Abstract:
The project goal was to reduce waste disposal volume, costs and minimize the negative impact that regulated waste treatment and disposal has on the environment. This was accomplished by diverting bypass circuits from the traditional regulated medical waste (RMW) to clear bag waste, or municipal solid waste (MSW). To qualify circuits to be disposed of through MSW stream, the circuits needed to be void of any free-flowing blood and be “responsibly clear.” Traditionally the perfusion bypass circuit was emptied through the cardioplegia pump starting shortly after decannulation and heparin reversal. Up to 2000 mL of additional prime solution was added until the bypass circuit was rinsed clear. Three hundred sixty of 400 procedures (90%) had a complete circuit rinse and successful diversion to MSW. An additional 240 mL of processed cell salvage blood was available for transfusion. No additional time was spent in the operating room as a result of this procedure. Based on our procedure case volume and circuit weight of 15 pounds, almost 15,000 pounds (7.5 tons) of trash will be diverted from RMW. This technique represents another way for perfusionists to participate in sustainability efforts. Diverting the bypass circuit to clear bag waste results in a reduced environmental impact and annual cost savings. The treatment of RMW is associated with various environmental implications. MSW, or clear bag waste, on the other hand can now be disposed of in waste-to-energy facilities. This process not only releases a significantly less amount of carbon dioxide into the environment, but also helps generate renewable energy. Therefore, the bypass circuit diversion pilot project effectively demonstrates decreases in the carbon footprint of our organization and overall operating costs.
Keywords: cardiopulmonary bypass, cardiac surgery, blood management, alternative perfusion techniques, total quality management, best evidence-based practices, safety
Regulated medical waste (RMW), also known as red bag waste, is produced primarily in operating rooms and acute care areas. As the country’s largest industry, hospitals produce approximately 5 millions pounds of waste per year (1). Additionally, little has been written in regard to contributions made by cardiac surgery services, one of the most common surgeries performed, either as being a primary contributor to this waste stream or by the efforts to reduce the amount of generated RMW. As part of sustainability efforts at our institution, our group worked to divert the heart–lung machine (HLM) bypass circuits from the traditional RMW to clear bag waste, or municipal solid waste (MSW). The goal was to reduce waste disposal volume, minimize the negative impact that regulated waste treatment and disposal has on the environment, and to possibly reduce costs. We aimed to maintain the same level of labor output and supply use, all while maintaining employee safety.
According to New York State regulations, hospital staff is required to dispose of any item(s) saturated with blood or that contain free-flowing blood as regulated medical waste (2). However, according to these same regulations, plastic materials that have not come in contact with infectious materials may be disposed of carefully and MSW need not be labeled as hazardous waste. Furthermore, rinsing free-flowing blood from perfusion bypass circuit tubes postoperatively leaving the plastic container and appendages visually clear qualifies the HLM circuits to be disposed of by MSW stream.
METHODS
The HLM circuit consisted of an integrated oxygenator, tubing, centrifugal pump, and cardioplegia delivery kit only. The cell salvage set-up was excluded from the rinsing process. Traditionally our HLM bypass circuit was chased with saline into the salvage device through the cardioplegia delivery pump starting shortly after decannulation and heparin reversal. When a satisfactory cardiac output was obtained and the skin was completely closed, the entire circuit was suctioned out to the Cell Saver 5 cell-salvage device (CSD; Haemonetics). For this study a more complete rinsing was accomplished.
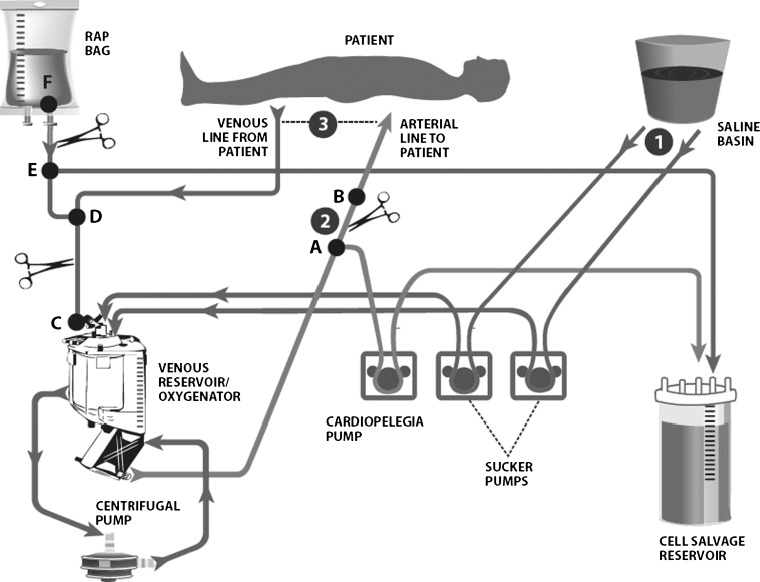
The HLM circuit was similar for all procedures. During the pilot of this evaluation, five circuits were weighed postprocedure and the average weight was 15 pounds. Only adult cases were included in this trial. The steps were similar to our traditional procedure of emptying the HLM. However (Figure 1), shortly after termination of bypass, 300 mL of saline was aspirated through each of the table suction lines (Step 1). The arterial line was clamped between Points A and B. The circuit was then almost completely emptied into the CSD (Step 2). A liter of saline was added to the venous reservoir. The arteriovenous loop was reconnected (Step 3). A quarter-inch sterile line from the CSD was then connected to the retrograde autologus priming (RAP) bag, which was also “wyed” down into the venous line. The venous line was then clamped between the RAP line and the venous reservoir (Points C and D) to allow for the bypass circuit fluid to be completely diverted into the CSD. When the recirculating bypass circuit fluid and all purge/sampling lines were clear, no more fluid was added and the bypass circuit was completely aspirated of all saline. The cell salvage blood was processed and sent to the delivery bag and disconnected from the CSD. We then used the quarter-inch aspiration line to aspirate out additional remaining fluid from the stopcocks for compete circuit emptying. Up to 2000 mL of additional prime solution was added until the bypass circuit was rinsed clear. All syringes were removed from the circuit before disposal and placed in a sharps container.
