Abstract
Background
The association of overall diet, as characterized by dietary patterns, with risk of incident acute coronary heart disease (CHD) has not been studied extensively in samples including sociodemographic and regional diversity.
Methods and Results
We used data from 17,418 participants in Reasons for Geographic and Racial Differences in Stroke (REGARDS), a national, population-based, longitudinal study of white and black adults aged ≥45 years, enrolled from 2003-2007. We derived dietary patterns with factor analysis, and used Cox proportional hazards regression to examine hazard of incident acute CHD events – nonfatal myocardial infarction and acute CHD death – associated with quartiles of consumption of each pattern, adjusted for various levels of covariates. Five primary dietary patterns emerged: Convenience, Plant-based, Sweets, Southern, and Alcohol and Salad. A total of 536 acute CHD events occurred over a median (IQR) 5.8 (2.1) years of follow-up. After adjustment for sociodemographics, lifestyle factors, and energy intake, highest consumers of the Southern pattern (characterized by added fats, fried food, eggs, organ and processed meats, and sugar-sweetened beverages) experienced a 56% higher hazard of acute CHD (comparing quartile 4 to quartile 1: HR = 1.56; 95% CI: 1.17, 2.08; P for trend across quartiles = 0.003). Adding anthropometric and medical history variables to the model attenuated the association somewhat (HR = 1.37; 95% CI: 1.01, 1.85; P = 0.036).
Conclusions
A dietary pattern characteristic of the southern US was associated with greater hazard of CHD in this sample of white and black adults in diverse regions of the US.
Keywords: coronary disease, diet, epidemiology, follow-up studies, nutrition
Although coronary heart disease (CHD) mortality decreased 36% in the US between 1999-2001 and 2008-2010, CHD still was responsible for 1 of every 6 deaths in the US in 2010 – nearly 380,000 in total1. Documented risk factors for CHD include dyslipidemia, diabetes mellitus, hypertension, overweight/obesity, cigarette smoking, and physical inactivity2. Observational and intervention studies provide evidence that diet also influences the development of CHD, likely through its effects on several of these key risk factors3.
While individual foods and nutrients (e.g., red meat and saturated fat) have been studied extensively in relation to CHD risk4, the relationship between overall diet and CHD risk may be more informative because foods typically are eaten in combination, not in isolation5. Empirically deriving dietary patterns a posteriori with cluster or factor analysis has facilitated investigations into the role overall diet may play in the etiology of chronic diseases6,7. Factor analysis, a data-driven exploratory method, assesses eating patterns in specified groups without preconceived judgments about which foods commonly are consumed together. Factor analysis has been used in previous studies to derive dietary patterns which subsequently were related to CHD risk8-16. However, studies examining associations among a posteriori-derived dietary patterns and CHD risk in a large US population sample including sociodemographic and regional diversity are lacking.
Reasons for Geographic and Racial Differences in Stroke (REGARDS) is a large cohort study designed to identify factors which increase the risk of stroke in blacks and persons residing in the southern US17. REGARDS includes a regionally and socioeconomically diverse population sample, with approximately equal numbers of men and women and a high proportion of black participants. REGARDS included a comprehensive assessment of diet, sociodemographic factors, and anthropometric measures at the baseline examination. Dietary patterns previously have been derived in the REGARDS cohort and related to incidence of stroke and mortality from end-stage renal disease18,19. The ongoing REGARDS-Myocardial Infarction (REGARDS-MI) study includes rigorous ascertainment of acute CHD outcomes. We tested the hypothesis that dietary patterns derived empirically using factor analysis were associated with hazard of incident acute CHD in REGARDS participants free of CHD at baseline.
Methods
Study Population
Details on the design and methods of REGARDS have been published17. Briefly, REGARDS is a national, population-based, longitudinal cohort of 30,239 community-dwelling black and white women and men aged 45 years or older, recruited from 2003-2007 via mail and telephone using commercially available lists of US residents. REGARDS used the same lists to contact potential participants as the Behavioral Risk Factor Surveillance System (BRFSS), and the demographics of REGARDS mirror those of BRFSS. The telephone response (those answering the phone) was 33% and cooperation (those answering the phone who agreed to participate) was 49%, similar to that of other cohort studies20,21. For this analysis, we included only those without a history of CHD (n=24,297). The sampling scheme included 30% of participants from the stroke belt (North Carolina, South Carolina, Georgia, Tennessee, Alabama, Mississippi, Arkansas, and Louisiana), 20% from the stroke buckle (the coastal plain of North Carolina, South Carolina, and Georgia), and 50% from elsewhere in the continental US. The baseline cohort was 42% black and 55% women.
Criteria for inclusion in the sample included having a name, telephone number, and address in the commercially available nationwide database from which the sample was selected, and age ≥45 years. Exclusion criteria included race other than white or black, active treatment for cancer, chronic medical conditions precluding long-term participation, cognitive impairment, current or impending residence in a nursing home, or inability to communicate in English. An initial telephone interview was used to survey participants and establish eligibility. Following verbal consent, demographic information and medical history (including risk factor evaluation) was collected by computer assisted telephone interviewing. Race was self-classified by participants using the following options defined by the investigators: white, black or African American, Asian, Native Hawaiian or other Pacific Islander, and American Indian or Alaska Native. Race was assessed in REGARDS because blacks have the highest disparity in stroke mortality compared to other race/ethnic groups. An in-home examination then was conducted to perform various physical measurements, medication inventory, phlebotomy, and urine collection among those eligible. Written informed consent was obtained from all participants, and the study was approved by the institutional review boards at all participating institutions.
Dietary Assessment
Diet was assessed with the Block 98 food frequency questionnaire (FFQ), a validated semi-quantitative FFQ that assessed usual dietary intake of 110 food items (NutritionQuest, Berkeley, CA)22,23. For each line item on the FFQ, participants were asked how often, on average, they consumed the food (or group of foods) during the previous year. Participants selected from nine possible frequencies ranging from “never” to “every day.” For each item on the FFQ, the quantity of the food consumed also was recorded. For unitary items (i.e., eggs or slices of bacon), the usual number consumed each time the food was eaten was queried (1, 2, 3, or 4). For non-unitary foods, a photo was provided to participants to aid in estimating usual portions for foods served on plates (1/4, 1/2, 1, or 2 cups) and three different usual portions for foods served in bowls (1/2, 1, or 2 cups). The FFQ included adjustment questions (e.g., inquiring about the type of milk consumed – low-fat, non-fat, etc.).
The FFQ was self-administered by participants after the in-home visit and mailed to the REGARDS Operations Center, where they were checked for completeness and scanned. Scanned FFQ files were forwarded to NutritionQuest for processing and analysis. Amounts of each food on the FFQ consumed by a participant were calculated by multiplying the frequency of consumption of that food by the usual amount consumed.
