Abstract
The health impact of retinoic acid (All Trans Retinoic Acid; ATRA) in the development of lung pathology and tissue remodeling has not been well established in the literature. Equally, the role of Citral (inhibitor of retinoid function) in the improvement of lung pathology has not been ascertained in vivo. Therefore, it is hypothesized that ATRA and Ovalbumin (Egg albumin; OVA) exposure will sensitize lung tissues leading to lung tissue pathology and that citrals (C1 and C2) will reverse or ameliorate the related pathological damage to lung tissues. The study used an IACUC approved between-subject in vivo randomized split plot factorial design (F344 rat model; N=35). Animals were sensitized to OVA and then exposed to six different treatments; negative control (−ve), ATRA, Citrals (C1 and C2) and their triple combinations (OVA+ ATRA + C1, OVA+ ATRA + C2), by intra-peritoneal route. Rat weight data and blood were collected on Days 1 and 21, all animals were sacrificed on day 21, and lung tissues were processed for histopathology. Results from rat weights and blood (ANOVA and Duncan) as well as from the histopathological analysis of exposing the F344 rats to OVA in combinations with ATRA and citrals, revealed various levels of lung tissue damage that was impacted by exposure to citral. We conclude that OVA+ATRA+C1 combination treatment did improve lung pathology as compared to single individual treatments. However, the OVA+ATRA+C2 combination not only failed to improve these parameters, but even worsened the lung pathology of this model. This promising study showed variable responses on the interaction of Ovalbumin, citrals, and ATRA as related to their damage/improvement of related lung tissue pathologies.
Keywords: ATRA, Citral, F344, Ovalbumin, Chronic Lung Pathology, Hpervitaminosis A
INTRODUCTION
Chronic pulmonary diseases including asthma are afflicting a great number of patients worldwide. The connection of retinoic acid in the development of such ailments was unclear at best. Retinoids represent the chemical derivatives of vitamin A or all-trans retinol. These include retinol, retinaldehyde, and all forms of the final oxidized product retinoic acid (RA). Vitamin A is generally obtained from the diet in the form of retinyl esters that are linked to fatty acids such as palmitic acid or in the form of carotenoids which are dimers of retinal; the oxidative aldehyde form of retinoid isomers [1, 2, 3 and 4]. The current known clinical uses of some selected retinoids include the treatment of dermatologic diseases such as acne, psoriasis, and eczema, photo-damaged skin, and specific forms of cancer [2, 4]. Biological effects of retinoids are generally exerted through a series of nuclear receptors that are ligand-inducible transcription factors belonging to the steroid/thyroid receptor superfamily such as RAR and RXR retinoid nuclear receptors (1, 2, 1nd 5).
Recent challenges in the treatment of chronic lung disease include restoration of alveolar surface area, respiratory and mechanical function of the lung parenchyma has led to a focus on retinoids as therapeutic agents [6, 7, and 8]. Retinoids are known alveolar morphogens based on the fact that RA was shown to ameliorate emphysema in rats after the intra-tracheal instillation of elastase [9, 10, and 11]. Circulating retinoids as well as the endogenous stores furnish the required amounts of retinoids to body cells through the hydrolysis of RP [12, 13]. Retinoids are pleiotropic regulatory compounds that are capable of modulating the structure and function of a wide range of inflammatory, immune and structural body cells. They possess a hormone-like function that regulate epithelial cell proliferation, pattern formation in developing tissues, morphogenesis in the lung, and cellular differentiation It is known that alveolar architecture depends on the anatomy of prenatal airways in mice, rats and humans. Airway branching, elongation, and cellular differentiation are influenced by retinoids, however, one of the important component of the alveolus is the septum which is composed of epithelial and endothelial cells, fibroblasts and some immune and neuro-endocrine cells [14]..
Citral has been reported to exhibit activity as a Vitamin A antagonist by inhibiting the oxidation of retinal to retinoic acid. This suggests that Citral is able to block the endogenous RA signaling pathway [15]. Hypervitaminosis A is a condition representing retinoid toxicity, which may reflect its effects on the lungs as a damaging agent. To this end and in reference to the literature where the findings on the responses to ATRA both in vitro and in vivo appeared to be contadictory [2, 3 and 16]. This study was undertaken to explore this controversy.
This paradox in the function of retinoids [17-23] as curing or damaging agents prompted the execution of our study with the hypothesis that application of supraphysiologic levels of retinoids ATRA will cause lung pathologic damage similar to ovalbumin exposure. The objective of the study was to assess the impact of exposing the F344 rat model to supraphysiologic levels of triple combinations of ATRA, OVA, C1, C2, and their comparison to untreated controls, aiming to produce insights into the development of chronic lung disease in an in vivo setting.
METHODS
High purity All Trans Retinoic Acid (ATRA), Ovalbumin, OVA, Aluminum hydroxide, Citral 1 (C1; diethyl acetal and Citral 2 (C2; cis and Trans dimethyl), DMSO, Isoflurane and PBS were purchased from Sigma Aldrich Company, St. Louis, MO.
