Abstract
PURPOSE
We aimed to evaluate the added value of diffusion-weighted imaging (DWI) to standard magnetic resonance imaging (MRI) for detecting post-treatment cervical cancer recurrence. The detection accuracy of T2-weighted (T2W) images was compared with that of T2W MRI combined with either dynamic contrast-enhanced (DCE) MRI or DWI.
METHODS
Thirty-eight women with clinically suspected uterine cervical cancer recurrence more than six months after treatment completion were examined with 1.5 Tesla MRI including T2W, DCE, and DWI sequences. Disease was confirmed histologically and correlated with MRI findings. The diagnostic performance of T2W imaging and its combination with either DCE or DWI were analyzed. Sensitivity, positive predictive value, and accuracy were calculated.
RESULTS
Thirty-six women had histologically proven recurrence. The accuracy for recurrence detection was 80% with T2W/DCE MRI and 92.1% with T2W/DWI. The addition of DCE sequences did not significantly improve the diagnostic ability of T2W imaging, and this sequence combination misclassified two patients as falsely positive and seven as falsely negative. The T2W/DWI combination revealed a positive predictive value of 100% and only three false negatives.
CONCLUSION
The addition of DWI to T2W sequences considerably improved the diagnostic ability of MRI. Our results support the inclusion of DWI in the initial MRI protocol for the detection of cervical cancer recurrence, leaving DCE sequences as an option for uncertain cases.
Cervical cancer is the fourth most frequent cancer in women worldwide (1). Early stage disease is treated with surgery or chemoradiotherapy and has a good prognosis. However, around 30% of all patients treated for cervical carcinoma develop progressive or recurrent tumors (2).
Recurrent cervical cancer is defined as local tumor regrowth or the development of distant organ/lymph node metastases at least six months after regression of the initial lesion. Approximately two-thirds of recurrences appear within the first two years following initial treatment, with 90% recurring by five years post-treatment (3). Risk factors for recurrence include histopathologic features, depth of tumor invasion, and nodal status (4).
Pelvic recurrence can be located centrally (cervix, uterus, vagina, parametria, ovaries, bladder, or rectum) or in the pelvic sidewalls. Extrapelvic recurrence most commonly involves the para-aortic lymph nodes, lungs, liver, or bone (4–6).
Treatment of recurrent cancer depends on the primary treatment approach, location, and extension. Patients with locally recurrent disease can be offered salvage treatments with curative potential (chemoradiotherapy, if not given previously, or pelvic exenteration in patients who already received chemoradiotherapy). Distant metastases, however, are nearly always incurable (3).
In patients who successfully completed primary treatment, surveillance has been advocated to detect the residual or recurrent disease at curable stages (7). The use of imaging studies such as magnetic resonance imaging (MRI) is indicated on the basis of clinical suspicion (8).
T2-weighted (T2W) imaging is the reference sequence for cervical cancer staging (9). Recurrent tumors are known to show high signal intensity on T2W MRI, contrasting with the low signal intensity of the cervical stroma. However, some benign conditions such as necrosis, inflammation, and edema may also increase signal intensity on T2W images, representing a potential challenge to the radiologist, particularly after radiotherapy (10–13).
Moreover, post-treatment changes can result in areas of fibrosis that are also difficult to differentiate from recurrence (14). MRI has proven to be superior to computed tomography (CT) in distinguishing fibrosis and scarring from active disease, but imaging findings are sometimes indeterminate, complicating the evaluation of recurrent disease (3).
In recent years, the functional MRI techniques such as dynamic multiphase contrast-enhanced (DCE) MRI and diffusion-weighted imaging (DWI) have emerged as fundamental tools in female pelvic imaging evaluation (15). Although DCE was shown to be more accurate than T2W alone for tumor recurrence identification, the use of both sequences is recommended (10).
Recently, DWI has been added to pelvic MRI protocols to increase diagnostic accuracy in tumor staging. This technique is a functional tool that relies on tissue water displacement to create a contrasted image. For correct evaluation and avoidance of pitfalls, the generated images must be interpreted alongside anatomical sequences. The apparent diffusion coefficient (ADC) map is also needed to reduce image misinterpretation, for example due to the T2 shine-through effect (15). In highly cellular tissues, water movement is restricted and such lesions appear bright at high b-values (1000 s/mm2) and have low ADC value, appearing dark gray on ADC maps in contrast to areas of freely moving water such as urine in the bladder (14). Some recent studies have suggested that DWI and ADC maps can be potentially useful in oncologic follow-up (14, 16).
The purpose of this study was to compare the accuracy of T2W/DWI with that of conventional anatomical sequences alone and T2W/DCE imaging sequences in the evaluation of recurrent disease in patients treated for uterine cervical carcinoma.
Methods
Patient selection
This is a retrospective, institutional review board-approved single-center study. From May 2013 until July 2014, a total of 38 female patients (median age, 58 years; range, 28–85 years) with clinically suspected cervical cancer recurrence underwent standard pelvic examinations and pelvic MRI. All patients included in the study were women who had undergone treatment for cervical cancer, had completed their therapeutic regimens at least six months prior to study entry, and had clinical suspicion of tumoral recurrence.
As primary treatment, nine patients underwent hysterectomy, one received radiotherapy only, and the remaining 28 patients received combined radiochemotherapy.
Clinical suspicion of recurrence was associated with particular symptoms such as pelvic pain (n=25), metrorrhagia (n=2), hematuria (n=1), and fecaluria (n=1). The other nine patients had macroscopic lesions detected during gynecologic follow-up examinations.
Thirty-four women underwent biopsy of the suspicious lesion and four women underwent surgery for lesion excision.
