Abstract
OBJECTIVES: Emergency department (ED) providers are faced with the challenge of diagnosing and treating patients in a timely fashion given many obstacles including limited patient information, complex disease states, and high patient turnover. Time delays in administration or selection of appropriate drug therapies have been associated with negative outcomes in severe infections. This study was conducted to assess the impact of an emergency medicine pharmacist (EPh) on the selection of appropriate antibiotics and the timeliness of administration in pediatric patients in the ED.
METHODS: Patients younger than 18 years were evaluated who were admitted through the ED and received 1 dose of intravenous antibiotic for the following conditions: community-acquired pneumonia, complicated skin and soft tissue infection (SSTI), meningitis, and sepsis. To evaluate the impact of the presence of an EPh, patients with orders placed during the EPh's hours of 1 pm and 11 pm were compared to those with an order placed between 11 pm and 1 pm.
RESULTS: A total of 142 patients were included in the study. Patients seen during EPh hours received an appropriate first antibiotic 93.4% of the time (p = 0.157) and second antibiotic 96.8% of the time (p = 0.023). Time from order to verification was significantly shorter for the first 2 antimicrobials in the EPh group (10.5 minutes [p = 0.003] and 11.4 minutes [p = 0.047], respectively). The days from discharge to return to readmission to the ED were also significantly different (17.5 days vs. 62.4 days, p = 0.008).
CONCLUSIONS: The available data suggest that patients are more likely to receive appropriate doses of antimicrobials, and in a more timely fashion, whenever the EPh is present. Areas for future investigation include whether the presence of EPhs at the bedside has the potential to impact areas of patient care, including readmission rates, drug costs, and medication errors.
INDEX TERMS: antibiotic, adverse reactions, emergency medicine, medication errors, pediatrics
INTRODUCTION
The emergency department (ED) serves as the gateway to the hospital setting for most patients, including pediatric patients. Emergency medicine providers are faced with diagnosing and treating patients with mild to severe infections in a timely fashion given multiple obstacles (i.e., high patient turnover, limited available information).1 Major pharmacotherapy hurdles to overcome across all age groups in the ED are antibiotic selection, dosing, and timeliness of antibiotic administration. Inappropriate dosing is one of the most common medication errors that is reported in the pediatric patient population.2,3 This is related to several factors including the need to dose medications by weight as compared to an adult population where doses are relatively standard and independent of weight or age. Also, there may be inconsistencies in growth rates as a pediatric patient ages, which further adds to the inability of providers to quickly recognize when a dose is incorrect even in patients of the similar age. In addition to opportunities associated with empiric antibiotic dosing (e.g., computer order entry, different recommendations from various resources), ensuring the timeliness of antibiotic administration in the ED can also be an issue. Time delays in medication administration may be linked to presentation-level factors, patient-level factors, and system-level factors. Examples include, but are not limited to, extended waiting times for evaluation and diagnosis, atypical presentations, and ED crowding. These time delays may not impact patients with minor infections, but studies4–6 have shown that antibiotic timing does impact outcomes in adult patients with pneumonia and other severe infections. Though these evaluations did not have a pediatric emphasis, the clinical impact of their results transcends age categories, and clinicians can assume that the importance of timely antimicrobial administration applies to severe pediatric infections as well.
Outcomes in health care can be optimized when a team approach is used. It is no exception that providers can use this team approach when it comes to dosing and selection of empiric antibiotics and timeliness of antibiotic administration.1–3,5,6 The role of emergency medicine pharmacists (EPhs) continues to evolve, and research has shown that EPhs play an important role in optimizing the pharmacotherapy provided to patients while in the ED.4,7,8 Emergency medicine pharmacists have the knowledge and skills to evaluate appropriate antimicrobial therapy at adequate doses and to facilitate the delivery of medications to the bedside to ensure timely therapy.