Animals and housing
Fisher rats (F344; 260-324 g) were purchased from Harlan Laboratories (Frederic, MD). The animals were housed at the Jackson State University (JSU) Animal Core Facilities (Olaw class 2 level). Animals were acclimatized for a week and all protocols including handling, husbandry, anesthesia, euthanasia, and experimental designs were approved by JSU-IACUC (protocol # 08-13-08) and were performed according to Olaw recommendations. Animals were kept under a controlled environment at 12/12 light /dark cycles and were allowed unrestricted access to water and rodent chow. Each animal was kept in a separate rat cage that was well maintained by a technical staff supervised by a veterinarian.
Experimental design
A total of 30 F344 rats were used in this study. Five animals were not treated and designated as negative control. The remaining 25 animals were divided into 5 different groups of 5 animals each and were exposed to treatments through intra-peritoneal (iP) route on day 1 using Ovalbumin-Aluminum hydroxide (OVA; following manufacturer’s protocols) for all groups except for the negative control; Ovalbumin is known to create lung pathology and is used to create a background of lung pathology in the study. After one week of exposure to OVA, each designated group was injected with the corresponding chemicals in combination that include ATRA (80 mg/Kg), citral 1 (C1; 50 mg/Kg), and citral 2 (C2; 50 mg/Kg) by the intra-peritoneal route. All animals were weighed on days 1 and 21 and were sacrificed (euthanized by inhalation of CO2 in special chamber) on day 21 following approved protocols and blood was collected for parameter analysis. Dead animals were subjected to in-house post-mortem (Necropsy) procedures and entire lungs from all animals were collected in 10% formalin for histopathological analysis. Blood analysis was done by the Mississippi State Veterinary lab; using an automated cell sorter.
Tissue processing, slide preparation and digitizing
Formalized lung tissue was processed for histopathology following standard procedures. Tissues were embedded in paraffin blocks and were then sectioned using a Leica Microtome to produce 5μm sections. Sections were floated in a water bath, adhered to standard glass slides and allowed to dry. Slides were then stained using standard Hematoxylin and Eosin staining procedure for further analysis. Slides were examined under the microscope and digitized into photos to document pathological changes from the impact of their exposure to these chemicals.
Statistical analysis
As based on the experimental design of the study, factorial analysis statistics for F-ratios associated with ANOVA was employed to support significance and interpretation of data using the standard software packages SPSS. Variance in mean differences (p<0.05) was determined by ANOVA and the Duncan ranking statistics and presented as mean ± SD.
RESULTS
Data on the comparison of weight gain and survival of the F344 rat model upon exposure to 7 different treatments is displayed in table 1. Rat weights ranged between 229±9.5 and 305±3.0 g. As can be seen, even though the exposure to both OVA and ATRA is not statistically significant from the negative (−) control, exposure to C1 in the three unit combination is highly antagonistic; both ATRA and OVA in this combination failed to reverse the negative effects of C1 on weight gain by the model (9.55*, 97.05* vs 36.70* %; one dead animal). In contrast to the C1 impact on weight gain, OVA and ATRA showed the ability to reverse the negative effects on weight gain by C2 on the model; the addition of C2 to this combination showed a further improvement in the negative effects on weight gain by the C2 control (27.50* vs 102.53* %). All animals in this group survived to term except for one animal in the OVA+ATRA+C1 group.
Table 1.
Comparison of weight data and survival of F344 rats exposed to ATRA, OVA+ATRA+C1, C1, OVA+ATRA+C2, C2 and OVA (n=35)
| # | Treatment Type | N | Initial Weight (g) |
Final Weight (g) |
Weight Difference (g) |
Standard Difference (g) |
Weight Gain/Av Control % |
Survival to term |
|---|---|---|---|---|---|---|---|---|
| 1 | − Control | 5 | 264.0±8.0 | 287.7±2.6 | 23.7 | 0.00 | 100.00 | +++++ |
| 2 | + ATRA Control | 5 | 229.7±9.5 | 251.3±17.6 | 21.7 | −2.00 | 91.55 | +++++ |
| 6 | OVA + ATRA + C1 | 5 | 251.0±14.9 | 259.7±10.5 | 8.7* | −15.00 | 36.70 | −++++ |
| 3 | + C1 Control | 5 | 244.6±10.3 | 255.0±4.6 | 10.4* | −13.30 | 44.00 | +++++ |
| 7 | OVA + ATRA + C2 | 5 | 260.6±4.7 | 284.9±7.2 | 24.3 | +0.60 | 102.53 | +++++ |
| 4 | + C2 Control | 5 | 261.4±8.4 | 267.9±9.8 | 6.5* | −17.12 | 27.50 | +++++ |
| 5 | + OVA Control | 5 | 272.6±3.8 | 305.6±3.0 | 23.0 | −0.70 | 97.05 | +++++ |
Statistically significant at p<0.05.
