Abstract
STUDY DESIGN
Randomized controlled trial.
OBJECTIVES
Examine the effects of weight-bearing (WB) biofeedback training on WB symmetry and functional joint moments following unilateral total knee arthroplasty (TKA).
BACKGROUND
Individuals post unilateral TKA place more weight on the non-surgical limb compared to the surgical limb during function. It is unknown if targeted intervention can improve surgical limb use and resolve altered movement patterns.
METHODS
Twenty-six patients were randomized to 2 groups: RELOAD or CONTROL. The RELOAD group had standard of care rehabilitation augmented with WB biofeedback training and the CONTROL group had dose-matched standard of care. Lower limb weight-bearing ratios (WBRs) were measured preoperatively and 6 and 26 weeks after TKA during a Five Times Sit-to-Stand Test (FTSST) and walking. Secondary outcomes were FTSST time, walking speed, and lower limb joint moments during the FTSST and walking.
RESULTS
No between-group differences were found in WBR. FTSST time improved in the RELOAD group compared to the CONTROL group at 6 (P=.021) and 26 weeks (P=.021) and there was a tendency for improved walking speed in the RELOAD group at 26 weeks (P=.068). There were no between-group differences in knee extension moment during the FTSST. Surgical-limb knee extension moments during walking increased from baseline to 26 weeks in the RELOAD group and decreased in the CONTROL group (P=.008).
CONCLUSION
WB biofeedback training had no effect on functional WB symmetry or knee extension moments during the FTSST. However, the biofeedback training resulted in increases of knee extension moments during gait and improved FTSST times.
LEVEL OF EVIDENCE
Therapy, level 2b.
Keywords: Gait, Joint Moments, Movement Asymmetry, Sit to Stand, TKA
INTRODUCTION
Individuals recovering from unilateral total knee arthroplasty (TKA) have asymmetrical lower extremity movement patterns, characterized by decreased weight-bearing (WB) and decreased knee extension moments on the surgical limb compared to the non-surgical limb.4, 13, 22, 31 Such asymmetrical WB and lower limb joint mechanics following TKA are associated with poor physical function outcomes3, 24, 30 and are linked to weakness in the quadriceps, which is a key muscle related to physical function following TKA.22, 30 Decreased surgical limb WB during functional activity may also be linked to long-term problems following unilateral TKA, including functional limitations and contralateral knee and hip joint pain.25
Recovery of typical movement patterns following unilateral TKA may be possible through early interventions targeting symmetry training. A symmetry retraining intervention has been described in a case report of a patient after unilateral TKA.20 The patient followed in the report demonstrated improved knee motion symmetry, which was comparable to a “healthy” cohort. These findings are preliminary evidence that such a rehabilitation approach may lead to improved symmetry of gait mechanics and better physical function. Similar positive results of movement pattern training have been noted after unilateral TKA in a longitudinal cohort study.32 In that study, movement symmetry training during leg-press and squat exercises resulted in greater use of the surgical knee, as measured by knee extension moments during walking, compared to an historical cohort without symmetry training.
Movement pattern re-education is rarely described as a component of physical rehabilitation programs, and few studies have examined the efficacy of these reeducation techniques in patients following joint replacement.14, 20, 27 Only 1 randomized controlled trial has examined the use of WB biofeedback to retrain movement patterns following TKA,14 but follow up was limited to the immediate postoperative period (first 2 weeks after surgery), the study included a diverse population of patients (TKA, total hip arthroplasty, lower extremity amputation, and hip fracture), and the authors only examined WB on the affected limb as the outcome. Identifying the effect of movement pattern re-education on lower limb movement symmetry and overall physical function is necessary to inform rehabilitation guidelines following TKA.
The purpose of this study was to conduct a preliminary examination of WB biofeedback training in altering WB between-limb symmetry and physical function after unilateral TKA. The primary aim was to examine lower limb WB symmetry during sit-to-stand transitions and walking. The secondary aim was to examine the initial effects of the WB biofeedback training on functional performance and lower limb joint moments during the same motions of sit-to-stand transitions and walking. We hypothesized that post TKA, the interventional RELOAD group, compared to the CONTROL group, would have greater symmetry in WB at the end of 6 weeks for both sit-to-stand transitions and walking, and that those between-group differences would persist over time (26 weeks).
METHODS
This study was a randomized controlled trial with blinded evaluators. Patients were randomly assigned to 1 of 2 groups: standard of care rehabilitation plus WB biofeedback training (RELOAD) or standard of care rehabilitation alone (CONTROL). Total dose of exercise was designed to be similar between groups. The protocol for this study was approved by the Colorado Multiple Institutional Review Board. Informed consent was obtained from all patients prior to participation.
