Abstract:
Multiple studies have evaluated the efficacy of pulsatile flow during cardiopulmonary bypass (CPB) showing controversial results. Suggested benefits to pulsatile perfusion include reducing the systemic inflammatory response syndrome associated with bypass, decreased need for inotropic support, shortened hospital stay, and superior organ preservation. This study aims to compare prior studies to determine if there is a significant difference in post-operative renal function with pulsatile perfusion compared to non-pulsatile perfusion during cardiac surgery. Studies included in the analysis were identified by searching keywords - pulsatile perfusion, pulse, pulsatile flow, cardiopulmonary bypass, and cardiac surgery. To maintain a homogenous sample, manuscripts were included if they met the following criteria: research was prospective in nature, subjects were human, paper contained documented baseline demographics, outcome data included markers of renal function. A meta-analysis was performed to compare post-op renal function between pulsatile and non-pulsatile perfusion groups. A total of 298 articles were screened. Ten articles met the criteria, of these, 477 patients underwent non-pulsatile perfusion while 708 received pulsatile perfusion during CPB. There was insufficient evidence to show a difference in mean postoperative creatinine or BUN between the groups, however, the pulsatile perfusion group had significantly higher creatinine clearance (standardized difference in means = 2.48, p = .004) and lower serum lactate levels (standardized difference in means = −2.08, p = .012) in the intensive care unit. This study found that there is great variability among pulsatile perfusion research. The methods to create and assess effective pulsatility on bypass varied widely among manuscripts. This analysis suggests that pulsatile perfusion during CPB is beneficial in renal preservation and should be considered.
Keywords: pulsatile perfusion, pulse, meta-analysis, renal, kidney
Multiple studies have looked at the efficacy of pulsatile flow during cardiopulmonary bypass (CPB) and show controversial results. Advantages to pulsatile per-fusion include a reduction of systemic inflammatory response syndrome and endocrine response associated with bypass, superior organ preservation as seen by better cerebral perfusion, decreased need for inotropic support, better myocardial function, less pulmonary edema and intubation times, greater urine output, and lower lactate levels post bypass (1–6). Disadvantages may include greater hemolysis and gaseous micro emboli production when pulsatile perfusion is used (7,8). The practice of pulsatile perfusion during CPB is accomplished using either an intra-aortic balloon pump, pulsatile roller pump, or a rotational pump, such as the Medos Deltastream (Stolberg, Germany). Pulsatile perfusion is quantified by pulse pressure or energy equivalent pressure (9,10). The energy equivalent pressure takes into account the hemodynamic energy gradient rather than a pressure gradient during each pulse cycle. The purpose of this meta-analysis is to compare prior studies published on the use of pulsatile perfusion during CPB to determine if there is a significant difference in postoperative renal function with pulsatile perfusion compared with non-pulsatile perfusion during cardiac surgery.
METHODS
A literature search was performed using PubMed, Ovid, and Medline databases. The original keyword search included “pulsatile perfusion,” “pulse, pulsatile flow,” “cardiopulmonary bypass,” and “cardiac surgery.” No date restrictions were placed on the search. To maintain a homogenous sample, manuscripts were included if they met the following criteria: research was prospective in nature, subjects were human, paper contained documented baseline demographics, and outcomes data included markers of renal function.
The following data were extracted from each study meeting the inclusion criteria: first author, year of publication, study type, number of subjects, method of pulsatile perfusion, demographics data, and outcomes data. Demographics data included preoperative creatinine, preoperative creatinine clearance (CrCl), preoperative blood urea nitrate (BUN), cardiopulmonary bypass (CPB) time, cross clamp time, and mean arterial pressure (MAP) on bypass. Outcome data was retrieved wherever possible on the following variables of interest: intensive care unit length of stay, hospital length of stay, creatinine, CrCl, BUN, systemic vascular resistance (SVR), and serum lactate levels.
A meta-analysis was performed using Comprehensive Meta-Analysis version 2.2 (Biostat, Englewood, NJ) for Windows (Microsoft Corp, Redmond, WA). Data are expressed as standardized difference in mean and standard error. A random effects model was used when heterogeneity of effect sizes was present.
RESULTS
A total of 298 articles were initially identified by the keyword search. Ten articles met the inclusion criteria (Table 1). In these 10 studies, a total of 708 patients received pulsatile perfusion during bypass and 477 underwent non-pulsatile perfusion.
Table 1.
