Abstract
Background:
A cardiac catheterization laboratory can be a frightening environment and music can be a supportive source of environmental sound that stimulates and maintains relaxation. However, the results of studies are conflicting in this regard.
Objectives:
The aim of this study was to investigate the effect of music therapy on patients’ anxiety and hemodynamic parameters during percutaneous transluminal coronary angioplasty.
Patients and Methods:
This was a randomized controlled trial, conducted in the Catheterization Laboratory Unit of Baqiyatallah Hospital, in Tehran, Iran. A sample of 64 patients, who were planned to undergo coronary angioplasty, was recruited. Patients were randomly allocated to either the control or the experimental groups. In the experimental group, patients received a 20 to 40-minute music therapy intervention, consisting of light instrumental music albums by Johann Sebastian Bach and Mariko Makino. Patients in the control group received the routine care of the study setting, which consisted of no music therapy intervention. Study data were collected by a demographic questionnaire, the Spielberger’s State Anxiety Inventory, and a data sheet for documenting hemodynamic parameters. Chi-square, independent-samples t tests, paired-samples t-test and repeated measures analysis of variance were used to analyze the data.
Results:
Before the intervention, the study groups did not differ significantly in terms of anxiety level and hemodynamic parameters. Moreover, the differences between the two groups, regarding hemodynamic parameters, were not significant after the intervention (P > 0.05). However, the level of post-intervention anxiety in the experimental group was significantly lower than the control group (32.06 ± 8.57 and 38.97 ± 12.77, respectively; P = 0.014). Compared with the baseline readings, the level of anxiety in the control group did not change significantly after the study (41.91 ± 9.88 vs. 38.97 ± 12.77; P = 0.101); however, in the experimental group, the level of post-intervention anxiety was significantly lower than the pretest readings (32.06 ± 8.57 vs. 41.16 ± 10.6; P = 0.001).
Conclusions:
Music therapy is a safe, simple, inexpensive, and non-invasive nursing intervention, which can significantly alleviate patients’ anxiety during coronary angioplasty.
Keywords: Music Therapy, Coronary Angioplasty, Anxiety, Hemodynamics
1. Background
Percutaneous transluminal coronary angioplasty (PTCA) is one of the most common invasive procedures performed in patients with coronary artery diseases (CAD). This procedure involves advancing a balloon-tipped catheter through a coronary artery to dilate the stenotic area of the vessel lumen and improve the coronary artery blood flow (1). Patients who are expected to undergo cardiac catheterization experience considerable anxiety (2-4). Astin et al. have reported that more than 36% of patients who undergone PTCA experienced sever anxiety (5). Another study has reported that the prevalence of acute and chronic anxiety in these patients is 70 - 80% and 20 - 25%, respectively (6).
Anxiety is an emotional state, which is associated with tension, anger, apprehension, fear, increased serum levels of epinephrine and norepinephrine, heightened autonomic activity, and activated stress responses, which collectively expand the workload of the cardiovascular system (7). The major causes of anxiety in patients who undergo PTCA are the noises of angioplasty equipment, healthcare professionals’ talks, pain, unfamiliar environment of the catheterization laboratory, fear of the results and the complications of the procedure, previous experiences of PTCA, probability of requiring surgery and having uncertainty over future (8).
Feeling severe anxiety during a critical procedure, such as PTCA, can increase the risk for developing mental and physical problems (9). Anxiety increases heart rate (HR) and blood pressure (BP) (10, 11), expands cardiac output, heightens cardiac workload, and increases myocardial oxygen demand and the length of hospital stay (12). Given the profound effects of anxiety on different systems of the body, anxiety management is one of the major nursing priorities (4, 13).
There are multiple pharmacological strategies for managing PTCA-associated anxiety (9). However, anxiolytic medications are usually associated with different side effects, as well as the likelihood of developing drug dependence (14).
