Abstract
PURPOSE
We aimed to establish the first diagnostic reference levels (DRLs) for computed tomography (CT) examinations in adult and pediatric patients in Turkey and compare these with international DRLs.
METHODS
CT performance information and examination parameters (for head, chest, high-resolution CT of the chest [HRCT-chest], abdominal, and pelvic protocols) from 1607 hospitals were collected via a survey. Dose length products and effective doses for standard patient sizes were calculated from the reported volume CT dose index (CTDIvol).
RESULTS
The median number of protocols reported from the 167 responding hospitals (10% response rate) was 102 across five different age groups. Third quartile CTDIvol values for adult pelvic and all pediatric body protocols were higher than the European Commission standards but were comparable to studies conducted in other countries.
CONCLUSION
The radiation dose indicators for adult patients were similar to those reported in the literature, except for those associated with head protocols. CT protocol optimization is necessary for adult head and pediatric chest, HRCT-chest, abdominal, and pelvic protocols. The findings from this study are recommended for use as national DRLs in Turkey.
Computed tomography (CT) scanners have been used in diagnostic radiology since the early 1970s and have gained popularity worldwide owing to their substantial and life-saving clinical benefits. However, the increase in the use of CT applications has led to the emergence of radiologic concerns, such as cancer risk, because of the incremental collective effective dose (ED) associated with its use. Even if the number of CT exams is small among all radiography procedures, a large proportion of medical radiation exposure comes from CT applications. CT contributes the biggest part of radiation from medical sources in the United States (~66%), United Kingdom (~47%), and Germany (~60%) (1, 2). Owing to these concerns, protection of patients of all age groups from the effects of unnecessary and harmful radiation has become a priority in CT examinations (1–3).
Dose constraint is one of the fundamental radiation protection principles; however, this cannot be applied in radiologic examinations (3). Therefore, the optimization principle has become increasingly important and needs to be performed with considerable attention in medical practice. Comparison of CT application parameters and patient radiation doses with diagnostic reference levels (DRLs) is a recommended method often considered the first step for optimization in CT examinations (4). Medical practitioners utilize national DRLs as an indicator of dose, in accordance with hospital CT protocols. When patient doses exceed the national DRL, CT examinations should be re-evaluated and optimized (5). The establishment of DRLs for individual countries has been recommended by international organizations such as the International Commission on Radiological Protection (ICRP) and the European Commission (EC) (6–8).
The justification of CT examinations may necessitate the willingness of radiology personnel to participate in decision-making regarding the use of radiographic examinations; however, more important input may be derived from the optimization of scanning protocols. Patient radiation doses originating from radiologic examinations can exhibit large variations, even when they are performed in the same hospital department (9, 10). The existence of DRLs for specific radiologic examinations enables standardization across the majority of patients. However, DRLs are neither realistic boundaries for CT technicians nor are they regarded as an indicator of good medical practice. Determination of actual dose levels for targeted patient groups and attempts to maintain radiation exposure below the DRLs may reduce the detrimental health effects associated with radiologic procedures (11, 12).
A recent study performed in Turkey investigated patients who underwent CT examinations while pregnant, unbeknownst to the patient and technicians. Mean patient radiation doses from abdominal CT examinations were reported to be approximately three-fold higher than those published in the literature (13). Therefore, there is an urgent need for establishment of national DRLs and for the optimization of CT scanning protocols. In 2012, there were more than 1600 CT devices used in Turkey and a technical report from the country’s national authority revealed that there is insufficient information concerning radiation doses from CT devices (14).
Methods
Institutional approval from Turkey’s national authority was granted prior to the study. Since no patient information was collected or revealed in this study, ethical committee approval was not required (15).
Data accumulation process
The study was conducted in two phases: a survey data collection period followed by data analysis. For better understanding the procedure, single-phase CT scanning of the relevant body region of head, chest (including high-resolution CT of the chest [HRCT-chest]), abdomen and pelvic regions were called as “protocols.” Since CT scanning protocols vary according to target body region and clinical scenario, single-phase studies were preferentially selected for evaluation in this study. The survey form was sent to hospitals in Turkey, along with written instructions.
The survey form comprised of two parts. The first part collected the following information: hospital name, address, production year of the CT equipment, number of patients who underwent examinations for each protocol in 2013, number of examined patients, and scanned body regions. Protocol parameters including name and contact information of the person who provided the information, scanning mode (axial or helical), kV, mA, slice thickness and gap, rotation time, beam collimation, pitch value, and CT dose index (CTDIvol) were recorded in the second part of the survey. In each survey, radiology departments provided 25 protocol parameters for five different age groups (<1 years, 1 to <5 years, 5 to <10 years, 10 to <15 years, and adults [≥15 years], n=5 per age group).