Articles included in meta-analysis.
| Article | Pediatrics or Adults | Sample Size (PP/NP) | Method of Pulsatility |
|---|---|---|---|
| Badner et al., 1992 (11) | Adults | 27/26 | Roller pump |
| Louagie et al., 1992 (12) | Adults | 50/50 | Roller pump |
| Poswal et al., 2004 (13) | Adults | 50/50 | Roller pump |
| Onorati et al., 2005 (14) | Adults | 20/20 | IABP |
| Alkan et al., 2006 (15) | Pediatrics | 25/25 | Roller pump |
| Alkan et al., 2007 (16) | Pediatrics | 151/64 | Roller pump |
| Onorati et al., 2007 (17) | Adults | 50/50 | IABP |
| Onorati et al., 2009a (18) | Adults | 40/40 | IABP |
| Onorati et al., 2009b (19) | Adults | 87/71 | IABP |
| Akcevin et al., 2010 (20) | Pediatrics | 208/81 | Roller pump |
PP, pulsatile perfusion; NP, non-pulsatile perfusion; IABP, intra-aortic balloon pump.
The standardized difference in means was used to determine significant difference. There was no significant difference between groups for pre-operative creatinine, CrCl, CPB time, or cross clamp time (Table 2). The on-bypass MAP was significantly lower in the pulsatile group (p = .03), however the difference was less than 2 mmHg.
Table 2.
Demographic data.
| PP (mean) | NP (mean) | Standardized Difference in Means | Standard Error | Significance | |
|---|---|---|---|---|---|
| Pre-op Creatinine (mg/dL) | .83 | .85 | −.01 | .07 | NS |
| Pre-op CrCl (mL/min) | 70.6 | 70.1 | −.3 | .26 | NS |
| CPB Time (min) | 103.65 | 104.23 | .11 | .1 | NS |
| XC Time (min) | 65.33 | 64.95 | .32 | .24 | NS |
| MAP (mmHg) | 67.4 | 69.2 | −.99 | .46 | .03 |
PP, pulsatile perfusion; NP, non-pulsatile perfusion; XC, cross clamp; NS, not significant.
Data did not show a significant difference in means between groups for post-operative creatinine, BUN, or SVR. Post-operative CrCl was significantly greater with pulsatile perfusion (Z = 2.88, standardized difference in means = 2.48, standard error = .86, range .79–4.16, p <.01) (Figure 1). There was also a significant reduction in post-operative serum lactate levels with pulsatile perfusion (Z = −2.52, standardized difference in means = −2.079, standard error = .83, range −3.7–.46, p = .01) (Figure 2). Studies using an intra-aortic balloon pump to generate pulsatile perfusion had more favorable results than other methods.
Figure 1.
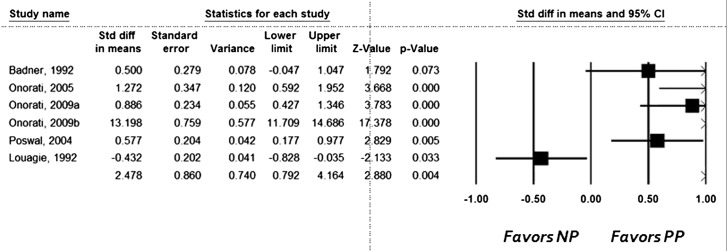
Meta-analysis results for postoperative CrCl. The standardized difference in means is represented as PP-NP, where PP = pulsatile perfusion, and NP = nonpulsatile perfusion.
Figure 2.
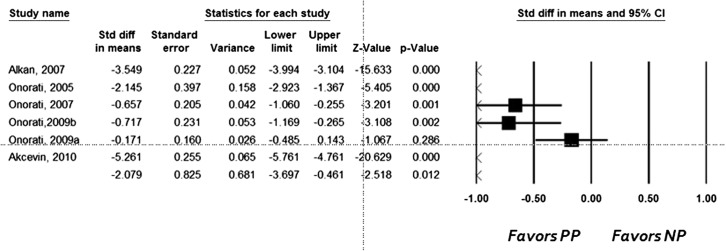
Meta-analysis results for postoperative serum lactate levels. The standardized difference in means is represented as PP-NP, where PP = pulsatile perfusion, and NP = nonpulsatile perfusion.
