Abstract
Background
Bile duct reconstruction (BDR) is used to manage benign and malignant neoplasms, congenital anomalies, bile duct injuries and other non-malignant diseases. BDR outcomes overall, by year, and by indication were compared.
Methods
Retrospective analysis of Nationwide Inpatient Sample discharges (2004–2011) including ICD-9 codes for BDR. All statistical testing was performed using survey weighting. Univariate analysis of admission characteristics by chi square testing. Multivariate modelling for inpatient complications and inpatient death by logistic regression.
Results
Identified 67 160 weighted patient admissions: 2.5% congenital anomaly, 37.4% malignant neoplasm, 2.3% benign neoplasm, 9.9% biliary injury, 47.9% other non-malignant disease. Most BDRs were performed in teaching hospitals (69.6%) but only 25% at centres with a BDR volume more than 35/year. 32.3% involved ≥ 1 complication, and 84.7% were discharges home. There was a 4.2% inpatient death rate. The complication rate increased but the inpatient death rate decreased over time. The rates of acute renal failure increased. Significant multivariate predictors of inpatient death include indication of biliary injury or malignancy, and predictors of any complication include public insurance and non-elective admission.
Conclusion
This is the first national description of BDRs using a large database. In this diverse sampling, both procedure indication and patient characteristics influence morbidity and mortality.
Introduction
The term bile duct reconstruction (BDR) encompasses a variety of surgical procedures with one overarching purpose: to restore the natural flow of bile from the liver to the intestines. The indications for BDR are numerous, ranging from biliary trauma to malignancy to non-malignant diseases to congenital problems. However, the national rate of BDRs in the United States is unknown.
The literature on outcomes for BDR is sparse and mostly limited to small, single-centre studies that evaluate particular types of reconstructions in specific populations.1–4 A great deal of the literature using nationwide data has focused on biliary tract malignancies5,6 and the prevention7 or changing management of bile duct injuries.8,9
As the first investigation at the national scale of admissions for BDRs of all types, we aim to characterize the population receiving these procedures, identify trends in BDR and distinguish factors associated with worse inpatient outcomes.
Patients and methods
Patient population
A retrospective, population-based analysis was performed using discharge records from the Nationwide Inpatient Sample (NIS) for the years 2004–2011. As the largest national hospital inpatient administrative database in the US, the NIS provides a 20% sample of short-term, non-federal hospitals, amounting to 40 million weighted admissions annually.10
Inclusion criteria were patient age ≥ 18 years and an ICD-9 procedure code suggestive of BDR: 51.36, 51.37, 51.39 (choledochoenterostomy), 51.69, 51.63 (excision of bile duct), 51.72, 51.79 (choledochoplasty), 51.93 (closure of biliary fistula) and 51.94 (revision of biliary anastomosis). Exclusion criteria included any diagnosis code of liver transplant or associated transplant complications. Admissions with missing data for age, gender, inpatient death, length of stay (LOS), elective status and hospital information were also excluded.
Patient and hospital characteristics
Patient characteristics of interest were gender, age, race, quartile for median household income based on the patient's ZIP code, insurance status, concomitant diagnoses and the Elixhauser comorbidity score, calculated using the Healthcare Cost and Utilization Project Comorbidity Software, Version 3.7.11 Hospital characteristics included teaching status and annual BDR volume. High BDR volume hospitals were those in the top tertile of facilities included, defined as those performing > 25 BDRs per year.
Admission characteristics
Admissions were divided into five hierarchical groups based on the indication for BDR: congenital anomaly (including choledochal cyst), malignant neoplasm, benign neoplasm, bile duct injury or trauma and other non-malignant disease. A malignant neoplasm refers to any primary or secondary malignant neoplasm or neoplasm of uncertain behaviour, including carcinoma in situ and malignancies of the liver, biliary system, stomach, pancreas, small intestine, large intestine, spleen, retroperitoneum and abdominal lymph nodes. The ‘other non-malignant disease category’ included strictures, non-malignant obstructions and non-congenital cysts, as well as any remaining non-malignant biliary processes. Dual diagnoses were not permitted, and admission indications were categorized based on the aforementioned hierarchy. Please refer to Appendix A1 for a list of ICD-9 codes by procedure and diagnosis.
Admissions were further characterized by year range (2004–2006, 2007–2009 and 2010–2011) as well as urgency of admission. Imaging type, including intra-operative cholangiogram (IOC) or biliary X-ray, endoscopic retrograde cholangiogram (ERC) or endoscopic retrograde cholangiopancreatography (ERCP), diagnostic ultrasound, CT scan, MRI or magnetic resonance cholangiopancreatography (MRCP), performed during a BDR-related admission was identified by ICD-9 code.
Outcomes
Outcomes of interest included inpatient complications (listed in Appendix A1) and mortality, LOS, disposition status and cost, which was determined using supplemental NIS HCUP Cost-to-Charge Ratio files.12
Statistical analysis
All statistical analysis was performed using the weighted survey methods in SAS (version 9.3/9.4; SAS Institute, Cary, NC, USA), and all amounts reported are weighted values. P-values of < 0.05 were considered significant. Continuous variables were divided into categories based on clinical significance. Univariate analysis was performed using chi-square tests. The Cochran–Armitage trend test was used to assess for trends over time across year groups.
A subset analysis comparing outcomes in BDRs performed with hepatectomies (ICD-9 procedure codes 50.22 or 50.3) and without hepatectomies for malignant neoplasm was performed.
Logistic regression models were created for inpatient death and any complication. Covariates were included in the models based on an univariate screen, with confounding prioritized over collinearity in the process of model building. Considered for insertion into the models were: indication, BDR procedure, gender, race, income quartile, insurance type, age category, Elixhauser score, elective status, hospital teaching status, hospital volume cluster and year category. Additionally, post-operative infection, cholangitis, acute pancreatitis, acute renal failure, acute liver failure, operative bleeding, deep vein thrombosis (DVT)/pulmonary embolism (PE), acute myocardial infarction (MI) and gastrointestinal (GI) bleed were considered for insertion into the inpatient death model. Indication was collapsed into three categories (malignant, non-malignant and biliary injury/trauma) for the inpatient death model in order to avoid small cell sizes and model instability.
