Abstract
Introduction
Concurrent use of cigarettes and smokeless tobacco is common, but little is known regarding the association of smokeless tobacco use with cigarette smoking cessation. Dual users may have lower cigarette consumption levels, which may also play a role in smoking cessation.
Methods
The 2010–2011 Tobacco Use Supplement to the Current Population Survey included 26,760 current cigarette smokers, of which 675 concurrently used smokeless tobacco. We compared characteristics of the most recent cigarette smoking quit attempt of the past year between dual users and exclusive smokers, using multivariate regression.
Results
Dual users (45%) were more likely than exclusive smokers (37%) to have made a cigarette smoking quit attempt during the previous year (p<0.01), even after adjusting for demographic differences and cigarette dependence levels (ORadj 1.33, 95% CI 1.15–1.53). Half (48%) of dual users who made a quit attempt tried to quit “by switching to smokeless tobacco”. However, once in a quit attempt, dual users relapsed more quickly than exclusive smokers (Cox regression HRadj 1.13, 95% CI 1.02–1.26). There was no difference in 30-day abstinence rates on the most recent quit attempt (ORadj 1.09, 95% CI 0.88–1.37). For both groups, the best predictor of past 30-day abstinence was cigarette consumption level.
Conclusions
Current cigarette smokers who also use smokeless tobacco are more likely to have tried to quit, but relapse more quickly than exclusive smokers, and are not more likely to have attained 30 day smoking cessation. Prospective studies at the population level are needed.
Keywords: Smokeless Tobacco, Smoking Cessation, Poly-Tobacco Use
1. Introduction
Cigarette smoking prevalence has declined in the United States, due in part to cigarette excise taxes and clean indoor air laws, awareness of the health effects of smoking and second hand smoke, and social norms which are increasingly critical of smoking.1 As cigarette sales have declined, tobacco industry marketing expenditures for smokeless tobacco products (including snuff, snus and chewing tobacco) have increased.2,3 Concurrent use of cigarettes and smokeless tobacco is common, particularly among younger male smokers and smokers with low income or educational level.4–6
Whether the use of smokeless tobacco products results in a net public health benefit remains an empirical question. It is possible that exclusive use of smokeless tobacco might be associated with fewer health risks than cigarette smoking,7,8 so that complete substitution of smokeless tobacco for cigarettes might result in reduced harm from tobacco use. Therefore, if increased use of smokeless tobacco were to increase cigarette smoking cessation rates9,10 there might be a public health benefit. However if smoking cessation rates remained unchanged or were reduced, increased smokeless tobacco use would be a net public health loss.11–14 Some studies suggest that cigarette smokers may preferentially use smokeless tobacco where smoking is not allowed, potentially undermining clean air policies that have been shown to increase smoking cessation rates at the population level.2,15 Thus, whether smokeless tobacco use is associated with increased or decreased smoking cessation is an important public health question.
Several studies have investigated cigarette smoking cessation rates among dual users of cigarettes and smokeless tobacco at the population level in the US.6,9,15–17 A nationally representative study of US consumers found that dual users were less likely to intend to quit smoking in the next 6 months compared to cigarette-only smokers.6 An investigation of the 1998 National Health Interview Survey concluded that while current smokers who used snuff were more likely to try to quit smoking, analysis of ever-smokers suggested they were less likely to succeed.15 Additionally, an analysis of ever-smokers in 4 nationally representative US surveys from 1999 to 2007 came to similar conclusions for non-daily snuff users,4 although these studies did not directly compare cessation histories between dual users and exclusive smokers. A nationally representative longitudinal cohort within the 2002 TUS-CPS showed no association of smokeless tobacco use with cigarette smoking cessation, although the number of dual users was small (n=48).16 In contrast, an analysis of the 2002 National Health Interview Survey reported that smokers who had used smokeless tobacco to quit cigarette smoking in the past 12 months (n=43) were more likely to be former smokers at the time of the survey than those who had used nicotine replacement therapy,9 although the difference was not tested for statistical significance. Thus, it remains an important question whether smokeless tobacco use is associated with increased or decreased smoking cessation in the US.
Smoking dependence measures such as number of cigarettes smoked per day and time to first cigarette after waking are well-established predictors of attempted smoking cessation and duration of abstinence.18 Thus, any comparison of smoking cessation rates between dual users and exclusive cigarette smokers should account for cigarette dependence. However, it is unknown the extent to which these cigarette dependence measures predict smoking cessation among dual users who have other sources of nicotine. One cancer-prevention trial demonstrated that cigarette consumption level did not predict cigarette smoking abstinence among dual cigarette and smokeless tobacco users.17 Because these dependence measures are used to guide public policy and treatment guidelines for cigarette smoking cessation,18 their ability to predict smoking cessation success has important implications for policy makers.
We used the large nationally representative 2010–2011 TUS-CPS to compare cigarette smoking quit attempts among current cigarette smokers who also use smokeless tobacco (“dual users”) and cigarette smokers who do not use smokeless tobacco (“exclusive smokers”). Because cigarette dependence measures are only available for current smokers, we restricted our analysis to retrospective recall of the most recent cigarette quit attempt among those currently smoking cigarettes at survey. We controlled for demographics and cigarette dependence. We also investigated differences between dual users and exclusive smokers in the relation of cigarette dependence with smoking cessation attempts.
