Abstract
Objective
We aimed to measure separately the contributions of heat and humidity to changes in levels of hemoglobins A and S in dried-blood-spot (DBS) samples.
Design and methods
We stored paired sets of DBSs at 37 °C for predetermined intervals in low-humidity and high-humidity environments. Hemoglobin A and S levels of all samples in each complete set were measured in a single high performance liquid chromatography run.
Results
During the one-month storage intervals, both hemoglobin species lost about 35% of initial levels in low-humidity storage and almost all of initial levels in high-humidity storage.
Conclusions
Minimizing both humidity and temperature in the transportation and storage environments of DBS samples is essential to maintaining the integrity of the hemoglobin tetramer molecules.
Keywords: Newborn screening, Sickle cell disease, Hemoglobin S, Hemoglobin A, Dried blood spots, Hemoglobin stability, Storage temperature, Storage humidity
1. Introduction
Sickle cell diseases are inborn blood disorders caused by the presence of an abnormal form of hemoglobin, hemoglobin S (HbS). Molecules of both HbS and normal adult hemoglobin (HbA) consist of two α polypeptide chains and two β polypeptide chains. The α chains of the two hemoglobins are identical, but the glutamic acid that is the 6th amino acid residue from the N-terminus of the HbA β chain is replaced by a valine residue in HbS. This small difference in the molecular composition of HbS causes clinically significant sickle cell diseases in persons who: 1) are homozygous for HbS, 2) are heterozygous for HbS and one of several other abnormal hemoglobins; or 3) are carriers of both the HbS mutation and mutations that cause thalassemias (decreased globin chain production which leads to decreased HbA production). Sickle cell diseases cause anemia, acute pain episodes, and in some cases, death during the early years of life. Data from a number of state wide newborn screening programs show that mortality from sickle cell disease during the first 3 to 4 years of life is virtually eliminated by universal screening and appropriate follow-up and treatment [1]. Three sickle cell diseases (sickle cell anemia, sickle hemoglobin C disease, and sickle β thalassemia) are included in the United States' recommended uniform screening panel [2]. Newborn screening for these disorders is universal in the United States where newborn screening samples are collected on filter paper, dried, and transported at ambient temperatures and humidities to state, regional, or state-associated contract laboratories for analysis. Little information about the stabilities of HbS (the marker of sickle cell diseases) or HbA in dried-blood spot (DBS) samples during transport and storage is available. Understanding and controlling for environmental variables are critical in sustaining effective operations of newborn screening and associated quality assurance programs that store and transport DBS samples in a wide range of environments.
In 2011, we performed accelerated degradation studies of 34 disorder markers as part of routine evaluations of DBS materials prepared by the Newborn Screening Quality Assurance Program of the Centers for Disease Control and Prevention (CDC) to assist laboratories with monitoring the performance of their newborn screening tests [3].We examined the stabilities of those markers in a single normalized study design that included temperature and humidity variables [4].We were unable to include HbS (the marker for the three recommended sickle cell diseases) or HbA in our 2011 studies because of methodological limitations. A recently acquired high performance liquid chromatography (HPLC) system has enabled us to measure levels of hemoglobin species and examine their stabilities in DBSs stored under various environmental conditions. We initiated accelerated degradation studies to compare the stabilities of HbS and HbA in DBSs stored at an elevated temperature (37 °C) and at low (below 30%) or high (above 50%) relative humidity for predetermined intervals. The objectives of the studies were to measure separately the contributions of heat and humidity to the degradation of HbS and HbA in DBS samples.
2. Materials and methods
2.1. Preparation of DBS materials
The DBS materials for these studies were made from blood collected in EDTA from a single anonymous adult HbS carrier (HbS carriers have one gene carrying the HbS mutation and one gene without the mutation.). The whole blood was adjusted to 50 ± 1% hematocrit by plasma removal to simulate the hematocrit of newborns and dispensed in 75 μL aliquots onto horizontally suspended sheets of Ahlstrom 226 (www.perkinelmer.com) filter paper. The blood spots were dried overnight under ambient conditions before 6 representative sheets, taken from throughout the production batch, were removed for the characterization of initial HbS and HbA levels and the evaluation of the production batch homogeneity. All other sheets of DBSs were separated by sheets of weighing paper (www.fishersci.com) and placed in Bitran Series S liquid-tight zip-closure specimen bags (com-pac.com)with desiccant packets (polylam.com) and 30–50% humidity indicator cards (www.desiccare.com) to ensure that storage humidity was maintained below 30%. The sealed bags of DBS materials were stored at −70 °C until use (results from stability studies of lysosomal enzymes have shown that proteins in dried-blood spots stored at −70 °C are stable for more than a year [5]).