Figure 1.
Heart–lung machine (HLM) circuit with listed steps for rinsing: Step 1—aspiration of .9% sterile saline solution saline solution into table suction lines to the HLM; Step 2—active pumping of HLM reservoir blood to cell salvage reservoir; Step 3—reconnection of arteriovenous loop and active pumping to the cell salvage reservoir. Points A through E are listed for descriptive reference.
RESULTS
Of 400 consecutive procedures, 360 (90%) had a complete circuit rinse and successful diversion to MSW. The complete rinse was based on perfusion staff observation. Figure 2 depicts the effectiveness of the circuit rinsing. On average, an additional 240 mL of processed cell salvage blood was available for transfusion. Additionally, the cell salvage blood was available sooner since the rinsing process was initiated and completed at an early stage of surgery. This was a result of having more blood to process and not having to discard incomplete bowls from the CSD. Because more blood was available, we were able to use processed blood to fill any incomplete bowls.
Figure 2.

Effectiveness of perfusion circuit rinsing.
Although slightly more effort is involved with this procedure, no additional time was spent in the operating room. Average total operating room time was 332 minutes for the study group vs. 330 minutes for historic operating room time. Approximately 1800 mL of rinse solution was required to accomplish complete rinsing of the bypass circuit. The cost of additional saline rinse was less than $2.00. There were no employee incidents related to this procedure. Based on an average circuit weight of 15 pounds and our procedure case volume of 1,000 cases, 15,000 pounds (7.5 tons) of trash will be diverted from RMW.
CONCLUSIONS
This technique represents another way for perfusionists to participate is sustainability efforts within their medical facility. Diverting the bypass circuit to clear bag waste results in reduced environmental impact and annual cost savings. The treatment of RMW is associated with various environmental implications (3). Before disposal, RMW must be decontaminated through various processes. Auto-claving, a popular process used to steam sterilize RMW, does contribute to the nation’s dioxins and mercury emissions. Another process for handling RMWis incineration, a process that is a leading source of dioxin, mercury, and lead. These common disposal methods emit hazardous air pollutants that are known or suspected to cause cancer or other serious health effects such as reproductive effects or birth defects or adverse environmental effects (4,5). MSW, or clear bag waste, on the other hand can now be disposed of in waste-to-energy facilities, a process that not only releases a significantly less amount of carbon dioxide into the environment, but also helps generate renewable energy. Another benefit of this technique is reduced cost. At a cost of five times higher, RMW significantly adds to operating expenses. Therefore, the bypass circuit diversion pilot project effectively demonstrates decreases in the carbon footprint of our organization and overall operating costs.
DISCUSSION
This technique represents another way for perfusionists to participate is sustainability efforts within their medical facility. It also provides evidence that other disposable products that cannot be reprocessed can most likely be rinsed clean and made suitable for municipal waste or clear bag waste. In addition to the environmental and economical benefits of this technique, evidence suggests that staff satisfaction is improved with increased involvement in “green” activities (6).
REFERENCES
- 1.Lauer M.. Reducing healthcare’s ecological footprint. Am J Nurs. 2009;109:2. [DOI] [PubMed] [Google Scholar]
- 2.Human blood and blood product. Available at: www.health.ny.gov/facilities/waste/#human_blood. Accessed March 1, 2013.
- 3.Sattler B, Condon M.. Nurses-defenders of environmental health. The problems posed by medical waste incineration. N M Nurse. 2005;50:10. [Google Scholar]
- 4.Landrigan PJ, Sonawane B, Mattison D, et al. Chemical contaminants in breast milk and their impacts on children’s health: An overview. Environ Health Perspect. 2002;110:A313–A315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gautam V, Thapar R, Sharma M.. Biomedical waste management: Incineration versus environmental safety. Indian J Med Microbiol. 2010;28:191–192. [DOI] [PubMed] [Google Scholar]
- 6.Walsh C, Sulkowski AJ.. A greener company makes for happier employees more so than a valuable one. Interdisciplinary Environ mental Review. 2010;11:4. [Google Scholar]