Consequently, there is currently a growing desire for using non-pharmacological anxiety management strategies. For instance, Molavi Vardanjani et al. made use of reflexology (15), while Adib-Hajbaghery et al. used a multidimensional package (16) to alleviate the cardiac patients’ anxiety. One of the most common non-pharmacological anxiety management strategies is music therapy (17). Music therapy is a safe, simple, inexpensive, and non-invasive nursing intervention, which can be used as a complementary therapy for anxiety management (18, 19). It can promote patients’ comfort through enhancing stress threshold, regulating the internal processes of the body, and boosting immunity (20, 21). Almerud and Petersson have noted that music stimulates the central nervous system to produce endorphins. Endorphins are endogenous morphine-like substances, which can decrease BP, HR, and respiratory rate and promote relaxation through alleviating fear and anxiety (22). In a review study, Vanderboom has noted that non-pharmacological anxiety management strategies, such as music therapy, can decrease patients’ HR and BP and eliminate the need for general anesthesia during invasive procedures (23). On the other hand, music can alleviate patients’ pain and anxiety by distracting their attention from anxiety-producing factors (24). Probably, music exerts its anxiolytic effects through interacting with perceptive, cognitive, and affective processes and also, through preventing patients from hearing the sounds that fill operating rooms and catheterization laboratories. Moreover, music-induced positive feelings and mood improvements can help manage clinical conditions, such as pain and anxiety (25). Nilsson (26) and Sendelbach et al. (27) have studied the effect of music intervention on stress response in patients undergoing cardiac surgery and reported that the intervention was not significantly effective. Due to the inconsistencies in the results of previous studies, more investigations are yet needed to fully understand the effect of music intervention on patients undergoing cardiac procedures. On the other hand, many of the researchers applied their intervention before the cardiac procedures (15, 16) and few studies are available on the effect of music therapy implemented during the procedure, on PTCA-associated anxiety. Therefore, the present study was conducted to address this knowledge gap.
2. Objectives
The aim of this study was to investigate the effect of music therapy on anxiety and hemodynamic parameters among patients receiving PTCA.
3. Patients and Methods
3.1. Study Design and Participants
This was a non-blind, two-group parallel, randomized, controlled trial that was conducted on patients undergoing PTCA in the catheterization lab units of Baqiyatallah Hospital, Tehran, Iran. The study was conducted from January to April 2014.
The sample size was calculated using the results of a previous study (10). Considering a power of 80%, the type I error probability of 95%, the Pocock’s sample size formula, and a medium effect size (0.5), a total of 32 patients were estimated to be necessary in each group. Therefore, 64 patients were consecutively recruited and randomly allocated to either the experimental or the control groups (32 patients in each group). The first and the second patients were randomly allocated to respectively the control and the experimental groups and then, other patients were allocated alternately.
The inclusion criteria were: patient’s desire for participating in the study; undergoing PTCA for the first time; being able to understand and speak Persian; having an age of 45 - 82 years; having no hearing impairment; having no drug or alcohol addiction; having no previous history of complicated gross surgeries or undergoing a PTCA; receiving no anxiolytic medication during the past 6 months; having no history of severe psychological disorder during the past 6 months; and needing no emergency cardiac catheterization. Patients who chose to withdraw from the study, needed emergency intervention for treating cardiac dysrhythmias, or had to undergo emergency open-heart surgery were excluded from the study.
3.2. The instruments
Data were collected using a demographic questionnaire, a data sheet for documenting hemodynamic parameters and the Spielberger’s State Anxiety Inventory (SSAI). A panel of experts affiliated to the Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran, confirmed the content validity of the first two parts of the instrument. The demographic questionnaire consisted of questions on patients’ demographic characteristics, including the subjects’ age, gender, level of education, and marital status. The SSAI consists of 20 questions which measure anxiety state on a four-point scale, ranging from Never (scored 1) to Always (scored 4). Several questions have been worded negatively, which should be scored reversely. The possible total score of the SSAI would be 20‒80. Higher scores stand for more severe state anxiety. The Persian version of the SSAI was validated by Yeganehkhah et al. and its reliability has been confirmed through internal consistency method, with a Coronbach’s alpha of 0.852 (28).
