Abstract
Aim:
The aim was to determine the difficulties faced by family physicians, and compare how satisfied those working with the Ministry of Health (MOH) are with their counterparts who work at some selected non-MOH hospitals.
Methods:
An analytical, cross-sectional study was conducted at King Abdulaziz University Hospital, King Faisal Specialist Hospital and Research Center (KFSH and RC), and 40 MOH primary health care centers across Jeddah. A structured multi-item questionnaire was used to collect demographic data and information on the difficulties family physicians face. The physicians’ level of satisfaction and how it was affected by the difficulties was assessed.
Results:
Women constituted 71.9% of the sample. Problems with transportation formed one of the main difficulties encountered by physicians. Compared to non-MOH physician, a significantly higher proportion of MOH physicians reported unavailability of radiology technicians (P = 0.011) and radiologists (P < 0.001), absence of the internet and computer access (P < 0.001), unavailability of laboratory services (P = 0.004), reagents (P = 0.001), X-ray equipment (P = 0.027), ultrasound equipment (P < 0.001), an electronic medical records system (P < 0.001), insufficient laboratory tests (P = 0.0001), and poor building maintenance (P < 0.001). Family physicians with the MOH were less satisfied with their jobs compared with non-MOH physicians (P = 0.032).
Conclusion:
MOH family physicians encountered difficulties relating to staff, services, and infrastructure, which consequently affected their level of satisfaction.
Keywords: Family medicine, family physicians, Ministry of Health, difficulties, primary health care
INTRODUCTION
Family medicine is the cornerstone of the health care system[1] because family physicians screen everyone seeking help, regardless of age, gender, or disease.[2,3] However, these physicians face several difficulties and problems that decrease their job satisfaction and hamper the delivery of medical services. This in turn lowers patient satisfaction and increases the turnover of staff at primary health care (PHC) centers. By overcoming the obstacles in PHC systems, the level of job satisfaction among family physicians will rise, eventually leading to improved quality of health care services and the health care system as a whole.
In the Arab world, several problems hinder the development of family medicine. Until the beginning of the twenty first century, one of the problems faced by family physicians in Arab nations was the absence of adequately equipped PHC centers, some of which were old houses converted into clinics.[4] However, secondary and tertiary care hospitals were well constructed and furnished. Another problem was inadequate financial support for primary care and family physicians. These factors together resulted in lower job satisfaction among PHC family physicians compared to doctors who worked in secondary and tertiary care hospitals.[4]
In Saudi Arabia, PHC centers also face many obstacles that affect the quality of services provided to the community. These include a deficiency of diagnostic tests, drugs, shortage of diagnostic facilities and staff, as well as lack of adequate resources and inability to access scientific journals through the internet or libraries.[5,6] These obstacles cause stress and dissatisfaction among family physicians and can consequently affect their creativity, commitment, and the quality of care they provide to patients.[7] Unfortunately, these studies only describe the difficulties faced by PHC physicians and/or nurses and do not consider the difficulties faced by family physicians working in other health sectors.
The objectives of this study were to determine the difficulties faced by family physicians working with the Ministry of Health (MOH) and how these relate to their satisfaction in comparison with the level of satisfaction of their counterparts at non-MOH hospitals.
METHODS
This analytical, cross-sectional study was done between December 2012 and February 2013 on family physicians at two non-MOH hospitals (King Abdulaziz University Hospital [KAUH] and King Faisal Specialist Hospital and Research Center [KFSH and RC]) and 40 PHC centers in Jeddah.
The sample included all family physicians at PHC centers in Jeddah, Saudi Arabia or non-MOH institutions, namely KAUH or KFSH and RC who were available during the data collection period. Physicians were invited to participate in this survey by phone calls or E-mails. The study questionnaire was uploaded and the survey link sent to the E-mail addresses of those physicians who accepted the invitation to participate. In some cases, we visited physicians at their offices to complete the questionnaire using the iPad.
The questionnaire, based on extensive literature review and discussion with some family physicians, was constructed by two epidemiologist family physicians. It was reviewed by two expert family physicians who evaluated the questionnaire for meaning, flow, and clarity of instructions, and modified as necessary
We used a fully-structured multi-item questionnaire that comprised three parts. The first part comprised questions on basic demographic and professional data, including age, gender, marital status, nationality, and education. The second part had questions that assessed the difficulties faced by family physicians because of deficiencies in the health facility, and had only “Yes” or “No” answer options. The third part used Likert scale to determine the level of satisfaction of family physicians and how it was affected by the difficulties they encountered in their practice.
