Abstract
Background
Hepatopancreatobiliary (HPB) surgery fellowship training has multiple paths. Prospective trainees and employers must understand the differences between training pathways. This study examines self-reported fellowship experiences and current scope of practice across three pathways.
Methods
An online survey was disseminated to 654 surgeons. These included active Americas Hepato-Pancreato-Biliary Association (AHPBA) members and recent graduates of HPB, transplant–HPB and HPB–heavy surgical oncology fellowships.
Results
A total of 416 (64%) surgeons responded. Most respondents were male (89%) and most were practising in an academic setting (83%). 290 (70%) respondents underwent formal fellowship training. Although fellowship experiences varied, current practice was largely similar. Minimally invasive surgery (MIS) and ultrasound were the most commonly identified areas of training deficiencies and were, respectively, cited as such by 47% and 34% of HPB-, 49% and 50% of transplant-, and 52% and 25% of surgical oncology-trained respondents. Non-HPB cases performed in current practice included gastrointestinal (GI) and general surgery cases (56% and 49%, respectively) for HPB-trained respondents, transplant and general surgery cases (87% and 21%, respectively) for transplant-trained respondents, and GI surgery and non-HPB surgical oncology cases (70% and 28%, respectively) for surgical oncology-trained respondents.
Conclusions
Fellowship training in HPB surgery varies by training pathway. Training in MIS and ultrasound is deficient in each pathway. The ultimate scope of non-transplant HPB practice appears similar across training pathways. Thus, training pathway choice is best guided by the training experience desired and non-HPB components of anticipated practice.
Introduction
Hepatopancreatobiliary (HPB) surgery has become an increasingly popular subspecialty within general surgery. As most general surgery residents in the USA perform fewer than 15 pancreas, 13 hepatic and six complex biliary cases during residency,1 surgical trainees interested in HPB surgery careers have long sought fellowship training to augment residency operative experiences. Traditionally, formal HPB training was most often achieved through the completion of a fellowship in either transplant surgery or surgical oncology with or without a designated HPB track. Informal training could also be pursued through apprenticeship models at a variety of institutions with practitioners with widely varied practice emphases. More recently, another avenue for HPB surgery training has arisen through the Fellowship Council (FC) and Americas Hepato-Pancreato-Biliary Association (AHPBA)-accredited HPB surgery fellowships, which have drawn on the model of a few existing dedicated training pathways in HPB surgery. These programmes focus on the management of benign and malignant disease of the pancreas and liver and often also encompass some training in transplant surgery.
The training modalities presently available offer variable experiences in pancreas, liver and biliary cases, and each pathway offers unique training foci. In order to better understand the differences among graduates of the most common training pathways in HPB surgery, and to understand the impacts of these differences on future careers, the present authors conducted a survey of HPB surgeons. Specifically, the survey sought to assess current practice patterns as they relate to respondent fellowship training experiences.
Materials and methods
Survey development
The Education and Training Committee of the AHPBA in collaboration with representatives of the surgical oncology and transplant surgery community developed the survey. A survey statistician assisted with the construction of the survey questions. Questions evaluated demographics, type of fellowship training, perceived advantages and deficits of training within the respondent's respective fellowship pathway, and current practice patterns. Prior to dissemination, the survey was validated with 10 non-HPB general surgeons, general surgery residents and current HPB fellows in accredited fellowships in academic settings for clarity and response times.
Survey participants
The survey was disseminated to 654 surgeons, including active AHPBA members and recent graduates of HPB fellowships, transplant fellowships with substantial volumes of elective HPB cases, and surgical oncology fellowships with significant HPB training, using SurveyGizmo® Version 3.0 V2005–2014 (Widgix, LLC, Boulder, CO, USA). Survey distribution lists were compiled and culled to exclude duplicates. The survey population was gathered from lists of graduates of all AHPBA FC-accredited HPB surgery programmes from 2000 to 2011 and select Society of Surgical Oncology (SSO) programmes known to have high volumes of HPB surgery, American Society of Transplant Surgeons (ASTS) transplant surgery fellows who had applied for recent ASTS–HB or ASTS–HPB certificates, and active North American members of the AHPBA. Survey responses were collected between October 2012 and January 2013. Portions of the data from this survey have been reported previously.2
Data analysis
Summary and descriptive statistics were applied. Qualitative data were analysed from the comments received from survey participants to identify themes provided by respondents from each of the three formal training tracks.