2. Methods
The Current Population Survey (CPS) is a cross-sectional monthly household survey administered by the US Census Bureau, which assesses the labor force characteristics of the civilian, non-institutionalized population aged 18 years and older.19 The CPS uses a multistage probability sample of addresses from the 2000 Decennial Census in a monthly rotating panel design, with response rate > 90%.19 The Tobacco Use Supplements (TUS) to the CPS are administered generally every three to four years, sponsored by the National Cancer Institute, using three independent monthly CPS samples.20 The 2010–2011 TUS-CPS was given May and August, 2010, and January, 2011. The 2010/2011 TUS-CPS sample contained 26,760 exclusive cigarette smokers and 675 dual users ages 18 years and older who provided self-reported tobacco use. The response rate was 61.1%, among the highest in population research.
2.1. Tobacco use measures
Respondents who reported smoking at least 100 lifetime cigarettes were classified as ever-smokers, and were asked to report the age of first regular cigarette smoking (age of initiation) which we categorized as ≤ 15 or > 15 years of age.21,22 Current smokers were defined as ever-smokers who reported currently smoking daily or some days.
Current smokeless tobacco use was assessed by the question, “Do you now use smokeless tobacco, such as moist snuff, dip, spit, chew tobacco or snus, every day, some days, or not at all?”; those reporting daily or non-daily use were classified as current smokeless tobacco users. Dual users were defined as current users of both cigarettes and smokeless tobacco. Exclusive smokers were defined as cigarette smokers who did not report current use of smokeless tobacco.
Cigarette consumption and time to first cigarette after waking was assessed using standard questions on the TUS-CPS.23,24 As in prior studies,25–28 time to first cigarette was categorized as smoking within 30 minutes of waking or as waiting longer than 30 minutes. Cigarette consumption was determined from self-report of number of cigarettes smoked on smoking days, and number of days smoked in the previous 30 days. The 2010/11 TUS-CPS split out those who smoked on fewer than 12 days out of the previous 30 and asked a slightly different question on quitting, and we categorized these as “low rate” smokers. For the remaining smokers, consumption was categorized into the levels 0 to 10 cigarettes per day (cpd) on average, 11 to 20 cpd, and ≥ 21 cpd.
Current smokers were asked whether they had made a quit attempt of one day or longer in the past year “because they were trying to quit smoking” or whether they had “tried to quit smoking completely” (asked of low-rate smokers) and those who responded affirmatively were asked the length of the most recent quit attempt. They were also asked “The (last time/time) you tried to quit smoking in the past 12 months, did you try to quit by switching to smokeless tobacco such as chewing tobacco, snuff, or snus?”. Respondents reporting a quit attempt of at least one day in the past year were counted as having made a quit attempt. Cessation outcomes were any quit attempt in the past year, and, for those who had made a quit attempt, time to relapse of most recent quit attempt, and attainment of at least 30 days abstinence on that attempt.
2.2. Demographic variables
Demographic variables included age, grouped as in our prior studies26–28 (18–24 years, 25–34 years, 35–49 years, 50–64 years, and ≥ 65 years); gender; race/ethnicity (White, Hispanic/Latino, African American, Asian/Pacific Islander, and Mixed race/Other); and level of educational attainment (less than high school, high school graduate, some college, and college graduate).
2.3. Statistical analysis
Analyses used SAS version 9.3 (SAS Institute, Cary, NC). All estimates were weighted by the published survey weights for the TUS–CPS which account for selection probabilities and adjust in part for survey non-response.20 Variance estimates and p-values used the published replicate weights with Fay’s balanced repeated replication.29 Tests of significance are two sided at the 5% level. We used weighted logistic or cox regression to compare outcomes, adjusting for cigarette dependence measures (i.e. cigarette consumption and time to first cigarette after waking) and demographic factors. Interaction terms between tobacco use status (dual user vs exclusive smoker) and cigarette dependence measures were screened for inclusion at the 10% significance level. Interactions between group status and cigarette dependence measures were parameterized by allowing a main effect for tobacco use status, and then computing effect sizes for each dependence measure within each tobacco use group. In doing so, we were able to estimate effect sizes for each cigarette dependence measure separately for dual users and exclusive smokers.
3. Results
3.1. Sample characteristics
Among current cigarette smokers, 2.7% (95% CI 2.5%–2.9%) were dual users overall, including 4.7% (95% CI 4.4%–5.0%) of males, 0.3% (95% CI 0.2–0.4%) of females, and 12.9% (95% CI 11.1–14.7%) of young adult (ages 18–24 years) non-Hispanic white male smokers. Dual users were predominately male and non-Hispanic white (Table 1), and were more likely to be under 35 years of age than were exclusive smokers. Dual users were more likely to be low-rate smokers, and were substantially more likely to report current use of additional forms of combusted tobacco such as cigars. Dual users were somewhat more likely to report smoking within 30 minutes of waking and to initiate smoking at a young age (≤15 years).
Table 1.
