Abstract
Objective
Pediatric loss of control (LOC) eating is predictive of partial- and full-syndrome binge eating disorder. The interpersonal model proposes that LOC eating is used to cope with negative mood states resulting from interpersonal distress, possibly on a momentary level. We therefore examined temporal associations between interpersonal problems, negative affect, and LOC eating among overweight adolescent girls using ecological momentary assessment (EMA).
Method
Thirty overweight and obese (≥85th body mass index (BMI) percentile; BMI: M = 36.13, SD = 7.49 kg/m2) adolescent females (Age: M = 14.92, SD = 1.54 y; 60.0% African American) who reported at least two LOC episodes in the past month completed self-report momentary ratings of interpersonal problems, state affect, and LOC eating for 2 weeks. A series of 2-level multilevel models with centering within subjects was conducted.
Results
Between- and within-subjects interpersonal problems (p’s < .05), but not between- (p = .12) or within- (p = .32) subjects negative affect predicted momentary LOC eating. At the between-subjects level, interpersonal problems significantly predicted increases in negative affect (p < 001).
Discussion
Naturalistic data lend support to the predictive value of interpersonal problems for LOC eating among adolescents. Interventions targeting interpersonal factors on a momentary basis may be useful during this developmental stage.
Keywords: loss of control eating binge eating, interpersonal model, adolescents, negative affect, eating disorders
Introduction
Loss of control (LOC) eating, defined as the subjective experience of being unable to stop eating or control what or how much one is eating, is reported by approximately 1.5–28% of nonclinical adolescents and is disproportionally reported by girls compared to boys.1 LOC eating is predictive of worsening general and eating-related psychopathology,2 excess weight gain,1 and metabolic dysfunction.3 Importantly, LOC eating during childhood and adolescence may represent a developmental precursor to binge eating disorder (BED) in vulnerable individuals.2 Examination of proximal psychosocial factors promoting LOC eating during youth is needed to inform developmental risk models and refine intervention targets.
One theoretical model to explain LOC eating is the interpersonal model.4 This model proposes that interpersonal problems lead to the experience of negative affect that, in turn, precipitates LOC eating. The model’s underpinnings emerge from interpersonal theory,5 which holds that interpersonal patterns can either promote self-esteem or result in hopelessness, anxiety, and psychopathology. Interpersonal theory stems from the developmental theory of attachment,6 emphasizing the importance of early relationship quality on interpersonal functioning and psychological outcome. Cross-sectional, retrospective data using structural equation modeling appear to support the interpersonal model of LOC eating in nontreatment seeking children and adolescents7 and adolescent girls, specifically.8
The first association proposed by the interpersonal model is that between interpersonal problems and negative affect. Cross-sectional and prospective studies in pediatric samples consistently support a relationship between interpersonal difficulties, such as isolation, lack of dyadic friendships, peer victimization and rejection, and negative mood, such as internalizing problems including depression and low self-esteem (e.g., Ref. 9). Interpersonal difficulties may be especially salient for overweight adolescent girls, among whom LOC eating is disproportionally represented.1 Overweight youth tend to report more frequent teasing, social isolation, and generally compromised interpersonal functioning compared with nonoverweight youth.10,11 Furthermore, several longitudinal studies have shown that weight-based teasing and critical comments by family members are risk factors for the onset of LOC eating during adolescence.12,13
The second link proposed by the model is the relationship between negative affect and LOC eating. Consistently, studies support a robust relationship between trait and state negative affect and aberrant eating in youth as measured by self-report questionnaires. Prospectively, increases in depressive symptoms and decreases in self-esteem predict the persistence of LOC eating from childhood to adolescence13 and from adolescence to adulthood.14 Prior to a laboratory test meal, youth with LOC eating report greater negative affect compared with those without LOC eating.15 Furthermore, premeal state negative affect has been shown to predict palatable food consumption among adolescent girls with LOC eating.16
Given that the potential associations between components of the interpersonal model may occur on a momentary level, ecological momentary assessment (EMA) is an ideal methodology to study LOC eating among youth in their natural environments. To date, there are limited naturalistic data in pediatric samples. The only pediatric study using EMA to study disordered eating found insufficient evidence to suggest that negative mood significantly contributed to LOC episodes during middle childhood.17 However, this study did not examine social difficulties. By contrast, a number of studies in adults have used EMA to examine binge eating, and negative affect has been well documented as a precipitant of binge episodes.18 One EMA study examining the interpersonal model among adult women with sub-threshold binge eating found that interpersonal problems predicted binge eating, and this effect was mediated by negative affect.19 However, there are no EMA data in relation to social functioning and negative affect in adolescents with LOC eating.
Taken together, scientific theory,4 preliminary cross-sectional research,20 and one adult EMA study in women with subclinical eating pathology19 lend support to the interpersonal model. Yet, inconsistent findings across adult and child studies regarding the relationship between negative affect and disordered eating behavior suggest that developmetal factors may moderate the relationships among interpersonal model variables. Among youth, the relationship between negative affect and LOC eating may be different than among adults and those with more severe forms of eating pathology. Furthermore, no study has directly examined the interpersonal model in overweight adolescent girls, a particularly vulnerable sample. We therefore used EMA to test the relationships between interpersonal model variables using a naturalistic design. We hypothesized that interpersonal problems would predict negative affect and LOC eating, and that negative affect would directly predict LOC. In exploratory analyses, we tested the hypothesis that the relationship between interpersonal problems and LOC eating would be mediated via change in negative affect.