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 20 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were computed for all variables. The Chi-square test was used to establish the relationship between categorical variables, while the independent t-test was used to check differences between group means if normality was assumed. Otherwise, Welch's t-test was used. Pearson's correlation coefficient was utilized to test the correlation between variables. Significance was set at P < 0.05.
A scoring system was used to assess the level of satisfaction of the physicians. We used an additive method to calculate the overall scored responses, which included the percentage of physicians who were satisfied with a particular factor, based on listed criteria that belonged to each domain.
Internal consistency was used to validate and verify the reliability of the participants’ responses. We asked correlated questions, such as “Do you have problems with biomedical services?” and “How satisfied are you with biomedical services?” Cross tabulation was performed to test the reliability of the responses, which was 94.4%.
Agreement to fill the questionnaire was taken as consent. Collected information was kept confidential and used only for the purpose of this research. The study was approved by the ethics committees of KAUH, KFSH and RC, and the Directorate of Health Affairs in Jeddah.
RESULTS
One hundred and three questionnaires were either distributed or forwarded via E-mail: 77 and 26 questionnaires were sent to MOH and non-MOH physicians, respectively. Seventy MOH (91%) and 25 non-MOH (96.2%) physicians participated in the survey, representing an overall response rate of 92.2%.
The mean (SD) age of the physicians was 39.8 (7.3) years (range, 24–57 years; median, 40 years). Females constituted more than half of the sample, giving a female:male ratio of 2.6:1 [Table 1]. Most physicians earned >30,000 Saudi Riyals (SR); however, a larger proportion of family physicians in the non-MOH sector earned higher salaries than MOH family physicians [P = 0.039; Figure 1].
Table 1.
Demographic characteristics of the physicians (n=95)
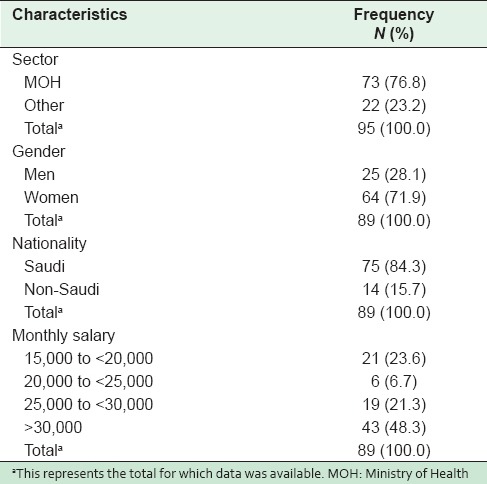
Figure 1.
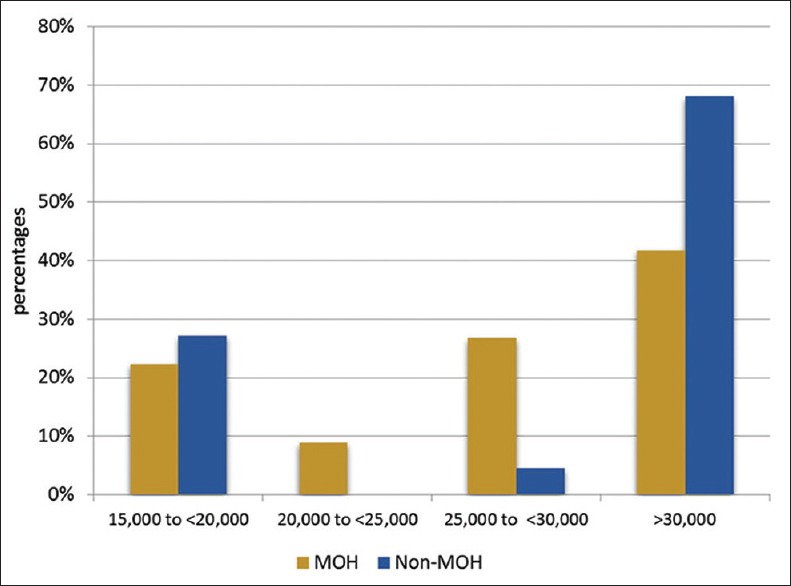
Salary comparison between Ministry of Health and non-Ministry of Health family physicians
The mean length of service in our sample was 10.5 ± 6.6 years (range, 1.0–25.0 years; median, 9.5). Physicians had on average 5.8 ± 2.8 clinics/week (range, 2–10; median, 5) and saw about 22.3 ± 10.7 patients/day (range, 3–55; median, 20 patients/day).
