Abstract
Although radiotherapy is effective in managing abdominal and pelvic malignant tumors, radiation enteropathy is still unavoidable. This disease severely affects the quality of life of cancer patients due to some refractory lesions, such as intestinal ischemia, mucositis, ulcer, necrosis or even perforation. Current drugs or prevailing therapies are committed to alleviating the symptoms induced by above lesions. But the efficacies achieved by these interventions are still not satisfactory, because the milieus for tissue regeneration are not distinctly improved. In recent years, regenerative therapy for radiation enteropathy by using mesenchymal stem cells is of public interests. Relevant results of preclinical and clinical studies suggest that this regenerative therapy will become an attractive tool in managing radiation enteropathy, because mesenchymal stem cells exhibit their pro-regenerative potentials for healing the injuries in both epithelium and endothelium, minimizing inflammation and protecting irradiated intestine against fibrogenesis through activating intrinsic repair actions. In spite of these encouraging results, whether mesenchymal stem cells promote tumor growth is still an issue of debate. On this basis, we will discuss the advances in anticancer therapy by using mesenchymal stem cells in this review after analyzing the pathogenesis of radiation enteropathy, introducing the advances in managing radiation enteropathy using regenerative therapy and exploring the putative actions by which mesenchymal stem cells repair intestinal injuries. At last, insights gained from the potential risks of mesenchymal stem cell-based therapy for radiation enteropathy patients may provide clinicians with an improved awareness in carrying out their studies.
Facts
Radiation enteropathy severely affected the quality of life of cancer patients nowadays.
Preclinical data suggest the pro-regenerative effects of mesenchymal stem cells on irradiated intestine.
Epinal case report reveals the specific effectiveness of mesenchymal stem cells in managing pelvic radiotherapy-induced lesions in rectum and bladder lesions.
Open Questions
Due to most of radiation enteropathy patients are cancer survivors, is really that mesenchymal stem cells will initiate or promote their tumor growth?
How to carry out a clinical trial for evaluating the therapeutic potentials of mesenchymal stem cells for radiation enteropathy?
Will the mesenchymal stem cell-based therapy be an attractive tool for clinicians in managing radiation enteropathy patients in the future?
Radiotherapy is powerful in treating malignant tumors. According to the published data, at least 50% of cancer patients need radiotherapy during their treatment course, and approximately 25% of solid tumors undergo complete remission after radiotherapy.1 However, damage to healthy tissue within the radiation field remains unavoidable. For abdominopelvic radiotherapy, the intestine is defined as an organ at risk (OAR). Herein, small intestine commonly presents acute injuries due to its high α/β ratio of >10 Gy according to linear-quadratic (L-Q) model. Besides, the estimated α/β ratio in rectum varies between 4.8 Gy and 5.4 Gy, commonly allowing for grade ≥2 toxicity happening.2, 3 Radiation-induced intestinal injuries/toxicities are known as radiation enteropathy (RE), which can be classified into two phases. Early RE commonly occurs within 3 months of radiotherapy, with an incidence of ~50%.4 Late RE can be observed from 1 to 20 years post radiotherapy, with the incidence of 2–20%.5, 6 Several factors are involved in the development of late RE, including progressive cell loss and vascular obliteration in irradiated intestine, which will result in emergent or even fatal complications, such as obstruction, perforation, intestinal necrosis or acute hemorrhage.6, 7
Current clinical interventions for early RE mainly aim to relieve abdominal pain and diarrhea through spasmolysis and anti-edema drugs, maintaining electrolyte balance through conditional nutrient supplementation and alleviating inflammation or infection using antioxidants, glucocorticoids or antibiotics.8 For late RE, lesioned intestine can be managed merely by surgery.8 However, resection of diseased intestine appears to be not very effective, because the fibrogenesis in irradiated intestine could not be inhibited. Additionally, intestinal adhesion following surgery and dystrophia induced by removing a large portion of intestine adversely affect patient quality of life.9 In recent years, the outcome from clinical studies exhibited the effectiveness of Pentoxifylline-Vitamin E in preventing intestinal fibrosis.10, 11 Meanwhile, several preclinical studies proposed some available agents for managing late RE, including ROCK inhibitor (Y-27632),12 Pravastatin13 and Simvastatin.14 In addition to developing potential drugs, several preclinical studies were carried out for evaluating the therapeutic potentials of mesenchymal stem cells (MSCs) for RE.
MSCs, a population of undifferentiated cells deriving from early ectoderm and can be harvested from various tissues and organs.15 MSCs can secret various types of growth factors, immune mediators and anti-fibrotic effectors, which are potent in mediating tissue regeneration.16, 17, 18 And several clinical trials revealed the immunomodulatory benefits of MSCs in treating graft versus host disease (GVHD), inflammatory bowel disease (IBD), systemic lupus erythematosus (SLE) and arthritis.19, 20, 21, 22 Moreover, four patients, suffering from pelvic radiotherapy-induced injuries in rectum and in bladder, were successfully treated in Epinal Medical Center by using MSCs.6, 23 The effectiveness of MSCs lies in reducing abdominal pain, stanching rectal hemorrhage and healing fistula.23 On this basis, we propose that managing RE patients by using MSCs will be an attractive therapeutic approach in the future.
In this review, we will build on evidence of an effect of MSCs on irradiated intestine by discussing the actions behind this effect, together with evidence relating to advances in anticancer therapy by using MSCs, to suggest the feasibility of MSCs in treating cancer patients with RE. At last, we will introduce the future efforts into carrying out MSC-related clinical trials for managing RE.
Potential Factors Involved in Pathogenesis of RE
Refractory lesions in the irradiated intestine develop through a lengthy process comprising multiple steps and contributory factors, although the mechanisms involving in RE pathogenesis remain unclear. Radiation-induced injuries refer to the histopathological changes in the epithelium and endothelium, where the oxidative stress and extended inflammation played a predominant role in leading to lesions, including ischemia, ulcer, necrosis or fibrosis.24, 25 In this section, current understanding on the pathogenesis of RE will be shared.
Epithelial event: Intestinal stem cell injury-induced de-epithelialization
The intestinal epithelium has a rapid self-renewal capacity, with a complete turnover time of ~96 h due to rapid cycling of cells within the crypts of Liberkühn.26 The crypt base columnar (CBC) stem cells are responsible for maintaining homeostasis of intestinal epithelium by their producing progeny: transit-amplifying cells, which are committed into mature epithelial cells after 4–5 divisions (Figure 1).27, 28
Figure 1.
The structure of villus-crypt axis. This figure shows the homeostasis of intestinal epithelium regulating by CBC stem cells
The CBC stem cells are radiosensitive.29 It was reported that irradiation doses of at least 0.01 Gy are sufficient to result in apoptosis in 10% of CBC stem cells.30 The pro-apoptotic effects of ionizing irradiation on CBC stem cells are dependent on their cell-cycle stage.29 Ionizing irradiation will cause more DNA double-strand breaks (DSB) in G2/M phase than in G1/S phase.31 The average dividing time of CBC cells is reported to be 21.5 h, which classifies them as rapid cycling and radiosensitive cells thereby.32
Recent evidence suggested that the CBC stem cells are indispensable for epithelial regeneration upon being irradiated.33 If the intestine receives the doses between 6 Gy and 12 Gy, CBC stem cells can be replenished by another pool of intestinal stem cells at the 4+ position of crypts.34, 35 Yet, if the irradiation doses are higher than 12 Gy, the CBC stem cells will rapidly die along with subsequent depletion of Paneth cells, who form the niches of CBC stem cells.33, 36 Together with the following processes, such as vascular damage-induced ischemia, oxidative stress and extended inflammation in irradiated sites, the milieus feeding CBC stem cells are further deteriorated, which even results in crypt death.37 Ultimately, the barrier function of epithelium is lost thereby (Figure 2).
Figure 2.
The pathogenesis of radiation enteropathy. Four events are involved in the pathogenesis of radiation enteropathy, including de-epithelization, ischemia, oxidative stress and fibrogenesis
Vascular event: endothelial injury-induced ischemia
The endothelial cells are primary targets of ionizing irradiation, and the apoptosis of endothelial cells accounts for the severity of lesions within irradiated intestine.38, 39 Evidence lie in that during the first 4 h after lethal irradiation, the apoptotic cells, most of which are positive for CD31, are mainly located in the laminar propria of the villi rather than the epithelial layer.40 However, at 10 h post irradiation, numerous apoptotic cells are diffusely located in the epithelial layer from villi to crypt compartments rather than the laminar propira.40 This switch of apoptosis from endothelial cells to epithelial cells indicates that injuries in irradiated intestinal cells are first occurred in endothelium.39, 40
After endothelial injury occurring, sub-endothelial extracellular matrix (ECM) components are exposed to platelets, which initiate hemostasis mechanisms by forming clots.41 The coagulation cascade is hyperactivated by excessive secretion of von Willebrand factor (vWF) from injured endothelial cells, which results in vascular occlusion ultimately.42 Then, vascular permeability will be increased, which leads to hyperemia or hemorrhage within injured sites.43 As a result, the irradiated intestine has a poor blood supply (Figure 2).
Inflammatory event: increasing oxidative stress and extending inflammation
The chemical reactions that reduce cell viability in irradiated tissues have been identified as excessive production of ROS, such as superoxide radicals and hydrogen peroxide, which derive from intracellular water oxidized by radiation energy and from mitochondria.44, 45 Under this condition, ROS can activate the signaling pathways leading to cell death in irradiated sites.46, 47 Following these processes, leucocytes roll to the damaged intestine in a short time for eliminating dead cells (Figure 2).48, 49
Regarding the development of inflammation, current opinions believe that the molecular reactions in this process occur at sites extremely close to the vascular endothelium.50 Upon endothelial apoptosis, pro-inflammatory effectors will be secreted for the recruitment of leucocytes recruitment to injured sites.48, 50 Herein, neutrophils are the first cells to adhere to endothelium and migrate to injured sites, where they eliminate dead cell debris for facilitating tissue repair.41, 48, 49, 51 However, the irradiated epithelium always leads to a reduced barrier function.1 On this occasion, neutrophils also participate in eliminating large amounts of pathogens within the enteric cavity through secreting high levels of anti-pathogenic effectors, such as myeloperoxidase (MPO);52 this process will increase the oxidative stress within injured intestine and reduce tissue regeneration thereby (Figure 2). Meanwhile, upon exposure of injured tissues to pathogens, the cytotoxic T lymphocytes will eliminate the cells infected by these foreign stimuli through secreting cytolytic substances, such as perforin and granzymes, and through Fas/Fas ligand binding-induced apoptosis (Figure 2).53, 54 Thus, the presence of pathogens promotes inflammation and induces a switch from an innate immune response to an adaptive immune response,48, 54 which has the inflammation extended in irradiated sites.
