Abstract
Background and Objectives:
Therapeutic laparoscopy was incorporated into surgical practice more than 25 y ago. Several modifications have since been developed to further minimize surgical trauma and improve results. Minilaparoscopy, performed with 2- to 3-mm instruments was introduced in the mid 1990s but failed to attain mainstream use, mostly because of the limitations of the early devices. Buoyed by a renewed interest, new generations of mini instruments are being developed with improved functionality and durability. This study is an objective evaluation of a new set of mini instruments with a novel low-friction design.
Method:
Twenty-two medical students and 22 surgical residents served as study participants. Three designs of laparoscopic instruments were evaluated: conventional 5 mm, traditional 3 mm, and low-friction 3 mm. The instruments were evaluated with a standard surgical simulator, emulating 4 exercises of various complexities, testing grasping, precise 2-handed movements, and suturing. The metric measured was time to task completion, with 5 replicates for every combination of instrument–exercise–participant.
Results:
For all 4 tasks, the instrument design that performed the best was the same in both the medical student and surgical resident groups. For the gross-grasping task, the 5-mm conventional instruments performed best, followed by the low-friction mini instruments. For the 3 more complex and precise tasks, the low-friction mini instruments outperformed both of the other instrument designs.
Conclusion:
In standard surgical simulator exercises, low-friction minilaparoscopic instruments outperformed both conventional 3- and 5-mm laparoscopic instruments for precise tasks.
Keywords: Low-friction instruments, Microlaparoscopy, Minilaparoscopy, Needlescopic surgery, Surgical simulator
INTRODUCTION
Therapeutic laparoscopy was incorporated into the practice of general surgery more than 25 years ago. Since that time, several modifications to minimally invasive access and surgery have been developed with the purpose of further minimizing surgical trauma and improving results: minilaparoscopy, computer-assisted robotic surgery, single-incision laparoscopic surgery, and natural orifice surgery. The lack of clear improvement in overall safety, effectiveness, and value has kept these other approaches from replacing conventional laparoscopy.1,2
Smaller diameter (2–3 mm) instruments, trocars, and scopes for use in procedures usually termed minilaparoscopy were introduced in the mid 1990s.3 Minilaparoscopy was promoted to minimize scarring, reduce postoperative pain, improve visualization in small fields, and improve surgical results, but it failed to become mainstream for a variety of reasons.4–9 Renewed interest in this approach has developed recently on the part of surgeons and medical device companies. Significant effort is being devoted to improving the ease of use, functionality, quality, and durability of minilaparoscopic instruments. A novel design of mini instruments was recently developed and precisely manufactured to minimize friction between instruments and trocars (0.1 N vs. 4.3 N), based on exact experimentally determined optimal tolerances (minimal gap between trocar and instrument) and absence of trocar valves.10–14 We conducted a study to evaluate these new low-friction mini instruments, comparing them to both 3-mm mini instruments and 5-mm traditional instruments, in a standardized set of simulation exercises.
METHOD
Institutional Review Board Approval
The authors submitted the proposal for this study to the Institutional Review Board at the University of Pernambuco, and a full exemption was provided, with consideration that the study subjects were medical students and residents working in a dry lab setting, with no patients or patient data involved.
Study Participants
Study participants were selected by testing surgical novices (medical students) and individuals with beginner–intermediate surgical experience (postgraduate year [PGY]-1 and -2 surgical residents); excluding participants with known visual, motor, or other impairment; excluding participants with prior advanced training in conventional or minilaparoscopy (experts); and training all study participants on all instrument designs, with at least 2 h of training occurring on 2 separate days. We opined that the results would be cleaner and easier to interpret if we excluded surgeons who could have been expert in the use of any of the 3 instrument designs. Including an expert in the use of any of the instruments could have biased that group toward that instrument, thus potentially confounding any actual differences attributable to the design. Based on pilot studies, it was determined that 22 medical students and 22 surgical residents would provide an adequate sample size to detect a difference in instrument performance (power, 80%; confidence level, 95%; Win episcope version 2.0 statistical software; developed by the Veterinary Faculty, University of Zaragoza, Spain, and the Department of Animal Husbandry, Wageningen Agricultural University, The Netherlands). The students and the residents were tested and analyzed as 2 separate groups.
