Abstract
PURPOSE
A second opinion is a valuable resource in confirming proper medical diagnosis and treatment. This study evaluates the effectiveness of second-opinion radiology consultations to reassess the cervical spine computed tomography (CT) scans of the trauma patients referred to our hospital.
METHODS
Cervical spine CT scans of 301 consecutive adult trauma patients, who were referred to our hospital from outside institutions, were analyzed. The emergency radiologists at our institution completed the over-read reports on the CT images obtained at the outside facilities. A single radiologist compared the outside- and over-read reports and determined the discrepancy of the radiologic reports.
RESULTS
Based on the outside reports, 31% of the CT scans had cervical traumatic injury. In 92% of patients, the first-read and the over-read reports had consistent radiologic findings. About 90% of the positive, and 93% of the negative radiologic findings, were reported consistently in the over-read reports. Our analysis showed that the over-read reporting resulted in reassurance of negative findings in 63%; confirmation of positive findings in 29%; clearing a false diagnosis in 3%; and detection of a missed diagnosis in 5%. A rescan was done in 80% of patients with inconsistent and 20% of patients with consistent findings (P < 0.05). The most common missed radiologic findings in the first-reports were transverse and spinous process fractures and the most common misdiagnoses were dens fractures.
CONCLUSION
For a service offering second-opinion consultations on cervical spine trauma, review of outside CT studies improves diagnosis and benefits patient care.
The quality of healthcare has become a target of increasing public scrutiny and governmental concern while radiologic evaluation has assumed an increasingly important role in the diagnosis and management of patients (1). Public attention and awareness have increased and amplified the focus on the quality of healthcare (2). Some medical errors are extremely costly particularly with respect to patient morbidity and mortality.
Patients referred to the tertiary care centers often arrive with radiologic imaging having already been performed at the primary institution. As part of the care to be delivered by the radiologists at the referral center, a second-opinion interpretation of the imaging studies is often requested, and the formal reports are incorporated into the patient’s permanent medical record at the referral institution where the patient’s management and treatment are determined.
The added value of the point-of-care second interpretations can be viewed from the medical perspective of guiding and expediting appropriate treatment as well as from the financial perspective of avoiding unnecessary studies, at times incurring additional patient radiation exposure, when initial examinations need to be repeated or when additional examinations are suggested by the radiologist at an outside institution (3).
Multidetector CT is an essential part of the assessment of patients suspected of having cervical spine injury after trauma. Despite all the advantages of multidetector CT, suspected spinal injury continues to be a daily challenge in clinical practice (4). Spine injuries are frequently missed; therefore, a second opinion can potentially improve the diagnosis (5). The purpose of this study was to evaluate the effectiveness of second-opinion radiology consultations to reassess the cervical spine CT scans of the trauma patients referred to our hospital.
Methods
We performed a retrospective analysis of 301 consecutive cases with cervical spine CT who were referred to our institution, over a period of 16 months from March 2011 to July 2012. The inclusion criteria were: 1) patients with a cervical spine CT at an outside facility with available radiology report, 2) adults (age ≥18 years), 3) having a history of trauma as an indication for requesting cervical spine CT, and 4) request to the radiology service (by the referring physician in our hospital) for a second-opinion consultation on the outside CT scans. This study followed the Health Insurance Portability and Accountability Act guidelines and was approved by our institutional review board.
Patients’ data were obtained using QPID (queriable patient inference dossier), which is a health intelligence platform incorporating an electronic health record search engine in our hospital. The CT images of the patients were imported to our picture archiving and communication system and the subspecialty-trained emergency radiologists in our hospital completed the over-read reports on the outside CT images.
Cervical spine injuries were categorized according to the classification by Harris and Mirvis (with aggregation of some of the small groups) (6). A single emergency radiologist (GC, 10 years of experience in radiology) compared the outside and the over-read reports. The outcome of over-read reporting of the cervical spine CT scans were classified as: a) reassurance of negative findings (i.e., reassurance for patients and the responding clinicians when both the outside and over-read showed negative trauma-related injury); b) confirmation of positive findings (where both the outside and over-read showed a similar trauma-related injury); c) clearing a false diagnosis (where the over-read showed that the outside read reported an injury that was not really a trauma-related injury); and d) showing a missed finding (where the over-read showed a trauma-related injury that was not reported in the outside report). Additionally, the over-read reports were classified as inconsistent or consistent with the outside reports. Inconsistency between the first and over-read reports (the c + d categories) was defined when a trauma-related injury was not reported in the outside report (missed finding/diagnosis) or there was a misdiagnosis in the outside read; i.e., the outside radiologist reported an injury, whereas in the over-read it turned out to be not related to trauma (false positive initial reads, e.g., a normal variant, an artifact, or a misdiagnosis).