Results
A total of 416 of 654 survey recipients completed the survey for a response rate of 64%. Because respondents’ ages and lengths of time in practice varied widely, training experiences included non-traditional training tracks, such as those based on apprenticeship models, and the study population included surgeons with no formal HPB training who currently have substantial HPB practices. Responses from individuals with no formal HPB training (n = 126) were excluded from analysis for the purposes of this study as the current study was designed to evaluate the variability in the training and practice of individuals completing formal training in one of three accredited North American HPB training pathways involving, respectively, HPB surgery, transplant surgery or surgical oncology. Of the 290 respondents completing formal fellowship training, 141 (49%) had completed transplant surgery training, 106 (37%) had completed a surgical oncology fellowship, and 43 (15%) had completed an FC-accredited AHPBA fellowship. As detailed in Table 1, the majority of respondents from all disciplines were males younger than 50 years of age. Within each fellowship pathway, the most commonly identified current practice type for graduates was academic practice in a university setting.
Table 1.
Demographics of respondents (n = 290) as a function of training track
| Transplant surgery (n = 141) | Surgical oncology (n = 106) | HPB surgery (n = 43) | |
|---|---|---|---|
| Age group, n (%) | |||
| 30–40 years | 27 (19%) | 47 (44%) | 27 (63%) |
| 41–50 years | 79 (56%) | 50 (47%) | 15 (35%) |
| 51–60 years | 28 (20%) | 9 (8%) | 1 (2%) |
| 61–70 years | 7 (5%) | 0 | 0 |
| Gender, n (%) | |||
| Male | 130 (92%) | 90 (85%) | 37 (86%) |
| Female | 11 (8%) | 16 (15%) | 6 (14%) |
| Current practice, n (%) | |||
| Private | 7 (5%) | 7 (7%) | 9 (21%) |
| Academic – university | 113 (80%) | 77 (73%) | 23 (53%) |
| Academic – community | 19 (14%) | 19 (18%) | 10 (23%) |
| Government | 2 (1%) | 3 (3%) | 1 (2%) |
| Years since fellowship training completed, median (range) | 10 (1–34) | 7 (1–23) | 3 (1–23) |
HPB, hepatopancreatobiliary.
In response to questions regarding perceived deficits in fellowship training, respondents from each fellowship pathway indicated they would have liked to have received more training in minimally invasive surgery (MIS) and ultrasonography (Fig. 1). The transplant surgery-trained (ASTS) respondents also indicated they would have preferred an increased volume of non-transplant pancreas operative cases (Fig. 1). In addition to the deficiencies demonstrated in Fig. 1, 42 (30%) ASTS, 10 (23%) HPB and 11 (10%) SSO respondents indicated a desire for training in tumour ablation techniques. Emergent themes were derived from the comments provided by individuals completing training across all pathways (Table 2).
Figure 1.
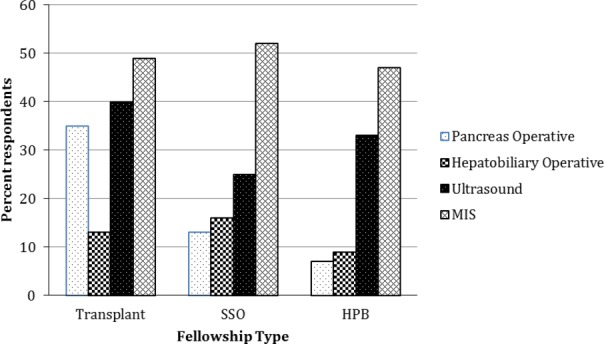
Prevalences of perceived deficits in training by training track. HPB, hepatopancreatobiliary (Fellowship Council track); MIS, minimally invasive surgery; SSO, Society of Surgical Oncology
Table 2.
