Abstract
Background
There is limited information from population-based investigations of the associations between sleep duration and sleep disorders and parameters of glucose homeostasis. The objective of the present study was to examine cross-sectional associations between sleep duration and sleep disordered breathing with concentrations of insulin, fasting and 2-h glucose, and HbA1c.
Methods
Data from 11 815 adults aged ≥20 years without diagnosed diabetes (5002 with an oral glucose tolerance test) from the National Health and Nutrition Examination Survey 2005–2010 were used. Information about sleep duration (2005–2010) and sleep apnea and sleep-disordered breathing (2005–2008) was obtained via questionnaire.
Results
An estimated 36.0% of participants reported sleeping ≤6 h/night, 62.0% reported sleeping 7–9 h/night, and 2.0% reported sleeping ≥10 h/night. In 2005–2008, 33.0% reported snoring ≥5 nights per week, 5.9% reported they snorted, gasped, or stopped breathing ≥5 nights/week, and 4.2% reported sleep apnea. Sleep duration was significantly associated with fasting concentrations of insulin and concentrations of HbA1c only in models that did not adjust for body mass index (BMI). Concentrations of fasting and 2-h glucose were significantly associated with sleep duration in models that adjusted only for age. Snoring frequency was positively associated with concentrations of insulin and HbA1c. Frequency of snorting or stopping breathing and sleep apnea status were associated with concentrations of insulin and of HbA1c only when BMI was not accounted for.
Conclusion
In a representative sample of US adults, concentrations of insulin and HbA1c were significantly associated with short sleep duration, possibly mediated by BMI.
Keywords: glucose, glycated hemoglobin, insulin, sleep apnea, sleep
Introduction
In modern society, the quantity and quality of sleep has increasingly come under assault, and sizable percentages of the population experience inadequate quantity or quality of sleep. For example, approximately 28% of US adults reported insufficient rest or sleep for 14 or more days during a 30-day period.1 Furthermore, there is evidence that the quantity of sleep may have declined in recent decades.2–6
A growing base of research has linked inadequate or excessive sleep and sleep disordered breathing, which includes snoring and sleep apnea, to a host of adverse somatic and psychological effects. For example, disturbances of sleep duration have been linked to obesity,7 diabetes,8 cardiovascular disorders,9 and all-cause mortality.10,11 Previous studies have found that short (<7 h) and long (≥9 h) sleep durations are associated with diabetes and impaired glucose tolerance.12,13 Furthermore, a review of prospective studies has shown that short sleep duration predicted the development of impaired fasting glucose14 and diabetes.11 Some research has shown that sleep disordered breathing may be associated with insulin resistance15–18 and disturbances of glucose homeostasis.19–25
In light of the growing burden of diabetes in the US,26 an improved understanding of the possible relationships between sleep disturbances and the disturbance of glucose homeostasis may provide important clues to reducing the burden of this disease. Relatively little information about the associations between sleep duration with fasting and 2-h glucose concentrations is available. Because the pathophysiology of fasting and 2-h glucose involves different processes and the rate of progression of impaired fasting glucose and impaired glucose tolerance to diabetes differs, examining the associations between sleep duration and these glucose parameters may provide insights into the mechanisms through which sleep duration may affect the development of diabetes. Furthermore, observational studies have yielded mixed evidence concerning the associations between sleep duration and insulin resistance,13,14,27–33 and thus additional evidence is useful to better evaluate these potential associations. Therefore, the objective of the present study was to examine the cross-sectional associations between self-reported sleep duration and several parameters of sleep-disordered breathing with several glycemic measures, including concentrations of fasting glucose, 2-h glucose, and HbA1c as well as insulin in a nationally representative sample of adults in the US.
Methods
The present study included data from the National Health and Nutrition Examination Survey (NHANES) 2005–2010. Each 2-year cycle yields a nationally representative sample of the civilian, non-institutionalized US population selected by using a multistage, stratified sampling design. Participants were interviewed at home and were invited to attend a mobile examination center, where they were asked to complete additional questionnaires, to undergo a set of examinations, and to provide a blood sample. Interview and examination response rates for the three consecutive 2-year cycles exceeded 70%. The surveys received approval from the National Center for Health Statistics Research Ethics Review Board, and participants were asked to sign an informed consent form. Details about the survey may be found elsewhere.34
Participants who responded affirmatively to the question “Have you ever been told by a doctor or health professional you have diabetes or sugar diabetes?” were considered to have diagnosed diabetes and were excluded from the study. Concentrations of glucose were measured by using the hexokinase method (NHANES 2005–2006: Roche/Hitachi 911 [Roche Diagnostics, Indianapolis, IN, USA]; NHANES 2007–2010: Roche Modular P chemistry analyzer [Roche Diagnostics]). Concentrations of insulin were measured by using the ELISA method (NHANES 2005–2009: Merocodia Insulin [Mercodia AB, Uppsala, Sweden]) or chemiluminescent immunoassay (NHANES 2009–2010: Elecsys 2010 analyzer [Roche Diagnostics]). Concentrations of HbA1c were measured on an A1c 2.2 Plus Glycohemoglobin Analyzer during 2005–2006 or an A1c G7 HPLC Glycohemoglobin Analyzer during 2007–2010 (Tosoh Medics, South San Francisco, CA, USA).
A subset of participants attending the morning examination and who had fasted for at least 9 h was subjected to an oral glucose tolerance test (OGTT). Fasting and 2-h plasma glucose measurements were obtained.
From 2005 to 2010, sleep duration was assessed with the question, “How much sleep do you usually get at night on weekdays or workdays?” Because the National Sleep Foundation suggests sleeping 7–9 h per night (http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need, accessed 20 October 2013), we created the following three categories of sleeping duration: (i) ≤6 h/night; (ii) 7–9 h/night; and (iii) ≥10 h/night. In addition, for 2005–2008, participants were asked “In the past 12 months, how often did you snore while you were sleeping?” and “In the past 12 months, how often did you snort, gasp, or stop breathing while you were asleep?” Response categories for both questions included never, rarely (1–2 nights/week), occasionally (3–4 nights/week), and frequently (5 or more nights/week). Participants were also asked about having been diagnosed with a sleep disorder with the question “Have you ever been told by a doctor or other health professional that you have a sleep disorder?” and were then asked if that disorder included sleep apnea.
Covariates included age, gender, race or ethnicity (White, African American, Mexican American, other Hispanic, other race), educational status (<high school, high school graduate or equivalent, >high school), smoking status (never, former, current), self-reported leisure-time physical activity, alcohol use, body mass index (BMI; kg/m2), and histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid problems, liver disease, and cancer. Current cigarette smokers were defined as participants who had smoked ≥100 cigarettes during their lifetime and were still smoking. Former smokers were defined as participants who had smoked ≥100 cigarettes during their lifetime but had stopped. Participants who had smoked <100 cigarettes during their lifetime were classified as never having smoked. To estimate leisure-time physical activity for 2005–2006, we summed the product of weekly time spent in each activity reported by the participant multiplied by the metabolic equivalent of task (MET) value for that activity yielding a MET-h index. One MET is the energy expenditure of 1 kcal/kg body weight per h. For 2007–2010, the physical activity questionnaire was changed. We estimated weekly MET-h for moderate and vigorous activities from questions asking participants about their participation in moderate and vigorous activities, the number of days per week engaged in these activities, and the number of minutes engaged in these activities on a typical day. Using questions from the alcohol use questionnaire, the following three levels of alcohol use were created: excessive (men: >2 drinks/day; women: >1 drink/day); moderate (men between >0 and <2 drinks/day; women between >0 and 1 drink/day); and none. The BMI was calculated from measured weight and height. Participants were considered to have cardiovascular disease if they reported they had ever been told by a doctor or other health professional that they had congestive heart failure, coronary heart disease, angina, heart attack, or stroke. Participants were defined as having chronic obstructive pulmonary disease if they reported that they still had chronic bronchitis or had ever been told they had emphysema.