Neuroimmune event: interactions between mast cells and enteric neurons
The neuroimmune interactions between enteric neurons and mast cells formulate a network for controlling intestinal responses to ionizing irradiation, presenting the lesions of mucositis and fibrosis.55 But the mast cells distinguish their contributions to the pathogenesis of RE.55 Upon being irradiated, the mast cells within intestinal mucosa will be activated, presenting the release of some effectors, such as TNF-α and leukotriene (LT), for attracting neutrophils to clear bacteria-induced infection (Figure 3).55 Moreover, these activated mast cells will enhance TNF-α secretion by macrophages as well as macrophage-mediated fibrin deposition for coagulation (Figure 3).55 But for the mast cells in connective tissue, their contribution to RE is secreting some pro-fibrotic effectors, such as TGF-β1, IL-4 and TNF-α (Figure 3).55 Although the exact mechanism by which neuroimmune interactions regulate the development of RE remains unknown, it is clear that the mediators from enteric sensory neurons, such as substance P and calcitonin gene-related peptide (CGRP), are critical for regulating the activation of mast cells. Herein, substance P is capable of amplifying the pro-inflammatory and pro-fibrotic responses of mast cells to ionizing irradiation through enhancing the secretions of histamine, TNF-α and TGF-β1 by these cells, whereas the CGRP protects intestine against radiation-induced injuries (Figure 3).55 From this aspect, it is rational to propose that substance P is even important in deciding the severity of RE through activating mast cells.
Figure 3.
The contribution of neuroimmune interactions to RE development. Upon being irradiated, the mast cells will be activated, presenting the release of pro-inflammatory and pro-fibrotic effectors, including TNF-α, histamine, LT, IL-4 and TGF-β1. These actions will be amplified by substance P, whereas be reversed by CGRP. LT, leukotriene; CGRP, calcitonin gene-related peptide
Microbial event: dysbiosis post-irradiation
McLaughlin et al.56 reported that the germ-free mice present radiation resistance comparing with conventional mice, indicating a potential link between the microbiota and host response to ionizing irradiation. As we are aware, the healthy gut contains nearly 300–500 bacterial species.57 These commensal bacteria confer the intestine a barrier function, presenting persistent epithelial turnover and vigorous immunity.57 For example, the NF-κB signaling pathway in epithelial cells and some intestine-specific immune cells will be activated upon the interactions between their toll-like receptors and luminal bacteria, which stimulate the epithelial proliferation as well as lead to immune tolerance of intestine to foreign antigens.58 However, when the epithelium loses its integrity post-irradiation, the commensal bacteria will transmigrate into intestinal tissue, functioning as bioterrorists for even triggering sepsis.57, 58 In this context, dysbiosis commonly occurs. Manichanh et al.59 reported that the bacterial constitution of feces is altered after the patients receiving pelvic radiotherapy, presenting the increased clusters of Bacilli and Actinobacteria, whereas decreasing in clostridial cluster. Besides, previous data indicated that the microbiota confer the intestinal endothelium and lymphocyts radiation sensitivity, which is linked to the suppression of fasting-induced adipose factor by luminal microbiota.60 To a certain extent, this finding corresponds to that endothelial injuries are the primary lesions of RE.40 In current opinions, the interactions between the microbiota and host regulate the intestinal responses to ionizing irradiation, and not all intestinal bacteria promote pathogenesis of RE.57, 58 For example, the microbiota can induce epithelial expression of nucleotide-binding oligomerization domain-containing protein 2 (NOD-2) against ischemia/reperfusion-induced hypoxic stress and autophagy,61 indicating the bacteriotherapy for RE is also promising.62
Fibrotic event: fibrogenesis after tissue injuries
Radiation-induced injuries in epithelium and endothelium have a central role in initiating intestinal fibrosis, which can be promoted by the extended inflammation within injured sites.24, 25 Upon epithelial injuries, irradiated intestine will reduce its barrier functions.1 On this occasion, the innate immune cells, such as macrophages and dendritic cells (DCs), will be activated by pathogens in enteric cavity, leading to secretion of pro-inflammatory cytokines, such as TNF-α, IL-1, IL-4 and IL-8.63 These cytokines activate some adaptive immune cells, such as Th2 and Th17 cell, which separately secrete IL-13 and IL-17 for promoting tissue remodeling (Figure 2).41, 63 Upon endothelial injuries, the blood vessels will increase their permeability, enabling recruitment of pro-inflammatory cells to injured sites.41 Among these infiltrated cells, the monocyte-macrophage system is reported to facilitate fibrosis through secreting PDGF, CTGF and TGF-β1, allowing for fibroblast-myofibroblast transition, myofibroblast proliferation and ECM deposition at injured sites (Figure 2).64, 65
Stem Cell-Based Regenerative Therapy for Rodent Models of RE
In the past decade, extensive efforts have been made in stem-cell based therapy for rodent models of RE (Table 1).
Table 1. Advances in regenerative therapy for rodent models of RE.
| Year | Researcher (Ref.) | MSC/ESC (gene-modified), source and specie | Animal | Total dose (position) | Main findings |
|---|---|---|---|---|---|
| 2006 | Sémont et al.66 | BM-MSC, human | NOD/SCID mice | 3.5 Gy (WBI)+4.5 Gy (AI) | •Hypertrophic villus-crypt axis •Maintaining the epithelial integrity |
| 2007 | Kudo et al.69 | ESC, 129/Sv cell line | ICR nu/nu mice | 30 Gy (AI) | •ESCs are committed to epithelial cells •Fail in prolong the lifespan of irradiated mice |
| 2008 | Zhang et al.79 | BM-MSC (CXCR4), β-Gal-transgenic mice | C57BL/6 J mice | 13 Gy (AI) | •Hypertrophic villus-crypt axis •Reducing intestinal permeability |
| 2010 | Kudo et al.68 | BM-MSC, C57BL/6 | ICR nu/nu mice | 30 Gy (AI) | •Decreasing mortality rate •Increasing body weight •Maintaining epithelial integrity |
| 2010 | Sémont et al.67 | BM-MSC, human | NOD/SCID mice | 3.5 Gy (WBI)+7 Gy (AI) | •Decreasing mortality rate •Maintaining absorptive function of epithelium •Restoring the integrity of epithelium •Increased number of proliferative cells in crypt •Decreased number of apoptotic cells in crypt |
| 2011 | Saha et al.70 | BM-MSC, C57BL/6 mice | Dipeptidlyl-peptidase-deficient mice; Lgr5-EGFP-IRES-CreERT2 mice | 10.4 Gy (WBI) 18 Gy (AI) | •Decreasing motality •Maintaining the integrity of epithelium •Mitigating inflammation |
| 2012 | Francois et al.71 | BM-MSC, C57BL/6 and IL-6−/− (B6. 129S2-Il6tmlKopf/J) | Barb/C mice | 9 Gy (WBI) | •Protecting mice against radiation-induced death •Hypertrophic villi •Stimulating epithelial regeneration mainly by MSC-derived IL-6 |
| 2012 | Gao et al. 72 | UC-MSC,a human | Barb/C mice | 7, 8.5, 10, 11.5 and 13 Gy (AI) | •Extending the life span of mice receiving 10 Gy •Hypertrophic villi •Maintaining epithelial integrity |
| 2013 | Chang et al.73 | Ad-MSC, human | Sprague-Dawley rats | 15 Gy (AI) | •Decreasing mortality rate •Increasing body weight •Mitigating inflammation •Accelerating neovascularization •Restoring epithelial integrity |
| 2013 | Linard et al.74 | BM-MSC, Göttingen pig | Göttingen pigs | 21–29 Gy (PI) | •Mitigating inflammation •Inhibiting fibrosis in irradiated site •Facilitating angiogenesis in irradiated site |
| 2013 | Yang et al.80 | BM-MSC (MSD), human | NOD/SCID mice | 4–6 Gy (AI) | •Decreasing mortality rate •Reducing the number of apoptotic cells •Mitigating inflammation •Maintaining integrity of epithelium |
| 2013 | Hu et al.81 | UC-MSC (Trx-1), human | NOD/SCID mice | 4.5 Gy (WBI) | •Maintaining epithelial integrity •Reducing oxidative stress |
| 2014 | Bessout et al.75 | BM-MSC, Sprague-Dawley rats | Sprague-Dawley rats | Gy (PI) | •Reducing mucosal inflammation •Promoting the proliferation of epithelial cells •Inducing apoptosis of radiation-activated T cells •Inhibiting infiltration and proliferation of T cells •Elevating the local levels of corticosterone •Upregulating the local expression of HSD11b1-steroidogenic enzyme |
Abbreviations: BM, bone marrow; Ad, adipose tissue; UC, umbilical cord; WBI, whole body irradiation; AI, abdominal irradiation; PI, Pelvic irradiation; HSD11b1, 11β-hydroxysteroid dehydrogenase type 1.
Using conditioned medium of UC-MSCs.
The therapeutic effects of MSCs on RE
To our knowledge, the first study was performed by Sémont et al.66 Their data showed that human MSCs exhibited potentials for maintaining the integrity of irradiated intestine.66 After MSC intervention, the irradiated mice survived longer than controls, and the epithelium showed hypertrophic villi, comprising increased numbers of proliferative cells and fewer apoptotic cells in the crypts. In addition, the newborn villus maintained its absorptive function via normal levels of Na+-K+-ATPase expression.67 Similarly, Kudo et al.68 reported that MSCs could extend the life span of irradiated mice, which was distinct from their previous data by using embryonic stem cells (ESCs) transplantation.69 Regarding the repair actions by MSCs, Saha et al.70 reported that MSCs could protect irradiated intestine by increasing serum levels of R-spondin1, KGF, IL-10 and PGE2, which function as effectors for promoting proliferation and inhibiting both apoptosis and inflammation within irradiated intestine. Besides, MSCs were capable of promoting epithelial regeneration using their secretion of IL-6.71 Moreover, the MSC-conditioned medium also exhibited the pro-regenerative potentials for irradiated epithelium.72 Besides, we found that MSC infusion could accelerate neovascularization within irradiated sites by triggering the intrinsic repair action of upregulated expressions of SDF-1, VEGF, basic FGF and Flk-1.73 Afterwards, by using a pig model of radiation proctitis, Linard et al.74 reported that repeated autologous transplantation of MSCs could counter act the inflammation in rectal mucosa by increasing host IL-10 production, and protect rectum against radiation-induced fibrosis by reducing local Col1a2/Col3a1 and TGF-β/CTGF expression and altering the matrix metalloproteinase (MMP)-tissue inhibitor of metalloproteinase (TIMP) balance as well. Similarly, based on using a rat model of radiation proctitis, Bessout et al.75 reported that autologous transplantation of MSCs was capable of mitigating the aberrant inflammation in the colorectal mucosa by elevating the local levels of glucocorticoid, which would inhibit the proliferation and induce apoptosis in radiation-activated T cells. These preclinical studies indicate that MSC-based therapy is potent for repairing the lesions associated with RE. Especially for using heterogenic MSCs, the host repair can be triggered as well, attributing to the autocrine/paracrine actions achieved by MSCs.
