Abstract:
Health disparities are “differences in the quality of health and health care across different populations.” Potential disparities associated with race, ethnicity, gender, and socioeconomic status should be considered when attempting to develop models for survival and neurodevelopmental outcomes in neonates undergoing congenital heart surgery. Each of the aforementioned sociodemographic factors is related to postsurgical mortality because they are frequently linked to measures of access to care in addition to location of care (geographically) and the type of institution (teaching vs. nonteaching) where patients receive care. Traditionally these factors have not been considered in models of surgical treatment outcomes in conditions such as hypoplastic left heart syndrome. However, we believe these factors should at least be included in risk analysis models to help explain their impact on outcomes and in predicting outcomes. Therefore, the purpose of this article is to highlight some of the nonsurgical influences that affect survival after neonatal heart surgery such as race, ethnicity, gender, and socioeconomic status.
Keywords: health disparities, hypoplastic left heart syndrome, socioeconomic status, race/ethnicity
The 2008 National Healthcare Disparities Report defines “health disparities” as “differences in the quality of health and health care across different populations.” These include “differences in the presence of disease, health outcomes, or access to health care across racial, ethnic, sexual orientation and socioeconomic groups” (1). The report concluded that health disparities are common and that the lack of health insurance is an important contributor to disparities. According to the Agency for Healthcare Research and Quality, disparities in health exist among a number of “special” or “priority” populations such as low-income groups, women, children, older adults >65 years of age, residents of rural areas, and individuals with special health needs (disabilities or end-of-life care). Unfortunately, health disparities are increasing, and some areas need the most attention: cancer, heart failure, and pneumonia. More importantly, health disparities can exist even when access to care is equalized as depicted in Figure 1 (2).
Figure 1.
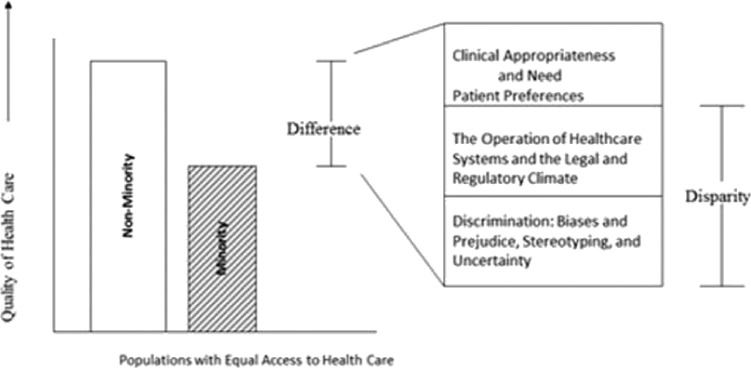
Differences, disparities, and discrimination: Populations with equal access to healthcare. (Reprinted with permission)
To fully understand sociodemographic contributors to disparities in surgical outcomes, it will be helpful to give consideration to the contribution and reporting of race, ethnicity, gender, and socioeconomic factors to general health outcomes. The American Psychological Association Publication Manual suggests that researchers should “report major demographic variables such as sex, age, and race/ethnicity and where possible and appropriate, characteristics such as socioeconomic status (SES), disability status and sexual orientation” (3). These reporting standards were established because the aforementioned sociodemographic factors are believed influence health-related outcomes. For example, “SES is one variable that encompasses a complex interaction of a wide range of associated variables such as income, education, insurance status, access to care and health related beliefs that have the potential to influence an individual’s quality of care” (4). Therefore, we believe the relationship between these sociodemographic factors and surgical outcomes has not been adequately considered in studies of postsurgical outcomes. The mechanism by which these sociodemographic factors influence postsurgical outcomes is depicted in our conceptual model (Figure 2). The proposed model outlines the manner by which disparities in outcomes emerge as a result of nonsurgical factors that are associated with surgical survival.
Figure 2.
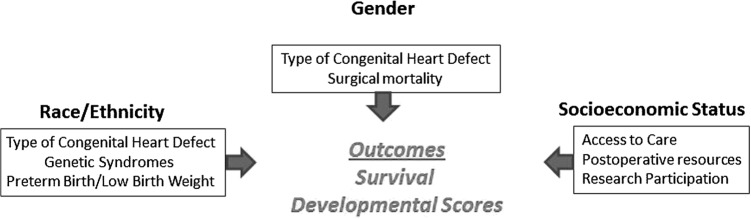
Conceptual model of nonsurgical factors affecting survival and developmental outcomes in neonatal heart surgery.