MRI protocol
All MRI studies were performed on a 1.5 Tesla body scanner unit (Philips Intera Pulsar) with a pelvic phased-array coil (Synergy). Peristalsis was suppressed with 40 mg of N-butylscopolamine bromide. Superior and anterior saturation bands were used.
The pelvis was examined using axial turbo spin-echo T1-weighted sequence (TR/TE, 400 ms/10 ms; matrix size, 512×512; slice thickness, 4 mm; gap, 0.4 mm) and a set of spin-echo T2-weighted sequence (TR/TE, 5000 ms/102 ms; matrix size, 512×512; number of excitations, 2; slice thickness, 4 mm; gap, 0.4 mm) in the sagittal and axial planes. In women who did not undergo surgery as primary treatment, an additional T2W (slice thickness, 5 mm; gap, 0.5 mm) axial oblique (perpendicular to the cervical canal) sequence was performed. An axial spin-echo T2W sequence (slice thickness, 6 mm; gap, 1 mm) of the abdomen extending from the pelvic brim to the left renal vein was also performed.
Fat-suppressed T1 3D gradient echo acquisitions of the pelvis (frequency-selective suppression SPAIR—Spectral Attenuated Inversion Recovery) were obtained in the sagittal or axial plane (accordingly to the individual preferences of the performing radiologist) after a bolus injection of gadoteric acid (Dotarem, Laboratoire Guerbet) at a dose of 0.1 mmol/kg of body weight followed by a rapid infusion of normal saline solution (10 mL). Injection started after the first acquisition, and scanning was conducted at 30, 60, 90, 120, and 150 s after the injection. We also obtained a late (taken at 5 min) T1W spectral presaturation inversion recovery (SPIR) sequence in the axial plane.
In three patients, contrast-enhanced imaging was impossible due to impaired renal function (glomerular filtration rate <30 mL/min).
DWI was performed for both the abdomen and pelvis using single-shot echo-planar imaging and the array spatial sensitivity encoding technique (SENSE) (TR/TE, 3100 ms/53 ms; matrix size, 256×256; number of excitations, 3; slice thickness, 4 mm; gap, 1 mm; R factor, 2; flip angle, 90º) in the axial plane with a b-value of 0, 600, and 1000 s/mm2. The image software automatically generated ADC maps.
Image analysis
Two radiologists (with 4 and 19 years of experience in interpreting pelvic MRI) performed a consensus interpretation of all images while blinded to the histopathology reports to determine whether lesions were recognizable on T2W and DCE imaging, and also on DWI (with b=1000).
Four separate sets of images were analyzed: anatomical images only (T2W), DCE sequences, T2W and DCE sequences (T2W/DCE), and T2W and DWI sequences (T2W/DWI). To minimize any recall bias, the exams were sorted randomly and a two-week interval was present was present between interpretation sessions. T1-weighted images were also analyzed in each set to exclude potential pitfalls such as hemorrhage.
DWI sequences were not evaluated alone because of the lack of anatomical references. In the combined sets of sequences, DCE and DWI sequences were synchronized with T2W images for better lesion localization and the avoidance of pitfalls.
DWI (with b=1000) was analyzed qualitatively according to the signal intensity of uterine cervical cancer, as determined by visually comparing the signal intensity with the myometrium signal. ADC maps were also analyzed qualitatively. T2 shine-through artifacts (high signal on DWI with normal or high-signal ADC) were not considered as true restricted diffusion.
For DCE MRI, all acquisitions were analyzed together, and the early enhancements (30–90 s) of any abnormal structure, as well as isolated enhancing areas, were registered. Each observer individually recorded the presence and location of lesions in each set of images (T2W, DCE, and DWI), assigning each as: (a) “suspicious for recurrent disease” (in patients exhibiting lesions with a high signal intensity on T2W imaging compared with muscle, early contrast uptake on DCE sequence, or bright and dark areas on DWI and ADC maps); (b) “unapparent disease” (when no lesion was identifiable); or (c) “ill-defined/equivocal disease” (when there was only a slight signal elevation in an ill-defined area on T2W image, delayed contrast uptake on DCE image, or only a discrete signal elevation on b=1000 or a discrete hyposignal on the ADC map).
In the combination sets, when at least one technique was suspicious for malignancy the global result was considered suspicious for recurrent disease.
Histopathology examination
All biopsy results were reviewed by genitourinary pathologists blinded to the imaging findings.
Statistical analysis
MRI and histopathology results were correlated for each patient. A general descriptive analysis was performed for each variable. Using the histology results as a gold standard, we calculated sensitivity, positive predictive value, and accuracy for T2W and DCE imaging alone and for sequences combinations (T2W/DCE and T2W/DWI). The accuracy of the T2W sequence was compared with that of the DCE sequence and the sequence combinations (T2W/DCE and T2W/DWI) using a nonparametric test (McNemar two-tailed test). Then, a similar statistical comparison was made between the two sequence combinations. A P ≤ 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics for Windows, Version 17.0 (SPSS Inc.).
Results
Of the 38 suspicious lesions on MRI, 36 were proven to be recurrent disease on histopathologic examination and two showed no signs of neoplastic disease. The sites of recurrent disease were the cervix (n=13), vaginal vault (n=9), vaginal wall (n=4), uterine body (n=1), posterior bladder wall (n=1), and retroperitoneal lymph nodes (n=10).
Patient demographics, histology of the primary treated tumor, FIGO stage at diagnosis, and histology and location of the suspicious lesion are summarized in Table 1.
Table 1.