2.2. Characterization of initial marker levels and validation of homogeneity of the DBS production lot
We performed duplicate analyses of the first, 21st, 41st, 61st, 81st, and last sheets of the prepared DBS materials on each of five days. We used the acquired data to measure initial marker levels in the DBSs and to estimate the variability of the analyses. We used previously described statistical procedures [6] to evaluate the homogeneity of the production batch. In brief, we calculated a best-fit line from the average marker level of each card plotted against the card number. We calculated the batch deviation by multiplying the best-fit line slope by the number of cards in the production batch, and we calculated the residual deviation of the batch by taking the square root of the average of the variation of each of the 6 cards tested. We considered the marker level to be homogenous throughout the batch if the absolute value of the batch deviation was smaller than the residual deviation.
2.3. Accelerated degradation study design
We performed accelerated degradation studies of hemoglobins A and S according to the normalized study design we used to examine stabilities of 34 other disorder markers [4]. In accordance with that design, we stored eleven-member paired sets of the DBS materials at 37 °C in Bitran Series S zip-closure specimen bags containing humidity indicator cards that indicated by color change humidities below 30% (blue) and above 50% (pink). One set of the pair was stored with relative humidity controlled below 30% by enclosing desiccant packets with the DBSs and zip-sealing the bags before storage. The other set was stored without desiccant in open Bitran bags in a high-humidity chamber which was monitored by periodic hygrometer readings to maintain humidity above 90%. The Day 0 member of each sample set (in a zip-closure bag with humidity maintained below 30%) remained in −70 °C storage throughout the study to serve as the storage stability control for its sample set. At predetermined intervals throughout the 31-to-32 day accelerated degradation studies, we removed DBSs from each sample set from 37 °C storage and transferred them to optimal storage at −70 °C. Immediately before transfer, we added desiccant packets to the bags containing DBSs that had been stored at high humidity and zip-sealed those bags to ensure that they were stored at optimal humidity. We measured the marker levels of all samples in each complete sample set in triplicate in a single analytic run.
2.4. HPLC analysis method
We used a Trinity Biotech Genesys Ultra2 Variant HPLC system (www.trinitybiotech.com) to quantitate, in each high-resolution chromatogram, the peak areas of HbS and HbA and the total area of all peaks. We also purchased the expendable supplies for the hemoglobin variant assay (reagents, hemoglobin reference material and controls, GeneSys™ variant ion exchange column, vials, filter frits, and microplate sealing film) from Trinity Biotech.
In this analytic system, the percentage of the total peak area attributable to each marker is used to express the marker concentrations. We used these percentages to express initial levels of HbS and HbA in the DBS materials and to monitor the degradation of the hemoglobin molecules during the accelerated degradation studies.
2.5. Analysis of accelerated degradation studies data
We used geometric means of triplicate measurements of initial (Day 0) marker levels and marker levels remaining on the last day of each degradation study to determine the percentage of each marker's initial level that was lost during the study. We attributed marker losses from samples stored at low humidity to the effects of the elevated storage temperature. We subtracted the percentage loss of each marker from the sample set stored at low humidity from the percentage loss sustained by the paired sample set stored at high humidity and attributed the difference to the effects of elevated storage humidity.
3. Results
3.1. DSB characterization results
Average initial hemoglobin levels, obtained from HPLC analysis and expressed as the ratio of hemoglobin-marker peak area to total peak area × 100%, were: HbA―51.3% ± 0.9% and HbS―31.6% ± 1.9% (Table 1). The DBS characterization data, analyzed by our routinely used homogeneity evaluation protocol [6], showed that the DBS production lot met the criterion for acceptable homogeneity (Table 1).
Table 1.
Characterization of hemoglobin A (Hb A) and hemoglobin S(Hb S) levels in dried-blood-spot materials used for accelerated degradation studies.
| Method | High performance liquid chromatography | |
|---|---|---|
| Hemoglobin | Hb A | Hb S |
| Averagea | 51.27% | 31.58% |
| Standard deviation | 0.87 | 1.90 |
| Coefficient of variation | 1.69% | 6.00% |
| Slopeb | −0.004 | −0.003 |
| Batch deviationc | −0.357 | −0.299 |
| Residual deviationd | 0.868 | 1.975 |
| Homogenouse | Yes | Yes |
Expressed as the percentage of total peak area attributable to each marker.
Best fit line slope from the average marker level of each card versus card number.
Batch deviation = slope × number of cards in the batch.
Residual deviation = square root of the average of the variation of each card.
Homogenous if absolute value of batch deviation is smaller than residual deviation.