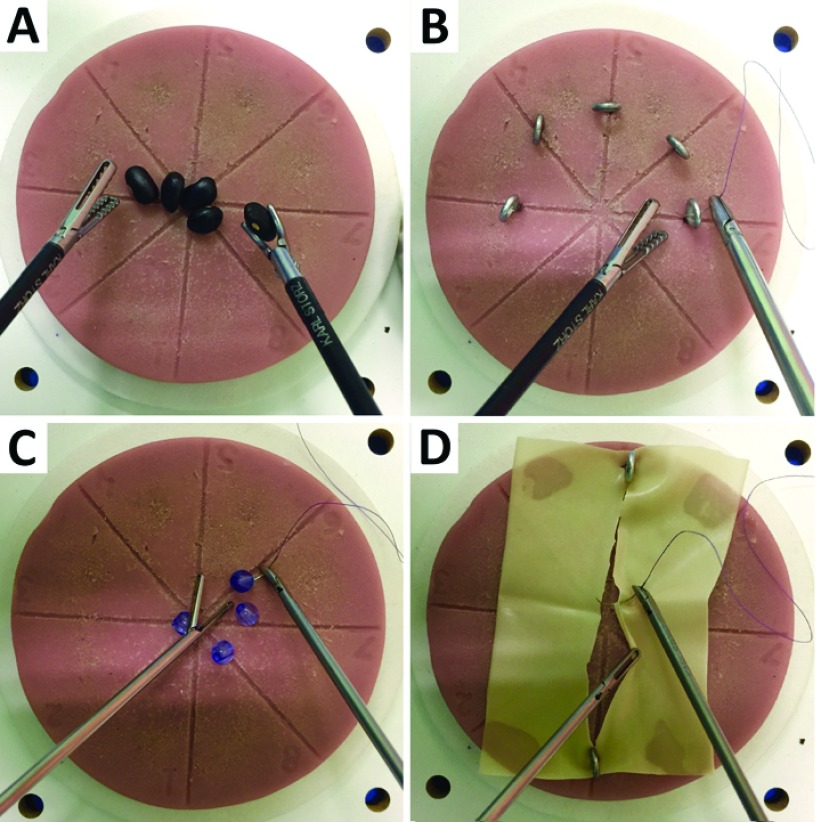
Laparoscopic Simulation
The surgical simulator was selected for its recognized applicability, portability, and ease of use (ProDelphus E-Knot, Olinda, Brazil) (Figure 1A). Four standardized tasks were selected to simulate grasping, 2-handed movement, manipulation, and suturing, respectively: bean collection—grasping and moving 5 beans, one by one, into a bowl; small rings—passing a suture through 5 variously oriented fixed metal rings (eye bolts); pearl necklace—2-handed threading of a suture through four beads to create a necklace; and suture and knot—passing a curved needle and suture through a laceration in a Penrose drain, using a simple suture technique and a single square knot, with a 15-cm-long 5-0 polyglactin suture (Vicryl; Ethicon, Sao Paulo, Brazil) (Figure 2).
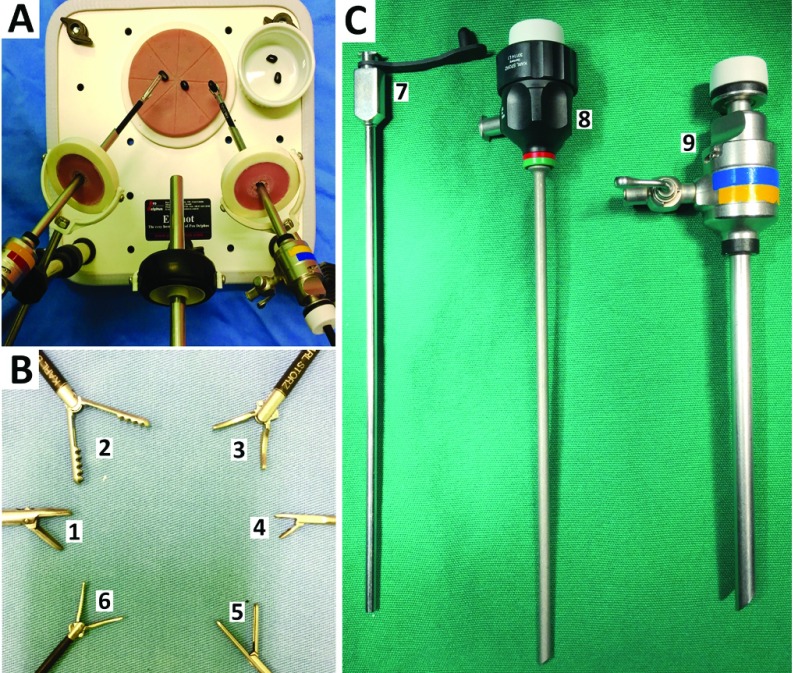
Figure 1.