3.3. Intervention
On a daily basis, the first author referred to the cardiac care units of the study setting and recruited the eligible patients to the study. Data collection was performed at patients’ bedside. All patients were asked to complete the demographic questionnaire and the SSAI. Thereafter, when patients were admitted to the catheterization lab, we measured their baseline vital signs and allocated them alternately, to one of the study groups. Hemodynamic parameters of all patients, including systolic and diastolic BP (SBP and DBP), HR and percutaneous oxygen saturation (SaO2) were monitored using the catheterization device (Siemens, Germany) and the X110 Cardioset monitoring device (Iran Electronics Industries, Tehran, Iran) at five time-points. The X110 Cardioset monitoring device was calibrated by the manufacturer. The measurement time-points were 10 minutes before PTCA (T1), immediately after starting it (T2), 10 and 20 minutes after starting it (T3 and T4), and 30 minutes after its completion (T5). The anxiety posttest was also performed, 30 minutes after PTCA. Given the fact that patient’s chest was not visible during the procedure, respiratory rate was measured only twice (T1 and T5). Patients’ hemodynamic parameters were monitored while they were in the supine position.
The music intervention started 6 minutes after local anesthesia of the groin site with lidocaine (i.e. immediately before inserting the arterial sheath and catheter). All patients received the same dose of lidocaine. Music was played using a digital MP3 player and a headphone. The music consisted of light instrumental music albums by Johann Sebastian Bach and Mariko Makino. This album has been shown to affect the cardiovascular system (29). Music therapy sessions lasted for 20 - 40 minutes, depending on the length of PTCA. We used headphones to help patients concentrate on the played music and to prevent the played music from disturbing catheterization laboratory personnel. Headphones were disposable and were disinfected before use. The patients in the control group were treated similar to the intervention group, except that they did not receive the music intervention. All patients also received the routine care of the study setting.
3.4. Ethical Considerations
The Ethics Committee of Baqiyatallah University of Medical Sciences, Tehran, Iran, approved the study (the approval code was S/340/3/6770). Patients were informed of the study aim. They were free to choose whether to participate or withdraw from the study at any time. Moreover, we ensured them that withdrawing from the study never affects their course of treatment. Written informed consent was obtained from all patients.
3.5. Data Analysis
We used the SPSS, v. 13 (SPSS Inc., Chicago, IL, USA) for data analysis. Study data were described using frequency tables and the measures of central tendency. The Chi-square and the independent-samples t tests were used for between-group comparisons. Moreover, the paired-samples t-test was used for within-group comparisons. We also employed the within-subjects repeated measures analysis of variance (RMANOVA) to compare the differences of hemodynamic variables across the five measurement time-points. Pairwise comparison was performed by using the post-hoc Bonferroni’s test. The P values which were less than 0.05 were considered as significant.
4. Results
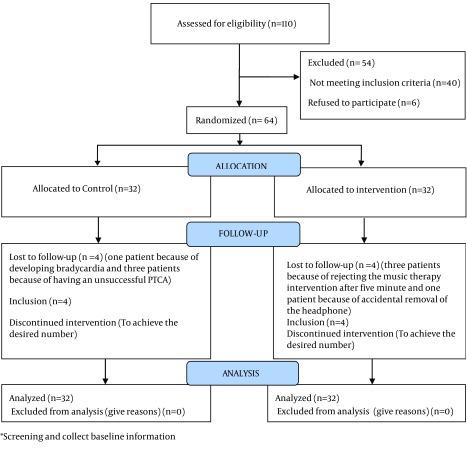
Four patients from the control group (one patient because of developing bradycardia and three patients because of having an unsuccessful PTCA) and four patients from the experimental group (three patients because of rejecting the music intervention after 5 minutes and one patient because of accidental removal of the headphone) were excluded from the study. Accordingly, we recruited eight more patients in the follow-up step (Figure 1).
Figure 1. CONSORT Flow Diagram Participant Recruitment Intervention and Control.
Participants ranged in age from 45 to 81 years, with a mean age of 58.39 ± 9.09 years. The mean age of participants in the control and the experimental groups were 56.78 ± 8.47 and 60.00 ± 9.53, respectively. Totally, 41 male (64.06%) and 23 female (35.94%) patients participated in the study. No significant differences were found between the two groups in terms of demographic variables, such as age, gender, marriage, educational status and the duration of PTCA procedure (P value > 0.05) (Table 1).