Patient characteristics
| Number of patients | 38 |
|
| |
| Histology of primary tumor, n (%) | |
| Squamous cell carcinoma | 34 (89.5) |
| Adenocarcinoma | 4 (10.5) |
|
| |
| FIGO stage at diagnosis, n ( %) | |
| IA | 1 (2.6) |
| IB | 2 (5.2) |
| IIA | 7 (18.4) |
| IIB | 23 (60.5) |
| IIIA | 1 (2.6) |
| IIIB | 4 (10.5) |
|
| |
| Histology of suspicious lesion, n (%) | |
| Squamous cell carcinoma | 34 (89.5) |
| Adenocarcinoma | 2 (5.25) |
| Benign | 2 (5.25) |
|
| |
| Median age at recurrence diagnosis (years) | 58 |
|
| |
| Location of the lesion suspicious of recurrence, n (%) | |
| Cervix | 13 (34.2) |
| Vaginal vault | 9 (23.7) |
| Vaginal wall | 4 (10.5) |
| Uterine body | 1 (2.6) |
| Posterior bladder wall | 1 (2.6) |
| Retroperitoneal lymph nodes | 10 (26.3) |
FIGO, International Federation of Gynecology and Obstetrics.
Table 2 depicts the concordance between the MRI analyses and the histology results. For each image set, the sensitivity, positive predictive value, and accuracy for lesion detection are also presented.
Table 2.
Performance of each MRI technique separately and in combination
| T2W | DCE | T2W/DCE | T2W/DWI | |
|---|---|---|---|---|
| n | 38 | 35 | 35 | 38 |
| TP/correctly identified | 28 (73.7) | 28 (80) | 28 (80) | 33 (86.8) |
| FP/incorrectly identified | 2 (5.3) | 2 (5.7) | 2 (5.7) | 0 (0) |
| TN/correctly rejected | 0 (0) | 0 (0) | 0 (0) | 2 (5.3) |
| FN/incorrectly rejected | 8 (21.0) | 5 (14.3) | 5 (14.3) | 3 (7.9) |
| Unable to perform | 0 | 3 | 3 | 0 |
| PPV, TP/(TP+FP) | 93.3 | 93.3 | 93.3 | 100 |
| Sensitivity, TP/(TP+FN) | 77.8 | 84.8 | 84.8 | 91.7 |
| Accuracy, (TP+TN)/total | 73.6 | 80 | 80 | 92.1 |
| P (comparison with T2W) | - | 1.000 | 1.000 | 0.016 |
Data are presented as n (%).
T2W, T2-weighed; DCE, dynamic contrast-enhanced; DWI, diffusion-weighted imaging; n, number of patients; TP, true positive; FP, false positive; TN, true negative; FN, false negative; PPV, positive predictive value.
T2W sequences correctly depicted 28 tumoral recurrences via hyperintensity criteria. Four lesions were misclassified as “unapparent disease” because they were isointense/slightly hypointense and four were misclassified as “ill-defined/equivocal disease” because there was only a slight signal elevation that was difficult to differentiate from the normal myometrium (Fig. 1). Two patients were erroneously classified as having “recurrent disease” due to focal cervical (Fig. 2) and retroperitoneal lymph node hyperintensity.
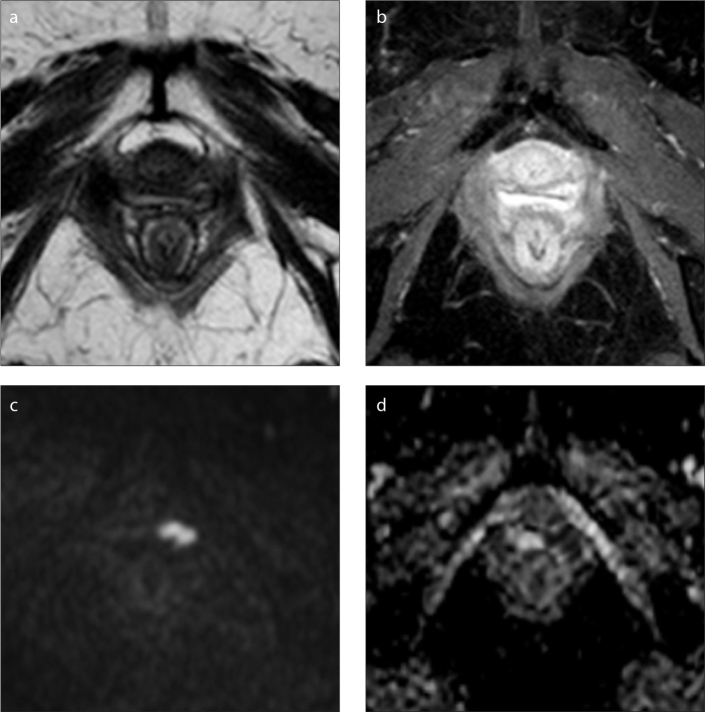
Figure 1.
a–d. MRI in the axial plane of the pelvis denoting vaginal recurrence of endometrioid adenocarcinoma of the cervix (initial stage IIB) treated with chemoradiotherapy. On T2-weighted (a) and dynamic contrast-enhanced (DCE) (b) MRI sequences, no obvious lesion was identified. On diffusion-weighted imaging (DWI) with b=1000 s/mm2 (c), the tumor is clearly defined with a hypersignal and low signal on the apparent diffusion coefficient (ADC) map (d).