A, The surgical simulator used for the 4 tasks (ProDelphus E-Knot, Olinda, Brazil). B, C, Photographs of the 5-mm conventional laparoscopic instruments, 3-mm mini instruments, and 3-mm low-friction mini instruments (Karl Storz Endoscopy, Tuttlingen, Germany). B1, 5-mm needle-holder; B2, 5 mm grasper forceps; B3, 5-mm Maryland forceps; B4, 3-mm needle holder; B5, 3-mm grasper forceps; B6, 3-mm Maryland forceps; C7, 3.5-mm-diameter, 15-cm-long low-friction mini trocar; C8, 3.8-mm-diameter, 15-cm-long conventional mini trocar; and C9, 6-mm diameter, 10.5-cm-long laparoscopic trocar.
Figure 2.
Four standardized tasks were selected to simulate grasping, 2-handed movement, manipulation, and suturing, respectively: A, collect beans—grasping and moving five beans, one by one, into a bowl; B, small rings—passing a suture through 5 variously oriented and fixed metal rings (eye bolts); C, pearl necklace—2-handed threading of a suture through 4 beads to create a necklace; and D, suture and knot—passing a curved needle and suture through a laceration in a Penrose drain, using a simple suturing technique and a single square knot with a 15-cm-long 5-0 polyglactin suture.
Instruments
The conventional laparoscopic instruments (5 mm) and trocars (6 mm) and the conventional-friction mini instruments (3 mm) and trocars (3.8 mm) are commercially available from Karl Storz Endoscopy (Tuttlingen, Germany). The low-friction configuration was created by replacing the conventional mini trocars with the new low-friction valveless trocars and retaining the same 3-mm mini instruments (Figure 1B, C). To increase precision of movement and decrease surgical stress for the surgeon and the patient during minilaparoscopic procedures, no seal or valve is used with the novel low-friction trocars, thus minimizing (essentially eliminating) the usual friction forces between trocar and instrument. The special trocar was designed to resemble a long needle, with very precise tolerances matching exactly the diameter of the corresponding 3-mm instruments. With this trocar system, the space between the instrument and the trocar is minimal, thereby eliminating the need for a rubber seal or valve to prevent gas loss. These low-friction mini trocars (3.5 mm) are also commercially available from Karl Storz Endoscopy. For each of the 3 instrument lines, the following instruments were chosen for use in this study: grasping forceps, curved Maryland dissectors, and needle drivers. (Figure 1B, C).
Data Acquisition
The exercises were performed with the surgical trainer placed on a surgical table in a hospital operating room (University Hospital Oswaldo Cruz, Recife, Brazil). All participants were allowed a 5-minute warm-up period. They were randomly assigned to perform each of the 4 standardized tasks, with each of the 3 sets of instruments (5-mm, mini, and low-friction mini) used in random order. The order of tasks and instruments was randomized to avoid potential confounding by serial performance or learning effects. All exercise–instrument combinations were performed in 5 replicates. The metric was time for task performance.
Data Analysis
Data analysis was performed by two independent consultant biostatisticians who had no interest in the study outcome (Ulisses Ramos Montarroyos, University of Pernambuco; Jose Edmilson Mazza Batista, Federal University of Pernambuco). Before the study was conducted, we decided to analyze the results for the 22 medical students and the 22 surgical residents as 2 separate groups. The biostatisticians recommended that all 5 replicates for each exercise–instrument combination be included in the analysis (there were insufficient outlier values to exclude highest and lowest values). Data sets were found to be normally distributed (Kolmogorov-Smirnov test). The data are graphically presented as mean (±SD) for each exercise–instrument–participant group combination. Paired samples were compared by Student's t test, α = 0.05 (STATA, version 12.0; StataCorp, College Station, Texas).