Sample characteristics by tobacco use status (Tobacco Use Supplement to the Current Population Survey 2010–2011, N= 27,435)
| Exclusive smokers N=26,760 | Dual users a N=675 | |
|---|---|---|
| Age (%)*** | ||
| 18–24 years | 13.4 (13.1–13.7) | 30.6 (27.5–33.4) |
| 25–34 years | 21.0 (20.6–21.4) | 30.7 (28.1–33.2) |
| 35–49 years | 29.6 (29.1–20.0) | 25.9 (23.3–28.6) |
| 50–64 years | 27.74 (27.3–28.2) | 10.6 (9.2–12.1) |
| ≥ 65 years | 8.3 (8.1–8.6) | 2.2 (1.4–2.9) |
| Gender (%)*** | ||
| Men | 53.1 (52.7–53.5) | 95.1 (93.9–96.4) |
| Women | 46.9 (46.5–47.3) | 4.9 (3.6–6.1) |
| Race/ethnicity (%)*** | ||
| White | 73.4 (73.0–73.9) | 88.7 (87.2–90.4) |
| Hispanic | 9.7 (9.4–10.0) | 4.8 (3.5–6.1) |
| African American | 12.1 (11.8–12.4) | 2.9 (2.1–3.8) |
| Asian/PI | 2.8 (2.6–3.0) | 1.0 (0.4–1.6) |
| Mixed/Other | 2.0 (1.9–2.1) | 2.5 (1.8–3.3) |
| Education (%)* | ||
| Less than high school | 17.6 (17.3–18.0) | 16.8 (14.7–18.8) |
| High school | 39.3 (38.8–39.8) | 42.5 (39.7–45.3) |
| Some college | 30.8 (30.4–31.2) | 30.6 (28.2–33.0) |
| College graduate | 12.3 (12.2–12.4) | 12.2 (11.6–12.8) |
| Cigarette consumption (%)b*** | ||
| < 12 days of month (“low rate”) | 7.9 (7.6–8.1) | 17.0 (14.5–19.4) |
| 0 to 10 cpd | 44.5 (44.0–45.0) | 37.5 (34.6–40.4) |
| 11 to 20 cpd | 36.6 (36.2–37.0) | 35.5 (32.5–38.5) |
| ≥ 21 cpd | 7.7 (7.5–8.0) | 8.7 (7.0–10.3) |
| Cigarette dependence (%)b | ||
| Smoking ≤ 30 min of waking* | 46.2 (45.8–46.7) | 50.2 (47.1–53.2) |
| Smoking > 30 minutes of waking | 45.0 (44.6–49.5) | 45.2 (42.3–48.2) |
| Smoking initiation ≤ age15 years* | 27.0 (26.6–27.5) | 30.0 (27.2–32.8) |
| Smoking initiation > age15 years | 69.6 (69.2–70.1) | 65.8 (62.7–68.9) |
| Age of initiation (Mean)*** | 17.9 (17.9–18.0) | 16.7 (16.5–16.9) |
| Current use of other combustible tobacco (%) | ||
| Cigar use*** | 5.0 (4.8–5.3) | 23.8 (21.4–26.2) |
| Pipe tobacco use*** | 0.8 (0.7–0.9) | 5.7 (4.2–7.2) |
| Hookah use*** | 0.8 (0.7–.9) | 4.3 (2.9–5.6) |
Current cigarette smokers who also report current use of smokeless tobacco
Column percentages do not add up to 100% because of missing responses
p < 0.05
p<0.001
3.2. Association of dual use with cigarette smoking quit attempts and 30-day abstinence
Dual users were approximately 20% more likely than exclusive smokers to have made a cigarette quit attempt in the past year (44.7%, 95% CI 41.6–47.8% versus 37.0%, 95% CI 36.5–36.6) (Figure 1). Nearly half (48.0%, 95% CI 43.5%–52.6%) of dual users reported using smokeless tobacco for cessation on their most recent quit attempt. However, the proportion who abstained from cigarettes for ≥ 30 days (11.7%, 95% CI 9.5–13.8% versus 10.2%, 95% CI 9.8–10.5%) or ≥ 6 months (3.6%, 95% CI 2.4–4.7% versus 2.6%, 95% CI 2.5–2.8%) did not differ appreciably between dual users and exclusive smokers.
Figure 1.