Method
Participants
Participants were 30 adolescent girls, 12–17 years, with a body mass index (BMI; kg/m2) at or above the 85th percentile for age and sex21 who reported engaging in at least two episodes of LOC eating during the month prior to assessment. This LOC frequency criterion was selected in order to maximize the likelihood that adolescents would experience at least one LOC episode during the study monitoring period. Participants were required to be English speaking. Exclusion criteria were the presence of a parent-reported major medical illness, use of medications affecting eating or body weight, pregnancy, or presence of a major psychiatric disorder. The study was approved by the USUHS institutional review board, and all adolescents and parents provided written assent and consent, respectively, for study participation.
Adolescents were recruited from the Washington, DC metropolitan area and local suburbs in Maryland and Virginia. Recruitment efforts were targeted toward parents of overweight adolescent girls and included a number of methods: (1) Flyers posted at local facilities (e.g., libraries, supermarkets) with permission; (2) Direct mailings to families in the greater Washington D.C. metropolitan area obtained from a direct marketing services company; and (3) Direct mailings and email contact with families who expressed an interest in our prior eating-related research studies for adolescent girls. Interested participants were screened over the telephone to determine potential eligibility. If an individual was eligible, she was scheduled for a screening visit at the USUHS Developmental Laboratory for Eating and Weight Behaviors. The number of adolescents screened at each phase of recruitment is provided in Supporting Information Figure 1.
Procedure
The study procedure consisted of three main components, a screening visit, a one-day practice day, and a 14-day data collection period.
Part 1
The screening visit, lasting ~4 h, determined study eligibility. Participants completed fasting assessments of height, weight, and body composition, ate breakfast, and then completed interviews and questionnaires to assess eating pathology and psychological functioning. Following baseline assessments, eligible participants were trained on how to use the EMA device.
Part 2
Immediately following the screening visit, enrolled study participants completed an EMA practice period lasting 1 day. The practice day involved completing the EMA assessments in a manner consistent with the EMA training. In EMA research, participants often find the practice period to be helpful in clarifying the requirements of the protocol.22 If the participant was compliant with the procedure during the practice period (defined as responsiveness to the majority of random recordings and by demonstrating an understanding of protocol requirements), the data collection phase of the study was initiated. A second aim of the practice period was to attenuate any reactive effects of the self-monitoring.
Part 3
During the EMA data collection period, participants completed EMA recordings and met with the study team approximately one to two times per week to upload data and receive feedback regarding their compliance. At the end of the 2-week EMA assessment, participants returned their palm top computer and completed evaluation forms.
EMA Protocol
Self-monitoring of psychosocial variables was completed on a handheld palm top computer (Handspring Visor™) and downloaded using Satellite Forms™ 3.1 software. A combination of signal-contingent and event-contingent recordings was used to ensure comprehensive sampling of the target behavior, LOC eating, as well as other variables of interest (e.g., state affect, interpersonal problems). Signal-contingent recordings consisted of a series of questions primarily regarding interpersonal problems and state affect.
Participants were signaled by the palm top computer three to five times per day to complete signal-contingent reports. At these times, girls reported on their level of control over eating, interpersonal problems, and state affect. To ensure adequate sampling throughout the day, the entire sampling period (11:00–23:00) was stratified into five intervals. Signals were randomly distributed around target times of 11:10, 13:50, 16:30, 19:10, and 23:50, each occurring within one of the five intervals. Given the sample’s age, programming of the palm top computers was tailored to ensure that participants were not signaled during the school day. Therefore, girls were signaled only after 15:00 between Monday and Friday, resulting in three signals on weekdays. Prior work supports tailoring the signaling schedule in youth.17 Furthermore, LOC eating episodes typically occur after school hours in the afternoon and evening,15,23 suggesting that this approach would reasonably capture most LOC episodes. In determining the timing of the first EMA signal on weekends, the advantage of capturing a LOC episode or other relevant data prior to 10:50 was weighted against the potential burden of waking adolescents earlier than they prefer, in combination with data showing that most LOC episodes occur during afternoons and evenings.15,23 We therefore elected to begin the protocol between 10:50 and 11:30, surrounding an 11:10 anchor time. This signaling schedule, in which participants completed three recordings on weekdays and five on weekend days, was maintained throughout the summer for consistency.
Participants were also instructed to complete event-contingent recordings whenever the target behavior, eating, occurred. Consistent with the definition of an “eating episode” as explained to youth during administration of the EDE,24 “eating episodes” were systematically defined to participants as: “Any time of eating or drinking that you consider to be a meal or snack. If the food or drink was considered an ‘eating episode’ to you, we would like you to report on it.” Examples were provided systematically and in response to girls’ queries. Prior EMA studies suggest that participants were able to reliably report the target behavior of interest.22 Consistent with adult research regarding binge eating in the natural environment,22 adolescents were asked to make event-contingent reports before and after eating. Before-eating, adolescents reported their level of control over eating, interpersonal problems, state affect, and hunger. After eating, participants reported their level of LOC eating and state affect. Supporting Information Figure 2 depicts the questions presented to adolescents on the EMA device during each type of recording.
