Abstract
Background
High intake of sugar-sweetened beverages (SSB) has been suggested to contribute to the pediatric obesity epidemic, however, how the home food environment influence children’s intake of SSB among Hispanic families is still poorly understood.
Objectives
To evaluate the relationships between the home food environment and Hispanic children’s diet in relation to weight status and insulin resistance (IR).
Methods
A food frequency questionnaire was administered to 187 Hispanic children (ages 10 to 14 years), and anthropometrics were measured. IR was estimated from fasting insulin and glucose levels using the homeostasis model assessment of insulin resistance (HOMAIR). Parents reported on family demographics and the home food environment. A structural equation modeling approach was applied to examine the hypothesized relationships among variables.
Results
The prevalence of childhood overweight and obesity was 52.8% and it was positively associated with HOMAIR (β=0.687, P <.0001). Children’s SSB consumption was positively associated with children’s BMI z-score (β=0.151, P <0.05) and subsequently to HOMAIR. Children’s SSB consumption was predicted by home availability (β=0.191) and parental intake of SSB (β=0.419) (P <0.05). The model fit indices [X2 = 45.821 (d.f. = 30, P > 0.01 and < 0.05), X2/d.f. = 1.53, RMSEA = 0.053 (90% C.I. = 0.016, 0.082), CFI = 0.904] suggested a satisfactory goodness-of-fit.
Conclusions
The home food environment and parental diet seem to play an important role in the children’s access to and intake of SSB, which in turn predicted children’s weight status.
Keywords: Family eating habits, home environment, insulin resistance, obesity
Introduction
Excess weight has been documented in children and in adults, and substantially increases the risk of cardiovascular disease, dyslipidemia, and Type 2 Diabetes (T2D) [1]. In the United States (US), the burden of obesity falls disproportionately on children from minority groups where the prevalence of obesity among non-Hispanic White children was 16.1% while that for Hispanics children was greater than 23% [2]. Further, obesity greatly increases the risk for insulin resistance (IR), a major risk factor for developing T2D, which is also markedly higher among Hispanic children when compared to their non-Hispanic White counterparts [3].
Food environments that promote diets high in energy-dense, nutrient-poor foods and beverages, usually lead to a positive energy imbalance and excess weight gain [4]. Among these, sugar-sweetened beverages (SSB) have been a particular concern since SSB consumption among youth has almost doubled in the past decades [5]. Because of the temporal relationship between these changes and a high degree of association, it has been suggested that high intakes SSB can or have contributed to the pediatric obesity epidemic [6].
Current research has focused on children’s weight status at the individual level, but there has been an increasing interest in the home food environment and how it can influence the modifiable risk factors of childhood obesity. Some examples include findings that parental support for healthy eating and greater availability of healthy foods at home contribute to children’s diet [7]. Similarly, it was also reported that the availability of soft drinks at home is positively associated with children’s intake of these beverages. Furthermore, evidence from focus groups among Hispanic families regarding SSB consumption suggest that the availability of these beverages at home is one of the key factors contributing to high intakes of SSB [8]. However, there are no studies to our knowledge further evaluating whether the availability of energy-dense, nutrient-poor beverages at home relates to Hispanic children’s diet. Therefore, this study aimed to evaluate the associations between familial and individual dietary behaviors in relation to Hispanic children’s weight and IR using the structural equation modeling (SEM).
Relationships among familial, parental and children’s diet and biometric (physiological, metabolic) indicators have been largely examined by a substantial number of studies using multivariate regression analyses [4, 5, 7]. This approach is useful for providing insights into direct associations between independent variables and dependent variable. However, the SEM is a powerful technique for multivariate analysis that permits simultaneous estimation of multiple regression equations of hypothesized associations [9]. In an SEM, the same variable can be the dependent variable in one regression equation and the independent variable in other regression equations. This study context certainly involves multiple relationships among variables since it hypothesizes that parental intake of SSB affects children’s intake of SSB, which influences children’s IR through increased weight gain. The SEM has its origin in the field of biometric [10] and it became more popular in psychology and social sciences [11] given its advantages in flexibility to estimate dichotomous, ordered and categorical data under non-normal conditions [12]. Using the SEM approach, the present study set out to provide deeper insights into the directional associations among children’s IR and an array of individual, parental and familial correlates, as well as to explore significant indirect associations.