We limited the analyses to participants who were aged ≥20 years and who reported not having been diagnosed with diabetes. Analyses pertaining to concentrations of fasting and 2-h glucose and fasting insulin were limited to those who had an OGTT. Analyses pertaining to HbA1c used all fasting and non-fasting participants. The significance of differences in mean and percentage values was tested with t-tests and Chi-squared tests, respectively. We used linear regression analysis to calculate adjusted least-squares mean concentrations of glucose and glycosylated hemoglobin and geometric mean concentrations of insulin after various adjustments. We examined the associations between sleeping parameters and plasma concentrations of fasting and 2-h glucose, serum concentrations of insulin, and concentrations of HbA1c. We used SUDAAN (RTI International, Research Triangle Park, NC, USA) for our statistical analyses to account for the complex survey design. Sampling weights were used to calculate estimates (means, percentages).
Results
Sleep duration
A total of 17 132 participants attended the mobile examination center and, of these, 6225 had an OGTT in 2005–2010. Measurements of fasting and 2-h glucose concentrations and fasting concentrations of insulin were available for 6225, 5462, and 6144 participants, respectively. After excluding pregnant women and participants with missing values for these variables, covariates, and sleeping duration and sleep disorder, 5002 participants were included in the analyses of sleep duration. The 5002 participants who had an OGTT included 2545 men, 2457 women, 2568 Whites, 867 African Americans, 904 Mexican Americans, and 663 of another race or ethnicity. The median age was 45 years.
Of the attendees to the mobile examination center, 15 612 had a measurement for HbA1c. After excluding pregnant women and participants with missing values for covariates, and sleeping duration and sleep disorder, 11 815 participants who had an examination were included in analyses involving HbA1c.
Relationships between covariates and sleep duration are given in Table 1.
Table 1.
Selected age-adjusted characteristics among participants aged ≥20 years without diagnosed diabetes according to level of sleeping duration, National Health and Nutrition Examination Survey 2005–2010
| Sleep duration (h/night) | |||||
|---|---|---|---|---|---|
| 1–6 | 7–9 | 10+ | Plinear trend | Pquadratic trend | |
| Results for HbA1c sample | |||||
| No. subjects | 4586 | 6948 | 281 | – | – |
| Unadjusted prevalence, weighted (%) | 36.0 (0.7) | 62.0 (0.7) | 2.0 (0.1) | – | – |
| Age (years) | 45.3 ± 0.4 | 46.2 ± 0.4 | 47.1 ± 1.6 | 0.270 | 0.977 |
| BMI (kg/m2) | 28.8 ± 0.1 | 27.9 ± 0.1 | 27.1 ± 0.5 | <0.001 | 0.970 |
| Physical activity (MET-h/week) | 15.4 ± 0.6 | 16.2 ± 0.6 | 10.4 ± 2.4 | 0.056 | 0.007 |
| Men (%) | 51.6 (0.8) | 47.8 (0.6) | 39.4 (3.4) | 0.001 | 0.258 |
| White (%) | 66.4 (2.1) | 76.2 (1.6) | 68.9 (3.9) | 0.467 | <0.001 |
| ≥ High school graduate (%) | 80.9 (0.8) | 83.6 (1.0) | 73.7 (2.2) | 0.003 | <0.001 |
| Current smoker (%) | 27.5 (1.0) | 19.3 (0.8) | 37.7 (3.6) | 0.007 | <0.001 |
| Excess alcohol intake (%) | 8.4 (0.6) | 9.3 (0.5) | 14.5 (2.8) | 0.026 | 0.155 |
| History of: | |||||
| CVD (%) | 8.3 (0.5) | 5.9 (0.3) | 9.0 (1.8) | 0.700 | 0.008 |
| COPD (%) | 4.8 (0.5) | 2.9 (0.3) | 6.7 (1.8) | 0.296 | 0.003 |
| Arthritis (%) | 26.7 (0.7) | 21.6 (0.5) | 31.6 (3.7) | 0.200 | <0.001 |
| Thyroid (%) | 8.6 (0.5) | 9.8 (0.4) | 11.5 (2.3) | 0.198 | 0.870 |
| Liver (%) | 3.2 (0.3) | 2.6 (0.2) | –‡‡ | – | – |
| Cancer (%) | 8.5 (0.5) | 9.3 (0.4) | 8.8 (2.1) | 0.868 | 0.548 |
| Snoring ≥5 nights/week (%)* | 37.3 (1.2) | 29.7 (1.0) | 39.7 (7.0) | 0.738 | 0.019 |
| Snorting, gasping, or stopping breathing ≥5 nights/week (%)† | 7.3 (0.6) | 5.0 (0.5) | –‡‡ | – | – |
| Sleep apnea (%)‡ | 5.2 (0.5) | 3.6 (0.3) | –‡‡ | – | – |
| Results for OGTT sample | |||||
| No. subjects | 1943 | 2939 | 120 | – | – |
| Unadjusted prevalence, weighted (%) | 36.3 (1.2) | 61.7 (1.3) | 2.0 (0.2) | – | – |
| Age (years) | 44.7 ± 0.5 | 46.0 ± 0.5 | 46.3 ± 2.1 | 0.474 | 0.694 |
| BMI (kg/m2) | 28.9 ± 0.2 | 28.0 ± 0.1 | 27.8 ± 1.0 | 0.229 | 0.494 |
| Physical activity (MET-h/week) | 16.3 ± 0.8 | 16.2 ± 0.8 | 9.7 ± 2.1 | 0.005 | 0.001 |
| Men (%) | 52.8 (1.3) | 47.0 (1.0) | 38.9 (4.5) | 0.003 | 0.682 |
| White (%) | 65.8 (2.1) | 75.7 (1.6) | 70.4 (5.4) | 0.381 | 0.014 |
| ≥High school graduate (%) | 82.3 (1.0) | 83.9 (0.9) | 70.9 (4.6) | 0.021 | 0.004 |
| Current smoker (%) | 25.9 (1.3) | 19.4 (1.1) | 37.4 (5.7) | 0.051 | <0.001 |
| Excess alcohol intake (%) | 8.1 (1.0) | 9.5 (0.7) | –‡‡ | – | – |
| History of: | |||||
| CVD(%) | 9.2 (0.8) | 5.9 (0.5) | 7.2 (1.6) | 0.287 | 0.024 |
| COPD (%) | 4.6 (0.6) | 3.5 (0.4) | –‡‡ | – | – |
| Arthritis (%) | 27.5 (1.4) | 22.9 (0.8) | 44.0 (5.9) | 0.008 | <0.001 |
| Thyroid (%) | 7.9 (0.8) | 10.3 (0.6) | –‡‡ | – | – |
| Liver (%) | 3.1 (0.6) | 2.9 (0.3) | –‡‡ | – | – |
| Cancer (%) | 8.4 (0.7) | 9.1 (0.5) | –‡‡ | – | – |
| Snoring ≥5 nights/week (%)§ | 37.0 (1.5) | 29.4 (1.4) | 42.5 (10.1) | 0.570 | 0.065 |
| Snorting, gasping, or stopping breathing ≥5 nights/week (%)** | 7.6 (0.8) | 4.8 (0.8) | –‡‡ | – | – |
| Sleep apnea (%)†† | 5.2 (0.7) | 3.0 (0.5) | –‡‡ | – | – |
Data are given as either the mean ± SE or as percentage (SE).