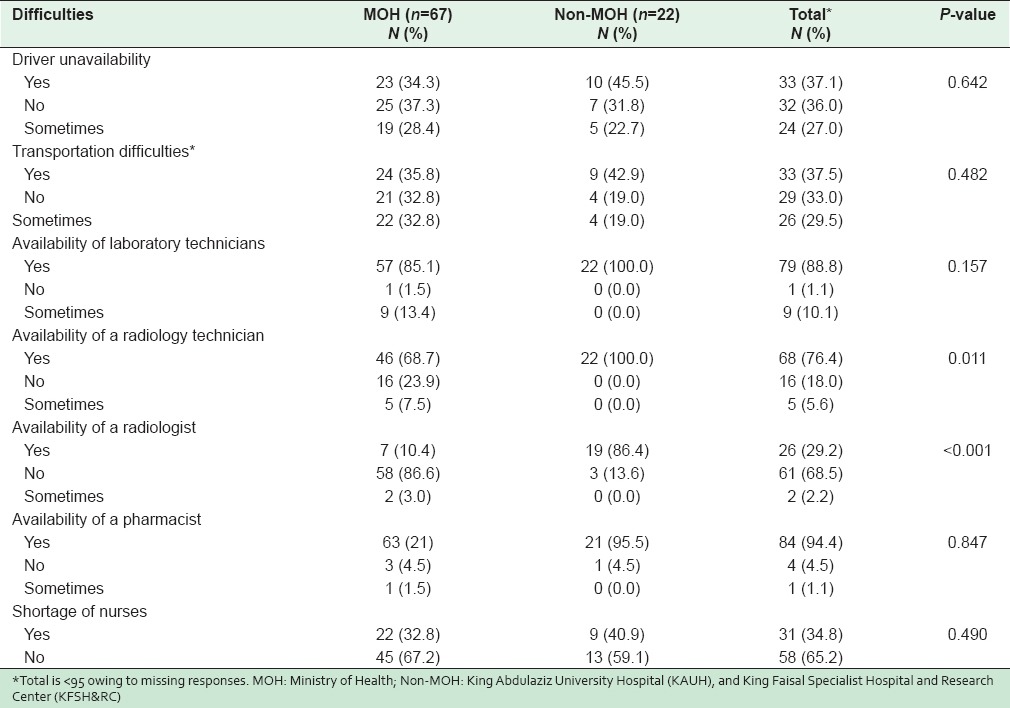
As shown in Table 2, MOH family physicians were more likely to report a lack of laboratory technicians (P = 0.157), unavailability of radiology technicians (P = 0.011) and radiologists (P < 0.001), and shortage of nurses (P = 0.490).
Table 2.
Difficulties related to transportation and staff
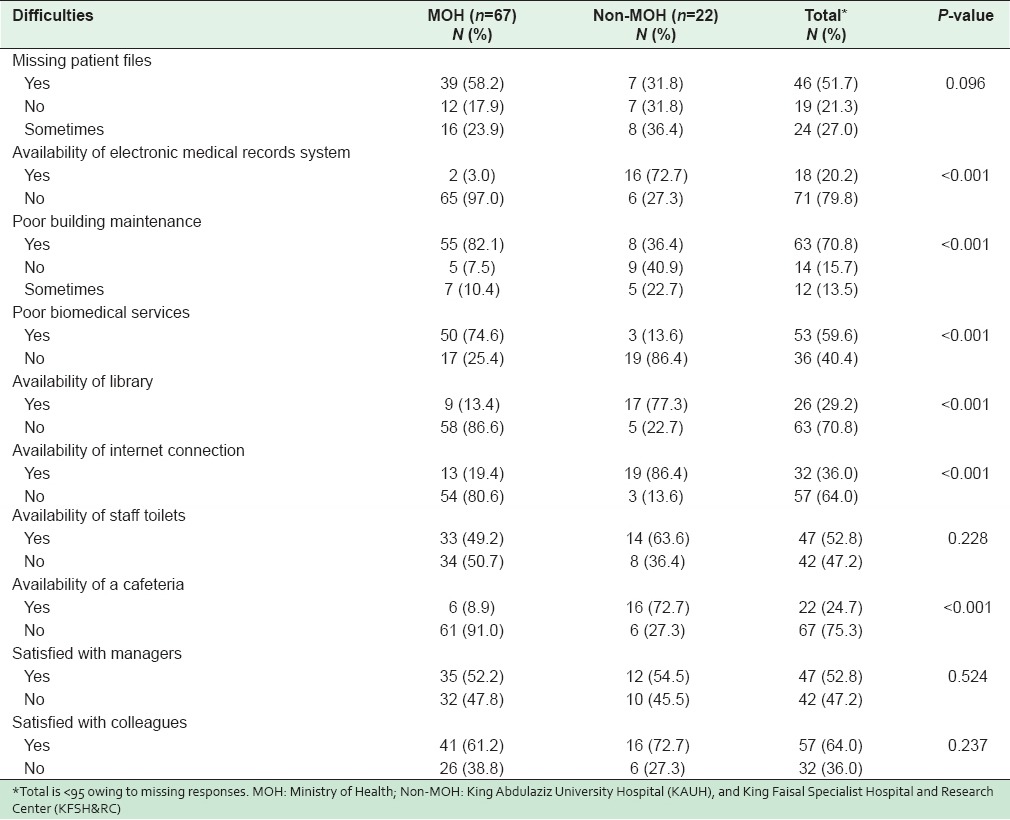
Difficulty with transportation was cited as one of the main obstacles encountered by physicians; four MOH and two non-MOH family physicians reported using taxis to get to work. Lack of an electronic medical records system (P < 0.001) and the lack of internet and computer access (P < 0.001) were great sources of dissatisfaction among MOH physicians. More MOH family physicians reported the loss of papers from patients’ medical records than did non-MOH family physicians (P = 0.096) [Table 3]. Regarding the work