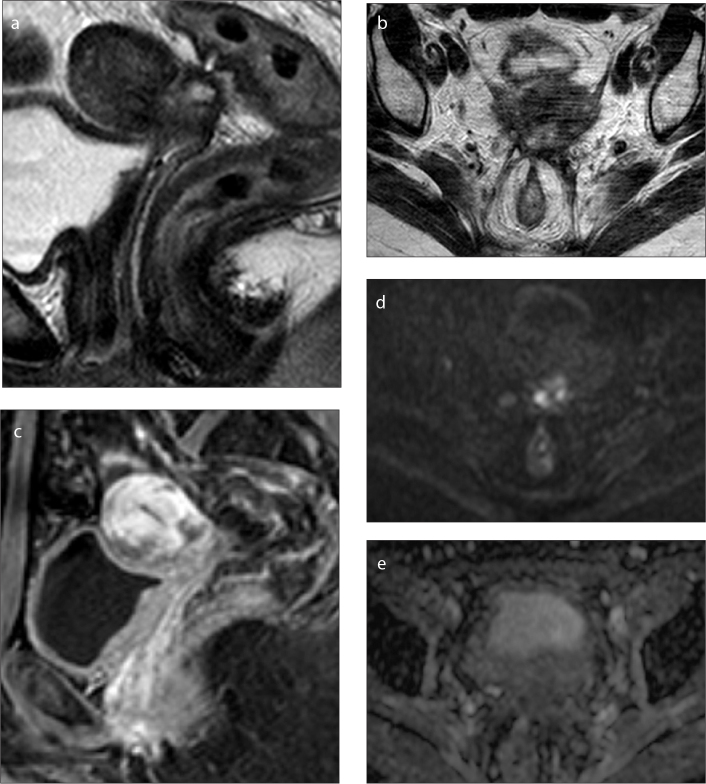
Figure 2.
a–e. Pelvic MRI of a 42-year-old patient who underwent chemoradiotherapy for cervical cancer that ended one year ago (initial stage IIB). On sagittal (a) and axial (b) T2-weighted images an irregular cervical nodular lesion is identified with necrotic center and ill-defined intermediate signal on the periphery. On sagittal DCE MRI (c) an early heterogeneous peripheral enhancement is seen. On axial DWI with b=1000 s/mm2 (d) the lesion shows diffuse hyperintense signal, mainly due to central necrosis and there is no peripheral low signal on the correspondent ADC map (e) denoting T2 shine-through effect, without evidence of restricted diffusion. Histopathology examination revealed only inflammatory changes.
Only 35 patients underwent DCE sequence since a contrast-enhanced study was impossible in three patients due to kidney function impairment. Considering all DCE acquisitions for each patient, 28 malignant lesions were identified. Of these, 27 lesions had also been depicted on T2W imaging. The last lesion was only defined after contrast administration. Four malignant lesions showed no significant early contrast uptake and were classified as “unapparent disease,” and another with just discrete contrast uptake was considered equivocal. Two lesions with early contrast enhancement were benign on histopathologic work-up (false positive findings). There was no statistically significant difference between the accuracy of T2W and DCE imaging (P > 0.05).
The T2W/DCE imaging combination correctly classified 28 lesions as malignant. The addition of contrast allowed for the correct identification of one additional lesion in a patient with an enhancing focal area not seen on the morphologic (T2W) sequence. However, one patient with a suspicious lesion on T2W imaging could not be evaluated with DCE MRI (due to contraindications to contrast administration) and was therefore not included in the statistical analysis of this combination. Combined T2W/DCE imaging was unable to exclude malignancy in two women with clinical suspicion of recurrent disease (both complaining of pelvic pain) but only benign changes on pathologic analysis. There was no statistically significant difference between the accuracies of T2W and T2W/DCE imaging (P > 0.05).
When evaluating the combined imaging findings of T2W/DWI, 33 of the recurrent tumors were correctly identified (Fig. 3).
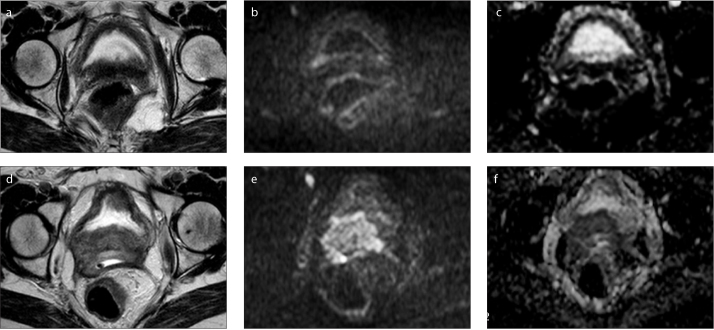
Figure 3.
a–f. Pelvic MRI of a 55-year-old patient who underwent chemoradiotherapy for cervical cancer (initial stage IIIB) with central recurrent disease after treatment. On axial T2-weighted image performed four years after treatment (a), no lesion was promptly identifiable, although DWI with b=1000 (b) showed a small focal area of hyperintensity on the right posterior bladder wall with a discrete hyposignal on the ADC map (c) that was not promptly considered relevant by the clinicians. After this examination, a targeted biopsy was performed confirming recurrence of cervical squamous cell carcinoma (this first evaluation was the one included in our study). The patient refused treatment for personal reasons and one year later, a hyperintense heterogeneous cervical mass with right posterior bladder invasion is readily visible on T2-weighted image (d) along with a high signal on DWI with b=1000 s/mm2 (e) and a low signal on the ADC map (f).
The two disease-free women who were misclassified using the T2W/DCE sequences were correctly categorized as “unapparent disease” with this combination. Three lesions were unapparent (Fig. 4). There was no statistically significant difference in accuracy between the T2W/DCE and T2W/DWI combinations (P > 0.05). However, the difference in diagnostic accuracy between T2W imaging and T2W/DWI was statistically significant (P = 0.016).