Materials and Methods
Study population
This study is part of a multi-disciplinary research project between investigators at the University of Wisconsin-Madison and the United Community Center (UCC) – Bruce Guadalupe Charter School (BGCS) in Milwaukee, WI. Our study focused on a single school serving an inner-city Hispanic population experiencing significant health disparities, including high rates of childhood obesity and increased risk for T2D. The target population was children attending BGCS and their parents. Inclusion criteria were academic attendance at the BGCS in grades fifth through eighth (n=300) and Hispanic ethnicity. Recruitment included sending descriptive study materials to their homes, and providing oral and written information during school family events. The University of Wisconsin Institutional Review Board approved the study.
Weight status and insulin resistance assessments
Children’s weight was measured using a beam balance scale and height was measured using a stadiometer at school without shoes and in light clothing. Centers for Disease Control and Prevention growth charts were used for the definition of childhood overweight and obesity [13]. BMI z-score was also examined as a continuous outcome variable. IR was assessed using a single blood test of fasting glucose and insulin levels, using the derived homeostasis model assessment of IR (HOMAIR). This validated equation [(glucose*0.055)*insulin/22.5] provides a reliable assessment of IR in youth and is highly correlated with the gold standard of euglycemic clamp studies [14]. Although tanner age may be associated with IR, the validation study by Gungor N. et al. [14] demonstrated that HOMAIR was not different between adolescents versus pre-pubertal children.
Dietary intake assessment
Dietary intake was assessed using the food frequency questionnaire (FFQ) Block for Kid’s Questionnaire with Hispanic foods [15]. Study personnel administered the questionnaire. Individual portion size was asked, and pictures were provided to enhance accuracy of quantification. The original questionnaire was validated in numerous studies and in a variety of populations, including a validation study among a multi-ethnic population of children (57% Hispanic) in which the FFQ was compared to two 24-hour recalls. All reliability intra-class correlations were >0.30, except for energy coming from protein [16]. The survey was pre-tested in a small sample of study participants (n=10) to ensure content coverage and comprehension.
Home food environment and family demographics assessments
A literature review was conducted to assess available validated measures to evaluate the home environment in relation to children’s diet, where items were taken from the most widely used instruments and questions were adapted from validated home environment surveys [7, 17, 18]. The survey development took several iterations and was guided by the social ecological theory. Gattshall et al. [17] previously validated a home environment survey to evaluate home food availability, including the availability of SSB at home and test-rest reliability was reported at r ≥ 0.75 for all single measures. Pilot testing of the survey was conducted with parents (n=10) for applicability and comprehension. Family demographics were assessed through a self-administered demographic questionnaire for the parents. All questionnaires were available in English and Spanish.
Statistical analysis
A total of 188 children were enrolled in the present study. One non-Hispanic white child (n=1) was removed from subsequent analysis, and subjects (n=8) with implausible reported energy intakes (<500 kcal or >3,500 kcal) were removed from further analysis. New variables were created for availability of SSB at home and parental intake of SSB by combining responses on soda and fruit drink. Regression models adjusted for children’s age and gender were used to evaluate the relationships between children’s diet and BMI z-score (SAS software version 9.3, SAS Institute Inc., Cary, NC). In addition to examining pair-wise correlation relationships among variables (Tables S1), the SEM approach was employed to determine the directional associations among variables (MPlus software, Muthén & Muthén, v6.1 Los Angeles, CA).
As the sample size was limited (n=187), the full maximum likelihood estimator (MLE) was used in model estimation so that subjects with partially missing data could be retained in the sample. To meet the multivariate normality assumption of MLE, multiple variables (parental SSB consumption, parental milk consumption, number of years in the US, family income, parental BMIs, and children’s HOMAIR) that departed from normality were log-transformed. Relationships were measured with regression coefficients (β) and their statistical significance level was set at P ≤ 0.05. Squared multiple correlations (R^(2)) were computed to assess the variation in endogenous variables as explained by the model. The model goodness-of-fit was measured by chi-square (χ2), relative chi-square (χ2/d.f.), root mean square error of approximation (RMSEA), and comparative fit index (CFI).