3.2. Accelerated degradation results
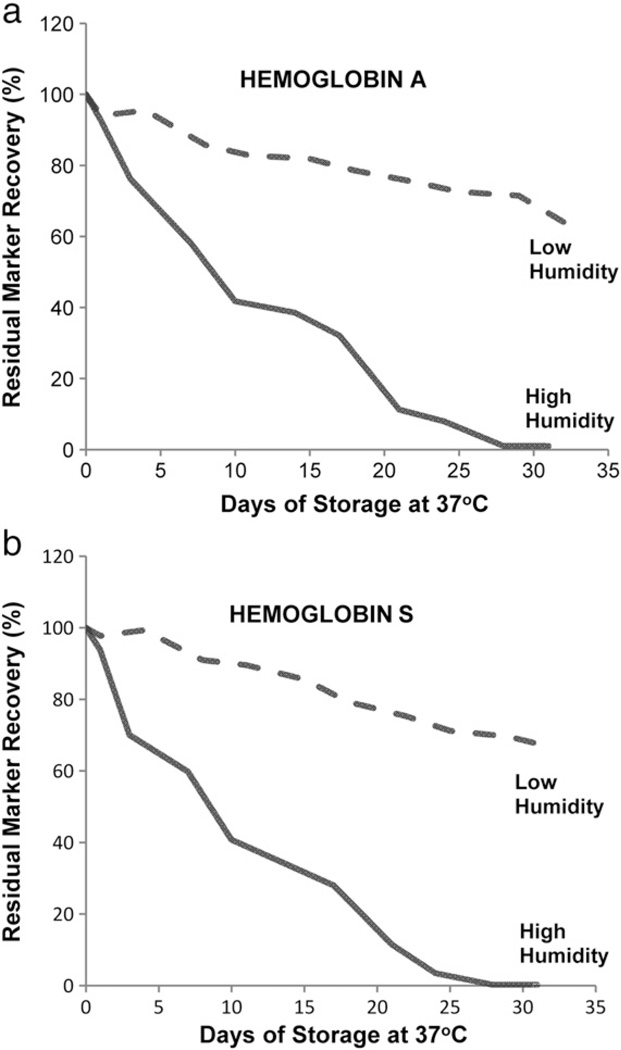
The degradations of HbA and HbS molecules after each storage interval are shown as the remaining percentages of initial (Day 0) hemoglobin levels (Fig. 1). Results from the comparison of intact hemoglobin tetramer levels on the initial and final days of the 37 °C accelerated degradation study indicate that HbA and HbS levels in DBSs stored at low humidity experienced about 35% loss during a 32-day storage period. In DBSs stored at high humidity, both HbA and HbS lost more than 99% of their initial levels during a 31-day storage period. We subtracted the degradation that occurred during low humidity storage (and was attributed to effects of the elevated storage temperature) from the almost 100% degradation that occurred during high humidity storage to find that about 65% of the degradation was attributable to the effects of high storage humidity (Table 2).
Fig. 1.
Recoveries of hemoglobins A and S from dried-blood spots stored for pre-determined intervals at 37 °C in low-humidity and high-humidity environments.
Table 2.
Percentagesa of hemoglobins A and S lost from dried-blood spots stored at 37 °C in low-humidity and high-humidity environmentsb.
| Hemoglobin | Study length |
Loss during storage at high humidity |
Loss during storage at low humidity |
Approximate loss attributable to effects of high humidity |
|---|---|---|---|---|
| (days) | (%)c | (%) | (%)d | |
| A | 31 + 1 | >99 | 36 | 64 |
| S | 31 + 1 | >99 | 33 | 67 |
Percentages shown were derived from geometric means of triplicate determinations.
Low relative humidity < 30%; high relative humidity > 50%.
Approximate loss. Amount remaining was less than 1% of total peak area of the HPLC chromatogram.
Derived by subtracting loss during storage at low humidity from loss during storage at high humidity.
4. Discussion
The standardized protocol used to characterize the initial marker levels and the homogeneity of marker distribution in the DBS material production batch is used routinely by the Newborn Screening Quality Assurance Program to validate its proficiency testing specimens. The initial levels of HbA (51.3%) and HbS (31.6%) in the DBS materials prepared for our stability studies are typical of circulating levels of the two hemoglobin species in HbS carriers [7, 8].
The accelerated degradation studies were carried out at 37 °C at low and high relative humidities for 31 to 32 days for study convenience (elevated storage temperature [9, 10] or elevated humidity [11, 12] accelerates the degradation process, thus enabling the measurement of changes in marker levels in a short study period.) Additionally, the study conditions mimic those encountered during some transportation environments, such as summer transit in hot courier trucks, in which DBSs may be exposed to elevated temperatures before arrival at testing laboratories.