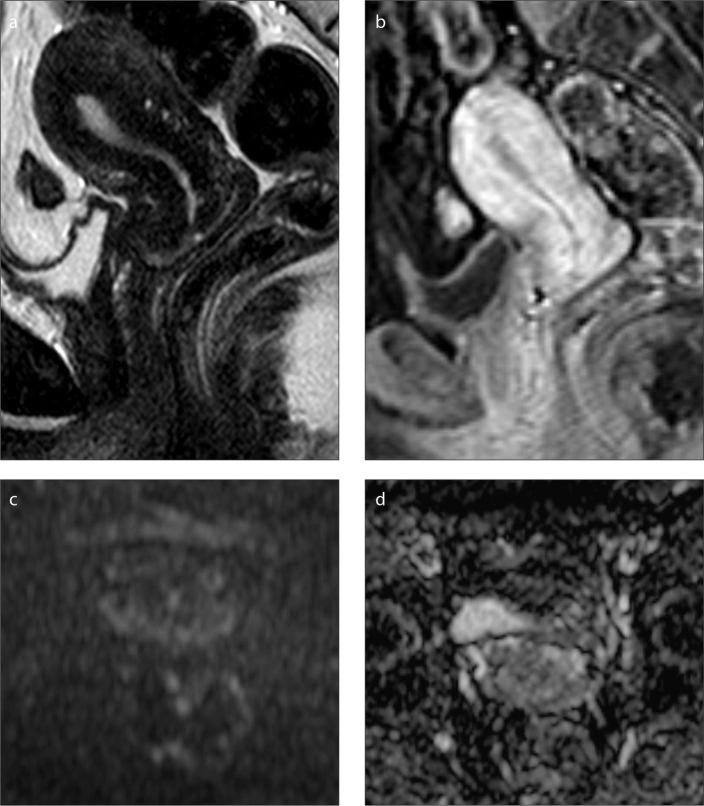
Figure 4.
a–d. Pelvic MRI of a 59-year-old patient who underwent chemoradiotherapy for cervical cancer that ended two years ago (initial stage IIB). No lesion is depicted on either sagittal T2-weighted (a) or DCE (b) images. In addition, no hyperintense lesion is seen on axial DWI with b=1000 s/mm2 (c) or on the corresponding ADC map (d). However, due to on-going pelvic pain, the patient underwent a cervical biopsy that was positive for recurrence of cervical squamous cell carcinoma.
These results support the assumption that the rates of tumor recurrence detection are similar between a complete multi-parametric MRI study (combination of morphologic sequences with DCE and DWI) and a combination of T2W/DWI.
Discussion
In our study, the combination T2W/DWI had a positive predictive value of 100% and an accuracy of 92.1% for recurrent disease detection, while both T2W imaging alone and the combination T2W/DCE MRI registered values of 93.3% and 80%, respectively. Also there were no false positive findings with T2W/DWI.
The identification of a recurrent tumor has a major impact on the survival outcomes of patients treated for cervical cancer. Imaging is undertaken only in the presence of suspicious clinical symptoms. However, residual disease is difficult to evaluate and the accuracy of MRI depends on the time elapsed since the end of therapy, as local inflammatory or fibrotic phenomena may hamper accurate diagnosis (7, 11, 14, 17, 28).
Conventional MRI has a high sensitivity but low specificity for recurrent disease detection. Thus, the added value provided by functional MRI is becoming increasingly important in oncologic diagnosis, particularly in gynecologic cancers, where newer applications have been gaining ground (18, 19).
In DCE MRI, a dynamic image acquisition is performed after the administration of an intravenous bolus of gadolinium-based contrast agent. The paramagnetic contrast molecules lead to changes in local field strength and thus reflect the tumor microvascular network (20). Typically, cervical tumors enhance avidly in the early dynamic phase compared with the slight enhancement of the cervical epithelium and stroma, which may allow for the distinction of recurrent tumors from radiation fibrosis (21). However, the use of gadolinium-based contrast media is limited in patients with kidney impairment (patients with glomerular filtration rates <30 mL/min, patients on dialysis, and patients with acute kidney insufficiency), as well as in cases of allergy requiring medical treatment, pregnancy, or patient refusal (22).
DWI is a noninvasive technique based on molecular diffusion that, combined with conventional T2W imaging, enables the assessment of morphologic and physiologic changes in a single examination. It also allows for a quantitative evaluation of ADC from images with different b-values (15, 23, 24). DWI can provide excellent tissue contrast, making it an excellent choice in cases where contrast administration is not possible. Furthermore, the additional scanning time is relatively short.
Numerous studies have described the use of DWI for the diagnosis and staging of cervical cancer (3, 9, 14–16, 23, 25, 26). However, only few studies have analyzed the utility of DWI in assessing early tumor response to treatment (4, 17, 24, 27). To our knowledge, there are no published data on the use of DWI for cervical tumor recurrence detection and no studies have compared DCE MRI and DWI in this field.
We recognize that pelvic DWI is an extremely motion-sensitive sequence plagued by artefacts related to arterial pulsation, bowel peristalsis, and susceptibility effects. However, advances in hardware and sequences have contributed to the minimization of these effects, increasing the use of DWI in pelvic pathology (26). It is also well known that high b-value images have low anatomical detail, but this can be overcome by fusing the images with anatomical sequences to optimize anatomical correlation. These fused images can be displayed in inverted grey-scale or arbitrary color-coded scales (15).
In our study, T2W imaging alone could identify recurrent tumors with a sensitivity of 77.8%. Histopathology examinations of the false negative patients revealed squamous cell carcinoma cells involved by abundant fibrous tissue. This may justify the absence of a high signal on T2W imaging, especially considering that six of these patients have had chemoradiotherapy, which is known to decrease tumor signal intensity on MRI (28, 29).
