Abstract
Background
Magnetic resonance–guided high-intensity focused ultrasound (MRgHIFU) is a noninvasive uterine-preserving treatment alternative to hysterectomy for women with symptomatic uterine leiomyomas (fibroids). Uterine fibroids commonly occur, have a broad impact on women's health and lifestyle, continue to be the main indication for hysterectomy, and represent a costly public health burden.
Objectives
The objectives of the analysis were to evaluate patients’ eligibility for MRgHIFU treatment of symptomatic uterine fibroids and the technical success, safety, effectiveness, and durability of this treatment. The review also compared the safety and effectiveness of MRgHIFU with other minimally invasive uterine-preserving treatments and surgeries for uterine fibroids.
Methods
A literature search was performed on March 27, 2014, using Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid EMBASE, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), and EBM Reviews, for studies published from January 1, 2000, to March 27, 2014.
Results
The evidence review identified 2 systematic reviews, 2 RCTs, 45 cohort study reports, and 19 case reports involving HIFU treatment of symptomatic uterine fibroids. Eligibility for MRgHIFU treatment was variable, ranging from 14% to 74%. In clinical cohort studies involving 1,594 patients, 26 major complications (1.6%) were reported. MRgHIFU resulted in statistically and clinically significant reductions in fibroid-related symptoms in studies conducted in 10 countries, although few involved follow-up longer than 1 year. Retreatment rates following MRgHIFU were higher in early clinical studies involving regulated restrictions in the extent of fibroid ablation than in later reports involving near-complete ablation. Emergent interventions, however, were rare. Although a desire for fertility was an exclusion criteria for treatment, spontaneous term pregnancies did occur following HIFU. There were no randomized trials comparing MRgHIFU and other guidance methods, other minimally invasive treatments, or surgeries for symptomatic uterine fibroids. Limitations with MRgHIFU included restricted eligibility, requirement for a dedicated MR device to guide the treatment, lengthy procedure time, and loss of MR opportunity time.
Conclusions
For women failing medical therapy and seeking alternatives to hysterectomy for symptomatic uterine fibroids, MRgHIFU provides a safe and effective, noninvasive, uterine-preserving treatment from which they rapidly recover. The treatment advantages of MRgHIFU are potentially offset by restrictive eligibility, lengthy procedure time, and dependence on availability of an MR device. The lack of comparative evidence between MRgHIFU and other, more established uterine-preserving treatments limits informed decision making among treatment options.
PLAIN LANGUAGE SUMMARY
Uterine fibroids are the most common benign tumours in women of child-bearing age. They can cause pain, heavy menstrual bleeding, and fertility problems, and fibroids are the main reason women have a hysterectomy (surgery to remove the uterus). For women whose fibroids do not shrink through the use of medication, several treatments have been developed that are less invasive than surgery and do not remove the uterus, which means women may not lose the ability to bear children in future. Magnetic resonance–guided high-intensity focused ultrasound (MRgHIFU) is one of these treatments, a noninvasive uterine-preserving alternative to hysterectomy for women with fibroids. MRgHIFU is not currently available in Ontario except through clinical trials.
Health Quality Ontario conducted an evidence review to determine the safety and effectiveness of this new technology and to compare it to other treatments. We found more than 40 clinical studies at hospitals in many countries showing that fibroid-related symptoms were significantly improved after MRgHIFU treatment and that women recover rapidly after the procedure. However, the follow-up of women in most of the studies was usually only 12 months so we are less certain about whether this treatment reduces symptoms for the long term. Major complications were rare in these studies, and there was a low risk that women would need further treatments after the procedure, particularly any emergency treatments. Although women were excluded from the studies if they hoped to have children in the future, successful pregnancies have been reported after the treatment. This suggests that MRgHIFU may have a role in preserving fertility for women with uterine fibroids. This technology has two important disadvantages, however: there are many clinical and technical restrictions that limit the number of women who can be eligible for the treatment, and each procedure takes several hours and requires the use of dedicated magnetic resonance imaging (MRI) equipment for the entire procedure.