Measures
Baseline Measures
Anthropometrics
Physical assessments included girls’ height measured in triplicate to the nearest millimeter by an electronic stadiometer and weight measured to the nearest 0.1 kg by a digital scale. Body weight and the average of the three heights were used to calculate BMI. The Center for Disease Control and Prevention growth charts were used to convert BMI to BMI-Z scores.25 Total fat-free mass (kg) and percent body fat mass were assessed using air displacement plethysmography (Life Measurement Inc., Concord, CA).
Eating Pathology
The Eating Disorder Examination (EDE) version 14.024 was used to assess LOC episodes and DSM-IV-TR and DSM-5 eating disorders.26 The EDE has demonstrated excellent inter-rater reliability for identifying LOC eating episodes in adolescents.27
Psychopathology
Depressive symptoms were assessed using the Beck Depression Inventory, Second edition (BDI-II),28 a 21-item self-report measure that assesses depressive symptoms. Each response is assigned a score between zero and three, with total scores ranging from 0 to 63. If an adolescent met criteria for Major Depression, defined by a BDI score exceeding 29, she was excluded from study participation. The Schedule for Affective Disorders and Schizophrenia for School-Age Children (KSADS)29 was used to assess psychiatric status, including the presence of a major psychiatric disorder warranting study exclusion. The KSADS is a semistructured diagnostic interview with good inter-rater reliability that assesses a range of childhood and adolescent psychiatric diagnoses. If an adolescent met criteria for a major psychiatric disorder, she was excluded from study participation.
EMA Measures
Interpersonal Problems
The ‘Interpersonal Problems’ construct was developed from the Social Adjustment Scale, Self-Report (SAS-SR)30 which assesses interpersonal problems. The SAS-SR is a 23-item measure of social functioning in four domains: school, friends, family, and dating. Items queried included the extent to which the adolescent argued with someone, felt rejected, felt lonely, wished her relationships were better, and wished she had more friends. Participants provided ratings of each item on a 1–5 point Likert-type scale. The construct of interpersonal problems has been successfully adapted for EMA assessment in past research.31
Negative Affect
The Positive and Negative Affect Scale (PANAS),32 a 30-item self-report measure of positive and negative momentary affect, was used to assess state negative affect. The PANAS has good psychometric properties, demonstrating excellent internal consistency and acceptable convergent and discriminant validity.32 Since the PANAS is overly burdensome for EMA use, we administered the six items that loaded highest onto the negative affect factor, including upset, scared, miserable, lonely, blue, and sad. Participants provided ratings of the extent to which they felt each emotion on a 1–5 point Likert-type scale. The PANAS has been used extensively in EMA assessment as a brief, reliable and valid means of measuring momentary emotional states (e.g., Ref. [23]) and was used in the only prior EMA study in children with LOC eating.17
LOC Eating
To assess LOC eating in an EMA compatible format, relevant items from the EDE24 were adapted and used. For the purposes of the present study, the EMA-adapted questions allowed participants to rate the degree to which LOC was experienced on a 1–5 item Likert – type scale ranging from “No, not at all,” through “Yes, very much.” Specific items queried included the adolescent’s perceived “level of control,” “loss of control,” “ability to stop” and the sensation of “out of control.” Using a similar format, LOC eating has been successfully assessed in past EMA protocols.22
Data Analyses
Compliance with random recordings was calculated by dividing the number of random recordings completed within 1 h of stratified anchor times (e.g., 11 : 10, 13 : 50, 16 : 30, 19 : 10, 21 : 50) by the total number of possible random recordings. The time at which the adolescent completed an EMA report was determined based on the palm top time and date stamp. Respective composite scores constituting the primary dependent variables were calculated from five interpersonal items, six negative affect items, and three LOC eating items. Three LOC eating items, as opposed to four, were included because the internal reliability of the LOC composite scale was higher when the item “Did you feel like you were able to stop eating during the meal you just finished?” was excluded. Cronbach’s alpha values for the interpersonal, negative affect, and LOC eating composite scores were good,33 ranging between 0.89 and 0.93.
To conduct mediation analysis, three recordings, comprising an interpersonal problem rating (Time 1), a negative affect rating (Time 2), and a LOC eating rating (Time 3), were required to have been completed by the same participant across the same day. This requirement resulted in a significant reduction in the number observations available for model testing because girls began completing recordings after school and frequently completed only two recordings within a given day, or they completed more than two recordings but not in the order required to test mediation. Examination of individual Paths A–C, by contrast, required the presence of two recordings only: (1) Path A: interpersonal problems (Time 1) and negative affect (Time 2); (2) Path B: negative affect (Time 1) and LOC eating (Time 2); (3) Path C: interpersonal problems (Time 1) and LOC eating (Time 2). Weighing the advantage of maximizing the data available to conduct separate, more powerful tests of individual model paths over the advantage of maximizing parsimony by testing the model only once with fewer cases included, we conducted two sets of analyses. For individual tests of Paths A–C, we used all available pairs of recordings in which the independent variable preceded the dependent variable. Next, we reanalyzed individual paths to evaluate mediation using only the data comprising sets of three recordings that included an interpersonal problem rating at Time 1, a negative affect rating at Time 2, and an LOC eating rating at Time 3.