These results are concordant with the work of Hricak et al. (12), who found that tumors with intense desmoplastic reactions demonstrate a low signal on T2W imaging. In addition, Kinkel et al. (10) found that the presence of both fibrosis and tumor cells in the same lesion could justify the lower signal intensity on T2W imaging, with a higher reported T2W imaging sensitivity (91.4%). However, this study included other gynecologic cancers besides cervical cancer, which can explain this difference. On the other hand, all the false negative lesions in their study were from patients treated for cervical cancer, reflecting the difficulties in establishing this diagnosis.
In this study, in cases where the morphologic sequences failed to identify tumor recurrence, DCE MRI could correctly identify only one additional lesion. This was in a patient treated with chemoradiotherapy who showed an early enhancing area in the vaginal wall that was ill-defined and difficult to depict on T2W imaging, probably due to the presence of radiation-induced fibrosis precluding higher signal intensity on T2W imaging.
Three patients could not undergo a contrast-enhanced study due to kidney impairment (in one of these patients a tumoral lesion was readily identified on T2W imaging) and five patients remained incorrectly diagnosed (false negative). This did not represent a significant difference in sensitivity between these two sequences. Sala et al. (15) also concluded that DCE MRI was not necessary during staging, as it could not improve accuracy compared with T2W imaging alone, which increased our confidence. In the Kinkel et al. study (10) based on subtraction DCE MRI, there was also no increment in sensitivity with contrast-enhanced studies compared with anatomical sequences only. However, tumor identification accuracy was superior with contrast, with maximum tumor enhancement occurring between 45 and 90 s after contrast administration (10). In our study, all patients with early enhancement (30–90 s) were histologically proven.
Among lesions that did not show early enhancement (false negative), two were recurrences in the vaginal vaults of hysterectomized patients who received neoadjuvant chemotherapy and three were cervical lesions in patients who completed chemoradiotherapy at least two years ago. On pathology, all these lesions revealed abundant fibrous stroma with scant microscopic tumor foci. The former may be related to post-surgical fibrosis, whereas the latter may be due to post-radiotherapy vasculopathy, which affects the microvasculature of irradiated fields and thereby limits the early enhancing capacity of these lesions (12).
We found that the two false-positive findings on T2W imaging remained false positive after the addition of DCE MRI. Histopathologic examination of these patients revealed inflammatory changes, necrosis, and hyperemia in a cervical lesion of a patient who completed chemoradiotherapy one year ago and an enlarged retroperitoneal lymph node with inflammatory changes and increased vessel density in a patient who underwent hysterectomy 18 months prior. Engin (28) reviewed postirradiation changes in pelvic organs and found that sometimes the tumoral signal decrease typical of radiation therapy may be delayed, and a high-signal-intensity stroma may persist longer (28). In the study by Hricak et al. (12), there was also nonspecific enhancement of the cervix after radiation therapy related to benign changes such as postirradiation fibrosis, inflammation, and necrosis. Furthermore, in another paper by Hawighorst et al. (13), the visual inspection of a lesion’s contrast enhancement alone was considered unhelpful in establishing a malignancy diagnosis because of nonspecific tissue changes that can show similar enhancement. In contrast with these works, Kinkel el al. (10) found that DCE MRI is helpful in improving the specificity and accuracy of tumor recurrence detection. They also proved that in the first five months after radiation therapy, induced inflammatory changes are known to be responsible for early enhancement that mimics recurrence. We believe that this effect may be prolonged in some patients.
In our study, we observed that the combination of T2W imaging and DWI could predict tumor recurrence with a higher sensitivity than the combination of T2W and DCE MRI (91.7% vs. 84.8%). The addition of DWI to T2W imaging allowed five patients to be reclassified as having a recurrent tumor.
On the other hand, the two false-positive patients with bright lesions on T2W imaging and early enhancement after contrast administration did not show water restriction on DWI, denoting the absence of high cellularity of these benign changes (Fig. 3). These results are in concordance with those of Chen et al. (26), who found that patients without disease after treatment showed no residual hyperintense lesions in the cervical areas on DWI.
The three cases that remained falsely negative on all sequences represented biopsy-proven local recurrences of well-differentiated squamous carcinoma that did not show marked restricted diffusion, probably due to their low cellularity (30).
Globally, in this study, the accuracy was 73.6% for T2W imaging, 80% for DCE MRI, 80% for combined T2W/DCE MRI, and 92.1% for combined T2W/DWI.
Our study had several limitations. First, our population was small and had a high prevalence of recurrence, which could lead to the overestimation of sensitivity and render the estimation of specificity impossible. Second, DWI was assessed only qualitatively by inspecting signal intensity, as there is no established ADC value that is diagnostic for neoplastic tissue (because imaging parameters change from center to center, making standardization almost impossible). Third, contrast could not be administered in three patients, thus the entire patient sample could not undergo evaluation with the T2W/DCE MRI combination. However, this is also a limitation in everyday practice, which reinforces the role of DWI as an alternative to contrasted studies in tumoral recurrence follow-up. Fourth, the patient group is not homogeneous with regard to therapeutic options that may have conditioned the appearance of pelvic structures on follow-up MRI. This point warrants further studies with larger samples. Finally, there is inhomogeneity regarding recurrence site, but this actually represents the pattern of cervical cancer recurrence, which can have a local or regional distribution in the form of pelvic or para-aortic adenopathy (28).