BACKGROUND
Magnetic resonance–guided high-intensity focused ultrasound (MRgHIFU) is a new noninvasive treatment for women with symptomatic uterine leiomyomas (fibroids). It has been offered as a treatment option that preserves the uterus for women seeking alternatives to hysterectomy to treat their fibroid symptoms. Uterine fibroids are common, have a broad impact on women's overall health and lifestyle, and continue to be the main indication for hysterectomy. (1) Fibroids can also adversely impact fertility (2) and, with the societal trend of women delaying child-bearing to later ages (3) when fibroids commonly occur, women increasingly have a need for treatment options that not only preserve the uterus but also their fertility. Overall, uterine fibroids represent a public health burden that is costly to women, their families, employers, and the health care system. (4–6)
Objective of Analysis
The objectives of this analysis were to review studies that have evaluated patients’ eligibility for MRgHIFU treatment; to review the technical success and durability of MRgHIFU for treatment of symptomatic uterine fibroids; and to evaluate the comparative safety and effectiveness of MRgHIFU with other minimally invasive, uterine-preserving treatments and with surgeries to treat uterine fibroids.
Clinical Need and Target Population
Uterine leiomyomas (fibroids) are the most common pelvic tumour among women of reproductive age. (1) They are benign tumours that arise from the smooth muscle cells of the myometrium, and their pathogenesis is believed to depend on estrogens and progesterone and an interaction with growth factors, cytokines, and extracellular matrix components. (7;8) As fibroid development and growth are hormonally mediated, fibroids rarely develop before menarche and are thought to regress after menopause. (9) They are often classified by their location in the uterus as either subserosal, intramural, or submucosal (10) and can occur as a single localized mass or as heterogeneous clusters and can vary greatly in size. (9)
Although fibroids are benign tumours, they can cause significant morbidity. Depending on their location in the uterus, symptoms can range from bleeding, mass effects, and impacts on fertility. Their effects on menstrual functions include excessive blood loss (menorrhagia); lengthy, irregular, or non-cyclical periods; and periods associated with pain (dysmenorrhea) and anemia. (1) The mass effects caused by large fibroids can range from bladder dysfunctions such as urinary frequency or nocturia (frequent night-time urination) to bowel dysfunctions such as constipation or painful bowel movements to sexual dysfunctions involving dyspareunia (painful intercourse). Fibroids can also affect fertility and pregnancy, causing repeated miscarriages or delivery complications. (11–15)
Prevalence and Incidence
Uterine fibroids are generally asymptomatic, and prevalence estimates generally range from 20% to 40% for women 30 years or older. (16) A population-based survey in the United States estimated the incidence of uterine fibroids using self-reports, medical records, and ultrasounds of premenopausal women aged 35 to 49 years. (17) In this age group, 16% reported already being surgically or naturally menopausal. Thirty-five percent of the women in the survey reported already having a diagnosis of uterine fibroids. Black women were more than twice as likely as white women to report a previous diagnosis of fibroids (45% vs. 21%), and they were also diagnosed at a significantly younger age than white women (33 years vs. 36 years; P < 0.001). Fifty-one percent of those not having a prior diagnosis of fibroids were found to have ultrasonographic evidence of fibroids, and again the proportion was higher for black women (59% vs. 43%).