Therefore, the purpose of this article is to briefly examine the contribution of sociodemographic factors, i.e., race/ ethnicity, gender, low income, or SES to survival after neonatal heart surgery. Traditionally, risk adjustment models (Aristotle Complexity Score [ARISTOTLE], Risk Assessment for Congenital Heart Surgery [RACHES-1], and Society of Thoracic Surgeons [STS]) used to develop survival projections are based on the either individual or combined medical procedures have not incorporated these other demographic factors. In this article, we provide evidence that these sociodemographics are integrally associated with outcomes and should be included in the risk analysis.
POSTSURGICAL OUTCOMES: HYPOPLASTIC LEFT HEART SYNDROME
Successful surgical treatment for hypoplastic left heart syndrome (HLHS) is considered an important quality indicator for pediatric cardiac surgical programs. HLHS is the eighth most common congenital heart defect and occurs in 1.8/10,000 live births. Cardiac surgery during the neonatal period is often very complex and is associated with high mortality and morbidity. The 12-month survival or freedom from cardiac transplantation after Norwood Stage I surgical repair and the subsequent Bidirectional Glenn procedure is between 64% and 74% (5).
RACE AND ETHNICITY
Association with Congenital Heart Defects
Population-based national estimates for selected birth defects including ethnic/racial variation between 1999 and 2001 were reported in 2006 by Canfield. Racial and ethnic patterns for several congenital cardiac defects were described with truncus arteriosus, tetralogy of Fallot, and atrioventricular canal occurring most frequently in non-Hispanic blacks. For Transposition of the great arteries and HLHS, the prevalence is greatest in non- Hispanic whites.
Association with Genetic Syndromes
The prevalence of genetic syndromes differs by race and ethnicity. Down syndrome (trisomy 210) has the highest prevalence Hispanics followed by non-Hispanic whites. Non-Hispanic blacks have the highest rate of trisomy 13 and trisomy 18 (6). The annual report for birth defects in Hawaii recorded the prevalence of Turner syndrome for the seven racial/ethnic groups. Rates were highest for Japanese, black, and Chinese followed by white and Filipino and lowest for Hawaiian and Samoan (7).
The presence of a known chromosomal syndrome doubles the risk of death after surgery for hypoplastic heart syndrome. The most common in the HLHS population is Turner syndrome. Mortality is increased in the patients with a known genetic syndrome, although the cause of death is usually not attributed to the noncardiac defect (8).
Association with Low Birth Weight
Low birth weight significantly increases mortality and morbidity after cardiac surgery in infancy (9). Nembhard in 2009 (10) outlined the risks of preterm birth (PTB) in infants with congenital heart disease by ethnic group. “The greatest risk for PTB was for non-Hispanic black infants with conotruncal CHD. Non-Hispanic blacks with Truncus Arteriosus, Transposition of the Great Vessels and Tetralogy of Fallot had an increased risk of PTB compared to non-Hispanic whites” (odds ratio [OR] = 4.8, 3.1, and 2.0, respectively; all p < .05). Non-Hispanic blacks with HLHS had 2.0 times the risk for PTB as non-Hispanic whites (10). Preterm birth is associated with low birth weight; therefore, mortality rates after Norwood Stage I operation may be associated with racial/ethnic factors.
Association with Mortality
A secondary analysis using data in a national study on hospital mortality after Norwood stage (11) indicated that the mortality rate for whites was 21.1% (n = 52) and for nonwhites was 27.8% (n = 58). The secondary analysis was completed by constructing a two-by-two contingency table to observe the difference in mortality based on race. Race differences approximated statistical significance (p = .06) based on a c2 test (one-tailed Fisher’s exact test).