The goal of these studies was to measure the separate contributions of elevated temperature and elevated humidity exposure to changes in levels of HbS, the marker for sickle cell diseases, and in levels of the normal adult hemoglobin, HbA.
HPLC results from our accelerated degradation studies showed that degradation curves of HbS and Hb A were similar and that both hemoglobins were highly susceptible to the adverse effects of high humidity in the DBS storage environment. Comparison of hemoglobin levels on the initial and final days of the 37 °C accelerated degradation studies indicates that most of their degradation was attributable to the adverse effects of high humidity. Both HbA and HbS lost more than 99% of their initial levels before the end of the month-long high-humidity degradation study (Table 2), and both hemoglobins lost more than half of their initial levels within the first 10 days of high-humidity storage (Fig. 1).
Understanding susceptibilities of markers in DBS samples to heat-related and moisture-related degradation is important for maintaining sample integrity for high-quality measurements. We have shown that minimizing both humidity and temperature of the DBS transport and storage environment is essential for ensuring the integrity of hemoglobin molecules especially when transportation time exceeds a few days. The DBS samples from CDC's Newborn Screening Quality Assurance Program are transported worldwide in closed containers with desiccant to assure that high-quality DBSs arrive for the assessment of laboratory performance.
Acknowledgment
Co-author D. L. Chafin was funded by the Research Participation Program at the Centers for Disease Control and Prevention, an interagency agreement with the U.S. Department of Energy administered by the Oak Ridge Institute for Science and Education. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Abbreviations
- HbS
hemoglobin S
- HbA
hemoglobin A
- DBS
dried-blood spot
- CDC
Centers for Disease Control and Prevention
- HPLC
high performance liquid chromatography
References
- 1.Kaye CI. Newborn screening fact sheets. Pediatrics. 2006;118:e934–e963. doi: 10.1542/peds.2006-1783. [DOI] [PubMed] [Google Scholar]
- 2.Watson MS, Mann MY, Lloyd-Puryear MA, Rinaldo P, Howell RR. Newborn screening: toward a uniform screening panel and system—executive summary. Pediatrics. 2006;117S:S296–S307. doi: 10.1542/peds.2005-2633I. [DOI] [PubMed] [Google Scholar]
- 3.Bell CJ. In: Newborn Screening Quality Assurance Program 2011 annual summary report. Bell CJ, editor. Atlanta. GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 4.Adam BW, Hall EM, Sternberg M, Lim TH, Flores SR, O'Brien S, et al. The stability of markers in dried-blood spots for recommended newborn screening disorders in the United States. Clin Biochem. 2011;44:1445–1450. doi: 10.1016/j.clinbiochem.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adam BW, Orsini JJ, Jr, Martin M, Hall EM, Zobel SD, Caggana M, et al. The preparation and storage of dried-blood spot quality control materials for lysosomal storage disease screening tests. Clin Biochem. 2011;44:704–710. doi: 10.1016/j.clinbiochem.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Schiffer JM, Mei JV, Hannon WH. Association of public health laboratories: newborn screening and genetic testing symposium. Portland, OR: Association of Public Health Laboratories; 2005. A standardized testing procedure for determination of lot homogeneity; p. 59. [Google Scholar]
- 7.Cooper MR, Toole JF. Sickle-cell trait: benign or malignant? Ann Intern Med. 1972;77:997–998. doi: 10.7326/0003-4819-77-6-997. [DOI] [PubMed] [Google Scholar]
- 8.Barbedo MM, McCurdy PR. Red cell life span in sickle cell trait. Acta Haematol. 1974;51:339–343. doi: 10.1159/000208316. [DOI] [PubMed] [Google Scholar]
- 9.Chace DH, Adam BW, Smith SJ, Alexander JR, Hillman SL, Hannon WH. Validation of accuracy-based amino acid reference materials in dried-blood spots by tandem mass spectrometry for newborn screening assays. Clin Chem. 1999;45:1269–1277. [PubMed] [Google Scholar]
- 10.Li L, Zhou Y, Bell CJ, Earley MC, Hannon WH, Mei JV. Development and characterization of dried blood spot materials for the measurement of immunoreactive trypsinogen. J Med Screen. 2006;13:79–84. doi: 10.1258/096914106777589623. [DOI] [PubMed] [Google Scholar]
- 11.Frazier DM, Clemons EH, Kirkman HN. Minimizing false positive diagnoses in newborn screening for galactosemia. Biochem Med Metabol Biol. 1992;48:199–211. doi: 10.1016/0885-4505(92)90066-8. [DOI] [PubMed] [Google Scholar]
- 12.Freer DE. Observations on heat/humidity denaturation of enzymes in filter-paper blood spots from newborns. Clin Chem. 2005;51:1060–1062. [Google Scholar]