Perceived deficits in fellowship experience training by track
| Themes: perceived deficits in training | Illustrative quotes representing the theme |
|---|---|
| Insufficient non-transplant HPB operative volume (ASTS, SSO) | • Greater volume would have been appreciated |
| • More complex biliary cases | |
| • More pancreas volume other than transplant | |
| Insufficient MIS operative volume (ASTS, SSO, HPB) | • More laparoscopic and MIS approaches |
| Insufficient benign HPB disease exposure (ASTS, SSO) | • More pancreatitis management |
| • Minimal exposure to benign biliary disease and pancreatitis | |
| Insufficient ultrasound training (ASTS, SSO, HPB) | • Formal ultrasound training would have been helpful |
| • Insufficient didactics [ultrasound], need constructive guidance | |
| • More intraoperative ultrasound training would be desirable | |
| Insufficient training in tumour ablation techniques (ASTS, SSO, HPB) | • Had little exposure |
| • Our group did not use ablation often | |
ASTS, American Society of Transplant Surgeons; HPB, hepatopancreatobiliary (Fellowship Council); MIS, minimally invasive surgery; SSO, Society of Surgical Oncology.
Figures 2a, b demonstrates self-reported case volumes for pancreas procedures performed in fellowship training and in current practice stratified by fellowship training pathway. Similarly, Figures 2c, d demonstrates self-reported hepatobiliary procedures completed in training and in current practice. Figure 2a shows that SSO and HPB fellowship training provides greater exposure to pancreas procedures than ASTS training. This generally translates to a more robust pancreas practice following completion of fellowship training; however, it is of note that 23% of ASTS-trained fellows reported that they perform over 25 pancreas cases annually in their current practice (Fig. 2b). Conversely, despite the more robust training in pancreatectomy reported by SSO and HPB fellowship-trained respondents (Fig. 2a), a substantial number of respondents reported performing fewer than 25 pancreatectomies annually in their current practice (44% of SSO-trained respondents and 40% of HPB-trained respondents) (Fig. 2b).
Figure 2.
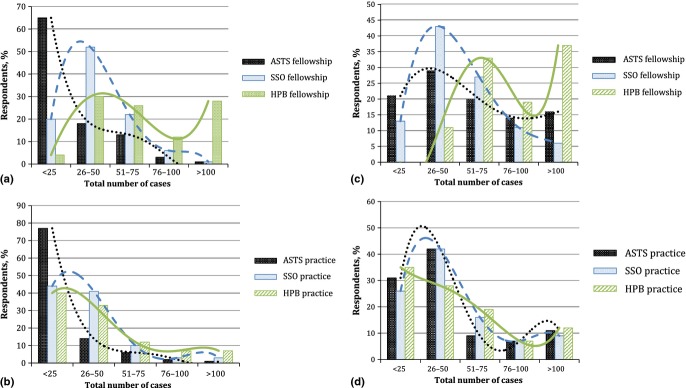
Fellowship and practice hepatobiliary and pancreas operative volumes stratified by training pathway. (a) Fellowship operative pancreas volume. (b) Current practice operative pancreas volume. (c) Fellowship operative hepatobiliary volume. (d) Current practice operative hepatobiliary volume. ASTS, American Society of Transplant Surgeons; HPB, hepatopancreatobiliary (Fellowship Council track); SSO, Society of Surgical Oncology
Figure 2c demonstrates a more varied distribution of hepatobiliary cases performed during fellowship training. As the trend lines show, the modal response of ASTS- and SSO-trained fellows referred to 26–50 cases, whereas that of HPB fellows indicated that over 100 hepatobiliary cases had been performed during fellowship training (Fig. 2c). Despite these differences in hepatobiliary training experience, the hepatobiliary volumes reported in current practice are very similar amongst graduates of all training pathways (Fig. 2d).
Figure 3 demonstrates the number of MIS cases performed per year as a function of the number of years since training. A small observable trend demonstrates that surgeons who are 10–15 years from training completion more commonly undertake slightly higher rates of MIS HPB cases. However, the vast majority of surgeons, regardless of graduating year, perform fewer than 20 MIS cases per year in current practice.
Figure 3.