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 2584, 3929, and 144, respectively.
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 2643, 4069, and 148, respectively.
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 2783, 4298, and 166, respectively.
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 1112, 1655, and 58, respectively.
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 1126, 1706, and 56, respectively.
Results available for 2005–2008 only. Sample sizes in the 1–6, 7–9, and 10+ h/night groups are 1187, 1784, and 65, respectively.
Data do not meet standards of precision or reliability (relative standard errors >30%).
BMI, body mass index; MET-h, metabolic equivalent-hour; OGTT, oral glucose tolerance test; CVD, cardiovascular disease; COPD, chronic obstructive pulmonary disease.
In models that did not adjust for BMI, sleep duration was significantly associated with fasting mean concentrations of insulin and concentrations of HbA1c reflecting significant differences between participants who reported sleeping ≤6 h/night and those who reported sleeping 7–9 h/night (Table 2). However, after adjusting for BMI no significant associations remained. Of the 5002 participants with an OGTT, mean concentrations of fasting and 2-h glucose were significantly associated with sleep duration only in models that adjusted for age.
Table 2.
Adjusted geometric mean (± SE) insulin concentrations and mean (± SE) values for fasting plasma glucose, 2-h plasma glucose, and HbA1c levels according to self-reported sleep duration among participants aged ≥20 years without diagnosed diabetes, National Health and Nutrition Examination Survey 2005–2010
| Sleep duration (h/night) | |||||
|---|---|---|---|---|---|
| 1–6 | 7–9 | 10+ | Padjusted Wald F-test | Plinear contrast | |
| No. subjects | 4586 | 6948 | 281 | – | – |
| HbA1c (%) | |||||
| Model 1* | 5.45 ± 0.01 | 5.38 ± 0.01 | 5.39 ± 0.04 | <0.001 | 0.154 |
| Model 2† | 5.43 ± 0.01 | 5.39 ± 0.01 | 5.37 ± 0.04 | 0.002 | 0.119 |
| Model 3‡ | 5.43 ± 0.01 | 5.40 ± 0.01 | 5.36 ± 0.04 | 0.007 | 0.086 |
| Model 4§ | 5.43 ± 0.01 | 5.40 ± 0.01 | 5.36 ± 0.04 | 0.007 | 0.079 |
| Model 5** | 5.42 ± 0.01 | 5.40 ± 0.01 | 5.39 ± 0.04 | 0.155 | 0.427 |
| No. subjects | 1943 | 2939 | 120 | – | – |
| Insulin (pmol/L) | |||||
| Model 1* | 58.7 ± 1.3 | 52.6 ± 1.2 | 52.1 ± 4.9 | 0.002 | 0.218 |
| Model 2† | 57.8 ± 1.3 | 53.1 ± 1.2 | 51.8 ± 4.7 | 0.015 | 0.245 |
| Model 3‡ | 58.0 ± 1.3 | 52.9 ± 1.1 | 51.7 ± 4.4 | 0.008 | 0.194 |
| Model 4§ | 57.8 ± 1.3 | 53.1 ± 1.1 | 50.8 ± 4.4 | 0.010 | 0.150 |
| Model 5** | 55.8 ± 1.0 | 54.1 ± 0.9 | 54.0 ± 4.3 | 0.277 | 0.696 |
| Fasting glucose (mmol/L) | |||||
| Model 1* | 5.6 ± <0.1 | 5.5 ± <0.1 | 5.5 ± 0.1 | 0.026 | 0.207 |
| Model 2† | 5.6 ± <0.1 | 5.5 ± <0.1 | 5.5 ± 0.1 | 0.129 | 0.265 |
| Model 3‡ | 5.6 ± <0.1 | 5.5 ± <0.1 | 5.5 ± 0.1 | 0.129 | 0.261 |
| Model 4§ | 5.6 ± <0.1 | 5.5 ± <0.1 | 5.5 ± 0.1 | 0.150 | 0.288 |
| Model 5** | 5.6 ± <0.1 | 5.5 ± <0.1 | 5.5 ± 0.1 | 0.632 | 0.608 |
| 2-h Glucose (mmol/L) | |||||
| Model 1* | 6.6 ± 0.1 | 6.3 ± 0.1 | 6.7 ± 0.2 | 0.034 | 0.628 |
| Model 2† | 6.5 ± 0.1 | 6.3 ± 0.1 | 6.6 ± 0.2 | 0.085 | 0.937 |
| Model 3‡ | 6.6 ± 0.1 | 6.3 ± 0.1 | 6.6 ± 0.2 | 0.075 | 0.957 |
| Model 4§ | 6.6 ± 0.1 | 6.3 ± 0.1 | 6.6 ± 0.2 | 0.084 | 0.899 |
| Model 5** | 6.5 ± 0.1 | 6.4 ± 0.1 | 6.7 ± 0.2 | 0.173 | 0.450 |
Adjusted for age.
Adjusted for age, gender, race or ethnicity, and education.
Adjusted for age, gender, race or ethnicity, education, smoking status, leisure-time physical activity, and alcohol use.
Adjusted for variables in Model 3 plus histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid disease, liver disease, and cancer.
Adjusted for variables in Model 4 plus body mass index.
The associations between sleep duration and concentrations of insulin (Pinteraction = 0.039) but not concentrations of HbA1c (Pinteraction = 0.980), fasting glucose (Pinteraction = 0.247), and 2-h glucose (Pinteraction = 0.075) differed by gender for Model 5. Among men, adjusted mean (± SE) concentrations of insulin were 60.7 ± 1.5 pmol/L for men sleeping ≤6 h/night, 56.0 ± 1.1 pmol/L for men sleeping 7–9 h/night, and 59.5 ± 9.9 pmol/L for men sleeping ≥10 h/night (Padjusted Wald F-test = 0.011). Among women, adjusted mean (± SE) concentrations of insulin were 51.2 ± 1.4 pmol/L for women sleeping ≤6 h/night, 52.3 ± 1.1 pmol/L for women sleeping 7–9 h/night, and 49.0 ± 4.7 pmol/L for women sleeping ≥10 h/night (Padjusted Wald F-test = 0.651).
Furthermore, the associations between sleep duration and concentrations of 2-h glucose (Pinteraction = 0.039), but not insulin (Pinteraction = 0.438), fasting glucose (Pinteraction = 0.093), and HbA1c (Pinteraction = 0.634), differed by race or ethnicity. The mean (± SE) concentrations of 2-h glucose for participants who reported sleeping 1–6, 7–9, or ≥10 h/night were 6.6 ± 0.1, 6.4 ± 0.1, and 6.5 ± 0.2 mmol/L, respectively, for Whites (Padjusted Wald F-test = 0.386); 6.1 ± 0.1, 6.3 ± 0.1, and 5.6 ± 0.4 mmol/L, respectively, for African Americans (Padjusted Wald F-test = 0.211); and 6.8 ± 0.2, 6.5 ± 0.2, and 8.9 ± 0.9 mmol/L, respectively, for Mexican Americans (Padjusted Wald F-test = 0.011).