It has been shown that medication errors can be reduced with the presence of a clinical pharmacist providing immediate, direct feedback at the time of order entry and medication administration, up to 58% in 1 evaluation.1,7,9–11 Dosing errors have also been noted as one of the most frequent opportunities identified and one of the most common errors prevented by EPhs.4,7,12 This study attempts to delineate whether the presence of an EPh impacts the appropriateness of antibiotic selection or the timeliness of administration.
MATERIALS AND METHODS
Following obtainment of institutional review board approval, patients meeting inclusion criteria who presented to the ED during the study period of January 1, 2011, and December 31, 2011, were retrospectively reviewed. Informed consent was not required by the institutional review board. The inclusion criteria included patients younger than 18 years who received at least 1 dose of an intravenous antimicrobial agent and were admitted to the institution through the ED. Patients were identified by pharmacy charges for commonly prescribed antimicrobials for the following indications: community-acquired pneumonia, complicated skin and soft tissue infection (SSTI), meningitis, and sepsis, as these are often the most common infections that necessitate inpatient admission, have existing treatment guidelines, and afford the ability to track outcomes. Patients were excluded if they were 18 years of age or older, pregnant, had a prior diagnosis of cystic fibrosis, were discharged from the ED, or were not being treated for one of the predetermined infections previously stated.
The University of Kentucky Chandler Medical Center is a 569-bed university teaching hospital that is designated as a Level I Adult/Pediatric Trauma Center and houses a 65-bed ED with an annual volume of approximately 70,000 patient visits per year. Emergency medicine pharmacists with specialized residency training provide clinical coverage to the ED from 1 pm to 11 pm, 7 days per week. The emergency medicine physicians rotate through day and night shifts and cover both pediatric and adult patient populations. Clinical pharmacists in the ED are responsible for various activities that include providing consultative pharmacotherapy services, implementing evidence-based drug therapy, providing emergency management services, developing necessary protocols, ensuring appropriate and timely first-dose antibiotics by order verification and medication preparation at bedside, providing education to nurses and physicians, and providing medication reconciliation counseling to targeted patient populations. Consultative services are provided on an informal basis and can be initiated through provider or allied health personnel inquisition or through the proactive involvement of the EPh.
The EPhs focus their proactive involvement toward patients presenting to the hospital with any critical illness including status epilepticus, sepsis, stroke, and trauma. The pharmacy orders are processed through a computerized physician order entry system and medications can be procured through the central pharmacy (open 24/7), the pediatric pharmacy satellite (open 7 am–10 pm), or through automated dispensing cabinets located in the ED. There are no antimicrobial stewardship policies that impact availability of any medications being dispensed to ED patients. For many pediatric orders, given that doses are not standardized, medications are prepared in either the central pharmacy or the pediatric pharmacy satellite if the EPh is not present to facilitate preparation and delivery. During the study period there were no available prebuilt order sets to facilitate physician order entry. Control group data were collected for patients who presented during the hours when the EPhs were not present (11 pm–1 pm), and treatment group data were collected for patients who presented during the hours that clinical pharmacy services were present in the ED (1 pm–11 pm).
The primary outcome of this study was to evaluate the incidence of appropriate antimicrobial selection and dosing with and without the presence of an EPh. Appropriateness of antibiotic therapy was established before data collection and was based on the indication and the recommended dose from published guidelines or accepted clinical standards.13–16 For patients who were being treated for one of the predetermined infections, but had unique clinical characteristics that fell outside usual guideline criteria, accepted clinical standards were used in assessing appropriateness (e.g., those with a ventriculoperitoneal shunt or immunocompromised patients). The secondary outcomes included determining if there was a statistical difference between the groups with regard to timeliness of administration, and whether appropriate antimicrobial therapy was associated with differences in intensive care length of stay (LOS), hospital LOS, or return visits to the ED. The patient was identified as having a return visit to the ED only if that visit was related to the infection from the previous admission.