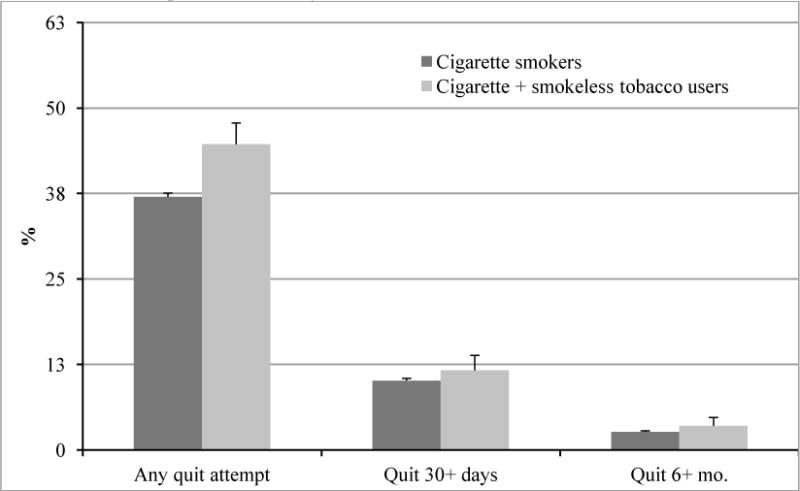
Quit attempts of 1 day or longer in the past year, ≥ 30 days, and ≥ 6 month among current cigarette smokers and cigarette and smokeless tobacco users (Tobacco Use Supplement to the Current Population Survey 2010–2011, N= 27,435)a
aP-value for difference in proportions between cigarette and cigarette and smokeless users for: quit attempt ≥ 1 day, p < 0.001; ≥ 30 days, p=0.1, ≥ 6 months, p=0.09
We used multivariate logistic regression to compare the rate of cigarette smoking quit attempts for dual users and exclusive smokers, accounting for cigarette dependence and adjusting for age, gender, and race/ethnicity. In the model with main effects only (not shown), the adjusted odds ratio (ORadj) for dual use was 1.33 (95% CI 1.15–1.53) demonstrating that dual users were more likely to have made a quit attempt compared to similar exclusive smokers, consistent with the bivariate results. However, the interaction terms between tobacco use status and cigarette consumption category (p<0.001) and between tobacco use status and time to first cigarette (p<0.01), met criteria for inclusion in the model, indicating that the difference between dual users and exclusive smokers varied by cigarette dependence. We incorporated these interactions by using stratified versions of the cigarette dependence indicators (Table 2). In the final model the main effect for dual use was no longer significant; thus, among less dependent smokers, i.e. low rate smokers (reference category) and those waiting more than 30 minutes to smoke in the morning (reference category), there was no significant difference between dual users and exclusive smokers in odds of making a quit attempt. However, with increased cigarette dependence, whether measured by greater daily cigarette consumption or smoking within 30 minutes of waking, there were lower odds of making a quit attempt among exclusive smokers, but not among dual users. Hence, for less dependent smokers, dual users and exclusive smokers made quit attempts at the same rate; among more dependent smokers, dual users were more likely to have made a quit attempt. As expected, quit attempts were more likely among younger and more highly educated smokers, and more likely among African Americans and less likely among Hispanics, compared to non-Hispanic whites.
Table 2.
Multivariate logistic regression models with outcome a quit attempt of 1 day or longer in the past year, among current smokers (TUS-CPS 2010–2011, N=24,537)
| Adjusted odds ratio (95% CI) | |
|---|---|
| Tobacco use status | |
| Exclusive smokers (reference) | 1 |
| Dual users | 0.96 (0.66–1.39) |
| Cigarette consumption within tobacco use statusb | |
| Exclusive smokers and < 12 cigarettes per month (reference) | 1 |
| Exclusive smokers and 0 to 10 cpd | 0.92 (0.85–1.00) |
| Exclusive smokers and 11 to 20 cpd | 0.54 (0.49–0.59)*** |
| Exclusive smokers and ≥ 21 cpd | 0.36 (0.32–0.49)*** |
| Dual users and < 12 cigarettes per month (reference) | 1 |
| Dual users and 0 to 10 cpd | 0.96 (0.62–1.49) |
| Dual users and 11 to 20 cpd | 0.85 (0.52–1.38) |
| Dual users and ≥ 21 cpd | 0.65 (0.36–1.18) |
| Time to first cigarette within tobacco use statusc | |
| Exclusive smokers and time to first cigarette ≥30 minutes after waking | 1 |
| Exclusive smokes and time to first cigarette < 30 minutes after waking | 0.76 (0.73–0.80)*** |
| Dual users and time to first cigarette ≥30 minutes after waking | 1 |
| Dual users and time to first cigarette < 30 minutes after waking | 0.89 (0.64–1.25) |
| Age | |
| 18–24 years (reference) | 1 |
| 25–34 years | 0.93 (0.86–1.01) |
| 35–49 years | 0.83 (0.77–0.91)*** |
| 50–64 years | 0.78 (0.72–0.85)*** |
| ≥ 65 years | 0.62 (0.56–0.67)*** |
| Sex | |
| Female (reference) | 1 |
| Male | 1.01 (0.96–1.05) |
| Race/ethnicity | |
| White (reference) | 1 |
| Hispanic | 0.87 (0.79–0.95)** |
| African American | 1.11 (1.03–1.21)** |
| Asian/PI | 0.87 (0.75–1.01) |
| Mixed/Other | 1.14 (0.99–1.28) |
| Education | |
| < High school (reference) | 1 |
| High school | 1.09 (1.02–1.16)* |
| Some college | 1.26 (1.17–1.35)*** |
| College graduate | 1.10 (1.02–1.19)* |
| Age of smoking initiation | |
| Age of smoking initiation > 15 years (reference) | |
| Age of smoking initiation ≤ 15 years | 1.01 (0.96–1.06) |
p < 0.05
p< 0.005
p<0.001
p-value for interaction term between tobacco use status and consumption < 0.001
p-value for interaction term between tobacco use status and smoking within 30 minutes of waking < 0.01
We then used multivariate logistic regression to compare the rate of 30 day smoking abstinence between dual users and exclusive smokers, adjusting for demographic factors. Dual use was not associated with achieving 30 day abstinence on the most recent quit attempt in an adjusted logistic regression model (Table 3), consistent with the bivariate results. There was no difference in the effect of cigarette dependence levels between dual users and exclusive smokers (p-value for each interaction > 0.25). Higher cigarette consumption and smoking within 30 minutes of waking were associated with markedly decreased odds of abstinence at 30 days, equally for both groups.