GENDER
Gender has been shown to influence survival after infant heart surgery. Males are more likely to have more complex congenital cardiac surgery in infancy, which often requires multiple surgical procedures. However, the mortality rate after risk adjusting for females was found to be significantly higher (OR = 1.2; 95% confidence interval [CI] = 1.08–1.36) in the high-risk group. The authors concluded that “this is the largest study to document that the overall adjusted risk of in-hospital mortality was 21% higher in females but this was accounted for only by female neonates who had a RACHS-1 risk category of 4 to 6, a group that comprised less than 15% of all those undergoing cardiac surgery but accounted for as much as 40% of all CHD surgical deaths” (12).
SOCIOECONOMIC STATUS
Socioeconomic status is an important factor influencing surgical mortality in adults. In a review of more than one million medical records for 13 complex surgical procedures and calculation of SES on median household incomes using zip code data, univariate analyses indicated that patient SES, race, insurance status, admission status, hospital procedure-specific volume, and hospital SES were all significant predictors of postoperative survival. Multivariate analysis after adjustment for patient and hospital factors showed that SES was the strongest indicator for survival. A single-level decrease is SES was associated with a 7.1% increased operative mortality risk (13).
Association with Access to Care
The combination of geographic location and SES is known to affect access to care. Families of patients from SES backgrounds have limited resources for researching surgical options. For example, only approximately one-third of Americans have Internet access. However, Internet access is very low among racial–ethnic minorities and individuals from low SES backgrounds. Consequently, they are often unable to compare outcomes from individual institutions and therefore cannot select those institutions where the highest quality care is offered based on published outcomes. Higher SES is associated with behaviors that seek a higher procedure volume and institutional reputation for a given surgical specialty, and this could be extremely important in high-risk neonatal cardiac surgical procedures. It may be necessary to travel to another city to access a higher quality of care and that may not be possible with low SES. Therefore, SES appears to be a critical variable associated with surgical outcomes.
Geographic location and the type of institution (teaching vs. nonteaching) significantly influences Norwood Stage I mortality (14). Hospital mortality for Norwood Stage I was 31.3% in the South vs. 11.2% in the Northeast (11). More than 10 years ago in 1997, the difference in mortality for teaching vs. nonteaching hospitals was 17% and that was reduced to only 3% by 2000. In 1997, surgical mortality after Norwood Stage I in hospitals performing one to two procedures/year approached 50%. Recognition of this high mortality in nonteaching centers during this time period caused a shift in surgical volume to teaching hospitals.
Association with Neurodevelopmental Outcomes
In a review of 2-year survival and mental development scores after the Norwood operation, regression analysis showed that SES as determined by the Bishen Index (15) was an independent predictor of Mental Development Index (MDI) scores ( p = .01). Patients in this study had the Modified Blalock-Taussig shunt in the earlier period and then right ventricle to pulmonary artery in the later era (starting in 2002). Regardless of the type of primary repair, lower SES was associated with a decreased MDI score. In the same study, gender was found to be an independent predictor of the Psychomotor Development Index (PDI) score and male gender was associated with lower PDI scores (p = .03) (16).
Association with Available Resources after Surgery
Interstage mortality is greatly reduced by home surveillance programs. Home surveillance includes daily oxygen saturation monitoring and weight measurement and is associated with a reduction in interstage mortality from 15% to 0% (17). The cost of these programs, the time commitment, and the equipment involved may be a challenge for families with low SES. Patients with HLHS require a tremendous amount of postoperative care to maintain consistent weight gain and prevent infection to successfully progress through all three operations and thus available resources are critical to their outcome.
LACK OF RESEARCH PARTICIPATION AMONG MINORITIES
Assessment of outcomes in minority patient populations is especially difficult as a result of decreased enrollment in clinical research studies. One example is the significant difference in the number enrolled patents who returned for follow-up in a study on neurodevelopmental outcomes after surgery for HLHS, 56% vs. 44%, white vs. nonwhite (18). A secondary analysis of published data based on c2 analysis indicates that this is a highly significant difference (p < .001).
CONCLUSION
Disparities in outcomes associated with race, ethnicity, gender, and SES are present in survival after complex surgery during infancy. Although they are traditionally considered “associated factors,” they may be more important to outcomes than previously thought and should be considered in the development of risk models for survival and neurodevelopmental outcomes in this population. We believe these sociodemographic factors should at least be included in the risk analysis to help explain their impact on the outcomes in the future. Although they may be associated with other risk factors, in some models, they can potentially play a significant role in predicting outcomes.