The MSC-based gene therapy for RE
The chemotactic properties of MSCs enable themselves to be used as delivery vehicles for the targeted secretion of tissue repair factors at injured sites. Herein, several lines of evidence showed that radiation-induced upregulation in CXCL12 expression is important for the homing of MSCs to injured sites through the interaction between CXCR4 and CXCL12.76, 77, 78 For improving the homing efficacy of MSCs toward irradiated intestine, Zhang et al. 79 established the MSCs, overexpressing CXCR4 gene, and found that the restoration of epithelial integrity was accelerated upon intervention by CXCR4 gene-modified MSCs. In another study, Yang et al. 80 reported that manganese superoxide dismutase (MSD) gene-modified MSCs were more effective than control MSCs in reducing mortality of irradiated mice, relieving gastrointestinal symptoms and restoring epithelial integrity with a spot of apoptotic cells in irradiated mice. Moreover, Hu et al.81 revealed that MSCs overexpressing Trx-1 gene were powerful in reducing oxidative stress in the irradiated intestine. Overall, the superior effectiveness of gene-modified MSCs over unmodified MSCs in healing RE can be attributed to the dual therapeutic effects of the high expression of ectopic genes and the intrinsic functions of MSCs.
Putative Actions Involved in RE Resolution by MSC Infusion
At present, the mechanisms involved in the repair of irradiated intestine by MSCs are still not fully investigated. But according to recent advances, we suggest several putative actions of RE management achieved by MSCs. In our opinion, the putative actions by which MSCs repair RE can be summarized as follows (Figure 4). Primarily, the engrafted MSCs induce infiltrated immune cells to switch from pro-inflammatory to anti-inflammatory cytokine secretion, resulting in milieus that promote anti-inflammatory events. As a secondary effect, repair responses are boosted by systemic events, such as elevated levels of regenerative facilitators, despite the rapid disappearance of donor MSCs.82 Thus, benign cytokine milieus cause regeneration of the injured intestine to be accelerated.
Figure 4.
The putative actions by which MSCs repair radiation enteropathy. Four steps are involved in the processes of MSCs healing injuries in irradiated intestine, including cell-homing, interacting with immune cells, boosting intrinsic repair actions and reversing the homeostasis of injured tissue
Step 1: homing to injured sites
Homing of infused MSCs to injured sites can be regarded as a prerequisite. According to recent data, several events mediated this homing process, such as CXCR1/2-CXCL8, CXCR4-CXCL12, CX3CR1-fractalkine, CCR7-CCL21 and ICAM-1/VCAM-1.77, 83, 84, 85 Upon these molecular bindings, MSCs first adhere to the endothelium, forming a defensive barrier against pathogens together with the pre-existing pericytes.86 The foreign MSCs then migrate to the laminar propria, where they perform pro-regenerative functions.87
Step 2: interacting with immune cells and bacteria
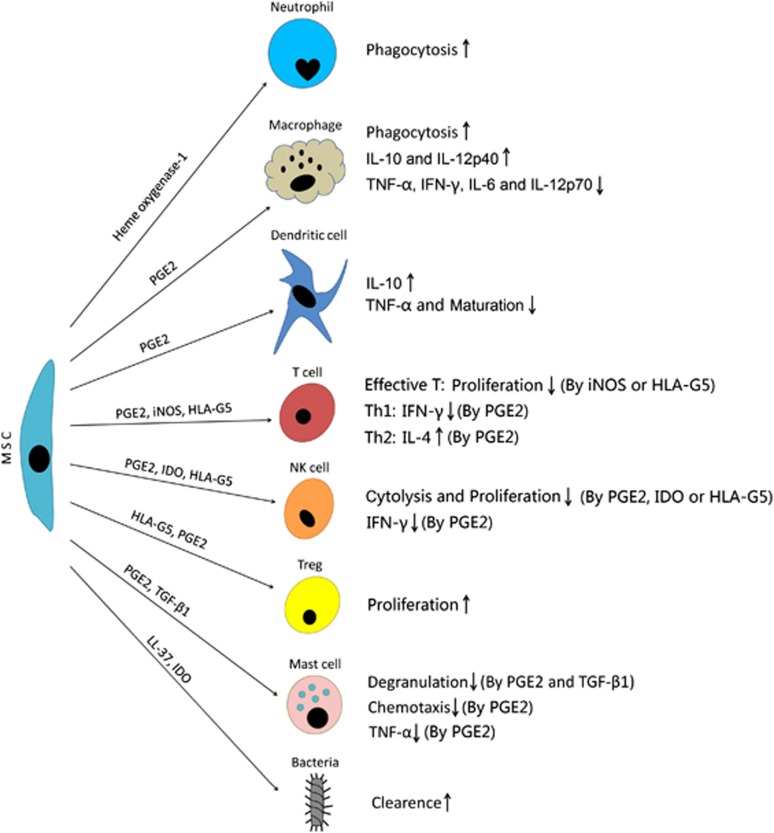
Cytokines secreted by both immune cells and MSCs mediate crosstalk among these cell types through regulatory feedback mechanisms, termed as ‘Educational action' of MSCs (Figure 5).17 The engrafted MSCs will alter the inflammatory milieus through interacting with infiltrated immune cells via secretion central immune mediators, including IL-10, PGE2, iNOS, IDO and HLA-G5.17 For example, in a co-culturing system, BM-MSC increases the IL-10 secretion and decreases the TNF-α secretion in DCs; reduces IFN-γ secretion in Th1 cells and natural killer (NK) cells, and increases IL-4 secretion in Th2 cells.88 Under the same conditions, macrophages increase IL-10 and IL-12p40 secretion, while reducing TNF-α, IFN-γ, IL-6 and IL-12p70 secretion.89 These effects have also been observed in vivo: Németh et al. 90 found that MSC infusion-induced elevation of host PGE2 has a central role in enhancing IL-10 synthesis by monocytes and macrophages from the lungs of septic mice, while reducing IL-12 secretion from these immune cells. These events inhibited neutrophil infiltration and IL-12-induced activations of both NK cells and cytotoxic T lymphocytes.90, 91
Figure 5.
The interactions between MSCs and immune cells/Bacteria. Upon co-culturing with MSCs, the pro-inflammatory profiles of immune cells, including macrophages, dendritic cells, T effector cells, NK cells and mast cells, will be altered into the anti-inflammatory ones. By contrast, the proliferation of Tregs will be promoted by MSCs. Besides, MSCs have the anti-bacterial potentials, and the phagocytosis by neutrophils and macrophages will be strengthened by MSCs
In addition to the antagonistic effects of MSCs on immune cell pro-inflammatory profiles, the MSCs can inhibit the proliferation of effective T lymphocytes through secreting iNOS or HLA-G5, inhibiting DC maturation using PGE2, and inhibiting NK-mediated cytolysis and NK proliferation using PGE2, HLA-G5 or IDO (Figure 5).92, 93, 94 In contrast to their anti-proliferative effects on such immune cells, MSCs will stimulate proliferation of regulatory T cells (Tregs) via secreting HLA-G5 and PGE2 (Figure 5).94, 95 Recent in vivo data also confirmed that MSC infusion can increase the Treg number in mice with colitis; this increase is dependent on MSCs migrating to the spleen and interacting with splenic CD11b+ innate immune cells.96, 97 But for radiation proctitis, current opinion on whether IL-10 and/or Tregs participate in suppressing mucosal inflammation seems to be contradictive. A previous study found that the antagonistic effect of MSCs on the inflammation in colorectal mucosa of rat exhibited the IL-10/Treg-independent manner, which is opposite to the finding by using a pig model.74, 75 In spite of similar strategies in establishing animal models of radiation proctitis and carrying out autologous transplantation, the mechanism by which MSCs mitigate intestinal inflammation probably varies among species. In addition, the following issues, including delivery times and doses of MSCs, appear to affect the host responses in clearing systemic or local inflammation.
As described above, neuroimmune interactions and dysbiosis contribute to the pathogenesis of RE. Fortunately, recent data suggested that MSCs antagonized the activation of mast cells by secreting PGE2 and TGF-β1, leading to decreased degranulation, reduced ability of chemotaxis and reduced release of TNF-α by mast cells (Figure 5).98, 99 Moreover, accumulative evidence suggest that human MSCs are powerful in protecting against Gram-negative bacteria-induced sepsis, relying on their secretions of LL-37, IDO and heme oxygenase-1 (HO-1), and strengthening the phagocytosis by neutrophils and macrophages as well (Figure 5).100, 101, 102, 103
Step 3: amplification of intrinsic repair
To date, it is still difficult to define the extent to which allogenic/heterogenic MSCs contribute to tissue regeneration, because immune rejection driven by recipient CD4+ and/or CD8+ T lymphocytes and oxidative stress within injured areas were reported to limit viability of infused MSCs.82, 104 But relatively few ectopic MSCs can lead to excellent therapeutic effects on injured host tissues that have a lost a large number of functional cells. A previous study reported that enhanced tissue repair achieved despite donor MSCs being rapidly eliminated after transplantation.105 From this point, we conclude that MSCs act as facilitators via triggering and boosting systemic repair responses. In spite of no consensus on whether the anti-inflammatory effect of MSCs on irradiated rectum of IL-10 and/or Treg involvment, reduced inflammation is always achieved after infusion of MSCs.74, 75 Combining with the actions of MSCs in clearing bacteria and minimizing the activation of mast cells, benign milieus for tissue regeneration are established, which will be beneficial to attract host bone marrow progenitors for reconstructing the niches of CBC stem cells and building on vasculature.106, 107 On this basis, by using the assistances from locally upregulated mitotic facilitators,70, 83 re-epithlialization and angiogenesis/neovascularization in the injured intestine are accelerated thereby.
Step 4: post-regeneration reversion of tissue homeostasis
When the neo-formed epithelium or endothelium is restored to its normal size and structure, p53-mediated cell-cycle arrest halts cell proliferation and prevents tissue hypertrophy. Levels of cytokine or hormone secretion are altered in the host tissue to maintain physiological epithelial homeostasis.108, 109 This process provides an adequate blood supply to the gut, eliminates inflammation and prevents fibrosis from developing in the irradiated intestine.