Data on the comparison of RBC parameters is shown in table 2. Statistically significant differences from the reference mean (standard mean for this parameter for the animal model used) are shown for RBCs by C1 control only (−2.20±1.9* M/μL). In regard to HCT, statistical significance was recorded for ATRA (−) and OVA (+) controls, as well as a synergy for OVA+ATRA+C1 (12.84±3.92*%). MCV and MHC parameters did not show significance for any of the seven treatments. The Hb showed significance for C1 and OVA+ATRA+C1 (−5.10±2.7* and −3.30±1.35* g/dl). MCH showed no significance for any treatment and the MCHC parameter showed significance for ATRA control (−4.03±2.43 g/dl), OVA+ATRA+C1 (−5.20±1.07 g/dl), C1 and C2 (−3.98±0.61 and −3.93±3.53 g/dl). ATRA control, C1 control, OVA+ATRA+C1, and C2 control produced changes in RBC parameters as compared to the other three treatments that did not cause any changes in these parameters. Means for these parameters were within the reference mean range for this model. OVA+ATRA+C1 did not improve the negative effects of individual treatments on RBC parameters. OVA+ATRA+C2 are inconclusive due to unavailable data (table.2).
Table 2.
Comparison of RBC parameters of F344 rats exposed to ATRA, OVA+ATRA+C1, C1, OVA+ATRA+C2. C2 and OVA (n=35)
| # | Treatment Type | N | RBCs (M/μL) | HCT (%) |
MCV (fl) |
Hb (g/dl) |
MCH (Pg) |
MCHC (g/dl) |
|---|---|---|---|---|---|---|---|---|
| 1 | − Control | 5 | 1.11±0.69 | 12.84±3.92 | 2.48±0.95 | 0.72±0.97 | −1.46±0.38 | −5.20±1.07 |
| 2 | + ATRA Control | 5 | −0.96±0.50 | −4.35±10.54* | −2.80±1.00 | −2.03±0.85 | −0.43±0.21 | −4.03±2.43* |
| 6 | OVA + ATRA + C1 | 5 | 1.09±0.67 | 12.84±3.92* | 2.48±o.95 | −3.30±1.35* | −1.62±0.21 | −5.20±1.07* |
| 3 | + C1 Control | 5 | −2.20±1.9* | −0.63±2.02 | 1.68±0.43 | −5.10±2.72* | −1.10±1.21 | −3.98±0.61* |
| 7 | OVA + ATRA + C2 | 5 | ND | ND | ND | ND | ND | ND |
| 4 | + C2 Control | 5 | −0.39±0.37 | −2.57±2.72 | 0.50±0.40 | −2.18±0.54 | −1.63±0.29 | −3.93±3.53* |
| 5 | + OVA Control | 5 | 0.04±0.26 | 4.38±2.28* | 0.80±1.06 | −0.85±0.54 | −1.00±0.14 | −3.00±0.67 |
| Reference Mean** | 8.95±1.69 | 52.24±3.90 | 54.48±2.95 | 15.72±2.80 | 18.36±1.38 | 35.20±1.07 |
Statistically significant at p<0.05. ND=no data. Data was centered on untreated group mean (standardized).
Data on total white blood cells WBC) and percent of Lymphocyte (Lymph), Monocyte, Eosinophil and segmented neutrophils (Segs) parameters upon exposure to 7 different treatments on the F344 rat model is presented in table.3. Except for ATRA control and Segs (−9.00±6.53* %), C1 and C2 and Eosinophils (3.00±2.00* and −1.5±1.00* %), the other four treatments did not show significant differences from control or reference means for any of the WBC parameters. The combination of ATRA and C1 with OVA seems to abolish their individual effects on the WBC parameters. Means for these parameters were within the normal cited reference mean range for this model**. OVA+ATRA+C1 combination reversed the negative effects of individual treatments on the WBC parameters. The OVA+ATRA+C2 combinations are inconclusive because of unavailable data (table 3).
Table 3.
Comparison of Lymph and WBC parameters of F344 rats exposed to ATRA, OVA+ATRA+C1, C1, OVA+ATRA+C2, C2 and OVA (n=35)
| # | Treatment Type | N | Lymph (%) | WBC (k/μL) | Monocytes (%) | Eosinophils (%) | Segs (%) |
|---|---|---|---|---|---|---|---|
| 1 | − Control | 5 | 0.00±0.00 | 2.01±3.70 | 0.70±1.79 | −1.00±0.00 | −16.15±3.85 |
| 2 | + ATRA Control | 5 | 0.00±0.00 | −0.33±2.80 | 0.00±0.00 | −0.50±1.00 | −9.00±6.53* |
| 6 | OVA + ATRA + C1 | 5 | 0.00±0.00 | 0.80±3.95 | 0.00±0.00 | −1.00±0.00 | −3.83±13.32 |
| 3 | + C1 Control | 5 | 0.00±0.00 | −1.58±2.85 | 0.00±0.00 | 3.00±2.00* | −0.25±10.84 |
| 7 | OVA + ATRA + C2 | 5 | ND | ND | ND | ND | ND |
| 4 | + C2 Control | 5 | 0.00±0.00 | 0.35±1.08 | 0.00±0.00 | −1.50±1.00* | −1.50±7.33 |
| 5 | + OVA Control | 5 | 0.00±0.00 | −1.83±2.43 | 0.00±0.00 | 1.00±0.00 | −4.50±3.42 |
| Reference Mean* * | 82.2±5.12 | 8.80±1.97 | 2.00±0.67 | 0.00±0.00 | 33.1±2.34 |
Statistically significant at p<0.05. ND=no data. Data was centered on untreated group mean (standardized).