Table 1. Demographic Characteristics of the Study Groups a.
| Variable | Group | P Value | |
|---|---|---|---|
| Control | Experimental | ||
| Education level | 0.205 b | ||
| Illiterate | 3 (9.4) | 8 (25) | |
| Primary education | 4 (12.5) | 5 (15.6) | |
| Secondary education | 9 (28.1) | 11 (34.4) | |
| Diploma | 9 (28.1) | 3 (9.4) | |
| Academic degree | 7 (21.9) | 5 (15.6) | |
| Marital status | 0.356 c | ||
| Single | 0 | 1 (3.1) | |
| Married | 32 (100) | 30 (93.8) | |
| Widow | 0 | 1 (3.1) | |
| Divorced | 0 | 0 | |
| Gender | 0.434 b | ||
| Male | 19 (59.4) | 22 (69) | |
| Female | 13 (46.6) | 10 (31) | |
| Age, y | 56.78 ± 8.47 | 60 ± 9.53 | 0.54 d |
| Duration of the procedure, min | 35.64 ± 11.81 | 31.41 ± 11.16 | 0.148 d |
a Data are presented as No. (%) or Mean ± SD.
b Chi-square Test.
c Exact Fisher’s test.
d Independent-samples t-test.
As Tables 2 and 3 show, before the intervention, the study groups did not differ significantly regarding anxiety level and hemodynamic parameters (P > 0.05), confirming the similarity of the groups before the study. Moreover, the study groups did not differ significantly in terms of hemodynamic parameters at different measurement time-points (P > 0.05; Table 2). However, after the intervention, the level of anxiety in the experimental group was significantly lower than the control group (32.06 ± 8.57 vs. 38.97 ± 12.77, respectively; P = 0.014; Table 3). Moreover, the results of the paired-samples T test revealed that, compared with baseline readings, the level of anxiety in the experimental group significantly decreased after the intervention (32.06 ± 8.57 vs. 41.16 ± 10.6; P = 0.001; Table 3). However, the level of anxiety in the control group did not decrease significantly at the end of the study (Table 3).
Table 2. Hemodynamic Parameters in Both Study Groups Throughout the Study a.
| Group | Time, min | P Value b | ||||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T5 | ||
| SBP, mmHg | ||||||
| Control | 137.12 ± 17.69 | 139.94 ± 32.55 | 138.75 ± 24.28 | 136.32 ± 23.08 | 130.56 ± 3.21 | 0.208 |
| Experimental | 138.81 ± 20.54 | 153.63 ± 32.57 | 142.38 ± 23.93 | 139.84 ± 22.34 | 130.09 ± 21.39 | 0.001 |
| P value c | 0.726 | 0.098 | 0.550 | 0.545 | 0.925 | - |
| DBP, mmHg | ||||||
| Control | 85.22 ± 11.64 | 83.22 ± 12.01 | 80.44 ± 10.29 | 81.19 ± 11.24 | 79.59 ± 10.15 | 0.094 |
| Experimental | 84.81 ± 10.46 | 87.44 ± 15.65 | 85.38 ± 15.92 | 83.31 ± 12.51 | 78.56{14.16 | 0.006 |
| P value c | 0.884 | 0.231 | 0.147 | 0.279 | 0.739 | - |
| HR, Per min | ||||||
| Control | 75.34 ± 15.51 | 79.28 ± 14.40 | 80.16 ± 14.26 | 79.31 ± 12.64 | 74.37 ± 14.03 | 0.001 |
| Experimental | 75.94 ± 12.91 | 78.28 ± 15.13 | 79.41 ± 13.31 | 78.68 ± 12.81 | 71.91 ± 9.64 | 0.001 |
| P value c | 0.868 | 0.787 | 0.829 | 0.844 | 0.415 | - |
| SaO2, % | ||||||
| Control | 95.03 ± 2.18 | 93.72 ± 1.27 | 93.22 ± 2.3 | 93.19 ± 2.63 | 94.09 ± 1.91 | 0.001 |
| Experimental | 94.38 ± 2.60 | 93.34 ± 2.54 | 91.91 ± 3.08 | 92.32 ± 3.37 | 94.19 ± 2.42 | 0.001 |
| P value c | 0.278 | 0.459 | 0.058 | 0.260 | 0.864 | - |
| RR, Per min | ||||||
| Control | 19.22 ± 2.52 | - | - | - | 18.66 ± 3.31 | - |
| Experimental | 19 ± 2.53 | - | - | - | 19.44 ± 10.14 | - |
| P value c | 0.732 | - | - | - | 0.680 | - |
a Abbreviations: DBP, Diastolic blood pressure; HR, Hear rate; SBP, systolic blood pressure; RR, Respiration rate; SaO2, Saturation of arterial oxygen.
b Results of the RM ANOVA.
c Results of independent-samples T test.
