Abstract
Background
The purpose of this study was to estimate the incidence and prevalence of hearing loss for noise-exposed U.S. workers by industry sector and 5-year time period, covering 30 years.
Methods
Audiograms for 1.8 million workers from 1981–2010 were examined. Incidence and prevalence were estimated by industry sector and time period. The adjusted risk of incident hearing loss within each time period and industry sector as compared with a reference time period was also estimated.
Results
The adjusted risk for incident hearing loss decreased over time when all industry sectors were combined. However, the risk remained high for workers in Healthcare and Social Assistance, and the prevalence was consistently high for Mining and Construction workers.
Conclusions
While progress has been made in reducing the risk of incident hearing loss within most industry sectors, additional efforts are needed within Mining, Construction and Healthcare and Social Assistance.
Keywords: occupational hearing loss, material hearing impairment, hazardous noise, noise-induced hearing loss, surveillance, trends, prevalence, incidence
INTRODUCTION
Occupational hearing loss (OHL) is the most common work-related illness in the United States [NIOSH, 2013a]. It most often results from chronic exposure to hazardous noise (≥85 dBA) but can be caused by a single instantaneous high noise exposure or exposure to ototoxic chemicals [Nelson et al., 2005]. Approximately 22 million U.S. workers are exposed to hazardous noise at work [Tak et al., 2009]. Noise regulations exist in most industries to prevent or ameliorate hazardous occupational noise. However, noise exposure limits and mandated prevention efforts vary by industry [NIOSH, 1998]. Some industries, such as agriculture, have no noise regulation at all [Suter, 2003]. Hearing loss is permanent, potentially debilitating, and affects workers both at home and on the job [Hetu et al., 1995; Morata et al., 2005; Seidman and Standring, 2010]. However, OHL resulting from noise and ototoxic chemical exposures is entirely preventable [Themann et al., 2013a,b].
The level of hearing loss deemed acceptable in establishing U.S. noise regulations is based on preserving hearing for conversational speech, defined by the National Institute for Occupational Safety and Health (NIOSH) as an average hearing level of 25 dBor less (better) at the frequencies 1,000, 2,000, 3,000, and 4,000 Hertz (Hz). When hearing ability exceeds the 25 dB average, a worker is said to have developed a “material hearing impairment.” No known studies have examined whether current regulations are effectively preventing material hearing impairment among U.S. workers and few studies have examined trends in worker hearing loss.
Daniell et al. [2002] reported that workers’ compensation claims for hearing loss doubled between 1984 and 1991 and multiplied by twelve by 1998 in Washington State. They postulated that the large increase was likely due to reporting phenomena. McCall and Horwitz [2004] reported that workers’ compensation claims decreased in Oregon between 1984 and 1998 following improvements in state occupational safety and health standards.
Tak and Calvert [2008] examined the overall trend in the prevalence of self-reported hearing difficulty among workers during 1997–2003 and found that the prevalence slowly decreased until 2000, but then fluctuated thereafter. Bureau of Labor Statistics (BLS) data has indicated a gradual reduction in the incidence of Occupational Safety and Health Administration (OSHA) standard threshold shifts in hearing during 2004–2007 [Hager, 2006, 2007, 2008, 2009]. However, BLS estimates must be interpreted with caution, in part since certain types of employers are not represented [Leigh and Miller, 1998], and economic incentives may encourage under-reporting [Leigh and Miller, 1998; Azaroff et al., 2002].
NIOSH established the OHL Surveillance Project in 2009 to address the lack of a national surveillance program for OHL. Through partnerships with audiometric testing service providers and others, hereafter referred to as providers, NIOSH collects de-identified worker audiograms originally completed for regulatory compliance purposes, including historical audiograms.
The purpose of this study was to estimate the incidence and prevalence of material hearing impairment, hereafter referred to as hearing loss, for noise-exposed U.S. workers by industry sector and time period using NIOSH OHL Surveillance Project data. The risk of incident hearing loss as compared with a reference time period was also estimated. No previous studies have examined 30 years of hearing loss prevalence, incidence and risk by industry sector.
MATERIALS AND METHODS
Study Design and Population
This longitudinal study of a retrospective cohort estimated and compared the prevalence and incidence of U.S. worker hearing loss by industry sector and time period. Worker audiograms and related information from the NIOSH OHL Surveillance Project were used and are described in detail by Masterson et al. [2013]. In short, de-identified audiometric tests previously conducted by providers predominantly for workers exposed to high noise (≥85 dBA) were shared with NIOSH and assigned arbitrary employee IDs. Male and female workers ages 18 to 75 years during the years 1981–2010 and meeting study quality standards (defined below under Audiogram Inclusion and Exclusion Criteria) were included. We chose this time period because there were insufficient numbers of audiograms prior to 1981 and 2010 was the latest year of data available. The data were analyzed in 5-year blocks to increase sample size in industry sectors and power to detect trends:
1981–1985 (Period 1)
1986–1990 (Period 2)
1991–1995 (Period 3)
1996–2000 (Period 4)
2001–2005 (Period 5)
2006–2010 (Period 6)
It was necessary for the estimation of incidence to establish that each worker was free of hearing loss before he/she could become an incident case. Incidence was therefore counted beginning in Period 2. After case determination, only the last audiogram for each worker in each time period was retained for the analyses, and was used to determine worker age. Since all audiograms were de-identified, this project was determined by the NIOSH Institutional Review Board to be research not involving human subjects.
Beginning with 8,597,503 U.S. audiograms for 2,198,124 workers ages 18–75 during 1981–2010, 2,338,034 audiograms (27%) were eliminated from the analysis due to the quality deficiencies identified in Table I (additional description in the Audiogram Inclusion and Exclusion Criteria section). Next, we retained only the last audiogram for each worker in each time period (3,314,799 audiograms eliminated, no workers eliminated). Our final study sample contained 2,944,670 audiograms for 1,816,812 workers at 33,572 companies, and was used for the prevalence analyses. A subset of the sample, 560,320 workers with at least two valid audiograms, was used for the incidence analyses, detailed under Statistical Analyses.
TABLE I.