Results
The prevalence of childhood overweight and obesity were 24.7% and 28.1%, respectively (Table 1). Mean fasting blood levels of glucose and insulin were used to calculate HOMAIR (mean, 4.0 ± 2.5). Children’s reported intake of total sugar was high (31.4 ± 8.5, % total energy), and accounted for a large percentage (>50%) of the reported total carbohydrate daily intake (58.5 ± 7.5%). Children’s intake of added sugars and SSB were positively associated with children’s BMI z-score (β =0.19 and β =0.27, P <0.05) (Table S2).
Table 1.
Children Characteristics (N = 187)
|
n (%) or Mean ± standard deviation |
|
|---|---|
| Gender (male) | 88 (47%) |
| Age (years) | 11.9 ± 1.4 |
| BMI z-score | 0.9 ± 0.9 |
| BMI percentile categories* | |
| Healthy weight: ≥ 5 to 85th percentile | 84 (47%) |
| Overweight: ≥ 85 to < 95th percentile | 44 (25%) |
| Obese: ≥ 95th percentile | 50 (28%) |
| HOMAIR | 4.0 ± 2.5 |
| Glucose (mg/dl) | 89.3 ± 7.2 |
| Insulin (uIU/ml) | 17.9 ± 10.5 |
| Children’s reported dietary intake (n= 174) | |
| Macronutrients | |
| Total carbohydrates (% energy) | 58.5 ± 7.0 |
| Total sugar (% energy) | 31.4 ± 8.5 |
| Protein (% energy) | 13.6 ± 2.4 |
| Total fat (% energy) | 29.9 ± 4.9 |
| Saturated fat (% energy) | 11.1 ± 2.2 |
| Foods | |
| Fruits (cups per 1,000 kcal) | 1.2 ± 0.7 |
| Vegetables (cups per 1,000 kcal) | 0.7 ± 0.4 |
| Milk (cups per 1,000 kcal) | 1.0 ± 0.8 |
| Added sugars (teaspoons per 1,000 kcal) | 8.5 ± 3.9 |
| Sugar-sweetened beverages (kilocalories per 1,000 kcal) | 72.3 ± 67.5 |
BMI percentile categories for age and sex.
SD, standard deviation; HOMAIR, derived homeostasis model assessment of insulin resistance.
Table 2 summarizes familial characteristics. Ninety percent of fathers and 67% of mothers were overweight or obese. Families were mostly of Mexican descent (77%), while 22% of the families were of Puerto Rican descent. Families have lived in the US for 20 ± 10 years (y). As for language preferences, 45% of the parents preferred Spanish, 19% preferred English, and 43% preferred English and Spanish, while most children preferred both Spanish and English (72%). Proxy measures of acculturation, including the number of years in the US and language preferences were not associated with children’s BMI z-score or HOMAIR (Supplementary Table 3). Further, the odds ratio (95% CI) for childhood overweight and obesity were calculated for >16 y versus ≤16 y in the US. For children whose families have lived in the US for >16 years there was not a significant association with higher odds of being overweight or obese: OR=0.81 (0.45, 1.47) (Data not shown). However, the number of years in the US was positively associated with children’s SSB consumption. More than half of the families reported having soda (56%) or fruit drinks (54%) available at home, while 42% and 38% of the parents reported frequent intake of soda and fruit drinks, respectively. Most families reported having milk available at home (83%) and 91% of parents consumed milk at least twice per week. Eighty-nine percent of the families reported frequently having a meal together as a family, although only 15% reported eating out.
Table 2.