Data collected included patient demographic information, past medical history, chief complaint upon admission, date and time of presentation to the ED, severity of illness determined using the Pediatric Risk of Mortality (PRISM) index,17 and information regarding antimicrobial therapy, including date and time of order and administration of the drug, dose in milligram per kilogram (mg/kg), whether the antimicrobial was appropriate, and whether there was a pharmacist intervention at any point in the medication-use process. A pharmacist was documented as having an intervention if the pharmacist changed the medication order and re-entered an optimized order to reflect the changes, entered an order based on a “Pharmacist to Dose” order placed by a provider, or if there was anything noted in the clinical record of a pharmacist's intervention. Time from order of antibiotic to verification of antibiotic was retrospectively obtained by time-stamps archived on the electronic orders. The time from order to administration of the antibiotic was retrospectively obtained by the time-stamp on the electronic order and the time of documentation from the electronic medication administration record.
The study was designed to have an 80% power to detect a 15% reduction in inappropriate antibiotics during the hours the EPh was available. Sample-size calculations showed that approximately 120 patients total were required to find a statistical significance level of 0.05. Continuous data were assessed by using Wilcoxon rank sum test or Student t test and categorical variables were assessed by using chi-square analysis or Fisher exact test. All statistical analyses were conducted by using SigmaStat 3.5 Software (Systat Software, San Jose, CA).
RESULTS
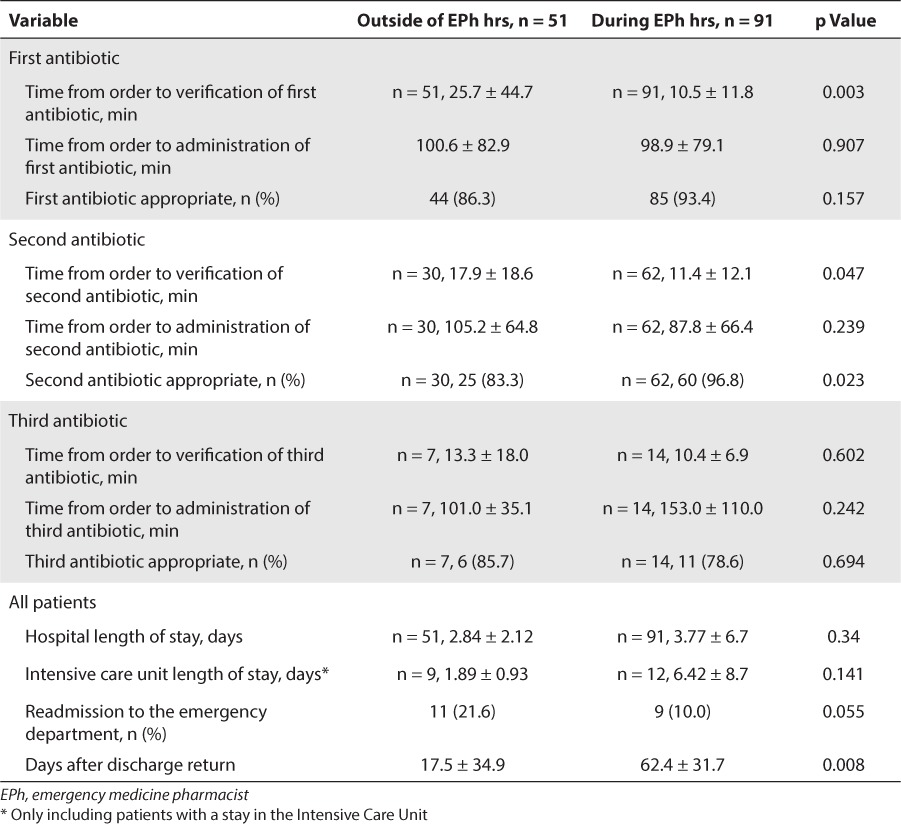
A total of 142 patients were identified as meeting all inclusion criteria and 91 patients were found to have presented during EPh hours, while 51 patients presented outside EPh hours. Demographic data are included in Table 1. There were no statistically significant differences between the study groups with regard to prior past medical history. There was a statistically significant difference in the number of patients presenting with sepsis when comparing the patients admitted outside EPh hours to those admitted during EPh hours (16 [31.4%] patients versus 13 [14.3%] patients; p = 0.015). However, when looking at patients with life-threatening infections (intra-abdominal infection, meningitis, pneumonia, and sepsis), there was no statistically significant difference between the groups (p = 0.083). With regard to the primary outcome, when the EPh was present, patients received an appropriate first antibiotic 93.4% of the time (p = 0.157). Patients received appropriate second and third antimicrobials 96.8% (p = 0.023) and 78.6% (p = 0.694) of the time, respectively (Table 2). During EPh hours, the time from order entry to order verification by a pharmacist was significantly shorter for the first and second antimicrobials (25.7 minutes vs. 10.5 minutes [p = 0.003] and 17.9 minutes vs. 11.4 minutes [p = 0.047], respectively). Patients treated while the EPh was present were also found to have fewer, albeit non-significant, return visits to the ED (11 vs. 9; p = 0.055) and a significantly longer duration of time from discharge to their ED return visit (17.5 days vs. 62.4 days; p = 0.008).