DISCUSSION
There are many physiologic alterations that occur during bypass that can lead to renal dysfunction including exposure of blood to a foreign surface, hemodilution, hypothermia, and non-pulsatile blood flow. During CPB, hemodilution is often used to reduce homologous blood requirements and decrease blood viscosity, while hypothermia is used to protect organs by lowering oxygen consumption, thus allowing for decreased perfusion flows during hypothermia (21). Hypothermia and hemodilution tend to act as opposing forces in relation to blood viscosity. Similarly, as hemodilution decreases oxygen-carrying capacity, hypothermia decreases oxygen demand. An animal study, by Utley et al., comparing the effects of hypothermia and hemodilution on blood flow, oxygen delivery, and renal function found that both hypothermia and hemodilution decrease MAP, reduce blood flow in the outer and inner renal cortex, and decrease oxygen delivery to the kidneys (22). Hemodilution was also found to increase urine output, thus being somewhat beneficial to kidney function.
Non-pulsatile perfusion may impact the kidney more than other organs because renin secretion is increased with non-pulsatile perfusion, which increases SVR during bypass and causes redistribution of intra-renal blood flow (23–25). Many studies have shown an increase in renin secretion during non-pulsatile flow, probably due to decreased renal pulse pressure stimulating the release of renin (26). This has a pronounced effect on the kidney and can lead to acute renal insufficiency or failure.
Other physiologic effects of non-pulsatile blood flow include release of catecholamines, vasopressin, and local tissue vasoconstrictors, resulting in vasoconstriction and increased afterload (27). It is suggested that there is a decrease in vasomotor reflexes in the aortic arch and carotid sinus with non-pulsatile perfusion, which may be a cause of increased SVR. Increases in SVR are also thought to occur due to the increased synthesis and release of endothelin by the vasculature onto smooth muscle cells (28). It is suggested that the release of endothelin may be associated with absence of pulsatile perfusion, as well as decreased pulmonary flow, stress of surgery, and thromboxane release from activated platelets (29). Other authors suggest that an increase in SVR may be caused by a decrease in hydraulic energy with non-pulsatile perfusion. This may cause loss of patency in the microcirculation of small arterioles and precapillary sphincters (30), which decreases perfusion and gas exchange at the capillary level. As a result, some ischemia occurs, which is represented by increased lactate levels and acidosis. Increased afterload has an additional deleterious effect on the heart as the cross clamp is removed and the left ventricle attempts to pump against increased SVR (31,32). Some studies show improved cardiac function in patients with pulsatile per-fusion compared with non-pulsatile perfusion (33).
Studies suggest that increased serum lactate levels during and after bypass are an independent predictor of morbidity and mortality after pediatric and adult cardiac surgery (34,35). Prior studies have shown a decrease in tissue oxygen pressure and an increase in lactate levels with non-pulsatile perfusion (36). We hypothesized that when peripheral perfusion and organ perfusion on bypass is improved by implementing pulsatile perfusion, the tissues will be able to extract more oxygen and thereby produce less lactate. This study suggests that pulsatile per-fusion provides a benefit to renal function compared with non-pulsatile perfusion as seen by decreased lactate levels and increased CrCl in the pulsatile perfusion group.
There were several limitations to this study. Studies included used different modalities of pulsatile perfusion, both pediatric and adult studies were used, and quantification of pulsatile perfusion was not always reported. The studies used in this meta-analysis did not follow the same hypothermia (28–33°C) or homologous blood transfusion protocols, which may have influenced the final outcome. However, within the analysis there was approximately an even number of patients in the pulsatile and non-pulsatile groups represented from each study. Additionally, publication bias always exists, with researchers tending to publish positive results more often than insignificant findings.
CONCLUSION
This study found that pulsatile perfusion results in greater creatinine clearance and reduced post-operative lactate levels compared with non-pulsatile perfusion, suggesting that pulsatile perfusion is beneficial in renal preservation and increases oxygen delivery to the tissues. In the studies included in this meta-analysis, patients received pulsatile or non-pulsatile perfusion without regard to their individual risk for renal failure. We hypothesize that selected patients at a high risk for renal failure following cardiopulmonary bypass may especially benefit from the use of pulsatile perfusion to maximize renal blood flow.