Results
Patient and hospital characteristics
Sixty-seven thousand one hundred and sixty weighted admissions in which a BDR was performed were identified over an 8-year period. One thousand six hundred and seventy-five BDRs (2.5%) were performed for congenital anomalies, 25 150 (37.4%) for malignancy, 1528 (2.3%) for benign neoplasms, 6653 (9.9%) for biliary injury/trauma and 32 155 (47.9%) for other non-malignant disease. The majority involved women (37 119, 55.3%), white patients (39 190, 58.4%) and patients with government insurance (36 540, 54.4%). The distribution for age was left-skewed, with 45.3% of patients (30 403) age 65 years or older. A plurality of BDR-related admissions (25 075, 37.3%) involved patients with an Elixhauser score of 3 or greater. 69.6% (46 743) were admissions to a teaching hospital. Please see Table 1 for a comparison of characteristics by indication. The median yearly volume of BDRs per hospital was 10, with an interquartile range of 4–35.
Table 1.
Patient and hospital characteristics by indication for bile duct reconstruction
| Congenital anomaly 1675 |
Malignant neoplasm 25 150 |
Benign neoplasm 1528 |
Biliary injury or trauma 6653 |
Other non-malignant disease 32 155 |
Total 67 160 | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | % | ||
| Gender | ||||||||||||
| Male | 441 | 26.3 | 13 385 | 53.2 | 619 | 40.5 | 2382 | 35.8 | 13 214 | 41.1 | 44.7 | <0.0001 |
| Female | 1233 | 73.7 | 11 765 | 46.8 | 909 | 59.5 | 4271 | 64.2 | 18 941 | 58.9 | 55.3 | |
| Age | ||||||||||||
| < 40 years | 592 | 35.4 | 486 | 1.9 | 128 | 8.4 | 1718 | 25.8 | 4907 | 15.3 | 11.7 | <0.0001 |
| 40–64 years | 727 | 43.4 | 10 717 | 42.6 | 714 | 46.7 | 2680 | 40.3 | 14 088 | 43.8 | 43.1 | |
| ≥ 65 years | 355 | 21.2 | 13 946 | 55.5 | 686 | 44.9 | 2255 | 33.9 | 13 161 | 40.9 | 45.3 | |
| Race | ||||||||||||
| White | 930 | 55.5 | 15 674 | 62.3 | 870 | 56.9 | 3627 | 54.5 | 18 088 | 56.3 | 58.4 | <0.0001 |
| Black | 102 | 6.1 | 1705 | 6.8 | 165 | 10.8 | 515 | 7.7 | 2235 | 6.9 | 7.0 | |
| Other/Unknown | 642 | 38.4 | 7770 | 30.9 | 493 | 32.3 | 2510 | 37.7 | 11 832 | 36.8 | 34.6 | |
| Income Quartile by ZIP Code | ||||||||||||
| Less than 25th percentile | 371 | 22.1 | 6149 | 24.4 | 358 | 23.4 | 1891 | 28.4 | 8490 | 26.4 | 25.7 | 0.0002 |
| 26–50th percentile | 452 | 27.0 | 6263 | 24.9 | 331 | 21.7 | 1736 | 26.1 | 8682 | 27.0 | 26.0 | |
| 51–75th percentile | 433 | 25.9 | 5958 | 23.7 | 421 | 27.6 | 1644 | 24.7 | 7383 | 23.0 | 23.6 | |
| 76–100th percentile | 379 | 22.6 | 6126 | 24.4 | 398 | 26.0 | 1250 | 18.8 | 6786 | 21.1 | 22.2 | |
| Insurance | ||||||||||||
| Government | 587 | 35.0 | 14 752 | 58.7 | 821 | 53.7 | 3207 | 48.2 | 17 174 | 53.4 | 54.4 | <0.0001 |
| Private | 836 | 49.9 | 9060 | 36.0 | 648 | 42.4 | 2786 | 41.9 | 11 869 | 36.9 | 37.5 | |
| Other/unknown | 252 | 15.2 | 1337 | 5.3 | 59 | 3.9 | 660 | 9.9 | 3112 | 9.7 | 8.1 | |
| Elixhauser score | ||||||||||||
| 0 | 542 | 32.4 | 1672 | 6.6 | 357 | 23.4 | 1873 | 28.2 | 6639 | 20.6 | 16.5 | <0.0001 |
| 1 | 484 | 28.9 | 5143 | 20.4 | 413 | 27.1 | 1628 | 24.5 | 7788 | 24.2 | 23.0 | |
| 2 | 339 | 20.2 | 6366 | 25.3 | 344 | 22.5 | 1364 | 20.5 | 7132 | 22.2 | 23.1 | |
| ≥3 | 310 | 18.5 | 11 969 | 47.6 | 413 | 27.0 | 1788 | 26.9 | 10 596 | 33.0 | 37.3 | |
| Elective Status | ||||||||||||
| Elective | 1019 | 60.8 | 17 069 | 67.9 | 1200 | 78.6 | 2519 | 37.9 | 14 813 | 46.1 | 54.5 | <0.0001 |
| Non-elective | 655 | 39.1 | 8081 | 32.1 | 328 | 21.4 | 4135 | 62.1 | 17 342 | 53.9 | 45.5 | |
| Hospital type | ||||||||||||
| Teaching | 1107 | 66.1 | 20 037 | 79.7 | 1249 | 81.7 | 4334 | 65.1 | 20 016 | 62.2 | 69.6 | <0.0001 |
| Non-teaching | 567 | 33.9 | 5113 | 20.3 | 279 | 18.3 | 2319 | 34.9 | 12 139 | 37.8 | 30.4 | |
| Hospital BDR volume | ||||||||||||
| Low volume (≤5) | 708 | 42.3 | 5764 | 22.9 | 410 | 26.9 | 2940 | 44.2 | 13 866 | 43.1 | 35.3 | <0.0001 |
| Medium volume (6–25) | 479 | 28.6 | 9048 | 36.0 | 442 | 28.9 | 1963 | 29.5 | 10 373 | 32.3 | 33.2 | |
| High volume (>25) | 488 | 29.1 | 10 337 | 41.1 | 675 | 44.2 | 1751 | 26.3 | 7916 | 24.6 | 31.5 | |
| Year | ||||||||||||
| 2004–2006 | 544 | 32.5 | 9065 | 36.0 | 510 | 33.4 | 2439 | 36.7 | 12 814 | 39.9 | 37.8 | 0.0155 |
| 2007–2009 | 679 | 40.6 | 9530 | 37.9 | 583 | 38.1 | 2404 | 36.1 | 11 726 | 36.5 | 37.1 | |
| 2010–2011 | 451 | 26.9 | 6554 | 26.1 | 435 | 28.5 | 1809 | 27.2 | 7615 | 23.7 | 25.1 | |
In the cohort of BDRs conducted for malignancy, pancreatic malignancy was the most common indication for BDR (13 590, 53.9%), followed by liver maligancy at 25.3% (6391), extra-hepatic biliary malignancy at 14.1% (3558), intra-hepatic biliary malignancy at 7.4% (1875), gallbladder malignancy at 6.1% (1545) and malignancy in a non-specific liver, gallbladder or biliary location at 3.1% (789).