MSC and Cancer: A Latent Factor Affecting Security of MSCs for RE
The clinical responses of four Epinal patients to MSC-based therapy preliminarily revealed the specific roles of MSCs in treating pelvic radiotherapy-induced injuries in rectum and in bladder.6, 23 Although no evidence indicating the relapses in their prostate cancers after MSC intervention,23 the debate over whether MSCs promote the growth and metastasis of cancer cells or initiate new cancers persists for a long time, because truth lies in that majority of RE patients are still cancer survivors.110
‘Negative effects' of MSCs on tumor growth and their oncogenicity
Unrestricted cancer cell proliferation is largely driven by dysregulated growth signals originating from mutated genes.110 Some researchers believe that MSC-initiated immune suppression, immune cell dysfunction, cell division and angiogenesis could promote cancer progression.111, 112 In addition, MSCs would undergo spontaneous malignant transformation during a culture period of 105 weeks.113, 114, 115 Genomic instability, such as spontaneous p53 mutation in aged or in p21-deficient MSCs, was related to fibrosarcoma formation in vivo.114, 115, 116, 117 By contrast, the risk of genetic mutations or cell aging could be minimized, if MSCs are cultured for less than 16 weeks.118, 119
‘Positive effects' of MSCs on tumor growth and their anticancer potential
Recent data also suggested that MSCs exhibited potentials for inhibiting tumor growth through arresting cell cycling and activating signaling pathways related to cell death (Table 2).120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133 For example, human adipose MSCs could inhibit tumor cell expansion via secreting Dickkopf-related protein 1, a Wnt signaling antagonist.134, 135, 136 Another anticancer activity of MSCs involved the blockade of PI3K/Akt signaling pathway, leading to increased levels of cell-death related molecules, while decreased levels of cell survival-related molecules (Table 2).121, 133, 137
Table 2. Typical cases indicating the antagonistic effects of MSCs on tumor growth.
| Researcher (Ref.) | Study type | Tumor/cell line | MSC source/species | Gene modification (yes/no) | Molecular alteration in tumor cells | Main findings |
|---|---|---|---|---|---|---|
| Khakoo et al.121 | Ex/In vivo | Kaposi's sarcoma (KS) | BM human | No | Akt activity↓ | •Reducing KS cell growth ex vivo •Inhibiting KS tumorigenesis in vivo |
| Li et al.122 | Ex/In vivo | Multiple myeloma (MM)/H929 | Placenta human | No | Unknown | •Dose-dependent inhibition of MSCs on MM growth in vivo •Inducing apoptosis of osteoc-last precursor in vivo •Promoting bone formation in vivo •Inhibiting growth of H929 cell ex vivo |
| Ahn et al.123 | Ex/In vivo | Melanoma/AS375SM and A375P | Ad human | No | G0/G1 arrest | •Inducing the apoptosis in AS375SM and A375P cells ex vivo •Inhibiting melanoma growth in vivo |
| Nasuno et al.124 | Ex/In vivo | Azoxymethane-induced colonic carcinoma/IEC-6 | BM rat | No | G1 arrest pSmad2, IκBα and p21↑ 79 genes of WNT signaling pathway↓ | •Reducing tumor number in vivo •Altering the WNT and TGF-β/Smad signaling pathways in tumorigenesis in vivo •Suppressing AARGC(a genotoxic carcinogen)-induced acute apoptotic response in vivo •Reducing the formation of aberrant crypt foci in vivo •Reducing the number of DNA adducts of O6MeG in colonic epithelial cells •Inducing apoptosis of IEC-6 cells ex vivo |
| Katsuno et al.125 | Ex/In vivo | 1,2-dimethylhydrazine and dextran sulfate sodium-induced colorectal tumor/ACL15 | BM rat | No | TGF-β1↑ | •Reducing the number of aberrant crypt foci in vivo •Inhibiting the proliferation of ACL15 cells ex vivo |
| Lu et al.126 | Ex/In vivo | Hepatoma/H22 Lymphoma/YAC-1 and EL-4 Insulinoma/INS-1 | BM mouse | No | p21 and Caspase-3↑ G0/G1 arrest | •Dose-dependent inhibition of MSCs on tumor cell growth ex vivo •Inhibiting hepatoma growth in vivo |
| Qiao et al.127 | Ex/In vivo | Hepatoma/H7402 and HepG2 | DT human | No | β-Catenin, Bcl-2, PCNA and survivin↓ | •Inhibiting hepatoma growth in vivo •Inducing apoptosis of H7402 cells ex vivo •Reducing proliferation of H7402 cells ex vivo •Altering the malignant phenotype of HepG2 cells ex vivo |
| Abd-Allah et al.128 | Ex/In vivo | Hepatoma/Hepa 1-6 | BM mouse | No | Caspase-3, p21 and p53↑ Bcl-2 and survivin↓ | •Inhibiting growth of Hepa 1–6 ex vivo •Reducing serum alanine transaminase (ALT), aspartate transaminase (AST) and albumin levels in vivo •Inducing dysplasia of hematoma in vivo |
| Abdel Aziz et al.132 | In vivo | Experimental hepatocellular carcinoma | BM rat | No | β-Catenin, PCNA, cyclin D and survivin↓ | •Reducing liver damage •Decreasing the serum ALT, AST and α-fetoprotein levels |
| Ahn et al.129 | Ex/In vivo | T-cell lymphoma/EL4 | Ad human | No | G0/G1 arrest | •Inducing apoptosis of EL4 cells ex vivo •Inhibiting lymphoma growth in vivo •Prolonging survival time of lymphoma bearing mice |
| Chien et al.130 | In vivo | Glioma/U87MG | BM human | No | Unknown | •Limiting the progression of glioma |
| Vegh et al.131 | In vivo | Mammary tumor | Placenta human | No | Unknown | •Inhibiting the growth of primary mammary tumor •Inhibiting the development of new tumors |
| Ma et al.133 | Ex/In vivo | Mammary tumor/MDA-MB-231 and MCF-7 | UC human | No | PI3K/Akt↓ G2/M arrest | •Decreasing proliferation of MDA-MB-231 and MCF-7 cells ex vivo •Inducing apoptosis of MDA-MB-231 and MCF-7 cells ex vivo •Inhibiting the growth of mammary tumor in vivo |
| Zhu et al.134 | Ex vivo | Leukemia/K562 and HL60 and Mammary tumor/MCF-7 | Ad/Human | No | G0/G1 arrest; β-catenin, c-Myc and Cyclin D2↓ p21CIP1 and p27KIP1↑ | •Inhibiting proliferation of tumor cells |
| Han et al.137 | Ex/In vivo | Prostate cancer/PC-3 | UC human | No | Cleaved caspase 3/9, PARP, JNK and Bax↑ PI3K/Akt, ERK↓Bcl-2, Bcl-xl, survivin Mcl-1 and clAP -1↓ | •Inducing apoptosis of PC-3 cells ex vivo •Inducing PC-3 cell-death in vivo |
| Xiang et al.138 | Ex/In vivo | Fibrosarcoma/Rif-1 | BM rat | Yes (iNOS) | Unknown | •Inhibiting Rif-1 tumor growth in vivo •Inducing apoptosis of Rif-1 cells ex vivo |
| Nakamura et al.139 | Ex/In vivo | Glioma/9 L | BM rat | Yes (IL-2) | Unknown | •Inhibiting proliferation of 9 L cells ex vivo •Inhibiting the growth of glioma in vivo •Prolonging the survival time of glioma bearing mice in vivo |
| Gao et al.140 | In vivo | Renal cell carcinoma (RCC) /786-0 | BM human | Yes (IL-12) | Unknown | •Reducing the growth of 786-0 RCC ex vivo •Prolonging the survival time of RCC bearing mice in vivo |
Abbreviations: Ad, adipose; BM, bone marrow; UC, umbilical cord; DT, dermal tissue.
In addition, MSC-based gene therapy for various solid tumors improves host anticancer responses through releasing the foreign gene-encoded proteins, such as iNOS, IL-2 and IL-12.138, 139, 140 Optimistically, some clinical trials for evaluating the specific potentials of MSCs on treating cancer and cancer regimen-related disorders are being carried out (ClinicalTrials.gov data). Relevant results will be referred for anticipating the potential risks related to MSC-based therapy.
Future Efforts into MSC-Based Therapy for RE Patients
Because of the success in treating Epinal patients by using MSCs, a new protocol for treating late severe damages of abdominal radiotherapy has been performed in Epinal Medical Center since 2013.141 Certainly, the ‘Epinal experiences' will deserve being referred worldwide in the future. If so, then MSC-based therapy is merely an attractive tool in managing RE patients. And clinical use of MSCs should focus on the following rules: (i) Ensuring the quality control of MSCs, including the processes for generating MSCs, identifying MSCs, detecting pathogens and endotoxin, and removing residual supplements.142 A detailed protocol for generating clinical grade human MSCs can be consulted,143 if using autologous MSCs. If using allogenic MSCs, then some FDA-approved products are available nowadays. But when allogenic MSCs are poorly tolerated, MSC exosomes are expected to become alternative candidates for managing RE. First, MSC exosomes show the potentials in mediating tissue regeneration because they contain a broad spectrum of bioactive substance.144 For example, the adenylate kinase and nucleoside-diphosphate kinase within exosomes are critical in increasing ATP production within injured cells.144 Additionally, CD73 molecules presenting in MSC exosomes are capable of hydrolyzing AMP into adenosine, an activator for cell survival by stimulating MAPK and PI3K/Akt signaling pathways.144 Moreover, MSC exosomes contain more than 200 immunomodulatory proteins, which confer the anti-inflammatory capability on exosomes.144 Second, the MSC exosomes seem to be stable in vitro, because their integrities and sizes were seldom affected by repeated freezing-thawing,145 allowing single extraction of exosomes for multiple administrations clinically. (ii) Formulating a protocol for MSC therapy for RE, including the delivery route of MSCs, timing and frequency of injection, the optimal dose and passage.146 (iii) Making countermeasure against possible complications or emergencies related to MSC infusion, such as fever, allergy or even shock.142, 147 (iv) Establishing the criteria for evaluating the effectiveness achieved by MSC infusion in RE resolution, which somewhat guarantees the researchers avoid overstating the positive outcomes.148, 149, 150
Conclusions
Overall, data from preclinical study and Epinal case report highlight the essentiality of futuristic use of MSCs in RE management. MSC-based therapy is expected to have beneficial effects on the quality of life of RE patients.
Acknowledgments
This study was funded by the National Natural Science Funds of China (Grant: 81372929).
Glossary
- CBC
crypt base columnar
- CGRP
calcitonin gene-related peptide
- DC
dendritic cell
- DSB
double-strand break
- ECM
extracellular matrix
- FI
fecal inconvenience
- GVHD
graft versus host disease
- HO-1
heme oxygenase-1
- IBD
inflammatory bowel disease
- LT
leukotriene
- RE
radiation enteropathy
- SLE
systemic lupus erythematosus
- TLR
toll-like receptor
- MMP
matrix metalloproteinase
- MPO
myeloperoxidase
- MSC
mesenchymal stem cell
- MSD
manganese superoxide dismutase
- NE
neutropenic enterocolitis
- NF-κB
nuclear factor-kappa B
- NOD-2
nucleotide-binding oligomerization domain-containing protein 2
- OAR
organ at risk
- TIMP
tissue inhibitor of metalloproteinase
- Treg
regulatory T cell
- vWF
von Willebrand factor
The authors declare no conflict of interest.