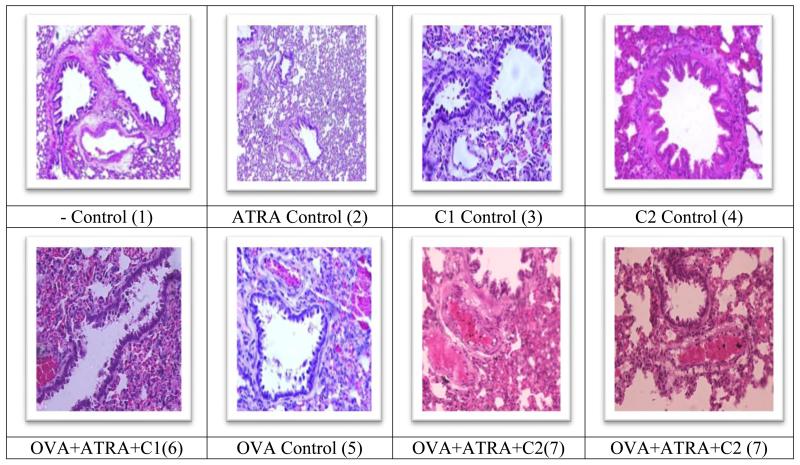
The results from OVA and ATRA are consistent with hypersensitivity, bronchoconstriction and vascular congestion rather than damage to lung tissue as impacted by C1 and C2 exposures (Fig 1; side by side panel view). . In comparison, the single treatment controls are showing as seen in figure 1: Panel (1) is the no treatment control of the F344 rat lung illustrating normal lung tissue of with bronchial walls as well as variable sized bronchioles made up of ciliated pseudostratified columnar epithelium and smooth muscles. Panel (5) is the OVA control showing hypersensitivity, congestion of blood vessels and damaged bronchi. Panel (2) depicts the ATRA control treatment of the F344 rat lung showing thickening and constriction of alveoli, congestion, constricted vessels and appearance of papillary projections into lumens of bronchioles. Panel (3); the C1 control illustrating an abundance of papillary projections, very thick alveolar walls, more basophilic condition, columnar epithelium, evident congestion and constricted vessels and alveoli. Panel (4); the C2 Control illustrating thick alveolar walls but with clear evidence for inflammation, eosinophilic appearance, thick walled and dilated blood vessels with numerous red blood cells, vessel congestion and major constriction of the alveoli.
Fig 1.
Comparison of lung pathology of F344 rats exposed to OVA + ATRA+C1. In comparison to relative controls, this treatment show loss of alveolar boarders as well as loss of alveolar projections, constriction of alveoli and loss of lung space.
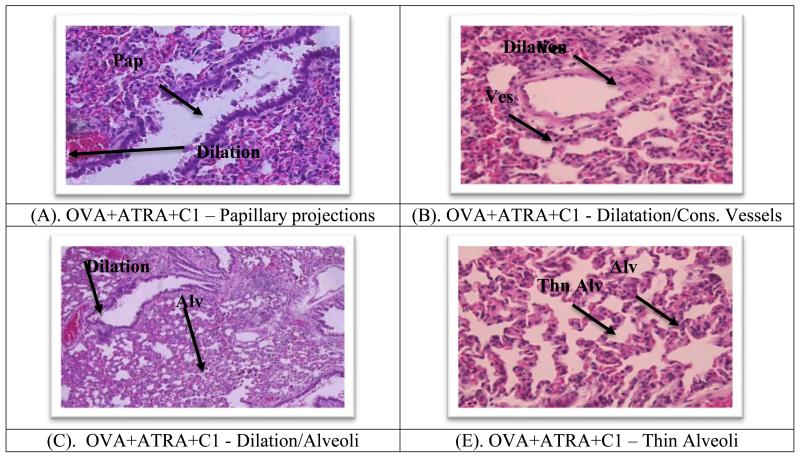
As seen in Figures 2 (400× magnification): For OVA+ATRA+C1; Panel (A) is showing histopathological results of treating the F344 rat lung portraying papillary projections, columnar epithelium and congestion. Panel (10B) illustrating the presence of dilated vessels similar to the negative control and an evidence of massive inflammatory cells throughout the section view. Panel (10C) is the presence of alveoli that appears thinner than the negative control, congested and dilated vessels that are standing wide open, and Panel (10E) is illustrating dilated, congested and thin alveoli.