Table 3.
Adjusted logistic regression model predicting a 30-day quit attempt among current smokers (TUS-CPS 2010–2011, N= 24,537)
| Adjusted odds ratio (95% CI)b, c | |
|---|---|
| Tobacco use status | |
| Exclusive smokers (reference) | 1 |
| Dual users | 1.09 (0.88–1.37) |
| Cigarette consumption | |
| < 12 cigarettes per month (reference) | 1 |
| 0 to 10 cigarettes per day | 0.42 (0.38–0.47)*** |
| 11 to 20 cigarettes per day | 0.24 (0.22–0.27)*** |
| ≥ 21 cigarettes per day | 0.14 (0.11–0.12)*** |
| Time to first cigarette | |
| Time to first cigarette ≥30 minutes after waking | 1 |
| Time to first cigarette < 30 minutes after waking | 0.64 (0.58–0.69)*** |
| Age | |
| 18–24 years (reference) | 1 |
| 25–34 years | 1.11 (0.97–1.27) |
| 35–49 years | 0.95 (0.85–1.07) |
| 50–64 years | 0.87 (0.77–0.98)* |
| ≥ 65 years | 0.94 (0.89–1.10) |
| Sex | |
| Female (reference) | 1 |
| Male | 1.03 (0.96–1.09) |
| Race/ethnicity | |
| White (reference) | 1 |
| Non-white | 1.19 (1.09–1.28)*** |
| Education | |
| < High school (reference) | 1 |
| High school | 1.07 (0.97–1.27) |
| Some college | 1.14 (1.03–1.27)* |
| College graduate | 1.13 (1.01–1.28)* |
| Age of smoking initiation | |
| Age of smoking initiation > 15 years (reference) | |
| Age of smoking initiation ≤ 15 years | 1.16 (1.07–1.25)*** |
p < 0.05
p< 0.005
p<0.001
p-value for interaction term between tobacco use status and consumption =0.253
p-value for interaction term between tobacco use status and smoking within 30 minutes of waking = 0.91
3.3. Duration of abstinence among those who made a quit attempt
For those who had made a quit attempt, we compared the duration of abstinence between dual users and exclusive smokers using Cox proportional hazards regression (Table 4). Middle aged smokers, Hispanics and African Americans had significantly higher hazard of relapse than did younger or non-Hispanic white smokers. Increased cigarette consumption was associated with a greater hazard of relapse, equally for dual users and exclusive smokers (p-value for interaction 0.5), becoming nearly double at the highest consumption level (HRadj 1.95). Time to first cigarette within 30 minutes of waking was associated with a 20% higher hazard of relapse to smoking among exclusive smokers, but did not confer increased risk of relapse among dual users. The main effect for dual use conferred a 13% increased risk of relapse, at all cigarette dependence levels.
Table 4.
Cox proportional hazards model predicting time to relapse on most recent quit attempt, among current smokers who made a quit attempt in the past year (TUS-CPS 2010–2011, N= 9249). Note: HR>1 indicates faster relapse.
| Adjusted hazard ratio (95% CI) | |
|---|---|
| Tobacco use status | |
| Exclusive smokers (reference) | 1 |
| Dual users | 1.13 (1.02–1.26)* |
| Cigarette consumption | |
| < 12 cigarettes per month (reference) | 1 |
| 0 to 10 cigarettes per day | 1.49 (1.41–1.56)*** |
| 11 to 20 cigarettes per day | 1.70 (1.61–1.79)*** |
| ≥ 21 cigarettes per day | 1.95 (1.79–2.13)*** |
| Smoking within 30 minutes of waking | NA |
| Time to first cigarette within tobacco use statusc | |
| Exclusive smokers and time to first cigarette ≥30 minutes after waking | 1 |
| Exclusive smokes and time to first cigarette < 30 minutes after waking | 1.20 (1.16–1.25)*** |
| Dual users and time to first cigarette ≥30 minutes after waking | 1 |
| Dual users and time to first cigarette < 30 minutes after waking | 1.00 (0.84–1.20) |
| Age | |
| 18–24 years (reference) | 1 |
| 25–34 years | 0.98 (0.93–1.04) |
| 35–49 years | 1.06 (1.00–1.12)* |
| 50–64 years | 1.07 (1.02–1.13)* |
| ≥ 65 years | 1.02 (0.94–1.08) |
| Sex | |
| Female (reference) | 1 |
| Male | 0.99 (0.96–1.02) |
| Race/ethnicity | |
| White (reference) | 1 |
| Hispanic | 0.93 (0.88–0.99)* |
| African American | 0.93 (0.88–0.97)** |
| Asian/PI | 0.93 (0.88–0.99) |
| Mixed/Other | 1.09 (0.99–1.20) |
| Education | |
| < High school (reference) | 1 |
| High school | 1.01 (0.97–1.08) |
| Some college | 1.02 (0.97–1.08) |
| College graduate | 0.98 (0.92–1.04) |
| Age of smoking initiation (regular use) | |
| Age of smoking initiation > 15 years (reference) | 1 |
| Age of smoking initiation ≤ 15 years | 0.97 (0.93–1.00) |
p < 0.05
p< 0.005
p<0.001
p-value for interaction term between tobacco use status and consumption = 0.32
p-value for interaction term between tobacco use status and time to first cigarette after waking = 0.06
4. Discussion
In this nationally representative sample of current adult cigarette smokers, we found a higher proportion of dual users (45%) than exclusive smokers (37%) had attempted to quit cigarette smoking during the previous year. In models which adjusted for demographic factors, dual users remained significantly more likely than exclusive smokers to have made a cigarette smoking quit attempt. Indeed, many dual users appeared to use smokeless tobacco as a smoking cessation aid: 48% of dual users who made a quit attempt reported “trying to quit smoking by switching to smokeless tobacco” on their most recent attempt. We also investigated the duration of the most recent past year quit attempt. In Cox models adjusted for demographic differences and cigarette dependence, dual users showed a 13% higher hazard of relapse to smoking than exclusive smokers. Thus, dual users appeared to have made a quit attempt more readily but also to have relapsed more quickly, with the result that there was no difference between dual users and exclusive smokers in the proportion which attained 30-day smoking abstinence on their most recent quit attempt, in adjusted or unadjusted models.