Mixed linear modelling (MLM) was conducted, with the within-subjects time variable (Level 1) nested within the between-subjects person variable (Level 2). We also examined three- level MLMs, with the time variable (Level 1, within-subjects) nested within day (Level 2, within subjects), nested within person (Level 3, between subjects). Time was coded continuously within each day (00:00–23:59). A limitation inherent in testing multilevel data and mediation using MLM is that MLM combines between- versus within-subjects effects, which, when used to examine mediation, may result in biased or inaccurate estimates if the between- and within-subjects effects differ.34 To address this limitation, participants’ mean level for each independent variable as well as a difference score (the difference between the participant’s mean and each assessment) was included. In the 3-level models, we included participants’ mean level for each independent variable; a difference score between participants’ overall mean and her daily average; and a difference score between the daily average and each momentary value. Significant within-subjects daily and momentary effects would signify temporal relationships between model constructs. For mediation, we used a 1 : 1 : 1 model, referring to the level of the independent variable, mediator, and dependent variable, respectively. For all models, a random (subject-specific) intercept and a variance components correlation structure were used. The need for random slopes for the primary independent variables was examined by evaluating model fit indices and testing the significance of the difference of the covariance estimate from zero. In all models, the level of the dependent variable at Time 1 was included in the model, as were relevant demographic variables. To examine whether effects were specific to weekdays or school days, we also controlled for type of day (weekday versus weekend; school day versus nonschool day). Notably, whether girls attended school on each day they participated in the study was not queried at the time participants completed recordings. Therefore, the variable pertaining to school day versus nonschool day was coded retrospectively by the research team using records of participants’ visit schedules in combination with calendars from participants’ school districts. When nonsignificant, covariates were removed from analyses. Since LOC eating was not queried except during after-meal recordings, a proxy for LOC eating, “Level of control,” was included as the Time 1 predictor in all analyses predicting LOC eating at Time 2. In all analyses, only random and before-meal recordings (but not after-meal recordings) were included as independent variables in prediction models of LOC eating. This approach was used in order to control for the potential impact of eating behavior on subsequent LOC eating. Similarly, in prediction models of negative affect, only nonmeal (but not before- or after-meal) recordings were included as independent variables, in order to control for the potential impact of eating on subsequent affective state. For mediation examining the indirect effect of interpersonal problems on LOC eating via negative affect, coefficients from Paths A and B were multiplied and tested for significance.35 Statistical Package for the Social Sciences (SPSS) version 22.036 was used.
Results
Participant Characteristics
Participants were 30 overweight and obese adolescent girls (60% African American, 26.7% Caucasian, 3.3% Hispanic, 10.0% Mixed Race), with a mean age of 14.92 (SD = 1.54, range = 12.25–17.35), mean BMI 36.13 (SD = 7.49, range = 24.98–50.72), and average percent adiposity of 22.20 (SD 7.50, range = 22.20–53.70). BDI-II scores ranged from 0 to 24, will a mean of 11.87 (SD = 6.08), reflective of mild depression. By design, no girl met criteria for full-syndrome major depressive disorder, as adolescents with clinically significant depression were excluded from participation. Based on the EDE interview, girls reported 7.4 (SD = 8.4, range = 2–39) LOC eating episodes in the month prior to assessment. About one-third (36.7%) of adolescents reported only subjective bulimic episodes, 30% reported only objective bulimic episodes, and the remainder (33.3%) reported both types of LOC episodes. The majority (n = 19, 63.3%) of adolescents reported at least four LOC episodes within the month prior to assessment, and about one-fourth (26.7%) of girls reported at least eight LOC episodes in the month prior to assessment. No adolescent met full criteria for either DSM-IV-TR or DSM-5 BED based on the requisite criteria of objective bulimic episodes. When considering LOC episodes in place of objectively large binge eating, one girl (3.3%) met DSM-IV-TR criteria and three adolescents (10.0%) met DSM-5 criteria for sub-threshold BED.
EMA Data
Data Screening
EMA data were examined for missing and incomplete recordings. Recordings were considered incomplete if any question was unanswered. Incomplete recordings (k = 34 out of 2,029 total recordings [1.7%]) were removed from the dataset. The dataset was examined for random recordings occurring within less than 10 min of previous random recordings, and these cases (n = 13) were removed from the dataset.
Compliance
Excluding one adolescent who contributed only four EMA recordings within 3 h due to technical problems, adolescents completed an average of 12.79 (SD = 2.30) days of EMA data collection. Each day, participants completed an average of 2.30 (SD = 0.52) random recordings, which produced an overall compliance rate of 69.4%. Compliance across participants ranged between 38% and 90%. Excluding four adolescents with compliance rates lower than 50%, compliance was 74.1%. Adolescents also completed 1.27 (SD = 0.69) before-meal recordings, and 1.17 (SD = 0.62) after meal recordings per day. Compliance was non-significantly higher on weekends (71.3%) compared to weekdays (67.9%, Fisher’s Exact Test p = 0.21) and during summers/holidays (72.3%) compared with non-summer/holidays (68.1%, Fisher’s Exact Test p = 0.11). While there was no main effect of time of day on adolescents’ compliance, examination of contrasts revealed a significant difference between adolescents’ compliance with the last recording of the day (74.1%, occurring between 21:30 and 22:10) compared with the evening recording (66.6%, occurring between 18:50 and 19:30, p(contrast) = .03).