As seen in Table 2, 9.0% of BDR-related admissions (6015) involved a concomitant diagnosis of cholangitis, 6.9% (4634) acute pancreatitis and 2.1% (1404) a bile duct fistula. The highest rate of all concomitant diagnoses was seen in the other non-malignant disease group with 12.4% of admissions (3988) with cholangitis, 9.2% (2952) with acute pancreatitis and 3.7% (1203) with a bile duct fistula. Within the other non-malignant disease group, 61.6% of admissions (19 811) had a diagnosis of cholelithiasis, cholecystitis or cholangitis and 2.2% had biliary stent failure (705).
Table 2.
Time trends in admission characteristics and outcomes for bile duct reconstruction
| 2004–2006 |
2007–2009 |
2010–2011 |
All BDR Admissions |
P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| 25 373 |
24 922 |
16 865 |
67 160 |
||||||
| n | % | n | % | n | % | n | % | ||
| Any imaging | 9099 | 35.9 | 8103 | 32.5 | 4920 | 29.2 | 22 122 | 32.9 | <0.0001 |
| IOC or Biliary X-ray | 6744 | 26.6 | 5825 | 23.4 | 3480 | 20.6 | 16 048 | 23.9 | <0.0001 |
| ERC or ERCP | 2772 | 10.9 | 1889 | 7.6 | 1048 | 6.2 | 5709 | 8.5 | <0.0001 |
| Diagnostic ultrasound | 448 | 1.8 | 836 | 3.4 | 778 | 4.6 | 2063 | 3.1 | <0.0001 |
| CT scan | 414 | 1.6 | 535 | 2.1 | 299 | 1.8 | 1247 | 1.9 | 0.1173 |
| MRI/MRCP | 135 | 0.5 | 177 | 0.7 | 82 | 0.5 | 394 | 0.6 | 0.8340 |
| Any complication | 7427 | 29.3 | 8473 | 34.0 | 5800 | 34.4 | 21 700 | 32.3 | <0.0001 |
| Post-operative infection | 2919 | 11.5 | 3585 | 14.4 | 2482 | 14.7 | 8986 | 13.4 | <0.0001 |
| Acute renal failure | 1447 | 5.7 | 2375 | 9.5 | 2043 | 12.1 | 5865 | 8.7 | <0.0001 |
| Operative bleeding | 934 | 3.7 | 1372 | 5.5 | 824 | 4.9 | 3131 | 4.7 | <0.0001 |
| GI bleed | 436 | 1.7 | 648 | 2.6 | 318 | 1.9 | 1402 | 2.1 | 0.0381 |
| Acute liver failure | 202 | 0.8 | 445 | 1.8 | 335 | 2.0 | 982 | 1.5 | <0.0001 |
| DVT/PE | 265 | 1.0 | 352 | 1.4 | 272 | 1.6 | 890 | 1.3 | <0.0001 |
| Acute MI | 243 | 1.0 | 294 | 1.2 | 105 | 0.6 | 642 | 1.0 | 0.0042 |
| Concomitant diagnoses | |||||||||
| Cholangitis | 2329 | 9.2 | 2258 | 9.1 | 1429 | 8.5 | 6015 | 9.0 | 0.0170 |
| Acute pancreatitis | 1623 | 6.4 | 1900 | 7.6 | 1111 | 6.6 | 4634 | 6.9 | 0.1470 |
| Bile duct fistula | 556 | 2.2 | 505 | 2.0 | 343 | 2.0 | 1404 | 2.1 | 0.2321 |
| Concomitant procedure | |||||||||
| Hepatectomy | 1348 | 5.3 | 1850 | 7.4 | 1682 | 10.0 | 4880 | 7.3 | <0.0001 |
| Elective | 13 174 | 51.9 | 13 371 | 53.7 | 10 074 | 59.7 | 36 620 | 54.5 | <0.0001 |
| Inpatient death | 1102 | 4.3 | 1051 | 4.2 | 648 | 3.8 | 2802 | 4.2 | 0.0148 |
| Length of stay > 14 days | 6858 | 27.0 | 6588 | 26.4 | 4521 | 26.8 | 17 966 | 26.8 | 0.4922 |
| Cost > $40,000 | 4481 | 18.9 | 5925 | 25.3 | 4460 | 28.8 | 14 865 | 23.7 | <0.0001 |
BDR, bile duct reconstruction; DVT/PE, deep vein thrombosis/pulmonary embolism; ERC, endoscopic retrograde cholangiogram; ERCP, endoscopic retrograde cholangiopancreatography; GI, gastrointestinal; IOC, intra-operative cholangiogram; MI, myocardial infarction; MRCP, magnetic resonance cholangiopancreatography; MRI, magnetic resonance imaging.
The rate of concomitant hepatectomy also varied by indication, with hepatectomies performed with 15.6% (3919) of BDRs for a malignant neoplasm, 7.8% (119) for a benign neoplasm, 5.9% (99) for a congenital anomaly and less than 2% for other non-malignant disease and biliary injury or trauma (626 and 118, respectively).