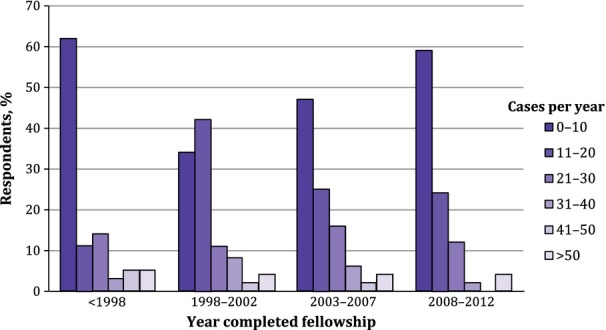
Current practice minimally invasive hepatopancreatobiliary surgery case mix as a function of year of training completion
Non-HPB cases routinely performed in practice most often consisted of gastrointestinal (GI) surgery and general surgery cases (56% and 49%, respectively) for HPB-trained respondents, transplant and general surgery cases (87% and 21%, respectively) for transplant-trained respondents, and GI surgery and non-HPB surgical oncology cases (70% and 28%, respectively) for surgical oncology-trained respondents.
Discussion
As increasing numbers of trainees interested in HPB pathways seek formal fellowship training, it is important to understand the differences between the various training pathways available in HPB surgery. Transparency around the components of training and how that translates into the scope of a surgeon's ultimate practice is critical information for all stakeholders, including trainees, hospitals and patients. In addition, the current study provides information on the perceived deficits in training, as well as current practice patterns of surgeons who have embarked upon various training pathways in HPB surgery. This work provides further insight into ongoing work underway in the HPB surgery community, which seeks to ensure that graduating trainees are adequately and more uniformly prepared for successful practice. Recent efforts such as the Consensus Conference on Training in HPB Surgery (http://www.ahpba.org/ahpba-sponsored-consensus-conferences) reflect a desire amongst leaders of the AHPBA, SSO and ASTS to establish appropriately robust and transparent metrics for HPB training for graduating fellows across all HPB training pathways. This collaboration will facilitate the development of a more consistently qualified graduate of HPB training, and may ultimately provide guidance to hospitals in their evaluation and privileging of prospective HPB surgeons.
The present study demonstrates that HPB fellows in all fellowship pathways desire greater experience with ultrasound, MIS and ablation techniques. Unique to the transplant and surgical oncology pathways are the desires for greater experience with (non-transplant) HPB cases and exposure to the management of benign HPB disease. Specifically, 35% of ASTS fellows desired more pancreas operative experience and 65% of ASTS fellows reported performing fewer than 25 pancreas cases during fellowship training. Although the majority of ASTS-trained HPB surgeons perform fewer than 25 pancreas cases in practice per year, 23% reported that pancreas cases represent a significant proportion of their practice and that they undertake over 25 cases annually. Similarly, in the qualitative comments, SSO-trained HPB surgeons reported a desire for greater fellowship experience in the management of benign disease, most commonly pancreatitis. This is likely to reflect the fact that surgeons completing ASTS and SSO pathways of training who then develop a dedicated HPB practice are called upon to manage benign HPB disease and benign/inflammatory pancreatic disease even if their fellowship did not encompass this scope of practice. Further support of this organ-based transference in practice derives from the fact that similar current practice patterns are seen across all training tracks, which implies that when a practitioner advertises as an HPB surgeon, he or she will be presented with a certain case mix.
The limits of this study include the likelihood of recall and selection biases, given that there was no defined protocol for selecting the fellowship graduates chosen for survey dissemination. Nevertheless, this study demonstrates that the breadth of operative training experience varies quite considerably across fellowship training pathways. For instance, HPB fellowship-trained respondents reported the greatest depth of experience in pancreas and hepatobiliary cases performed during fellowship, with 28% of respondents reporting the completion of more than 100 pancreas cases (Fig. 2a) and 37% reporting the completion of over 100 hepatobiliary cases (Fig. 2c) during fellowship training. This increased experience is not surprising in light of the fact that these fellowships are focused solely on HPB training, whereas SSO- and ASTS-trained fellows also learn skills in other relevant domains unique to their fellowship training pathways. Interestingly, despite these differences, practice patterns with respect to pancreas and hepatobiliary operative volumes are ultimately quite similar. Thus, the primary difference in ultimate practice reflects the composition of the rest of the surgeon's case mix, which appears to fluctuate by fellowship training pathway. In light of this observation, the selection of a particular fellowship training pathway should be driven by the trainee's desired training experience and scope of future practice.