Hypothesis Testing
Path A: Interpersonal Problems and Negative Affect
Six hundred forty-one nonmeal recordings that included an interpersonal problem rating preceded a random recording or before-meal recording that included a state affect rating. The average interval between measurement of interpersonal problems and state affect was 2:00:17. For Path A, AIC/BIC values suggested that the 2-level model was a better fit to the data than the 3-level model. Model fit indices and Type III tests of fixed effects suggested that time and day should be included as random, but not fixed, effects. The random intercept was non-significant in the final model (p = .51). Controlling for the impact of Time 1 negative affect (estimate = 0.41, p < .001), there was a significant effect of interpersonal problems on Time 2 negative affect at the between-subjects level (estimate = 0.09, p < .001, Supporting Information Table 1). However, the effect of within-subjects interpersonal problems was non-significant (p = .80). The pseudo R2 for the full model was 0.16, which is between a medium (R2 = 0.14) and a large (R2 = 0.40) effect size.37 Mixed model estimates of all random and fixed effects, standard errors (se), and p-values are presented in Supporting Information Table 1.
Path B: Negative Affect and LOC Eating
To test the impact of negative affect on LOC eating, 426 after-meal recordings that included an LOC rating (Time 2) were preceded by a nonmeal recording that included a state affect rating (Time 1), separated by an average of 28:37. Examination of model fit indices suggested that the two-level model was superior to the three-level model. Model fit indices and the significant and marginal estimates of covariance parameters for the random effects of time (p = .007) and date (p = .08) suggested inclusion of these variables as random effects. Time and day were excluded as fixed effects based on model fit indices. The random intercept was not estimable in the final model. Controlling for level of control over eating at time 1 (estimate = −0.10, p < .01), neither between- (estimate = 1.21, p = .12) nor within-subjects (estimate = 0.33, p = .32) negative affect significantly predicted LOC eating. However, the between-subjects effect was in the expected direction, such that adolescents with higher negative affect were nonsignificantly more likely to report LOC eating. All estimates, standard errors (se), and p-values are reported in Supporting Information Table 1. The model pseudo R2 was (0.13), constituting a small effect size.37
Path C: Interpersonal Problems and LOC Eating
Four hundred twenty-six nonmeal or premeal recordings that included an interpersonal problem rating were preceded by after-meal recordings that included an LOC eating rating, separated by 28:37. For Path C, model fit indices suggested that the two-level model with random, but not fixed, effects of time and day was the best fit to the data. The random intercept was not estimable in the final model. There were significant effects of Time 1 between- (estimate = 0.30, p = .04) and within- (estimate = 0.14, p = .05) subjects interpersonal problems on Time 2 LOC eating, controlling for Time 1 level of control over eating (estimate = −0.10, p = .01, Supporting Information Table 1). The pseudo R2 for the full model was 0.14.
Indirect Path A × B: Exploratory Effect of Mediation by Negative Affect
One hundred and eighty-four sets of recordings comprised an interpersonal problem rating, followed by a state affect rating, followed by an LOC eating rating. When individual paths were examined, effects observed in prior models were attenuated due to the loss of power incurred by including only 183 observations. The only significant effect was the impact of time 1 between-subjects interpersonal problems on negative affect (estimate = 0.04, p = .02), controlling for time 1 negative affect (estimate = 0.63, p < .001). There were no significant effects of interpersonal problems on LOC eating at the between- (p = .14) or within- (p = .22) subjects levels, controlling for level of control over eating at time 1. Similarly, there were no significant effects of negative affect on LOC eating at the between- or within-subjects levels (p’s > .46). In light of these findings, mediation was not tested.
Discussion
This study used a naturalistic design to investigate the links proposed in the interpersonal model of LOC eating in overweight adolescent girls. Findings supported significant relationships between interpersonal problems and LOC eating at the between- and within- subjects levels. In addition, findings at the between-subjects level suggested that adolescents with higher interpersonal problems had greater momentary negative affect. Although the effect size for negative affect was approximately equivalent to that for interpersonal problems, results did not support a significant effect of negative affect on LOC eating at either the between- or within-subjects levels; however, the between-subjects effect was in the expected direction such that adolescents with greater negative mood reported higher LOC.
Overall, study data support the hypothesis that interpersonal problems predict LOC eating among adolescent girls. These findings are consistent with past self-report studies documenting prospective associations between interpersonal problems and LOC eating12,13 and extend current literature in several important ways. First, the use of multiple momentary observations facilitated examination of between- versus within- subjects effects of interpersonal problems on LOC eating. Our findings demonstrate that the mechanism underlying the association between interpersonal problems and LOC eating may be twofold: first, individuals with higher interpersonal problems are more likely to experience LOC eating, and second, across participants, times when adolescents experience high interpersonal problems, compared with times when low levels of interpersonal problems are experienced, are more likely to be followed by LOC eating. This dual effect is worth exploring in studies with greater power to detect whether overall interpersonal problem severity moderates the momentary impact of interpersonal problems on LOC eating. It is possible that repeated episodes of binge or LOC eating in response to interpersonal problems worsen both interpersonal distress and LOC eating.