Patients
Twenty-six patients (mean ± age, 67.4 ± 8.2 years) with knee osteoarthritis (OA), scheduled to undergo unilateral TKA were enrolled in the study. Patients were recruited from March 2011 to April 2012 from 2 local hospital systems with a total of 9 participating orthopedic surgeons. Patients were excluded for the following reasons: 1) neurological, vascular, or cardiac problems that limited function, 2) contralateral knee pain (pain with activity greater than 2/10 on a numerical rating scale), 3) other orthopedic conditions in the lower extremities that limited function, 4) body mass index greater than 40 kg/m2, 5) uncontrolled diabetes, 6) smoking or drug abuse, 7) living greater than 45 minutes away from the outpatient rehabilitation clinic, 8) admission to a sub-acute inpatient rehabilitation facility, or 9) a surgical complication necessitating an altered course of rehabilitation. Patients were also excluded if they were unable to walk 30 meters without an assistive device or unable to rise from a chair without arm use.
Eligible volunteers were randomized with concealed allocation to 1 of 2 groups (RELOAD and CONTROL) using block sizes of 4 with stratification on sex. Randomization was carried out with a random number generator and occurred at the time of discharge from acute hospitalization to home. The timing of randomization allowed exclusion of patients who were discharged to sub-acute inpatient rehabilitation rather than home to better standardize the course of rehabilitation. A blinded investigator who did not have any interaction with the patients during the screening and enrollment process managed group allocation assignments.
Sample Size Determination
The primary outcome measure for this study was the WB ratio (WBR) during a Five Times Sit-to-Stand Test (FTSST) and walking. This outcome was chosen as it accurately quantifies WB asymmetry for patients post TKA.6, 22 Standard deviation of WBR during the FTSST was estimated to be 0.16 at 6 weeks after TKA based upon previous data from our laboratory.7 Group sample sizes of 12 were calculated to achieve 80% power to detect a between-group difference in means of 0.19 in WBR using a 2-sided t-test at an alpha level of .05 (SAS Institute, Cary, NC).
Intervention
All patients, regardless of group assignment, received rehabilitation in the acute care setting and home-health physical therapy setting. Patients were seen twice a day in the acute care setting with a mean ± SD length of stay of 3.2 ± 0.6 days. Both hospitals utilized in the study had similar postoperative physical therapy protocols that consist of performing active and passive range of motion (ROM) exercises, transfer training, gait training, and stair training (if a patient has stairs to enter their home). Patients were seen 1 to 3 times per week in the home-health setting depending on the plan of care dictated by the treating therapist. A suggested home exercise program (HEP) was given to therapists for patient implementation and a study coordinator spoke with patients and treating therapists in both groups on a weekly basis to ensure similarity of HEPs between groups. Patients in both groups completed an adherence log, which tracked number of daily exercise sessions. Patients in both groups were contacted on a weekly basis to remind them to complete the log.
Patients discharged from home-health physical therapy prior to the 6-week testing session received additional outpatient physical therapy treatment. All patients in outpatient physical therapy were treated by 1 of 2 physical therapists. Outpatient physical therapy treatment included passive and active ROM exercises, WB functional activities, stationary biking, modalities (ice and heat), and education. Home-health and outpatient rehabilitation did not include techniques such as mirrors or bathroom scales to retrain movement patterns. Exercise dosage was controlled by having patients in the CONTROL group complete their HEP twice daily over the 6 week period, whereas patients in the RELOAD group were instructed to complete their standard of care HEP once daily and their WB biofeedback HEP once daily.
Patients in the RELOAD group were seen twice weekly in the home setting over the 6 weeks following surgery for WB biofeedback training. All treatments were performed by the same physical therapist. A Nintendo Wii gaming system was installed on a television of the patient’s choosing at the first visit and patients kept this system for the remainder of their treatment. The Nintendo Wii Fit Plus game and associated Wii Balance Board were utilized for WB biofeedback training (Nintendo of America, Inc, Redmond, WA). A standard bariatric walker was placed around the balance board, which was placed in front of a sturdy chair so the patient was protected on all sides from a potential fall. Patients were instructed in a progressive series of games, depending on ability level, and received feedback on proper performance of each task while playing the corresponding game (TABLE 1). All patients began with a static bilateral stance task and a sit to stand task. Their program was progressed to include dynamic elements, such as weight shifting during bilateral stance, and sit to stand was progressed with depth and speed based on the tolerance and ability to perform progressively more difficult tasks. Unilateral stance activities were added to the intervention program once patients could place 100% of their body weight through their surgical limb. Lunging activities were added to the intervention program once patients were able to perform a sit to stand with symmetrical WB. Patients were issued a WB biofeedback HEP corresponding to their level of ability at the end of each treatment and instructed to complete that HEP once daily until the next treatment.
TABLE 1.
Description of activities for the RELOAD group using weight-bearing biofeedback
| Activity | Weight-bearing Biofeedback Progression Tasks (Games) |
|---|---|
| Bilateral Stance |
|
| Unilateral Stance |
|
| |
| Sit to Stand |
|
| |
| |
| |
| Lunging |
|
|
Note: Patients were progressed within each activity as able.
Outcome Measures
WB and movement pattern outcomes were assessed with 3-dimensional motion analysis, with the data collected and processed by an evaluator who was blinded to group assignment. All patients were tested at pre-op (1–2 weeks prior to TKA), the end of the intervention (6 weeks after TKA), and a long-term follow up (26 weeks after TKA). Kinetic and kinematic data were collected with 2 embedded force plates (Bertec Corporation, Columbus, OH) to measure vertical ground reaction force at 2000 Hz and a 6-camera motion analysis system (Vicon Motion Systems, Oxford, UK) to measure reflective marker positions at 100 Hz. Reflective markers were placed on the patient at specific landmarks of the upper limbs, trunk, and lower limbs (modified Helen Hayes marker set).15 Marker coordinates and force data were low-pass filtered using a fourth order Butterworth filter (cut-off frequency: 6 Hz for the reflective markers and 20 Hz for the ground reaction forces).