environment, only 34.4% of MOH physicians felt safe at the work place as against 76.9% of non-MOH physicians (P = 0.012). In addition, a significant proportion of MOH family physicians reported the unavailability of a cafeteria (P < 0.001) and poor building maintenance (P < 0.001).
Table 3.
Difficulties related to infrastructure and work environment
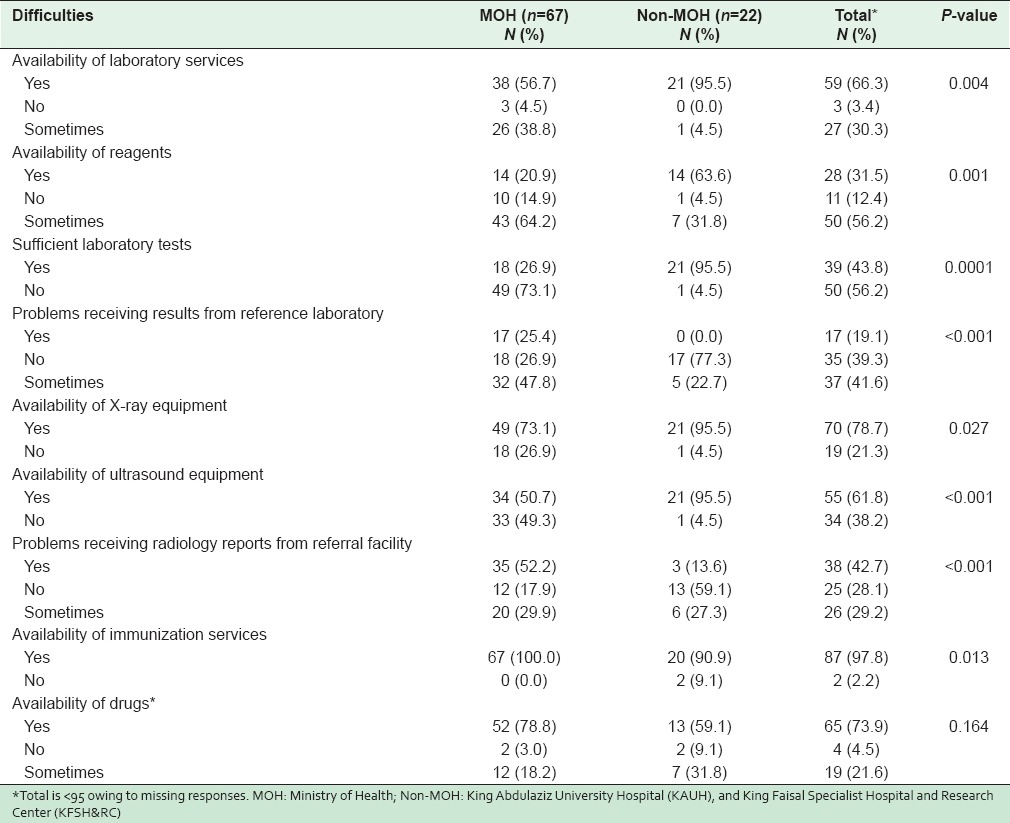
MOH family physicians were also more likely to report unavailability of laboratory services (P = 0.004), reagents (P = 0.001), X-ray equipment (P = 0.027), ultrasound equipment (P < 0.001) and insufficient laboratory tests [P = 0.0001; Table 4]. On the other hand, the unavailability of immunization services was was more commonly reported by non-MOH family doctors (P = 0.013). There was no difference between MOH and non-MOH physicians regarding the unavailability of drugs [P = 0.164; Table 4].