Food Groups
The methods for constructing food groups and deriving dietary patterns in REGARDS have been described elsewhere24. Briefly, we constructed food groups using the original 110 individual food variables on the FFQ, based on culinary use and nutrient similarities, as well as a review of previous studies. When an item could be considered for multiple categories, we considered the nutritional content and/or cooking method of the item as well as the use of the item. For example, one line item was “beverages containing some juice like Hi-C.” We grouped this item with sugar-sweetened beverages due to nutritional content (i.e., added sugar). We created separate groups to differentiate more and less healthy alternatives for similar foods, such as low-fat and high-fat dairy. When we considered potatoes, fish, and chicken, we separated the fried items from the non-fried items due to the higher fat content of fried foods and expected differences of use across populations. Some items, such as “Chinese food,” were left as stand-alone food groups due to the uniqueness of the items. Additionally, we created multiple categories of vegetables (cruciferous, dark yellow, green leafy, tomato, and other) to preserve regional variability in vegetable intake. Finally, we kept coffee and tea in separate groups as the two often are consumed in different manners across the US. Initially, this resulted in 58 food groups, but evaluation of communality and zero values identified two groups for elimination: the diet shakes/meal replacement variable was excluded, and breakfast/power bars were moved into the sweet breakfast foods group. This resulted in 56 final food groups on which dietary patterns were based.
Dietary Patterns
We used split sample replication to 1) derive the dietary patterns using exploratory factor analysis, and 2) test the patterns using confirmatory factor analysis25. We conducted three separate analyses: by sex (male/female), race (black/white), and region (southeastern US stroke belt/non-belt), and coefficients of congruence were determined for each stratification pair. The coefficient of congruence is used in multivariate statistics to test the similarity of factors across groups (in this case sex, race, and region)24,26. The final number of factors retained was chosen based on the eigenvalue (scree plot) and the solution providing the optimal congruence across sex, race, and region. As congruence between sex, race, and region was high, we calculated final factor loadings using factor analysis with varimax rotation of five factors on the full sample (Table 1). For simplicity, we are presenting only those factors with loadings greater than 0.15, in agreement with previous studies5,6; however, all food groups were used in calculating the final score, regardless of loading. We named patterns based on the factor loadings that contributed most highly to each pattern. Factor 1 loaded heavily on mixed dishes, pasta dishes, pizza, Mexican food, and Chinese food and was designated the “Convenience” pattern. Factor 2 had high factor loadings for vegetables, fruits, fruit juice, cereal, beans, fish, poultry, and yogurt and was named the “Plant-based” pattern. Factor 3 loaded on added sugars, desserts, chocolate, candy, and sweetened breakfast foods and was named the “Sweets” pattern. Factor 4 loaded heavily on added fats, fried food, eggs and egg dishes, organ meats, processed meats, and sugar-sweetened beverages. This diet reflected a culinary pattern observed in the southeastern US and was named the “Southern” pattern. Factor 5 loaded highly on beer, wine, liquor, green leafy vegetables, tomatoes, and salad dressing. Accordingly, we named it the “Alcohol and Salad” pattern.
Table 1. Final Factor Loadings Derived from 17,418 Participants in the REGARDS Cohort (Only Factor Loadings with an Absolute Value >0.15 Are Shown).
| Food Group | Dietary Patterns | ||||
|---|---|---|---|---|---|
|
| |||||
| Convenience | Plant-based | Sweets | Southern | Alcohol and Salads | |
| Beans | 0.36 | 0.38 | |||
| Beer | -0.16 | 0.23 | |||
| Bread | 0.47 | 0.37 | |||
| Bread – whole grain | 0.30 | 0.18 | |||
| Butter | 0.17 | 0.32 | |||
| Candy | 0.40 | ||||
| Cereal | 0.38 | -0.20 | |||
| Cereal – high-fiber | 0.24 | -0.25 | |||
| Chinese food | 0.44 | ||||
| Chocolate | 0.46 | ||||
| Coffee | 0.22 | -0.16 | 0.30 | ||
| Condiments | 0.25 | 0.31 | 0.29 | ||
| Desserts | 0.20 | 0.53 | -0.17 | ||
| Dairy – high-fat | 0.18 | 0.37 | 0.21 | ||
| Dairy – low-fat | 0.20 | -0.19 | |||
| Eggs and egg dishes | 0.42 | 0.29 | |||
| Fats – added | 0.40 | 0.38 | 0.25 | ||
| Fish | 0.27 | 0.38 | 0.21 | ||
| Fried food | 0.24 | 0.56 | |||
| Fruit juice – 100% | 0.25 | 0.17 | -0.17 | ||
| Fruits | 0.58 | ||||
| Grains – refined | 0.31 | 0.17 | 0.20 | 0.20 | |
| Liquor | 0.31 | ||||
| Margarine | 0.37 | ||||
| Meat – organ | 0.17 | 0.47 | |||
| Meat – processed | 0.25 | 0.26 | 0.45 | 0.22 | |
| Meat – red | 0.45 | 0.18 | 0.26 | 0.26 | |
| Mexican food | 0.48 | ||||
| Milk alternatives | 0.18 | ||||
| Milk – high-fat | 0.18 | 0.24 | |||
| Milk – low-fat | 0.16 | -0.42 | |||
| Mixed dishes with meat | 0.61 | ||||
| Pasta dishes | 0.59 | 0.17 | |||
| Pizza | 0.45 | -0.18 | 0.20 | ||
| Potatoes | 0.36 | 0.26 | |||
| Potatoes – fried | 0.37 | 0.28 | 0.16 | ||
| Poultry | 0.29 | 0.31 | |||
| Salad dressing/sauces | 0.30 | 0.55 | |||
| Salty snacks | 0.32 | 0.30 | |||
| Seeds, nuts | 0.26 | 0.19 | 0.19 | ||
| Shell fish | 0.28 | 0.23 | 0.24 | ||
| Soda | -0.23 | 0.24 | |||
| Soup | 0.44 | 0.32 | |||
| Sugar – miscellaneous | 0.54 | 0.19 | |||
| Sugar-sweetened beverages | 0.37 | -0.15 | |||
| Sweet breakfast foods | 0.19 | 0.39 | |||
| Tea | 0.31 | ||||
| Vegetable mixed dishes | 0.35 | 0.31 | -0.25 | ||
| Vegetables – cruciferous | 0.59 | ||||
| Vegetables – dark yellow | 0.41 | -0.17 | |||
| Vegetables – green leafy | 0.16 | 0.49 | -0.22 | 0.48 | |
| Vegetables – other | 0.48 | ||||
| Vegetables – tomato | 0.32 | 0.27 | |||
| Water | 0.32 | ||||
| Wine | 0.36 | ||||
| Yogurt | 0.31 | -0.25 | |||
Outcome Ascertainment
We defined incident acute CHD as nonfatal MI or acute CHD death in participants free of CHD at baseline. Incident cases of CHD were captured by participant report and adjudicated by physician adjudicators with appropriate expertise. Participants were contacted by telephone every six months to assess vital status. If a suspected heart event was reported, medical records were pursued. MIs were adjudicated based on the presence of signs or symptoms suggestive of ischemia; diagnostic cardiac enzymes (rising and/or falling pattern in cardiac troponin or creatine phosphokinase-MB isoenzyme concentrations over six or more hours with a peak concentration greater than twice the upper limit of normal); and electrocardiogram changes consistent with ischemia or MI, guided by the Minnesota Code and classified as evolving diagnostic, positive, nonspecific, or not consistent with ischemia27. In the case where a participant died outside of the hospital, interviews with family members or other proxies, proximal hospitalizations, baseline medical history, death certificates, and the National Death Index were used to identify CHD as the underlying cause of death.