Admission characteristics
Nearly one-third of BDR-related admissions (22 122, 32.9%) involved imaging. The most common type of imaging performed was an IOC, or biliary X-ray (16 048, 23.9% of admissions) and the least common was MRI or MRCP (394, 0.6%). As shown in Table 2, the rate of any imaging performed during the same admission as a BDR decreased over time (P < 0.0001); the only type of imaging to increase in use was diagnostic ultrasound (P < 0.0001).
The mean number of BDRs performed per year was 8395 with the greatest number performed in 2008 (9430, 14.0%). 54.5% of admissions for BDR (36 620) were elective. The greatest rates of BDRs performed electively were for malignant and benign neoplasms (17 069, 67.9 and 1200, 78.6%, respectively). The rate of elective admissions increased over time (P < 0.0001).
Outcomes
Nearly one-third (21 700, 32.3%) of admissions involved at least one complication. The most common coded complication was a post-operative infection, occurring in 13.4% (8986) of all admissions. DVT/PE and acute MI were the least common complications, only occurring in 1.3% (890) and 1.0% of admissions (642), respectively. Operative bleeding occurred in 4.7% (3 131) of BDR-related admissions. The rate of any documented complication increased over time (P < 0.0001), with a notable increase in rates of post-operative acute renal failure (P < 0.0001), as seen in Table 2.
Within the malignant neoplasm cohort, the mortality rate for BDR when no concomitant hepatectomy was performed was 5.1% (1085/21 279) versus 10.5% (412/3942) when performed with a hepatectomy (P < 0.0001). Similarly, the complication rate with no concomitant hepatectomy was 33.1% (7042/21 279) versus 41.3% (1628/3942) with a hepatectomy (P = 0.0002). As shown in Table 2, there has been an increase in concomitant hepatectomies over time (P < 0.0001).
The median LOS was 9 days (IQR 6, 15), with the majority of admissions (31 076, 46.3%) lasting between 1 and 2 weeks. The shortest LOSs were for BDRs performed for congenital anomalies, with 46.9% (786) of those admissions lasting less than a week. In contrast, the longest LOSs were for those admissions during which a BDR was performed for malignant disease, with almost one-third (8233, 32.7%) lasting longer than 2 weeks. The rate of admissions that lasted longer than 2 weeks did not change significantly over time (0.4922).
4.2% (2 802) of BDR-related admissions resulted in inpatient death. 5.9% (1 492) of admissions for BDR performed for malignancy resulted in inpatient death, in contrast to 4.1% (275) for biliary injury or trauma, and 3.0% (980) for other non-malignant disease. The rates of inpatient death for congenital anomalies and benign neoplasms were too low to report. The majority of inpatient deaths (1577, 56.3%) occurred in admissions that lasted over 2 weeks. The rate of inpatient death decreased over time (P = 0.0148).
For any admission resulting in discharge alive from the hospital, 84.7% (54 531) were discharges home (versus rehabilitation centre or skilled nursing facility). The lowest rates of discharge home were for biliary injury or trauma (5294, 83.0%), a malignant neoplasm (20 027, 84.7%) and other non-malignant disease (26 393, 84.7%).
Among the 62 633 admissions with complete cost data, median cost was $22 230 (IQR $14 399, $38 358.) Of these admissions, 23.7% (14 865) cost more than $40 000, with the rate of these costly admissions increasing over time (P < 0.0001). 38.8% of BDR admissions for the congenital anomaly (650) cost less than $15 000. Please refer to Table 3 for outcomes by indication.
Table 3.
Outcomes by indication for bile duct reconstruction
| Congenital anomaly |
Malignant neoplasm |
Benign neoplasm |
Biliary injury or trauma |
Other Non-malignant disease |
All BDR admissions |
P-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1675 |
25 150 |
1 528 |
6 653 |
32 155 |
67 160 |
|||||||||
| N | % | n | % | n | % | n | % | n | % | n | % | |||
| LOS | ||||||||||||||
| <7 days | 786 | 46.9 | 4418 | 17.6 | 338 | 22.1 | 2130 | 32.0 | 10 447 | 32.5 | 18 119 | 27.0 | <0.0001 | |
| 7–14 days | 626 | 37.4 | 12 499 | 49.7 | 770 | 50.4 | 3007 | 45.2 | 14 174 | 44.1 | 31 076 | 46.3 | ||
| >14 days | 263 | 15.7 | 8233 | 32.7 | 421 | 27.5 | 1516 | 22.8 | 7534 | 23.4 | 17 966 | 26.7 | ||
| Median LOS (IQR) | 7 (5, 10) | 10 (7, 17) | 10 (7, 16) | 8 (6, 14) | 8 (6, 14) | 9 (6, 15) | <0.0001 | |||||||
| Cost per admission | ||||||||||||||
| <$15 000 | 650 | 38.8 | 3758 | 14.9 | 245 | 16.0 | 1927 | 29.0 | 10 416 | 32.4 | 16 996 | 25.3 | <0.0001 | |
| $15 000–40 000 | 709 | 42.3 | 12 945 | 51.5 | 818 | 53.5 | 3012 | 45.3 | 13 289 | 41.3 | 30 772 | 45.8 | ||
| >$40 000 | 211 | 12.6 | 6714 | 26.7 | 349 | 22.8 | 1282 | 19.3 | 6310 | 19.6 | 14 865 | 22.1 | ||
| Median cost (IQR) | 16 546 (11 247, 26 924) | 26 825 (17 873, 43 524) | 25 529 (17 313, 39 646) | 20 844 (13 235, 34 744) | 19 280 (12 441, 34 468) | 22 230 (14 399, 38 358) | <0.0001 | |||||||
| Discharged Home | 1536 | 93.0 | 20 027 | 84.7 | 1 282 | 85.8 | 5 294 | 83.0 | 26 393 | 84.7 | 54 531 | 84.7 | 0.0012 | |
BDR, bile duct reconstruction; IQR, interquartile range; LOS, length of stay.