Table 1.
Demographic Data
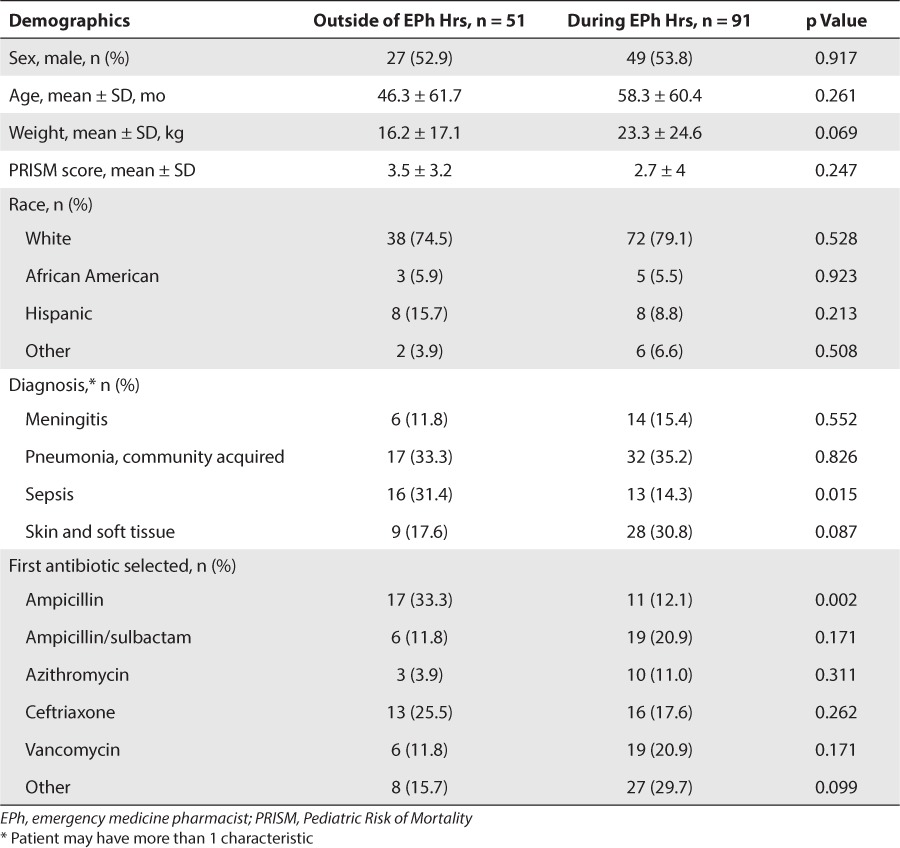
Table 2.