REFERENCES
- 1.Lonzarone E, Gelmini F, Tessari M, Menon T, Suzuki H.. Preservation of endothelium nitric oxide release by pulsatile flow cardiopulmonary bypass when compared with continuous flow. Artif Organs. 2009;33:926–934. [DOI] [PubMed] [Google Scholar]
- 2.Sezai A, Shiono M, Nakata K, et al. Effects of pulsatile CPB on interleukin-8 and endothelin-1 levels. Artif Organs. 2005;29:708–713. [DOI] [PubMed] [Google Scholar]
- 3.Akcevin A, Alkan-Bozkaya T, Qiu F, Undar A.. Evaluation of perfusion modes on vital organ recovery and thyroid hormone homeostasis in pediatric patients undergoing cardiopulmonary bypass. Artif Organs. 2010;34:879–884. [DOI] [PubMed] [Google Scholar]
- 4.Murkin JM, Martzke JS, Buchan AM, Bentley C, Wong CJ.. A randomized study of the influence of perfusion technique and pH management strategy in 316 patients undergoing coronary artery bypass surgery. J Thorac Cardiovasc Surg. 1995;110:340–347. [DOI] [PubMed] [Google Scholar]
- 5.Alkan T, Akcevin A, Undar A, Turkoglu H, Paker T, Aytac A.. Benefits of pulsatile perfusion on vital organ recovery during and after pediatric open heart surgery. ASAIO. 2007;53:651–654. [DOI] [PubMed] [Google Scholar]
- 6.Undar A, Masai T, Beyer EA, et al. Pediatric physiologic pulsatile pump enhances cerebral and renal blood flow during and after cardiopulmonary bypass. Artif Organs. 2002;26:919–923. [DOI] [PubMed] [Google Scholar]
- 7.Zhao J, Liu JP, Feng ZY, Liu YL, Li SJ, Long C.. Clinical application of pulsatile perfusion during cardiopulmonary bypass in pediatric heart surgery. ASAIO. 2009;55:300–303. [DOI] [PubMed] [Google Scholar]
- 8.Schreiner RS, Rider AR, Myers JW, et al. Microemboli detection and classification by innovative ultrasound technology during simulated neonatal cardiopulmonary bypass at different flow rates, perfusion modes, and perfusate temperatures. ASAIO. 2008;54:316–324. [DOI] [PubMed] [Google Scholar]
- 9.Shepard RB, Simpson DC, Sharp JF.. Energy equivalent pressure. Arch Surg. 1966;93:730–740. [DOI] [PubMed] [Google Scholar]
- 10.Undar A.. Myths and truths of pulsatile and nonpulsatile perfusion during acute and chronic cardiac support. Artif Organs. 2004;28:439–443. [DOI] [PubMed] [Google Scholar]
- 11.Badner NH, Murkin JM, Lok P.. Differences in pH management and pulsatile/nonpulsatile perfusion during cardiopulmonary bypass do not influence renal function. Anesth Analg. 1992;75:696–701. [DOI] [PubMed] [Google Scholar]
- 12.Louagie YA, Gonzalez M, Collard E, et al. Does flow character of cardiopulmonary bypass make a difference? J Thorac Cardiovasc Surg. 1992;104:1628–1638. [PubMed] [Google Scholar]
- 13.Poswal P, Mehta Y, Juneja R, et al. Comparative study of pulsatile and nonpulsatile flow during cardio-pulmonary bypass. Ann Card Anaesth. 2004;7:44–50. [PubMed] [Google Scholar]
- 14.Onorati F, Cristodoro L, Mastroroberto P, et al. Should we discontinue intraaortic balloon during cardioplegic arrest? Splanchnic function results of a prospective randomized trial. Ann Thorac Surg. 2005;80:2221–2228. [DOI] [PubMed] [Google Scholar]
- 15.Alkan T, Akcevin A, Undar A, et al. Effects of pulsatile and nonpulsatile perfusion on vital organ recovery in pediatric heart surgery: A pilot clinical study. ASAIO. 2006;52:530–535. [DOI] [PubMed] [Google Scholar]
- 16.Alkan T, Akcevin A, Undar A, et al. Benefits of pulsatile perfusion on vital organ recovery during and after pediatric open heart surgery. ASAIO. 2007;53:651–654. [DOI] [PubMed] [Google Scholar]
- 17.Onorati F, Presta P, Fuiano G, et al. A randomized trial of pulsatile perfusion using an intraaortic balloon pump versus nonpulsatile perfusion on short-term changes in kidney function during cardiopulmonary bypass during myocardial reperfusion. Am J Kidney Dis. 2007;50:229–238. [DOI] [PubMed] [Google Scholar]