In the same survey, women with clinically relevant fibroids were defined as those having 1 of the following: enlarged uterus (≥ 10 cm in length and comparable to a 9-week pregnancy); at least 1 fibroid larger than 4 cm in diameter; or at least 1 submucosal fibroid (which are most likely to cause bleeding). Clinically relevant fibroid were found to increase with age and again were significantly more common in black women (odds ratio [OR], 2.6; 95% confidence interval [CI], 2.2–3.0; P < 0.001). In premenopausal women aged 35 to 39 years, 30% to 40% of black women (10% to 15% of white women) had clinically significant fibroids increasing to 50% of black women (35% of white women) in their late forties. (17)
Many other studies have consistently shown that uterine fibroids have a differential impact on black women compared to white women. Black women have 2- to 3-fold higher incidence rates; experience onset at earlier ages; are affected over a greater age span; see no decrease in fibroid growth in perimenopause; have more severe disease at presentation and at surgery; and have higher rates of fibroid-related hospitalization and hysterectomy. (18–20)
Impact on Quality of Life
Clinically relevant tumours have also been defined as those associated with symptoms severe enough to disrupt activities of daily living and adversely impact quality of life. (21) Women have reported broad impacts of fibroids on their overall health and lifestyle. These impacts have included fatigue, self-consciousness, weight gain, interference with physical activities, interference with daily and social activities, effect on relationships with partners and with family and friends, impaired ability to take care of home or children, and missed work days. (21)
A disease-specific symptom and quality of life questionnaire, the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire, was designed to evaluate the broad range of fibroid symptoms as well as their impact on health-related quality of life (HRQOL). (22) The questionnaire consists of 72 items with response options as a 5-level Likert scale (ranging from “not at all” to “a very great deal”), an 8-item symptom severity scale (SSS-UFS-QOL), and 29 health-related quality of life questions focusing on 6 subscales: concern, activities, energy/mood, control, self-consciousness, and sexual function. The questionnaire has been documented to have high psychometric properties including high test-retest reliability and validity; it is able to discriminate between women with and without fibroids and among women with different degrees of fibroid-related symptoms. (23;24)
Fibroid Management
For women with asymptomatic fibroids, the recommended care is conservative management with occasional follow-up. (25) For those with symptomatic fibroids, including menstrual dysfunctions, various medical therapies are available, although their use is often short term, for temporary relief of symptoms, because of their limited effectiveness and known or uncertain long-term risks. (9;26) There is, however, an expanding range of minimally invasive treatment options for women with symptomatic uterine fibroids who have failed or are intolerant to medical therapy. (27) Among these minimally invasive options are uterine artery embolization (UAE, a procedure involving injections into the uterine arteries that aim to shrink the fibroids) (28) and various ablation therapies using different energy sources such as radiofrequency, microwave, ultrasound, and laser. (27;29–31) In most cases these treatments preserve the uterus, do not involve general anesthesia, require limited or no hospital stay, and result in fewer complications and quicker recovery, often within days. High-intensity focused ultrasound guided by magnetic resonance imaging (MRgHIFU) is the latest in these treatment options and is currently the only noninvasive procedure for symptomatic uterine fibroids.
Hysterectomy is the most common gynecological surgery in the world, and uterine fibroids are the leading indication for hysterectomy. Up to 1 in 3 women who receive a new diagnosis of fibroids has related surgery within the year. In Canada, hysterectomy is also the second most common surgery for women, after Caesarean section, and uterine fibroids are the leading indication for hysterectomy, frequently accompanied by oophorectomy (the removal of ovaries). In 2008/2009, almost 47,000 Canadian women had a hysterectomy and rates between provinces varied substantially (185 to 512 per 100,000 women) and by rural/urban residence (464 to 318 per 100,000). (32)
Women's Preferences
Although hysterectomy is the common final treatment for symptomatic uterine fibroids because it relieves all symptoms by removing the uterus, this treatment is associated with significant morbidity and lengthy hospital stays and recovery time. For these reasons, many women reject hysterectomy as a treatment for uterine fibroids. (33–35) For younger women who have not completed their families, hysterectomy also terminates any future reproductive options, and if they have an oophorectomy at the same time, they immediately enter menopause, often years before they would naturally. Women have reported in surveys that uterine fibroid treatment options that preserve the uterus and potentially spare their fertility are particularly important to them. (21)
Women often have difficulty finding comprehensive information on treatment options for their fibroid-related symptoms. Multidisciplinary fibroid centres that include a variety of specialists (e.g., radiologists, reproductive endocrinologists, and internists, in addition to gynecologists) have reported some success in providing women with comprehensive information and second opinions. (36) At one of these centres, only 4% of women who had previously been recommended for hysterectomy were, after joint consultations, still recommended to be candidates for hysterectomy. The majority of patients at the centre underwent an alternative therapy, such as UAE, MRgHIFU, or myomectomy (surgery that removes the fibroids but preserves the uterus). Patients attending the multidisciplinary clinic had been either referred by their physicians or self-referred after searching on-line and finding information on uterine fibroid treatments. (36) Another group investigating the information-seeking behaviour of women, specifically for UAE as an alternative to hysterectomy, reported that 60% only became aware of this treatment option through mass media, friends, or family members. (37)
Ontario Prevalence, Incidence, and Treatments
We used provincial administrative health care databases for Ontario, a population with universal health insurance, to estimate the incidence of newly diagnosed symptomatic uterine fibroids and their treatments (Table 1). In 2012, 22,912 women came to medical attention for fibroid symptoms and received a new diagnosis of uterine fibroids. We calculated a crude 10-year prevalence burden (2002–2012) of women receiving a new diagnosis of symptomatic uterine fibroids by correcting for fibroid surgeries during the period. Subtracting both hysterectomies and myomectomies gave a crude 10-year prevalence of symptomatic uterine fibroids of 137,720 women.