Footnotes
Edited by D Aberdam
References
- Hauer-Jensen M, Denham JW, Andreyev HJ. Radiation enteropathy-pathogenesis, treatment and prevention. Nat Rev Gastroenterol Hepatol. 2014;11:470–479. doi: 10.1038/nrgastro.2014.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker SL, Thames HD, Michalski JM, Bosch WR, Mohan R, Winter K, et al. Estimation of α/β for late rectal toxicity based on RTOG 94-06. Int J Radiat Oncol Biol Phys. 2011;81:600–605. doi: 10.1016/j.ijrobp.2010.11.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner DJ. Fractionation and late rectal toxicity. Int J Radiat Oncol Biol Phys. 2004;60:1013–1015. doi: 10.1016/j.ijrobp.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Kennedy GD, Heise CP. Radiation colitis and proctitis. Clin Colon Rectal Surg. 2007;20:64–72. doi: 10.1055/s-2007-970202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreyev HJ, Davidson SE, Gillespie C, Allum WH, Swarbrick E. Practice guidance on the management of acute gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61:179–192. doi: 10.1136/gutjnl-2011-300563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaple A, Francois S, Douay L, Benderitter M, Voswinkel J. New insights for pelvic radiation disease treatment: multipotent stromal cell is a promise mainstay treatment for the restoration of abdominopelvic severe chronic damages induced by radiotherapy. World J Stem Cells. 2013;5:106–111. doi: 10.4252/wjsc.v5.i4.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert JD, Byard RW. Fatal ischemic enteritis with hemorrhage-a late complication of treated Wilms tumor. J Forensic Sci. 2013;58:234–236. doi: 10.1111/j.1556-4029.2012.02264.x. [DOI] [PubMed] [Google Scholar]
- Sarin A, Safar B. Management of radiation proctitis. Gastroenterol Clin North Am. 2013;42:913–925. doi: 10.1016/j.gtc.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Spinelli A, Correale C, Szabo H, Montorsi M. Intestinal fibrosis in Crohn's disease: medical treatment or surgery. Curr Drug Targets. 2010;11:242–248. doi: 10.2174/138945010790309984. [DOI] [PubMed] [Google Scholar]
- Gothard L, Cornes P, Brooker S, Earl J, Glees J, Hall E, et al. Phase II study of vitamin E and pentoxifylline in patients with late side effects of pelvic radiotherapy. Radiother Oncol. 2005;75:334–341. doi: 10.1016/j.radonc.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Hamama S, Delanian S, Monceau V, Vozenin MC. Therapeutic management of intestinal firbosis induced by radiation therapy: from molecular profiling to new intervention strategies et vice et versa. Fibrogenesis Tissue Repair. 2012;5:S13. doi: 10.1186/1755-1536-5-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgier C, Haydont V, Milliat F, Francois A, Holler V, Lasser P, et al. Inhibition of Rho kinase modulates radiation induced fibrogenic phenotype in intestinal smooth muscle cells through alteration of the cytoskeleton and connective tissue growth factor expression. Gut. 2005;54:336–343. doi: 10.1136/gut.2004.051169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydont V, Bourgier C, Pocard M, Lusinchi A, Aigueperse J, Mathé D, et al. Pravastatin Inhibits the Rho/CCN2/extracellular matrix cascade in human fibrosis explants and improves radiation-induced intestinal firbosis in rats. Clin Cancer Res. 2007;13:5331–5340. doi: 10.1158/1078-0432.CCR-07-0625. [DOI] [PubMed] [Google Scholar]
- Wang J, Boerma M, Fu Q, Kulkarni A, Fink LM, Hauer-Jensen M. Simvastatin ameliorates radiation enteropathy development after localized, fractionated irradiation by a protein C-independent mechanism. Int J Radiat Oncol Biol Phys. 2007;68:1483–1490. doi: 10.1016/j.ijrobp.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002;418:41–49. doi: 10.1038/nature00870. [DOI] [PubMed] [Google Scholar]
- Park BS, Kim WS, Choi JS, Kim HK, Won JH, Ohkubo F, et al. Hair growth stimulated by conditioned medium of adipose-derived stem cells is enhanced by hypoxia: evidence of increased growth factor secretion. Biomed Res. 2010;31:27–34. doi: 10.2220/biomedres.31.27. [DOI] [PubMed] [Google Scholar]
- Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, Kobayashi N, et al. Mesenchymal stem cells: mechanisms of immunomodulation and homing. Cell Transplant. 2010;19:667–679. doi: 10.3727/096368910X508762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Saraiva L, Elkinton PT, Friedland JS. Regulation of matrix metalloproteinase-1,-3 and -9 in Mycobaterium tuberculosis-dependent respiratory networks by the rapamycin-sensitive PI3K/p70(S6K) cascade. FASEB J. 2014;28:85–93. doi: 10.1096/fj.13-235507. [DOI] [PubMed] [Google Scholar]
- Newell LF, Deans RJ, Maziarz RT. Adult adherent stromal cells in the management of graft-versus-host disease. Expert Opin Biol Ther. 2014;14:231–246. doi: 10.1517/14712598.2014.866648. [DOI] [PubMed] [Google Scholar]
- Wang D, Li J, Zhang Y, Zhang M, Chen J, Li X, et al. Umbilical cord mesenchymal stem cell transplantation in active and refractory systemic lupus erythematosus: a multicenter clinical study. Arthritis Res Ther. 2014;16:R79. doi: 10.1186/ar4520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh YG, Choi YJ. Intrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee. 2012;19:902–907. doi: 10.1016/j.knee.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Herreros MD, Garcia-Arranz M, Guadalajara H, De-La-Quintana P, Garcia-Olmo D, FATT Collaborative Group Autologous expanded adipose-derived stem cells for the treatment of complex cryptoglandular perianal fistulas: a phase III randomized clinical trial (FATT 1: fistula Advanced Therapy Trial 1) and long-term evaluation. Dis Colon Rectum. 2012;55:762–772. doi: 10.1097/DCR.0b013e318255364a. [DOI] [PubMed] [Google Scholar]
- Voswinkel J, Francois S, Simon JM, Benderitter M, Gorin NC, Mohty M, et al. Use of mesenchymal stem cells (MSCs) in chronic inflammatory fistulizing and fibrotic diseases: a comprehensive review. Clin Rev Allergy Immunol. 2013;45:180–192. doi: 10.1007/s12016-012-8347-6. [DOI] [PubMed] [Google Scholar]
- Langberg CW, Sauer T, Reitan JB, Hauer-Jensen M. Relationship between intestinal fibrosis and histopathologic and morphometric changes in consequential and late radiation enteropathy. Acta Oncol. 1996;35:81–87. doi: 10.3109/02841869609098484. [DOI] [PubMed] [Google Scholar]
- Latella G, Di Gregorio J, Flati V, Rieder F, Lawrence IC. Mechanisms of initiation and progression of intestinal fibrosis in IBD. Scand J Gastroenterol. 2015;50:53–65. doi: 10.3109/00365521.2014.968863. [DOI] [PubMed] [Google Scholar]
- Umar S. Intestinal stem cells. Curr Gastroenterol Rep. 2010;12:340–348. doi: 10.1007/s11894-010-0130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- van der Flier LG, Clevers H. Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annu Rev Physiol. 2009;71:241–260. doi: 10.1146/annurev.physiol.010908.163145. [DOI] [PubMed] [Google Scholar]
- Ishizuka S, Martin K, Booth C, Potten CS, de Murcia G, Bürkle A. Poly(ADP-ribose) polymerase-1 is a survival factor for radiation-exposed intestinal epithelial stem cells in vivo. Nucleic Acids Res. 2003;31:6198–6205. doi: 10.1093/nar/gkg840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Huang YF, Kek C, Bulavin DV. Apoptosis differently affects lineage tracing of Lgr5 and Bmi1 intestinal stem cell populations. Cell Stem Cell. 2013;12:298–303. doi: 10.1016/j.stem.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Frankenberg-Schwager M, Gebauer A, Koppe C, Wolf H, Pralle E, Frankenberg D. Single-strand annealing, conservative homologous recombination, nonhomologous DNA end joining, and the cell cycle-dependent repair of DNA double-strand breaks induced by sparsely or densely ionizing radiation. Radiat Res. 2009;171:265–273. doi: 10.1667/RR0784.1. [DOI] [PubMed] [Google Scholar]
- Schepers AG, Vries R, van den Born M, van de Wetering M, Clevers H. Lgr5 intestinal stem cells have high telomerase activity and randomly segregate their chromosomes. EMBO J. 2011;30:1104–1109. doi: 10.1038/emboj.2011.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalfe C, Kljavin NM, Ybarra R, de Sauvage FJ. Lgr5+ stem cells are indispensible for radiation-induced intestinal regeneration. Cell Stem Cell. 2014;14:149–159. doi: 10.1016/j.stem.2013.11.008. [DOI] [PubMed] [Google Scholar]
- Sangiorgi E, Capecchi MR. Bmi1 is expressed in vivo in intestinal stem cells. Nat Genet. 2008;40:915–920. doi: 10.1038/ng.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery RK, Carlone DL, Richmond CA, Farilla L, Kranendonk ME, Henderson DE, et al. Mouse telomerase reverse transcriptase (mTert) expression marks slowly cycling intestinal stem cells. Proc Natl Acad Sci USA. 2011;108:179–184. doi: 10.1073/pnas.1013004108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato T, van Es JH, Snippert HJ, Stange DE, Vries RG, van den Born M, et al. Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature. 2011;469:415–418. doi: 10.1038/nature09637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert S, Nivarhi H, Mayhew CN, Lo YH, Noah TK, Vallance J, et al. Activated STAT5 confers resistance to intestinal injury by increasing intestinal stem cell proliferation and regeneration. Stem Cell Reports. 2015;4:209–225. doi: 10.1016/j.stemcr.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungvari Z, Podlusky A, Sosnowska D, Tucsek Z, Toth P, Deak F, et al. Ionizing radiation promotes the acquisition of a senescence-associated secretory phenotype and impairs angiogenic capacity in cerebromicrovascular endothelial cells: role of increased DNA damage and decreased DNA repair capacity in microvascular radiosensitiivity. J Gerontol A Biol Sci Med Sci. 2013;68:1443–1457. doi: 10.1093/gerona/glt057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abderrahmani R, Francois A, Buard V, Tarlet G, Blirando K, Hneino M, et al. PAI-1-dependent endothelial cell death determines severity of radiation-induced intestinal injury. PLoS One. 2012;7:e35740. doi: 10.1371/journal.pone.0035740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paris F, Fuks Z, Kang A, Capodieci P, Juan G, Ehleiter D, et al. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science. 2001;293:293–297. doi: 10.1126/science.1060191. [DOI] [PubMed] [Google Scholar]