Weight-bearing Ratio
WBRs of peak vertical ground reaction force (vGRF) under each limb were calculated during the FTSST as previously described and during the stance phase of walking as previously described:6
A WBR of 1.0 indicates perfect symmetry during the performance of the task. Ratios less than 1.0 indicate less weight being placed on the surgical limb and greater asymmetry.
Functional Performance
The FTSST was used to measure the time required to rise from and return to a chair 5 times in a row.28 Previous studies have shown that WB asymmetry during the FTSST is related to strength and functional performance.6, 17 Patients began this test seated on an armless bath chair set to the height of their fibular head and were then asked to stand up and sit down 5 times in a row as fast as they could. Patients were not allowed to use their arms to push on their thighs or on the chair, thus eliminating any attempts to compensate for lower extremity weakness with arm strength. The patients were given verbal instruction, as the instructor performed the test for demonstration. The patients were then allowed to practice several sit-stand transitions before performance of the timed test trials. The patient performed 2 trials and the average data of the 2 trials were used for analysis. The FTSST has high test-retest reliability, with correlation coefficients greater than 0.90 for older adult populations.11, 17 A 2.3 second change in FTSST time has been positively correlated with improvements on the Timed Up and Go Test and improvements on the Dynamic Gait Index in adults undergoing vestibular rehabilitation.21
Gait trials were collected while patients walked on a 12-meter walkway equipped with the embedded force plates. Each patient was tested at his/her self-selected walking speed. All patients walked approximately 5 minutes to acclimate to the walkway. After acclimation, self-selected walking speed was recorded for 3 passes through the middle 6 meters of the walkway and the average of the 3 passes was used as the targeted self-selected speed for the measurement trials. Measurement of vGRF was completed after the acclimation period until 3 walking trials at the desired speed were recorded with clean force platform contacts by each foot and within ±5 % of the targeted gait speed for the trial. Gait speed has low measurement error for older adults (<5%)12 and good test-retest reliability, having within-session correlation coefficients ranging from 0.90–0.98 and between-session correlation coefficients ranging from 0.78–0.94 for patients with knee OA.23 Clinically important changes in gait speed have been estimated between 0.1 and 0.2 m/s for adults with pathology2 and adults undergoing short-term rehabilitation after TKA.1
Average vGRF during the FTSST was used as the WB measure for transitions between sitting and standing. Peak vGRF during the loading response phase of stance period, averaged over 3 trials, was used as the WB measure for the walking trials.
Movement Patterns
Joint moments were calculated during the FTSST trials using an inverse dynamics approach, with maximum hip, knee, and ankle moments identified and recorded for the rising (sit-to-stand) phase (average of the 5 repeated cycles). Similarly, individual joint moments were calculated at the time of maximum total limb support moment29 during the stance period of gait. All joint moments were normalized to total body mass. Joint moments are positively associated with joint loading at the knee, as well as degenerative cartilage changes over time for patients with knee OA.5, 18 A case report suggests that surgical knee extension moments increase after TKA rehabilitation focused on improving symmetry of WB during functional activities, including gait.32
Data Analysis
Differences between baseline and the postsurgical time points were analyzed using restricted maximum likelihood estimation of a multivariate repeated-measures mixed-effects model using all available data.16 All models contained fixed effects for the group by time interaction and a random effect for patients. If a significant group by time interaction was found post hoc testing was performed using linear contrasts conditioned on baseline values. The α level was set at .05 for all between group comparisons. All joint moment comparisons between groups were made for the surgical limb. Cohen’s D effect sizes for significant differences were calculated using the between-group magnitude of change from baseline divided by the pooled standard deviation at baseline at both 6 weeks and 26 weeks.10 Cohen’s D values of 0.20, 0.50, and 0.80 represent small, moderate, and large effect sizes, respectively.9
RESULTS
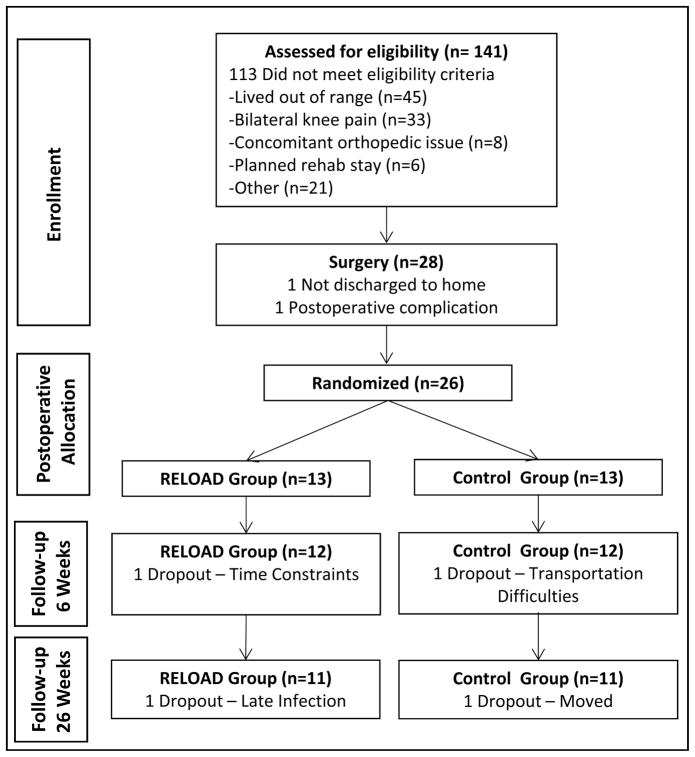
One hundred forty-one patients scheduled for TKA were assessed for eligibility (FIGURE 1). Prior to surgery, 113 patients did not meet the eligibility criteria. Following surgery, 2 patients were not enrolled due to a surgical complication and a change in discharge destination. Therefore, 26 patients (13 males, 13 females) were enrolled. One patient from each group dropped out of the study during the intervention, leaving 24 patients who completed the intervention and were assessed at the 6-week time point. One additional patient from each group dropped out between the 6 and the 26-week time point leaving 22 patients assessed at the 26-week time point.