Table 3. The Levels of Anxiety in Both Study Groups Before and After the Intervention a.
| Group | Time, min | ||
|---|---|---|---|
| T1 | T5 | P Value b | |
| Control | 41.91 ± 9.88 | 38.97 ± 12.77 | 0.101 |
| Experimental | 41.16 ± 10.65 | 32.06 ± 8.57 | 0.001 |
| P value c | 0.771 | 0.014 | - |
a Data are presented as Mean ± SD.
b Results of paired-samples T test.
c Results of independent-samples T test.
5. Discussion
The aim of this study was to examine the effect of music therapy on patients’ anxiety and hemodynamic parameters during PTCA. Study findings revealed that music therapy had significant effects on patients’ anxiety. However, despite receiving standard nursing care, patients in the control group did not experience any significant change in their anxiety level. Argstatter et al. (30), Weeks et al. (31) and Dogan and Senturan (32) have also found that music intervention can significantly reduce patients’ anxiety during cardiac catheterization, coronary angiography and PTCA. In contrast, Nilsson found that music therapy was not effective in alleviating cardiac surgery-related anxiety (26). Almerud and Petersson noted that music affects the brain, stimulates the generation of alpha brain waves and the secretion of endorphins, produces relaxation, and relieves fear and anxiety (22). Moreover, it alleviates patients’ pain and anxiety through distracting them from the causes of anxiety (21). Accordingly, it seems that music intervention in the present study might also alleviated anxiety by distracting patients’ attention from the environmental factors that caused anxiety.
The present study also showed that music intervention did not significantly affect patients’ hemodynamic parameters. The insignificant changes of hemodynamic parameters, following music therapy, can be attributed to the fact that, during PTCA, hemodynamic parameters are monitored and maintained at normal levels to prevent patients from developing life-threatening complications. For instance, if a patient develops bradycardia or hypertension, atropine and nitroglycerin are administered to normalize HR and BP, respectively. Previous studies reported conflicting findings regarding the effect of music therapy on hemodynamic parameters. Argstatter et al. found no significant HR changes following music therapy (30). Sendelbach et al. have also reported that music therapy had no significant effect on HR, DBP, and SBP in patients undergoing cardiac surgery (27). Moreover, Chan found that music therapy significantly affected SBP, DBP, RR, HR, and SaO2 in patients undergoing a C-clamp procedure, after coronary catheterization (33). The contradiction between the findings of different studies can be attributed to the time of administrating music therapy. For instance, we administered music therapy during PTCA, while Chan delivered it after the procedure.
In conclusion, the music intervention, in the present study, could significantly alleviate patients’ anxiety during PTCA. Given the serious adverse effects of anxiety and anxiolytic agents on different organs, the safety and simplicity of music therapy intervention and the difficulty and expensiveness of administrating other non-pharmacological interventions, using music therapy, as a nursing intervention for managing PTCA-associated anxiety, is recommended. However, further studies are needed to provide conclusive evidence regarding the effectiveness of music therapy in alleviating anxiety and improving hemodynamic status before, during, and after PTCA.
This study also had several limitations. The environmental factors (noises), patients’ differences regarding psychological and personality characteristics, as well as their attitudes and beliefs about music might have affected our findings. We also conducted the study on a small sample of patients. Therefore, further studies on larger sample sizes and with controlling the environmental variables can be suggested.
Acknowledgments
This article reported the findings of a Master’s thesis, Baqiyatallah University of Medical Sciences, Tehran, IR Iran. We would like to sincerely thank the dean, the research administrator and the Nursing faculty and Behavioral Sciences Research Center of Baqiyatallah University of Medical Sciences, Tehran, IR Iran, as well as the administrators, physicians, and nursing staff of Baqiyatallah Hospital, Tehran, IR Iran, who helped and supported us during the study. This clinical trial was registered in the Iranian Registry of Clinical Trials under the registration code IRCT2014043014770N2R1.