Comparison of Control Group Versus Study Group if Admitted During Pharmacist Hours
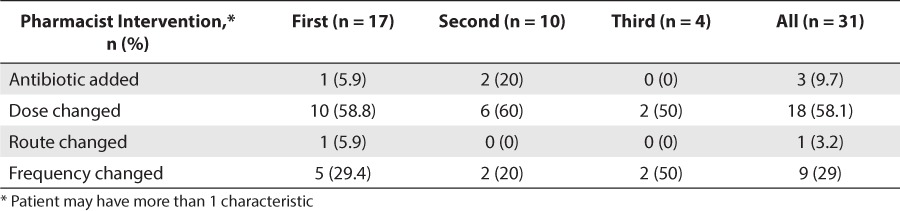
Adjustments to the initial dose (either down or up) ordered by the provider was the most common intervention (58.1%) for those patients who had a pharmacist's intervention (n = 31). This was also the most common prescribing error identified (n = 28, 71%). Other notable interventions by ED pharmacists included changing the frequency of antibiotic dosing based on age and indication (29%) and recommending the addition of another antimicrobial (9.7%) (Table 3).
Table 3.
Type of Pharmacist Intervention
DISCUSSION
In this retrospective review, we found that patients were likely to receive the appropriate dose and selection of antibiotic for their infection and receive it in a timely fashion whenever the EPh was present. Upon comparison of patients treated without the presence of the EPh versus those that were, the appropriateness of the first antibiotic was not found to be statistically significant (86.3% vs. 93.4%, p = 0.157). Although this comparison did not reach statistical significance, there is substantial clinical importance in the fact that such a large proportion of patients was treated appropriately while the EPh was present during the shift. This enhanced level of care has the potential to yield clinical and financial implications for both the patients and the institutions through decreased and less frequent readmissions. Also, several pediatric infections share common antibiotics as appropriate first-line agents. Often, providers become accustomed to selecting a particular agent as the first empiric antibiotic and tailor additional selections on a more narrow differential diagnosis. This increases the likelihood of the provider selecting the appropriate first antibiotic and might explain why the statistical significance was seen with the selection of the second antibiotic.
When specifically evaluating a pediatric ED patient population, it has been shown that when medications are ordered between the hours of midnight and 8 am, there is a stronger association with prescribing errors.18 This may be attributed to several factors including physician workload and fewer attending physicians immediately available at bedside to double-check the resident physician; moreover, patients seen during those hours may be more critically ill, and providers may have varying degrees of prior experience treating pediatric patients with complex disease states. This time frame represents an increased likelihood for errors and is outside the hours when an EPh is normally available at the study institution (1 pm-11 pm). During this study, significant impacts on care were still noted even without EPh presence during that vulnerable period of midnight to 8 am. Thus, expansion of clinical coverage into this period would be theorized to yield even greater reduction in errors and enhancement in care. As prior evaluations have highlighted, medication errors occur more frequently in the intensive care areas including the ED, likely due to intensity and complexity of the clinical scenarios.1,7,9,18 When the additional variable of patient age (i.e., <18 years of age) is added to the clinical picture, it adds an entirely new set of variables to the equation, such as unfamiliarity with the specific medications and their doses or lack of knowledge of appropriate pediatric drug references.18 A clinical pharmacist's presence allows education to be provided to those staff members at the bedside, potentially impacting outcomes such as overall drug costs, drug utilization, and avoidance of potentially harmful medication errors. There also exists a possible substantial medical and economic benefit from the addition of a clinical pharmacist in the ED setting through cost avoidance associated with misdosing, inappropriate drug selection, and readmissions. The financial and economic impacts of the EPh intervention were not variables that were retrospectively reviewed in the present study. Future investigations in this field should include this as a primary outcome parameter. This study is limited by its retrospective nature and its assessment of only the population treated at a single institution. In addition, clinical documentation was limited with regard to whether there were specific patient-level factors that impacted either the dosing of antimicrobials in the prescribing phase or the administration phase of the medication-use process (including medication delivery, limited intravenous access, inability to maximize infusion times). Nevertheless, both groups would be equally susceptible to this variable and therefore this should not have a significant impact on the results.