Statistical Analysis
Of the participants free from CHD at baseline (n=24,297), we excluded those who were missing FFQ data altogether, had more than 15% missing data on the FFQ, or had implausible reported energy intakes (<800 or >5000 kcal/d in men and <500 or >4500 kcal/d in women). This resulted in a final sample of 17,418 (71.7% of the sample free of CHD at baseline). We grouped consumption of the five dietary patterns into quartiles, with quartile 1 representing the lowest consumption of each pattern and quartile 4 representing the highest consumption of the pattern. We calculated descriptive statistics (including proportions and measures of central tendency) for demographic, socioeconomic, lifestyle, anthropometric, medical history, and nutrient variables at the baseline assessment according to these quartiles using the chi-square test (for proportions) and analysis of variance (for continuous variables). We used Cox proportional hazards regression to examine the hazard of incident acute CHD associated with consumption of each of the five dietary patterns, using the lowest quartile of consumption (quartile 1) as the referent quartile throughout. Years since study entry was the time metric, with participants censored at the date of incident CHD, date of withdrawal from the study, date of death, or December 31, 2013, whichever came first. We examined Schoenfeld residuals and confirmed that proportional hazards assumptions were met. We built models sequentially by first adding demographic variables (age, sex, race, age-race interaction) (model 1); model 1 plus socioeconomic factors (education, household income) and region (model 2); model 2 plus total energy intake (model 3); model 3 plus lifestyle factors (smoking, physical activity) (model 4); and model 4 plus anthropometric measures (body mass index (BMI), waist circumference) and medical history (hypertension, dyslipidemia, diabetes) (model 5). We performed analyses using SAS statistical software, version 9.3 (SAS Institute, Cary, NC).
Results
The 17,418 REGARDS participants included in this analysis included 59% who were women, 35% who were black, and 56% who were residents of the stroke belt. Demographic, socioeconomic, lifestyle, anthropometric, and medical history characteristics by quartile of consumption of each dietary pattern are provided in Table 2. Compared to participants with a lower consumption of the Southern dietary pattern, participants with a higher consumption of the Southern pattern were less likely to be older than 65 years and more likely to be male, black, a non-high school graduate with an annual household income of <$20,000, and a resident of the stroke belt. Greater consumption of the Southern pattern also was associated with a higher likelihood of smoking, a lower likelihood of being physically active, and higher mean BMI and waist circumference compared to lower consumption. Finally, greater consumption of the Southern pattern was associated with a higher prevalence of hypertension, dyslipidemia, and diabetes.
Table 2.
Characteristics of Participants (n=17,418) Based on Quartiles of Consumption of the Five Dietary Patterns among the 17,418 Participants in the REGARDS Cohort.
| Dietary Pattern | Characteristic | Quartile 1 (Lowest Consumption), % or Mean ± SD | Quartile 2, % or Mean ± SD | Quartile 3, % or Mean ± SD | Quartile 4 (Highest Consumption), % or Mean ± SD | P Value* |
|---|---|---|---|---|---|---|
| Convenience | Age >65 y | 57.0 | 49.0 | 44.0 | 34.1 | <0.001 |
| Male | 30.9 | 35.8 | 44.1 | 51.9 | <0.001 | |
| Black | 47.0 | 38.8 | 28.9 | 23.8 | <0.001 | |
| Did not graduate from high school | 27.5 | 25.3 | 23.9 | 23.2 | <0.001 | |
| Household income <$20,000/y | 19.6 | 15.6 | 12.5 | 11.9 | <0.001 | |
| Resident of stroke belt† | 56.2 | 57.6 | 56.0 | 55.2 | <0.001 | |
| Current smoker | 13.1 | 13.3 | 12.6 | 14.4 | <0.001 | |
| Physically active‡ | 31.8 | 28.7 | 30.2 | 28.8 | <0.001 | |
| Body mass index (kg/m2) | 28.9 ± 6.2 | 27.9 ± 6.0 | 27.8 ± 6.1 | 28.5 ± 6.2 | <0.001 | |
| Waist circumference (cm) | 92.7 ± 15.4 | 92.7 ± 15.3 | 94.0 ± 15.3 | 96.5 ± 15.5 | <0.001 | |
| Hypertension§ | 59.6 | 56.2 | 51.2 | 48.7 | <0.001 | |
| Dyslipidemia‖ | 52.3 | 52.5 | 53.8 | 55.9 | 0.004 | |
| Diabetes# | 18.6 | 17.3 | 14.1 | 14.6 | <0.001 | |
| Plant-based | Age >65 y | 36.0 | 46.8 | 50.8 | 50.4 | <0.001 |
| Male | 50.3 | 41.8 | 37.0 | 33.6 | <0.001 | |
| Black | 28.5 | 35.7 | 35.8 | 38.5 | <0.001 | |
| Did not graduate from high school | 29.5 | 25.0 | 24.7 | 20.7 | <0.001 | |
| Household income <$20,000/y | 14.8 | 15.2 | 15.0 | 14.6 | <0.001 | |
| Resident of stroke belt | 56.2 | 57.6 | 56.0 | 55.2 | 0.43 | |
| Current smoker | 23.1 | 13.3 | 9.7 | 7.3 | <0.001 | |
| Physically active | 25.3 | 28.1 | 29.8 | 36.3 | <0.001 | |
| Body mass index (kg/m2) | 28.2 ± 6.1 | 28.2 ± 6.1 | 28.0 ± 6.2 | 27.8 ± 6.2 | 0.038 | |
| Waist circumference (cm) | 95.3 ± 15.2 | 94.0 ± 15.6 | 94.0 ± 15.4 | 92.1 ± 15.4 | <0.001 | |