- 18.Onorati F, Santarpino G, Rubino AS, et al. Body perfusion during adult cardiopulmonary bypass is improved by pulsatile flow with intra-aortic balloon pump. Int J Artif Organs. 2009;32:50–61. [DOI] [PubMed] [Google Scholar]
- 19.Onorati F, Santarpino G, Presta P, et al. Pulsatile perfusion with intraaortic balloon pumping ameliorates whole body response to cardiopulmonary bypass in the elderly. Crit Care Med. 2009;37:902–911. [DOI] [PubMed] [Google Scholar]
- 20.Akcevin A, Alkan-Bozkaya T, Qiu F, Undar A.. Evaluation of perfusion modes on vital organ recovery and thyroid hormone homeostasis in pediatric patients undergoing cardiopulmonary bypass. Artif Organs. 2010;34:879–884. [DOI] [PubMed] [Google Scholar]
- 21.Swain JA, McDonald TJ Jr, Griffith PK, et al. Low-flow hypothermic cardiopulmonary bypass protects the brain. J Thorac Cardiovasc Surg. 1991;102:76–83. [PubMed] [Google Scholar]
- 22.Utley JR, Wachtel C, Cain RB, Spaw EA, Collins JC, Stephens DB.. Effects of hypothermia, hemodilution, and pump oxygenation on organ water content, blood flow and oxygen delivery, and renal function. Ann Thorac Surg. 1981;31:121–133. [DOI] [PubMed] [Google Scholar]
- 23.Many M, Soroff HS, Birtwell WC, et al. The physiologic role of pulsatile and non-pulsatile blood flow. Effects on renal function. Arch Surg. 1968;95:762–767. [DOI] [PubMed] [Google Scholar]
- 24.Taylor KM, Bain WH, Morton JJ, et al. The role of angiotensin II in the development of peripheral vasoconstriction during open heart surgery. Am Heart J. 1980;100:935–937. [DOI] [PubMed] [Google Scholar]
- 25.Norman JC.. Renal complications of cardiopulmonary bypass. Dis Chest. 1968;54:50–54. [DOI] [PubMed] [Google Scholar]
- 26.Kohlstaedt LA, Page IH.. The liberation of renin by perfusion of kidneys following reduction of pulse pressure. J Exp Med. 1940;72:201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minami K, Korner MM, Vyska K, et al. Effects of pulsatile perfusion on plasma catecholamine levels and hemodynamics during and after cardiac operations with cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1990;99:82–91. [PubMed] [Google Scholar]
- 28.Miyauchi T.. Pathophysiology of endothelin in the cardiovascular system. Annu Rev Physiol. 1999;6:391–415. [DOI] [PubMed] [Google Scholar]
- 29.Spinale FG.. The bioactive peptide endothelin causes multiple biologic responses relevant to myocardial and vascular performance after cardiac surgery. J Thorac Cardiovasc Surg. 1990;123:1031–1034. [DOI] [PubMed] [Google Scholar]
- 30.Milnor WR.. Pulsatile blood flow. N Engl J Med. 1972;287:27–21. [DOI] [PubMed] [Google Scholar]
- 31.Hornick P, Taylor K.. Pulsatile and non-pulsatile perfusion: The continuing controversy. J Cardiothorac Vasc Anesth. 1997;11:310–315. [DOI] [PubMed] [Google Scholar]
- 32.Sonnenblick E, Downing S.. Afterload as a primary determinant of ventricular performance. Am J Physiol. 1963;204:604–608. [DOI] [PubMed] [Google Scholar]
- 33.Murkin JM, Martzke JS, Buchan AM, et al. A randomized study of the influence of perfusion technique and pH management strategy in 316 patients undergoing coronary artery bypass surgery. I. Mortality and cardiovascular morbidity. J Thorac Cardiovasc Surg. 1995;110:340–347. [DOI] [PubMed] [Google Scholar]
- 34.Monoz R, Laussen PC, Palacio G, Zienko L, Piercey G, Wessel DL.. Changes in whole blood lactate levels during cardiopulmonary bypass for surgery for congenital cardiac disease: An early indicator of morbidity and mortality. J Thorac Cardiovasc Surg. 2000;119:155–162. [DOI] [PubMed] [Google Scholar]
- 35.Demers P, Elkouri A, Martineau R, Couturier A, Cartier R.. Outcome with high blood lactate levels during cardiopulmonary bypass in adult cardiac operation. Ann Thorac Surg. 2000;70:2082–2086. [DOI] [PubMed] [Google Scholar]
- 36.Mukherjee ND, Beran AV, Hirai J.. In vivo determination of renal tissue oxygenation during pulsatile and non-pulsatile left heart bypass. Ann Thorac Surg. 1973;15:334–363. [DOI] [PubMed] [Google Scholar]