REFERENCES
- 1.National HealthCare Disparities Report—U.S. Department of Health and Human Services Agency for Healthcare Research and Quality, AHRQ Publication No. 09-0002. March 2009. [Google Scholar]
- 2.Gomes C, McGuire TG. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment, Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003:4. [PubMed] [Google Scholar]
- 3.American Psychological Association. Publication Manual of the American Psychological Association, 5th edition; 2001:18. [Google Scholar]
- 4.Ellis C.. Does race/ethnicity really matter in adult neurogenics? Am J Speech Lang Pathol. 2009;18:310–314. [DOI] [PubMed] [Google Scholar]
- 5.Ohye RG, Sleeper LA, Mahony L, et al. . Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362:1980–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Canfield MA, Honein MA, Yuskiv N, et al. . National estimates and race/ethnic-specific variation of selected birth defects in the United States, 1999–2001. Birth Defects Res A Clin Mol Teratol. 2006;76:747–756. [DOI] [PubMed] [Google Scholar]
- 7.Merz RD, Forrester MB.. Hawaii Birth Defects Program, 1986–1999 Statewide Data, Surveillance Report Number 8 on Birth Defects in Hawaii, January 1, 1986–December 31, 1999. December 2000:1–126. [Google Scholar]
- 8.Patel A, Hickey E, Mavroudis C, et al. . Impact of noncardiac congenital and genetic abnormalities on outcomes in hypoplastic left heart syndrome. Ann Thorac Surg. 2010;89:1805–1813. [DOI] [PubMed] [Google Scholar]
- 9.Ades AM, Dominguez TE, Nicolson SC, et al. . Morbidity and mortality after surgery for congenital cardiac disease in the infant born with low weight. Cardiol Young. 2010;20:8–17. [DOI] [PubMed] [Google Scholar]
- 10.Nembhard WN, Salemi JL, Loscalzo ML, Wang T, Hauser KW.. Are black and Hispanic infants with specific congenital heart defects at increased risk of preterm birth? Pediatr Cardiol. 2009;30:800–809. [DOI] [PubMed] [Google Scholar]
- 11.Hirsch JC, Gurney JG, Donohue JE, Gebremariam A, Bove EL, Ohye RG.. Hospital mortality for Norwood and arterial switch operations as a function of institutional volume. Pediatr Cardiol. 2008;29:713–717. [DOI] [PubMed] [Google Scholar]
- 12.Marelli A, Gauvreau K, Landzberg M, Jenkins K.. Sex differences in mortality in children undergoing congenital heart disease surgery: A United States population-based study. Circulation. 2010;122(Suppl):S234–S240. [DOI] [PubMed] [Google Scholar]
- 13.Bennett KM, Scarborough JE, Pappas TN, Kepler TB.. Patient socioeconomic status is an independent predictor of operative mortality. Ann Surg. 2010;252:552–557. [DOI] [PubMed] [Google Scholar]
- 14.Berry JG, Cowley CG, Hoff CJ, Srivastava R.. In-hospital mortality for children with hypoplastic left heart syndrome after stage I surgical palliation: Teaching versus nonteaching hospitals. Pediatrics. 2006;117:1307–1313. [DOI] [PubMed] [Google Scholar]
- 15.Blishen BR.. The 1981 socioeconomic index for occupations in Canada. Can Rev Soc Antropol. 1987;24:465–488. [Google Scholar]
- 16.Atallah J, Dinu IA, Joffe AR, et al. . Two-year survival and mental and psychomotor outcomes after the Norwood procedure: An analysis of the modified Blalock-Taussig shunt and right ventricle-topulmonary artery shunt surgical eras. Circulation. 2008;118:1410–1418. [DOI] [PubMed] [Google Scholar]
- 17.Ghanayem NS, Hoffman GM, Mussatto KA, et al. . Home surveillance program prevents interstage mortality after the Norwood procedure. J Thorac Cardiovasc Surg. 2003;126:1367–1377. [DOI] [PubMed] [Google Scholar]
- 18.Tabbutt S, Nord AS, Jarvik GP, et al. . Neurodevelopmental outcomes after staged palliation for hypoplastic left heart syndrome. Pediatrics. 2008;121:476–483. [DOI] [PubMed] [Google Scholar]