Results also add to an extensive literature regarding the relationship between negative affect and LOC eating by contributing momentary data among adolescents. A significant relationship between negative affect and LOC at the between-subjects level would suggest that girls with higher negative affect have greater LOC eating in the natural environment. This effect was in the expected direction, but nonsignificant. By study design, our finding may be impacted by insufficient statistical power, or may stem from deficits in our chosen measure of negative affect, the PANAS, to detect emotional states contributing to aberrant eating behavior among youth. The PANAS assesses such emotional states as sad, scared, and other emotions of high negative valence but does not capture more subtle perturbations in emotional state such as anxiety, guilt, irritability, or agitation, which may be likely to contribute to LOC among adolescents. Our findings may also reflect a true absence of an impact of negative affect on LOC eating among adolescents, which is consistent with a prior EMA study among children ages 8–13.17 Notably, our findings are in contrast to laboratory data among adolescents with LOC16 that support a predictive role of negative affect in eating behavior at the between-subjects level. Furthermore, findings at the within-subjects level did not suggest that negative affect contributed to momentary LOC eating, in contrast to adult EMA data describing that momentary negative mood does predict binge episodes among adults with BED.38
Consistent with the notion that adolescence is a developmental stage during which interpersonal relationships are highly valued, particularly among girls,39 interpersonal problems may be a more robust predictor of aberrant eating among adolescents than negative affect. Few adult studies have examined the impact of interpersonal problems on LOC eating, however, a laboratory study among youth demonstrated that 8–13 year old children’s intake during an ad libitum snack period (which followed a standard meal) was positively associated with parental weight-related criticism during the meal.40 It is possible that the relationships among interpersonal problems, negative affect, and LOC eating may shift over the course of development. Specifically, children and those with sub-clinical, infrequent eating pathology may be less likely to identify links between affective states and LOC, whereas adults and individuals with full-syndrome BED may be more likely to draw connections between LOC episodes and negative affect. Interpersonal problems, comprising objective, concrete, observable events may be more developmentally salient and therefore easier for adolescents to identify and report, as compared with emotional states, which are typically subjective, abstract, and require insight and reflection abilities that improve as youth mature cognitively and emotionally.
A potential moderating variable between negative affect and LOC is alexithymia, defined as difficulty identifying and reporting one’s emotional state and having a concrete and externally oriented thinking style. Interpersonal problems may be identifiable among all adolescents with LOC eating by virtue of their developmental salience, whereas only those with low levels of alexithymia may be able to readily report on their state affect in the natural environment. In one study examining alexithymia among LOC youth, those with the most severe type of interpersonal problems, interpersonal deficits (22%), had greater levels of alexithymia compared to adolescents with other interpersonal problem types.41 Therefore, it is conceivable that adolescent girls with the most severe interpersonal problems may have the greatest difficulty reporting on their negative mood states. Current data suggest that the severity of adolescents’ interpersonal problems is associated with LOC eating severity. Additional research is needed to elucidate the potential moderating role of alexithymia among constructs involved in the interpersonal model. Objective psychophysiological measurements that signal the presence of negative affect may be helpful by providing an alternative inroad to adolescents’ emotional states.
While the compliance rate among adolescents in the current study was only 69.4%, this is comparable to rates observed in prior childhood EMA studies of binge and LOC eating.17,42 Notably, these rates are lower than those reported in an adult studies of binge eating disorder, in which higher compliance (93%) was reported.38 Observed differences between compliance rates in pediatric and adult samples may reflect youth’s relative cognitive immaturity or lack of control over their schedules compared to adults. Indeed, the normative developmental course of complex cognitive processes associated with prefrontal cortical maturity impacting executive function continues through late adolescence into early adulthood.43 Executive functioning may relate to compliance via its impact on planning ability, organization, and prioritizing multiple tasks. Further, whereas most adults may bring their EMA device wherever they travel throughout the day, youth are more likely to be restricted by external environmental requirements such as school rules. Trend level data from our study suggested that adolescents were more likely to comply with event-contingent recordings during the summer, holidays, and weekends compared to school-days. They were also significantly more compliant with the last recording of the day compared with the evening recording, potentially representing the time when they are least likely to be involved in other activities. Adolescents in the current study commonly cited “not having the device with me” as the most common reason for missing recordings, and many teens indicated that they could not respond to the device while at school or after school activities.
Strengths of the study include the racially- and ethnically diverse sample comprised of adolescents reporting sub-clinical eating pathology; the use of interview methodology to assess LOC eating and psychiatric functioning; and the use of EMA for measuring state mood and behavior in the natural environment over an extended sampling period of 2 weeks, intended to improve generalizability from laboratory settings. Limitations include sample homogeneity; we restricted the sample to overweight adolescent girls because girls are thought to be more sensitive to interpersonal distress compared to boys,44 and because being overweight,45 and female1 are both associated with increased likelihood of reporting LOC eating during adolescence. As a result, inferences regarding application of the interpersonal model to nonoverweight adolescents and boys cannot be made. Furthermore, the size of our sample, while ideal for a pilot study aimed to examine feasibility, was not adequately powered to examine mediation. Replication of the current findings within larger samples of adolescents will inform the generalizability of results and will provide greater information regarding the potential interplay between interpersonal problems and negative affect in producing LOC eating.