Fig 2.
Ovalbumin sensitized lung histopathological display of Fischer 344 rat model. As seen in Figure 2 (A) OVA+ATRA+C1 treatment to F344 rat lung portraying papillary projections, columnar epithelium and congestion. (B) OVA+ATRA+C1 treatment to F344 rat lung illustrating the presence of dilated vessels as similar to negative control and evidence of massive inflammatory cells throughout.(C) OVA+ATRA+C1 treatment to F344 rat lung illustrating the presence of alveoli that appears not as thick as the negative control, congested and dilated standing wide open. (D) OVA+ATRA+C1 treatment to F344 rat lung illustrating dilated alveoli and vessels, slight congestion, massive inflammatory cells, slightly thick alveoli unlike negative control and no papillary projections. (E) OVA+ATRA+C1 treatment to F344 rat lung illustrating dilated, congested and thin alveoli; 400×.
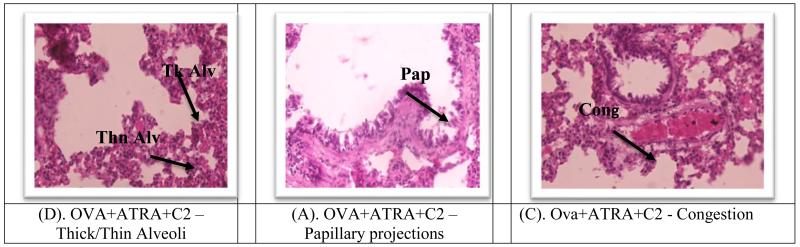
As seen in Figure 3: Panel (A) for OVA+ATRA+C2 treatment of the F344 rat lung illustrating the presence of papillary projections within the alveoli. Panel (C) illustrating evident congestion, the presence of red blood cells within the bronchi and the presence of papillary projections; and Panel (D) illustrating evident congestion, thick and thin alveolar walls and collection of red blood cells within bronchi The major findings are that OVA+ATRA+C1 combination treatment did improve lung pathology as compared to single individual treatments. However, the OVA+ATRA+C2 combination have failed to improve lung pathology due to the adverse effects of the C2 individual treatment in the combination (Fig 3).
Figure 3.
Comparison of lung pathology of F344 rats exposed to OVA+ATRA+C2. In comparison to relative controls, this treatment show loss of alveolar boarders as well as loss of alveolar projections, constriction of alveoli and loss of lung space. Mold + C2 showed eosinophilia changes and lung structure destruction. 400×.
DISCUSSION
In reference to weight gain, individual treatments with ATRA, OVA didn’t affect weight gain as compared to the −control. The combination of ATRA and OVA was synergistic and boosted weight gain 62% more than the −control. The C1 and C2 treatments have negative impact on weight gain. The combination of OVA and C1 reversed the negative effects by C1 (OVA is antagonistic to C1). Ova failed to reverse the adverse effects by C2 on weight gain [24]. The triple OVA+ATRA+C1 combination did not reverse the adverse effects of C1 on weight gain; OVA and ATRA did not protect the model from weight loss impacted by exposure to C1 treatment (97.05, 91.55 and 44.00 vs 34.70). In contrast OVA+ATRA+C2 combination completely reversed the negative effects of C2 on weight gain (97.05, 91.55 and 27.50 vs 102.5 3; table 1). This combination confirmed that ATRA and C2 are antagonistic in their action and also showed that C2, in addition to its traditional antagonistic role in vitamin A oxidation and ATRA production, did inhibit and reversed ATRA impact and function under in vivo application (C1 failed to reverse weight loss by the combination in the presence of OVA and ATRA); this is a completely new finding with regards to the relationship of C1, C2 and ATRA in the presence of ovalbumin. The findings from the combination of OVA, ATRA and C2 also showed the contrast in the relationship between ATRA and C2 in the reversal of weight loss impact by C2 leading to the conclusion that C2 but not C1 and ATRA are antagonistic in their function; establishing a new finding from this study. DiRenzo et al. [25] demonstrated that citral inhibits the synthesis of retinoic acid but the mechanism still remains unknown. Nenegola et al. [26] demonstrated the inhibitory effects of citral in retinoic acid synthesis. Beeman et al. [27] showed the blockage of initiation of murine odontogenesis in vitro by citral. Other supportive studies [28, 29, 30, 31, 32, 33, 34, 35, and 36].