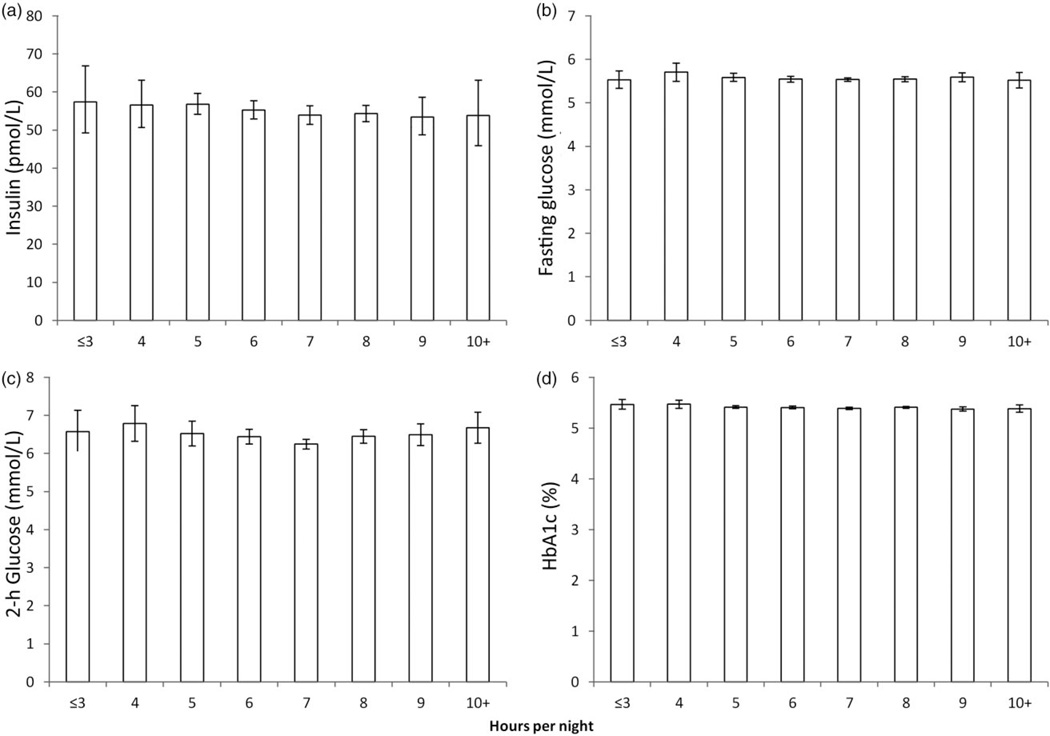
To examine adjusted mean concentrations of the four measures across a broader range of categories of sleep duration, we created eight categories of sleep duration. After maximal adjustment as in Model 5 of Table 2, no significant associations between sleep duration and concentrations of insulin (Padjusted Wald F-test = 0.701; Plinear contrast = 0.391), fasting glucose (Padjusted Wald F-test = 0.389; Plinear contrast = 0.557), and 2-h glucose (Padjusted Wald F-test = 0.188; Plinear contrast = 0.705) were present (Fig. 1). However, a small but significant inverse linear trend for concentrations of HbA1c was present (Padjusted Wald F-test = 0.080; Plinear contrast = 0.047).
Figure 1.
Adjusted mean concentrations of (a) insulin, (b) fasting glucose, (c) 2-h glucose, and (d) HbA1c as a function of sleep duration among adults aged ≥20 years, National Health and Nutrition Examination Survey 2005–2010. Mean values were adjusted for age, gender, race or ethnicity, education, smoking status, leisure-time physical activity, alcohol use, histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid disease, liver disease, and cancer, and body mass index. Data show the mean ± 95% confidence interval.
Sleep disorders
From 2005 to 2008, 7456 adults aged ≥20 years had an HbA1c measurement after excluding participants with diagnosed diabetes, pregnant women, and people with missing values for covariates. Of these, 6657 were included in analyses for snoring, 6860 for snorting, gasping, or stopping breathing, and 7247 for apnea.
Of the 3849 adults aged ≥20 years who had an OGTT, consecutive exclusions for participants with diagnosed diabetes, pregnant women, participants with missing values for covariates left 3336, 3322, and 3124 adults, respectively. Of these participants, 2825 were included in analyses for snoring, 2888 for snorting, gasping, or stopping breathing, and 3036 for apnea.
Snoring
Without adjustment for BMI, robust linear trends for increasing mean concentrations of insulin, fasting glucose, 2-h glucose, and HbA1c were present (Table 3). After additional adjustment for BMI, no significant associations between snoring frequency and mean concentrations of fasting and 2-h glucose were evident. However, significant increases in mean concentrations of insulin and HbA1c remained, although the increases were greatly attenuated. We did not detect significant interactions for concentrations of the four outcomes by gender or by race or ethnicity.
Table 3.
Adjusted geometric mean (± SE) insulin concentrations and mean (± SE) values for fasting plasma glucose, 2-h plasma glucose, and HbA1c levels according to self-reported snoring frequency among participants aged >20 years without diagnosed diabetes, National Health and Nutrition Examination Survey 2005–2008
| Snore frequency (nights/week) | ||||||
|---|---|---|---|---|---|---|
|
Padjusted (Wald F-test) |
Plinear contrast | |||||
| Never | 1–2 | 3–4 | 5 + | |||
| No. subjects, unweighted | 1921 | 1281 | 1253 | 2202 | – | – |
| Unadjusted prevalence, weighted (%) | 28.8 ±0.9 | 19.7 ±0.6 | 18.5±0.8 | 33.0 ±0.8 | – | – |
| HbA1c (%) (n = 6657) | ||||||
| Model 1 * | 5.30 ± 0.01 | 5.31 ± 0.01 | 5.39 ± 0.02 | 5.44 ± 0.02 | <0.001 | <0.001 |
| Model 2† | 5.30 ± 0.01 | 5.31 ± 0.01 | 5.39 ± 0.02 | 5.43 ± 0.02 | <0.001 | <0.001 |
| Model 3‡ | 5.30 ± 0.01 | 5.32 ± 0.01 | 5.39 ± 0.02 | 5.43 ± 0.02 | <0.001 | <0.001 |
| Model 4§ | 5.30 ± 0.01 | 5.32 ± 0.01 | 5.39 ± 0.02 | 5.43 ± 0.02 | <0.001 | <0.001 |
| Model 5** | 5.34 ± 0.01 | 5.33 ± 0.01 | 5.38 ± 0.02 | 5.39 ± 0.02 | 0.001 | <0.001 |
| No. subjects | 782 | 561 | 541 | 941 | – | – |
| Unadjusted prevalence, weighted (%) | 27.8 ± 1.2 | 20.5 ± 1.0 | 19.0 ± 1.0 | 32.7 ± 1.1 | – | – |
| Insulin (pmol/L) (n = 2825) | ||||||
| Model 1 * | 42.2 ± 1.7 | 47.2 ± 1.9 | 53.9 ± 2.1 | 62.8 ± 2.2 | <0.001 | <0.001 |
| Model 2† | 42.5 ± 1.7 | 47.4 ± 1.9 | 53.6 ± 2.1 | 62.3 ± 2.3 | <0.001 | <0.001 |
| Model 3‡ | 42.0 ± 1.5 | 47.4 ± 1.8 | 53.0 ± 2.2 | 63.4 ± 2.2 | <0.001 | <0.001 |
| Model 4§ | 42.1 ± 1.5 | 47.2 ± 1.8 | 53.1 ± 2.2 | 63.4 ± 2.1 | <0.001 | <0.001 |
| Model 5** | 48.9 ± 1.7 | 49.7 ± 1.6 | 52.5 ± 1.8 | 54.4 ± 1.7 | 0.034 | 0.016 |
| Fasting glucose (mmol/L) (n = 2825) | ||||||
| Model 1 * | 5.4 ± 0.0 | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.7 ± 0.0 | <0.001 | <0.001 |
| Model 2† | 5.5 ± 0.0 | 5.5± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 0.007 | 0.001 |
| Model 3‡ | 5.5 ± 0.0 | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 0.006 | <0.001 |
| Model 4§ | 5.5 ± 0.0 | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 0.009 | 0.001 |
| Model 5** | 5.6 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 5.5 ± 0.0 | 0.485 | 0.764 |
| 2-h Glucose (mmol/L) (n = 2825) | ||||||
| Model 1 * | 6.1 ± 0.1 | 6.3 ± 0.1 | 6.5 ± 0.1 | 6.6 ± 0.1 | 0.001 | <0.001 |
| Model 2† | 6.1 ± 0.1 | 6.3 ± 0.1 | 6.4 ± 0.1 | 6.6 ± 0.1 | 0.002 | <0.001 |
| Model 3‡ | 6.1 ± 0.1 | 6.3± 0.1 | 6.4 ± 0.1 | 6.6 ± 0.1 | 0.001 | <0.001 |
| Model 4§ | 6.1 ± 0.1 | 6.3± 0.1 | 6.4 ± 0.1 | 6.6 ± 0.1 | 0.001 | <0.001 |
| Model 5** | 6.3 ± 0.1 | 6.4 ± 0.1 | 6.4 ± 0.1 | 6.4 ± 0.1 | 0.659 | 0.226 |
Adjusted for age.