| Hypertension | 51.1 | 55.0 | 55.4 | 54.2 | <0.001 | |
| Dyslipidemia | 55.9 | 53.4 | 54.3 | 51.0 | <0.001 | |
| Diabetes | 13.9 | 16.6 | 16.9 | 17.2 | <0.001 | |
| Sweets | Age >65 y | 43.8 | 48.5 | 47.4 | 44.3 | <0.001 |
| Male | 35.0 | 37.5 | 44.1 | 46.0 | <0.001 | |
| Black | 46.1 | 34.5 | 29.0 | 28.8 | <0.001 | |
| Did not graduate from high school | 23.7 | 23.5 | 24.5 | 28.2 | <0.001 | |
| Household income <$20,000/y | 15.1 | 13.9 | 14.1 | 16.5 | <0.001 | |
| Resident of stroke belt | 53.3 | 55.0 | 56.5 | 60.2 | <0.001 | |
| Current smoker | 12.0 | 11.5 | 13.1 | 16.8 | <0.001 | |
| Physically active | 32.0 | 29.5 | 29.7 | 28.3 | <0.001 | |
| Body mass index (kg/m2) | 28.3 ± 6.2 | 28.1 ± 5.9 | 27.8 ± 6.1 | 28.1 ± 6.3 | 0.19 | |
| Waist circumference (cm) | 94.0 ± 15.7 | 94.0 ± 14.9 | 94.0 ± 15.4 | 94.6 ± 15.7 | <0.001 | |
| Hypertension | 57.0 | 54.4 | 53.1 | 51.2 | <0.001 | |
| Dyslipidemia | 51.3 | 54.3 | 54.1 | 54.8 | <0.001 | |
| Diabetes | 18.6 | 17.8 | 15.1 | 13.1 | <0.001 | |
| Southern | Age >65 y | 45.9 | 47.4 | 48.2 | 42.4 | <0.001 |
| Male | 33.6 | 34.9 | 42.3 | 52.0 | <0.001 | |
| Black | 9.5 | 24.8 | 43.0 | 61.4 | <0.001 | |
| Did not graduate from high school | 19.5 | 22.6 | 27.2 | 30.6 | <0.001 | |
| Household income <$20,000/y | 8.0 | 11.6 | 16.9 | 23.2 | <0.001 | |
| Resident of stroke belt | 48.8 | 53.6 | 58.7 | 64.0 | <0.001 | |
| Current smoker | 8.2 | 10.6 | 14.2 | 20.5 | <0.001 | |
| Physically active | 32.9 | 28.3 | 28.3 | 29.9 | <0.001 | |
| Body mass index (kg/m2) | 26.6 ± 5.3 | 27.6 ± 5.8 | 28.4 ± 6.2 | 29.6 ± 6.7 | <0.001 | |
| Waist circumference (cm) | 88.9 ± 14.5 | 91.4 ± 14.9 | 95.3 ± 14.7 | 99.1 ± 15.8 | <0.001 | |
| Hypertension | 41.9 | 51.3 | 58.4 | 64.1 | <0.001 | |
| Dyslipidemia | 50.6 | 54.9 | 53.4 | 55.6 | <0.001 | |
| Diabetes | 8.7 | 13.5 | 18.2 | 24.2 | <0.001 | |
| Alcohol and Salads | Age >65 y | 52.5 | 47.2 | 45.0 | 39.4 | <0.001 |
| Male | 33.1 | 36.6 | 44.1 | 48.9 | <0.001 | |
| Black | 52.0 | 39.4 | 27.5 | 19.7 | <0.001 | |
| Did not graduate from high school | 28.8 | 27.6 | 23.5 | 20.0 | <0.001 | |
| Household income <$20,000/y | 24.8 | 16.1 | 11.5 | 7.4 | <0.001 | |
| Resident of stroke belt | 58.9 | 59.3 | 55.8 | 51.0 | <0.001 | |
| Current smoker | 11.2 | 13.4 | 14.2 | 14.6 | <0.001 | |
| Physically active | 27.8 | 28.4 | 29.8 | 33.4 | <0.001 | |
| Body mass index (kg/m2) | 28.1 ± 6.4 | 28.1 ± 6.2 | 28.9 ± 5.9 | 28.9 ± 6.0 | 0.030 | |
| Waist circumference (cm) | 94.3 ± 15.3 | 94.7 ± 15.2 | 94.7 ± 15.4 | 94.3 ± 15.8 | 0.006 | |
| Hypertension | 60.1 | 54.9 | 51.7 | 49.0 | <0.001 | |
| Dyslipidemia | 55.4 | 54.3 | 53.4 | 51.5 | 0.004 | |
| Diabetes | 18.3 | 17.4 | 15.7 | 13.2 | <0.001 |
SD indicates standard deviation.
Chi-square test (for proportions) and analysis of variance (for continuous variables).
Stroke belt consists of North Carolina, South Carolina, Georgia, Tennessee, Alabama, Mississippi, Arkansas, and Louisiana.
Physically active defined as four or more days of exercise (enough to work up a sweat) per week.
Hypertension defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg or self-reported current use of medication to control blood pressure.
Dyslipidemia defined as total cholesterol ≥6.22 mmol/L (240 mg/dL) and/or low-density lipoprotein cholesterol ≥4.14 mmol/L (160 mg/dL) and/or high-density lipoprotein cholesterol ≤1.04 mmol/L (40 mg/dL) or self-reported current use of medication to control cholesterol.
Diabetes defined as fasting glucose ≥6.99 mmol/L (126 mg/dL) and/or non-fasting glucose ≥11.10 mmol/L (200 mg/dL) or self-reported current use of medication to control blood sugar.
Dietary variables by quartile of consumption of each dietary pattern are provided in Table 3. In general, higher consumption of each of the five patterns was associated with higher total energy intake. This also was the case for total fat intake (as % of total energy), except for the Plant-based pattern, where greater consumption was associated with lower total fat intake. Higher consumption of the Southern pattern was associated with lower intakes of dietary fiber, vegetables, and fruits, while higher consumption of the Plant-based pattern was associated with higher intakes of dietary fiber, vegetables, fruits, and whole grains.
Table 3.
Intake of Energy, Selected Nutrients, and Food Groups Based on Quartiles of Consumption of the Five Dietary Patterns among the 17,418 Participants in the REGARDS Cohort.
| Dietary Pattern | Component | Quartile 1 (Lowest Consumption), Median (IQR) | Quartile 2, Median (IQR) | Quartile 3, Median (IQR) | Quartile 4 (Highest Consumption), Median (IQR) | P Value* |
|---|---|---|---|---|---|---|
| Convenience | Energy (kcal/d) | 1332 (720) | 1340 (671) | 1612 (714) | 2169 (974) | <0.001 |
| Fat (% energy) | 36.2 (11.9) | 37.1 (10.1) | 37.6 (9.4) | 38.7 (8.5) | <0.001 | |
| Carbohydrate (% energy) | 52.0 (13.3) | 48.9 (11.7) | 47.4 (10.9) | 45.3 (10.1) | <0.001 | |