FIGURE 1.
Participant flow diagram
The CONTROL group performed the standard of care HEP 1.8 ± 0.4 sessions per day, and the RELOAD group performed the standard of care HEP 1.0 ± 0.3 and the Wii HEP 0.8 ± 0.2 sessions per day. The total time spent for the RELOAD group with the Wii HEP was 14.2 ± 5.2 minutes per day, for a total time of 538 ± 199 minutes over the 6-week intervention. The RELOAD and CONTROL groups were comparable in age, sex distribution, and anthropometric measures (TABLE 2).
TABLE 2.
Pre-op characteristics of patients in both groups*
| Variable | RELOAD group (N = 13) | CONTROL group (N = 13) |
|---|---|---|
| Age (years) | 68.2 ± 8.6 | 66.6 ± 8.1 |
| Sex (n, % male) | 7 (53.8%) | 6 (46.2%) |
| Height (m) | 1.7 ± 0.1 | 1.7 ± 0.1 |
| Body mass (kg) | 83.5 ± 18.2 | 79.3 ± 12.2 |
| WBR during FTSST | 0.79 ± 0.10 | 0.85 ± 0.10 |
| WBR during Gait | 0.96 ± 0.06 | 0.94 ± 0.08 |
| FTSST time (s) | 11.4 ± 2.4 | 10.3 ± 2.5 |
| Walking speed (m/s) | 1.19 ± 0.22 | 1.24 ± 0.18 |
Abbreviations: FTSST, five times sit to stand test; WBR, weight-bearing ratio.
Values are mean ± standard deviation, except for sex.
Weight-Bearing Ratio
There were no statistically significant differences between groups in WBR during the FTSST (P=.329) or walking (P=.891) at the 6-week time point (TABLE 3).
TABLE 3.
Between group comparisons of WBR during functional tasks at each time point.
| Variable | Time Point | RELOAD group* | CONTROL group* | RELOAD-CONTROL** | Effect Size (Cohen’s D) |
|---|---|---|---|---|---|
| WBR during FTSST | Pre-op | 0.79 ± 0.10 | 0.85 ± 0.10 | - | - |
| 6-Week | 0.77 ± 0.10 | 0.80 ± 0.11 | 0.03 (−0.04, 0.10) P=.329 |
0.31 | |
| 26-Week | 0.88 ± 0.11 | 0.91 ± 0.13 | 0.03 (−0.06, 0.12) P=.511 |
0.31 | |
| WBR during Walking (Self-Selected Speed) | Pre-op | 0.96 ± 0.06 | 0.94 ± 0.08 | - | - |
| 6-Week | 0.94 ± 0.08 | 0.92 ± 0.09 | −0.01 (−0.08, 0.07) P=.891 |
−0.14 | |
| 26-Week | 0.98 ± 0.06 | 0.93 ± 0.06 | 0.03 (−0.05, 0.11) P=.402 |
0.41 |
Abbreviations: FTSST, five times sit to stand test; WBR, weight-bearing ratio
Values are means ± SD
Values are mean (95% CI) difference between groups from Pre-op
Functional Performance
There were between-group differences in the change of FTSST times from pre-op to 6 weeks (P=.021) and pre-op to 26 weeks (P=.021), with the CONTROL group having a greater increase in time to perform the test at 6 weeks and the RELOAD group having greater reduction in time to perform the test at 26 weeks (TABLE 4). There were no differences between groups in walking speed at 6 weeks (TABLE 5). However, at 26 weeks there was a tendency towards a faster walking speed by the RELOAD group (P=.068).
TABLE 4.