In 2013, a total of 1607 institutions provided a CT clinical service. Surveys were sent to every private or governmental health facility in Turkey without randomization; data were collected over a one-year period. In total, 200 hospitals (108 state hospitals and 92 private hospitals) responded to the survey. CT examination parameters were reported by 167 of 200 hospitals that responded to the survey. The remaining 33 hospitals were not eligible for evaluation. The number of CT examinations performed by responding hospitals ranged from 251 to 11,308 (mean, 10,606) in 2013, out of 734,962 for the whole country. Between 49 and 79 (mean±standard deviation, 60±9) hospitals did not correctly report all of the examination parameters for adult or pediatric patients for some of their protocols. The remaining information was analyzed even if the data was incomplete, but only if it still contained sufficient information for investigatory purpose (mean number of protocols, 103; range, 88–114). Despite attempts to collect the protocol parameters in detail, CTDIvol was the only suitable parameter for homogenized analysis of the cohort. The remaining parameters, including dose length product (DLP), were discarded owing to incompatibility or irrelevancy.
Data analysis
For each of the 167 CT scanners, the CTDIvol values for five different protocols, in each of the five age groups, were evaluated by descriptive statistics. The DLP (in mGy.cm) related to each CTDIvol value was calculated by multiplying the scan length and CTDIvol. The EDs for each protocol were estimated by multiplying the DLP with region-specific normalized ED coefficients (mSv mGy−1 cm−1) (16).
Standard patient body sizes and scan lengths for each age group and body region were adapted from previously published studies (16, 17); further information is presented in Appendix 1. The minimum, maximum, SD, median, mean, and the first, second, and third quartiles were calculated for CTDIvol, DLP, and EDs using Statistical Package for the Social Sciences (SPSS) software (SPSS for Windows, version 16.0, SPSS Inc.). The third quartiles of CTDIvol, DLP, and ED values were compared with the DRL values recommended by the EC and/or those reported in the published literature.
Results
The number of hospitals reporting on five different body region CT protocols (head, abdominal, chest, HRCT-chest, and pelvic) ranged from 88 to 114 (mean, 102) (Table 1). Since some of the institutions did not disclose scanning parameters for all age groups (mainly due to limited patient numbers, particularly for specific age groups, or lack of protocols for specific body regions), protocol information was not always equal to the number of CT equipment. There were 49 to 75 missing protocols (mean, 60 protocols) across the different age groups.
Table 1.
Hospital participation in the survey according to CT protocols and age groups
| Number of hospitals providing information for protocols of | |||||
|---|---|---|---|---|---|
| Age group | Head | Chest | HRCT-chest | Abdominal | Pelvic |
| Adult | 95 | 96 | 89 | 96 | 95 |
|
| |||||
| 10–15 years | 113 | 113 | 95 | 113 | 105 |
|
| |||||
| 5–10 years | 114 | 114 | 92 | 114 | 99 |
|
| |||||
| 1–5 years | 110 | 110 | 88 | 110 | 96 |
|
| |||||
| <1 year | 122 | 121 | 92 | 121 | 104 |
CT, computed tomography; HRCT-chest; high-resolution computed tomography of the chest.
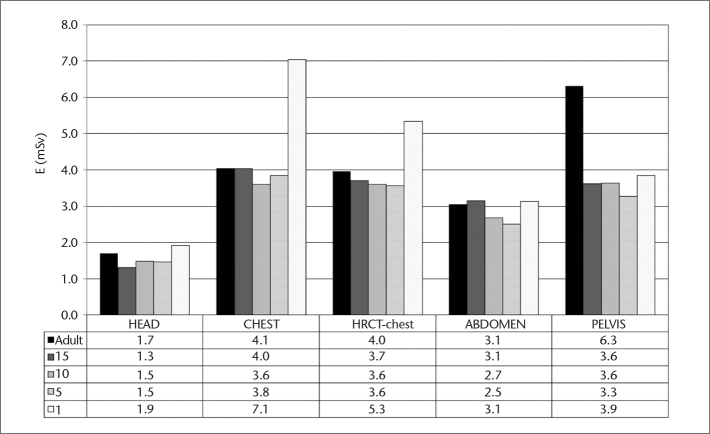
CT dose parameters for the five different protocols including the reported CTDIvol, calculated DLPs and EDs (tube output data), and the number of respondent institutions for all age groups are presented in Appendix 2. The first, second, and third quartiles of the dose values are presented for a broad representation of the country. The third quartile CTDIvol values for each of the protocols, across the five age groups, compared with similar published studies from different countries, are presented in Fig. 1. For adult patients, third quartile CTDIvol values for head, chest, HRCT-chest, abdominal, and pelvic CT examinations were 66.4, 11.6, 11.3, 13.3, and 19.4 mGy, respectively (Table 2). These results were comparable to international reference levels and were consistent with similar published studies, with the exception of the pelvic protocol.
Figure 1.