Adjusted for age, gender, race or ethnicity, and education.
Adjusted for age, gender, race or ethnicity, education, smoking status, leisure-time physical activity, and alcohol use.
Adjusted for variables in Model 3 plus histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid disease, liver disease, and cancer.
Adjusted for variables in Model 4 plus body mass index.
Snorting, gasping, or stopping breathing
The frequency of snorting, gasping, or stopping breathing was not significantly associated with mean concentrations of fasting and 2-h glucose in any of the models. Without adjustment for BMI, mean concentrations of insulin and HbA1c increased significantly as the frequency of snorting, gasping, or stopping breathing increased (Table 4). Once BMI was controlled for, no significant associations remained. No significant interactions for any of the four outcomes by gender were present, and no significant interactions for concentrations of insulin, fasting glucose, and 2-h glucose by race or ethnicity were present. However, the association between snorting, gasping, or stopping breathing and concentrations of HbA1c varied among the three major racial or ethnic groups (Pinteraction = 0.020). No significant associations between snorting, gasping, or stopping breathing and concentrations of HbA1c were present among Whites (Padjusted Wald F-test = 0.354) and Mexican Americans (Padjusted Wald F-test = 0.426). Among African Americans, the frequency of snorting, gasping, or stopping breathing and concentrations of HbA1c were inversely associated (Padjusted Wald F-test = 0.003).
Table 4.
Adjusted geometric mean (± SE) insulin concentrations and mean (± SE) values of fasting plasma glucose, 2-h plasma glucose, and HbA1c according to self-reported snorting or stopping breathing frequency among participants aged ≥20 years without diagnosed diabetes, National Health and Nutrition Examination Survey 2005–2008
| Snorting/stopping breathing frequency (nights/week) |
Padjusted (Wald F-test) |
Plinear contrast | ||||
|---|---|---|---|---|---|---|
| Never | 1–2 | 3–4 | 5 + | |||
| No. subjects | 5463 | 585 | 424 | 388 | – | – |
| Unadjusted prevalence, weighted (%) | 79.7 ± 0.7 | 8.5 ± 0.3 | 5.9 ± 0.3 | 5.9 ± 0.5 | – | – |
| HbA1c (%) (n = 6860) | ||||||
| Model 1* | 5.34 ± 0.01 | 5.38 ± 0.02 | 5.42 ± 0.03 | 5.47 ± 0.04 | 0.001 | 0.001 |
| Model 2† | 5.34 ± 0.01 | 5.38 ± 0.02 | 5.40 ± 0.03 | 5.47 ± 0.04 | 0.002 | 0.002 |
| Model 3‡ | 5.34 ± 0.01 | 5.38 ± 0.02 | 5.40 ± 0.03 | 5.46 ± 0.04 | 0.005 | 0.004 |
| Model 4§ | 5.34 ± 0.01 | 5.38 ± 0.02 | 5.40 ± 0.03 | 5.46 ± 0.04 | 0.007 | 0.004 |
| Model 5** | 5.35 ± 0.01 | 5.37 ± 0.02 | 5.38 ± 0.03 | 5.40 ± 0.04 | 0.507 | 0.225 |
| No. subjects | 2291 | 251 | 184 | 162 | – | – |
| Unadjusted prevalence, weighted (%) | 79.1 ± 0.9 | 8.5 ± 0.5 | 6.5 ± 0.4 | 5.9 ± 0.6 | – | – |
| Insulin (pmol/L) (n = 2888) | ||||||
| Model 1* | 48.6 ± 1.2 | 57.6 ± 3.7 | 59.5 ± 4.2 | 71.6 ± 5.3 | <0.001 | <0.001 |
| Model 2† | 48.7 ± 1.2 | 57.0 ± 3.6 | 59.2 ± 4.2 | 71.0 ± 5.4 | <0.001 | <0.001 |
| Model 3‡ | 48.7 ± 1.1 | 57.0 ± 3.7 | 59.7 ± 3.9 | 70.8 ± 5.2 | <0.001 | <0.001 |
| Model 4§ | 48.8 ± 1.1 | 57.1 ± 3.6 | 59.3 ± 3.8 | 69.6 ± 5.1 | <0.001 | <0.001 |
| Model 5** | 50.7 ± 1.0 | 51.7 ± 3.3 | 53.0 ± 2.9 | 54.3 ± 2.9 | 0.600 | 0.179 |
| Fasting glucose (mmol/L) (n = 2888) | ||||||
| Model 1* | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.1 | 5.7 ± 0.1 | 0.045 | 0.013 |
| Model 2† | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 0.292 | 0.125 |
| Model 3‡ | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.1 | 5.6 ± 0.0 | 0.313 | 0.141 |
| Model 4§ | 5.5 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.0 | 5.6 ± 0.1 | 0.385 | 0.193 |
| Model 5** | 5.6 ± 0.0 | 5.5 ± 0.0 | 5.5 ± 0.0 | 5.5 ± 0.1 | 0.424 | 0.379 |
| 2-h Glucose (mmol/L) (n = 2888) | ||||||
| Model 1* | 6.3 ± 0.1 | 6.6 ± 0.1 | 6.2 ± 0.2 | 6.6 ± 0.2 | 0.080 | 0.448 |
| Model 2† | 6.3 ± 0.1 | 6.5 ± 0.1 | 6.2 ± 0.2 | 6.6 ± 0.2 | 0.103 | 0.564 |
| Model 3‡ | 6.3 ± 0.1 | 6.5 ± 0.1 | 6.2 ± 0.2 | 6.6 ± 0.2 | 0.105 | 0.612 |
| Model 4§ | 6.3 ± 0.1 | 6.5 ± 0.1 | 6.2 ± 0.2 | 6.5 ± 0.2 | 0.084 | 0.681 |
| Model 5** | 6.4 ± 0.1 | 6.4 ± 0.1 | 6.0 ± 0.2 | 6.2 ± 0.2 | 0.141 | 0.079 |
Adjusted for age.