| Protein (% energy) | 13.0 (3.7) | 14.1 (3.8) | 14.8 (3.7) | 15.5 (3.7) | <0.001 | |
| Dietary fiber (g/d) | 12.4 (8.8) | 12.2 (8.4) | 14.3 (9.2) | 18.9 (10.6) | <0.001 | |
| Vegetables (servings/d) | 2.0 (2.2) | 2.0 (2.0) | 2.5 (2.2) | 3.2 (2.7) | <0.001 | |
| Fruit (servings/d) | 1.4 (1.4) | 1.1 (1.4) | 1.1 (1.3) | 1.1 (1.2) | <0.001 | |
| Whole grains (servings/d) | 3.0 (2.5) | 3.0 (2.3) | 3.6 (2.4) | 4.8 (3.1) | <0.001 | |
| Plant-based | Energy (kcal/d) | 1430 (873) | 1431 (796) | 1576 (792) | 1901 (923) | <0.001 |
| Fat (% energy) | 38.9 (9.6) | 37.9 (9.7) | 37.4 (9.6) | 35.9 (10.3) | <0.001 | |
| Carbohydrate (% energy) | 45.7 (11.7) | 47.8 (11.4) | 48.5 (11.4) | 50.4 (12.0) | <0.001 | |
| Protein (% energy) | 13.5 (3.9) | 14.0 (3.8) | 14.6 (3.8) | 15.4 (3.9) | <0.001 | |
| Dietary fiber (g/d) | 9.3 (5.9) | 11.7 (6.0) | 15.6 (6.7) | 22.9 (10.1) | <0.001 | |
| Vegetables (servings/d) | 1.4 (1.1) | 1.9 (1.4) | 2.8 (1.9) | 4.6 (3.0) | <0.001 | |
| Fruit (servings/d) | 0.6 (0.7) | 1.0 (0.9) | 1.4 (1.1) | 2.1 (1.7) | <0.001 | |
| Whole grains (servings/d) | 2.9 (2.4) | 3.3 (2.4) | 3.7 (2.5) | 4.5 (3.2) | <0.001 | |
| Sweets | Energy (kcal/d) | 1173 (642) | 1370 (586) | 1672 (665) | 2227 (939) | <0.001 |
| Fat (% energy) | 34.9 (11.0) | 36.6 (9.9) | 38.1 (9.5) | 39.6 (8.3) | <0.001 | |
| Carbohydrate (% energy) | 46.8 (14.6) | 48.6 (12.2) | 48.5 (11.1) | 48.4 (9.8) | <0.001 | |
| Protein (% energy) | 15.6 (4.8) | 14.9 (3.8) | 14.3 (3.4) | 13.2 (3.2) | <0.001 | |
| Dietary fiber (g/d) | 11.4 (8.6) | 13.2 (8.9) | 15.1 (9.2) | 18.0 (10.5) | <0.001 | |
| Vegetables (servings/d) | 2.3 (2.4) | 2.2 (2.2) | 2.5 (2.2) | 2.8 (2.6) | <0.001 | |
| Fruit (servings/d) | 1.1 (1.4) | 1.2 (1.4) | 1.2 (1.4) | 1.1 (1.4) | <0.001 | |
| Whole grains (servings/d) | 2.3 (1.8) | 3.2 (2.0) | 4.0 (2.3) | 5.2 (3.2) | <0.001 | |
| Southern | Energy (kcal/d) | 1589 (797) | 1373 (747) | 1474 (769) | 1991 (1057) | <0.001 |
| Fat (% energy) | 35.8 (10.2) | 37.4 (9.8) | 37.9 (9.6) | 38.6 (9.8) | <0.001 | |
| Carbohydrate (% energy) | 49.6 (11.0) | 48.4 (11.7) | 48.0 (11.9) | 46.4 (12.1) | <0.001 | |
| Protein (% energy) | 15.1 (3.8) | 14.2 (3.7) | 13.9 (3.9) | 14.2 (4.2) | <0.001 | |
| Dietary fiber (g/d) | 17.1 (10.8) | 13.5 (9.2) | 12.6 (8.9) | 14.5 (10.1) | <0.001 | |
| Vegetables (servings/d) | 2.9 (2.6) | 2.3 (2.3) | 2.2 (2.1) | 2.4 (2.4) | <0.001 | |
| Fruit (servings/d) | 1.5 (1.5) | 1.2 (1.4) | 1.1 (1.2) | 1.0 (1.2) | <0.001 | |
| Whole grains (servings/d) | 3.7 (2.6) | 3.1 (2.4) | 3.3 (2.5) | 4.3 (3.4) | <0.001 | |
| Alcohol and Salads | Energy (kcal/d) | 1467 (898) | 1426 (772) | 1581 (799) | 1877 (934) | <0.001 |
| Fat (% energy) | 33.9 (8.8) | 36.8 (8.8) | 38.9 (9.0) | 41.1 (10.5) | <0.001 | |
| Carbohydrate (% energy) | 54.1 (10.2) | 50.1 (9.6) | 46.6 (9.6) | 41.1 (10.3) | <0.001 | |
| Protein (% energy) | 13.8 (3.9) | 14.2 (3.7) | 14.5 (3.8) | 15.0 (4.2) | <0.001 | |
| Dietary fiber (g/d) | 14.1 (11.0) | 12.7 (9.0) | 14.5 (9.2) | 16.2 (10.4) | <0.001 | |
| Vegetables (servings/d) | 1.9 (2.0) | 2.0 (1.9) | 2.5 (2.2) | 3.4 (2.8) | <0.001 | |
| Fruit (servings/d) | 1.3 (1.3) | 1.1 (1.4) | 1.2 (1.4) | 1.1 (1.5) | <0.001 | |
| Whole grains (servings/d) | 3.8 (3.0) | 3.4 (2.6) | 3.5 (2.5) | 3.5 (2.9) | <0.001 |
IQR indicates interquartile range.
Kruskal-Wallis.
A total of 536 cases of acute CHD were adjudicated over a median (IQR) 5.8 (2.1) years of follow-up. After adjustment for age, sex, race, education, household income, region, energy, smoking, and physical activity, participants with the highest consumption of the Southern pattern experienced a 56% higher hazard of acute CHD (comparing quartile 4 to quartile 1: HR = 1.56; 95% CI: 1.17, 2.08; P for trend across quartiles = 0.003) (Table 4). Adding BMI, waist circumference, and history of hypertension, dyslipidemia, and diabetes to the model attenuated the association somewhat, but a significant association remained (HR = 1.37; 95% CI: 1.01, 1.85; P for trend = 0.036). No other dietary pattern was associated with the hazard of acute CHD in multivariable models adjusted beyond age, sex, and race. A Kaplan-Meier plot demonstrates a lower probability of acute CHD-free survival in the quartile of highest consumption of the Southern pattern compared to the other dietary patterns (Figure).
Table 4.
Hazard of Acute Incident Coronary Heart Disease by Quartile of Consumption of the Various Dietary Patterns.
| Dietary Pattern | Model | Quartile 1 (Lowest Consumption), HR (95% CI) | Quartile 2, HR (95% CI) | Quartile 3, HR (95% CI) | Quartile 4 (Highest Consumption), HR (95% CI) | P Value for Trend |
|---|---|---|---|---|---|---|
| Convenience | n = 4344 (142*) | n = 4356 (132) | n = 4373 (136) | n = 4345 (126) | ||
| 58.7† | 54.8 | 55.7 | 51.9 | 0.36 | ||
| 1‡ | 1(referent) | 0.99 (0.78, 1.26) | 0.99 (0.78, 1.26) | 0.98 (0.76, 1.26) | 0.88 | |
| 2§ | 1(referent) | 1.02 (0.81, 1.30) | 1.04 (0.82, 1.33) | 1.05 (0.81, 1.35) | 0.69 | |