Multivariate analysis
Significant predictors for inpatient death, highlighted in Table 4, include biliary injury or trauma (versus non-malignant disease), malignant disease (versus non-malignant disease), revision of biliary anastomosis (versus choledochoenterostomy), public insurance (versus private insurance), age 40–64 years (versus younger than 40 years), age < 64 years (versus younger than 40 years), post-operative infection, acute renal failure, operative bleeding, GI bleed, DVT/PE, acute MI and acute liver failure.
Table 4.
Model of inpatient death for bile duct reconstruction
| Unadjusted OR | [95% CI] | Adjusted OR | [95% CI] | |||
|---|---|---|---|---|---|---|
| Indication | ||||||
| Non-malignant disease | Ref | |||||
| Biliary injury or trauma | 1.429 | 1.068 | 1.914 | 1.757 | 1.240 | 2.489 |
| Malignant disease | 2.091 | 1.719 | 2.543 | 2.147 | 1.703 | 2.706 |
| Type of Bile duct reconstruction | ||||||
| Choledochoenterostomy | Ref | |||||
| Choledochoplasty | 0.946 | 0.727 | 1.232 | 0.935 | 0.667 | 1.311 |
| Closure of biliary fistula | 0.945 | 0.663 | 1.347 | 1.022 | 0.666 | 1.570 |
| Excision of bile duct | 1.002 | 0.662 | 1.518 | 0.804 | 0.490 | 1.319 |
| Revision of biliary anastomosis | 3.302 | 2.183 | 4.996 | 3.053 | 1.890 | 4.934 |
| Gender | ||||||
| Male | 1.293 | 1.093 | 1.529 | 0.908 | 0.745 | 1.106 |
| Female | Ref | |||||
| Payer Type | ||||||
| Private Insurance | Ref | |||||
| Public Insurance | 3.061 | 2.474 | 3.786 | 1.641 | 1.224 | 2.200 |
| Other Insurance | 1.190 | 0.767 | 1.846 | 1.560 | 0.988 | 2.463 |
| Age category | ||||||
| Younger than 40 years | Ref | |||||
| Age 40–64 years | 3.558 | 1.741 | 7.272 | 2.827 | 1.381 | 5.786 |
| Age > 64 years | 10.463 | 5.295 | 20.673 | 6.324 | 3.024 | 13.224 |
| Elixhauser Score | ||||||
| 0 | Ref | |||||
| 1 | 1.616 | 1.063 | 2.457 | 0.883 | 0.576 | 1.356 |
| 2 | 2.079 | 1.402 | 3.085 | 0.837 | 0.556 | 1.258 |
| ≥3 | 3.644 | 2.512 | 5.287 | 0.931 | 0.623 | 1.390 |
| Elective status | ||||||
| Elective | Ref | |||||
| Non-elective | 1.498 | 1.259 | 1.781 | 1.125 | 0.908 | 1.394 |
| Complications | ||||||
| Post-operative infection | 3.770 | 3.068 | 4.633 | 2.001 | 1.584 | 2.528 |
| Acute renal failure | 13.595 | 11.400 | 16.211 | 7.858 | 6.289 | 9.819 |
| Operative bleeding | 4.185 | 3.275 | 5.347 | 2.481 | 1.883 | 3.270 |
| GI bleed | 6.286 | 4.526 | 8.731 | 3.154 | 2.123 | 4.684 |
| DVT/PE | 4.778 | 3.118 | 7.321 | 2.270 | 1.285 | 4.013 |
| Acute MI | 8.257 | 5.650 | 12.066 | 3.065 | 1.783 | 5.268 |
| Acute liver failure | 15.530 | 11.491 | 20.989 | 6.510 | 4.413 | 9.604 |
| Concomitant diagnoses | ||||||
| Cholangitis | 1.346 | 1.043 | 1.736 | 1.144 | 0.837 | 1.564 |
| Acute pancreatitis | 1.484 | 1.128 | 1.954 | 1.189 | 0.846 | 1.672 |
| Hospital teaching status | ||||||
| Teaching | Ref | |||||
| Non-teaching | 1.201 | 0.988 | 1.460 | 1.273 | 1.012 | 1.601 |
CI, confidence interval; DVT/PE, deep vein thrombosis/pulmonary embolism; GI, gastrointestinal; MI, myocardial infarction; OR, odds ratio.
Other covariates in the model: Elixhauser score, gender, elective status, cholangitis, acute pancreatitis. Bold values represent statistically significant odds ratio.
Included in the final model for any complication were: indication, BDR procedure, gender, insurance type, age category, Elixhauser score, elective status, year category and race. Significant predictors are depicted in Fig. 1.
Figure 1.
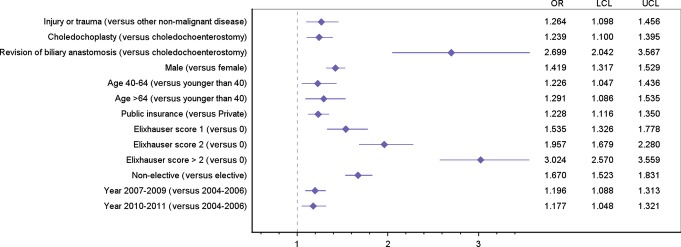
Adjusted significant predictors of any inpatient complication after bile duct reconstruction. Adjusted odds ratios with 95% confidence intervals. LCL, lower confidence limit; OR, odds ratio; UCL, upper confidence limit. Other covariates in model: race
Discussion
Even with the rising popularity of minimally invasive and endoscopic techniques,13,14 operative BDR remains a common procedure in the United States. Other non-malignant disease was the most common indication for a BDR, followed by malignant neoplasm, biliary injury, congenital anomaly and benign neoplasm. This study highlights that the burden of gallstone disease in this country extends beyond laparoscopic cholecystectomy and biliary stent placement and into more complex surgeries such as BDR. Although 32.3% of BDR-related admissions (21 700) involved at least one complication, only 4.2% of admissions (2802) resulted in inpatient death. In the malignant neoplasm group, the mortality rate more than doubled and the complication rate also rose when a concomitant hepatectomy was performed.