- Wynn TA. Integrating mechanisms of pulmonary fibrosis. J Exp Med. 2011;208:1339–1350. doi: 10.1084/jem.20110551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giblin JP, Hewlett LJ, Hannah MJ. Basal secretion of von Willebrand factor from human endothelial cells. Blood. 2008;112:957–964. doi: 10.1182/blood-2007-12-130740. [DOI] [PubMed] [Google Scholar]
- Kopaniak MM, Issekutz AC, Movat HZ. Kinetics of acute inflammation induced by E coli in rabbits. Quantitation of blood flow, enchanced vascular permeability, hemorrhage, and leukocyte accumulation. Am J Pathol. 1980;98:485–498. [PMC free article] [PubMed] [Google Scholar]
- Nikjoo H, O'Neill P, Terrissol M, Goodhead DT. Modelling of radiation-induced DNA damage: the early physical and chemical event. Int J Radiat Biol. 1994;66:453–457. doi: 10.1080/09553009414551451. [DOI] [PubMed] [Google Scholar]
- Hill S, Van Remmen H. Mitochondrial stress signaling in longevity: A new role for mitochondrial function in aging. Redox Biol. 2014;2:936–944. doi: 10.1016/j.redox.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martindale JL, Holbrook NJ. Cellular response to oxidative stress: signaling for suicide and survival. J Cell Physiol. 2002;192:1–15. doi: 10.1002/jcp.10119. [DOI] [PubMed] [Google Scholar]
- Almeida AS, Figueiredo-Pereira C, Vieira HL. Carbon monoxide and mitochondria-modulation of cell metabolism, redox response and cell death. Front Physiol. 2015;6:33. doi: 10.3389/fphys.2015.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal M, Siddigui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammatory and tissue injury. Antioxid Redox Signal. 2014;20:1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson LB, Riaz AA, Adawi D, Wittgren L, Bäck S, Thornberg C, et al. Radiation enteropathy and leucocyte-endothelial cell reactions in a refined small bowel model. BMC Surg. 2004;4:10. doi: 10.1186/1471-2482-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao RM, Yang L, Garcia-Cardena G, Luscinskas FW. Endothelial-dependent mechanisms of leukocyte recruitment to the vascular wall. Circ Res. 2007;101:234–247. doi: 10.1161/CIRCRESAHA.107.151860b. [DOI] [PubMed] [Google Scholar]
- Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13:159–175. doi: 10.1038/nri3399. [DOI] [PubMed] [Google Scholar]
- Reumaux D, de Boer M, Meijer AB, Duthilleul P, Roos D. Expression of myeloperoxidase (MPO) by neutrophils is necessary for their activation by anti-neutrophil cytoplasm autoantibodies (ANCA) against MPO. J Leukoc Biol. 2003;73:841–849. doi: 10.1189/jlb.1102567. [DOI] [PubMed] [Google Scholar]
- Wonderlich J, Shearer G, Livingstone A, Brooks A.Induction and measurement of cytotoxic T lymphocyte activity Curr Protoc Immunol 2006Chapter 3Unit 3.11. [DOI] [PubMed] [Google Scholar]
- Kugelberg E. Pattern recognition receptors: curbing gut inflammation. Nat Rev Immunol. 2014;14:583. doi: 10.1038/nri3735. [DOI] [PubMed] [Google Scholar]
- Wang J, Hauer-Jensen M. Neuroimmune interactions: potential target for mitigating or treating intestinal radiation injury. Br J Radiol. 2007;1:S41–S48. doi: 10.1259/bjr/33057885. [DOI] [PubMed] [Google Scholar]
- McLaughlin MM, Dacquisto MP, Jacobus DP, Horowitz RE. Effects of the germfree state on responses of mice to whole-body irradiation. Radiat Res. 1964;23:333–349. [PubMed] [Google Scholar]
- Ferreira MR, Muls A, Dearnaley DP, Andreyev HJ. Microbiota and radiation-induced bowel toxicity: lesions from inflammatory bowel disease for the oncologist. Lancet Oncol. 2014;15:e139–e147. doi: 10.1016/S1470-2045(13)70504-7. [DOI] [PubMed] [Google Scholar]
- Packey CD, Ciorba MA. Microbial influences on the small intestinal response to radiation injury. Curr Opin Gastroenterol. 2010;26:88–94. doi: 10.1097/MOG.0b013e3283361927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manichanh C, Varela E, Martinez C, Antolin M, Liopis M, Doré J, et al. The gut microbiota predispose to the pathophysiology of acute postradiotherapy diarrhea. Am J Gastroenterol. 2008;103:1754–1761. doi: 10.1111/j.1572-0241.2008.01868.x. [DOI] [PubMed] [Google Scholar]
- Crawford PA, Gordon JI. Microbial regulation of intestinal radiosensitivity. Proc Natl Acad Sci USA. 2005;102:13254–13259. doi: 10.1073/pnas.0504830102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Chanona E, Mühlbauer M, Jobin C. The microbiota protects against ischemia/reperfusion-induced intestinal injury through nucleotide-binding oligomerization domain-containing protein 2 (NOD2) signaling. Am J Pathol. 2014;184:2965–2975. doi: 10.1016/j.ajpath.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciorba MA, Stenson WF. Probiotic therapy in radiation-induced intestinal injury and repair. Ann NY Acad Sci. 2009;1165:190–194. doi: 10.1111/j.1749-6632.2009.04029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrance IC, Rogler G, Bamias G, Breynaert C, Florholmen J, Pellino G, et al. Cellular and molecular mediators of intestinal fibrosis J Crohns Colitis 2014. e-pub ahead of print 8 October 2014; doi: 10.1016/j.crohns.2014.09.008 [DOI] [PMC free article] [PubMed]
- Haydont V, Vozenin-Brotons MC. Maintenance of radiation-induced intestinal fibrosis: cellular and molecular features. World J Gastroenterol. 2007;13:2675–2683. doi: 10.3748/wjg.v13.i19.2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarnold J, Brotons MC. Pathogenetic mechanisms in radiation fibrosis. Radiother Oncol. 2010;97:149–161. doi: 10.1016/j.radonc.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Sémont A, Francois S, Mouiseddine M, Francois A, Saché A, Frick J, et al. Mesenchymal stem cells increase self-renewal of small intestinal epithelium and accelerate structural recovery after radiation injury. Adv Exp Med Biol. 2006;585:19–30. doi: 10.1007/978-0-387-34133-0_2. [DOI] [PubMed] [Google Scholar]
- Sémont A, Mouiseddine M, Francois A, Demarguay C, Mathieu N, Chapel A, et al. Mesenchymal stem cells improve small intestinal integrity though regulation of endogenous epithelial cell homeostasis. Cell Death Differ. 2010;17:952–961. doi: 10.1038/cdd.2009.187. [DOI] [PubMed] [Google Scholar]
- Kudo K, Liu Y, Takahashi K, Tarusawa K, Osanai M, Hu DL, et al. Transplantation of mesenchymal stem cells to prevent radiation-induced intestinal injury in mice. J Radiat Res. 2010;51:73–79. doi: 10.1269/jrr.09091. [DOI] [PubMed] [Google Scholar]
- Kudo K, Abe Y, Hu DL, Kijima H, Nakane A. Colonization and differentiation of transplanted embryonic stem cells in the irradiated intestine of mice. Tohoku J Exp Med. 2007;212:143–150. doi: 10.1620/tjem.212.143. [DOI] [PubMed] [Google Scholar]
- Saha S, Bhanja P, Kabarriti R, Liu L, Alfieri AA, Guha C. Bone marrow stromal cell transplantation mitigates radiation-induced gastrointestinal syndrome in mice. PLoS One. 2011;6:e24072. doi: 10.1371/journal.pone.0024072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francois M, Birman E, Forner KA, Gaboury L, Gallipeau J. Adoptive transfer of mesenchymal stromal cells accelerates intestinal epithelium recovery of irradiated mice in an interleukin-6-dependent manner. Cytotherapy. 2012;14:1164–1170. doi: 10.3109/14653249.2012.684378. [DOI] [PubMed] [Google Scholar]
- Gao Z, Zhang Q, Han Y, Cheng X, Lu Y, Fan L, et al. Mesenchymal stromal cell-conditioned medium prevents radiation-induced small intestine injury in mice. Cytotherapy. 2012;14:267–273. doi: 10.3109/14653249.2011.616194. [DOI] [PubMed] [Google Scholar]
- Chang P, Qu Y, Liu Y, Cui S, Zhu D, Wang H, et al. Multi-therapeutic effects of human adipose-derived mesenchymal stem cells on radiation-induced intestinal injury. Cell Death Dis. 2013;4:e685. doi: 10.1038/cddis.2013.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linard C, Busson E, Holler V, Strup-Perrot C, Lacave-Lapalun JV, Lhomme B, et al. Repeated autologous bone marrow-derived mesenchymal stem cell injections improve radiation-induced proctitis in pigs. Stem Cells Transl Med. 2013;2:916–927. doi: 10.5966/sctm.2013-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessout R, Sémont A, Demarguay C, Charcosset A, Benderitter M, Mathieu N. Mesenchymal stem cell therapy induces glucocorticoid synthesis in colonic mucosa and suppresses radiation-activated T cells: new insights into MSC immunomodulation. Mucosal Immunol. 2014;7:656–669. doi: 10.1038/mi.2013.85. [DOI] [PubMed] [Google Scholar]
- Zong ZW, Cheng TM, Su YP, Ran XZ, Shen Y, Li N, et al. Recruitment of transplanted dermal multipotent stem cells to sites of injury in rats with combined radiation and wound injury by interaction of SDF-1 and CXCR4. Radiat Res. 2008;170:444–450. doi: 10.1667/rr0744.1. [DOI] [PubMed] [Google Scholar]
- Ji JF, He BP, Dheen ST, Tay SS. Interactions of chemokines and chemokine receptors mediate the migration of mesenchymal stem cells to the impaired site in the brain after hypoglossal never injury. Stem Cells. 2004;22:415–427. doi: 10.1634/stemcells.22-3-415. [DOI] [PubMed] [Google Scholar]