| 3‖ | 1(referent) | 1.02 (0.81, 1.30) | 1.02 (0.80, 1.31) | 0.98 (0.75, 1.30) | 0.95 | |
| 4# | 1(referent) | 1.02 (0.80, 1.29) | 1.03 (0.81, 1.32) | 0.99 (0.75, 1.31) | 0.99 | |
| 5** | 1(referent) | 1.04 (0.81, 1.33) | 1.05 (0.82, 1.36) | 0.95 (0.71, 1.27) | 0.85 | |
| Plant-based | n = 4351 (140) | n = 4355 (146) | n = 4359 (136) | n = 4353 (114) | ||
| 57.3 | 60.4 | 56.2 | 47.1 | 0.11 | ||
| 1 | 1(referent) | 0.97 (0.77, 1.23) | 0.92 (0.73, 1.18) | 0.79 (0.62, 1.02) | 0.07 | |
| 2 | 1(referent) | 1.00 (0.79, 1.27) | 0.97 (0.76, 1.23) | 0.87 (0.67, 1.12) | 0.25 | |
| 3 | 1(referent) | 0.99 (0.78, 1.26) | 0.94 (0.73, 1.20) | 0.80 (0.61, 1.05) | 0.11 | |
| 4 | 1(referent) | 1.08 (0.85, 1.37) | 1.06 (0.82, 1.36) | 0.95 (0.72, 1.26) | 0.75 | |
| 5 | 1(referent) | 1.07 (0.84, 1.38) | 1.06 (0.82, 1.37) | 1.02 (0.76, 1.36) | 0.91 | |
| Sweets | n = 4349 (103) | n = 4357 (137) | n = 4355 (146) | n = 4357 (150) | ||
| 42.2 | 56.9 | 60.2 | 61.8 | 0.004 | ||
| 1 | 1(referent) | 1.26 (0.97, 1.63) | 1.28 (1.00, 1.66) | 1.35 (1.04, 1.74) | 0.031 | |
| 2 | 1(referent) | 1.24 (0.96, 1.61) | 1.22 (0.94, 1.57) | 1.22 (0.95, 1.58) | 0.19 | |
| 3 | 1(referent) | 1.24 (0.95, 1.60) | 1.19 (0.91, 1.55) | 1.16 (0.86, 1.56) | 0.40 | |
| 4 | 1(referent) | 1.22 (0.94, 1.59) | 1.18 (0.91, 1.54) | 1.14 (0.84, 1.54) | 0.47 | |
| 5 | 1(referent) | 1.24 (0.95, 1.62) | 1.28 (0.98, 1.69) | 1.18 (0.86, 1.62) | 0.27 | |
| Southern | n = 4370 (92) | n = 4362 (110) | n = 4346 (138) | n = 4340 (196) | ||
| 38.5 | 45.6 | 56.5 | 79.8 | <0.001 | ||
| 1 | 1(referent) | 1.17 (0.88, 1.54) | 1.37 (1.05, 1.80) | 2.00 (1.53, 2.61) | <0.001 | |
| 2 | 1(referent) | 1.13 (0.86, 1.50) | 1.23 (0.93, 1.62) | 1.65 (1.25, 2.18) | <0.001 | |
| 3 | 1(referent) | 1.13 (0.85, 1.50) | 1.23 (0.93, 1.62) | 1.66 (1.24, 2.20) | <0.001 | |
| 4 | 1(referent) | 1.09 (0.82, 1.45) | 1.15 (0.88, 1.52) | 1.56 (1.17, 2.08) | 0.003 | |
| 5 | 1(referent) | 1.04 (0.78, 1.40) | 1.09 (0.82, 1.46) | 1.37 (1.01, 1.85) | 0.036 | |
| Alcohol and Salads | n = 4338 (140) | n = 4354 (131) | n = 4368 (131) | n = 4358 (134) | ||
| 57.2 | 54.1 | 54.1 | 55.6 | 0.82 | ||
| 1 | 1(referent) | 0.99 (0.78, 1.26) | 0.97 (0.76, 1.24) | 1.03 (0.80, 1.32) | 0.86 | |
| 2 | 1(referent) | 1.01 (0.79, 1.28) | 1.04 (0.81, 1.33) | 1.17 (0.91, 1.51) | 0.22 | |
| 3 | 1(referent) | 1.01 (0.79, 1.28) | 1.03 (0.81, 1.32) | 1.15 (0.89, 1.49) | 0.31 | |
| 4 | 1(referent) | 0.99 (0.78, 1.26) | 0.99 (0.77, 1.26) | 1.09 (0.84, 1.42) | 0.57 | |
| 5 | 1(referent) | 0.95 (0.74, 1.22) | 0.98 (0.76, 1.27) | 1.00 (0.76, 1.32) | 0.95 |
CI indicates confidence interval; and HR, hazard ratio.
Number of events.
Crude coronary heart disease incidence rate per 10,000 person-years.
Model 1 adjusts for age, sex, race, and age-race interaction.
Model 2 adjusts for factors in model 1 plus education, household income, and region.
Model 3 adjusts for factors in model 2 plus total energy intake.
Model 4 adjusts for factors in model 3 plus smoking and physical activity.
Model 5 adjusts for factors in model 4 plus body mass index, waist circumference, and history of hypertension, dyslipidemia, and diabetes.
Figure 1.
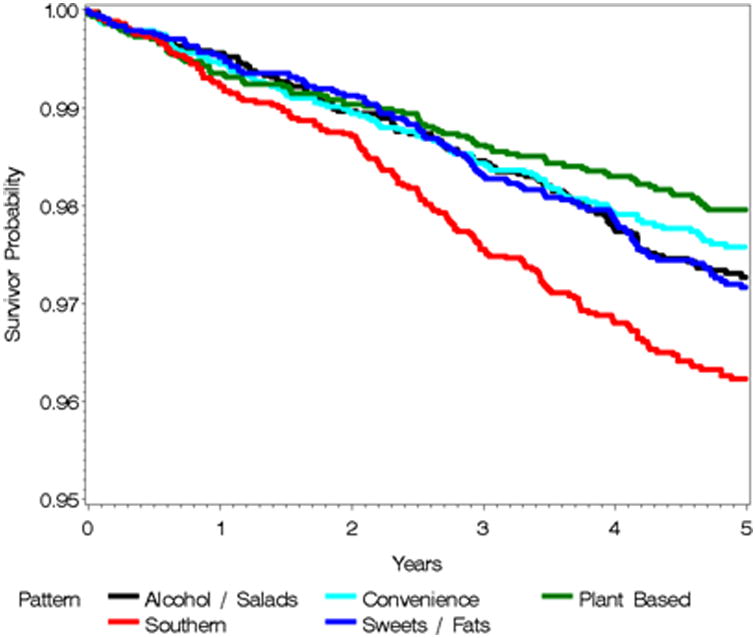
Probability of acute coronary heart disease-free survival in the quartile of highest consumption of the various dietary patterns.
Discussion
A dietary pattern labeled as Southern, characterized by added fats, fried food, eggs, organ meats, processed meats, and sugar-sweetened beverages, was positively associated with hazard of incident acute CHD in this population-based sample of black and white adults in the US. The other main dietary patterns derived in the REGARDS cohort were not associated with CHD hazard. The lack of an association with the Plant-based pattern was notable, based on the beneficial health effects of the food groups that loaded heavily in this pattern28,29.
Associations of factor analysis-derived dietary patterns have been investigated in diverse populations worldwide, with varying results. In agreement with the positive association of the Southern pattern with hazard of acute CHD in the REGARDS cohort, higher consumption of a pattern characterized by fried foods, eggs, and meat (similar to the Southern pattern) was associated with a greater risk of acute MI in 52 countries in the INTERHEART study11 and INTERHEART China study14. The US Health Professionals Follow-up Study (HPFS) and Nurses' Health Study (NHS) identified “Western” patterns, characterized by high loading of red meat, processed meat, refined grains, French fries, high-fat dairy products, and sweets (combining various aspects of our Southern and Sweets patterns). In both of these studies, consumption of the Western pattern was positively associated with CHD risk8,9. However, a dietary pattern loading heavily on French fries, fast foods, and sugar-sweetened beverages was not associated with CHD risk in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Netherlands cohort16.