Our results are generally concordant with an assortment of previously published studies that have focused on specific indications or procedures in various settings,15–17 although different classification schemes make direct comparison difficult. Small international studies of BDRs for benign biliary lesions (defined broadly) document post-operative complication rates of 13–49% and peri-operative mortality rates of 0–5%.18–22 Peri-operative mortality in a study of a choledochoduodenostomy for benign versus malignant disease in Israel from 1988 showed a peri-operative mortality rate of about 3.1% versus 8.6%, respectively.20 The previously reported peri-operative mortality rate is 1.7–4.5% and the complication rate 42–43% for patients undergoing biliary reconstruction for biliary injury after a laparoscopic cholecystectomy.9,23
In addition to being the first comprehensive study of BDRs in this country, our study sheds light on several aspects of BDRs that have been overlooked in the literature.
Although the volumes–outcome relationship has been well-established for complex surgical procedures including liver transplantation,24,25 a large number of BDRs, namely for congenital anomalies, non-malignant disease and biliary trauma, are still being performed at low-volume centres. Overall, 50% of BDRs were performed in centres with a yearly BDR volume of < 10 and 25% in centres with a yearly volume of < 4. It is important to note that this volume data is only based on the 20% of hospitals sampled by the NIS.
We have found that several indications, types of procedures and patient characteristics influenced the odds of any inpatient complication and inpatient death. Particularly, public insurance (versus private insurance) was both a predictor of inpatient death and complications. Although insurance has been shown to affect outcomes for various conditions,26,27 this is the first evidence of the importance of insurance in the field of biliary surgery.
In addition to providing complication and death rates for BDR, we also provide information on discharge location, an important consideration for patients. For all patients discharged alive from the hospital, the rate of discharge home (as opposed to a rehabilitation facility), was quite high at 84.7% (54 531) for this adult population, over one-third of whom had an Elixhauser score of 3 or greater.
Furthermore, we provide information on trends in imaging, cost per admission, LOS, concomitant hepatectomy, complications and inpatient death rates over an 8-year period. The decreasing rate of imaging performed during admission for BDR is an interesting contrast to the increasing rate of costly admissions and the stable rate of lengthy hospital stays. A closer look at these costly admissions reveals that the patients are older and have more comorbidities, with over two-thirds experiencing complications, including an especially high rate of operative bleeding. It is possible that the increased cost is related to interventions for these complications. Additionally, more elective admissions could mean more imaging completed in the outpatient setting prior to admission for BDR. Accordingly, the decreasing rate of admissions for BDR with a concomitant diagnosis of cholangitis could also be as a result of the more widespread use of stents and endoscopic procedures. The rate of a hepatectomy performed during the same admission as a BDR is rising. The increase in the rate of any inpatient complication could be related to more operations performed on sicker individuals, more technically difficult BDRs attempted or simply improved accuracy in the coding of complications. The stark increase in the rate of renal failure is concerning and should be a focus of special attention moving forward, especially given the associated high adjusted odds of inpatient death. In spite of this, there has been a decrease in the rate of inpatient death. This could be as a result of the judicious use of pre-operative endoscopic intervention, early identification and management of complications, or the omission of death at home or in hospice in this analysis.
There are several limitations to this study. First, the use of this a large administrative database restricts the available variables of interest which vary in the level of specificity and are susceptible to miscoding. The specialty of the operating surgeon (general, HPB, surgical oncology, etc.) is not identifiable from this dataset so any related differences in outcomes cannot be assessed, although the hospital's overall level of expertise with BDRs can be extrapolated from the available volume data. We were able to provide data on some specific operative complications such as infection and bleeding and several systemic complications but are unable to quantify other immediate outcomes such as bile leak owing to the limitations of administrative coding. Data are also restricted to the admission level without the ability to follow a patient longitudinally. This study includes initial biliary reconstructions as well as re-operations and both open and laparoscopic surgeries without a way to distinguish the two. In addition, neither the specific method of biliary reconstruction (whether end-to-end, side-to-side, or duct-to-duct) nor the location of the ductal anastomosis (duodenum versus jejunum) was available from the available ICD-9 procedure codes. The order of events during a hospitalization is unknown, so it not possible, for example, to ascertain whether the ‘cholangitis’ coded as a discharge diagnosis was a reason for admission or a complication of a procedure performed in-house. If more than one BDR was performed on a given admission, we categorized it in one group based on a predetermined hierarchy of procedures that prioritized congenital anomalies and malignancies. Cost data were estimated based on charge and the hospital-payer mix.
Nevertheless, the considerable size of the database over several years provides substantial power in the statistical analysis. We were able to examine both events and indications that are relatively uncommon, such as congenital anomalies as an indication for BDR and inpatient death as an outcome.
The population of patients in the US receiving BDRs is primarily older, and a majority are female, white and government insured. Most reconstructions are performed electively, with that rate increasing over time. A majority are also performed at teaching hospitals, but only 25% at centres with an annual BDR volume of > 35. Almost one-third of admissions involved an inpatient complication (a rate that has increased over time), with biliary trauma, choledochoplasty, revision of biliary anastomosis, older age and public insurance among significant predictors of inpatient complication. Notably, the rate of acute renal failure after BDR has increased over the last 8 years. Less than one-third of BDR admissions involved the use of imaging. The rate of admissions lasting over 2 weeks has remained stable over time, but the rate of admissions costing over $40 000 has increased. The inpatient mortality rate has decreased over time, with biliary trauma, malignant disease, revision of biliary anastomosis, older age and public insurance among significant predictors of inpatient mortality.
BDRs are morbid procedures with considerable risk. We have shown, from a national perspective, that an indication for the procedure, the procedure itself and patient characteristics significantly influence important inpatient outcomes associated with BDR. We have provided a framework for potential risk stratification of patients and data that can improve the counselling of patients with regards to complications and mortality. Where feasible, we recommend transfer to a centre of excellence for complex BDR. Finally, we advocate for prevention strategies via less invasive methods to minimize the need for BDR if possible.
We have identified trends, some worrisome and some reassuring, in the surgical management of biliary disease. An understanding of this unique population and the factors influencing morbidity and mortality can lead to more informed decision making and improved outcomes moving forward.