The triple level treatment with OVA+ATRA+C1 did not improve the negative effects of individual treatments on RBC parameters; supporting the none antagonistic relationship between ATRA and C1 in this combination based on OVA and C1 treatment as well as the impact of the triple combination on weight gain. OVA+ATRA+C2 treatment is not conclusive due to unavailable data (Table 2). OVA+ATRA+C1 combination reversed the negative effects of individual treatments on the WBC parameters; this difference may be explained by the fact that exposure of blood WBC to this combination could have less impact on this parameter, which is generally the case from our data; the blood WBCs may not be a sensitive system to reflect the relationship between ATRA and C1. OVA+ATRA+C2 treatment is inconclusive because of unavailable data (Table 3). Massaro and Massaro [37] showed that ATRA treatment of animals may promote repair, regeneration, or both in damaged alveoli which could result in improved diffusion capacity. OVA-sensitization of animals produces significant infiltration of inflammatory cells in the lungs (Hui-Fang, et al [38]. Kakazu et al. [39] demonstrated that OVA treatment of animal significantly increased levels of monocytes, lymphocytes, neutrophils, and eosinophils.
In reference to lung pathology, OVA+ATRA+C1 triple combination treatment did improve lung pathology due to the impact of C1 treatment to confirm the antagonistic actions of C1 and OVA as well as the synergy of ATRA and C1on lung pathology. However, the OVA+ATRA+C2 combination failed to improve lung pathology contrary to expectation and perhaps due to the damaging impact of C2 treatment to confirm the finding that C2 and ATRA actions in lung pathology are not antagonistic in the OVA- sensitized F344 rat Model (Fig 3).
The reversal of pathological findings by C1 on the lung of the F344 rat model by ATRA in the triple combination and failure to achieve that by ATRA and C2 will definitely show contradictory findings (reverse action) shown by other tests (weight and blood parameters) with regards to the relationship of ATRA, C1 and C2 in the presence of OVA; which we have found to be dependent on the type of parameter and the nature of the action site.
CONCLUSIONS
The objective of the study was to assess the impact of supraphysiologic levels of triple combinations of OVA, ATRA, C1 and C2 in the F344 rat model in comparison to untreated control and single treatments including OVA, ATRA, C1 and C2. ATRA was able to reverse the impact of both C1 and C2 on weight gain. The triple level treatment with OVA+ATRA+C1 did not improve the negative effects of individual treatments on RBC parameters; supporting a relationship that is not antagonistic between ATRA and C1. In reference to lung pathology, OVA+ATRA+C1 triple combination treatment did improve lung pathology due to the impact of C1 treatment to confirm the antagonistic actions of C1 and ATRA on lung pathology. However, the OVA+ATRA+C2 combination has failed to improve lung pathology due to the pathological impact of C2 treatment on lung tissues and confirmed the finding that C2 and ATRA actions in lung pathology are not antagonistic in the OVA- sensitized F344 rat Model. The reversal of pathological findings by C1 on the lung of the F344 rat model by ATRA in the triple combination and failure to achieve that by ATRA and C2 will definitely show contradictory findings (reverse action) shown by other tests (weight and blood parameters) with regards to the relationship of ATRA, C1 and C2 in the presence of OVA; which we have found to be dependent on the type of parameter and the nature of the action site. The findings of this study call for further investigation of these relationships to confirm the anti-inflammatory benefits of citrals.
ACKNOWLEDGMENTS
This research is supported by NIH/NCRR RCMI grant # G12-MD007581.
REFERENCES
- 1.McGowan SE. Contributions of Retinoids to the Generation and Repair of the pulmonary alveolus. Chest. 2002;121:206S–208S. doi: 10.1378/chest.121.5_suppl.206s. [DOI] [PubMed] [Google Scholar]