Familial Characteristics (N = 173)
|
N (%) or Mean ± standard deviation |
|
|---|---|
| Paternal BMI (kg/m2) | 29.0 ± 4.9 |
| Normal weight: BMI ≥ 18.5 to 24.9 | 9 (10%) |
| Overweight: BMI ≥ 25.0 to 29.9 | 55 (61%) |
| Obese: BMI ≥ 30.0 | 26 (29%) |
| Maternal BMI (kg/m2) | 28.0 ± 5.5 |
| Normal weight: BMI ≥ 18.5 to 24.9 | 39 (33%) |
| Overweight: BMI ≥ 25.0 to 29.9 | 42 (35%) |
| Obese: BMI ≥ 30.0 | 39 (32%) |
| Hispanic Ethnicity | |
| Mexican American | 144 (77%) |
| Puerto Rican | 43 (23%) |
| Acculturation Status | |
| Number of years living in the US | 20.2 ± 10.1 |
| Language preference by parents | |
| Spanish | 73 (45%) |
| English | 19 (12%) |
| Spanish and English | 72 (43%) |
| Language preference by children | |
| Spanish | 11 (7%) |
| English | 34 (21%) |
| Spanish and English | 117 (72%) |
| Family income ($/year) | |
| $0 to <23,000 | 56 (38%) |
| $23 to <35,000 | 41 (28%) |
| $35 to <50,000 | 27 (18%) |
| ≥ $50,000 | 23 (16%) |
| Typical home food availability (yes) | |
| Soda | 81 (56%) |
| Fruit drinks | 83 (54%) |
| Milk | 128 (83%) |
| Parental reported intake of beverages | |
| Soda (≥ 2 times per week) | 65 (42%) |
| Fruit drinks (≥ 2 times per week) | 60 (38%) |
| Milk (≥ 2 times per week) | 140 (91%) |
| Family dietary habits | |
| Family meals (≥ 2 times per week) | 138 (89%) |
| Eating out or having takeout food (≥ 2 times per week) | 24 (15%) |
SD, standard deviation
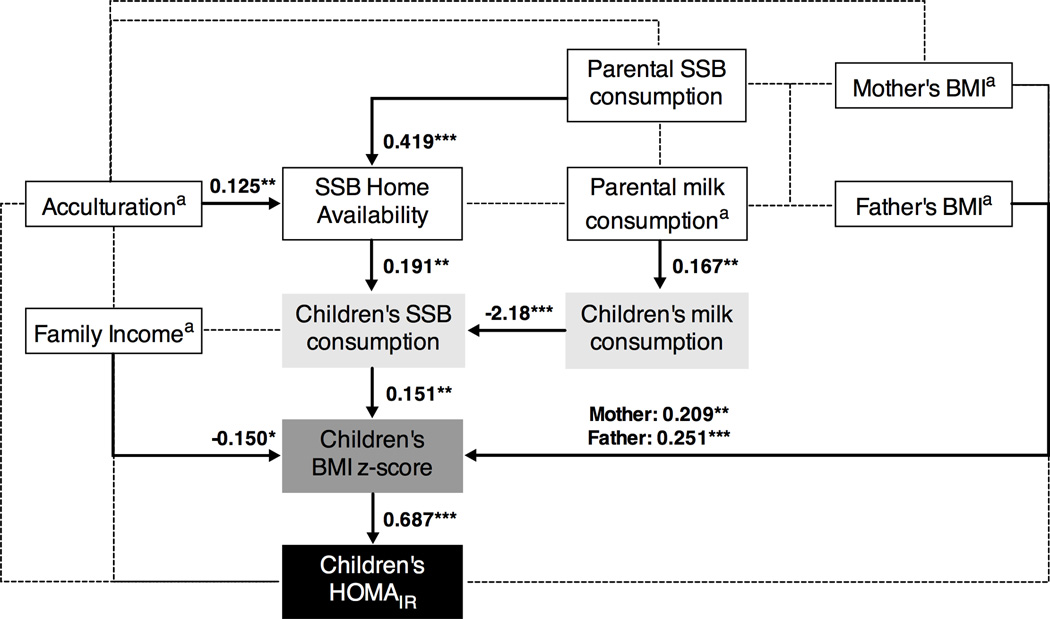
The SEM development in this study began with our research hypothesis that the home environment contribute to children’s diet, which in turn is associated with children’s weight status and IR. The model development went through several iterations estimating all variables available. The final model was obtained by including variables that contributed to the model goodness-of-fit and fit into our research hypothesis. The study final SEM describes the interactions between familial and individual dietary habits; and their correlates with children's weight status and HOMAIR. The goodness-of-fit indices were: X2 = 45.821 (d.f. = 30, P > 0.01 and < 0.05), X2/d.f. = 1.53, RMSEA = 0.053 (90% C.I. = 0.016, 0.082), and CFI = 0.904, indicating a satisfactory model fit to data. The model estimation results are reported in Figure 1 and Table 3. The path diagram in Figure 1 shows all significant standardized regression coefficients (β) along the pathways, and the relationships that were included in the final exploratory analysis, but were not significant (dashed lines).