In this study, we focused on current smokers at survey and investigated their recent cessation history, enabling us to measure cigarette dependence. Among all smokers, regardless of smokeless tobacco use, the most important determinant of attaining 30-day abstinence was cigarette consumption. Smokers with consumption greater than 20 cigarettes per day had 85% lower adjusted odds of having attained 30 day abstinence compared to low-rate smokers, and this applied equally to dual users and exclusive smokers. However, the pattern of cessation attempts and relapse was different for dual users and for exclusive smokers, and the difference was greater with higher levels of cigarette dependence.
At the lowest cigarette dependence levels, there was no difference in attempted cessation rates between dual users and exclusive smokers. Among exclusive smokers, as expected, higher cigarette dependence was associated with lower odds of a quit attempt. For example, those who smoked more than 20 cigarettes per day had odds of a quit attempt reduced by more than 60%. Similarly, exclusive smokers who smoked within 30 minutes of waking were 20% less likely to have made a quit attempt. However, among dual users neither of these cigarette dependence measures were associated with lower rates of cessation attempts, perhaps because heavily dependent dual users have an alternative nicotine source readily available.
Once in a cessation attempt, dual users had a faster rate of relapse, even at the lowest dependence levels. For both dual users and exclusive cigarette smokers, higher cigarette consumption predicted a faster relapse rate. Interestingly, the shorter time to first cigarette after waking predicted a higher relapse among exclusive smokers but not among dual users, again perhaps because heavily dependent dual users had an alternative nicotine source readily available. These differences in cessation behavior by cigarette consumption levels suggest the need for better generalized nicotine dependence measures, which account for use of multiple nicotine products.
Dual users were younger, more likely to be non-Hispanic white males, and more likely to have completed high school, but less likely to have attended college. These demographic variables have been associated with differences in both attempted and successful cessation in prior studies,26,28 and our models adjusted for these factors. The pattern of high cessation attempts and increased relapse is characteristic of younger smokers26 and was seen among dual users even in our adjusted models.
The high cessation attempt rate among dual users is consistent with their high reported use of smokeless tobacco as a cessation aid. Almost half of dual users who tried to quit reported “switching” to smokeless tobacco on their last quit attempt. In this cross-sectional study we were not able to assess smokeless use at the time of the quit attempt, and it is possible that some dual users may have initiated smokeless tobacco use as part of the smoking cessation attempt. Under this scenario, it is possible that dual use might be associated with lower rates of cigarette smoking cessation if, for example, smokeless tobacco was substituted for other potentially more effective smoking cessation aids. Because our data are cross-sectional, we are not able to rule out this possibility, highlighting the need for longitudinal studies of smoking behavior at the population level.
Few prior studies have compared population quit attempt rates between cigarette smokers who do and do not use smokeless tobacco. One study showed that daily snuff users were more likely than never-users to have quit smoking in the preceding 12 months, whereas occasional snuff users were more likely to have tried to quit smoking but were less likely to succeed,15 similar to our results in the present study. Another study reported a higher abstinence rate among those who used smokeless tobacco as a cessation aid on their last quit attempt;9 however, this study reported only 43 smokeless tobacco users. Additional studies were limited by a small sample size9 or a population that was not nationally representative.17
Strengths of our study include the use of a nationally representative sample, comparison of cessation behaviors between groups at the same time point using consistent methodology, and control of potential confounding factors including cigarette dependence. However, our study has several limitations. As in our prior work,26,27,30,31 we relied on self-reported recalled cessation history, potentially leading to recall bias and over- or under-estimation of cessation rates. However, as in prior studies, any such bias is expected to apply equally to our comparison groups, so that relative comparisons can be expected to be informative. Our smokeless tobacco use and cigarette consumption measures were assessed at the time of survey, not at the time of the quit attempt, a limitation of this cross-sectional study, and we lacked measures of smokeless tobacco use behaviors such as consumption level and frequency of use. We excluded recent former smokers who were still abstinent at survey because, as we have noted in prior work,26 recalled cigarette consumption among abstinent smokers is consistently biased upwards compared to current smokers, leading to the paradoxical result that high consumption predicts abstinence. Thus we compared very recent cessation history among current smokers. However, because the vast majority of cessation attempts end in relapse and the strongest predictor of prolonged abstinence is prior abstinence,30 such a comparison is highly relevant. Despite these limitations, our methodology is consistent in its treatment of exclusive smokers and dual users, and thus these relative comparisons are expected to be informative. However, prospective studies examining the association of smokeless tobacco use and subsequent cigarette cessation are needed.