- 2.Belloni PN, Garvin L, Mao C.-Ping, Bailey-Healy I, Leaffer D. Effects of All-Trans-Retinoic Acid in Promoting Alveolar Repair. Chest. 2000;117:235S–241S. doi: 10.1378/chest.117.5_suppl_1.235s. [DOI] [PubMed] [Google Scholar]
- 3.Massaro GD, Massaro D. Retinoic Acid Treatment Abrogates Elastase-induced Pulmonary Emphysema. Nature Med. 1997;3:675–703. doi: 10.1038/nm0697-675. [DOI] [PubMed] [Google Scholar]
- 4.Chambone PA. A Decade of Molecular Biology of Retinoic Acid Receptors. FASEB J. 1996;10:940–954. [PubMed] [Google Scholar]
- 5.Chytil F. Retinoids in Lung Development. FASEB J. 1996;10:986–992. doi: 10.1096/fasebj.10.9.8801181. [DOI] [PubMed] [Google Scholar]
- 6.M McGowan SE, Doro MM, Jackson SK. Endogenous Retinoids Increase Perinatal Elastin Gene Expression in Rat Lung Fibroblasts and Fetal Explants. Am. J. Physiol. Lung Cell Mol. Physiol. 1997;273:L410–L416. doi: 10.1152/ajplung.1997.273.2.L410. [DOI] [PubMed] [Google Scholar]
- 7.Massaro GD, Massaro D. Retinoic Acid Treatment Partially reverses Failed Septation in Rats and Mice. AM. J. Physiol. 2000;278:L955–L960. doi: 10.1152/ajplung.2000.278.5.L955. [DOI] [PubMed] [Google Scholar]
- 8.Morabia A, Menkes M, Comstock G, et al. Serum Retinol and Airway Obstruction. AM. J. Epidemiol. 1990;132:77–82. doi: 10.1093/oxfordjournals.aje.a115645. [DOI] [PubMed] [Google Scholar]
- 9.Paiva S, Goday I, Vannucchi H, et al. Assessment of Vitamin A Status in Chronic Obstructive Pulmonary Disease Patients and Healty Smokers. Am. J. Clin. Nutr. 1996;64:929–934. doi: 10.1093/ajcn/64.6.928. [DOI] [PubMed] [Google Scholar]
- 10.Napoli J. Retinoic Acid Biosynthesis and Metabolism. FASEB J. 1996;10:993–1001. doi: 10.1096/fasebj.10.9.8801182. [DOI] [PubMed] [Google Scholar]
- 11.Haq R, Pfahl M, Chytil F. Retinoic Acid Affects the E xpression of Nuclear Retinoic Acid Recptors in Tissues of Retinol Deficient Rats. Proc Natl Acad Sci USA. 1991;88:8272–8276. doi: 10.1073/pnas.88.18.8272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zachman R. Role of Vitamin A in Lung Development. J. Nutr. 1995;125(Suppl):1934S–1638S. doi: 10.1093/jn/125.suppl_6.1634S. [DOI] [PubMed] [Google Scholar]
- 13.Liu R, Harvey C, S McGowan. Retinoic Acid increase Elastin in Rat Lung Fibroblasts Cultures. Am. J. Physiol. 1993;265:L430–L437. doi: 10.1152/ajplung.1993.265.5.L430. [DOI] [PubMed] [Google Scholar]
- 14.Okabe T, Yorifuji H, Yamada E, et al. Isolation and characterization of Vitamin A Storing Lung Cells. Exp. Cell Res. 1984;154:125–135. doi: 10.1016/0014-4827(84)90673-6. [DOI] [PubMed] [Google Scholar]
- 15.Schuh TJ, Kraft J, Hall BL. V-erbA and Citral Reduce the Teratogenic Effects of all-trans Retinoic Acid and Retinol, Respectively, in Xenopus Embryogenesis. Development. 1993;119:785–798. doi: 10.1242/dev.119.3.785. [DOI] [PubMed] [Google Scholar]
- 16.Tanumihardjo SA, Penniston KL. The Acute and Chronic Toxic Effects of Vitamin A. American Journal of Clinical Nutrition. 2006;83:191–201. doi: 10.1093/ajcn/83.2.191. [DOI] [PubMed] [Google Scholar]
- 17.Massaro GD, Massaro D. Postnatal Treatment with Retinoic Acid Increases the Number of Pulmonary Alveoli in Rats. Am. J. Physiol. 1996;270:L305–L310. doi: 10.1152/ajplung.1996.270.2.L305. [DOI] [PubMed] [Google Scholar]
- 18.Swee M, Parks W, Pierce R. Developmental regulation of Elastin Production. J Biol Chem. 1995;270:14899–14906. doi: 10.1074/jbc.270.25.14899. [DOI] [PubMed] [Google Scholar]
- 19.Austead G. Steroids, Retinoids and Wound Healing. Adv. Wound Care. 1998;11:277–285. [PubMed] [Google Scholar]
- 20.Hunt T. Vitamin A and Wound Healing. J Am Acad Dermatol. 1986;15:817–821. doi: 10.1016/s0190-9622(86)70238-7. [DOI] [PubMed] [Google Scholar]
- 21.Tepper J, Pfeiffer J, et al. Can Retinoic Acid Ameliorate the Physiologic and Morphologiceffects of elastase instillation in the Rat. Chest. 117(suppl. 1):242S–244S. doi: 10.1378/chest.117.5_suppl_1.242s. [DOI] [PubMed] [Google Scholar]
- 22.Maple S, Mendelssohn C, Cardoso WV. Regulation of retinoic acid signaling during lung morphogenesis. Development. 2000;127:3057–3067. doi: 10.1242/dev.127.14.3057. [DOI] [PubMed] [Google Scholar]