The radiologists’ recommendations in the over-read were categorized as no recommendation; recommendation for rescan, or scan with a different modality. Data of these scans (with CT or a different modality such as MRI or CT angiography) were recorded. The data of discharge or admission to hospital was also recorded. Patients were admitted to hospital due to trauma to cervical spine or other injuries. We recorded if the patients were admitted for cervical spine injury (SI), or for other causes (O).
Statistical analysis
The statistical analysis was performed using SPSS software (version 19.0; IBM Corp.). Variables are expressed as mean and standard deviation (SD), or number and percentage. Categorical variables were compared using chi square analysis or Fisher’s Exact test as appropriate. The level of significance was set at P < 0.05.
Results
A total of 301 consecutive patients were analyzed (females: n=114, 38%). The patients’ age ranged from 18 to 97 years (mean: 56.4±23.1 years). The mechanism of injury was due to motor-vehicle accident in 56% (n=168), falls in 30% (n=89), and others (e.g., sport, assault) in 15% (n=44).
Characteristics of the patients are summarized in Table 1. Based on the outside reports, 31% of the cervical spine CT scans had an acute traumatic injury. The C1 injuries, dens, transverse process, and burst fractures had the highest frequency among the injuries. In 10 patients over-read was not performed by our radiology service due to inadequate imaging or poor image quality (e.g., thick slices or no sagittal/coronal reconstructions). These patients were not considered for further analysis.
Table 1.
Characteristics of the patients (n=301)
| Variables | n (%) |
|---|---|
| Age, years (mean±SD) | 56.4±23.1 |
|
| |
| Gender (females) | 114 (37.8) |
|
| |
| Injury type | |
| 1) No traumatic injury | 198 (65.8) |
| 2) Traumatic injurya | 93 (30.9) |
| C1 fracture (including anterior/posterior arch and Jefferson burst fracture) | 18 (6.0) |
| Traumatic spondylolisthesis of C2 (including Hangman’s fracture) | 12 (4.0) |
| Dens fracture | 14 (4.6) |
| Flexion-teardrop fracture | 14 (4.6) |
| Extension-teardrop fracture | 8 (2.6) |
| Burst fracture | 22 (7.3) |
| Compression fracture | 18 (6.0) |
| Hyperextension-dislocation | 5 (1.7) |
| Hyperflexion-anterior subluxation | 7 (2.3) |
| End-plate fracture | 6 (1.9) |
| Facetal fracture/dislocation | 12 (4.0) |
| Laminar fracture | 10 (3.3) |
| Osteophyte fracture | 6 (1.9) |
| Spinous process fracture | 13 (4.3) |
| Transverse process fracture | 16 (5.3) |
| Atlantoaxial dislocation | 3 (1.0) |
|
| |
| No over-read: request for rescan | |
| 1) Inadequate imaging | 7 (2.3) |
| 2) Poor image quality | 3 (1.0) |
|
| |
| Report comparison (outside vs. over-read)b | |
| 1) Consistent reports | 268 (92.1) |
| Reassurance of negative findings | 184 (63.2) |
| Confirmation of positive findings | 84 (28.9) |
| 2) Inconsistent reports | 23 (7.9) |
| Clearing a false diagnosis (misdiagnosis) | 9 (3.1) |
| Showing a missed finding/diagnosis | 14 (4.8) |
Based on the outside report. The aggregate percentage is more than 100% because of co-occurrence of injuries.
The percentages are calculated in patients for whom over-read was performed.
The first-read and the over-read reports had consistent findings in about 92% of patients and inconsistent radiologic findings in 8%. Our analysis showed that the over-read reporting resulted in reassurance of negative findings in 63%; confirmation of positive findings in 29%; clearing a false diagnosis in 3%; and detection of a missed diagnosis in 5% (Fig. 1). About 90% (84 out of 93) of the positive and 93% (184 out of 198) of the negative radiologic findings were reported consistently in the over-read reports. Figs. 2 and 3 show two examples where the over-read reporting revealed a missed finding or misdiagnosis in the outside reports.
Figure 1.