Figure 1. Structural Equation Model with Estimated Parameters for 187 Hispanic Children.
Familial and individual correlates of Hispanic children’s SSB consumption, BMI z-score, and HOMAIR. Statistically significant path coefficients are presented as: standardized regression coefficients (β); dashed lines represent relationships that were included in the final exploratory analysis, but were not significant. Model fit: X2 = 45.821 (d.f. = 30, P > 0.01 and < 0.05), X2/d.f. = 1.53, RMSEA = 0.053 (90% C.I. = 0.016, 0.082), and CFI = 0.904.
aThese variables were log-transformed to improve multivariate normality.
***P value <0.01; **P value <0.05, *P value ≤ 0.05.
Table 3.
Standardized Structural Equation Model Results of Individual and Familial Predictors of Children’s HOMAIR
| To | ||||||
|---|---|---|---|---|---|---|
| From | Direct association | Indirect association | ||||
| SSB home availability |
Children’s milk consumption |
Children’s SSB consumption |
Children’s BMI z-score |
Children’s HOMAIRa |
Children’s HOMAIRa | |
| Parental SSB consumption | 0.419*** (7.575) |
- | - | - | - | 0.010 (1.552) |
| Acculturationa | 0.125** (2.286) |
- | - | - | - | 0.003 (1.296) |
| Parental milk consumptiona | - | 0.167** (2.032) |
- | - | - | −0.004 (−1.304) |
| SSB home availability | - | - | 0.191** (2.526) |
- | - | 0.020 (1.585) |
| Children’s milk consumption | - | - | −0.218*** (−3.061) |
- | - | −0.023* (−1.717) |
| Family incomea | - | - | - | −0.150* (−1.916) |
- | −0.103* (−1.891) |
| Mother’s BMIa | - | - | - | 0.209** (2.376) |
- | 0.144** (2.333) |
| Father’s BMIa | - | - | - | 0.251*** (2.801) |
- | 0.172*** (2.720) |
| Children’s SSB consumption | - | - | - | 0.151** (2.136) |
- | 0.104** (2.101) |
| Children’s BMI z-score | - | - | - | - | 0.687*** (13.796) |
- |
These variables were log-transformed to improve multivariate normality. Values in parenthesis correspond to t-statistic.
P < 0.01,
P < 0.05,
P ≤ 0.05.
Parental SSB consumption (β = 0.419) and the number of years in the US (β = 0.125) were positively associated with SSB home availability. Children’s SSB consumption was predicted by SSB home availability (β = 0.191), and negatively associated to children’s milk consumption (β = −0.218), which in turn was predicted by parental milk intake (β = 0.167). Among the several exogenous variables that exhibited significant associations with children’s BMI z-score, higher BMI in parents (father: β = 0.251; mother: β = 0.209), lower family income (β = −0.150), and higher children’s SSB consumption (β = 0.151) were all positively associated with children’s BMI z-score. Finally, children’s BMI z-score was positively and strongly associated with children’s HOMAIR (β = 0.687).
Table 3 illustrates the direct associations and indirect associations. The relationships between the familial and individual dietary habits and children’s HOMAIR were not direct, but instead were indirect through children’s BMI z-score. Parental weight status and family income were indirectly related to children’s HOMAIR through children’s BMI z-score. Children’s SSB and milk consumption were also indirectly associated with children’s HOMAIR through children’s BMI z-score. Overall, this model accounted for 47% of the variance of children’s HOMAIR, 19% of the variance of children’s BMI z-score, 28% of the variance of SSB home availability, and 8% and 3% of the variance of children’s SSB and milk consumption, respectively.
Discussion
Familial and individual dietary behaviors were significantly associated with children’s HOMAIR through children’s weight status. Reported SSB consumption, parental BMI, and family income were all associated with children’s BMI z-score, and with HOMAIR through children’s weight status. These findings add to the evidence that Hispanic children’s consumption of SSB is associated with obesity and HOMAIR [19–21].