- 23.Mao JT, Goldin JG, Ermand J, et al. A pilot study of all-trans retinoic acid for the treatment of human emphysema. Am. J Respir. Crit. Care Med. 2002;165:718–723. doi: 10.1164/ajrccm.165.5.2106123. [DOI] [PubMed] [Google Scholar]
- 24.Farah IO, Holt-Gray C, Cameron JA, Tucci M, Cason Z, Benghuzzi HA. Impact of Paired Combinations of Retinoic Acid (ATRA) and Ovalbumin on F344 Rat Lung Tissues and Improvement of Related Pathology by Citral. Biomed. Sci. Instrum. 2014;50:423–30. [PMC free article] [PubMed] [Google Scholar]
- 25.DiRenzo F, Broccia ML, Giavini E, Menegola E. Citral, an inhibitor of retinoic acid synthesis, attenuates the frequency and severity of bronchial arch abnormalities induced by triazole-derivative fluconazole in rat embryos cultured in vitro. Reproductive Toxicology. 2007;24(3-4):326–32. doi: 10.1016/j.reprotox.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Nenegola E, Giavini E, DiRenzo F, Broccia Y. Citral, an inhibitor of retinoic acid synthesis, attenuates the frequency and severity of bronchial arch abnormalities induced by triazole-derivative fluconazole in rat’s embryos culture in vitro. Reproductive Toxicology. 2007;24(3):326–332. doi: 10.1016/j.reprotox.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Beeman C, Berndt CS, Kronmillera W, E. J, Nguyen T. Blockade of the initiation of murine odontogeness in vitro by citral, an inhibitor of endogenous retinoic acid synthesis. Archives of Oral Biology. 1995;4:7. doi: 10.1016/0003-9969(95)00015-h. [DOI] [PubMed] [Google Scholar]
- 28.McGowan S, Holmes A, Smith J. Retinoic acid reverses the airway hyperresponsiveness but not the parenchymal defect that is associated with vitamin A deficiency. American Journal of Physiology: Lung Cellular & Molecular Physiology. 2004;30(2):L437–L444. doi: 10.1152/ajplung.00158.2003. [DOI] [PubMed] [Google Scholar]
- 29.Belloni PN, Garvin L, Ping C, Mao I, Bailey-Healy D, Leaffer D. Effects of All-Trans-Retinoic Acid in Promoting Alveolar Repair. Chest. 2000;117:235S–241S. doi: 10.1378/chest.117.5_suppl_1.235s. [DOI] [PubMed] [Google Scholar]
- 30.Massaro GD, Massaro D. Postnatal Treatment with Retinoic Acid Increases the Number of Pulmonary Alveoli in Rats. Am. J Physiol. 1996;270:L305–L310. doi: 10.1152/ajplung.1996.270.2.L305. [DOI] [PubMed] [Google Scholar]
- 31.Chytil F. The lungs and vitamin A. American Journal of Physiology. 1992;262:L517–L527. doi: 10.1152/ajplung.1992.262.5.L517. [DOI] [PubMed] [Google Scholar]
- 32.Tanumihardjo SA, Penniston KL. The Acute and Chronic Toxic Effects of Vitamin A. American Journal of Clinical Nutrition. 2006;83:191–201. doi: 10.1093/ajcn/83.2.191. [DOI] [PubMed] [Google Scholar]
- 33.Hunt T. Vitamin A and Wound Healing. J Am Acad Dermatol. 1986;15:817–821. doi: 10.1016/s0190-9622(86)70238-7. [DOI] [PubMed] [Google Scholar]
- 34.Tepper J, Pfeiffer J, Aldrich M, et al. Can Retinoic Acid Ameliorate the Physiologic and Morphologic effects of elastase instillation in the Rat. Chest. 2000;117(suppl 1):242S–244S. doi: 10.1378/chest.117.5_suppl_1.242s. [DOI] [PubMed] [Google Scholar]
- 35.Malpe S, Mendelssohn C, Cardoso WV. Regulation of retinoic acid signaling during lung morphogenesis. Development. 2000;127:3057–3067. doi: 10.1242/dev.127.14.3057. [DOI] [PubMed] [Google Scholar]
- 36.Mao JT, Goldin JG, Ermand J, et al. A pilot study of all-trans retinoic acid for the treatment of human emphysema. Am. J Respir. Crit Care Med. 2002;165:718–723. doi: 10.1164/ajrccm.165.5.2106123. [DOI] [PubMed] [Google Scholar]
- 37.Massaro GD, Massaro D. Retinoic Acid Treatment Abrogates Elastase-induced Pulmonary Emphysema. Nature Med. 1997;3:675–703. doi: 10.1038/nm0697-675. [DOI] [PubMed] [Google Scholar]
- 38.Hui-Fang T, Yan-Hua S, Jun-Chun C. Upregulation of phosphodiesterase-4 in lung of allergic rats. American Journal of Respiratory and Critical Care Medicine. 2005;171:823–828. doi: 10.1164/rccm.200406-771OC. [DOI] [PubMed] [Google Scholar]
- 39.Kakazu T, Chihara J, Saito A, Nakajima S. Effect of RANTES on eosinophil adhesion to plates coated with recombinant soluble intercellular adhesion molecule-1 and expression of beta 2-integrin adhesion molecules on eosinophils. Int. Arch Allergy Immunol. 1995;108:9–11. doi: 10.1159/000237190. [DOI] [PubMed] [Google Scholar]