Audiograms Excluded From Analysis
| Reason for Exclusion | Number with characteristic | Total excluded in groupinga |
|---|---|---|
| Missing value for industry sector | 291,378 | |
| Missing value for dependent variableb | 15,418 | |
| Unlikely threshold values for left ear | 7,834 | |
| Unlikely threshold values for right ear | 7,982 | |
| Large inter-aural difference | 869,302 | |
| Negative slope | 1,446,658 | 2,338,034 |
| Not the most recent valid audiogram in each time period | 3,314,799 | |
| All exclusions | 5,652,833 |
Some audiograms were eliminated for more than one reason within groupings.
Includes eliminations of affected ear results due to “no response at maximum value” threshold values.
Materials
The results of worker audiograms were used to identify hearing loss. Audiometric records included date of birth, gender, threshold values at frequencies 500, 1,000, 2,000, 3,000, 4,000, 6,000, and 8,000 Hz, and North American Industry Classification System (NAICS) codes [U.S. Department of Commerce, The Kraus Organization Limited, 2007; U.S. Census Bureau, 2011]. NAICS codes range from two-digit to six-digit numbers and industry specificity increases with each digit. Date of hire and occupation were not available for most cases. Education, race, income, smoking status, noise and ototoxic chemical exposure information were also not available.
Audiogram Inclusion and Exclusion Criteria
Study audiograms were originally collected for non-research purposes and could contain incomplete or inaccurate information [Laurikkala et al., 2000]. The entire audiogram was excluded if the gender, year of birth, NAICS code or geographical region was missing and this information could not be imputed from another audiogram for the same worker. Missing birth months and days were imputed as July and 15, respectively, and July 1 was imputed if both fields were missing. By restricting the age range to 18–75, audiograms with unlikely birth years were excluded. Audiometric results for ears with missing thresholds at frequencies necessary for calculations of hearing loss or evaluations of quality were excluded.
Utilizing methods developed by senior NIOSH audiologists, we excluded audiograms that did not meet additional quality standards or displayed attributes indicating that hearing loss may be due to pathology or non-occupational factors. These methods and their rationale are described in detail in Masterson et al. [2013]. Briefly, we removed audiograms with threshold values depicting negative slope in either ear, indicating that background noise may have been excessive during testing, or the presence of middle ear pathology [Suter, 2002]. We also eliminated audiograms for ears with unlikely threshold values suggesting the presence of testing errors, and excluded the affected ear for audiograms with threshold values of “no response at maximum value”. If large inter-aural differences were identified such that a threshold at a given frequency in one ear differed by 40 dB or more from a threshold at the same frequency in the other ear, then the entire audiogram was excluded. Differences of this magnitude are rarely due primarily to occupational noise exposure [Arslan and Orzan, 1998], and without proper masking, inaccurate thresholds may be recorded for the poorer ear [Martin, 2009].
Statistical Analysis
The independent variables were time period and industry sector. Industry sectors were the NIOSH Occupational Research Agenda industry sectors [NIOSH, 2013b] with two modifications due to small group sizes: (i) Public Safety was combined with Services, and (ii) Oil and Gas Extraction was combined with Mining. The worker’s industry sector was based on the assigned NAICS code. The outcome was hearing loss, using the NIOSH definition of material hearing impairment: A pure-tone average threshold across frequencies 1,000, 2,000, 3,000 and 4,000 Hz of 25 dB or more in either ear [NIOSH, 1998]. After determining incident cases (discussed below), audiograms for years 1981–1985 (Period 1) were combined and the last audiogram for each worker was retained. This process was repeated for the other time periods to ensure each worker was only counted once during each time period. A worker could have audiograms in more than one time period.
Audiograms from Period 1 were used to determine which cases of hearing loss in Period 2 were incident. Workers with hearing loss in Period 1 were not included in Period 2 or later periods. Workers with hearing loss in Period 2 were not included in Period 3 or later periods, and this process was repeated for the other time periods. A worker counted as an incident case had to have a prior audiogram without hearing loss. A worker counted as a non-case also needed a prior audiogram without hearing loss to ensure all workers had an equal chance of being an incident case. We also ensured that there were no incident cases who lost their hearing within their first time period, for example, a worker’s first audiograms appeared in Period 4 and did not have hearing loss in 1997, but developed a hearing loss by 1999.
Six descriptive categories were used for worker age. States of worker employment were condensed into six geographical regions based on the U.S. Embassy region groupings [U.S. Embassy, 2008]. Providers were assigned arbitrary numbers. SAS version 9.3 statistical software was utilized for analyses (SAS Institute Inc., Cary, NC).
Prevalence and incidence percentages were estimated for each industry sector and time period. Probability ratios (PRs) for incident hearing loss were estimated using the SAS® genmod procedure for log-binomial regression [Spiegelman and Hertzmark, 2005]. PRs were calculated since some estimates were expected to exceed 10% and odds ratios should only be utilized for rare outcomes [Deddens and Petersen, 2008], and for ease of interpretation. The Repeated Statement was used to account for multiple observations for one worker. The log-binomial regression models did not converge and the copy method was used to estimate PRs [Deddens and Petersen, 2008].
The PRs, which identify the risk of becoming an incident case in each time period as compared with the reference time period, were adjusted for gender, age group, region and provider. When all industry sectors were combined, the PRs were also adjusted for industry sector. Confidence intervals were also calculated. The Quasi-Akaike Information Criterion (QIC) statistics were reviewed to determine if there was a significant interaction among the patterns of hearing loss for the industry sectors over time.
Period 2 was designated as the PR reference time period for all industry sectors except Mining, Quarrying, and Oil and Gas Extraction (hereafter referred to as Mining) and Healthcare and Social Assistance, due to insufficient sample size in Period 2. Periods 5 and 4 were used as reference time periods for these industry sectors, respectively. A PR >1 indicated that the risk was higher in the current time period than in the reference time period. A PR <1 indicated that the risk in the current time period was less than in the reference time period.
Results
Sample demographics by time period are provided in Table II. Within all time periods, most workers were males (77–82%) and the largest percentage were employed in the U.S. Midwest (39–49%). Over time, the percentages of female workers and older workers increased. Although the number of audiograms available in our sample increased dramatically over time, the proportions for industry sectors remained fairly constant. The manufacturing sector accounted for the majority of the audiograms (68–76%).
TABLE II.