Between group comparison of the Five-Times Sit-to-Stand Test and joint moments during the Five-Times Sit-to-Stand Test at each time point.
| Variable | Time Point | RELOAD group* | CONTROL Group* | RELOAD-CONTROL** | Effect Size (Cohen’s D) |
|---|---|---|---|---|---|
| FTSST Time (s) | Pre-op | 11.4 ± 2.4 | 10.3 ± 2.5 | - | - |
| 6-Week | 11.5 ± 1.6 | 12.7 ± 3.3 | −2.3 (−4.2,−0.4)) P=.021 |
−0.94 | |
| 26-Week | 9.5 ± 2.4 | 9.6 ± 1.6 | −1.3 (−2.3,−0.2) P=.021 |
−0.53 | |
| Hip Moment (Nm/kg) | Pre-op | 0.68 ± 0.35 | 0.70 ± 0.19 | - | - |
| 6-Week | 0.73 ± 0.28 | 0.80 ± 0.26 | −0.05 (−0.20, 0.10) P=.509 |
−0.17 | |
| 26-Week | 0.65 ± 0.24 | 0.63 ± 0.20 | 0.04 (−0.17, 0.25) P=.686 |
0.14 | |
| Knee Moment (Nm/kg) | Pre-op | 0.90 ± 0.14 | 0.92 ± 0.26 | - | - |
| 6-Week | 0.77 ± 0.21 | 0.72 ± 0.18 | 0.06 (−0.12, 0.24) P=.500 |
0.29 | |
| 26-Week | 1.03 ± 0.22 | 0.97 ± 0.11 | 0.07 (−0.11, 0.26) P=.434 |
0.34 | |
| Ankle Moment (Nm/kg) | Pre-op | 0.29 ± 0.20 | 0.28 ± 0.16 | - | - |
| 6-Week | 0.29 ± 0.14 | 0.31 ± 0.17 | −0.04 (−0.18, 0.10) P=.607 |
−0.22 | |
| 26-Week | 0.17 ± 0.16 | 0.24 ± 0.14 | −0.09 (−0.23, 0.06) P=.227 |
−0.50 |
Abbreviations: FTSST, five times sit to stand test
Values are means ± SD
Values are mean (95% CI) difference between groups from
TABLE 5.
Between group comparisons of walking speed and joint moments during walking at each time point.
| Variable | Time Point | RELOAD group* | CONTROL group* | RELOAD-CONTROL** | Effect Size (Cohen’s D) |
|---|---|---|---|---|---|
| Walking Speed (m/s) | Pre-op | 1.19 ± 0.23 | 1.24 ± 0.18 | - | - |
| 6-Week | 1.20 ± 0.23 | 1.16 ± 0.20 | 0.08 (−0.07, 0.24) P=.289 |
1.13 | |
| 26-Week | 1.29 ± 0.25 | 1.24 ± 0.13 | 0.10 (−0.01, 0.20) P=.068 |
0.48 | |
| Hip Moment (Nm/kg) | Pre-op | 0.30 ± 0.32 | 0.20 ± 0.23 | - | - |
| 6-Week | 0.28 ± 0.26 | 0.26 ± 0.21 | −0.09 (−0.33, 0.16) P=.480 |
−0.32 | |
| 26-Week | 0.28 ± 0.19 | 0.36 ± 0.22 | −0.18 (−0.44, 0.07) P=.160 |
−0.65 | |
| Knee Moment (Nm/kg) | Pre-op | 0.41 ± 0.39 | 0.60 ± 0.29 | - | - |
| 6-Week | 0.47 ± 0.22 | 0.46 ± 0.37 | 0.21 (−0.06, 0.47) P=.120 |
0.61 | |
| 26-Week | 0.61 ± 0.25 | 0.42 ± 0.44 | 0.38 (0.10, 0.65) P=.008 |
1.11 | |
| Ankle Moment (Nm/kg) | Pre-op | 0.17 ± 0.20 | 0.12 ± 0.24 | - | - |
| 6-Week | 0.17 ± 0.23 | 0.17 ± 0.32 | −0.04 (−0.27, 0.17) P=.668 |
−0.18 | |
| 26-Week | 0.09 ± 0.29 | 0.01 ± 0.19 | 0.02 (−0.21, 0.25) P=.877 |
0.09 |
Values are means ± SD
Values are mean (95% CI) difference between groups from Pre-op
Movement Patterns
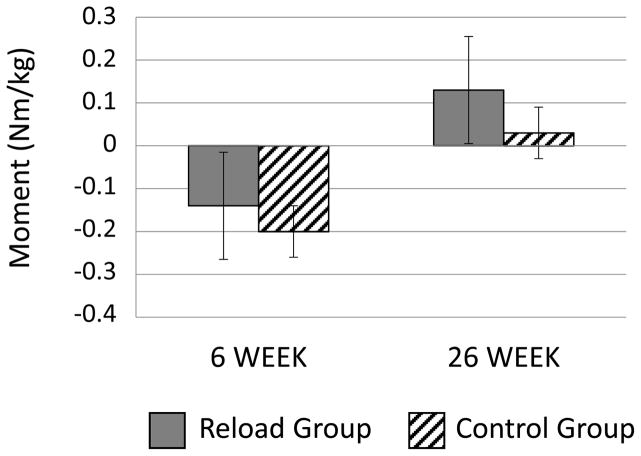
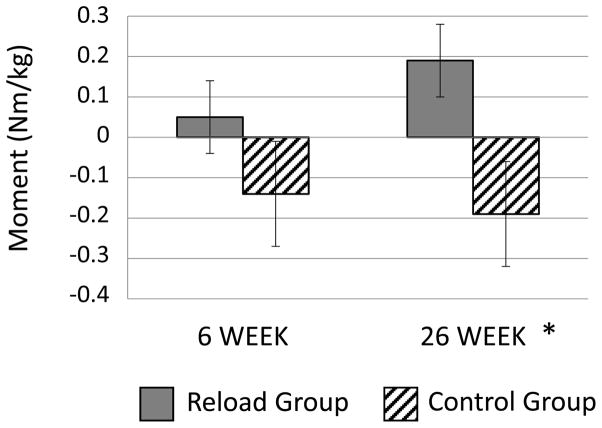
During the FTSST there were no statistically significant differences in any of the joint moments between groups (TABLE 4 and FIGURE 2). There was no statistically significant difference between groups in knee extension moment during walking from pre-op to 6 weeks, although a trend of increase was present for RELOAD compared to CONTROL (P=.101; TABLE 5 and FIGURE 3). From pre-op to 26 weeks, knee extension moment change showed a between-group difference (P=.008), with knee extension moments increasing in the RELOAD group and decreasing in the CONTROL group during walking. No statistically significant between-group differences were present for hip and ankle extension moments.