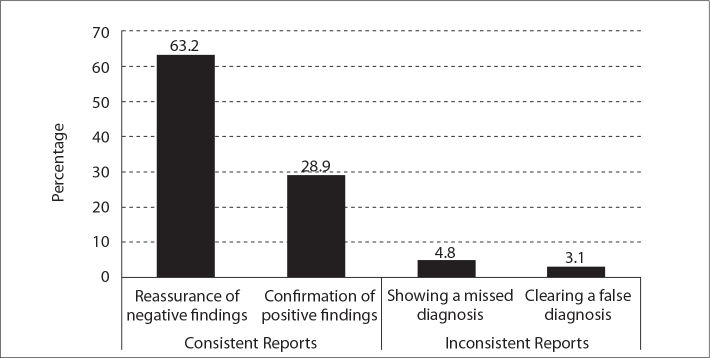
Outcome of second-opinion radiologic assessment. Our analysis showed that the over-read reporting of the cervical spine CT scans (n=291) resulted in reassurance of negative findings (n=184, 63.2%), confirmation of positive findings (n=84, 28.9%), clearing of false diagnoses (n=9, 3.1%), and detection of missed diagnoses (n=14, 4.8%).
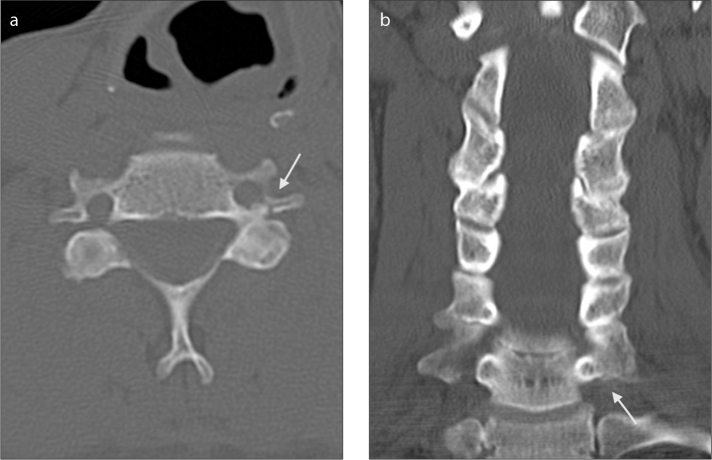
Figure 2.
a, b. Coronal (a) and sagittal (b) CT images represent the os odontoideum (arrow). A 58-year-old male had pain in the neck following a trivial fall. The outside CT radiologist reported odontoid fracture. Second opinion did not consider fracture and suggested os odontoideum. No further scan was recommended by our radiologist and the patient was safely discharged.
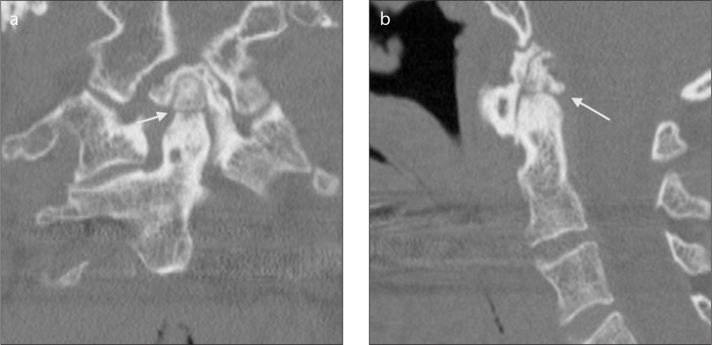
Figure 3.
a, b. Axial (a) and coronal (b) CT images represents the transverse process fracture (arrow) at C7 level. A 55-year-old male suffering from seizure disorder had a fall and injured his head. Outside CT scan reported no fracture. Second opinion picked up fracture through C7 transverse process on left side that passed through transverse foramen. Patient was admitted. As fractures involving transverse foramen have high chances of vertebral artery injury, a CT angiography of neck was considered; however, no left vertebral artery injury was found.
Table 2 shows the list of different missed findings, and misdiagnoses in the outside reports. The most common missed radiologic findings in the outside reports were transverse and spinous process fractures, and the most common misdiagnoses were dens fractures. After second-opinion assessment, all patients with misdiagnosed trauma-related spinal injuries were either discharged or admitted to hospital due to other causes (not related to cervical spine injury) (Table 2).
Table 2.