5. Conclusions
We compared the most recent past year cigarette smoking quit attempt between dual users of cigarettes and smokeless tobacco and exclusive smokers, and found that while dual users were more likely to have attempted to quit smoking, they were also faster to have relapsed. There was no difference in attained 30-day smoking abstinence rates between dual users and exclusive smokers. Many dual users reported use of smokeless tobacco as a smoking cessation aid, and the pattern of more likely cessation attempts, but faster relapse among dual users, was especially pronounced with greater cigarette consumption. Low cigarette consumption was the strongest predictor of having attained 30-day abstinence from smoking for dual users and exclusive smokers alike, with no difference in effect size. Our cross-sectional study compared current smokers to current dual users, and was unable to assess smokeless tobacco use at the time of the reported quit attempt. Prospective studies at the population level are needed to clarify the role of smokeless tobacco in cigarette smoking cessation.
Highlights.
We compared current cigarette smokers to concurrent users of cigarettes and smokeless tobacco.
Data were from the Tobacco Use Supplement - Current Population Survey, 2010/11.
Dual users were more likely to have tried to quit cigarette smoking in the past year.
Dual users were faster to relapse, and no more likely to report 30 day abstinence.
The best predictor of smoking abstinence was a low smoking rate, for both groups.
Acknowledgments
Role of Funding Sources
This project has been funded in whole or in part with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services, under Contract No. HHSN271201100027C, UC Tobacco-Related Disease Research Program grants 21RT-0135, and National Cancer Institute grant No. 1R01CA172058-02. The funding sources had no involvement in the study design, collection, analysis, or interpretation of data, writing the manuscript and the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Karen Messer, Maya Vijayaraghavan, Martha M. White, Yuyan Shi, Cindy Chang, Wilson M. Compton, and John P. Pierce, contributed to the study design, analysis, and interpretation of data and writing the manuscript. All authors contributed to and approved the final manuscript.
Conflict of Interest
Wilson Compton has a potential conflict of interest in that he has minimal stock holdings in Pfizer, General Electric, and 3M Corporation, all of whom are considered organizations related to health research. There are no conflicts of interest for any other authors of this manuscript.
Disclaimer: The views and opinions expressed in this presentation are those of the authors only and do not necessarily represent the views, official policy or position of the US Department of Health and Human Services or any of its affiliated institutions or agencies.
References
- 1.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services CfDCaP, Office of Smoking and Health; Atlanta, Georgia: 2012. [Google Scholar]
- 2.Carpenter CM, Connolly GN, Ayo-Yusuf OA, Wayne GF. Developing smokeless tobacco products for smokers: an examination of tobacco industry documents. Tob Control. 2009 Feb;18(1):54–59. doi: 10.1136/tc.2008.026583. [DOI] [PubMed] [Google Scholar]
- 3.Mejia AB, Ling PM. Tobacco industry consumer research on smokeless tobacco users and product development. Am J Public Health. 2010 Jan;100(1):78–87. doi: 10.2105/AJPH.2008.152603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: findings from national surveys. Tob Control. 2010 Apr;19(2):104–109. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Backinger CL, Fagan P, O’Connell ME, et al. Use of other tobacco products among U.S. adult cigarette smokers: prevalence, trends and correlates. Addict Behav. 2008 Mar;33(3):472–489. doi: 10.1016/j.addbeh.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McClave-Regan AK, Berkowitz J. Smokers who are also using smokeless tobacco products in the US: a national assessment of characteristics, behaviours and beliefs of ‘dual users’. Tob Control. 2011 May;20(3):239–242. doi: 10.1136/tc.2010.039115. [DOI] [PubMed] [Google Scholar]
- 7.Boffetta P, Hecht S, Gray N, Gupta P, Straif K. Smokeless tobacco and cancer. Lancet Oncol. 2008 Jul;9(7):667–675. doi: 10.1016/S1470-2045(08)70173-6. [DOI] [PubMed] [Google Scholar]
- 8.Levy DT, Mumford EA, Cummings KM, et al. The potential impact of a low-nitrosamine smokeless tobacco product on cigarette smoking in the United States: estimates of a panel of experts. Addict Behav. 2006 Jul;31(7):1190–1200. doi: 10.1016/j.addbeh.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Rodu B, Phillips CV. Switching to smokeless tobacco as a smoking cessation method: evidence from the 2000 National Health Interview Survey. Harm Reduct J. 2008;5:18. doi: 10.1186/1477-7517-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frost-Pineda K, Appleton S, Fisher M, Fox K, Gaworski CL. Does dual use jeopardize the potential role of smokeless tobacco in harm reduction? Nicotine Tob Res. 2010 Nov;12(11):1055–1067. doi: 10.1093/ntr/ntq147. [DOI] [PubMed] [Google Scholar]