Sample Demographics for 1,816,812 Workers, by Time Period, 1981–2010
| Period 1 1981–1985 |
Period 2 1986–1990 |
Period 3 1991–1995 |
Period 4 1996–2000 |
Period 5 2001–2005 |
Period 6 2006–2010 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographic | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Period total | 60,736 | 151,616 | 312,851 | 551,716 | 873,332 | 994,419 | ||||||
| Gender | ||||||||||||
| Male | 49,862 | 82.47 | 119,278 | 79.10 | 244,036 | 78.30 | 422,389 | 76.75 | 672,174 | 77.15 | 770,498 | 77.67 |
| Female | 10,601 | 17.53 | 31,514 | 20.90 | 67,640 | 21.70 | 127,937 | 23.25 | 199,033 | 22.85 | 221,497 | 22.33 |
| Missing | 273 | 824 | 1,175 | 1,390 | 2,125 | 2,424 | ||||||
| Age group (Years) | ||||||||||||
| 18–25 | 10,400 | 17.12 | 24,032 | 15.85 | 50,502 | 16.14 | 92,036 | 16.68 | 129,707 | 14.85 | 146,090 | 14.69 |
| 26–35 | 26,666 | 43.90 | 54,743 | 36.11 | 96,525 | 30.85 | 152,559 | 27.65 | 216,406 | 24.78 | 229,032 | 23.03 |
| 36–45 | 16,515 | 27.19 | 46,197 | 30.47 | 96,546 | 30.86 | 162,412 | 29.44 | 242,610 | 27.78 | 253,044 | 25.45 |
| 46–55 | 5,967 | 9.82 | 20,321 | 13.40 | 51,482 | 16.46 | 107,959 | 19.57 | 201,514 | 23.07 | 244,309 | 24.57 |
| 56–65 | 1,150 | 1.89 | 6,056 | 3.99 | 16,858 | 5.39 | 34,813 | 6.31 | 78,016 | 8.93 | 113,483 | 11.41 |
| 66–75 | 38 | 0.06 | 267 | 0.18 | 938 | 0.30 | 1,937 | 0.35 | 5,079 | 0.58 | 8,461 | 0.85 |
| Missing | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Geographical region | ||||||||||||
| Mid-Atlantica | 9,684 | 15.98 | 25,160 | 16.66 | 52,327 | 16.82 | 101,933 | 18.59 | 137,734 | 16.04 | 142,251 | 14.64 |
| Midwestb | 27,517 | 45.42 | 60,556 | 40.11 | 120,808 | 38.83 | 214,011 | 39.03 | 401,214 | 46.71 | 471,161 | 48.50 |
| New Englandc | 311 | 0.51 | 479 | 0.32 | 1,670 | 0.54 | 2,693 | 0.49 | 3,779 | 0.44 | 4,358 | 0.45 |
| Southd | 12,255 | 20.23 | 32,176 | 21.31 | 62,209 | 20.00 | 101,103 | 18.44 | 164,656 | 19.17 | 205,601 | 21.16 |
| Southweste | 1,167 | 1.93 | 2,887 | 1.91 | 5,780 | 1.86 | 14,273 | 2.60 | 18,856 | 2.20 | 16,146 | 1.66 |
| Westf | 9,656 | 15.94 | 29,720 | 19.68 | 68,300 | 21.95 | 114,361 | 20.85 | 132,714 | 15.45 | 132,049 | 13.59 |
| Missing | 146 | 638 | 1,757 | 3,342 | 14,379 | 22,853 | ||||||
| Industry sector (NAICS 2007 Code) | ||||||||||||
| Agriculture, Forestry, Fishing, and Hunting (11) | 1,403 | 2.31 | 2,439 | 1.61 | 3,888 | 1.24 | 10,952 | 1.99 | 10,035 | 1.15 | 10,655 | 1.07 |
| Mining, Quarrying, and Oil and Gas Extraction (21) | 10 | 0.02 | 18 | 0.01 | 337 | 0.11 | 1,307 | 0.24 | 2,606 | 0.30 | 3,240 | 0.33 |
| Construction (23) | 1,051 | 1.73 | 2,518 | 1.66 | 5,903 | 1.89 | 11,143 | 2.02 | 19,519 | 2.24 | 24,116 | 2.43 |
| Manufacturing (31–33) | 46,416 | 76.42 | 112,259 | 74.04 | 227,301 | 72.65 | 390,518 | 70.78 | 599,874 | 68.69 | 675,483 | 67.93 |
| Wholesale and Retail Trade (42, 44–45) | 3,656 | 6.02 | 8,726 | 5.76 | 16,571 | 5.30 | 30,529 | 5.53 | 61,606 | 7.05 | 74,702 | 7.51 |
| Transportation, Warehousing, and Utilities (48, 49, 22) | 3,483 | 5.73 | 13,390 | 8.83 | 33,235 | 10.62 | 58,955 | 10.69 | 95,560 | 10.94 | 111,105 | 11.17 |
| Healthcare and Social Assistance (62) | 59 | 0.10 | 472 | 0.31 | 957 | 0.31 | 1,790 | 0.32 | 5,901 | 0.68 | 5,662 | 0.57 |
| Services (51–56, 61, 71–72, 81, 92) | 4,658 | 7.67 | 11,794 | 7.78 | 24659 | 7.88 | 46,522 | 8.43 | 78,231 | 8.96 | 89,456 | 9.00 |
| Missing | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
Mid-Atlantic: Delaware, Maryland, New Jersey, New York, Pennsylvania, Washington, D.C.
Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin.
New England: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont.
South: Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, West Virginia.
Southwest: Arizona, New Mexico, Oklahoma, Texas.
West: Alaska, California, Colorado, Hawaii, Idaho, Montana, Nevada, Oregon, Utah, Washington, Wyoming.