Figure 2.
Mean +/− SD changes in peak surgical-limb knee extension moment over time, compared to pre-op, for both groups during the Five-Times Sit-to-Stand Test.
FIGURE 3.
Mean +/− SE changes in peak surgical-limb knee extension moment over time, compared to pre-op, for both groups during walking.
* = significant differences between groups from baseline to 26 weeks (P=.007)
DISCUSSION
Functional movement pattern symmetry is an important outcome of physical rehabilitation following unilateral TKA, as altered movement patterns are linked to muscle weakness and poor functional performance.7, 22 Data from this study indicate that the addition of WB biofeedback training was no more effective than standard of care at improving WB symmetry during sit-stand transfers and walking. However, joint moment data suggest that a 6-week training program to improve surgical limb WB following unilateral TKA can effectively alter the quality of movement patterns. The surgical limb knee extension moment (at the time of maximum total limb support moment) improved during walking in the RELOAD group compared to the CONTROL group from pre-op testing to 26 weeks post-TKA. Additionally, functional performance on the FTSST improved and there was a tendency for improved walking speed in the RELOAD group.
There were no differences between groups in WBR during either the FTSST or walking at self-selected speeds. In contrast, it has been shown previously that individuals post-TKA have significantly less WB during gait on the surgical limb compared to the non-surgical limb (3 months after surgery) and that symmetry improves by 3 years after surgery.31 With our study sample, the WBRs indicated a high amount of symmetry pre-op, creating a ceiling effect for the amount of change that could occur with intervention. It is evident from our data that although a sub-population of patients have significant WB asymmetry before and early after unilateral TKA,4, 6, 8, 31 asymmetrical WBR does not characterize all patients. Other measures of movement pattern may be superior to WBR for capturing changes in movement quality before and after TKA.22 For example, although WBR was not different between groups, surgical-knee extension moment increased in the RELOAD group and decreased in the CONTROL group during walking from pre-op to 26 weeks, indicating possible increased quadriceps use in the RELOAD group.
Differences in FTSST times were present at both the end of intervention (6-week post TKA) and at the 26-week post TKA follow-up. The RELOAD group improved 2.3 seconds on the FTSST compared to the CONTROL group by the end of intervention. This represents a clinically meaningful change and reflects a large effect size (0.94). By 26 weeks, the observed difference between groups decreased to 1.3 seconds favoring the RELOAD group, which may not be clinically meaningful and represents a medium effect size (0.53).
Although between-group differences in FTSST times were present at both the end of intervention (6-week) and at follow-up (26-week), there were no statistically significant differences in joint moments between groups for this task. Within-group increase in knee extension moments for the RELOAD group may explain the improved FTSST times. Alternatively, the differences in FTSST time between groups may have been related to movement pattern changes not captured by maximum joint moments. For example, velocity of knee extension movement has been shown to persist during sit-to-stand transitions for people with TKA compared to healthy people of similar age and body mass index.4
WB biofeedback training may have had an effect on the habitual behavior of patients, resulting in improved loading of the surgical limb during routine daily activity. Interestingly, there was a trend of surgical limb knee extension moment increase in the RELOAD group and decrease in the CONTROL group during walking immediately after intervention (6 week), but differences were not statistically significant until 26-week post-TKA. The effect size of the observed changes between groups was moderate (0.61) at 6 weeks and large (1.11) at 26 weeks. It is possible that without intentional change in quality of movement pattern, chronic deficits in knee function may remain following TKA. This idea is supported by a study examining between-limb knee muscle function over the first 3 years after unilateral TKA.31 Although between limb symmetry of muscle function improved by year 3 after unilateral TKA, improvements were largely attributable to losses of strength in the non-surgical limb, and not gains in the surgical limb.31
Changes in knee extension moments during walking were accompanied by a tendency for improved walking speed in the RELOAD group compared to the CONTROL group. Similar to joint moments, the magnitude of change between groups was greater at 26 weeks than at 6 weeks. At 26 weeks, the RELOAD group tended to improve 0.10 m/s from baseline compared to the CONTROL group (P=.068). This magnitude of change represents a small effect (0.48) and is clinically meaningful.1, 2
The rehabilitation strategy used in this study has some similarity to the strategy presented in a recent case report, which consisted of visual biofeedback from a computer screen to improve WB symmetry during functional activity and lower extremity quadriceps strengthening exercises.13 The patient demonstrated improved knee motion and maximum knee extension moments after symmetry training, with final values similar to healthy age-matched comparison values. The findings from this case report are consistent with our findings that biofeedback training to promote surgical limb loading early after TKA may improve the knee extensor function during walking.