- 11.Bates C, Fagerstrom K, Jarvis MJ, Kunze M, McNeill A, Ramstrom L. European Union policy on smokeless tobacco: a statement in favour of evidence based regulation for public health. Tob Control. 2003 Dec;12(4):360–367. doi: 10.1136/tc.12.4.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatsukami DK, Lemmonds C, Tomar SL. Smokeless tobacco use: harm reduction or induction approach? Prev Med. 2004 Mar;38(3):309–317. doi: 10.1016/j.ypmed.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Parascandola M. Tobacco harm reduction and the evolution of nicotine dependence. Am J Public Health. 2011 Apr;101(4):632–641. doi: 10.2105/AJPH.2009.189274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blank MD, Nasim A, Hart A, Jr, Eissenberg T. Acute effects of cigarillo smoking. Nicotine Tob Res. 2011 Sep;13(9):874–879. doi: 10.1093/ntr/ntr070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomar S. Snuff Use and Smoking in U.S. Men. Am J Prev Med. 2002;23(3):143–149. doi: 10.1016/s0749-3797(02)00491-9. [DOI] [PubMed] [Google Scholar]
- 16.Zhu SH, Wang JB, Hartman A, et al. Quitting cigarettes completely or switching to smokeless tobacco: do US data replicate the Swedish results? Tob Control. 2009 Apr;18(2):82–87. doi: 10.1136/tc.2008.028209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wetter DW, McClure JB, de Moor C, et al. Concomitant use of cigarettes and smokeless tobacco: prevalence, correlates, and predictors of tobacco cessation. Prev Med. 2002 Jun;34(6):638–648. doi: 10.1006/pmed.2002.1032. [DOI] [PubMed] [Google Scholar]
- 18.Fiore M, Jaén C, Baker T, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 19.U.S. Census Bureau. Current Population Survey - Design and Methodology. U.S Department of Labor Bureau of Labor Statistics USDoCEaSAUSCB; Vol Technical Paper 63RV2002. [Google Scholar]
- 20.US Department of Commerce CB. National Cancer Institute-sponsored Tobacco Use Supplement to the Current Population Survey 2010–11. Available At: http://appliedresearch.cancer.gov/tus-cps/. Technical documentation: http://www.census.gov/cps/methodology/techdocs.html. 2012 Accessed December, 2014.
- 21.Gilpin EA, Emery S, White MM, Pierce JP. Changes in youth smoking participation in California in the 1990s. Cancer Causes Control. 2003 Dec;14(10):985–993. doi: 10.1023/b:caco.0000007971.36237.a5. [DOI] [PubMed] [Google Scholar]
- 22.Gilpin EA, Lee L, Evans N, Pierce JP. Smoking initiation rates in adults and minors: United States, 1944–1988. Am J Epidemiol. 1994;140(6):535–543. doi: 10.1093/oxfordjournals.aje.a117280. [DOI] [PubMed] [Google Scholar]
- 23.Kozlowski LT, Porter CQ, Orleans CT, Pope MA, Heatherton T. Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug and Alcohol Depend. 1994;34(3):211–216. doi: 10.1016/0376-8716(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 24.Fagerstrom KO, Heatherton TF, Kozlowski LT. Nicotine addiction and its assessment. Ear, nose, & throat journal. 1990 Nov;69(11):763–765. [PubMed] [Google Scholar]
- 25.Pierce JP, Messer K, White MM, Cowling DW, Thomas DP. Prevalence of heavy smoking in California and the United States, 1965–2007. JAMA. 2011 Mar 16;305(11):1106–1112. doi: 10.1001/jama.2011.334. [DOI] [PubMed] [Google Scholar]
- 26.Messer K, Trinidad DR, Al-Delaimy WK, Pierce JP. Smoking cessation rates in the United States: a comparison of young adult and older smokers. Am J Public Health. 2008 Feb;98(2):317–322. doi: 10.2105/AJPH.2007.112060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Messer K, Pierce JP, Zhu SH, et al. The California Tobacco Control Program’s effect on adult smokers: (1) Smoking cessation. Tob Control. 2007 Apr;16(2):85–90. doi: 10.1136/tc.2006.016873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Messer K, Mills AL, White MM, Pierce JP. The effect of smoke-free homes on smoking behavior in the U.S. Am J Prev Med. 2008 Sep;35(3):210–216. doi: 10.1016/j.amepre.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 29.Judkins D. Fay’s Method for Variance Estimation. Journal of Official Statistics. 1990;6(3):223–239. [Google Scholar]
- 30.Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst. 1997;89:572–576. doi: 10.1093/jnci/89.8.572. [DOI] [PubMed] [Google Scholar]
- 31.Gilpin EA, Messer K, Pierce JP. Population effectiveness of pharmaceutical aids for smoking cessation: what is associated with increased success? Nicotine Tob Res. 2006 Oct;8(5):661–669. doi: 10.1080/14622200600910801. [DOI] [PubMed] [Google Scholar]