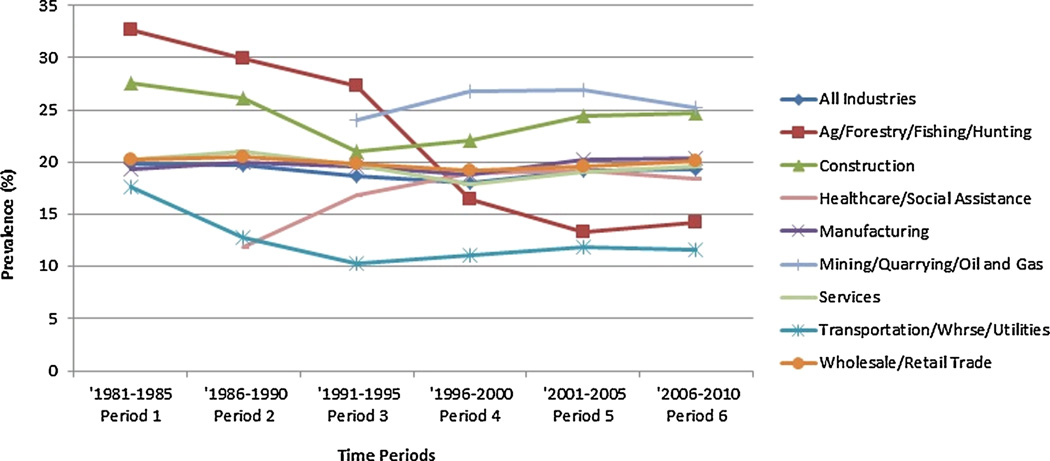
Table III includes the estimated prevalence of workers with hearing loss by industry sector over time. The overall prevalence of hearing loss for all industry sectors combined remained very consistent over time, with 20% in Period 1 and 19% in Period 6. The prevalence also remained consistent within most industry sectors over time, with the exception of (i) Agriculture, Forestry, Fishing and Hunting, which decreased from 33% to 14%; (ii) Transportation, Warehousing and Utilities, which decreased from 18% to 12%; and (iii) Healthcare and Social Assistance, which increased from 12% to 18%. The prevalence within the Mining sector stayed consistent and high (24–27% in Periods 3–6). The prevalence of hearing loss was also high in the Construction sector; above 24% in four of the six time periods. Figure 1 depicts these prevalence estimates in line graph format.
TABLE III.
Estimated Prevalence of Hearing Loss by Time Period and Industry Sector, 1981–2010, for 1,816,812 Workers
| Period 1 1981–1985 |
Period 2 1986–1990 |
Period 3 1991–1995 |
Period 4 1996–2000 |
Period 5 2001–2005 |
Period 6 2006–2010 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Industry Sector (NAICS 2007 Code) | (%) | 95% CIa | (%) | 95% CI | (%) | 95% CI | (%) | 95% CI | (%) | 95% CI | (%) | 95% CI |
| All industries | 19.80 | 19.48–20.12 | 19.66 | 19.46–19.86 | 18.71 | 18.57–18.85 | 17.96 | 17.86–18.06 | 19.15 | 19.07–19.23 | 19.37 | 19.29–19.45 |
| Agriculture, Forestry, Fishing, and Hunting (11) | 32.64 | 30.19–35.09 | 29.89 | 28.07–31.71 | 27.34 | 25.94–28.74 | 16.44 | 15.75–17.13 | 13.25 | 12.59–13.91 | 14.18 | 13.52–14.84 |
| Mining, Quarrying, and Oil and Gas Extraction (21) | ISSb | ISS | 24.04 | 19.48–28.60 | 26.78 | 24.38–29.18 | 26.98 | 25.28–28.68 | 25.22 | 23.73–26.72 | ||
| Construction (23) | 27.59 | 24.89–30.29 | 26.17 | 24.45–27.89 | 21.07 | 20.03–22.11 | 22.07 | 21.30–22.84 | 24.46 | 23.86–25.06 | 24.67 | 24.13–25.21 |
| Manufacturing (31–33) | 19.34 | 18.98–19.70 | 19.93 | 19.70–20.16 | 19.55 | 19.39–19.71 | 18.79 | 18.67–18.91 | 20.18 | 20.08–20.28 | 20.40 | 20.30–20.50 |
| Wholesale and Retail Trade (42, 44–45) | 20.21 | 18.91–21.51 | 20.56 | 19.71–21.41 | 19.88 | 19.27–20.49 | 19.20 | 18.76–19.64 | 19.65 | 19.34–19.96 | 20.06 | 19.77–20.35 |
| Transportation, Warehousing, and Utilities (48, 49, 22) | 17.63 | 16.36–18.90 | 12.79 | 12.22–13.36 | 10.25 | 9.92–10.58 | 11.13 | 10.88–11.38 | 11.83 | 11.63–12.04 | 11.65 | 11.46–11.84 |
| Healthcare and Social Assistance (62) | ISS | 11.86 | 8.94–14.78 | 16.82 | 14.45–19.19 | 18.94 | 17.13–20.76 | 19.13 | 18.13–20.13 | 18.47 | 17.46–19.48 | |
| Services (51–56, 61, 71–72, 81, 92) | 20.24 | 19.09–21.39 | 21.02 | 20.29–21.76 | 19.66 | 19.16–20.16 | 17.91 | 17.56–18.26 | 19.03 | 18.76–19.31 | 19.60 | 19.34–19.86 |
CI = 95% confidence interval.
ISS = insufficient sample size.
FIGURE 1.
Prevalence of hearing loss by time period and industry sector, 1981–2010, for 1,816,812 workers.
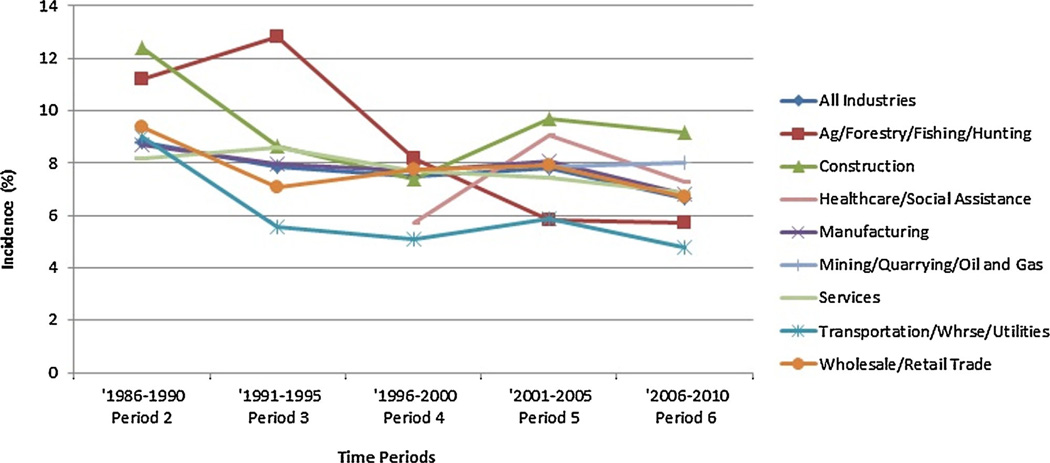
Hearing loss incidence estimates are provided in Table IV, and depicted graphically in Figure 2. The overall incidence of hearing loss for workers in all industry sectors slowly decreased over time, from 9% in Period 2 to 7% in Period 6, and this trend was observed within most industry sectors. Most values hovered around 7–9%. The incidence in several sectors increased in Period 5, dramatically so within Construction and Healthcare and Social Assistance, followed by a reduction. After an increase in Period 3, there was a dramatic drop in incidence within the Agriculture, Forestry, Fishing and Hunting sector. The Construction (9%) and Mining (8%) industry sectors had the highest incidences in Period 6, while Transportation, Warehousing and Utilities had the lowest (5%).