The finding of greater surgical knee extension moments for the RELOAD group compared to the CONTROL group at the 26-week test support further examination of WB training to improve movement patterns and functional performance after unilateral TKA. It is important to identify if long-term improvements in movement patterns can result from such training, and if declines in rates of contralateral knee and hip problems are possible. It has been shown that surgical limb unloading results in movement pattern asymmetries during tasks such as walking, stair climbing, and sit-stand transitions.4, 8, 26 It is also known that patients with unilateral TKA have a greater than 2-fold increase in likelihood of having a joint replacement for their contralateral hip or knee.1, 25
The persistence of movement patterns to unload the knee joint may be a result of a habitual movement pattern acquired prior to TKA, which does not resolve without intentional WB training.3, 7 People with medial tibiofemoral compartment OA tend to walk with less contribution of knee extension moment to maximum total limb support moments than healthy individuals at similar walking speeds,33 a movement pattern that persists after unilateral TKA.19, 30 The mechanism underlying the persistence of decreased knee extension moments after TKA is not completely understood, and should be the subject of future investigations.
Study Limitations
A small sample size and lack of long-term follow up limits the strength of conclusions. Larger trials should further examine efficacy of WB biofeedback training programs following unilateral TKA. A longer intervention time could be used to assess if increasing the intervention dose produces adaptations in knee extension strength, knee motion, and movement performance. The method of biofeedback can be further studied as well. While the use of constant visual feedback in this study is consistent with other interventions for patients with joint arthroplasty,14, 27, 32 optimal biofeedback schedules and modes have not been identified. Future work should compare various WB biofeedback schedules (eg, constant, random, summary) and modes (eg, auditory, tactile, verbal). In addition, the stationary balance board used to provide WB biofeedback limited the ability to perform highly dynamic training activities, such as gait, which may have limited the effectiveness of the training.
CONCLUSION
This study indicates that the addition of a 6 week intervention of WB biofeedback training to standard rehabilitation post TKA did not improve functional WB symmetry. However, WB biofeedback training successfully increased knee extension moments during walking, early after TKA. The long-term functional consequences of such changes in movement quality should be further studied in a larger sample.
KEY POINTS.
Findings
WB biofeedback training did not improve functional WB symmetry. Between-group differences in joint moments indicate that quality of functional movement changed with the training.
Implications
New approaches to improving movement asymmetries after TKA are needed. In addition, it is important to determine if changes in movement pattern quality result in long-term changes in function and/or joint health.
Caution
A small sample size and lack of long-term follow up limits the strength of conclusions. The results can be used to power sample size calculations of future trials to better examine efficacy of WB biofeedback training programs following unilateral TKA.
Acknowledgments
This work was funded in part through the Foundation for Physical Therapy (Marquette Challenge Research Grant and Promotion of Doctoral Studies Scholarship II) and the National Institutes of Health grants K23-AG029978, R01-HD065900, T32 AG00279
Footnotes
The Colorado Multiple Institution Review Board approved the protocol for this study.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
Public Trials Registry: NCT01333189
References
- 1.Barthuly AM, Bohannon RW, Gorack W. Gait speed is a responsive measure of physical performance for patients undergoing short-term rehabilitation. Gait Posture. 2012;36:61–64. doi: 10.1016/j.gaitpost.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Bohannon RW, Glenney SS. Minimal clinically important difference for change in comfortable gait speed of adults with pathology: a systematic review. Journal of evaluation in clinical practice. 2014;20:295–300. doi: 10.1111/jep.12158. [DOI] [PubMed] [Google Scholar]
- 3.Boonstra MC, De Waal Malefijt MC, Verdonschot N. How to quantify knee function after total knee arthroplasty? Knee. 2008;15:390–395. doi: 10.1016/j.knee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Boonstra MC, Schwering PJ, De Waal Malefijt MC, Verdonschot N. Sit-to-stand movement as a performance-based measure for patients with total knee arthroplasty. Phys Ther. 2010;90:149–156. doi: 10.2522/ptj.20090119. [DOI] [PubMed] [Google Scholar]