In conclusion, although we recognize that our data are presented on the basis of preliminary observations that are sustained by histopathologic confirmation and a significant difference on statistical analysis, we hypothesize that in follow-up study of patients treated for cervical cancer, contrast administration can be omitted from the initial protocol. We hereby support the notion that an initial follow-up protocol for treated cervical cancer can consist of a T2W/DWI combination, which can save both time and money. DCE MRI would only be performed if the radiologist remained uncertain regarding the diagnosis.
Main points.
Recurrent cervical cancer is defined as tumor regrowth or the development of metastases, at least six months after regression of the initial lesion.
Recurrent tumors are known to show high signal intensity on T2W imaging, but also necrosis, inflammation and edema. Post-treatment changes can result in areas of fibrosis that are also difficult to differentiate from recurrence.
The addition of DCE MRI improves T2W imaging sensitivity, however, sometimes it is not possible to administer contrast, e.g., due to kidney function impairment.
The rates of tumoral detection were higher with the combination of T2W/DWI sequences.
The initial MRI protocol for the detection of cervical cancer recurrence could consist of the combination of T2W imaging and DWI, leaving DCE MRI as an option.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Ferlay J, Soerjomataram I, Ervik M, et al. IARC cancer base no. 11. International Agency for Research on Cancer; Lyon, France: 2013. [Accessed on June 8, 2014]. GLOB-OCAN 2012 v 1.0, Cancer incidence and mortality worldwide. Available at: http://globocan.iarc.fr. [Google Scholar]
- 2.Long HJ. Management of metastatic cervical cancer: review of the literature. J Clin Oncol. 2007;10:2966–2974. doi: 10.1200/JCO.2006.09.3781. http://dx.doi.org/10.1200/JCO.2006.09.3781. [DOI] [PubMed] [Google Scholar]
- 3.Liyanage SH, Roberts CA, Rockall AG. MRI and PET scans for primary staging and detection of cervical cancer recurrence. Womens Health (Lond Engl) 2010;6:251–267. doi: 10.2217/whe.10.7. http://dx.doi.org/10.2217/whe.10.7. [DOI] [PubMed] [Google Scholar]
- 4.Schieda N, Malone SC, Dandan OA, Ramchandani P, Siegelman ES. Multi-modality organ-based approach to expected imaging findings, complications and recurrent tumour in the genitourinary tract after radiotherapy. Insights Imaging. 2014;5:25–40. doi: 10.1007/s13244-013-0295-z. http://dx.doi.org/10.1007/s13244-013-0295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gadducci A, Tana R, Cosio S, Cionini L. Treatment options in recurrent cervical cancer (Review) Oncol Lett. 2010;1:3–11. doi: 10.3892/ol_00000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fulcher AS, O’Sullivan SG, Segreti EM, Kavanagh BD. Recurrent cervical carcinoma: typical and atypical manifestations. Radiographics. 1999;19:103–116. doi: 10.1148/radiographics.19.suppl_1.g99oc19s103. http://dx.doi.org/10.1148/radiographics.19.suppl_1.g99oc19s103. [DOI] [PubMed] [Google Scholar]
- 7.Salani R, Backes FJ, Fung MF, et al. Posttreatment surveillance and diagnosis of recurrence in women with gynecologic malignancies: Society of Gynecologic Oncologists recommendations. Am J Obstet Gynecol. 2011;204:466–478. doi: 10.1016/j.ajog.2011.03.008. http://dx.doi.org/10.1016/j.ajog.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Koh WJ, Greer BE, Abu-Rustum NR, et al. Cervical cancer. J Natl Compr Canc Netw. 2013;11:320–343. doi: 10.6004/jnccn.2013.0043. [DOI] [PubMed] [Google Scholar]
- 9.Togashi K, Nishimura K, Sagoh T, et al. Carcinoma of the cervix: staging with MR imaging. Radiology. 1989;171:245–251. doi: 10.1148/radiology.171.1.2928532. http://dx.doi.org/10.1148/radiology.171.1.2928532. [DOI] [PubMed] [Google Scholar]
- 10.Kinkel K, Ariche M, Tardivon AA, et al. Differentiation between recurrent tumor and benign conditions after treatment of gynecologic pelvic carcinoma: value of dynamic contrast-enhanced subtraction MR imaging. Radiology. 1997;204:55–63. doi: 10.1148/radiology.204.1.9205223. http://dx.doi.org/10.1148/radiology.204.1.9205223. [DOI] [PubMed] [Google Scholar]
- 11.Antunes D, Cunha TM. Recurrent cervical cancer: how can radiology be helpful. OMICS J Radiology. 2013;2:138. [Google Scholar]
- 12.Hricak H, Swift PS, Campos Z, Quivey JM, Gildengorin V, Göranson H. Irradiation of the cervix uteri: value of unenhanced and contrast-enhanced MR imaging. Radiology. 1993;189:381–388. doi: 10.1148/radiology.189.2.8210364. http://dx.doi.org/10.1148/radiology.189.2.8210364. [DOI] [PubMed] [Google Scholar]
- 13.Hawighorst H, Knapstein PG, Schaeffer U, et al. Pelvic lesions in patients with treated cervical carcinoma: efficacy of pharmacokinetic analysis of dynamic MR images in distinguishing recurrent tumors from benign conditions. AJR Am J Roentgenol. 1996;166:401–408. doi: 10.2214/ajr.166.2.8553955. http://dx.doi.org/10.2214/ajr.166.2.8553955. [DOI] [PubMed] [Google Scholar]