Third quartile volume CT dose index values for adult and pediatric CT examinations in Turkey. CTDI, CT dose index; HRCT-chest, high-resolution CT of the chest.
Table 2.
Accumulated third quartile CTDIvol (mGy) results for adult and pediatric patients from Turkey (n=25) and other countries
| Adult examinations | Turkey 2014 | Syria (18) 2009 | Italy (22) 2014 | UK (17) 2003 | Ireland (20) 2012 | Luxembourg (12) 2014 |
|---|---|---|---|---|---|---|
| Head | 66.4 | 60.7 | 69 | 70 | 66.2 | 52.2 |
| Chest | 11.6 | 22 | 15 | 13 | 9.3 | 6.8 |
| HRCT-chest | 11.3 | 30.5 | - | 22 | 6.6 | - |
| Abdominal | 13.3 | 24.1 | 18 | 20 | 12.3 | 9.6 |
| Pelvic | 19.4 | 27.5 | 18 | 17 | 12.3 | - |
| Pediatric examinations | <1 year | 1–5 years | 5–10 years | 10–15 years | ||
| Head (Turkey) | 31 | 33.4 | 40.3 | 51.3 | ||
| Head (Kenya) (19) | 35/30 | 50/45 | 65/50 | - | ||
| Head (Ireland) (20) | 33 | 40 | 50 | - | ||
| Head (Germany) (30) | 30 | 40 | 50 | - | ||
| Head (Switzerland) (26) | 35 | 43 | 49 | - | ||
| Chest (Turkey) | 13.6 | 13.5 | 13.5 | 11.5 | ||
| HRCT-chest (Turkey) | 10.7 | 12.6 | 13.5 | 10.6 | ||
| Chest (Kenya) (19) | 6 | 6.5 | 10 | - | ||
| Chest (Ireland) (20) | 1.7 | 2.7 | 4.3 | - | ||
| Chest (Germany) (30) | 3 | 5.5 | 5.5 | - | ||
| Chest (Switzerland) (26) | 4.2 | 4.7 | 4.5 | - | ||
| Abdominal (Turkey) | 13 | 13.1 | 14.3 | 13.7 | ||
| Pelvic (Turkey) | 11.1 | 12 | 13.6 | 16 | ||
| Abdomen (Ireland) (20) | 2.5 | 4 | 6.5 | - | ||
| Abdomen (Germany) (30) | 4 | 4.5 | 7 | - | ||
| Abdomen (Switzerland) (26) | 3.9 | 5.5 | 4.8 | - | ||
CTDIvol, volume computed tomography dose index; mGy, milligray; UK, United Kingdom; HRCT-chest, high-resolution computed tomography of the chest.
Comparison of pediatric CTDIvol results from Turkey with those from other countries is presented in Table 2. The third quartile CTDIvol value for pediatric head CT examinations was consistent with previous studies which investigated all ages, but not with those which investigated pediatric age groups (<1 year, 1–5 years, and 5–10 years). The CTDIvol values were higher in Turkey compared with similar published studies in other countries (Table 2).
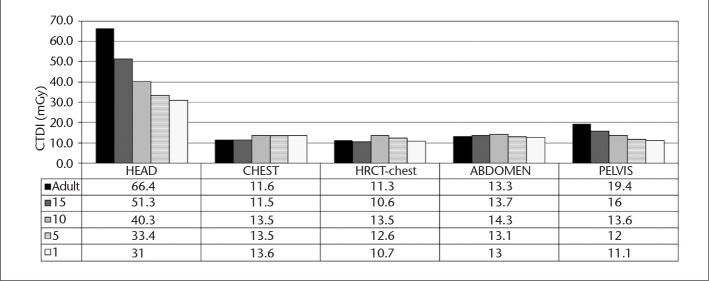
Third quartile DLP values for adult and pediatric CT examinations in Turkey are presented in Fig. 2 and comparison of these values with those from other countries is presented in Table 3. All adult findings from Turkey were consistent with the studies published in other countries (17–22). Pediatric patient findings were also consistent with similar published studies (19–21, 23–26), except for DLP values, which were higher in Turkey.
Figure 2.
Third quartile dose length product values for adult and pediatric CT examinations in Turkey. HRCT-chest, high-resolution CT of the chest; DLP, dose length product.
Table 3.