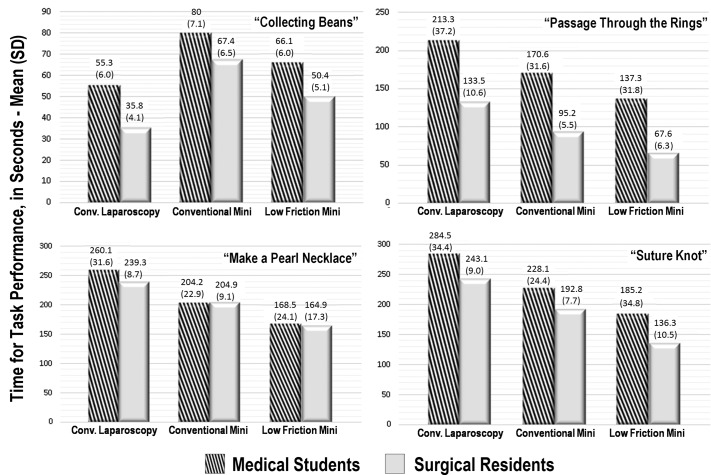
RESULTS
The results are summarized in Table 1 and are presented graphically in Figure 3, with means and standard deviations shown for every task–instrument–participant combination. For all 4 tasks, the instrument design that performed the best was the same for both the medical student group and the surgical resident group. For the bean-collection gross-grasping exercise, the 5-mm instruments performed best, followed by the low-friction mini instruments. For the other 3 more complex and precise exercises—small rings, pearl necklace, and suturing and knot—the low-friction mini instruments performed best, followed by the conventional mini instruments.
Table 1.
Time to Completion of the 4 Tasks
| Group | Beans | Small Rings | Pearl Necklace | Suture and Knot |
|---|---|---|---|---|
| Medical students | ||||
| Conventional laparoscopy | 55.3 ± 6.0 | 213.3 ± 37.2 | 260.1 ± 31.6 | 284.5 ± 31.6 |
| Conventional mini | 80.0 ± 7.1 | 170.6 ± 31.6 | 204.2 ± 22.9 | 228.1 ± 24.4 |
| Low-friction mini | 66.1 ± 6.0 | 137.3 ± 31.8 | 168.5 ± 24.1 | 185.2 ± 34.8 |
| Surgical residents | ||||
| Conventional laparoscopy | 35.8 ± 4.1 | 135.5 ± 10.6 | 239.3 ± 8.7 | 243.1 ± 9.0 |
| Conventional mini | 67.4 ± 6.5 | 95.2 ± 5.5 | 204.9 ± 9.1 | 192.8 ± 7.7 |
| Low-friction mini | 50.4 ± 5.1 | 67.6 ± 6.3 | 164.9 ± 17.3 | 136.3 ± 10.5 |
Average times are shown in seconds (mean ± SD) for the 3 laparoscopic instrument designs: 5-mm conventional laparoscopy, 3-mm conventional minilaparoscopy, and 3-mm low-friction minilaparoscopy. The results of all comparisons—conventional vs. conventional mini, conventional vs. low-friction mini, and conventional mini vs. low-friction mini—showed statistically significant differences for the 4 tasks. P < 0.0001.
Figure 3.
Results of all 4 tasks. Average times for both participant groups are shown in seconds (mean, SD) for the 3 different laparoscopic instrument designs: 5-mm conventional, 3-mm conventional mini, and 3-mm low-friction mini. All comparisons (conventional vs. conventional mini, conventional vs. low-friction mini, and conventional mini vs. low-friction mini) showed significant differences for all 4 tasks. P < .0001.