Adjusted for age, gender, race or ethnicity, and education.
Adjusted for age, gender, race or ethnicity, education, smoking status, leisure-time physical activity, and alcohol use.
Adjusted for variables in Model 3 plus histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid disease, liver disease, and cancer.
Adjusted for variables in Model 4 plus body mass index.
Sleep apnea
The mean (±SE) prevalence of sleep apnea was 4.2 ± 0.3% among 7247 participants in the HbA1c analytic sample and 3.8 ± 0.4% among 3036 participants in the OGTT sample. Mean concentrations of fasting and 2-h glucose did not differ significantly between adults reporting sleep apnea and those who did not (Table 5). Without adjustment for BMI, adults with sleep apnea had significantly higher mean concentrations of insulin and HbA1c. However, after adjustment for BMI, mean concentrations of insulin and HbA1c no longer remained significantly different between the two groups. We found no significant interactions by gender or race or ethnicity for the four outcomes.
Table 5.
Adjusted geometric mean (± SE) insulin concentrations and mean (± SE) values of fasting plasma glucose, 2-h plasma glucose, and HbA1c by levels of self-reported sleep apnea among participants aged ≥20 years without diagnosed diabetes, National Health and Nutrition Examination Survey 2005–2008
| Sleep apnea |
Padjusted (Wald F-test) |
||
|---|---|---|---|
| Yes | No | ||
| No. subjects | 283 | 6964 | – |
| HbA1c (%) (n = 7247) | |||
| Unadjusted prevalence, weighted (%) | 4.2 (0.3) | 95.8 (0.3) | |
| Model 1* | 5.49 ± 0.04 | 5.37 ± 0.01 | 0.004 |
| Model 2† | 5.51 ± 0.04 | 5.36 ± 0.01 | 0.002 |
| Model 3‡ | 5.50 ± 0.04 | 5.37 ± 0.01 | 0.004 |
| Model 4§ | 5.50 ± 0.04 | 5.37 ± 0.01 | 0.005 |
| Model 5** | 5.41 ± 0.05 | 5.37 ± 0.01 | 0.391 |
| No. subjects | 114 | 2922 | – |
| Insulin (pmol/L) (N = 3036) | |||
| Unadjusted prevalence, weighted (%) | 3.8 (0.4) | 96.2 (0.4) | |
| Model 1* | 81.4 ± 0.3 | 50.1 ± 0.3 | <0.001 |
| Model 2† | 81.7 ± 0.3 | 50.1 ± 0.3 | <0.001 |
| Model 3‡ | 79.2 ± 0.3 | 50.1 ± 0.3 | <0.001 |
| Model 4§ | 75.5 ± 0.3 | 50.2 ± 0.3 | <0.001 |
| Model 5** | 53.8 ± 0.3 | 50.9 ± 0.3 | 0.510 |
| Fasting Glucose (mmol/L) (N = 3036) | |||
| Model 1* | 5.7 ± 0.1 | 5.6 ± 0.0 | 0.093 |
| Model 2† | 5.7 ± 0.1 | 5.6 ± 0.0 | 0.148 |
| Model 3‡ | 5.7 ± 0.1 | 5.6 ± 0.0 | 0.165 |
| Model 4§ | 5.7 ± 0.1 | 5.6 ± 0.0 | 0.233 |
| Model 5** | 5.5 ± 0.1 | 5.6 ± 0.0 | 0.468 |
| 2-h Glucose (mmol/L) (N = 3036) | |||
| Model 1* | 6.7 ± 0.3 | 6.4 ± 0.1 | 0.474 |
| Model 2† | 6.7 ± 0.3 | 6.4 ± 0.1 | 0.348 |
| Model 3‡ | 6.7 ± 0.3 | 6.4 ± 0.1 | 0.393 |
| Model 4§ | 6.6 ± 0.3 | 6.4 ± 0.1 | 0.501 |
| Model 5** | 6.2 ± 0.3 | 6.4 ± 0.1 | 0.456 |
Adjusted for age.
Adjusted for age, gender, race or ethnicity, and education.
Adjusted for variables in Model 2 plus smoking status, leisure-time physical activity, and alcohol use.
Adjusted for variables in Model 3 plus histories of cardiovascular disease, chronic obstructive pulmonary disease, arthritis, thyroid disease, liver disease, and cancer.
Adjusted for variables in Model 4 plus body mass index.
Discussion
Using a large national sample of US adults, we found that sleep duration and sleep disordered breathing were most consistently associated with concentrations of HbA1c and insulin. These significant associations were substantially attenuated when BMI was adjusted for, suggesting that BMI may mediate the associations between sleep duration and sleep-disordered breathing and concentrations of HbA1c and insulin.
Cross-sectional and prospective studies have generally observed that short sleep duration is associated with hyperglycemia.11–14,16,35 A meta-analysis of seven prospective studies found that the relative risk for type 2 diabetes associated with short sleep duration was 1.28 (95% confidence interval 1.03, 1.60).11 Of the three glycemic parameters included in the present study (i.e. HbA1c, fasting glucose, and 2-h glucose) only concentrations of HbA1c were significantly associated with sleep duration. A previous analysis of NHANES data did not find a significant association between sleep duration and pre-diabetes.36
Short-term studies have mostly found that sleep restriction adversely affects insulin sensitivity.37–46 Of interest is a study reporting that sleep restriction during the first week of a 3-week period decreased insulin sensitivity, but that sleep restriction at the end of 3 weeks no longer had a significant effect on insulin sensitivity,46 raising the possibility that short-term sleep restriction exerts an acute effect on insulin sensitivity but that adaptive responses kick in with longer periods of sleep restriction.
The results from cross-sectional observational studies yield an inconsistent picture of associations between sleep duration and surrogate measures of insulin resistance.14,27–33 Sleep duration assessed in these studies probably reflects a mostly stable habitual sleep pattern. An analysis of 453 Japanese patients who were having a health examination reported that those sleeping <6 h had higher unadjusted homeostasis model assessment of insulin resistance (HOMA-IR) means than those sleeping ≥6 h.28 An analysis of data from over 900 participants of the Wisconsin Sleep Cohort Study found that sleep duration was not associated with fasting concentrations of insulin, but was significantly associated with the quantitative insulin-sensitivity check index.29 Of 740 adults in the Quebec Family study, participants who slept 7–8 h/night had significantly lower mean concentrations of insulin than participants sleeping <7 h and those sleeping 9–10 h.13 Data from 1455 participants from the Western New York Health study failed to find a significant association between sleep duration and HOMA-IR.14 A study of 115 participants without diabetes in the Coronary Artery Risk Development in Young Adults study who were studied with actigraphy failed to find significant associations with concentrations of insulin and glucose.27 Among 854 men and 640 women of the Anqing Twin Cohort, sleep duration ≤7 h/night was associated with HOMA-IR in women but not in men.30 However, the China Health and Nutrition Survey study of 1124 participants in Jiangsu Province did not find an association between sleep duration and HOMA-IR.31 Another study of 433 vegetarian Taiwanese adults did find a significant association between sleep duration dichotomized at 8 h and HOMA-IR.32 Finally, a cross-sectional study of 771 Danish adults did not find a significant association between sleep duration and several surrogate measures of insulin resistance.33
Because adjustment for BMI clearly had an important effect on the analyses, at least two interpretations concerning the models that adjusted for BMI should be considered. First, inadequate sleep or disturbances of sleep may promote increased BMI, which, in turn, leads to disturbances of glucose homeostasis. Second, BMI may act as a confounder of the association between sleep duration or disturbances and glycemic parameters.