Table 1:
Ontario Women with Symptomatic Uterine Fibroids and Their Treatments
| Ontario female population, 2012 | |
| Women aged 16–84 years, n | 5,516,196 |
| Women receiving a new diagnosis of uterine fibroids in 2012, na | 22,912 |
| 10-year prevalence for 2002–2012, n (number of women receiving a fibroid diagnosis – number of women having a fibroid-related hysterectomy or myomectomy) | 171,598 |
| Fibroid Management, 2012 | |
| Non-surgical management, n (%) | 13,156 (57.4%) |
| Hysterectomy, n (%) | 5,327 (23.2%) |
| Proportion of hysterectomy with oophorectomy surgery, n (%) | 2,510/5,327 (47%) |
| Myomectomy, n (%) | 3,851 (16.8%) |
| Uterine artery embolization, n (%) | 578 (2.5%) |
Number of women who came to medical attention and received a diagnosis of uterine fibroid (in hospital, had an intervention, or visited a physician for uterine fibroids)
Source: Data provided by the Institute for Clinical and Evaluative Sciences, July 10, 2014.
In 2012, of the almost 23,000 women newly diagnosed with uterine fibroids, more than half were primarily managed conservatively or with a range of medical therapies. Another 40% of the women had surgery, either hysterectomy (5,327 women) or myomectomy (3,851 women). Bilateral oophorectomy (removal of both ovaries) was performed in almost half of the hysterectomies. The risk status of women with symptomatic fibroids for ovarian cancer or breast cancer, however, is unknown. Just 2.5% of women were treated with UAE, a minimally invasive, uterine-preserving treatment alternative to hysterectomy for symptomatic uterine fibroids. UAE was introduced in Ontario in the early 2000s.