TABLE IV.
Estimated Incidence of Hearing Loss by Time Period and Industry Sector, 1986–2010, for 560,320 Workers
| Period 2 1986–1990 |
Period 3 1991–1995 |
Period 4 1996–2000 |
Period 5 2001–2005 |
Period 6 2006–2010 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Industry Sector (NAICS 2007 Code) | (%) | 95%CIa | (%) | 95%CI | (%) | 95%CI | (%) | 95%CI | (%) | 95%CI |
| All industries | 8.82 | 8.53–9.11 | 7.86 | 7.69–8.03 | 7.47 | 7.35–7.60 | 7.80 | 7.69–7.91 | 6.64 | 6.56–6.72 |
| Agriculture, Forestry, Fishing, and Hunting (11) | 11.20 | 8.98–13.42 | 12.81 | 11.04–14.58 | 8.17 | 6.90–9.44 | 5.84 | 4.84–6.84 | 5.73 | 4.89–6.57 |
| Mining, Quarrying, and Oil and Gas Extraction (21) | ISSb | ISS | ISS | 7.88 | 5.41–10.35 | 8.02 | 6.41–9.63 | |||
| Construction (23) | 12.38 | 9.76–15.00 | 8.62 | 7.21–10.03 | 7.38 | 6.38–8.39 | 9.70 | 8.85–10.56 | 9.17 | 8.50–9.84 |
| Manufacturing (31–33) | 8.69 | 8.37–9.01 | 7.98 | 7.78–8.18 | 7.70 | 7.55–7.85 | 8.06 | 7.93–8.19 | 6.83 | 6.73–6.93 |
| Wholesale and Retail Trade (42, 44–45) | 9.35 | 8.17–10.53 | 7.07 | 6.37–7.77 | 7.75 | 7.20–8.31 | 7.91 | 7.46–8.36 | 6.73 | 6.42–7.04 |
| Transportation, Warehousing, and Utilities (48, 49, 22) | 8.99 | 7.84–10.14 | 5.58 | 5.05–6.11 | 5.09 | 4.75–5.43 | 5.86 | 5.56–6.16 | 4.77 | 4.56–4.98 |
| Healthcare and Social Assistance (62) | ISS | ISS | 5.73 | 3.51–7.96 | 9.05 | 6.93–11.17 | 7.26 | 5.88–8.65 | ||
| Services (51–56, 61, 71–72, 81, 92) | 8.18 | 7.06–9.30 | 8.58 | 7.94–9.22 | 7.70 | 7.24–8.16 | 7.45 | 7.09–7.81 | 6.85 | 6.58–7.13 |
CI = 95% confidence interval
ISS = insufficient sample size
FIGURE 2.
Incidence of hearing loss by time period and industry sector, 1986–2010, for 560,320 workers.
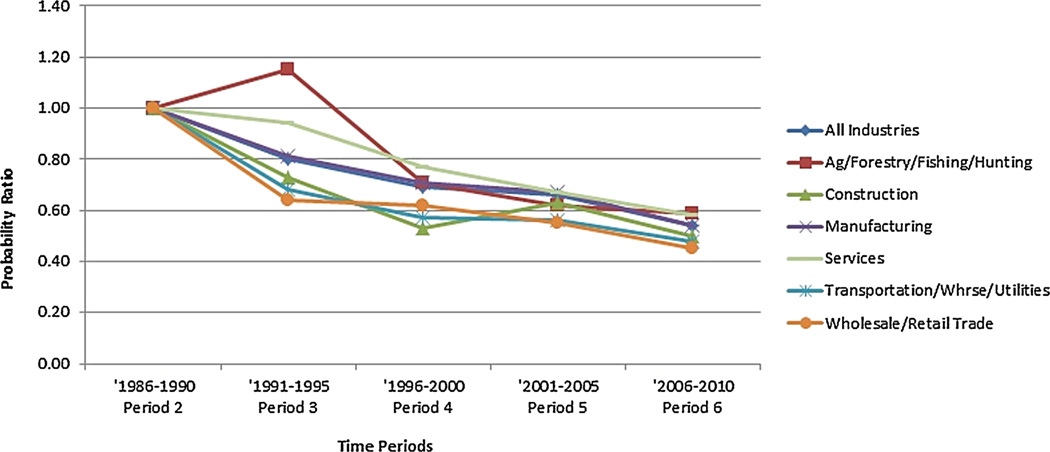
Table V includes adjusted risk estimates for incident hearing loss as compared with a reference time period. These risk estimates are depicted graphically in Figure 3, with the exception of the Mining and Healthcare and Social Assistance sectors, which have different reference groups. The risk of hearing loss for all industry sectors combined consistently decreased over time, from PR = 0.80 (CI = 0.77–0.83) in Period 3 to PR = 0.54 (CI = 0.52–0.55) in Period 6, which was significantly lower than the risk of incident hearing loss in the reference time period. Risks generally decreased over time within industry sectors. However, there was a statistically significant interaction between industry sector and time period (P < 0.05), indicating different patterns of hearing loss risk among the sectors.
TABLE V.