Footnotes
Authors’ Contributions:Elaheh Mottahedian Tabrizi and Masoumeh Forooghy, designed the study. Masoumeh Forooghy collected the data. Ebrahim Hajizadeh and Masoumeh Forooghy analyzed the data. Masoumeh Forooghy, Elaheh Mottahedian Tabrizi, Ebrahim Hajizadeh, and Bahram Pishgoo contributed to drafting the manuscript.
Funding/Support:Nursing faculty and Behavioral Sciences Research Center, Baqiyatallah University of Medical Sciences, Tehran, IR Iran.
References
- 1.Smeltzer SCOC, Bare BG, Hinkle JL, Cheever KH. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. Philadelphia: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 2.Janice L, Hincle Kerry H. Brunner & Suddarth's textbook of medical-surgical nursing. Lippincott Williams & Wilkins: Philadelphia; 2014. [Google Scholar]
- 3.Davidson C, Bonow R. Cardiac catheterization. 9th ed ,Philadelphia: Saunders Elsevier; 2011. [Google Scholar]
- 4.Taylorpiliae R, Chair S. The effect of nursing interventions utilizing music therapy or sensory information on Chinese patientsʼ anxiety prior to cardiac catheterization: a pilot study. Eur J Cardiovasc Nurs. 2002;1(3):203–11. doi: 10.1016/S1474-5151(02)00037-3. [DOI] [PubMed] [Google Scholar]
- 5.Astin F, Jones K, Thompson DR. Prevalence and patterns of anxiety and depression in patients undergoing elective percutaneous transluminal coronary angioplasty. Heart Lung. 2005;34(6):393–401. doi: 10.1016/j.hrtlng.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Cullum N, Ciliska D, Marks S, Haynes B. Evidence-Based Nursing: An Introduction. In: Cullum N, Ciliska D, Haynes RB, Marks S, editors. An introduction to evidence-based nursing. Evidence-Based Nursing. Oxford, UK: Blackwell; 2008. [Google Scholar]
- 7.Gagner-Tjellesen D, Yurkovich EE, Gragert M. Use of music therapy and other ITNIs in acute care. J Psychosoc Nurs Ment Health Serv. 2001;39(10):26–37. doi: 10.3928/0279-3695-20011001-11. [DOI] [PubMed] [Google Scholar]
- 8.Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of patient-controlled music therapy during coronary angiography on procedural pain and anxiety distress syndrome. Crit Care Nurse. 2003;23(2):50–8. [PubMed] [Google Scholar]
- 9.Uzun S, Vural H, Uzun M, Yokusoglu M. State and trait anxiety levels before coronary angiography. J Clin Nurs. 2008;17(5):602–7. doi: 10.1111/j.1365-2702.2007.02018.x. [DOI] [PubMed] [Google Scholar]
- 10.Lee KC, Chao YH, Yiin JJ, Hsieh HY, Dai WJ, Chao YF. Evidence that music listening reduces preoperative patients' anxiety. Biol Res Nurs. 2012;14(1):78–84. doi: 10.1177/1099800410396704. [DOI] [PubMed] [Google Scholar]
- 11.Wakim JH, Smith S, Guinn C. The efficacy of music therapy. J Perianesth Nurs. 2010;25(4):226–32. doi: 10.1016/j.jopan.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Hanser SB, Mandel SE. The effects of music therapy in cardiac healthcare. Cardiol Rev. 2005;13(1):18–23. doi: 10.1097/01.crd.0000126085.76415.d7. [DOI] [PubMed] [Google Scholar]
- 13.Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nurs Crit Care. 2006;11(5):224–31. doi: 10.1111/j.1478-5153.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- 14.DeMartinis NA, Kamath J, Winokur A. New approaches for the treatment of sleep disorders. Adv Pharmacol. 2009;57:187–235. doi: 10.1016/S1054-3589(08)57005-0. [DOI] [PubMed] [Google Scholar]