The list of misdiagnoses and missed findings and their admission/discharge outcome (n=23)
| Findings | n (%) | Admission/discharge* |
|---|---|---|
| Misdiagnoses revealed after over-read (n=9) | ||
| False fracture report of os odontoideum | 2 (8.7) | Discharged |
| False fracture report of a lucent line due to limbus vertebrae | 1 (4.3) | Admitted (O) |
| False report of C1 fracture (accessory ossicle) | 1 (4.3) | Admitted (O) |
| False report of dens fracture | 2 (8.7) | Discharged, n=1; admitted (O), n=1 |
| False report of endplate fracture | 1 (4.3) | Admitted (O) |
| False report of facet dislocation | 1 (4.3) | Discharged |
| False report of laminar fracture | 1 (4.3) | Discharged |
|
| ||
| Missed findings revealed after over-read (n=14) | ||
| Unilateral facet dislocation | 1 (4.3) | Admitted (SI) |
| Laminar fracture | 2 (8.7) | Admitted (SI), n=1; admitted (O), n=1 |
| Spinous process fracture | 3 (13) | Discharged, n=2; admitted (SI), n=1 |
| Transverse process fracture | 5 (17.4) | Discharged, n=2; admitted (SI), n=1; admitted (O), n=2 |
| Dens fracture | 2 (8.7) | Admitted (SI) n=1; discharged, n=1 |
| Endplate fracture | 1 (4.3) | Admitted (SI), n=1 |
Defined as admission to hospital due to cervical spine injury or other causes, or discharge.
O, other causes; SI, cervical spine injury.
Overall, 67% of patients were admitted and 33% were discharged. Table 3 shows results of comparison between consistent and inconsistent reports. The radiologist recommendation for rescan was significantly higher in patients with inconsistent findings compared with those with consistent findings (80% vs. 8%, P < 0.05). In inconsistent reports, the findings of the rescans confirmed the over-read reports in all cases. There were no significant differences in the degenerative findings between the two groups.
Table 3.
Comparison between consistent and inconsistent reports
| Variables | Inconsistent reports (n=23) | Consistent reports (n=268) |
|---|---|---|
| Radiologist’s recommendation | ||
| Rescans with CT | 16 (70) | 21 (8) |
| Scan with a different modality | 1 (4) | 5 (2) |
|
| ||
| Degenerative findings | 6 (26) | 62 (23) |
|
| ||
| Rescans | 18 (78) | 51 (19) |
| CTa | 14 (78)b | 16 (31)b |
| MRIa | 4 (22)b | 35 (70)b |
|
| ||
| Admission/discharge outcome | ||
| Admissionc | 13 (56) | 189 (71) |
| Discharge | 10 (43) | 79 (29) |
Data are presented as n (%).
P < 0.05 when comparing consistent and inconsistent reports.
Percentage is calculated in patients with rescan.
The admissions were due to cervical spine injury or other causes.
Discussion
The primary aim for second-opinion services is benefiting patients by maximizing their medical care; or sometimes providing reassurance by reinforcing that their current treatment is the best option (7, 8). Patients or referring physicians often seek a second opinion to research treatment options or reconfirm a diagnosis. Our results demonstrated that over-read reporting of cervical spine CT scans could show a missed finding or a misdiagnosis in 8% of cases referred for a second-opinion assessment. In the rest of patients the radiology reassessment could provide reassurance and confirmation of the findings (reporting consistent findings).
Cervical spine fractures can be classified based on their anatomical location (anterior and posterior column), mechanism of injury (hyperflexion/rotation, hyperextension/rotation, axial compression, lateral flexion, others) and degree of mechanical instability (e.g., odontoid fracture, Hangman fracture, Jefferson fracture, fracture with anterior subluxation, fracture with unilateral and bilateral facetal dislocation, vertebral body burst fracture) (6, 9–11). Assessment of cervical spine injuries plays a major role in evaluation of trauma patients. Cervical spine fractures are associated with an unfavorable outcome, especially in the elderly population, regardless of other associated traumatic injuries or spinal cord injury (12). This study showed that in trauma patients the most common missed radiologic findings in the cervical spine CT scans were the transverse and spinous process fractures and the most common misdiagnoses were dens fractures.
Several factors play as potential pitfalls in cervical spine CT imaging in a trauma setting (13). The normal variants, imaging artifacts, inadequate imaging, missing a finding by the radiologist, underestimating the extent of the fracture, and under-reporting a multilevel fracture, contribute to these pitfalls. Our study showed that in a trauma setting, where the radiologist is actively looking for a fracture in the CT images, a normal variation or a preexisting pathology could be misdiagnosed for fracture.