Adjusted Probability Ratios (PRs) for Hearing Loss Incidence, Comparing Time Periods during 1991–2010 with a Reference Time Period, by Industry Sector, for 560,320 Workers
| Period 2 1986–1990 |
Period 3 1991–1995 |
Period 4 1996–2000 |
Period 5 2001–2005 |
Period 6 2006–2010 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Industry Sector (NAICS 2007 Code) | PRa,b | 95%CIc | PR | 95%CI | PR | 95%CI | PR | 95%CI | PR | 95%CI |
| All Industries | 1.00 | 0.80 | 0.77–0.83 | 0.69 | 0.67–0.72 | 0.66 | 0.63–0.68 | 0.54 | 0.52–0.55 | |
| Agriculture, Forestry, Fishing, and Hunting (11) | 1.00 | 1.15 | 0.91–1.45 | 0.71 | 0.56–0.91 | 0.62 | 0.46–0.83 | 0.59 | 0.45–0.77 | |
| Mining, Quarrying, and Oil and Gas Extraction (21) | ISSd | ISS | ISS | 1.00 | 0.93 | 0.64–1.35 | ||||
| Construction (23) | 1.00 | 0.73 | 0.56–0.95 | 0.53 | 0.41–0.68 | 0.63 | 0.50–0.79 | 0.50 | 0.40–0.63 | |
| Manufacturing (31–33) | 1.00 | 0.81 | 0.76–0.84 | 0.71 | 0.68–0.74 | 0.67 | 0.65–0.70 | 0.54 | 0.52–0.56 | |
| Wholesale and Retail Trade (42, 44–45) | 1.00 | 0.64 | 0.54–0.74 | 0.62 | 0.54–0.71 | 0.55 | 0.48–0.63 | 0.45 | 0.40–0.52 | |
| Transportation, Warehousing, and Utilities (48, 49, 22) | 1.00 | 0.68 | 0.58–0.79 | 0.57 | 0.50–0.66 | 0.56 | 0.49–0.65 | 0.48 | 0.42–0.55 | |
| Healthcare and Social Assistance (62) | ISS | ISS | 1.00 | 1.24 | 0.80–1.92 | 0.91 | 0.59–1.39 | |||
| Services (51–56, 61, 71–72, 81, 92) | 1.00 | 0.94 | 0.81–1.10 | 0.77 | 0.67–0.89 | 0.67 | 0.58–0.77 | 0.58 | 0.51–0.67 | |
All PRs were adjusted for gender, age group, provider and region, and PRs for all industries were also adjusted for industry sector.
Reference time periods are indicated by PR = 1.00.
CI = 95% confidence interval.
ISS = insufficient sample size.
FIGURE 3.
Risk of incident hearing loss compared to the 1986–1990 time period, by industry sector, for 560,320 workers.
Nearly all of the industry sectors had PRs in Period 6 that were significantly lower than the reference time period. However, the Healthcare and Social Assistance sector had a risk increase in Period 5 and slight decrease in Period 6; neither risk estimate significantly different than the risk in the reference period (Period 4). While the risks in this sector appeared to be higher than the other sectors, we had used a later reference time period. In a subsequent analysis in which Period 4 was designated as the reference group for all industry sectors, the risks for workers in Healthcare and Social Assistance were still higher than the other sectors, with the exception of Construction (data not shown). The risk of incident hearing loss in the Mining sector in Period 6 was not significantly lower than the reference time period (Period 5). Lastly, after an increase in Period 3, there was a dramatic drop in the risk within the Agriculture, Forestry, Fishing and Hunting industry sector.
Discussion
Our study results indicated that overall, the prevalence of hearing loss remained fairly constant at 20% over the last 30 years. However, the incidence and adjusted risk of incident hearing loss steadily decreased, albeit slowly, for most industry sectors.
Transportation, Warehousing and Utilities had a lower prevalence of hearing loss than any other industry sector, and a low incidence and risk. This seemed counter-intuitive since some transportation workers, such as railroad workers, have been found to have a very high prevalence and risk of hearing difficulty [Tak and Calvert, 2008]. This sector groups NAICS codes 22, 48, and 49, which include workers with likely vastly different levels of noise exposure. In our sample, 65% of the workers in this sector were from the Couriers and Messengers industry (NAICS 492). The prevalence in this industry is among the lowest in the NIOSH data repository (8%) and we have used it as a reference industry in other analyses [Masterson et al., 2013]. The predominance of presumed low-exposed workers likely reduced the overall prevalence. There was also a 16% increase in the proportion of women working in this sector, and fewer women experience hearing loss than men [Palmer et al., 2001], likely due to a variety of reasons including differences in exposures [Themann et al., 2013a].
It is unclear why the Agriculture, Forestry, Fishing and Hunting sector had such a sharp drop in the prevalence and incidence of hearing loss. This sector has unique challenges in preventing OHL, which include a lack of noise regulation for agricultural workers and numerous barriers to regular audiometric testing. Recent papers indicate a moderate prevalence of hearing loss in this sector overall (15–16%), but also fairly high adjusted risks [Tak and Calvert, 2008; Masterson et al., 2013]. There was a 21% increase in the proportion of women in this sector from Periods 1 to 6, the largest increase of any sector. More research is needed in this sector.
The Mining and Construction sectors had the highest prevalence and incidence of hearing loss. These findings are consistent with the results of other studies [Tak and Calvert, 2008; Engdahl and Tambs, 2010; Masterson et al., 2013]. The Mining sector has proportionally more noise-exposed workers than any other U.S. industry [Tak et al., 2009], and the Construction sector has less stringent hearing conservation requirements than most industries. The mobile, seasonal nature of construction work and large proportion of independent contractors also contributes to the difficulty in implementing hearing conservation practices.
Healthcare and Social Assistance had the third highest incidence and one of the highest risks. This sector is not usually associated with a higher risk of hearing loss, and the prevalence has been estimated to be 9–10% overall [Tak and Calvert, 2008; Masterson et al., 2013]. However, other research [Masterson, 2012] has suggested that this sector has a higher prevalence of shifts in hearing. Shifts in hearing can be early indicators of hearing loss and are a measure of the effectiveness of hearing conservation programs [NIOSH, 1998]. Only a small proportion of this sector is exposed to hazardous noise (~3.5%) and it has been found that the self-reported use of hearing protection among noise-exposed workers is directly related to the prevalence of noise exposure in that industry [Tak et al., 2009]. Tak et al. [2009] observed that 74% of the noise-exposed workers in Healthcare and Social Assistance reported not wearing hearing protection. A culture of hearing loss prevention may be less likely to develop within industries with small numbers of noise-exposed workers due to a lack of awareness, experience or resources. Increased interventions in these industries may be warranted.