For feasibility reasons, adolescents were not queried about their experiences during the school day, a shortcoming that is mitigated by data suggesting that LOC episodes generally occur after school hours.15,23 However, interpersonal events and mood changes are likely to occur during school and these shifts were not able to be captured. As a result, the impact of interpersonal and affective factors on adolescents’ LOC eating behavior during school cannot be inferred from the current results. It is possible that factors differing between school and nonschool settings, such as food accessibility, may promote varying responses to interpersonal and affective stressors at school versus at home. However, inclusion of day type in model testing revealed no evidence to suggest that day type significantly influenced the impact of interpersonal and affective predictors on LOC eating, suggesting that the findings are generalizable across days. Finally, this study did not address factors related to adolescents’ eating episodes including the amount and types of foods consumed. Such information would aid in understanding the mechanisms by which LOC eating promotes excess weight gain1 and metabolic problems.3 Laboratory data suggest that the meal composition of youth with LOC eating may be comprised of a greater proportion of energy dense, palatable foods.46 While the amount and type of food consumed are not primary facets of the interpersonal model, they may be important to explore in the future.
This study examined interpersonal and affective predictors of LOC eating in the natural environment in overweight adolescent girls with LOC eating. Interpersonal problems appear to be predictive of LOC eating among overweight adolescent girls on individual and momentary levels. Differentiating the contributions of individual versus momentary level interpersonal problems has important intervention implications. Whereas the former implicates targeting teens who experience overall high interpersonal problems, the latter suggests helping adolescents with LOC evaluate and target the impact of interpersonal problems on LOC eating in the moment. Among adults with BED, interpersonal psychotherapy has been found to effectively reduce binge eating in the short- and long-term.47 Among adolescents girls, preliminary evidence from a pilot study suggested that interpersonal psychotherapy may be effective in reducing LOC eating episodes.4 Tailoring the approach of interpersonal psychotherapy to the temporal mechanism by which interpersonal problems impact LOC eating (e.g., individual-level, daily, and momentary) may aid in improving intervention effectiveness.
In conclusion, our results elucidate predictors of LOC eating in the natural environment during the key developmental phase of adolescence, an area that has not been thoroughly researched, to date. Our findings suggest that adolescents may be better at reporting on concrete interpersonal events as compared to internal emotional experiences in the natural environment. When comparing our findings to those of childhood and adult studies, it is possible that predictors of LOC may be impacted by chronological age or severity of eating pathology. Moreover, this study elucidates the potential utility of interpersonal factors as an intervention target among adolescents with LOC. Future research might further investigate specific interpersonal problem types and their relative impact on LOC eating among youth.
Supplementary Material
FIGURE 1.
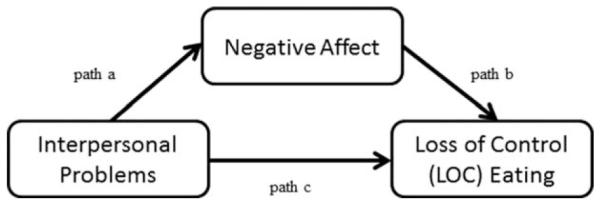
Interpersonal model of Loss of Control (LOC) eating. The interpersonal model posits that interpersonal problems precede and predict negative affect, which in turn precedes and predicts LOC eating. Negative affect is thought to serve as a mediating variable between interpersonal problems and LOC eating.
Acknowledgments
Supported by 5F31MH095348 from NIMH, by 1R01DK08090601A1 from NIDDK and by R072IC from USUHS.
Footnotes
Additional Supporting Information may be found in the online version of this article.
References
- 1.Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatrics. 2013;167:149–155. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120:108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, Dellavalle D, et al. Children’s binge eating and development of metabolic syndrome. Int J Obes (Lond) 2012;36:956–962. doi: 10.1038/ijo.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, et al. Preventing excessive weight gain in adolescents: Interpersonal psychotherapy for binge eating. Obesity (Silver Spring) 2007;15:1345–1355. doi: 10.1038/oby.2007.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan HS. The Interpersonal Theory of Psychiatry. Norton; New York: 1953. [Google Scholar]
- 6.Bowlby J. Attachment and Loss: Separation. Basic Books; New York: 1973. [Google Scholar]
- 7.Elliott CA, Tanofsky-Kraff M, Mirza NM. Parent report of binge eating in Hispanic, African American and Caucasian youth. Eat Behav. 2013;14:1–6. doi: 10.1016/j.eatbeh.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suisman JL, Slane JD, Burt SA, Klump KL. Negative affect as a mediator of the relationship between weight-based teasing and binge eating in adolescent girls. Eat Behav. 2008;9:493–496. doi: 10.1016/j.eatbeh.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brendgen M, Lamarche V, Wanner B, Vitaro F. Links between friendship relations and early adolescents’ trajectories of depressed mood. Dev Psychol. 2010;46:491–501. doi: 10.1037/a0017413. [DOI] [PubMed] [Google Scholar]
- 10.Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, Wilfley DE. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obes Res. 2005;13:1381–1392. doi: 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- 11.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 12.Neumark-Sztainer D, Wall MM, Haines JI, Story MT, Sherwood NE, van den Berg PA. Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Preventitive Med. 2007;33:359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 13.Hilbert A, Hartmann AS, Czaja J, Schoebi D. Natural course of preadolescent loss of control eating. J Abnorm Psychol. 2013;122:684–693. doi: 10.1037/a0033330. [DOI] [PubMed] [Google Scholar]