- Francois S, Bensidhoum M, Moureseddine M, Mazurier C, Allenet B, Sémont A, et al. Local irradiation not only induces homing of human mesenchymal stem cells at exposed sites but promotes their widespread engraftment to multiple organs: a study of their quantitative distribution after irradiation damage. Stem Cells. 2006;24:1020–1029. doi: 10.1634/stemcells.2005-0260. [DOI] [PubMed] [Google Scholar]
- Zhang J, Gong JF, Zhang W, Zhu WM, Li JS. Effects of transplated bone marrow mesenchymal stem cells on the irradiated intestine of mice. J Biomed Sci. 2008;15:585–594. doi: 10.1007/s11373-008-9256-9. [DOI] [PubMed] [Google Scholar]
- Yang C, Chen HX, Zhou Y, Liu MX, Wang JX, Ren SP, et al. Manganese superoxide dismutase gene therapy protects against irradiation-induced intestinal injury. Curr Gene Ther. 2013;13:305–314. doi: 10.2174/15665232113136660027. [DOI] [PubMed] [Google Scholar]
- Hu J, Yang Z, Wang J, Tang Y, Liu H, Zhang B, et al. Infusion of Trx-1-overexpressing huc MSC prolongs the survival of acutely irradiated NOD/SCID mice by decreasing excessive inflammatory injury. PLoS One. 2013;8:e78227. doi: 10.1371/journal.pone.0078227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zangi L, Margalit R, Reich-Zeliger S, Bachar-Lustig E, Beilhack A, Negrin R, et al. Direct imaging of immune rejection and memory induction by allogeneic mesenchymal stromal cells. Stem Cells. 2009;27:2865–2874. doi: 10.1002/stem.217. [DOI] [PubMed] [Google Scholar]
- Hu C, Yong X, Li C, Lü M, Liu D, Chen L, et al. CXCL12/CXCR4 axis promotes mesenchymal stem cell mobilization to burn wounds and contributes to wound repair. J Surg Res. 2013;183:427–434. doi: 10.1016/j.jss.2013.01.019. [DOI] [PubMed] [Google Scholar]
- Ren G, Zhao X, Zhang L, Zhang J, L'Huillier A, Ling W, et al. Inflammatory cytokine-induced intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 in mesenchymal stem cells are critical for immunosuppression. J Immunol. 2010;184:2321–2328. doi: 10.4049/jimmunol.0902023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringe J, Strassburg S, Neumann K, Endres M, Notter M, Burmester GR, et al. Towards in situ tissue repair: human mesenchymal stem cells express chemokine receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with CXCL8 but not CCL2. J Cell Biochem. 2007;101:135–146. doi: 10.1002/jcb.21172. [DOI] [PubMed] [Google Scholar]
- Paguet-Fifield S, Schlüter H, Li A, Aitken T, Gangatirkar P, Blashki D, et al. A role for pericytes as microenvironmental regulators of human skin tissue regeneration. J Clin Invest. 2009;119:2795–2806. doi: 10.1172/JCI38535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linero I, Chaparro O. Paracrine effect of mesenchymal stem cells from human adipose tissue in bone regeneration. PLoS One. 2014;9:e107001. doi: 10.1371/journal.pone.0107001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–1822. doi: 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- Maggini J, Mirkin G, Bognanni I, Holmberg J, Piazzón IM, Nepomnaschy I, et al. Mouse bone marrow-derived mesenchymal stromal cells turn activated macrophages into a regulatory-like profile. PLoS One. 2010;5:e9252. doi: 10.1371/journal.pone.0009252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Németh K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15:42–49. doi: 10.1038/nm.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pils MC, Pisano F, Fasnacht N, Heinrich JM, Groebe L, Schippers A, et al. Monocytes/macrophages and/or neutrophils are the target of IL-10 in the LPS endotoxemia model. Eur J Immunol. 2010;40:443–448. doi: 10.1002/eji.200939592. [DOI] [PubMed] [Google Scholar]
- Spaggiari GM, Abdelrazik H, Becchetti F, Moretta L. MSCs inhibit monocyte-derived DC maturation and function by selectively interfering with the generation of immature DCs: central role of MSC-derived prostaglandin E2. Blood. 2009;113:6576–6583. doi: 10.1182/blood-2009-02-203943. [DOI] [PubMed] [Google Scholar]
- Spaggiari GM, Capobianco A, Abdelrazik H, Becchetti F, Mingari MC, Moretta L. Mesenchymal stem cells inhibit natural killer-cell proliferation, cytotoxicity, and cytokine production: role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood. 2008;111:1327–1333. doi: 10.1182/blood-2007-02-074997. [DOI] [PubMed] [Google Scholar]
- Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, Borg C, et al. Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4+CD25highFOXP3+ regulatory T cells. Stem Cells. 2008;26:212–222. doi: 10.1634/stemcells.2007-0554. [DOI] [PubMed] [Google Scholar]
- Hsu WT, Lin CH, Chiang BL, Jui HY, Wu KK, Lee CM. Prostaglandin E2 potentiates mesenchymal stem cell-induced IL-10+IFN-γ+CD4+ regulatory T cells to control transplant arteriosclerosis. J Immunol. 2013;190:2372–2380. doi: 10.4049/jimmunol.1202996. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Rey E, Anderson P, González MA, Rico L, Büscher D, Delgado M. Human adult stem cells derived from adipose tissue protect against experimental colitis and sepsis. Gut. 2009;58:929–939. doi: 10.1136/gut.2008.168534. [DOI] [PubMed] [Google Scholar]
- Parekkadan B, Upadhyay R, Dunham J, Iwamoto Y, Mizoguchi E, Mizoguchi A, et al. Bone marrow stromal cell transplants prevent experimental enterocolitis and require host CD11b+ splenocytes. Gastroenterology. 2011;140:966–975. doi: 10.1053/j.gastro.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JM, Nemeth K, Kushnir-Sukhov NM, Metcalfe DD, Mezey E. Bone marrow stromal cells inhibit mast cell function via a COX2-dependent mechanism. Clin Exp Allergy. 2011;41:526–534. doi: 10.1111/j.1365-2222.2010.03685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Yun JW, Shin TH, Lee SH, Lee BC, Yu KR. Human umbilical cord blood mesenchymal stem cell-derived PGE2 and TGF-β1 Alleviate atopic dermatitis by reducing mast cell degranulation. Stem Cells. 2015;33:1254–1266. doi: 10.1002/stem.1913. [DOI] [PubMed] [Google Scholar]
- Lombard E, van der Poll T, DelaRosa O, Dalemans W. Mesenchymal stem cells as a therapeutic tool to treat sepsis. World J Stem Cells. 2015;7:368–379. doi: 10.4252/wjsc.v7.i2.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel R, Brockers S, Heseler K, Degistirici O, Bülle H, Woite C, et al. Human but not murine multipotent mesenchymal stromal cells exhibit broad-spectrum antimicrobial effector function mediated by indoleamine 2,3-dioxygenase. Leukemia. 2011;25:648–654. doi: 10.1038/leu.2010.310. [DOI] [PubMed] [Google Scholar]
- Krasnodembskaya A, Samarani G, Song Y, Zhou H, Su X, Lee JW, et al. Human mesenchymal stem cells reduce mortality and bacteremia in gram-negative sepsis in mice in part by enhancing the phagocytic activity of blood monocytes. Am J Physiol Lung Cell Mol Physiol. 2012;302:L1003–L1013. doi: 10.1152/ajplung.00180.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasnodembskaya A, Song Y, Fang X, Gupta N, Serikov V, Lee JW, et al. Antibacterial effect of human mesenchymal stem cells is mediated in part from secretion of the antimicrobial peptide LL-37. Stem Cells. 2010;28:2229–2238. doi: 10.1002/stem.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang W, Song BW, Moon JY, Cha MJ, Ham O, Lee SY, et al. Anti-death strategies against oxidative stress in grafted mesenchymal stem cells. Histol Histopathol. 2013;28:1529–1536. doi: 10.14670/HH-28.1529. [DOI] [PubMed] [Google Scholar]
- Lange C, Brunswig-Spickenheier B, Cappallo-Obermann H, Eggert K, Gehling UM, Rudolph C, et al. Radiation rescue: mesenchymal stromal cells protect from lethal irradiation. PLoS One. 2011;6:e14486. doi: 10.1371/journal.pone.0014486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brittan M, Chance V, Elia G, Poulsom R, Alison MR, MacDonald TT, et al. A regenerative role for bone marrow following experimental colitis: contribution to neovasculogenesis and myofibroblasts. Gastroenterology. 2005;128:1984–1995. doi: 10.1053/j.gastro.2005.03.028. [DOI] [PubMed] [Google Scholar]
- Okamoto R, Yajima T, Yamazaki M, Kanai T, Mukai M, Okamoto S, et al. Damaged epithelial regenerated by bone marrow-derived cells in the human gastrointestinal tract. Nat Med. 2002;8:1011–1017. doi: 10.1038/nm755. [DOI] [PubMed] [Google Scholar]
- Guan A, Gong H, Ye Y, Jia J, Zhang G, Li B, et al. Regulation of p53 by jagged 1 contributes to angiotensin II-induced impairment of myocardial angiogenesis. PLoS One. 2013;8:e76529. doi: 10.1371/journal.pone.0076529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demidov ON, Timofeev O, Lwin HN, Kek C, Appella E, Bulavin DV. Wip1 phosphatase regulates p53-dependent apoptosis of stem cells and tumorigenesis in the mouse intestine. Cell Stem Cell. 2007;1:180–190. doi: 10.1016/j.stem.2007.05.020. [DOI] [PubMed] [Google Scholar]
- John S. Mesenchymal stem cells in cancer. Stem Cell Rev. 2008;4:119–124. doi: 10.1007/s12015-008-9030-4. [DOI] [PubMed] [Google Scholar]
- Kuhn NZ, Tuan RS. Regulation of stemness and stem cell niche of mesenchymal stem cells: implications in tumorigenesis and metastasis. J Cell Physiol. 2010;222:268–277. doi: 10.1002/jcp.21940. [DOI] [PubMed] [Google Scholar]
- Han Z, Jing Y, Zhang S, Liu Y, Shi Y, Wei L. The role of immunesuppression of mesenchymal stem cells in tissue repair and tumor growth. Cell Biosci. 2012;2:8. doi: 10.1186/2045-3701-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røsland GV, Svendsen A, Torsvik A, Sobala E, Mc Cormack E, Immervoll H, et al. Long-term cultures of bone marrow-derived human mesenchymal stem cells frequently undergo spontaneous malignant transformation. Cancer Res. 2009;69:5331–5339. doi: 10.1158/0008-5472.CAN-08-4630. [DOI] [PubMed] [Google Scholar]