MRgHIFU Technology
Background
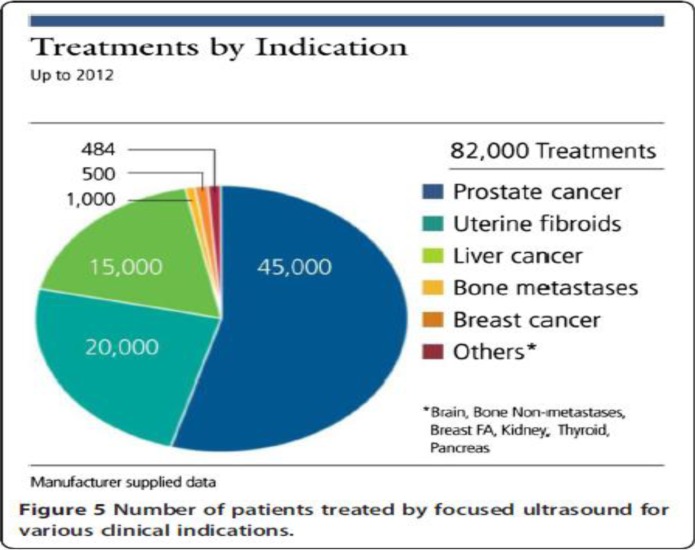
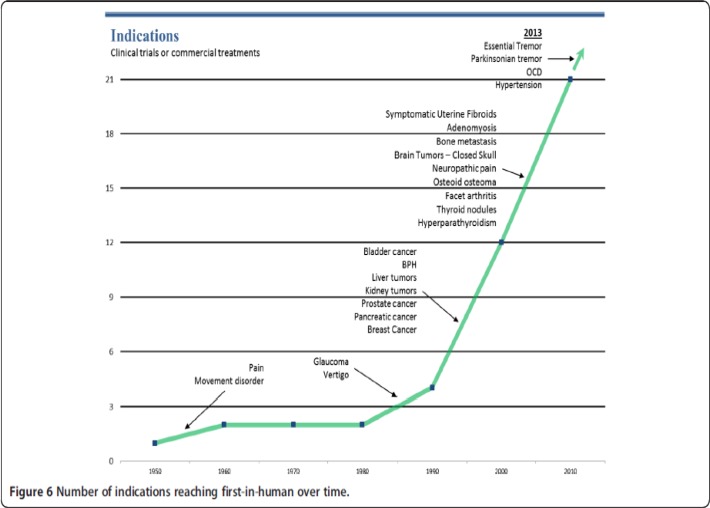
Magnetic resonance–guided high-intensity focused ultrasound is a noninvasive procedure that heats and destroys tumours (thermal ablation) by combining 2 technologies: magnetic resonance (MR) imaging and high-intensity focused ultrasound (HIFU). The MR and thermal mapping system are used to visualize the patient anatomy, map the volume of tissue to be treated, monitor in real-time the tissue temperature during the ablation process to allow treatment adjustment, and evaluate the treatment results. Although both ultrasound and MR guidance have been used with HIFU treatments, MR guidance is considered key to guiding and controlling the delivery of HIFU to ensure the treatment is safe and effective. HIFU has been investigated for a wide range of solid benign and malignant tumours in the uterus, breast, prostate, liver, kidney, pancreas, and brain and for painful bony metastases (Figure 1). (38) Since the 1950s there has been a gradual increase in the clinical indications for HIFU; currently, prostate cancer and uterine fibroids are the principal indications in clinical trials and commercial treatments (procedures done after the device was on the market) (Figure 2). (38)
Figure 1: High-Intensity Focused Ultrasound Treatment Volumes by Clinical Indications, as Reported by Device Manufacturers.
Reprinted from Tyshlek D, Auby JF, Haar G, Hananel A, Foley J, Eames M, et al. Focused ultrasound development and clinical adoption: 2013 update on the growth of the field. Journal of Therapeutic Ultrasound. 2014;2(0):2–7, with permission from BioMed Central.
Figure 2: Changes Over Time in Indications for High-Intensity Focused Ultrasound.
Abbreviations: BPH, benign prostatic hypertrophy; OCD, obsessive-compulsive disorder.
Reprinted from Tyshlek D, Auby JF, Haar G, Hananel A, Foley J, Eames M, et al. Focused ultrasound development and clinical adoption: 2013 update on the growth of the field. Journal of Therapeutic Ultrasound. 2014;2(0):2–7, with permission from BioMed Central.
Procedural Details for MRgHIFU Treatment of Uterine Fibroids
Patients are examined clinically and undergo physical and pelvic imaging or screening MR exams the day prior to the procedure to determine their eligibility and plan the treatment. A computerized planning module generates a treatment plan after calculating the energy, location, and number of ultrasound sonications, or energy bursts, needed to treat the fibroid volume. (39) The treatment is not a global therapy in that ablation is generally not directed at all the fibroids, but rather it is a targeted approach in which the fibroids suspected of causing the symptoms are targeted for ablation.