DISCUSSION
The potential advantages of minilaparoscopy are apparent and applicable to multiple stakeholders. To patients, the advantages of minilaparoscopy over traditional laparoscopy seem clear: smaller incisions, less scaring, and reduced postoperative pain.15,16 For surgeons, the transition from conventional laparoscopy to minilaparoscopy is intuitive: trocar and instrument positions are preserved, triangulation is maintained, operative technique is the same or similar, and the technical challenges inherent to natural orifice and single incision approaches are avoided. For payers and hospitals, there is no need to purchase giant equipment, and operating room costs are lower.17
Clinical studies have demonstrated some advantages of minilaparoscopy in technical feasibility, safety, effectiveness, and cost effectiveness for certain procedures.1–3,4,6,7,10,15,18–20 For laparoscopic cholecystectomy (LC), Sajid et al15 concluded in a meta-analysis that mini-LC results in less postoperative pain and better cosmesis than does conventional LC; Lima et al20 found a lower bile duct injury rate with mini-LC; and Carvalho et al17 demonstrated reduced hospital costs for clipless mini-LC. For laparoscopic inguinal hernia repair performed by using a mini technique, Lau and Lee21 found, in a prospective comparative study, less postoperative pain, and Carvalho et al22 found a shorter operative time. For transanal endoscopic microsurgery (TEM), Araujo et al11 concluded that mini instruments provide improved visualization in this limited working space compared to conventional 5-mm instruments. Improved visualization within in a small space may have contributed to the better results for the suturing task in this study. As we can see, in the endoscopic view, visualization was improved with the 3-mm mini instruments versus that attained with the 5-mm instruments at the same vantage point (Figure 4). Other clinical studies have found minilaparoscopy and conventional laparoscopy to yield similar outcomes. For mini-LC, Saad et al23 found no advantage in postoperative outcomes in a comparative study. For mini- versus conventional laparoscopic appendectomy, Sajid et al15 found similar perioperative outcomes and hospital stay. For hysterectomy, Ghezzi et al24 found no difference in postoperative pain with mini- versus conventional laparoscopy. None of these investigators used low-friction mini instruments, and none found standard-friction mini instruments to be inferior to conventional 5–10-mm laparoscopic instruments.
Figure 4.
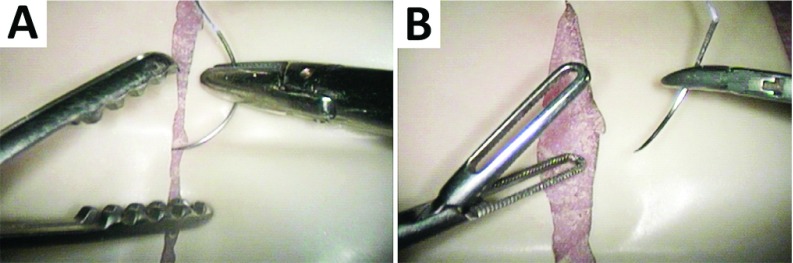
Endoscopic views taken by a 10-mm 30° scope (Karl Storz) of the suture-and-knot task. Photographs were taken at exactly the same vantage point for (A) 5-mm and (B) 3-mm instruments. The better visualization obtained with the mini instruments can be observed.
Why has minilaparoscopy failed to become more mainstream? In an elegant study in a dry lab, Rosser et al25 showed a decrease in the performance of laparoscopic surgeons when using early minilaparoscopic instruments when compared with traditional laparoscopic instruments. Early generations of 2- to 3-mm laparoscopic instruments had several mechanical limitations, including instrument bending, lack of insulation and electrocautery, suboptimal effector tip functionality, and poor durability. These limitations hampered adoption, experience, and, probably, outcomes. As computer-assisted robotic surgery, single-incision laparoscopy, and natural orifice surgery appeared, but then struggled to replace conventional laparoscopy, a renewed interest developed in minilaparoscopy, causing surgeon-innovators and industry leaders to begin developing newer generations of mini instruments with improved performance. One innovation is the development of novel low-friction reusable multifunctional mini trocars. The new low-friction trocars consist of an outside part, such as a needle, but are longer than the traditional mini trocars. The insert, with a progressively dilating tip and minimal gap, causes less damage to muscle layers and skin during insertion than do traditional trocars. To facilitate placement, the insert fits very firmly into a Luer lock connector type that can also be used for suction or gas inflation and is specially useful for creating the retroperitoneal space for totally extraperitoneal (TEP) hernia repair and lumbar sympathectomy.10,12,14 Research and development of these devices revealed that very narrow, exact clearances between precisely manufactured instruments and trocars would allow for the elimination of the CO2 valve from the trocar. Doing so resulted in a decrease in instrument friction from 4.3 to 0.13 N, with minimum leakage of CO2 (0.1 L/min).10,12–14 Early bench model tests of these low-friction mini instruments noted favorable surgeon perceptions.13 The notable reduction of the friction forces between the trocar and the mini instruments results in less trocar movement and fewer trocar dislocations from the abdominal wall, which should reduce abdominal wall trauma and contribute to improved cosmetics results.1,2,12,14
The experimental study reported herein was undertaken to test these low-friction instruments objectively, in a variety of simulated laparoscopic tasks, compared to both conventional minilaparoscopic instruments and conventional 5-mm instruments.