The risk assessment reported in the NIOSH recommended standard for occupational noise exposure [NIOSH, 1998] estimated that 25% of workers exposed to daily occupational noise levels of 90 dBA (the current exposure limit in most industries) would develop a material hearing impairment after a 40-year working lifetime. Because NIOSH considered 25% to be too high, it proposed an exposure limit that would protect more workers [NIOSH, 1998]. Our prevalence estimate of 20% approaches the 25% mark, but many of the workers in our sample do not have 40 years of noise-exposed work experience, suggesting that enhanced regulatory and preventive efforts may be needed.
Fortunately, our results also indicate that progress is being made. Although the prevalence has remained fairly constant over time, the incidence and risk of incident hearing loss has decreased in most industry sectors over the last 30 years. Hoffman et al. [2010] examined nationally-representative population data and reported that the prevalence of hearing impairment decreased significantly from the periods 1959–1962 to 1999–2004 for the general population. Reduction in occupational exposures, or improved hearing conservation efforts are possible explanations or contributors to the reduced prevalence observed by Hoffman and the reduced incidence observed in our study. However, other factors may be influencing these results, such as improved treatment of middle ear disorders, and the overall reduction in smoking prevalence, another risk factor for hearing loss [Agrawal et al., 2009].
This study had limitations. The data were a convenience sample from providers who agreed to share their data with NIOSH, and our sample may not be representative of all noise-exposed workers, especially within industries like Construction where audiometric testing is not required. However, estimates from other studies utilizing random samples have yielded mostly similar results [Tak and Calvert, 2008; Helmkamp et al., 2013]. Hearing loss can be determined from an audiogram but the work-relatedness of the loss can only be inferred in the absence of additional information. To strengthen this inference, audiograms with attributes unlikely to be related to OHL were excluded. The quality level of the audiometric data may have varied by provider and providers also “inherited” audiograms. In some cases, the industry coding was performed by the provider, with the potential for inconsistencies. When estimating prevalence, we examined one audiogram per worker without a “confirmation” audiogram. It is possible that a small number of hearing losses were temporary shifts in hearing. However, temporary threshold shift may be a sign that a worker is over-exposed to noise and can be a precursor of permanent hearing loss. All or nearly all the workers in the sample were noise-exposed workers, including workers in our reference time period. The reference period (1986–1990) was proximate to the 1983 OSHA Noise Standard amendment (29 CFR 1910.95), and pre-dated both the 2000 update to the Mining Noise Standard (30 CFR 62) and the 2002 Noise Standard for Construction (29 CFR 26.52). There is some evidence that regulations are protective [Verbeek et al., 2009]. As such, workers in our reference time period were assumed to be at higher risk than workers in later time periods. Most of the PRs are <1, indicating that the risk is lower now than in the reference time period. The PR values are not stand-alone estimates of risk. Finally, NAICS is an economic classification system which may not group workers with similar exposures together, and industries could only be examined by sector grouping due to sample size limitations.
This is the first known study to estimate and compare the prevalence and incidence of worker hearing loss by industry sector, and over such an expanded time period. Rather than relying on self-reported hearing ability, we examined audiograms from workers employed at thousands of U.S. companies. The sample size allowed us to exclude audiograms with negative slope, improving the accuracy. We also excluded audiograms of poor quality or depicting characteristics likely due to non-occupational exposures. With the exception of age group (slightly fewer younger workers were eliminated), the demographics of these excluded audiograms and the study sample were very similar, indicating no gender, geographical region, provider or industry sector was disproportionately removed from the study sample (data not shown).
This study elucidates the trends in the burden and risk of hearing loss among workers in hazardous noise environments. Efforts to reduce both the burden and risk are still needed. Special efforts should be targeted at the Mining, Construction, and Healthcare and Social Assistance industry sectors. Despite progress over the past three decades, OHL remains a problem in the U.S.
ACKNOWLEDGMENTS
The authors wish to thank David K. Wall for his contribution to the analysis, and also our data providers, without whom this research would not be possible. The authors do not have funding sources to declare.
Footnotes
Conflict of interest statement: The authors have no conflicts of interest to declare.
Disclaimer: The findings and conclusions in this article have not been formally disseminated by the National Institute for Occupational Safety and Health and should not be construed to represent any agency determination or policy.