If the first interpretation is true, several mechanisms have been postulated to explain the acute and chronic effects of sleep deprivation on concentrations of insulin. Sleep restriction may increase hunger and appetite, leading to increased energy intake and poor dietary habits,38,47–49 as well as reduced energy expenditure.50 Ultimately, these increases in energy intake and reductions in energy expenditure lead to weight gain51 and obesity,7 which are both related to increased concentrations of insulin and insulin resistance. In addition, disruption of the hypothalamic–pituitary axis may affect energy balance and weight. Weight gain as an explanation for hyperinsulinemia and insulin resistance reflects a longer-term effect of sleep disruption. However, shorter-term mechanisms may also be at work because previous studies have shown that sleep deprivation for as little as one night was able to affect insulin sensitivity.40,41,52–54 Mechanisms for these shorter-term disruptions of insulin sensitivity may operate, in part, through alterations in the sympathovagal balance and counter-regulatory hormones.55
Weight gain is a well-established cause for hyperglycemia, providing a ready explanation for potential long-term effects of sleep restriction on hyperglycemia. However, short-term mechanisms are at work as well. Epinephrine, norepinephrine, glucagon, cortisol, and non-esterified fatty acids have all been postulated as potential mechanisms linking short sleep duration to hyperglycemia. However, the evidence that short sleep duration affects these physiological mechanisms in ways that lead to hyperglycemia is mixed.38,39,41,52,55,56
With a few exceptions, we also failed to find that participants who reported having sleep disordered breathing (snoring; snorting, gasping, or stopping breathing; and sleep apnea) had higher concentrations of fasting and 2-h glucose, HbA1c, and insulin, especially once BMI was controlled for. Several cross-sectional epidemiologic studies using population-based samples have more specifically linked sleep-disordered breathing, mostly assessed with questionnaires, but some with polysomnography, to glucose intolerance and insulin resistance.16,21,23,35,57–59 The results from epidemiologic studies have found support from clinical studies using polysomnography or other laboratory methods.16,21 Furthermore, prospective studies have found that snoring predicts incident diabetes.60,61
The representative sample and large sample size were important strengths of the present study. The interpretation of our study results is constrained by several limitations. First, a cross-sectional study such as ours generally cannot establish the directionality of an association. However, because prospective studies have linked sleep duration to the incidence of diabetes,11 an effect of sleep restriction on concentrations of insulin is not inconceivable. Second, sleep duration was self-reported and subject to erroneous reporting and some degree of misclassification. However, research suggests an acceptable level of agreement between self-reported sleep duration and more objectively assessment of sleep duration.62 The question about sleep duration only pertained to week days or working days. Third, control of possible confounding factors is of critical importance, and residual confounding in the present study cannot be ruled out. Complicating decisions concerning the selection of possible confounders is the possibility that some of purported confounders may, in fact, be mediating variables. Fourth, the percentage of participants who reported sleeping ≥10 h/night was small and, therefore, estimates for this group may be more susceptible to sampling variation. Finally, a fraction of adults who snored, snorted, gasped, or stopped breathing may not have been identified because the participants were unaware of these concerns. To examine this latter concern, we conducted a sensitivity analysis for snoring in which we limited the analyses to participants who reported being married or living together (Model 5 in Table 2). The results were similar to the original analyses.
In conclusion, sleep duration and sleep disordered breathing indicators were mostly only significantly associated with concentrations of insulin, fasting and 2-h glucose, and HbA1c as long as BMI was not accounted for in this largest study to date of adults who had an OGTT. Future large-scale studies using actigraphy or other techniques will be valuable to gain further insights into the relationships between various measures of sleep pathology and glucose homeostasis and insulin resistance.
Significant findings of the study
Sleep duration, frequency of snorting, gasping, or stopping breathing, and sleep apnea were significantly associated with concentrations of fasting plasma glucose, insulin, and HbA1c as long as body mass index (BMI) was not controlled for. Snoring frequency was positively associated with concentrations of insulin and HbA1c even after controlling for BMI.
What this study adds
Using a representative sample of adults in the US, the present study provides new information about the associations between sleep duration and sleep morbidity and concentrations of fasting and 2-h glucose, fasting insulin, and HbA1c.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Disclosure
The authors have no conflict of interest to declare.
References
- 1.Centers for Disease Control and Prevention. Perceived insufficient rest or sleep among adults–United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1175–1179. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Percentage of adults who reported an average of <6 hours of sleep per 24-hour period, by sex and age group–United States, 1985 and 2004. MMWR Morb Mortal Wkly Rep. 2005;54:933. [Google Scholar]
- 3.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: Sleep time and its relationship to waking activities. Sleep. 2007;30:1085–1095. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kronholm E, Partonen T, Laatikainen T, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: A comparative review and re-analysis of Finnish population samples. J Sleep Res. 2008;17:54–62. doi: 10.1111/j.1365-2869.2008.00627.x. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. QuickStats: Percentage of adults aged >18 years who reported an average of <6 hours of sleep per 24-hour period, by sex and age group–National Health Interview Survey, United States, 1985 and 2006. MMWR Morb Mortal Wkly Rep. 2008;57:209. [Google Scholar]
- 6.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 10.Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 11.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 13.Chaput JP, Despres JP, Bouchard C, Tremblay A. Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia. 2007;50:2298–2304. doi: 10.1007/s00125-007-0786-x. [DOI] [PubMed] [Google Scholar]
- 14.Rafalson L, Donahue RP, Stranges S, et al. Short sleep duration is associated with the development of impaired fasting glucose: The Western New York Health Study. Ann Epidemiol. 2010;20:883–889. doi: 10.1016/j.annepidem.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vgontzas AN, Chrousos GP. Sleep-disordered breathing, sleepiness, and insulin resistance: Is the latter a consequence, a pathogenetic factor, or both? Sleep Med. 2002;3:389–391. doi: 10.1016/s1389-9457(02)00067-9. [DOI] [PubMed] [Google Scholar]
- 16.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol. 2003;136:167–178. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 17.Harsch IA, Hahn EG, Konturek PC. Insulin resistance and other metabolic aspects of the obstructive sleep apnea syndrome. Med Sci Monit. 2005;11:RA70–RA75. [PubMed] [Google Scholar]
- 18.Clarenbach CF, West SD, Kohler M. Is obstructive sleep apnea a risk factor for diabetes? Discov Med. 2011;12:17–24. [PubMed] [Google Scholar]
- 19.Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med. 2005;165:447–452. doi: 10.1001/archinte.165.4.447. [DOI] [PubMed] [Google Scholar]
- 20.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: A population-based study. Am J Respir Crit Care Med. 2005;172:1590–1595. doi: 10.1164/rccm.200504-637OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tasali E, Mokhlesi B, Van CE. Obstructive sleep apnea and type 2 diabetes: Interacting epidemics. Chest. 2008;133:496–506. doi: 10.1378/chest.07-0828. [DOI] [PubMed] [Google Scholar]
- 22.Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med. 2009;122:1122–1127. doi: 10.1016/j.amjmed.2009.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valham F, Stegmayr B, Eriksson M, Hagg E, Lindberg E, Franklin KA. Snoring and witnessed sleep apnea is related to diabetes mellitus in women. Sleep Med. 2009;10:112–117. doi: 10.1016/j.sleep.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Marshall NS, Wong KK, Phillips CL, Liu PY, Knuiman MW, Grunstein RR. Is sleep apnea an independent risk factor for prevalent and incident diabetes in the Busselton Health Study? J Clin Sleep Med. 2009;5:15–20. [PMC free article] [PubMed] [Google Scholar]
- 25.Priou P, Le VM, Meslier N, et al. Independent association between obstructive sleep apnea severity and glycated hemoglobin in adults without diabetes. Diabetes Care. 2012;35:1902–1906. doi: 10.2337/dc11-2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. 2011 National diabetes fact sheet. [accessed 20 September 2012]; Available from: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.