It is noteworthy that no association was seen with hazard of CHD for the Plant-based pattern in REGARDS participants, in contrast to the results of some, but not all, previous studies. A plant-based diet was inversely associated with CHD risk in the Spanish cohort of the EPIC study (EPIC-Spain)12. Higher consumption of fruit and vegetable patterns also was associated with a lower risk of acute MI in the INTERHEART study11 and INTERHEART China study14. A vegetable pattern was associated with a significantly reduced risk of CHD in women, although not in men, in the Japan Collaborative Cohort Study15, and a high fruits and vegetables pattern was associated with a decreased risk of coronary deaths and non-fatal MI in the Whitehall II study in England30. The HPFS and NHS identified “prudent” patterns, characterized by high loading of fruits, vegetables, legumes, whole grains, fish, and poultry (similar to our Plant-based pattern), that were inversely associated with CHD risk in both cohorts8,9. However, in agreement with our results, a vegetable pattern was not associated with risk of acute MI in Costa Rica10. In addition, a prudent pattern characterized by fruits and vegetables, along with wholemeal cereals, was not associated with CHD risk in a Danish cohort13.
There are several potential mechanisms through which greater consumption of the Southern dietary pattern was associated with increased hazard of CHD in this study. This pattern loaded heavily on processed meats and sugar-sweetened beverages. A systematic review and meta-analysis of observational studies and randomized trials provided evidence that processed meat consumption was associated with a higher incidence of CHD, which the authors speculated was due not only to their high sodium content, but also to their high nitrate preservative content, which (along with their byproducts) have been shown experimentally to promote atherosclerosis and vascular dysfunction31. A meta-analysis of prospective studies showed that sugar-sweetened beverage consumption was positively associated with the risk of CHD, with the effect attributed not only to increased BMI, but also to increased glycemic load, resulting in insulin resistance, β-cell dysfunction, and inflammation, setting the stage for atherosclerosis32. However, evidence linking some of the other foods on which the Southern pattern loaded heavily to increased risk of CHD is lacking. For example, while the Southern pattern loaded heavily on added fats, previous studies indicate that while the type of added fats appears to be related to CHD risk, the amount of added fats does not33. In addition, consumption of fried foods in the EPIC-Spain cohort was not associated with risk of CHD, although the type of oil, the degree of thermal degradation of the oil, and the type of food likely affect the production of atherosclerotic trans fatty acids during the frying process and, therefore, should be characterized34. Finally, results from the HPFS and NHS, along with a subsequent epidemiologic review and a meta-analysis of prospective cohort studies, showed that higher consumption of eggs (up to one egg per day) was not associated with increased risk of CHD in men or women35-37.
This study included both strengths and weaknesses that should be noted. Strengths of this study include the large population-based sample, the sociodemographic and regional diversity of the sample (including the large proportion of black participants), the comprehensive assessment of diet, and derivation of dietary patterns using a rigorous method – factor analysis. To our knowledge, this is the first time that data-derived dietary pattern methods have been applied to a population with a large proportion of participants from the stroke belt and buckle regions of the US.
Dietary patterns may be defined a priori by assessing degree of adherence to indices of healthy diets such as the Healthy Eating Index38. The advantage of such indices is that they are based on dietary recommendations or guidelines from official bodies based on current nutrition knowledge on what constitutes a healthy diet, most of which is generated from empirical research. In addition, using a standard index across multiple studies allows for consistency in how a healthy diet is assessed, and there may be a nascent trend toward scientific consensus on the guidelines underlying these indices. The primary advantage of factor analysis is that the resulting patterns are not defined a priori nor are they based on the authors' opinions on what defines a healthy or other dietary patterns; rather, statistical methods are used to derive patterns a posteriori based on the actual dietary data collected in the population of interest. However, a potential limitation of factor analysis is that subjectivity can come into play during the factor analysis process in such areas as collapsing primary dietary data, grouping the data, deciding on the number of patterns that should remain in the final solution, and even in the naming of the patterns. Resulting decisions made by investigators affect not only the number, but also the type of dietary patterns derived and reported6,39. It is possible that this subjectivity could have resulted in some of the variation of the published results noted above.
It should be noted that the Block 98 FFQ has yet to be validated in the REGARDS population. Measurement error is a potential limitation in any study relying on recall of dietary intake, as with an FFQ. It is possible that inaccuracies in reporting dietary intake may have resulted in misclassification. However, this would tend to bias results toward the null, potentially reducing the magnitude of the associations between dietary patterns and acute CHD observed in this analysis. Unfortunately, correction for potential measurement error was not possible. It is possible that selection bias may have resulted from using commercially available lists for recruitment, as not all persons have listed telephone numbers and/or a mailing address. We were missing dietary data on 28.3% of participants free of CHD at baseline. Those missing dietary data were more likely to have lower income and to have not graduated from high school. However, we had adequate numbers of individuals in those categories to provide assurance that this did not bias the results of the study; of those with dietary data, 1553 were not high school graduates and 2635 had an annual income less than $20,000. Finally, the results may not be generalizable to groups other than whites and blacks in the US.
In summary, a Southern dietary pattern, characterized by added fats, fried food, eggs and egg dishes, organ meats, processed meats, and sugar-sweetened beverages, was associated with a greater hazard of incident acute CHD in this sociodemographically and regionally diverse sample of white and black adults. Despite its high loading of putative “heart healthy” foods (including fruits, vegetables, fish, and beans), a Plant-based pattern was not associated with hazard of CHD in this sample.
Supplementary Material
Acknowledgments
The authors thank the other investigators, staff, and participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Funding Sources: This work was supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke and R01 HL080477 and K24 HL111154 from the National Heart, Lung, and Blood Institute, NIH, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke, National Heart, Lung, and Blood Institute, or the NIH. Representatives of the funding agencies have been involved in the review of the manuscript but not directly involved in the collection, management, analysis, or interpretation of the data. General Mills Bell Institute of Health and Nutrition generously supported the scanning and analysis of the dietary questionnaires used in this study.