Hospitalized pediatric patients are at high risk of adverse events associated with medication errors, as they are a unique patient population for which providers are prone to dosing errors or inappropriate drug selection. This study also highlights the fact that the role of clinical pharmacists has expanded beyond dispensing and preparation into their becoming vital members of the health care team with activities such as recommending changes to current drug therapy, optimization of drug dosing, and avoiding medication errors. Clinical pharmacists can facilitate more timely antimicrobial administration, assist in developing electronic order sets to limit medication errors while pharmacists are not available in the ED, and potentially impact patient outcomes including financial outcomes and hospital readmissions. Further investigations are needed to determine the extent of pharmacy interventions in a pediatric ED.
ABBREVIATIONS
- ED
emergency department
- EPhs
emergency medicine pharmacists
- LOS
length of stay
- PRISM
Pediatric Risk of Mortality
- SSTI
skin and soft tissue infection
Footnotes
Disclosure The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Leape LL, Cullen DJ, Clapp MD et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):267–270. doi: 10.1001/jama.282.3.267. [DOI] [PubMed] [Google Scholar]
- 2.Defrates SR, Weant KA, Seamon JP et al. Emergency pharmacist impact on health care-associated pneumonia empiric therapy. J Pharm Pract. 2012;26(2):125–130. doi: 10.1177/0897190012451933. [DOI] [PubMed] [Google Scholar]
- 3.Kumar A, Roberts D, Wood KE et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 4.Houck PM, Bratzler DW, Nsa W et al. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. 2004;164(6):637–644. doi: 10.1001/archinte.164.6.637. [DOI] [PubMed] [Google Scholar]
- 5.Gaieski DF, Mikkelsen ME, Band RA et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 6.Kalina M, Tinkoff G, Gleason W et al. A multidisciplinary approach to adverse drug events in pediatric trauma patients in an adult trauma center. Pediatr Emerg Care. 2009;25(7):444–446. doi: 10.1097/PEC.0b013e3181ab7846. [DOI] [PubMed] [Google Scholar]
- 7.Patanwala AE, Sanders AB, Thomas MC et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5):369–373. doi: 10.1016/j.annemergmed.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 8.Blum KV, Abel SR, Urbanski CJ, Pierce JM. Medication error prevention by pharmacists. Am J Hosp Pharm. 1988;45(9):1902–1903. [PubMed] [Google Scholar]
- 9.Kaushal R, Bates DW, Landrigan C et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 10.Moffett BS, Mott AR, Nelson DP, Gurwitch KD. Medication dosing and renal insufficiency in a pediatric cardiac intensive care unit: impact of pharmacist consultation. Pediatr Cardiol. 2008;29(4):744–748. doi: 10.1007/s00246-007-9170-3. [DOI] [PubMed] [Google Scholar]
- 11.Krupicka MI, Bratton SL, Sonnethal K, Goldstein B. Impact of a pediatric clinical pharmacist in the pediatric intensive care unit. Crit Care Med. 2002;30(4):919–921. doi: 10.1097/00003246-200204000-00035. [DOI] [PubMed] [Google Scholar]
- 12.Wang JK, Herzog NS, Kaushal R et al. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007;119(1):e77–e85. doi: 10.1542/peds.2006-0034. [DOI] [PubMed] [Google Scholar]
- 13.Stevens DL, Bisno AL, Chambers HF et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clinl Infect Dis. 2005;41(10):1373–1406. doi: 10.1086/497143. [DOI] [PubMed] [Google Scholar]
- 14.Tunkel AR, Hartman BJ, Kaplan SL et al. Practice guidelines for the management of bacterial meningitis. Clinl Infect Dis. 2004;39(9):1267–1284. doi: 10.1086/425368. [DOI] [PubMed] [Google Scholar]
- 15.Tunkel AR, Glaser CA, Bloch KC et al. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;47(3):303–327. doi: 10.1086/589747. [DOI] [PubMed] [Google Scholar]
- 16.Bradley JS, Byington CL, Shah SS et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med. 1988;16(11):1110–1116. doi: 10.1097/00003246-198811000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Kozer E, Scolnik D, Macpherson A et al. Variables associated with medication errors in pediatric emergency medicine. Pediatrics. 2002;110(4):737–742. doi: 10.1542/peds.110.4.737. [DOI] [PubMed] [Google Scholar]