Table 4.
Difficulties related to diagnostic, immunization, and pharmacy services
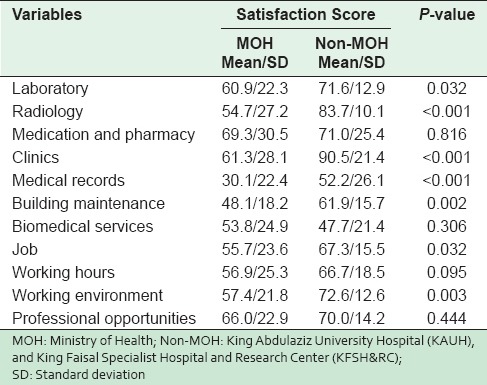
In general, MOH family physicians had lower satisfaction scores than their non-MOH colleagues (54.7 ± 17.7 as against 66.3 ± 6.7 for non-MOH physicians; P < 0.001). Table 5 shows that the mean satisfaction scores were significantly lower for MOH family physicians regarding laboratory (P = 0.032), radiology (P < 0.001) and medical records services (P < 0.001), building maintenance (P = 0.002), as well as clinics (P < 0.001). Similarly, MOH physicians were significantly less satisfied with their jobs (P = 0.032) and working environments (P = 0.003).
Table 5.
Comparison of satisfaction score between MOH and Non-MOH family physicians
DISCUSSION
The MOH in the Kingdom of Saudi Arabia adopted community-based health care through PHC centers as a means of making good quality health services accessible.[5] The provision of good quality health services, however, requires infrastructure, such as human resources, diagnostic and therapeutic facilities, and good transportation, including cars and ambulances.[8] As with many nations, the Kingdom of Saudi Arabia is seeking to promote the development of a comprehensive PHC strategy, and restructure its existing health care system in order to improve the quality of services provided to its citizens. Unfortunately, health care professionals continue to be confronted by considerable impediments.[7]
Although the organization of primary care services in Saudi Arabia has improved in recent years, as shown by the number of staff present in most PHC centers, studies point to several organizational obstacles, including staff turnover, stressful work conditions, overworked physicians, and shortage of resources.[5] In the current study, difficulties related to staff, inadequate infrastructure and services were common issues that family physicians at MOH PHC centers faced. Similar findings were reported among primary care physicians in studies conducted abroad.[9,10]
Transportation difficulties featured as an important problem, which may be because most of the physicians in our study were women, and women are prohibited from driving in Saudi Arabia. These difficulties were mainly because of the unavailability of drivers, whom female physicians had to rely on to go to work. These and other difficulties mentioned earlier may be the result of the lack of resources, which seem to impede the achievement of quality primary care in Saudi Arabia.[5] The only area in which MOH family physicians reported 100% satisfaction as compared with their colleagues at non-MOH facilities was immunization services. This reflects the success that Saudi government has had in making immunization easily accessible in the primary care setting.
Reports suggest that the electronic medical records systems has provided the advantage of improving the quality of health care,[11,12] decreasing the time spent on paperwork,[13] and increasing patient satisfaction.[14] In a study that explored the aspects of electronic medical record systems that contribute to user satisfaction, Joos et al.[15] found that most of the clinicians in their study either agreed or strongly agreed that the use of an electronic medical records system resulted in effective gains relative to the former setting with computer-retrievable laboratory results. Our finding that the lack of access to the internet and computers was more common among MOH family physicians is consistent with that of other authors who reported that only 10.6% of PHC physicians in Riyadh had access to the internet.[16] These difficulties translated into lower job satisfaction scores among MOH family physicians.