In this study, for the bean-collection task (a simple gross-movement exercise), the larger effector tips of the 5-mm instruments appeared to have the advantage over the smaller effector tips of the mini instruments. It is of interest, however, even with this task, that the low-friction mini instruments outperformed the conventional-friction mini instruments. For the other 3 tasks, all of which require 2-handed precise movements, the low-friction mini instruments outperformed either of the other 2 designs. In these experimental models, the low-friction design seemed to offer an advantage for precise coordinated surgical movements. Whether this same advantage will be observed with the clinical application of these low-friction trocars remains to be seen. Some early results from their application to mini-LC suggest that it may.2
The limitations of this study include those inherent in simulator-based basic research. The study was not clinical. The participants (intentionally) included novices, beginners, and those with intermediate experience, not specialists in minimally invasive surgery. Metrics were time based only, with no metrics for efficiency of movement, surgeon ergonomics, or surgeon perception of the experience. Finally, the simulated surgical tasks were of various levels of complexity, but still were less complex than the human surgical experience.
CONCLUSION
In standard surgical simulator exercises, low-friction minilaparoscopic instruments outperformed both conventional 3- and 5-mm laparoscopic instruments in executing precise tasks.
Contributor Information
Wood A. Firme, Faculty of Medical Sciences, University of Pernambuco, Recife, Brazil.; Private practice in plastic surgery, Recife, Brazil
Gustavo L. Carvalho, Faculty of Medical Sciences, University of Pernambuco, Recife, Brazil.; Surgical Clinic for Videolaparoscopy.
Diego L. Lima, Faculty of Medical Sciences, University of Pernambuco, Recife, Brazil.; TOA Surgical Specialists, Durham, North Carolina.
Vladmir Goldstein de Paula Lopes, Faculty of Medical Sciences, University of Pernambuco, Recife, Brazil..
Isabelle D. Montandon, Faculty of Medical Sciences, University of Pernambuco, Recife, Brazil.
Phillip P. Shadduck, TOA Surgical Specialists, Durham, North Carolina.; North Carolina Specialty Hospital, Duke Regional Hospital, and Duke University, Durham, North Carolina.
References:
- 1. Carvalho GL, Cavazzola LT, Rao P. Minilaparoscopic surgery: not just a pretty face! What can be found beyond the aesthetics reasons? J Laparoendosc Adv Surg Tech A. 2013;23:710–713. [DOI] [PubMed] [Google Scholar]
- 2. Lima DL, Passos GO, Jr., Barros JS, et al. Minilaparoscopic cholecystectomy: the lessons learned after 13 years of experience and 1750 cases (abstract). Surg Endosc. 2014;28(suppl):S247. [Google Scholar]
- 3. McCloy R, Randall D, Schug SA, et al. Is smaller necessarily better? A systematic review comparing the effects of minilaparoscopic and conventional laparoscopic cholecystectomy on patient outcomes. Surg Endosc. 2008;22:2541–2553. [DOI] [PubMed] [Google Scholar]
- 4. Gupta A, Shrivastava UK, Kumar P, Burman D. Minilaparoscopic versus laparoscopic cholecystectomy: a randomised controlled trial. Trop Gastroenterol. 2005;26:149–151. [PubMed] [Google Scholar]
- 5. Carvalho GL, Loureiro MP, Bonin EA, et al. Minilaparoscopic technique for inguinal hernia repair combining transabdominal pre-peritoneal and totally extraperitoneal approaches. JSLS. 2012;16:569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Krpata DM, Ponsky TA. Needlescopic surgery: what's in the toolbox? Surg Endosc. 2013;27:1040–1044. [DOI] [PubMed] [Google Scholar]
- 7. Mamazza J, Schlachta CM, Seshadri PA, Cadeddu MO, Poulin EC. Needlescopic surgery: a logical evolution from conventional laparoscopic surgery. Surg Endosc. 2001;15:1208–1212. [DOI] [PubMed] [Google Scholar]
- 8. Carvalho GL, Cavazzola LT. Can mathematic formulas help us with our patients? Surg Endosc. 2011;25:336–337. [DOI] [PubMed] [Google Scholar]
- 9. Loureiro M, Bonin E. Minilaparoscopy: here and now. Bras J Video Surg. 2011;4:30–34. [Google Scholar]
- 10. Carvalho GL, Melani AG, Veo CAR, et al. New low friction adapter for using minilaparoscopic instruments with transanal endoscopic microsurgery (TEM) improves visualization and dexterity (abstract). Surg Endosc. 2013;27:S164. [Google Scholar]
- 11. Araujo SEA, Mendes CRS, Carvalho GL, Lyra M. Surgeons' perceptions of transanal endoscopic microsurgery using minilaparoscopic instruments in a simulator: the thinner the better. Surg Endosc. 2015;29:2331–2338. [DOI] [PubMed] [Google Scholar]
- 12. Carvalho GL, Lima DL, Sales AC, et al. A new very low friction trocar to increase surgical precision and improve aesthetics in minilaparoscopy. Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), 2011, Program number: ETP077. Available at: Abstract web page, http://www.sages.org/meetings/annual-meeting/abstracts-archive/a-new-very-low-friction-trocar-to-increase-surgical-precision-and-improve-aesthetics-in-minilaparoscopy/ or Poster web page, http://www.sages.org/wp-content/uploads/posters/2011/36229.jpg?b52878 Accessed August 19, 2015.