In contrast, another study reported no association between SSB consumption and BMI in adolescents even though 65% reported consumption of SSB at least once per day [22]. Specifically with respect to Hispanic children, the present study is consistent with a study that included 42% Hispanic/Latino children in that daily SSB consumption was positively associated with children’s weight status [23]. Further, in a randomized trial aimed at reducing the consumption of SSB in in a multiethnic population of adolescents, there was a significant reduction in body weight after two years of intervention in the Hispanic subgroup. These findings suggest a genetic predisposition in the metabolic profile of Hispanic children that lead to a sustained weight loss [24]. Taken together, these data imply that SSB consumption contribute to positive energy balance, while reducing SSB consumption could have beneficial effects on body weight.
Possible mechanisms for SSB consumption on increased body weight and risk for T2D have been previously suggested [25, 26]. Liquid calories coming from SSB have been reported to have a less satiating effect than whole foods or beverages of higher nutritional value, such as milk, therefore increasing energy intake. In the present study, children’s milk consumption was inversely associated with SSB consumption (β = −0.218; P <0.01), suggesting a substitution of milk for SSB in their diets, which has been suggested by others [27]. Furthermore, diets high in simple sugars, such as fructose, induce weight gain through central effects that decrease satiety while stimulating hepatic de novo lipogenesis, leading to dyslipidemia and IR. Another possibility is that SSB consumption may be a marker for an unhealthy lifestyle. Children with high SSB consumption tend to be more sedentary and eat more frequently at fast food restaurants [20, 28].
In agreement with previous reports, several predictors of children’s SSB consumption were found, including home availability and parental intake of SSB [29]. Further, the inverse association between children intakes of SSB and milk was mediated by parental intake of milk, further suggesting parental influence given their role-modeling capabilities. The number of years in the US was directly associated with SSB home availability and indirectly associated to children SSB consumption, suggesting that more acculturated families were adopting US dietary habits, which are consistent with reports by others [30]. However, the number of years in the US or language preference, were not associated with children’s BMI z-score or HOMAIR.
Given the cross-sectional nature of the present study, future research is needed to confirm the results presented here. SEM results are limited to associations, and directionality cannot be proven. This shortcoming can be addressed by conducting longitudinal studies that measure the variables across two or more times to confirm the relationships modeled. Findings are probably only generalizable to Hispanic families, and are confined to self-reported measures of diet and home food environment that need to be further validated. Although HOMAIR has been validated in youth, the findings presented here should be interpreted with cautious given that the results didn’t include tanner stage. Finally, our study is one of few consulting within race/ethnic analyses among Hispanic families (77% of Mexican descent), which are critical in understanding the underlying mechanisms by which the home environment can contribute to Hispanic children’s diet-related risk for obesity and IR.
In conclusion, parental diet and the home food environment seem to play an important role in children’s access to and intake of SSB, which in turn increases their risk for obesity and T2D. SSB consumption provides little nutritional benefit and it may lead to increased energy intake with subsequent weight gain. Interventions aimed at reducing consumption of SBB as part of a healthy diet seem warranted where families are educated on the benefits of having a healthier home food environment.
Supplementary Material
Values correspond to correlation coefficient, P value, and number of observations for each association (N value).
**Correlation coefficient is significant at P value <0.01 (2-tailed).
*Correlation coefficient is significant at P value <0.05 (2-tailed).
aValues are beta coefficients (β) and 95% confident intervals (CI) for children’s BMI z-score for one unit increase in predictor variables; added sugars per 5 units, and SSB per 100 units, respectively.
bLinear regression models were adjusted for children’s age and gender. Cook’s distance test was used to determine influencing observations on linear associations.
SSB, sugar-sweetened beverages.
Values correspond to correlation coefficient, P value, and number of observations for each association (N value).
**Correlation coefficient is significant at P value <0.01 (2-tailed).
*Correlation coefficient is significant at P value <0.05 (2-tailed).
Acknowledgements
Funding for this project was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program (233-PRJ49PH), along with support from the UW Institute for Clinical and Translational Research, an NIH-funded Clinical and Translational Science Award (grant# UL1 TR000427).