- 14.Goldschmidt AB, Wall MM, Loth KA, Bucchianeri MM, Neumark-Sztainer D. The course of binge eating from adolescence to young adulthood. Health Psychol. 2014;33:457–460. doi: 10.1037/a0033508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, et al. A multisite investigation of binge eating behaviors in children and adolescents. J Consulting Clin Psychol. 2007;75:901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ranzenhofer LM, Hannallah L, Field SE, Shomaker LB, Stephens M, Sbrocco T, et al. Pre-meal affective state and laboratory test meal intake in adolescent girls with loss of control eating. Appetite. 2013;68:30–37. doi: 10.1016/j.appet.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, Czaja J. Loss of control eating and psychological maintenance in children: An ecological momentary assessment study. Behav Res Ther. 2009;47:26–33. doi: 10.1016/j.brat.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ansell EB, Grilo CM, White MA. Examining the interpersonal model of binge eating and loss of control over eating in women. Int J Eat Disord. 2012;45:43–50. doi: 10.1002/eat.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, et al. An examination of the interpersonal model of loss of control eating in children and adolescents. Behav Res Ther. 2010;48:424–428. doi: 10.1016/j.brat.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engel SG, Kahler KA, Lystad CM, Crosby RD, Simonich HK, Wonderlich SA, et al. Eating behavior in obese BED, obese non-BED, and non-obese control participants: A naturalistic study. Behav Res Ther. 2009;47:897–900. doi: 10.1016/j.brat.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 23.Smyth J, Wonderlich S, Heron KE, Sliwinski MJ, Crosby R, Engel SG, et al. Ecological momentary assessment of affect, stress, and binge-purge behaviors: Day of week and time of day effects in the natural environment. Int J Eat Disord. 2008;42:429–436. doi: 10.1002/eat.20623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fairburn CG, Cooper Z, editors. The Eating Disorder Examination. 12th Guilford Press; New York: 1993. [Google Scholar]
- 25.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 26.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th. American Psychiatric Association; Washington, DC: 2000. test revision (DSM-IV-TR) [Google Scholar]
- 27.Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim KR, Mirch MC, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol. 2007;32:95–105. doi: 10.1093/jpepsy/jsl012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- 29.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 31.Miller PJ, Niehuis S, Huston TL. Positive illusions in marital relationships: A 13-year longitudinal study. Pers Soc Psychol Bull. 2006;32:1579–1594. doi: 10.1177/0146167206292691. [DOI] [PubMed] [Google Scholar]
- 32.Laurent J, Catanzaro SJ, Joiner TE, Rudolph KD, Potter KI, Lambert S, et al. A measure of positive and negative affect for children: Scale development and preliminary validation. Psychol Assess. 1999;11:326–338. [Google Scholar]
- 33.Cortina J. What is coefficient alpha? An examination of theory and applications. J Appl Psychol. 1993;78:98–104. [Google Scholar]
- 34.Zhang Z, Zyphur MJ, Preacher KJ. Testing multilevel mediation using hierarchical linear models: Problems and solutions. Organizational Res Methods. 2009;12:95–719. [Google Scholar]
- 35.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- 36.IBM Corp . IBM SPSS Statistics for Windows. 20.0 IBM Corp; Armonk, NY: 2011. [Google Scholar]
- 37.Cohen J. Statistical Power for the Behavioral Sciences. Erlbaum; Hillsdale,NJ: 1988. [Google Scholar]
- 38.Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder? A prospective examination of precursors and consequences. Int J Eat Disord. 2007;40:195–203. doi: 10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- 39.Furman W, Buhrmester D. Age and sex differences in perceptions of networks of personal relationships. Child Dev. 1992;63:103–115. doi: 10.1111/j.1467-8624.1992.tb03599.x. [DOI] [PubMed] [Google Scholar]
- 40.Hilbert A, Tuschen-Caffier B, Czaja J. Eating behavior and familial interactions of children with loss of control eating: A laboratory test meal study. Am J Clin Nutr. 2010;91:510–518. doi: 10.3945/ajcn.2009.28843. [DOI] [PubMed] [Google Scholar]
- 41.Berger SS, Elliott C, Ranzenhofer LM, Shomaker LB, Hannallah L, Field SE, et al. Interpersonal problem areas and alexithymia in adolescent girls with loss of control eating. Comprehensive Psychiatry. 2014;55:170–178. doi: 10.1016/j.comppsych.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grenard JL, Stacy AW, Shiffman S, Baraldi AN, Mackinnon DP, Lockhart G, et al. Sweetened drink and snacking cues in adolescents. A study using ecological momentary assessment. Appetite C. 2013;67:61–73. doi: 10.1016/j.appet.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson VA, Anderson P, Northam E, Jacobs R, Catroppa C. Development of executive functions through late childhood and adolescence in an Australian sample. Dev Neuropsychol. 2001;20:385–406. doi: 10.1207/S15326942DN2001_5. [DOI] [PubMed] [Google Scholar]
- 44.Stroud LR, Salovey P, Epel ES. Sex differences in stress responses: Social rejection versus achievement stress. Biol Psychiatry. 2002;52:318–327. doi: 10.1016/s0006-3223(02)01333-1. [DOI] [PubMed] [Google Scholar]
- 45.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: Implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156:171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- 46.Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, et al. Laboratory assessment of the food intake of children and adolescents with loss of control eating. Am J Clin Nutr. 2009;89:738–745. doi: 10.3945/ajcn.2008.26886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kass AE, Kolko RP, Wilfley DE. Psychological treatments for eating disorders. Curr Opin Psychiatry. 2013;26:549–555. doi: 10.1097/YCO.0b013e328365a30e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