With respect to quality of training and readiness for HPB surgical practice, the issue of whether common minimal training standards should be established across all fellowship training pathways must be considered. The variability in experience in both pancreas and hepatobiliary training across fellowship pathways is remarkable, especially in the context of the similarities among ultimate practice patterns. Although there are currently only minimal data on the learning curve required for the attainment of proficiency in the performance of pancreas and hepatobiliary cases, minimum volumes of 20 pancreaticoduodenectomies to reach the inflection point for acceptable operative morbidity and 60 pancreaticoduodenectomies to achieve mortality rates comparable with those demonstrated by experts are considered necessary.3 In addition, training must obviously encompass all aspects of disease management and is not measured solely by case volumes.4,5 Many investigators in the USA have noted that high-volume centres and high-volume surgeons tend to have superior outcomes after complex pancreatic surgery and hepatic resection.6,7 These findings are also borne out in more straightforward HPB surgical procedures such as laparoscopic cholecystectomy in large-scale analyses.8 Thus, consideration of the development of minimum common standards for pancreas and hepatobiliary surgical training across pathways would be ideal and would decrease the variability in training presently observed across training pathways with respect to pancreas and hepatobiliary experiences. In addition, given the recent concerns expressed regarding the over-production of HPB surgeons in the USA and Canada, the elevation of consistent training standards in HPB surgery across all fellowship training pathways will potentially serve to mitigate the risk for over-production.2,9 This is not to suggest that the other aspects of fellowship training across the three training pathways should be the same; indeed, the diversity of training currently expressed in HPB, complex surgical oncology and ASTS–HB or ASTS–HPB fellowships with respect to the other elements of training is desirable because it will allow for the development of a more flexible surgical workforce.
Although there is not one optimal training modality for HPB fellowship training in North America, it is clear that the HPB surgeon of the future should anticipate a blended practice of HPB surgery along with another component of practice. As such, trainees would be best served by exposure to a variety of malignant and benign disease, as well as increased experience in MIS and ultrasonography during training.
Conflicts of interest
None declared.
References
- 1.Sachs TE, Ejaz A, Weiss M, Spolverato G, Ahuja N, Makary MA, et al. Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: is the operative experience enough? Surgery. 2014;156:385–393. doi: 10.1016/j.surg.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minter RM, Alseidi A, Hong JC, Jeyarajah DR, Greig PD, Dixon E, et al. Training in hepatopancreatobiliary surgery: assessment of the hepatopancreatobiliary surgery workforce in North America. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001096. PMID: 25751311 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010;145:634–640. doi: 10.1001/archsurg.2010.118. [DOI] [PubMed] [Google Scholar]
- 4.Merlino J. Defining the volume–quality debate: is it the surgeon, the center, or the training? Clin Colon Rectal Surg. 2007;20:231–236. doi: 10.1055/s-2007-984867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Langer B. Role of volume outcome data in assuring quality in HPB surgery. HPB. 2007;9:330–334. doi: 10.1080/13651820701611234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Jr, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J Am Coll Surg. 2004;199:31–38. doi: 10.1016/j.jamcollsurg.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009;249:635–640. doi: 10.1097/SLA.0b013e31819ed958. [DOI] [PubMed] [Google Scholar]
- 8.Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA. Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci. 2010;55:2398–2405. doi: 10.1007/s10620-009-1035-6. [DOI] [PubMed] [Google Scholar]
- 9.Scarborough JE, Pietrobon R, Bennett KM, Clary BM, Kuo PC, Tyler DS, et al. Workforce projections for hepato-pancreato-biliary surgery. J Am Coll Surg. 2008;206:678–684. doi: 10.1016/j.jamcollsurg.2007.11.016. [DOI] [PubMed] [Google Scholar]