The community-engaged research project, Healthy Activities Partnership Program for Youth (HAPPY), is a partnership among staff from the Community Research Office and Bruce Guadalupe Community School at the United Community Center in Milwaukee, and researchers from the University of Wisconsin-Madison, who are members of the Wisconsin Prevention for Obesity and Diabetes (WiPOD) network. Also contributing to the success of HAPPY is funding from the UW Collaborative Center for Health Equity, an NIH/NIMHD-funded Center of Excellence in Minority Health and Health Disparities (grant# 5 P60 MD 003428).
This manuscript represents original work that has not been published previously and is currently not considered by another journal. The authors confirm that the manuscript will not be published elsewhere in the same form, in English or any other language. Each author has seen and approved the contents of the submitted manuscript. All authors conceived the study and participated in its design and coordination, contributed to conception and design, acquisition of data, analysis or interpretation of data and revised the article critically for important intellectual content. In detail: M Santiago-Torres and DA Schoeller drafted the manuscript.
Abbreviations
- SSB
sugar-sweetened beverages
- IR
insulin resistance
- HOMAIR
homeostasis model assessment for insulin resistance
- BMI
body mass index
- T2D
Type 2 diabetes
- SEM
structural equation modeling
Footnotes
Conflicts of interest statement
All the authors declare that there are not any conflicts of interest.
References
- 1.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Jama. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta, GA: Department of Health and Human Services, Center for Disease Control and Prevention; 2011. [Google Scholar]
- 4.Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. International Journal of Obesity. 2006;30:1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- 5.French SA, Lin BH, Guthrie JF. National trends in soft drink consumption among children and adolescents age 6 to 17 years: Prevalence, amounts, and sources, 1977/1978 to 1994/1888. Journal of the American Dietetic Association. 2003;103:1326–1331. doi: 10.1016/s0002-8223(03)01076-9. [DOI] [PubMed] [Google Scholar]
- 6.Morgan RE. Does consumption of high-fructose corn syrup beverages cause obesity in children? Pediatric Obesity. 2013;8:249–254. doi: 10.1111/j.2047-6310.2013.00173.x. [DOI] [PubMed] [Google Scholar]
- 7.Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutrition. 2005;8:77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- 8.Bogart LM, Cowgill BO, Sharma AJ, Uyeda K, Sticklor LA, Alijewicz KE, Schuster MA. Parental and Home Environmental Facilitators of Sugar-Sweetened Beverage Consumption Among Overweight and Obese Latino Youth. Academic Pediatrics. 2013;13:348–355. doi: 10.1016/j.acap.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.kline RB. Principles and practice of structural equation modeling. Guilford press; 2010. [Google Scholar]
- 10.Wright S. Correlation and causation. Journal of Agricultural Research. 1921;20.7:557–585. [Google Scholar]
- 11.MacCallum RC, Austin JT. Applications of structural equation modeling in psychological research. Annu Rev Psychol. 2000;51:201–226. doi: 10.1146/annurev.psych.51.1.201. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan D. Structural equation modeling: Foundations and extensions. Sage Publications, Incorporated; 2008. [Google Scholar]
- 13.Kuczmarski RJ, Ogden CL, Guo SS. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat: National Center for Health Statistics. 2002 [PubMed] [Google Scholar]
- 14.Gungor N, Saad R, Janosky J, Arslanian S. Validation of surrogate estimates of insulin sensitivity and insulin secretion in children and adolescents. Journal of Pediatrics. 2004;144:47–55. doi: 10.1016/j.jpeds.2003.09.045. [DOI] [PubMed] [Google Scholar]
- 15.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 16.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. Journal of the American Dietetic Association. 2008;108:862–866. doi: 10.1016/j.jada.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 17.Gattshall ML, Shoup JA, Marshall JA, Crane LA, Estabrooks PA. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act. 2008;5:3. doi: 10.1186/1479-5868-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bauer KW, Neumark-Sztainer D, Fulkerson JA, Hannan PJ, Story M. Familial correlates of adolescent girls' physical activity, television use, dietary intake, weight, and body composition. International Journal of Behavioral Nutrition and Physical Activity. 2011;8 doi: 10.1186/1479-5868-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang JW, Mark S, Henderson M, O'Loughlin J, Tremblay A, Wortman J, Paradis G, Gray-Donald K. Adiposity and glucose intolerance exacerbate components of metabolic syndrome in children consuming sugar-sweetened beverages: QUALITY cohort study. Pediatric Obesity. 2013;8:284–293. doi: 10.1111/j.2047-6310.2012.00108.x. [DOI] [PubMed] [Google Scholar]