The cervical spine CT for evaluation of trauma is associated with several incidental findings (14). An os odontoideum or a limbus vertebra can mimic a fracture (15, 16). A fracture of C1 anterior arch can be mimicked by an accessory ossicle. For C1 fractures, congenital fusion anomalies and aplasias may simulate fracture (e.g., incomplete fusion of C1 posterior arch). These are identified from fracture by their smooth well-corticated margins. Degenerative changes may be confused with traumatic subluxation. In contrast to traumatic anterior subluxation, retrolisthesis is the usual consequence of cervical spondylosis because of normal cervical lordosis and posterior inclination of the articular facets. Degenerated facet joints are most commonly narrowed, with thinning of the bony facet from long-term wear. In traumatic subluxations, however, the facet joints are often abnormally widened. An artifact can also mimic a fracture. In these cases, a rescan can bring reassurance (17). Calcification of the alar ligament is also reported to mimic facture of cervical spine (18).
As part of the second-opinion assessments, patients were rescanned with CT or other modalities based on the recommendation of the radiologists or an order from the referring physician. There was a significantly higher number of rescans in patients with inconsistent reports (80%) compared with consistent reports (20%). This suggests that inconsistency of the radiology reports warrants more radiologic work-ups and possibly more radiation exposure to patients.
Our study showed that all patients with misdiagnosed spinal injuries were either discharged or admitted to hospital due to other causes (not related to cervical spine injury). This finding may point to the impact of the radiologic reassessments on the outcome of these patients. We should note that the over-read reporting of the cervical spine CT scans was part of the whole diagnostic work-up for these trauma patients. Patients had hospital admission/discharge due to various medical/surgical causes that we did not look into.
As a limitation for this study, it was not possible for us to directly evaluate the effect of changes in the radiology reports (misdiagnoses and missed findings) on patients’ admission/discharge outcome. This was mainly because there were many other medical/surgical factors that could effect on patients’ admission/discharge. A thorough assessment of the clinical significance of the missed findings or misdiagnoses, identified in the second-opinion reassessments, requires longitudinal prospective studies. Our retrospective study could not directly evaluate the clinical significance of the discrepancies between the reports. Another limitation was that we did not over-read the scans that were reported by the radiologists in our center. We considered the over-read reports in our hospital as a reference to measure the accuracy of the first reports. There is however, a very low possibility for a significant cervical injury to be missed or misdiagnosed by two radiologists, especially when the second radiologist is an experienced attending in a tertiary-care teaching hospital. A cost-effective study can be conducted to evaluate the role of second-opinion services in the referral hospitals and provide insight on potential ways to improve the effectiveness of these services. Studies on second-opinion assessments can provide educational insights on the areas where radiologists can potentially miss a diagnosis or finding.
In conclusion, for a service offering second-opinion consultations on cervical spine trauma, review of outside CT studies improves diagnosis and benefits patient care. Radiologic reassessments of the cervical spine CT scans can provide reassurance or confirmation of findings or demonstrate misdiagnoses or missed findings. More research on the effectiveness of second-opinion services can provide educational insight on the circumstances that may lead to overseeing, misdiagnosis, or misinterpretation of radiologic findings.
Main points.
Obtaining a second opinion on a cervical spine CT scan from the radiologists in a tertiary care hospital could provide reassurance and confirm the findings, or demonstrate misdiagnoses or missed findings.
Inconsistent radiology reports could be found in about 8% of the cervical spine CT scans after a second opinion assessment.