- Burns JS, Abdallah BM, Guldberg P, Rygaard J, Schrøder HD, Kassem M. Tumorigenic heterogeneity in cancer stem cells evolved from long-term cultures of telomerase-immortalized human mesenchymal stem cells. Cancer Res. 2005;65:3126–3135. doi: 10.1158/0008-5472.CAN-04-2218. [DOI] [PubMed] [Google Scholar]
- Rubio D, Garcia-Castro J, Martín MC, de la Fuente R, Cigudosa JC, Lloyd AC, et al. Spontaneous human adult stem cell transformation. Cancer Res. 2005;65:3035–3039. doi: 10.1158/0008-5472.CAN-04-4194. [DOI] [PubMed] [Google Scholar]
- Li H, Fan X, Kovi RC, Jo Y, Moguin B, Konz R, et al. Spontaneous expression of embryonic factors and p53 point mutations in aged mesenchymal stem cells: a model of age-related tumorigenesis in mice. Cancer Res. 2007;67:10889–10898. doi: 10.1158/0008-5472.CAN-07-2665. [DOI] [PubMed] [Google Scholar]
- Rodriguez R, Rubio R, Masip M, Catalina P, Nieto A, de la Cueva T, et al. Loss of p53 induces tumorigenesis in p21-deficient mesenchymal stem cells. Neoplasia. 2009;11:397–407. doi: 10.1593/neo.81620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo ME, Zaffaroni N, Novara F, Cometa AM, Avanzini MA, Moretta A, et al. Human bone marrow derived mesenchymal stem cells do not undergo transformation after long-term in vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res. 2007;67:9142–9149. doi: 10.1158/0008-5472.CAN-06-4690. [DOI] [PubMed] [Google Scholar]
- Choumerianou DM, Dimitriou H, Perdikogianni C, Martimianaki G, Riminucci M, Kalmanti M. Study of oncogenic transformation in ex vivo expanded mesenchymal cells, from paediatric bone marrow. Cell Prolif. 2008;41:909–922. doi: 10.1111/j.1365-2184.2008.00559.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerlin L, Park TS, Zambidis ET, Donnenberg VS, Donnenberg AD. Mesenchymal stem cell secretome and regenerative therapy after cancer. Biochimie. 2013;95:2235–2245. doi: 10.1016/j.biochi.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khakoo AY, Pati S, Anderson SA, Reid W, Elshal MF, Rovira II, et al. Human mesenchymal stem cells exert potent antitumorigenic effects in a model of Kaposi's sarcoma. J Exp Med. 2006;203:1235–1247. doi: 10.1084/jem.20051921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Ling W, Pennisi A, Wang Y, Khan S, Heidaran M, et al. Human placenta-derived adherent cells prevent bone loss, stimulate bone formation, and suppress growth of multiple myeloma in bone. Stem Cells. 2011;29:263–273. doi: 10.1002/stem.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn JO, Coh YR, Lee HW, Shin IS, Kang SK, Youn HY. Human adipose tissue-derived mesenchymal stem cells inhibit melanoma growth in vitro and in vivo. Anticancer Res. 2015;35:159–168. [PubMed] [Google Scholar]
- Nasuno M, Arimura Y, Nagaishi K, Isshiki H, Onodera K, Nakagaki S, et al. Mesenchymal stem cells cancel azoxymethane-induced tumor initiation. Stem Cells. 2014;32:913–925. doi: 10.1002/stem.1594. [DOI] [PubMed] [Google Scholar]
- Katsuno T, Ochi M, Tominaga K, Tanaka F, Sogawa M, Tanigawa T, et al. Mesenchymal stem cells administrated in the early phase of tumorigenesis inhibit colorectal tumor development in rats. J Clin Biochem Nutr. 2013;53:170–175. doi: 10.3164/jcbn.13-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu YR, Yuan Y, Wang XJ, Wei LL, Chen YN, Cong C, et al. The growth inhibitory effect of mesenchymal stem cells on tumor cells in vitro and in vivo. Cancer Biol Ther. 2008;7:245–251. doi: 10.4161/cbt.7.2.5296. [DOI] [PubMed] [Google Scholar]
- Qiao L, Xu Z, Zhao T, Zhao Z, Shi M, Zhao RC, et al. Suppression of tumorigenesis by human mesenchymal stem cells in a hepatoma model. Cell Res. 2008;18:500–507. doi: 10.1038/cr.2008.40. [DOI] [PubMed] [Google Scholar]
- Abd-Allah SH, Shalaby SM, El-Shai AS, Elkader EA, Hussein S, Emam E, et al. Effect of bone marrow-derived mesenchymal stromal cells on hepatoma. Cytotherapy. 2014;16:1197–1206. doi: 10.1016/j.jcyt.2014.05.006. [DOI] [PubMed] [Google Scholar]
- Ahn JO, Chae JS, Coh YR, Jung WS, Lee HW, Shin IS, et al. Human adipose tissue-derived mesenchymal stem cells inhibit T-cell lymphoma growth in vitro and in vivo. Anticancer Res. 2014;34:4839–4847. [PubMed] [Google Scholar]
- Chien LY, Hsiao JK, Hsu SC, Yao M, Lu CW, Liu HM, et al. In vivo magnetic resonance imaging of cell tropism, trafficking mechanism, and therapeutic impact of human mesenchymal stem cells in a murine glioma model. Biomaterials. 2011;32:3275–3284. doi: 10.1016/j.biomaterials.2011.01.042. [DOI] [PubMed] [Google Scholar]
- Vegh I, Grau M, Gracia M, Grande J, de la Torre P, Flores AI. Decidua mesenchymal stem cells migrated toward mammary tumors in vitro and in vivo affecting tumor growth and tumor development. Cancer Gene Ther. 2013;20:8–16. doi: 10.1038/cgt.2012.71. [DOI] [PubMed] [Google Scholar]
- Abdel aziz MT, EI Asmar MF, Atta HM, Mahfouz S, Fouad HH, Roshdy NK, et al. Efficacy of mesenchymal stem cells in suppression of hepatocarcinorigenesis in rats: possible role of Wnt signaling. J Exp Clin Cancer Res. 2011;30:49. doi: 10.1186/1756-9966-30-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Hao X, Zhang S, Zhang J. The in vitro and in vivo effects of human umbilical cord mesenchymal stem cells on the growth of breast cancer cells. Breast Cancer Res Treat. 2012;133:473–485. doi: 10.1007/s10549-011-1774-x. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Sun Z, Han Q, Liao L, Wang J, Bian C, et al. Human mesenchymal stem cells inhibit cancer cell proliferation by secreting DKK-1. Leukemia. 2009;23:925–933. doi: 10.1038/leu.2008.384. [DOI] [PubMed] [Google Scholar]
- Lee RH, Kim B, Choi I, Kim H, Choi HS, Suh K, et al. Characterization and expression analysis of mesenchymal stem cells from human bone marrow and adipose tissue. Cell Physiol Biochem. 2004;14:311–324. doi: 10.1159/000080341. [DOI] [PubMed] [Google Scholar]
- Fodde R, Brabletz T. Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr Opin Cell Biol. 2007;19:150–158. doi: 10.1016/j.ceb.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Han I, Yun M, Kim EO, Kim B, Jung MH, Kim SH. Umbilical cord tissue-derived mesenchymal stem cells induce aoptosis in PC-3 prostate cancer cells through activation of JNK and downregulation of PI3K/Akt signaling. Stem Cell Res Ther. 2014;5:54. doi: 10.1186/scrt443. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Xiang J, Tang J, Song C, Yang Z, Hirst DG, Zheng QJ, et al. Mesenchymal stem cells as a gene therapy carrier for treatment of fibrosarcoma. Cytotherapy. 2009;11:516–526. doi: 10.1080/14653240902960429. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Ito Y, Kawano Y, Kurozumi K, Kobune M, Tsuda H, et al. Antitumor effect of genetically engineered mesenchymal stem cells in a rat glioma model. Gene Ther. 2004;11:1155–1164. doi: 10.1038/sj.gt.3302276. [DOI] [PubMed] [Google Scholar]
- Gao P, Ding Q, Wu Z, Jiang H, Fang Z. Therapeutic potential of human mesenchymal stem cells producing IL-12 in a mouse xenograft model of renal cell carcinoma. Cancer Lett. 2010;290:157–166. doi: 10.1016/j.canlet.2009.08.031. [DOI] [PubMed] [Google Scholar]
- Chapel A, Francois S, Douay L, Benderitter M, Voswinkel J. Fifteen years of preclinical and clinical experiences about biotherapy treatment of lesions induced by accidental irradiation and radiotherapy. World J Stem Cells. 2013;5:68–72. doi: 10.4252/wjsc.v5.i3.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo ME, Fibbe WE. Safety and efficacy of mesenchymal stromal cell therapy in autoimmune disorders. Ann NY Acad Sci. 2012;1266:107–117. doi: 10.1111/j.1749-6632.2012.06667.x. [DOI] [PubMed] [Google Scholar]
- Robey PG, Kuznetsov SA, Ren J, Klein HG, Sabatino M, Stroncek DF. Generation of clinical grade human bone marrow stromal cells for use in bone regeneration. Bone. 2015;70:87–92. doi: 10.1016/j.bone.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai RC, Yeo RW, Lim SK. Mesenchymal stem cell exosomes. Semin Cell Dev Biol. 2015;40:82–88. doi: 10.1016/j.semcdb.2015.03.001. [DOI] [PubMed] [Google Scholar]
- Sokolova V, Ludwig AK, Hornung S, Rotan O, Horn PA, Epple M, et al. Characterisation of exosomes derived from human cells by nanoparticle tracking analysis and scanning electron microscopy. Colloids Surf B Biointerfaces. 2011;87:146–150. doi: 10.1016/j.colsurfb.2011.05.013. [DOI] [PubMed] [Google Scholar]
- Berardis S, Dwisthi Sattwika P, Najimi M, Sokal EM. Use of mesenchymal stem cells to treat liver fibrosis: Current situation and future prospects. World J Gastroenterol. 2015;21:742–758. doi: 10.3748/wjg.v21.i3.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmori K, Masuda K, DeBoer DJ, Sakaguchi M, Tsujimoto H. Immunoblot analysis for IgE-reactive components of fetal calf serum in dogs that developed allergic reactions after non-rabies vaccination. Vet Immunol Immunopathol. 2007;115:166–171. doi: 10.1016/j.vetimm.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbott A. Leaked files slam stem-cell therapy. Nature. 2014;505:139–140. doi: 10.1038/505139a. [DOI] [PubMed] [Google Scholar]
- Salem HK, Thiemermann C. Mesenchymal stromal cells: current understanding and clinical status. Stem Cells. 2010;28:585–596. doi: 10.1002/stem.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lodi D, Iannitti T, Palmieri B. Stem cells in clinical practice: applications and warnings. J Exp Clin Cancer Res. 2011;30:9. doi: 10.1186/1756-9966-30-9. [DOI] [PMC free article] [PubMed] [Google Scholar]