- 14.Nougaret S, Tirumani SH, Addley H, Pandey H, Sala E, Reinhold C. Pearls and pitfalls in MRI of gynecologic malignancy with diffusion-weighted technique. AJR Am J Roentgenol. 2013;200:261–276. doi: 10.2214/AJR.12.9713. http://dx.doi.org/10.2214/AJR.12.9713. [DOI] [PubMed] [Google Scholar]
- 15.Sala E, Rockall A, Rangarajan D, Kubik-Huch RA. The role of dynamic contrast-enhanced and diffusion weighted magnetic resonance imaging in the female pelvis. Eur J Radiol. 2010;76:367–385. doi: 10.1016/j.ejrad.2010.01.026. http://dx.doi.org/10.1016/j.ejrad.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 16.Thoeny HC, De Keyzer F. Extracranial applications of diffusion-weighted magnetic resonance imaging. Eur Radiol. 2007;17:1385–1393. doi: 10.1007/s00330-006-0547-0. http://dx.doi.org/10.1007/s00330-006-0547-0. [DOI] [PubMed] [Google Scholar]
- 17.Vincens E, Balleyguier C, Rey A, et al. Accuracy of magnetic resonance imaging in predicting residual disease in patients treated for stage IB2/II cervical carcinoma with chemoradiation therapy: correlation of radiologic findings with surgicopathologic results. Cancer. 2008;113:2158–2165. doi: 10.1002/cncr.23817. http://dx.doi.org/10.1002/cncr.23817. [DOI] [PubMed] [Google Scholar]
- 18.Mahajan M, Kuber R, Chaudhari KR, Chaudhari P, Ghadage P, Naik R. MR imaging of carcinoma cervix. Indian J Radiol Imaging. 2013;23:247–252. doi: 10.4103/0971-3026.120257. http://dx.doi.org/10.4103/0971-3026.120257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaur H, Silverman PM, Iyer RB, Verschraegen CF, Eifel PJ, Charnsangavej C. Diagnosis, staging and surveillance of cervical carcinoma. AJR Am J Roentgenol. 2003;180:1621–1632. doi: 10.2214/ajr.180.6.1801621. http://dx.doi.org/10.2214/ajr.180.6.1801621. [DOI] [PubMed] [Google Scholar]
- 20.O’Connor JPB, Tofts PS, Miles KA, Parkes LM, Thompson G, Jackson A. Dynamic contrast-enhanced imaging techniques: CT and MRI. Br J Radiol. 2011;84:S112–S120. doi: 10.1259/bjr/55166688. http://dx.doi.org/10.1259/bjr/55166688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hricak H, Swift PS, Campos Z, Quivey JM, Gildengorin V, Goranson H. Irradiation of the cervix uteri: value of unenhanced and contrast-enhanced MR imaging. Radiology. 1993;189:381–388. doi: 10.1148/radiology.189.2.8210364. http://dx.doi.org/10.1148/radiology.189.2.8210364. [DOI] [PubMed] [Google Scholar]
- 22.European Society of Urogenital Radiology. ESUR guidelines on contrast media. version 8.1. 2013. [Accessed Jan 2014]. Available at: http://www.esur.org/esur-guidelines/
- 23.Namimoto T, Awai K, Nakaura T, Yanaga Y, Hirai T, Yamashita Y. Role of diffusion-weighted imaging in the diagnosis of gynecological diseases. Eur Radiol. 2009;19:745–760. doi: 10.1007/s00330-008-1185-5. http://dx.doi.org/10.1007/s00330-008-1185-5. [DOI] [PubMed] [Google Scholar]
- 24.Levy A, Caramella C, Chargari C, et al. Accuracy of diffusion-weighted echo-planar MR imaging and ADC mapping in the evaluation of residual cervical carcinoma after radiation therapy. Gynecol Oncol. 2011;123:110–115. doi: 10.1016/j.ygyno.2011.06.009. http://dx.doi.org/10.1016/j.ygyno.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 25.McVeigh PZ, Syed AM, Milosevic M, Fyles A, Haider MA. Diffusion-weighted MRI in cervical cancer. Eur Radiol. 2008;18:1058–1064. doi: 10.1007/s00330-007-0843-3. http://dx.doi.org/10.1007/s00330-007-0843-3. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Zhang Y, Liang B, Yang Z. The utility of diffusion-weighted MR imaging in cervical cancer. Eur J Radiol. 2010;74:e101–106. doi: 10.1016/j.ejrad.2009.04.025. http://dx.doi.org/10.1016/j.ejrad.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 27.Harry VN, Semple SI, Gilbert FJ, Parkin DE. Diffusion-weighted magnetic resonance imaging in the early detection of response to chemoradiation in cervical cancer. Gynecol Oncol. 2008;111:213–220. doi: 10.1016/j.ygyno.2008.07.048. http://dx.doi.org/10.1016/j.ygyno.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 28.Engin G. Cervical cancer: MR imaging findings before, during, and after radiation therapy. Eur Radiol. 2006;16:313–324. doi: 10.1007/s00330-005-2804-z. http://dx.doi.org/10.1007/s00330-005-2804-z. [DOI] [PubMed] [Google Scholar]
- 29.Addley HC, Vargas HA, Moyle PL, Crawford R, Sala E. Pelvic imaging following chemotherapy and radiation therapy for gynecologic malignancies. Radiographics. 2010;30:1843–1856. doi: 10.1148/rg.307105063. http://dx.doi.org/10.1148/rg.307105063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whittaker CS, Coady A, Culver L, Rustin G, Padwick M, Padhani AR. Diffusion-weighted MR Imaging of female pelvic tumors: a pictorial review. Radiographics. 2009;29:759–778. doi: 10.1148/rg.293085130. http://dx.doi.org/10.1148/rg.293085130. [DOI] [PubMed] [Google Scholar]