- 20.Bremer AA, Auinger P, Byrd RS. Relationship between insulin resistance-associated metabolic parameters and anthropometric measurements with sugar-sweetened beverage intake and physical activity levels in US adolescents: findings from the 1999–2004 National Health and Nutrition Examination Survey. Arch Pediatr Adolesc Med. 2009;163:328–335. doi: 10.1001/archpediatrics.2009.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kondaki K, Grammatikaki E, Jimenez-Pavon D, De Henauw S, Gonzalez-Gross M, Sjostrom M, Gottrand F, Molnar D, Moreno LA, Kafatos A, et al. Daily sugar-sweetened beverage consumption and insulin resistance in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr. 2013;16:479–486. doi: 10.1017/S1368980012002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park S, Blanck HM, Sherry B, Brener N, O'Toole T. Factors associated with sugar-sweetened beverage intake among United States high school students. J Nutr. 2012;142:306–312. doi: 10.3945/jn.111.148536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giammattei J, Blix G, Marshak HH, Wollitzer AO, Pettitt DJ. Television watching and soft drink consumption: associations with obesity in 11- to 13-year-old schoolchildren. Arch Pediatr Adolesc Med. 2003;157:882–886. doi: 10.1001/archpedi.157.9.882. [DOI] [PubMed] [Google Scholar]
- 24.Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A Randomized Trial of Sugar-Sweetened Beverages and Adolescent Body Weight. New England Journal of Medicine. 2012;367:1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bray GA, Popkin BM. Calorie-sweetened beverages and fructose: what have we learned 10 years later. Pediatric Obesity. 2013;8:242–248. doi: 10.1111/j.2047-6310.2013.00171.x. [DOI] [PubMed] [Google Scholar]
- 26.Dekker MJ, Su QZ, Baker C, Rutledge AC, Adeli K. Fructose: a highly lipogenic nutrient implicated in insulin resistance, hepatic steatosis, and the metabolic syndrome. American Journal of Physiology-Endocrinology and Metabolism. 2010;299:E685–E694. doi: 10.1152/ajpendo.00283.2010. [DOI] [PubMed] [Google Scholar]
- 27.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Maternal milk consumption predicts the tradeoff between milk and soft drinks in young girls' diets. Journal of Nutrition. 2001;131:246–250. doi: 10.1093/jn/131.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frary CD, Johnson RK, Wang MQ. Children and adolescents' choices of foods and beverages high in added sugars are associated with intakes of key nutrients and food groups. J Adolesc Health. 2004;34:56–63. doi: 10.1016/s1054-139x(03)00248-9. [DOI] [PubMed] [Google Scholar]
- 29.Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. J Am Diet Assoc. 2004;104:1244–1249. doi: 10.1016/j.jada.2004.05.206. [DOI] [PubMed] [Google Scholar]
- 30.Allen ML, Elliott MN, Morales LS, Diamant AL, Hambarsoomian K, Schuster MA. Adolescent participation in preventive health behaviors, physical activity, and nutrition: Differences across immigrant generations for Asians and Latinos compared with whites. American Journal of Public Health. 2007;97:337–343. doi: 10.2105/AJPH.2005.076810. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Values correspond to correlation coefficient, P value, and number of observations for each association (N value).
**Correlation coefficient is significant at P value <0.01 (2-tailed).
*Correlation coefficient is significant at P value <0.05 (2-tailed).
aValues are beta coefficients (β) and 95% confident intervals (CI) for children’s BMI z-score for one unit increase in predictor variables; added sugars per 5 units, and SSB per 100 units, respectively.
bLinear regression models were adjusted for children’s age and gender. Cook’s distance test was used to determine influencing observations on linear associations.
SSB, sugar-sweetened beverages.
Values correspond to correlation coefficient, P value, and number of observations for each association (N value).
**Correlation coefficient is significant at P value <0.01 (2-tailed).
*Correlation coefficient is significant at P value <0.05 (2-tailed).