- 13. Passos GO, Jr, Lima DL, Silva FW, et al. Surgeons' perceptions in relation to the minilaparoscopic instruments in surgical knots construction (abstract). Surg Endosc. 2014;28(suppl):S333. [Google Scholar]
- 14. Carvalho GL, Sales AC, Silva JS, Rocha RG, Lima DL, Fernandes FA., Jr Are minilaparoscopic (needlescopic) trocars of 2 mm and 3 mm without valve and sealing membrane a viable option (abstract)? Surg Endosc. 2011;25(suppl):S351. [Google Scholar]
- 15. Sajid MS, Khan MA, Ray K, Cheek E, Baig MK. Needlescopic versus laparoscopic cholecystectomy: a meta-analysis. ANZ J Surg. 2009;79:437–442. [DOI] [PubMed] [Google Scholar]
- 16. Carvalho GL, Lima DL, Sales AC, et al. New minimally invasive surgical approaches—NOTES, less mini: which is the preferred among patients (abstract)? Surg Endosc. 2012;26(suppl):S291. [Google Scholar]
- 17. Carvalho GL, Coelho RDEMC, Paulo P, Albuquerque CDE. Clipless minilaparoscopic cholecystectomy vs. conventional laparoscopy: a comparative study of the hospital charges for minimally invasive treatments for call bladder diseases. Bras J Video Surg. 2010;3:37–42. [Google Scholar]
- 18. Novitsky YW, Kercher KW, Czerniach DR, et al. Advantages of mini-laparoscopic vs. conventional laparoscopic cholecystectomy: results of a prospective randomized trial. Arch Surg. 2005;140:1178–1183. [DOI] [PubMed] [Google Scholar]
- 19. Carvalho GL, Silva FW, Silva JSN, et al. Needlescopic clipless cholecystectomy as an efficient, safe, and cost-effective alternative with diminutive scars: the first 1000 cases. Surg Laparosc Endosc Percutan Tech. 2009;19:368–372. [DOI] [PubMed] [Google Scholar]
- 20. Lima DL, Passos GO, Jr, Barros JS, et al. Minilaparoscopic cholecystectomy is associated with a lower bile duct injury rate: a systematic review (abstract). Surg Endosc. 2014;28(suppl):S437. [Google Scholar]
- 21. Lau H, Lee F. A prospective comparative study of needlescopic and conventional endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2002;16:1737–1740. [DOI] [PubMed] [Google Scholar]
- 22. Carvalho GL, Loureiro MP, Bonin EA, et al. Minilaparoscopic technique for inguinal hernia repair combining transabdominal pre-peritoneal and totally extraperitoneal approaches. JSLS. 2015;16:569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saad S, Strassel V, Sauerland S. Randomized clinical trial of single-port, minilaparoscopic and conventional laparoscopic cholecystectomy. Br J Surg. 2013;100:339–349. [DOI] [PubMed] [Google Scholar]
- 24. Ghezzi F, Cromi A, Siesto G, et al. Minilaparoscopic versus conventional laparoscopic hysterectomy: results of a randomized trial. J Minim Invasive Gynecol. 2013;18:455–461. [DOI] [PubMed] [Google Scholar]
- 25. Rosser J, Olive D, Zreik T, Duleba A, et al. Decreased performance of skilled laparoscopic surgeons at microlaparoscopy versus traditional laparoscopy. J Am Assoc Gynecol. Laparosc. 1996;3(suppl 4):S44. [DOI] [PubMed] [Google Scholar]