The main strength of our study is the high response rate, which reflects the willingness of family physicians to report the problems they have. Nonetheless, all non-MOH family physicians in this study were recruited from two main hospitals in Jeddah. This may have introduced some bias in the analysis.
CONCLUSION
The results of our study demonstrate that family physicians who worked at MOH PHC centers encountered more problems than their counterparts in non-MOH health facilities. These difficulties affect the level of satisfaction of MOH family physicians, as their lower mean satisfaction scores show. It may also have implications for the quality of health care services and workforce recruitment in PHC settings. Thus, we recommend that health care administrators should make every effort to diminish difficulties faced by primary care physicians by providing the essential facilities and investing in capital structures, as these might improve physician satisfaction.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Murtagh JE. Paradigms of family medicine: Bridging traditions with new concepts; meeting the challenge of being the good doctor from 2011. Asia Pac Fam Med. 2011;10:9. doi: 10.1186/1447-056X-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nesbitt TS. Obstetrics in family medicine: Can it survive? J Am Board Fam Pract. 2002;15:77–9. [PubMed] [Google Scholar]
- 3.McGaha AL, Garrett E, Jobe AC, Nalin P, Newton WP, Pugno PA, et al. Responses to medical students’ frequently asked questions about family medicine. Am Fam Physician. 2007;76:99–106. [PubMed] [Google Scholar]
- 4.Al-Kurashi NY. Future of the arab family physician. J Family Community Med. 2002;9:17–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Ahmadi H, Roland M. Quality of primary health care in Saudi Arabia: A comprehensive review. Int J Qual Health Care. 2005;17:331–46. doi: 10.1093/intqhc/mzi046. [DOI] [PubMed] [Google Scholar]
- 6.Al Juhani AM, Kishk NA. Job satisfaction among primary health care physicians and nurses in Al-madinah Al-munawwara. J Egypt Public Health Assoc. 2006;81:165–80. [PubMed] [Google Scholar]
- 7.Sharaf E, Madan N, Sharaf A. Physician job satisfaction in primary care. Bahrain Med Bull. 2008;30:2. [Google Scholar]
- 8.WHO-EM/PHC?81-A/G/93. Riyadh: Al-Helal Press; The Scientific Committee of Quality Assurance in Primary Health Care. Quality Assurance in Primary Health Care Manual; pp. 10–41. [Google Scholar]
- 9.Manca MP, Varnhagen S, Brett-MacLean P, Allan M, Szafran O, Ausford A, et al. Satisfactions and challenges of family physicians. Can Fam Physician. 2007;53:277–86. [Google Scholar]
- 10.Reed AJ, Schmitz D, Baker E, Nukui A, Epperly T. Association of “grit” and satisfaction in rural and nonrural doctors. J Am Board Fam Med. 2012;25:832–9. doi: 10.3122/jabfm.2012.06.110044. [DOI] [PubMed] [Google Scholar]
- 11.Bates DW. Getting in step: Electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–6. doi: 10.1007/s11606-010-1252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saleem JJ, Flanagan ME, Wilck NR, Demetriades J, Doebbeling BN. The next-generation electronic health record: Perspectives of key leaders from the US department of veterans affairs. J Am Med Inform Assoc. 2013;20:e175–7. doi: 10.1136/amiajnl-2013-001748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ilie V, Van Slyke C, Parikh MA, Courtney JF. Paper versus electronic medical records: The effects of access on physicians’ decisions to use complex information technologies. Decis Sci. 2009;40:213–41. [Google Scholar]
- 14.de Lusignan S, Mold F, Sheikh A, Majeed A, Wyatt JC, Quinn T, et al. Patients’ online access to their electronic health records and linked online services: A systematic interpretative review. BMJ Open. 2014;4:e006021. doi: 10.1136/bmjopen-2014-006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joos D, Chen Q, Jirjis J, Johnson KB. An electronic medical record in primary care: Impact on satisfaction, work efficiency and clinic processes. AMIA Annu Symp Proc. 2006;2006:394–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Ansary LA, Khoja TA. The place of evidence-based medicine among primary health care physicians in Riyadh region, Saudi Arabia. Fam Pract. 2002;19:537–42. doi: 10.1093/fampra/19.5.537. [DOI] [PubMed] [Google Scholar]