- 5.Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2014;22:1833–1839. doi: 10.1016/j.joca.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christiansen CL, Bade MJ, Judd DL, Stevens-Lapsley JE. Weight-bearing asymmetry during sit-stand transitions related to impairment and functional mobility after total knee arthroplasty. Arch Phys Med Rehabil. 2011;92:1624–1629. doi: 10.1016/j.apmr.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christiansen CL, Bade MJ, Weitzenkamp DA, Stevens-Lapsley JE. Factors predicting weight-bearing asymmetry 1month after unilateral total knee arthroplasty: A cross-sectional study. Gait Posture. 2013;37:363–367. doi: 10.1016/j.gaitpost.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christiansen CL, Stevens-Lapsley JE. Weight-bearing asymmetry in relation to measures of impairment and functional mobility for people with knee osteoarthritis. Arch Phys Med Rehabil. 2010;91:1524–1528. doi: 10.1016/j.apmr.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen J. Statistical power analysis fo the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 10.Dunlop WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psych Methods. 1996:170–177. [Google Scholar]
- 11.Goldberg A, Chavis M, Watkins J, Wilson T. The five-times-sit-to-stand test: validity, reliability and detectable change in older females. Aging clinical and experimental research. 2012;24:339–344. doi: 10.1007/BF03325265. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg A, Schepens S. Measurement error and minimum detectable change in 4-meter gait speed in older adults. Aging clinical and experimental research. 2011;23:406–412. doi: 10.1007/BF03325236. [DOI] [PubMed] [Google Scholar]
- 13.Hatfield GL, Hubley-Kozey CL, Astephen Wilson JL, Dunbar MJ. The effect of total knee arthroplasty on knee joint kinematics and kinetics during gait. J Arthroplasty. 2011;26:309–318. doi: 10.1016/j.arth.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 14.Isakov E. Gait rehabilitation: a new biofeedback device for monitoring and enhancing weight-bearing over the affected lower limb. Eura Medicophys. 2007;43:21–26. [PubMed] [Google Scholar]
- 15.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 16.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 17.Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci. 2002;57:M539–543. doi: 10.1093/gerona/57.8.m539. [DOI] [PubMed] [Google Scholar]
- 18.Manal K, Gardinier E, Buchanan TS, Snyder-Mackler L. A More Informed Evaluation of Medial Compartment Loading: the Combined Use of the Knee Adduction and Flexor Moments. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2015 doi: 10.1016/j.joca.2015.02.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandeville D, Osternig LR, Lantz BA, Mohler CG, Chou LS. The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clin Biomech (Bristol, Avon) 2008;23:1053–1058. doi: 10.1016/j.clinbiomech.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 20.McClelland J, Zeni J, Haley RM, Snyder-Mackler L. Functional and biomechanical outcomes after using biofeedback for retraining symmetrical movement patterns after total knee arthroplasty: a case report. The Journal of orthopaedic and sports physical therapy. 2012;42:135–144. doi: 10.2519/jospt.2012.3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meretta BM, Whitney SL, Marchetti GF, Sparto PJ, Muirhead RJ. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. Journal of vestibular research : equilibrium & orientation. 2006;16:233–243. [PubMed] [Google Scholar]
- 22.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–1090. doi: 10.1016/j.orthres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Motyl JM, Driban JB, McAdams E, Price LL, McAlindon TE. Test-retest reliability and sensitivity of the 20-meter walk test among patients with knee osteoarthritis. BMC Musculoskelet Disord. 2013;14:166. doi: 10.1186/1471-2474-14-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ouellet D, Moffet H. Locomotor deficits before and two months after knee arthroplasty. Arthritis Rheum. 2002;47:484–493. doi: 10.1002/art.10652. [DOI] [PubMed] [Google Scholar]
- 25.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185–3189. doi: 10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 26.Stacoff A, Kramers-de Quervain IA, Luder G, List R, Stussi E. Ground reaction forces on stairs. Part II: knee implant patients versus normals. Gait Posture. 2007;26:48–58. doi: 10.1016/j.gaitpost.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 27.White SC, Lifeso RM. Altering asymmetric limb loading after hip arthroplasty using real-time dynamic feedback when walking. Arch Phys Med Rehabil. 2005;86:1958–1963. doi: 10.1016/j.apmr.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther. 2005;85:1034–1045. [PubMed] [Google Scholar]
- 29.Winter DA. Overall principle of lower limb support during stance phase of gait. Journal of biomechanics. 1980;13:923–927. doi: 10.1016/0021-9290(80)90162-1. [DOI] [PubMed] [Google Scholar]
- 30.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23:320–328. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshida Y, Zeni J, Snyder-Mackler L. Do patients achieve normal gait patterns 3 years after total knee arthroplasty? J Orthop Sports Phys Ther. 2012;42:1039–1049. doi: 10.2519/jospt.2012.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeni J, Jr, Abujaber S, Flowers P, Pozzi F, Snyder-Mackler L. Biofeedback to promote movement symmetry after total knee arthroplasty: a feasibility study. The Journal of orthopaedic and sports physical therapy. 2013;43:715–726. doi: 10.2519/jospt.2013.4657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeni JA, Higginson JS. Knee osteoarthritis affects the distribution of joint moments during gait. Knee. 2011;18:156–159. doi: 10.1016/j.knee.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]