Footnotes
Disclosures: None.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. doi: 10.1161/01.cir.0000442015.53336.12. [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 3.Kromhout D, Menotti A, Kesteloot H, Sans S. Prevention of coronary heart disease by diet and lifestyle: evidence from prospective cross-cultural, cohort, and intervention studies. Circulation. 2002;105:893–898. doi: 10.1161/hc0702.103728. [DOI] [PubMed] [Google Scholar]
- 4.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 5.Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–249. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 6.Newby PK, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev. 2004;62:177–203. doi: 10.1301/nr.2004.may.177-203. [DOI] [PubMed] [Google Scholar]
- 7.Van Horn L. Eating pattern analysis: the whole is more than the sum of its parts. J Am Diet Assoc. 2011;111:203. doi: 10.1016/j.jada.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Hu FB, Rimm EB, Stampfer MJ, Acherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72:912–921. doi: 10.1093/ajcn/72.4.912. [DOI] [PubMed] [Google Scholar]
- 9.Fung TT, Willett WC, Stampfer MJ, Manson JE, Hu FB. Dietary patterns and the risk of coronary heart disease in women. Arch Intern Med. 2001;161:1857–1862. doi: 10.1001/archinte.161.15.1857. [DOI] [PubMed] [Google Scholar]
- 10.Martinez-Ortiz JA, Fung TT, Baylin A, Hu FB, Campos H. Dietary patterns and risk of nonfatal acute myocardial infarction in Costa Rican adults. Eur J Clin Nutr. 2006;60:770–777. doi: 10.1038/sj.ejcn.1602381. [DOI] [PubMed] [Google Scholar]
- 11.Iqbal R, Anand S, Ounpuu S, Islam S, Zhang X, Rangarajan S, Chifamba J, Al-Hinai A, Keltai M, Yusuf S INTERHEART Study Investigators. Dietary patterns and the risk of acute myocardial infarction in 52 countries: results of the INTERHEART Study. Circulation. 2008;118:1929–1937. doi: 10.1161/CIRCULATIONAHA.107.738716. [DOI] [PubMed] [Google Scholar]
- 12.Guallar-Castillón P, Rodríguez-Artalejo F, Tormo MJ, Sanchez MJ, Rodriguez L, Quiros JR, Navarro C, Molina E, Martinez C, Marin P, Lopez-Garcia E, Larrañaga N, Huerta JM, Dorronsoro M, Chirlaque MD, Buckland G, Barricarte A, Banegas JR, Arriola L, Ardanaz E, González CA, Moreno-Iribas C. Major dietary patterns and risk of coronary heart disease in middle-aged persons from a Mediterranean country: the EPIC-Spain cohort study. Nutr Metab Cardiovasc Dis. 2012;22:192–199. doi: 10.1016/j.numecd.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Osler M, Helms Andreasen A, Heitmann B, Hoidrup S, Gerdes U, Morch Jorgensen L, Schroll M. Food intake patterns and risk of coronary heart disease: a prospective cohort study examining the use of traditional scoring techniques. Eur J Clin Nutr. 2002;56:568–574. doi: 10.1038/sj.ejcn.1601360. [DOI] [PubMed] [Google Scholar]
- 14.Guo J, Li W, Wang Y, Chen T, Teo K, Liu LS, Yusuf S INTERHEART China Study Investigators. Influence of dietary patterns on the risk of acute myocardial infarction in China population: the INTERHEART China study. Chin Med J. 2013;126:464–470. [PubMed] [Google Scholar]
- 15.Maruyama K, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A JACC Study Group. Dietary patterns and risk of cardiovascular deaths among middle-aged Japanese: JACC Study. Nutr Metab Cardiovasc Dis. 2013;23:519–527. doi: 10.1016/j.numecd.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Stricker MD, Onland-Moret NC, Boer JM, van der Schouw YT, Verschuren WM, May AM, Peeters PH, Beulens JW. Dietary patterns derived from principal component- and k-means cluster analysis: long-term association with coronary heart disease. Nutr Metab Cardiovasc Dis. 2013;23:250–256. doi: 10.1016/j.numecd.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The Reasons for Geographic and Racial Differences in Stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 18.Judd SE, Gutierrez OM, Newby PK, Howard G, Howard VJ, Locher JL, Kissela BM, Shikany JM. Dietary patterns are associated with incident stroke and contribute to excess risk of stroke in Black Americans. Stroke. 2013;44:3305–3311. doi: 10.1161/STROKEAHA.113.002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gutiérrez OM, Muntner P, Rizk DV, McClellan WM, Warnock DG, Newby PK, Judd SE. Dietary patterns and risk of death and progression to ESRD in individuals with CKD: a cohort study. Am J Kidney Dis. 2014;64:204–213. doi: 10.1053/j.ajkd.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 21.Jackson R, Chambless LE, Yang K, Byrne T, Watson R, Folsom A, Shahar E, Kalsbeek W. Differences between respondents and nonrespondents in a multicenter community-based study vary by gender ethnicity. J Clin Epidemiol. 1996;49:1441–1446. doi: 10.1016/0895-4356(95)00047-x. [DOI] [PubMed] [Google Scholar]
- 22.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 23.Mares-Perlman JA, Klein BEK, Klein R, Ritter LL, Fisher MR, Freudenheim JL. A diet history questionnaire ranks nutrient intakes in middle-aged and older men and women similarly to multiple food records. J Nutr. 1993;123:489–501. doi: 10.1093/jn/123.3.489. [DOI] [PubMed] [Google Scholar]
- 24.Judd SE, Letter AJ, Shikany JM, Roth DL, Newby PK. Dietary patterns derived using exploratory and confirmatory factor analysis are stable and generalizable across race, region, and gender subgroups in the REGARDS study. Front Nutr. 2015;1:29. doi: 10.3389/fnut.2014.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levine TR. Confirmatory factor analysis and scale validation in communication research. Comm Res Rep. 2005;22:335–338. [Google Scholar]
- 26.Lorenzo-Seva U, ten Berge JMF. Tucker's congruence coefficient as a meaningful index of factor similarity. Eur J Res Methods Behav Soc Sci. 2006;2:57–64. [Google Scholar]
- 27.Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, Lewis CE, Gamboa C, Cushman M, Howard V, Howard G REGARDS Investigators. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–1774. doi: 10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McEvoy CT, Temple N, Woodside JV. Vegetarian diets, low-meat diets and health: a review. Public Health Nutr. 2012;15:2287–2294. doi: 10.1017/S1368980012000936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu FB. Plant-based foods and prevention of cardiovascular disease: an overview. Am J Clin Nutr. 2003;78(suppl):544S–551S. doi: 10.1093/ajcn/78.3.544S. [DOI] [PubMed] [Google Scholar]
- 30.Brunner EJ, Mosdol A, Witte DR, Martikainen P, Stafford M, Shipley MJ, Marmot MG. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87:1414–1421. doi: 10.1093/ajcn/87.5.1414. [DOI] [PubMed] [Google Scholar]
- 31.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121:2271–2283. doi: 10.1161/CIRCULATIONAHA.109.924977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta-analysis of prosective studies. Atherosclerosis. 2014;234:11–16. doi: 10.1016/j.atherosclerosis.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 33.Hu FB, Manson JE, Willett WC. Types of dietary fat and risk of coronary heart disease: a critical review. J Am Coll Nutr. 2001;20:5–19. doi: 10.1080/07315724.2001.10719008. [DOI] [PubMed] [Google Scholar]
- 34.Guallar-Castillón P, Rodríguez-Artalejo F, Lopez-Garcia E, Leon-Munoz LM, Amiano P, Ardanaz E, Arriola L, Barricarte A, Buckland G, Chirlaque MD, Dorronsoro M, Huerta JM, Larrañaga N, Marin P, Martínez C, Molina E, Navarro C, Quirós JR, Rodríguez L, Sanchez MJ, González CA, Moreno-Iribas C. Consumption of fried foods and risk of coronary heart disease: Spanish cohort of the European Prospective Investigation into Cancer and Nutrition study. BMJ. 2012;344:e363. doi: 10.1136/bmj.e363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu FB, Stampfer MJ, Rimm EB, Manson JE, Acherio A, Colditz GA, Rosner BA, Spiegelman D, Speizer FE, Sacks FM, Hennekens CH, Willett WC. A prospective study of egg consumption and risk of cardiovascular disease in men and women. JAMA. 1999;281:1387–1394. doi: 10.1001/jama.281.15.1387. [DOI] [PubMed] [Google Scholar]
- 36.Kritchevsky SB, Kritchevsky D. Egg consumption and coronary heart disease: an epidemiologic overview. J Am Coll Nutr. 2000;19(5 Suppl):549S–555S. doi: 10.1080/07315724.2000.10718979. [DOI] [PubMed] [Google Scholar]
- 37.Rong Y, Chen L, Zhu T, Song Y, Yu M, Shan Z, Sands A, Hu FB, Liu L. Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analyss of prospective cohort studies. BMJ. 2013;346:e8539. doi: 10.1136/bmj.e8539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guenther PM, Casavale KO, Kirkpatrick SI, Reedy J, Hiza HAB, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113:569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