- 27.Knutson KL, Van Cauter E, Zee P, Liu K, Lauderdale DS. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: The Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care. 2011;34:1171–1176. doi: 10.2337/dc10-1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shigeta H, Shigeta M, Nakazawa A, Nakamura N, Yoshikawa T. Lifestyle, obesity, and insulin resistance. Diabetes Care. 2001;24:608. doi: 10.2337/diacare.24.3.608. [DOI] [PubMed] [Google Scholar]
- 29.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu R, Zee PC, Chervin RD, et al. Short sleep duration is associated with insulin resistance independent of adiposity in Chinese adult twins. Sleep Med. 2011;12:914–919. doi: 10.1016/j.sleep.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zuo H, Shi Z, Yuan B, et al. Interaction between physical activity and sleep duration in relation to insulin resistance among non-diabetic Chinese adults. BMC Public Health. 2012;12:247. doi: 10.1186/1471-2458-12-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang JK, Koo M, Kao VY, Chiang JK. Association of sleep duration and insulin resistance in Taiwanese vegetarians. BMC Public Health. 2012;12:666. doi: 10.1186/1471-2458-12-666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Byberg S, Hansen AL, Christensen DL, et al. Sleep duration and sleep quality are associated differently with alterations of glucose homeostasis. Diabet Med. 2012;29:e354–e360. doi: 10.1111/j.1464-5491.2012.03711.x. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. About the national health and nutrition examination survey. [accessed 18 March 2011]; Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 35.Facco FL, Grobman WA, Kramer J, Ho KH, Zee PC. Self-reported short sleep duration and frequent snoring in pregnancy: Impact on glucose metabolism. Am J Obstet Gynecol. 2010;203:142–145. doi: 10.1016/j.ajog.2010.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alshaarawy O, Teppala S, Shankar A. Markers of sleep-disordered breathing and prediabetes in US adults. Int J Endocrinol. 2012;2012:902324. doi: 10.1155/2012/902324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rasmussen MH, Wildschiodtz G, Juul A, Hilsted J. Polysomnographic sleep, growth hormone insulin-like growth factor-I axis, leptin, and weight loss. Obesity. 2008;16:1516–1521. doi: 10.1038/oby.2008.249. [DOI] [PubMed] [Google Scholar]
- 38.Nedeltcheva AV, Kessler L, Imperial J, Penev PD. Exposure to recurrent sleep restriction in the setting of high caloric intake and physical inactivity results in increased insulin resistance and reduced glucose tolerance. J Clin Endocrinol Metab. 2009;94:3242–3250. doi: 10.1210/jc.2009-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmid SM, Jauch-Chara K, Hallschmid M, Schultes B. Mild sleep restriction acutely reduces plasma glucagon levels in healthy men. J Clin Endocrinol Metab. 2009;94:5169–5173. doi: 10.1210/jc.2009-0969. [DOI] [PubMed] [Google Scholar]
- 40.Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59:2126–2133. doi: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Donga E, van Dijk M, van Dijk JG, et al. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95:2963–2968. doi: 10.1210/jc.2009-2430. [DOI] [PubMed] [Google Scholar]
- 42.Schmid SM, Hallschmid M, Jauch-Chara K, et al. Disturbed glucoregulatory response to food intake after moderate sleep restriction. Sleep. 2011;34:371–377. doi: 10.1093/sleep/34.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Broussard JL, Ehrmann DA, Van CE, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: A randomized, crossover study. Ann Intern Med. 2012;157:549–557. doi: 10.7326/0003-4819-157-8-201210160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gonnissen HK, Hursel R, Rutters F, Martens EA, Westerterp-Plantenga MS. Effects of sleep fragmentation on appetite and related hormone concentrations over 24 h in healthy men. Br J Nutr. 2012 doi: 10.1017/S0007114512001894. PMID: 22682471 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 45.St-Onge MP, O’Keeffe M, Roberts AL, RoyChoudhury A, Laferrere B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35:1503–1510. doi: 10.5665/sleep.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robertson MD, Russell-Jones D, Umpleby AM, Dijk DJ. Effects of three weeks of mild sleep restriction implemented in the home environment on multiple metabolic and endocrine markers in healthy young men. Metabolism. 2013;62:204–211. doi: 10.1016/j.metabol.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 47.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 48.Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr. 2010;91:1550–1559. doi: 10.3945/ajcn.2009.28523. [DOI] [PubMed] [Google Scholar]
- 49.St-Onge MP, Roberts AL, Chen J, et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am J Clin Nutr. 2011;94:410–416. doi: 10.3945/ajcn.111.013904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schmid SM, Hallschmid M, Jauch-Chara K, et al. Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am J Clin Nutr. 2009;90:1476–1482. doi: 10.3945/ajcn.2009.27984. [DOI] [PubMed] [Google Scholar]
- 51.Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity. 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 53.VanHelder T, Symons JD, Radomski MW. Effects of sleep deprivation and exercise on glucose tolerance. Aviat Space Environ Med. 1993;64:487–492. [PubMed] [Google Scholar]
- 54.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: A novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99:2008–2019. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 55.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11:163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schmid SM, Hallschmid M, Jauch-Chara K, Bandorf N, Born J, Schultes B. Sleep loss alters basal metabolic hormone secretion and modulates the dynamic counter-regulatory response to hypoglycemia. J Clin Endocrinol Metab. 2007;92:3044–3051. doi: 10.1210/jc.2006-2788. [DOI] [PubMed] [Google Scholar]
- 57.Juuti AK, Hiltunen L, Rajala U, et al. Association of abnormal glucose tolerance with self-reported sleep apnea among a 57-year-old urban population in Northern Finland. Diabetes Res Clin Pract. 2008;80:477–482. doi: 10.1016/j.diabres.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 58.Tuomilehto H, Peltonen M, Partinen M, et al. Sleep-disordered breathing is related to an increased risk for type 2 diabetes in middle-aged men, but not in women: The FIN-D2D survey. Diabetes Obes Metab. 2008;10:468–475. doi: 10.1111/j.1463-1326.2007.00729.x. [DOI] [PubMed] [Google Scholar]
- 59.Qiu C, Enquobahrie D, Frederick IO, Abetew D, Williams MA. Glucose intolerance and gestational diabetes risk in relation to sleep duration and snoring during pregnancy: A pilot study. BMC Womens Health. 2010;10:17. doi: 10.1186/1472-6874-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elmasry A, Janson C, Lindberg E, Gislason T, Tageldin MA, Boman G. The role of habitual snoring and obesity in the development of diabetes: A 10-year follow-up study in a male population. J Intern Med. 2000;248:13–20. doi: 10.1046/j.1365-2796.2000.00683.x. [DOI] [PubMed] [Google Scholar]
- 61.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: A prospective study. Am J Epidemiol. 2002;155:387–393. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 62.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–183. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]