Appendix A1 ICD-9 diagnosis and procedure codes for procedures, indications, imaging, concomitant diagnoses and complications of interest
| >ICD-9 Codes | |
|---|---|
| Procedures | |
| Choledochoenterostomy | |
| 51.36, 51.37, 51.39 | |
| Excision of bile duct | 51.69, 51.63 |
| Choledochoplasty | 51.72, 51.79 |
| Closure of biliary fistula | 51.93 |
| Revision of biliary anastomosis | 51.94 |
| Indications | |
| Congenital anomaly of gallbladder, bile ducts, liver or pancreas | 751.69, 751.60, 751.61, 751.62, 751.7, 751.8, 751.9 |
| Malignant neoplasma | Biliary intra-hepatic (155.1) Biliary extra-hepatic (156.1, 156.2) Gallbladder (156.0) Liver (155.0, 155.2, 197.7) Pancreas (157, 157.x) Unspecified biliary (156.8, 156.9, 230.8) Other (151, 151.x, 152, 152.x, 153, 153.x, 156.2, 158, 158.x, 159, 159.x, 197.4, 197.5, 197.6, 197.8, 230.2, 230.3, 230.7, 230.9, 209.0, 209.0x, 209.1, 209.1x, 209.2, 209.2x 196.2, 198.89, 197.8, 235) |
| Benign neoplasm | 209.4, 209.5, 209.6, 211.1, 211.2, 211.3, 211.5, 211.6, 211.7, 211.8, 211.9, 215.5 |
| Bile duct injury or trauma | 576.3, 868.02, 868.12, 998.2 |
| Other non-malignant diseaseb | 576.2, 576.8, 575.5, 577.2, 577.8, 560.31+ any remaining diagnoses |
| Imaging | |
| Cholangiogram or biliary X-ray | 87.53, 87.54, 87.59, 87.66 |
| Ultrasound | 88.74, 88.76 |
| CT scan of abdomen | 88.01 |
| MRI/MRCP | 88.97 |
| ERC/ERCP | 51.10, 51.11, 51.19 |
| Concomitant diagnoses | |
| Cholelithiasis/Cholecystitis | 574, 574.x, 574.xx, 575.0, 575.1x, 575.2 |
| Cholangitis | 576.1 |
| Acute pancreatitis | 577.0 |
| Bile duct fistula | 576.4 |
| Complications | |
| Post-operative infection | 996.64, 999.31, 998.5, 998.51, 998.59, 510, 510.0, 510.9, 513, 513,0, 513.1, 519.2, 590.1, 590.10, 590.11, 590.80, 683, 320, 320.0, 320.1, 320.2, 320.3, 320.7, 320.8, 320.81, 320.82, 320.89, 320.9, 008.4, 008.41, 008.42, 008.43, 008.44, 008.45, 008.46, 008.47, 008.49, 480, 480.0, 480.1, 480.2, 480.3, 480.8, 480.9, 481, 482, 482.0, 482.1, 482.2, 482.3, 482.30, 482.31, 482.32, 482.39, 482.4, 482.40, 482.41, 482.42, 482.49, 482.8, 482.81, 482.82, 482.83, 482.84, 482.89, 482.9, 483, 483.0, 483.1, 483.8, 484, 484.1, 484.3, 484.5, 484.6, 484.7, 484.8, 485, 486, 567.22, 567.3, 567.31, 567.38, 567.39 |
| Acute renal failure | 584, 584.5, 584.6, 584.7, 584.8, 584.9 |
| Operative bleeding | 998.1, 998.11, 998.12 |
| GI bleed | 530.82, 531.0, 531.00, 531.01, 531.1, 531.10, 531.11, 531.2, 531.20, 531.21, 531.3, 531.30, 531.31, 532.0, 532.00, 532.01, 532.1, 532.10, 532.11, 532.2, 532.20, 532.21, 532.3, 532.30, 532.31, 533.0, 533.00, 533.01, 533.11, 533.2, 533.20, 533.21, 533.3, 533.30, 533.31, 534.0, 534.00, 534.01, 534.1, 534.10, 534.11, 534.2, 534.20, 534.21, 534.3, 534.30, 534.31, 535.01, 535.41, 535.51, 535.61, 578, 578.0, 578.1, 578.9 |
| Acute liver failure | 570 |
| DVT/PE | 415.1, 415.11, 415.12, 415.13, 415.19, 453.4, 453.40, 453.41, 453.42 |
| Acute MI | 410, 410.00, 410.01, 410.02, 410.1, 410.11, 410.12, 410.2, 410.21, 410.22, 410.3, 410.30, 410.31, 410.32, 410.4, 410.40, 410.41, 410.42, 410.5, 410.50, 410.51, 410.52, 410.6, 410.60, 410.61, 410.62, 410.7, 410.70, 410.71, 410.72, 410.8, 410.80, 410.81, 410.82, 410.9, 410.91, 410.92 |
| Other complications | 507.x, 45.11, 451.11, 451.19, 451.2, 451.81, 453.8, 453.9, 514, 518.4, 518.5, 518.81, 518.82, 530.xx, 54.12, 54.61, 29.51, 31.61, 33.41, 33.43, 42.82, 44.61, 46.71, 46.75, 48.71, 50.61, 51.91, 55.81, 56.82, 57.81, 58.41, 69.41, 569.83, 575.4, 996.69, 996.62, 996.68, 996.63, 996.65, 998.5x, 567.3x, 999.88, 999.39, 995.27, 996.31, 998.13, 997.60, 998.81, 998.89, 569.6x, 536.4x, 998.9, 998.4, 998.0x, 998.7, 998.1x, 998.31, 998.32, 998.30, 998.83, 998.6 |
IOC, intra-operative cholangiogram; ERC, endoscopic retrograde cholangiogram; ERCP, endoscopic retrograde cholangiopancreatography; MRI, magnetic resonance imaging; MRCP, magnetic resonance cholangiopancreatography; GI, gastrointestinal; DVT/PE, deep venous thrombosis/pulmonary embolism; MI, myocardial infarction.