Third quartile dose length product (mGy.cm) results for adult and pediatric patients from Turkey (n=25) and other countries
| Adult examinations | Turkey 2014 | Syria (18) 2009 | Italy (22) 2014 | UK (17) 2003 | Ireland (20) 2012 | EC (21) 2011 |
|---|---|---|---|---|---|---|
| Head | 810 | 793 | 1312 | 760 | 940 | 733 |
| Chest | 289 | 520 | 569 | 430 | 393 | 394 |
| HRCT-chest | 283 | 133 | - | 80 | 276 | - |
| Abdominal | 204 | 721 | 555 | 510 | 598 | 464 |
| Pelvic | 421 | 542 | 360 | - | 598 | 434 |
| Pediatric examinations | <1 year | 1–5 years | 5–10 years | 10–15 years | ||
| Head (Turkey) | 288 | 368 | 467 | 625 | ||
| Head (Kenya) (19) | 270 | 470 | 620 | 620 | ||
| Head (Germany) (30) | 250 | 450 | 650 | 700 | ||
| Head (Switzerland) (26)* | 213 | 332 | 451 | 805 | ||
| Chest (Turkey) | 181 | 214 | 277 | 287 | ||
| HRCT-chest (Turkey) | 137 | 199 | 277 | 265 | ||
| Chest (Kenya) (19) | 6 | 6.5 | 10 | - | ||
| Chest (Germany) (30) | - | 100 | 300 | 800 | ||
| Chest (Switzerland) (26)* | 85 | 161 | 178 | 366 | ||
| Abdominal (Turkey) | 104 | 125 | 179 | 210 | ||
| Abdominal (Germany) (30) | - | 150 | 400 | 750 | ||
| Abdominal (Switzerland) (26)* | 107 | 238 | 308 | 398 | ||
| Pelvic (Turkey) | 128 | 164 | 242 | 241 | ||
UK, United Kingdom; EC, European Commission; HRCT-chest, high-resolution computed tomography of the chest.
Reference 26 reported mean values instead of third quartiles.
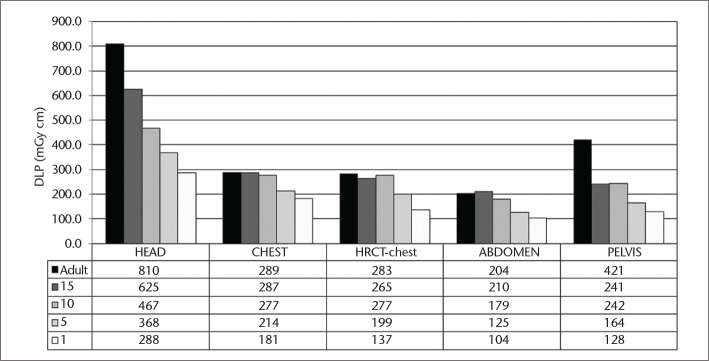
Third quartile ED results for adult and pediatric CT examinations in Turkey are presented in Fig. 3 and comparison of these findings with other countries is displayed in Table 4. For adults, the ED findings were comparable between Turkey and those reported in the literature from other countries (18, 23, 27–30). For pediatric patients, the EDs from chest, abdominal, and pelvic examinations were higher in Turkey than those reported in some of the published literature (17, 29–34), with the exception of pediatric head examinations, which were lower.
Figure 3.
Third quartile effective dose values for adult and pediatric CT examinations in Turkey. HRCT-chest, high-resolution CT of the chest.
Table 4.
Adult and pediatric effective dose (mSv) results from Turkey and other countries
| Adult examinations | Turkey 2014 | Syria (18) 2009 | Italy (28) 2014 | UK (17) 2003 | Ireland (20) 2012 | Greece (29) 2003 | Germany (30) 2001 |
|---|---|---|---|---|---|---|---|
| Head | 1.7 | 1.2 | 1.7 | 1.5 | 1.6 | 2.1 | 1.8 |
| Chest | 4.1 | 5.4 | 8 | 5.8 | 6.2 | 7.3 | 6.5 |
| HRCT-chest | 4.0 | - | - | - | - | - | - |
| Abdominal | 3.1 | 7.7 | 7.8 | 5.3 | 8.3 | 7.4 | - |
| Pelvic | 6.3 | 6.8 | 8.9 | - | 8.2 | 10.3 | 8 |
| Pediatric examinations | <1 year | 1–5 years | 5–10 years | 10–15 years | |||
| Head (Turkey) | 1.9 | 1.5 | 1.5 | 1.3 | |||
| Head (Germany) (30) | 3.6 | 2.4 | 2.0 | 1.4 | |||
| Head (USA) (32) | 2.3 | 1.5 | 1.7 | - | |||
| Head (UK) (17) | 2.5 | 1.5 | 1.6 | - | |||
| Chest (Turkey) | 7.1 | 3.8 | 3.6 | 4.0 | |||
| HRCT-chest (Turkey) | 5.3 | 3.6 | 3.6 | 3.7 | |||
| Chest (USA) (32) | 1.8 | 2.1 | 3.2 | 4.1 | |||
| Chest (Germany) (30) | 3.4 | 3.7 | 4.1 | 2.8 | |||
| Chest (USA) (33) | 1.1 | 1.6 | 2.5 | 3.4 | |||
| Chest (USA) (31) | 7.0 | 5.9 | 6.1 | 6.1 | |||
| Abdominal (Turkey) | 3.1 | 2.5 | 2.7 | 3.1 | |||
| Abdomen (USA) (32) | 4.2 | 3.7 | 3.7 | 3.6 | |||
| Abdomen (USA) (31) | 4.8 | 5.3 | 4.8 | 3.3 | |||
| Pelvic (Turkey) | 3.9 | 3.3 | 3.6 | 3.6 | |||
UK, United Kingdom; HRCT-chest, high-resolution computed tomography of the chest; USA, United States of America.