- 15.Molavi Vardanjani M, Masoudi Alavi N, Razavi NS, Aghajani M, Azizi-Fini E, Vaghefi SM. A randomized-controlled trial examining the effects of reflexology on anxiety of patients undergoing coronary angiography. Nurs Midwifery Stud. 2013;2(3):3–9. doi: 10.5812/nms.12167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adib-Hajbaghery M, Moradi T, Mohseni R. Effects of a multimodal preparation package on vital signs of patients waiting for coronary angiography. Nurs Midwifery Stud. 2014;3(1):e25800. doi: 10.17795/nmsjournal17518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barker R, Kober A, Hoerauf K, Latzke D, Adel S, Kain ZN, et al. Out-of-hospital auricular acupressure in elder patients with hip fracture: a randomized double-blinded trial. Acad Emerg Med. 2006;13(1):19–23. doi: 10.1197/j.aem.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Han L, Li JP, Sit JW, Chung L, Jiao ZY, Ma WG. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: a randomised controlled trial. J Clin Nurs. 2010;19(7-8):978–87. doi: 10.1111/j.1365-2702.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- 19.Stefano GB, Zhu W, Cadet P, Salamon E, Mantione KJ. Music alters constitutively expressed opiate and cytokine processes in listeners. Med Sci Monit. 2004;10(6):MS18–27. [PubMed] [Google Scholar]
- 20.Chang MY, Chen CH, Huang KF. Effects of music therapy on psychological health of women during pregnancy. J Clin Nurs. 2008;17(19):2580–7. doi: 10.1111/j.1365-2702.2007.02064.x. [DOI] [PubMed] [Google Scholar]
- 21.Chang SC, Chen CH. Effects of music therapy on women's physiologic measures, anxiety, and satisfaction during cesarean delivery. Res Nurs Health. 2005;28(6):453–61. doi: 10.1002/nur.20102. [DOI] [PubMed] [Google Scholar]
- 22.Almerud S, Petersson K. Music therapy--a complementary treatment for mechanically ventilated intensive care patients. Intensive Crit Care Nurs. 2003;19(1):21–30. doi: 10.1016/s0964-3397(02)00118-0. [DOI] [PubMed] [Google Scholar]
- 23.Vanderboom T. Does Music Reduce Anxiety During Invasive Procedures With Procedural Sedation? An Integrative Research Review. J Radiol Nurs. 2007;26(1):15–22. [Google Scholar]
- 24.Nakahara H, Furuya S, Masuko T, Francis PR, Kinoshita H. Performing music can induce greater modulation of emotion-related psychophysiological responses than listening to music. Int J Psychophysiol. 2011;81(3):152–8. doi: 10.1016/j.ijpsycho.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Koelsch S, Fuermetz J, Sack U, Bauer K, Hohenadel M, Wiegel M, et al. Effects of Music Listening on Cortisol Levels and Propofol Consumption during Spinal Anesthesia. Front Psychol. 2011;2:58. doi: 10.3389/fpsyg.2011.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart Lung. 2009;38(3):201–7. doi: 10.1016/j.hrtlng.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 27.Sendelbach SE, Halm MA, Doran KA, Miller EH, Gaillard P. Effects of music therapy on physiological and psychological outcomes for patients undergoing cardiac surgery. J Cardiovasc Nurs. 2006;21(3):194–200. doi: 10.1097/00005082-200605000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Yeganehkhah M, Mohamadi Shab Bolaghi F, Khankeh HR, Rahgozar M. [The Effects Of Slow-Stroke Back Massage On Hypertension In Elderly]. Iran J Nurs. 2008;21(54):73–83. [Google Scholar]
- 29.Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Syst Rev. 2006;(2):CD004843. doi: 10.1002/14651858.CD004843.pub2. [DOI] [PubMed] [Google Scholar]
- 30.Argstatter H, Haberbosch W, Bolay HV. Study of the effectiveness of musical stimulation during intracardiac catheterization. Clin Res Cardiol. 2006;95(10):514–22. doi: 10.1007/s00392-006-0425-4. [DOI] [PubMed] [Google Scholar]
- 31.Weeks BP, Nilsson U. Music interventions in patients during coronary angiographic procedures: a randomized controlled study of the effect on patients' anxiety and well-being. Eur J Cardiovasc Nurs. 2011;10(2):88–93. doi: 10.1016/j.ejcnurse.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Dogan MV, Senturan L. The effect of music therapy on the level of anxiety in the patients undergoing coronary angiography. Open J Nurs. 2012;02(03):165–9. [Google Scholar]
- 33.Chan MF. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: a randomized controlled trial. Heart Lung. 2007;36(6):431–9. doi: 10.1016/j.hrtlng.2007.05.003. [DOI] [PubMed] [Google Scholar]