REFERENCES
- Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: Data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009;30(2):139–145. doi: 10.1097/MAO.0b013e318192483c. [DOI] [PubMed] [Google Scholar]
- Arslan E, Orzan E. Audiological management of noise induced hearing loss. Scand Audiol Suppl. 1998;48:131–145. [PubMed] [Google Scholar]
- Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: Conceptual filters explain underreporting. Am J Public Health. 2002;92:1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniell WE, Fulton-Kehoe D, Cohen M, Swan SS, Franklin GM. Increased reporting of occupational hearing loss: Workers’ compensation in Washington State, 1984–1998. Am J Ind Med. 2002;42(6):502–510. doi: 10.1002/ajim.10146. [DOI] [PubMed] [Google Scholar]
- Deddens JA, Petersen MR. Approaches for estimating prevalence ratios. Occup Environ Med. 2008;65(481):501–486. doi: 10.1136/oem.2007.034777. [DOI] [PubMed] [Google Scholar]
- Engdahl B, Tambs K. Occupation and the risk of hearing impairment–results from the Nord-Trondelag study on hearing loss. Scand J Work Environ Health. 2010;36:250–257. doi: 10.5271/sjweh.2887. [DOI] [PubMed] [Google Scholar]
- Hager LD. Recordable hearing loss in the United States, 2004. Presented at the 31st annual conference of the National Hearing Conservation Association; Tampa, FL. 2006. [Google Scholar]
- Hager LD. Recordable hearing loss: Update, 2005. Presented at the 32nd annual conference of the National Hearing Conservation Association; Savannah, GA. 2007. [Google Scholar]
- Hager LD. Recordable hearing loss 2006: An update. Presented at the 33rd annual conference of the National Hearing Conservation Association; Portland, OR. 2008. [Google Scholar]
- Hager LD. BLS occupational hearing loss report for 2007. CAOHC Update. 2009;27:1. [Google Scholar]
- Helmkamp JC, Lincoln JE, Sestito J, Wood E, Birdsey J, Kiefer M. Risk factors, health behaviors, and injury among adults employed in the transportation, warehousing, and utilities super sector. Am J Ind Med. 2013;56(5):556–568. doi: 10.1002/ajim.22148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetu R, Getty L, Quoc HT. Impact of occupational hearing loss on the lives of workers. Occup Med. 1995;10:495–512. [PubMed] [Google Scholar]
- Hoffman HJ, Dobie RA, Ko CW, Themann CL, Murphy WJ. Americans hear as well or better today compared with 40 years ago: Hearing threshold levels in the unscreened adult population of the United States, 1959–1962 and 1999–2004. Ear Hear. 2010;31(6):725–734. doi: 10.1097/AUD.0b013e3181e9770e. [DOI] [PubMed] [Google Scholar]
- Laurikkala J, Kentala E, Juhola M, Pyykko I, Lammi S. Usefulness of imputation for the analysis of incomplete otoneurologic data. Int J Med Inform. 2000;58–59:235–242. doi: 10.1016/s1386-5056(00)00090-3. [DOI] [PubMed] [Google Scholar]
- Leigh JP, Miller TR. Occupational illnesses within two national data sets. Int J Occup Environ Health. 1998;4(2):99–113. doi: 10.1179/oeh.1998.4.2.99. [DOI] [PubMed] [Google Scholar]
- Martin FN, Clark JG. Introduction to audiology. 10th ed. chapter 4. Boston, MA: Allyn & Bacon; 2009. Pure-tone audiometry. [Google Scholar]
- Masterson EA. Dissertation Abstracts International 73 (08) 2012. Prevalence of workers with shifts in hearing by industry: A comparison of occupational noise exposure regulation criteria. (UMINo. 3503779) [Google Scholar]
- Masterson EA, Tak S, Themann CL, Wall DK, Groenewold MR, Deddens JA, Calvert GM. Prevalence of hearing loss in the United States by industry. Am J Ind Med. 2013;56:670–681. doi: 10.1002/ajim.22082. [DOI] [PubMed] [Google Scholar]
- McCall BP, Horwitz IB. An assessment of the effects of increased regulatory enforcement and legislative reform on occupational hearing loss workers’ compensation claims: Oregon 1984–1998. Am J Ind Med. 2004;45(5):417–427. doi: 10.1002/ajim.20007. [DOI] [PubMed] [Google Scholar]
- Morata TC, Themann CL, Randolph RF, Verbsky BL, Byrne DC, Reeves ER. Working in noise with a hearing loss: Perceptions from workers. Ear Hear. 2005;26:529–545. doi: 10.1097/01.aud.0000188148.97046.b8. [DOI] [PubMed] [Google Scholar]
- Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48(6):446–458. doi: 10.1002/ajim.20223. [DOI] [PubMed] [Google Scholar]
- NIOSH (National Institute for Occupational Safety and Health) Criteria for a Recommended Standard: Occupational Noise Exposure: Revised Criteria 1998. Cincinnati: Government Printing Office; 1998. [Google Scholar]
- NIOSH (National Institute for Occupational Safety and Health) Noise and hearing loss prevention. [Accessed August 17, 2013];2013a Available at http://www.cdc.gov/niosh/topics/noise/
- NIOSH (National Institute for Occupational Safety and Health) The National Occupational Research Agenda (NORA) [Accessed November 5, 2013];2013b Available at. [Google Scholar]
- Palmer KT, Coggon D, Syddall HE, Pannett B, Griffin MJ. Occupational exposure to noise and hearing difficulties in Great Britain. Suffolk: HSE Books; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman MD, Standring RT. Noise and quality of life. Int J Environ Res Public Health. 2010;7(10):3730–3738. doi: 10.3390/ijerph7103730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegelman D, Hertzmark E. Easy SAS calculations for risk and prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- Suter AH. Hearing conservation manual. 4th edition. Milwaukee, WI: Council for Accreditation in Occupational Hearing Conservation; 2002. [PMC free article] [PubMed] [Google Scholar]
- Suter AH. Standards and regulations. In: Berger EH, Royster LH, Royster JD, Driscoll DP, Layne M, editors. The noise manual. 5th edition. Fairfax, Virginia: American Industrial Hygiene Association; 2003. pp. 639–668. [Google Scholar]
- Tak S, Calvert GM. Hearing difficulty attributable to employment by industry and occupation: An analysis of the National Health Interview Survey—United States, 1997 to 2003. J Occup Environ Med. 2008;50(1):46–56. doi: 10.1097/JOM.0b013e3181579316. [DOI] [PubMed] [Google Scholar]
- Tak S, Davis RR, Calvert GM. Exposure to hazardous workplace noise and use of hearing protection devices among US workers—NHANES, 1999–2004. Am J Ind Med. 2009;52(5):358–371. doi: 10.1002/ajim.20690. [DOI] [PubMed] [Google Scholar]
- Themann CL, Suter AH, Stephenson MR, et al. National research agenda for the prevention of occupational hearing loss—Part 1. Semin Hear. 2013a;34(3):145–207. [Google Scholar]
- Themann CL, Suter AH, Stephenson MR, et al. National research agenda for the prevention of occupational hearing loss—Part 2. Semin Hear. 2013b;34(3):208–251. [Google Scholar]
- U.S. Census Bureau. North American Industry Classification System. [Accessed 17 August 2013];2011 Available at http://www.census.gov/eos/www/naics/
- U.S. Department of Commerce, The Kraus Organization Limited. North American Industry Classification System: United States, 2007. White Plains, MD: Automated Graphic Systems, Inc; 2007. [Google Scholar]
- U.S. Embassy. Travel & geography: Regions of the United States. [Accessed 3 August 2013];2008 Available at http://usa.usembassy.de/travel-regions.htm. [Google Scholar]
- Verbeek JH, Kateman E, Morata TC, Dreschler W, Sorgdrager B. Interventions to prevent occupational noise induced hearing loss. Cochrane Database Syst Rev. 2009;8(3) doi: 10.1002/14651858.CD006396.pub2. CD006396. [DOI] [PubMed] [Google Scholar]