Discussion
There is an urgent need to manage radiation doses from CT applications; the establishment of national DRLs has been one of the first attempts to meet this requirement. While the implementation of national DRLs is a challenging task, if successful, it will result in a reduction of the accumulated radiation doses to patients (9). It may be difficult to achieve widespread acceptance of protocols for a heterogeneous group of CT technology (34). It may also be challenging to manage and implement the findings of this type of research into routine clinical practice. For example, a previous study reported that less than 2% of renal colic protocols delivered low doses across 93 institutions in United States, which utilized the National Dose Registry data. It is difficult to perform surveys into radiation doses and therefore very few of the conducted audits may provide sufficient data for nationwide information (10).
Survey-based studies are associated with some limitations; however, they represent an effective way to conduct research when there is insufficient labor to collect the data directly. Due to large spatial scales and large number of CT devices in Turkey, the establishment of DRLs using direct measurements may be difficult. Therefore, this study collated CT appliance parameters and radiation dose information (CT-DIvol) from hospital radiology departments through questionnaires. In total, from more than 1600 available CT devices in Turkey, 200 were included in this study (a survey response rate of approximately 10%). This was assumed to be an important and necessary level of representation in order to establish national DRLs.
The questionnaire response rate was lower than expected; however, examination parameters were obtained for all protocols. The number of fully completed questionnaires for each protocol varied from 88 to 114. Since dose information for each protocol was obtained from more than 80 hospitals, third quartile data from Turkey was deemed acceptable for the determination of national DRL values for adult and pediatric CT examinations.
The radiation dose profiles in adult patients varied between the head and the other regions of the body. While head, HRCT-chest, and pelvic CTDIvol and DLPs were higher than the recommended EC dose limits, the other body regions (chest and abdominal) complied with the acceptable EC dose requirements for adult patients. These findings may be explained by the use of higher scanning parameters (kV, mAs, or exposure time). Since the DLP and ED values were calculated from CTDIvol with standard scanning distances, it was not possible to obtain more detailed information from actual scan lengths. In Europe, CTDIvol values for head CT applications should be maintained below 60 mGy values, unless medical situation necessitates a higher value. In the present study, maximum third quartile CTDIvol values for head examinations in adult patients were 66.4 mGy (Fig. 1). This indicates that a substantial number of the CT appliances in Turkey exceed the recommended radiation dose value for head examinations, which approximately comprise one third of all examinations performed in Turkey. The HRCT -chest and pelvic CTDIvol values were also higher in Turkey compared with the EC recommendations and some of the previously published surveys (17). The DLP values for adult head examinations, as expected from the results of CTDIvol, were similar to that reported in a previous study (21).
The DRL values were based on the upper limits of average values from periodical surveys or audits; the findings of which did not suggest poor medical practice. The evaluation of mean and first quartile values have been recommended for optimization processes (9). The present study compared the mean and first quartile values from adult protocols with currently available information from the published literature. The mean DLP was lower in Turkey than in Ireland (20) for head (660 vs. 857 mGy. cm), thorax (247 vs. 354 mGy.cm), and abdominal CT examinations (176 vs. 547 mGy. cm); however, values for HRCT-chest examinations were higher in Turkey (240 vs. 166 mGy cm). Mean DLP was also lower in Turkey compared with Italy (22) for head (660 vs. 1086 mGy.cm), thorax (247 vs. 453 mGy. cm), and abdominal (176 vs. 450 mGy.cm) examinations. In addition, the first quartile percentile DLP values for head (350 vs. 867 mGy.cm), thorax (131 vs. 282 mGy.cm), and abdominal (93 vs. 266 mGy.cm) examinations were lower in Turkey than in Italy (22).
It is important to develop and implement low-dose scanning protocols which also evaluate image quality with regards to noise level and contrast-to-noise ratio for specific body regions. However, in addition to the diversity of CT devices, variations between the different body protocols may complicate dose-lowering efforts (9, 22). Department-specific training for individual CT radiology professionals involves a dose-decreasing chain of inputs (33). Current multi-detector CTs may produce lower radiation doses than single-detector CT systems, because of their increased speed and reduced total scanning time; however, data to support this is limited.