Primary or secondary malignant neoplasm or neoplasm of uncertain behavior. Includes carcinoma in situ. Includes liver, biliary system, stomach, pancreas, small intestine, large intestine, spleen, retroperitoneum and abdominal lymph nodes.
Includes strictures, non-malignant obstructions, non-congenital cysts.
Funding sources
Howard Hughes Medical Institute Early Career Award, American Surgical Association Foundation Fellowship, American Cancer Society Mentored Research Scholar Grant (all to J.F.T.).
Conflict of interest
None to declare.
References
- 1.Rose JB, Bilderback P, Raphaeli T, Traverso W, Helton S, Ryan JA, Jr, et al. Use the duodenum, it's right there: a retrospective cohort study comparing biliary reconstruction using either the jejunum or the duodenum. JAMA Surg. 2013;148:860–865. doi: 10.1001/jamasurg.2013.2701. [DOI] [PubMed] [Google Scholar]
- 2.Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, et al. Postoperative bile duct strictures: management and outcomes in the 1990s. Ann Surg. 2000;232:430–441. doi: 10.1097/00000658-200009000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pitt HA, Sherman S, Johnson MS, Hollenbeck AN, Lee J, Daum MR, et al. Improved outcomes of bile duct injuries in the 21st century. Ann Surg. 2013;258:490–499. doi: 10.1097/SLA.0b013e3182a1b25b. [DOI] [PubMed] [Google Scholar]
- 4.Strasberg SM, Picus DD, Drebin JA. Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg. 2001;5:266–274. doi: 10.1016/s1091-255x(01)80047-0. [DOI] [PubMed] [Google Scholar]
- 5.Carroll JE, Jr, Hurwitz ZM, Simons JP, McPhee JT, Ng SC, Shah SA, et al. In-hospital mortality after resection of biliary tract cancer in the United States. HPB. 2010;12:62–67. doi: 10.1111/j.1477-2574.2009.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneider EB, Hyder O, Wolfgang CL, Hirose K, Choti MA, Makary MA, et al. Patient readmission and mortality after surgery for hepato-pancreato-biliary malignancies. J Am Coll Surg. 2012;215:607–615. doi: 10.1016/j.jamcollsurg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ragulin-Coyne E, Witkowski ER, Chau Z, Ng SC, Santry HP, Callery MP, et al. Is routine intraoperative cholangiogram necessary in the twenty-first century? A national view. J Gastrointest Surg. 2013;17:434–442. doi: 10.1007/s11605-012-2119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001;324:549–558. doi: 10.1097/00000658-200110000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolan JP, Diggs BS, Sheppard BC, Hunter JG. Ten-year trend in the national volume of bile duct injuries requiring operative repair. Surg Endosc. 2005;19:967–973. doi: 10.1007/s00464-004-8942-6. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project. Introduction to the HCUP Nationwide Inpatient Sample (NIS) [updated June 1013] Available at http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.pdf (last accessed 29 September 2014)
- 11.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality (HCUP) Cost-to-Charge Ratio Files [updated 22 October 2014] Available at http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. (last accessed 11 December 2014) [DOI] [PubMed]
- 13.Fatima J, Barton JG, Grotz TE, Geng Z, Harmsen WS, Huebner M, et al. Is there a role for endoscopic therapy as a definitive treatment for post-laparoscopic bile duct injuries? J Am Coll Surg. 2010;211:495–502. doi: 10.1016/j.jamcollsurg.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Weber A, Feussner H, Winkelmann F, Siewart JR, Schmid RM, Prinz C. Long-term outcome of endoscopic therapy in patients with bile duct injury after cholecystectomy. J Gastroenterol Hepatol. 2009;24:762–769. doi: 10.1111/j.1440-1746.2008.05713.x. [DOI] [PubMed] [Google Scholar]
- 15.Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy vs hepaticojejunostomy for reconstruction after resection of choledochal cyst. J Pediatr Surg. 2013;48:2336–2342. doi: 10.1016/j.jpedsurg.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 16.O'Rourke RW, Lee NN, Cheng J, Swanstrom LL, Hansen PD. Laparoscopic biliary reconstruction. Am J Surg. 2004;187:621–624. doi: 10.1016/j.amjsurg.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Pawlik TM, Olbrecht VA, Pitt HA, Gleisner AL, Choti MA, Shulick RD, et al. Primary sclerosing cholangitis: role of extrahepatic biliary resection. J Am Coll Surg. 2008;206:822–830. doi: 10.1016/j.jamcollsurg.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Rothlin M, Lopfe M, Schlumpf R, Largiader F. Long-term results of hepaticojejunostomy for benign lesions of the bile ducts. Am J Surg. 1998;175:22–26. doi: 10.1016/s0002-9610(97)00229-8. [DOI] [PubMed] [Google Scholar]
- 19.Khalid K, Shafi M, Dar HM, Durrani KM. Choledochoduodenostomy: reappraisal in the laparoscopic era. ANZ J Surg. 2008;78:495–500. doi: 10.1111/j.1445-2197.2008.04542.x. [DOI] [PubMed] [Google Scholar]
- 20.Birkenfeld S, Serour F, Levi S, Abulafia A, Balassiano M, Krispin M. Choledochoduodenostomy for benign and malignant biliary tract diseases. Surgery. 1988;103:408–410. [PubMed] [Google Scholar]
- 21.Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A. The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg. 1996;224:162–167. doi: 10.1097/00000658-199608000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zafar SN, Khan MR, Raza R, Khan MN, Kasi M, Rafiq A, et al. Early complications after biliary enteric anastomosis for benign diseases: a retrospective analysis. BMC Surg. 2011;11:19. doi: 10.1186/1471-2482-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005;241:786–792. doi: 10.1097/01.sla.0000161029.27410.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas L, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 25.Edwards EB, Roberts JP, McBride MA, Schulak JA, Hunsicker LG. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med. 1999;341:2049–2053. doi: 10.1056/NEJM199912303412703. [DOI] [PubMed] [Google Scholar]
- 26.Committee on the Consequences of Uninsurance. Care without coverage: too little, too late. Washington, DC: National Academy of Sciences; 2002. [Google Scholar]
- 27.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]


