Phys Med Rehabil 91: 1332–1338, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIlroy WE, Maki BE. Do anticipatory postural adjustments precede compensatory stepping reactions evoked by perturbation? Neurosci Lett 164: 199–202, 1993. [DOI] [PubMed] [Google Scholar]
- Mirabella G, Iaconelli S, Modugno N, Gianniani G, Lena F, Cantore G. Stimulation of subthalamic nuclei restores a near normal planning strategy in Parkinson's patients. PLoS One 8: e62793, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirabella G, Iaconelli S, Romanelli P, Modugno N, Lena F, Manfredi M, Cantore G. Deep brain stimulation of subthalamic nuclei affects arm response inhibition in Parkinson's patients. Cereb Cortex 22: 1124–323, 2012. [DOI] [PubMed] [Google Scholar]
- Nutt JG, Burchiel KJ, Comella CL, Jankovic J, Lang AE, Laws ER Jr, Lozano AM, Penn RD, Simpson RK Jr, Stacy M, Wooten GF. Randomized, double-blind trial of glial cell line-derived neurotrophic factor (GDNF) in PD. Neurology 60: 69–73, 2003. [DOI] [PubMed] [Google Scholar]
- Obeso I, Wilkinson L, Jahanshahi M. Levodopa medication does not influence motor inhibition or conflict resolution in a conditional stop-signal task in Parkinson's disease. Exp Brain Res 213: 435–445, 2011. [DOI] [PubMed] [Google Scholar]
- Obeso I, Wilkinson L, Rodríguez-Oroz MC, Obeso JA, Jahanshahi M. Bilateral stimulation of the subthalamic nucleus has differential effects on reactive and proactive inhibition and conflict-induced slowing in Parkinson's disease. Exp Brain Res 226: 451–462, 2013. [DOI] [PubMed] [Google Scholar]
- Pickering RM, Grimbergen YA, Rigney U, Ashburn A, Mazibrada G, Wood B, Gray P, Kerr G, Bloem BR. A meta-analysis of six prospective studies of falling in Parkinson's disease. Mov Disord 22: 1892–1900, 2007. [DOI] [PubMed] [Google Scholar]
- Ray NJ, Jenkinson N, Brittain J, Holland P, Joint C, Nandi D, Bain PG, Yousif N, Green A, Stein JS, Aziz TZ. The role of the subthalamic nucleus in response inhibition: evidence from deep brain stimulation for Parkinson's disease. Neuropsychologia 47: 2828–2834, 2009. [DOI] [PubMed] [Google Scholar]
- Rocchi L, Carlson-Kuhta P, Chiari L, Burchiel KJ, Hogarth P, Horak FB. Effects of deep brain stimulation in the subthalamic nucleus or globus pallidus internus on step initiation in Parkinson disease: laboratory investigation. J Neurosurg 117: 1141–1149, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocchi L, Chiari L, Horak FB. Effects of deep brain stimulation and levodopa on postural sway in Parkinson's disease. J Neurol Neurosurg Psychiatry 73: 267–274, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St George RJ, Carlson-Kuhta P, Burchiel KJ, Hogarth P, Frank N, Horak FB. The effects of subthalamic and pallidal deep brain stimulation on postural responses in patients with Parkinson disease. J Neurosurg 116: 1347–1356, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St George RJ, Carlson-Kuhta P, Nutt JG, Hogarth P, Burchiel KJ, Horak FB. The effect of deep brain stimulation randomized by site on balance in Parkinson's disease. Mov Disord 29: 949–953, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann N, Poizner H, Houser M, Gould S, Greenhouse I, Cai W, Strunk J, George J, Aron AR. Deep brain stimulation of the subthalamic nucleus alters the cortical profile of response inhibition in the beta frequency band: a scalp EEG study in Parkinson's disease. J Neurosci 31: 5721–5729, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Wildenberg WP, van Boxtel GJ, van der Molen MW, Bosch DA, Speelman JD, Brunia CH. Stimulation of the subthalamic region facilitates the selection and inhibition of motor responses in Parkinson's disease. J Cogn Neurosci 18: 626–636, 2006. [DOI] [PubMed] [Google Scholar]
- Vaughan CL, Andrews JG, Hay JG. Selection of body segment parameters by optimization methods. J Biomed Eng 104: 38–44, 1982. [DOI] [PubMed] [Google Scholar]
- Weaver F, Follett K, Stern M, Hur K, Harris C, Marks W, Rothlind J, Sagher O, Reda D, Moy C, Pahwa R, Burchiel K, Hogarth P, Lai E, Duda J, Holloway K, Samii A, Horn S, Bronstein J, Stoner G, Heemskerk J, Huang G. Bilateral deep brain stimulation vs. best medical therapy for patients with advanced Parkinson disease. JAMA 301: 63–73, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver FM, Follett KA, Stern M, Luo P, Harris CL, Hur K, Marks WJ Jr, Rothlind J, Sagher O, Moy C, Pahwa R, Burchiel K, Hogarth P, Lai EC, Duda JE, Holloway K, Samii A, Horn S, Bronstein JM, Stoner G, Starr PA, Simpson R, Baltuch G, De Salles A, Huang GD, Reda DJ. Randomized trial of deep brain stimulation for Parkinson disease: thirty-six-month outcomes. Neurology 79: 55–65, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt K, Pulkowski U, Herzog J, Lorenz D, Hamel W, Deuschl G, Krack P. Deep brain stimulation of the subthalamic nucleus improves cognitive flexibility but impairs response inhibition in Parkinson disease. Arch Neurol 61: 697–700, 2004. [DOI] [PubMed] [Google Scholar]