Pediatric scanning protocols exhibited different dose patterns compared to adult protocols. It is not surprising to encounter high-dose CT applications in pediatric patients, even in developed countries. Optimization of CT protocols for smaller sized patients is necessary because small body sizes absorb higher radiation doses than larger bodies. The greater sensitivity of pediatric tissues to the harmful effects of radiation and longer life expectancies compared with adults should also be taken into consideration. Radiology departments should therefore pay specific attention to the protocol parameters for pediatric patients in order to reduce radiation doses. The ICRP frequently emphasizes that the stochastic effects of radiation are more dangerous for younger patients (6, 7). The findings for the 10–15 year-old patients in the present study can be considered lower than the reference values because these patients are considered adults and can therefore be compared with adult reference values (19–21,24–26).
Optimization of patients’ radiation doses will require the involvement of several professional bodies within Turkey’s national authority. First, staff responsible for increasing the general awareness of patient radiation exposure protection and optimization will require further education and training. Second, instead of completing surveys, physicists have begun to visit CT departments to directly measure tube performances on site. However, while this data is more informative than survey-based information, it is a much slower process. Since there are more than 1600 CT machines across Turkey, outsourcing the dose measurement practice to contracted experts would be useful.
The easiest way to diagnose critical mistakes, which cause extremely high or low radiation exposures, would be to circulate more detailed survey forms in individual institutions. Such forms are required to collect more detailed information on CT protocols structured on clinical scenarios including interstitial lung disease, suspected urinary stones, or multiphase studies such as liver characterization or kidney masses. Similar surveys have been conducted in the UK and could be used as a template for future studies. Radiologists and technologists should also be encouraged to provide detailed feedback and regional meetings should be organized to educate these professionals after survey completion.
This study has several limitations. First, there are more than 1600 CT devices currently in operation in Turkey; however, the survey data represents only 10% of these, and therefore does not represent the whole country. In addition, approximately one year was required for radiologists to complete the survey; therefore, institutions may need to develop and maintain a more efficient communication system for such purposes. For example, the implementation of an internet-based survey may be useful for future studies of this nature. It is also necessary to improve CT technician availability and CT equipment for more frequent dose and quality control visits. The second limitation is the utilization of the main tube output data for the CTDIvol values and for the calculation of the other dose-dependent indicators (DLPs and EDs), because this may be associated with some scanning performance errors. In addition, potential increases in the radiation due to the well-recognized problem of over-scanning the targeted body region during CT examinations, may have been a source of underestimation in dose calculations. The quality of the supporting CT examination information was also weak since some of the responders were not able to complete the entire questionnaire. This highlights the importance of using more detailed forms, which are compatible with high-speed communication networks, such as those used in the EC surveys (17, 19, 20). Third, there was an issue related to image quality and its potential impacts on the diagnostic ability of CT applications. The decreased mean and first quartile dose levels may be explained by high noise, low-dose protocols. A fourth limitation was that the calculation of DLP and EDs from the tube output data may have masked the estimation and underestimate the real dose levels (like doses derived from 10 to 20 real patients’ electronic records). A final limitation is that the survey did not collect information relating to the use of automatic exposure control techniques, which may also influence the real patient doses. Dose-reduction effects of current tube techniques should also be evaluated in future studies. The information relating to scanning parameters could be strengthened by the utilization of internationally accepted software such as ImPACT Scan (St. George’s Healthcare NHS Trust) or CT Expo (Sascrad) for improved ED estimations. However, despite these limitations, this survey has been useful for highlighting the need for nationwide optimization of CT scanning protocols. Radiologists, medical physicists, and technicians have both the responsibility and the ability to reduce medical radiation exposure.
In conclusion, the third quartile CTDIvol of the CT protocols determined by the survey and the EDs calculated from the DLP values revealed that adult head examination doses and many of the pediatric doses in Turkey were higher than the EC recommendations. However, radiation doses for adult body protocols were similar to those reported in the literature. Radiation dose values were very similar in less than one-year-old and 1–5-year-old age groups, indicating the need for an urgent optimization study in pediatric examinations executed in Turkey. Dose optimization is required for adult head and all pediatric CT protocols to reduce patient radiation exposure.
Main points.
This is the first study to investigate the diagnostic reference levels (DRL) for CT doses of adult and pediatric patients in Turkey.
Third quartile CTDIvol values for adult pelvic and all pediatric body protocols were higher than the European Commission standards but were comparable to other published studies conducted internationally.
Third quartile adult CTDIvol values are 66.4, 11.6, 11.3, 13.3, and 19.4 mGy for head, chest, HRCT, upper abdomen, and lower abdomen CT exams, respectively. The findings are recommended for use as national DRLs in Turkey.