The most common missed radiological findings in cervical spine CT scans are transverse and spinous process fractures and the most common misdiagnoses are dens fractures.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency department transfer patients. J Am Coll Radiol. 2009;6:626–632. doi: 10.1016/j.jacr.2009.04.010. http://dx.doi.org/10.1016/j.jacr.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Al-Assaf AF, Bumpus LJ, Carter D, Dixon SB. Preventing errors in healthcare: a call for action. Hosp Top. 2003;81:5–12. doi: 10.1080/00185860309598022. http://dx.doi.org/10.1080/00185860309598022. [DOI] [PubMed] [Google Scholar]
- 3.Eakins C, Ellis WD, Pruthi S, et al. Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. AJR Am J Roentgenol. 2012;199:916–920. doi: 10.2214/AJR.11.7662. http://dx.doi.org/10.2214/AJR.11.7662. [DOI] [PubMed] [Google Scholar]
- 4.Munera F, Rivas LA, Nunez DB, Jr, Quencer RM. Imaging evaluation of adult spinal injuries: emphasis on multidetector CT in cervical spine trauma. Radiology. 2012;263:645–660. doi: 10.1148/radiol.12110526. http://dx.doi.org/10.1148/radiol.12110526. [DOI] [PubMed] [Google Scholar]
- 5.Zen E, Yousem DM, Carone M, Lewin JS. Second-opinion consultations in neuroradiology. Radiology. 2010;255:135–141. doi: 10.1148/radiol.09090831. http://dx.doi.org/10.1148/radiol.09090831. [DOI] [PubMed] [Google Scholar]
- 6.Harris JH, Mirvis SE. The radiology of acute cervical spine trauma. Philadelphia: Lippincott Williams & Wilkins; 1996. [Google Scholar]
- 7.West OC. Second opinion readings on outside studies: Should we bother? Appl Radiol. 2012;41:6. [Google Scholar]
- 8.Cheng T, Dumire R, Golden S, Gregory J. Impact on patient care of discordance in radiology readings between external overnight radiology services and staff radiology readings at a level 1 trauma center. Am J Surg. 2013;205:280–283. doi: 10.1016/j.amjsurg.2012.10.017. http://dx.doi.org/10.1016/j.amjsurg.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Van Goethem JW, Maes M, Ozsarlak O, van den Hauwe L, Parizel PM. Imaging in spinal trauma. Eur Radiol. 2005;15:582–590. doi: 10.1007/s00330-004-2625-5. http://dx.doi.org/10.1007/s00330-004-2625-5. [DOI] [PubMed] [Google Scholar]
- 10.Trafton PG. Spinal cord injuries. Surg Clin North Am. 1982;62:61–72. doi: 10.1016/s0039-6109(16)42634-4. [DOI] [PubMed] [Google Scholar]
- 11.Kalantar SB. Fractures of the C1 and C2 vertebrae. Sem Spine Surg. 2013;25:23–35. http://dx.doi.org/10.1053/j.semss.2012.07.002. [Google Scholar]
- 12.Golob JF, Jr, Claridge JA, Yowler CJ, Como JJ, Peerless JR. Isolated cervical spine fractures in the elderly: a deadly injury. J Trauma. 2008;64:311–315. doi: 10.1097/TA.0b013e3181627625. http://dx.doi.org/10.1097/TA.0b013e3181627625. [DOI] [PubMed] [Google Scholar]
- 13.Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539–560. doi: 10.1148/rg.233025121. http://dx.doi.org/10.1148/rg.233025121. [DOI] [PubMed] [Google Scholar]
- 14.Barboza R, Fox JH, Shaffer LE, Opalek JM, Farooki S. Incidental findings in the cervical spine at CT for trauma evaluation. AJR Am J Roentgenol. 2009;192:725–729. doi: 10.2214/AJR.08.1420. http://dx.doi.org/10.2214/AJR.08.1420. [DOI] [PubMed] [Google Scholar]
- 15.Klimo P, Jr, Coon V, Brockmeyer D. Incidental os odontoideum: current management strategies. Neurosurg Focus. 2011;31:E10. doi: 10.3171/2011.9.FOCUS11227. http://dx.doi.org/10.3171/2011.9.FOCUS11227. [DOI] [PubMed] [Google Scholar]
- 16.Huang PY, Yeh LR, Tzeng WS, et al. Imaging features of posterior limbus vertebrae. Clin Imaging. 2012;36:797–802. doi: 10.1016/j.clinimag.2012.01.031. http://dx.doi.org/10.1016/j.clinimag.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 17.Sugimoto Y, Ito Y, Shiozaki Y, Shimokawa T, Mazaki T. Motion induced artifact mimicking cervical dens fracture on the CT scan: a case report. Asian Spine J. 2012;6:216–218. doi: 10.4184/asj.2012.6.3.216. http://dx.doi.org/10.4184/asj.2012.6.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Che Mohamed SK, Abd Aziz A. Calcification of the alar ligament mimics fracture of the craniovertebral junction (CVJ): an incidental finding from computerized tomography of the cervical spine following trauma. Malays J Med Sci. 2009;16:69–72. [PMC free article] [PubMed] [Google Scholar]