CT protocol optimization is necessary for adult head, pediatric chest, HRCT, abdominal, and pelvic protocols.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Schauer DA, Linton OW. National council on radiation protection and measurements report shows substantial medical exposure increase. Radiology. 2009;253:293–296. doi: 10.1148/radiol.2532090494. http://dx.doi.org/10.1148/radiol.2532090494. [DOI] [PubMed] [Google Scholar]
- 2.IAEA. International Atomic Energy Agency. 1996. International basic safety standards for protection against ionizing radiation and for the safety of radiation sources. (Safety Series No:115). [Google Scholar]
- 3.Santos J, Foley S, Paulo G, McEntee MF, Rainford L. The establishment of computed tomography diagnostic reference levels in Portugal. Radiat Prot Dosim. 2014;158:307–317. doi: 10.1093/rpd/nct226. http://dx.doi.org/10.1093/rpd/nct226. [DOI] [PubMed] [Google Scholar]
- 4.ICRP. 1990 recommendations of the international commission on radiological protection. Ann ICRP. 1991;21:1–3. [PubMed] [Google Scholar]
- 5.ICRP. Radiation and your patient—a guide for medical practitioners. Ann ICRP. 2001;31:4. [PubMed] [Google Scholar]
- 6.ICRP. 2007 recommendations of the international commission on radiological protection (users edition) Ann ICRP. 2007;37:2–4. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 7.ICRP. Radiological protection in medicine. Ann ICRP. 2007;37:6. doi: 10.1016/j.icrp.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Council Directive 97/43/Euratom of 30 June 1997 on health protection of individuals against the dangers of ionizing radiation in relation to medical exposure, and repealing Directive 84/466/Euratom. [Accessed July 11, 2014]. Available at: http://ec.europa.eu/energy/nuclear/radioprotection/doc/legislation/9743_en.pdf. http://www.mh-hannover.de/1604.html.
- 9.Papaioannou G, Young C, Owens CM. Multi-detector row CT for imaging the paediatric tracheobronchial tree. Pediatr Radiol. 2007;37:515–529. doi: 10.1007/s00247-007-0434-0. http://dx.doi.org/10.1007/s00247-007-0434-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lukasiewicz A, Bhargavan-Chatfield M, Coombs L, et al. Radiation dose index of renal colic protocol CT studies in the United States: a report from the American College of Radiology National Radiology Data Registry. Radiology. 2014;271:445–451. doi: 10.1148/radiol.14131601. http://dx.doi.org/10.1148/radiol.14131601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diaconescu C, Iacob O. Survey of diagnostic paediatric radiology and the resulted collective effective dose (2000y) J Prev Med. 2002;10:3–9. [Google Scholar]
- 12.Tack D, Jahnen A, Kohler S, et al. Multidetector CT radiation dose optimisation in adults: short- and long-term effects of a clinical audit. Eur Radiol. 2014;24:169–175. doi: 10.1007/s00330-013-2994-8. http://dx.doi.org/10.1007/s00330-013-2994-8. [DOI] [PubMed] [Google Scholar]
- 13.Parmaksız A, Atac GK, Bulgurlu F, Bulur E, Öncü T, Inal T. Unintentional irradiation of conceptus by diagnostic imaging examinations in Turkey. Radiat Prot Dosim. 2013;162:322–328. doi: 10.1093/rpd/nct287. http://dx.doi.org/10.1093/rpd/nct287. [DOI] [PubMed] [Google Scholar]
- 14.Technical Report, Türkiye’de Radyasyon Kaynakları. 2012. [Accessed July 11, 2014]. Available at: http://www.taek.gov.tr/belgeler-formlar/func-startdown/886/
- 15.National code on clinical researches published in Official Gazette numbered with 28617 at Apr 13, 2013. Accessed 24 December 2014.
- 16.ICRP. International commission on radiological protection. 1990 recommendations of the international commission on radiological protection. ICRP Publication 60. Annals of the ICRP. 1991;21(1–3) [PubMed] [Google Scholar]
- 17.Shrimpton PC, Hillier MC, Lewis MA, Dunn M. National survey of doses from CT in the UK: 2003. Br J Radiol. 2006;79:968–980. doi: 10.1259/bjr/93277434. http://dx.doi.org/10.1259/bjr/93277434. [DOI] [PubMed] [Google Scholar]
- 18.Kharita MH, Khazzam S. Survey of patient dose in computed tomography in Syria. Radiat Prot Dosim. 2010;141:149–161. doi: 10.1093/rpd/ncq155. http://dx.doi.org/10.1093/rpd/ncq155. [DOI] [PubMed] [Google Scholar]
- 19.Korir GK, Wambani JS, Korir IK. Patient doses using multidetector computed tomography scanners in Kenya. Radiat Prot Dosim. 2012;151:267–271. doi: 10.1093/rpd/ncr484. http://dx.doi.org/10.1093/rpd/ncr484. [DOI] [PubMed] [Google Scholar]
- 20.Foley SJ, Mcentee MF, Rainford LA. Establishment of CT diagnostic reference levels in Ireland. Br J Radiol. 2012;85:1390–1397. doi: 10.1259/bjr/15839549. http://dx.doi.org/10.1259/bjr/15839549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pantos I, Thalassinou S, Argentos S, Kelekis NL, Panayiotakis G, Efstathopoulos EP. Adult patient radiation doses from non-cardiac examinations: a review of published results. Br J Radiol. 2011;84:293–303. doi: 10.1259/bjr/69070614. http://dx.doi.org/10.1259/bjr/69070614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palorini F, Origgi D, Granata C, Matranga D, Salerno S. Adult exposures from MDCT including multiphase studies: first Italian nationwide survey. Eur Radiol. 2014;24:469–483. doi: 10.1007/s00330-013-3031-7. http://dx.doi.org/10.1007/s00330-013-3031-7. [DOI] [PubMed] [Google Scholar]
- 23.ICRP Publication 121. Radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP. 2013;42 doi: 10.1016/j.icrp.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Huda W, Magill D, He W. CT effective dose per dose length product using ICRP 103 weighting factors. Med Phys. 2011;38:1261–1265. doi: 10.1118/1.3544350. http://dx.doi.org/10.1118/1.3544350. [DOI] [PubMed] [Google Scholar]
- 25.Brady Z, Ramanauskas F, Cain TM, Johnston PN. Assessment of paediatric CT dose indicators for the purpose of optimisation. Br J Radiol. 2012;85:1488–1498. doi: 10.1259/bjr/28015185. http://dx.doi.org/10.1259/bjr/28015185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verdun FR, Gutierrez D, Vader JP. CT radiation dose in children: a survey to establish age based diagnostic reference levels in Switzerland. Eur Radiol. 2008;18:1980–1986. doi: 10.1007/s00330-008-0963-4. http://dx.doi.org/10.1007/s00330-008-0963-4. [DOI] [PubMed] [Google Scholar]
- 27.Buls N, Bosmans H, Mommaert C, et al. CT paediatric doses in Belgium: a multi-center study: results of a dosimetry audit 2007–2009. [Accessed July 11, 2014]. Available at: http://www.fanc.fgov.be/GED/00000000/2400/2449.pdf.
- 28.Origgi D, Vigorito S, Villa G, Bellomi M, Tosi G. Survey of computed tomography techniques and absorbed dose in Italian hospitals: a comparison between two methods to estimate the dose-length product and the effective dose to verify fulfilment of the diagnostic reference levels. Eur Radiol. 2006;16:227–237. doi: 10.1007/s00330-005-2682-4. http://dx.doi.org/10.1007/s00330-005-2682-4. [DOI] [PubMed] [Google Scholar]
- 29.Papadimitriou D, Perris A, Manetou A, et al. A survey of 14 computed tomography scanners in Greece and 32 scanners in Italy. Examination frequencies, dose reference values, effective doses and doses to organs. Radiat Prot Dosim. 2003;104:47–53. doi: 10.1093/oxfordjournals.rpd.a006162. http://dx.doi.org/10.1093/oxfordjournals.rpd.a006162. [DOI] [PubMed] [Google Scholar]
- 30.Galanski M, Nagel HD, Stamm G. CT Expositionspraxis in der Bundesrepublik Deutschland. Ergebnisse einer bundesweiten Umfrage im Jahre 1999. Fortschr Rntgenstr. 2001;173:R1–R66. doi: 10.1055/s-2001-19474. http://dx.doi.org/10.1055/s-2001-19474. [DOI] [PubMed] [Google Scholar]
- 31.Huda W, Atherton JV, Ware DE, Cumming WA. An approach for the estimation of effective radiation dose at CT in pediatric patients. Radiology. 1997;203:417–422. doi: 10.1148/radiology.203.2.9114097. http://dx.doi.org/10.1148/radiology.203.2.9114097. [DOI] [PubMed] [Google Scholar]
- 32.Thomas KE, Wang B. Age-specific effective doses for pediatric MSCT examinations at a large children’s hospital using DLP conversion coefficients: a simple estimation method. Pediatr Radiol. 2008;38:645–656. doi: 10.1007/s00247-008-0794-0. http://dx.doi.org/10.1007/s00247-008-0794-0. [DOI] [PubMed] [Google Scholar]
- 33.Chapple CL, Willis S, Frame J. Effective dose in paediatric computed tomography. Phys Med Biol. 2002;47:107–115. doi: 10.1088/0031-9155/47/1/308. http://dx.doi.org/10.1088/0031-9155/47/1/308. [DOI] [PubMed] [Google Scholar]
- 34.Huda W. Radiation doses and risks in chest computed tomography examinations. Proc Am Thorac Soc. 2007;4:316–320. doi: 10.1513/pats.200611-172HT. http://dx.doi.org/10.1513/pats.200611-172HT. [DOI] [PubMed] [Google Scholar]