Prior to the procedure, patients must remove all hair in the pelvic/abdominal region to avoid skin burns as the ultrasound beam passes through that area of the body. The procedure itself can take up to 3 hours not including patient preparation or table set-up time. Generally, fibroids ranging from smaller sizes of 2 to 3 cm to larger sizes of 10 cm can be treated. A 3-hour session can be adequate to treat a single fibroid approximately 7 to 8 cm in size. (40) Initially, a 3-hour limit was arbitrarily established because of a concern that, with prolonged immobilization, patients were at risk for deep vein thrombosis. With experience, the initial time restrictions imposed by the Food Drug Administration (FDA) in the United States have been eased, and durations of 4 and 5 hours have been employed.
Patient preparation for the procedure is meticulous and time-consuming. (41) It requires an intravenous line for sedation and analgesia and placement of an indwelling urethral catheter. During positioning of the patient on the table, it is essential to ensure adequate coupling between the transducer (the ultrasound probe) and the targeted fibroid to avoid skin burns. For MRgHIFU to treat uterine fibroids, the patient must be in the prone position. (For bone indications, the procedure can be performed with variable positioning of the patient.) The narrow bore of the MR gantry (the structure that the patient is passed through) can also inhibit successful positioning of large patients although the degree of patient's abdominal adiposity may itself be a limiting factor. The sonication beam has a limited penetration depth, and excessive intervening adipose layers can prevent access to the target fibroid.
The temperature needed to induce tissue necrosis (destroy tissue) is dependent on several factors including temperature and duration of sonication: 50°C for 10 seconds or 56°C for 1 second induces tissue necrosis. (41) Typically, short (approximately 20 seconds) and multiple sonications (60–90 bursts of 1,000–7,000 joules of energy) are delivered, with continual thermal feedback provided during the procedure. Between sonications, there are 90-second pauses to limit thermal damage to non-targeted fields. (39) A room nurse monitors the patient for pain and assesses the location and severity of pain. During the procedure, the treating physician can alter multiple parameters including the steering of the beam, location of the focus, and volume of the target zone to be ablated. The procedure can be stopped at any time by the patient (who can activate a stop button if they experience pain) or by the physician, the nurse, or the device's over-ride safety programming.
At the end of the procedure, the technical success of the treatment is assessed using routinely acquired MR contrast-enhanced images that document the degree of ablated fibroid tissue, defined as non-perfused volume (NPV). The NPV is represented by the non-enhancing volume on contrast T1-weighted MR. (42) After the procedure, women are observed for several hours before being discharged. Although initially disallowed by FDA regulatory protocols, planned second HIFU procedures are currently performed, usually within days of the first procedure, when there is insufficient time to ablate the entire target volume in a single session.
Regulatory Status
There are presently 2 manufacturers of MRgHIFU devices: InSightec Ltd., an Israeli company that produces the ExAblate HIFU device requiring guidance by a GE MR scanner, and Philips Healthcare which produces the Sonalleve HIFU device requiring guidance by a Philips MR scanner. MR guidance for both devices usually involves a magnet field strength of 1.5 or 3.0 Tesla. Both companies have regulatory approvals in many countries for uterine fibroids and for palliation of painful bony metastases. InSightec's CE mark approval (the European Commission's regulatory process) also includes treatment of multiple myeloma and facet joint syndrome.
Regulatory approvals of the ExAblate MRgHIFU device have been obtained for the treatment of uterine fibroids and palliation of bony metastases in Canada and 11 other jurisdictions. (Personal Communication, Nadir Alikacem, Vice President, Regulatory Affairs, InSightec Ltd., May 2014) As of May, 2014, these jurisdictions and approval dates (fibroids / bony metastases) were as follows: United States (October 2004 / October 2012); Europe (October 2002 / May 2007); Japan (September 2009 / in progress); China (September 2013 / in progress); Australia (May 2006 / May 2006); Brazil (August 2006 / August 2006); Israel (August 2002 / April 2008); Korea (November 2005 / March 2009); Mexico (March 2007 / in progress); New Zealand (May 2006 / May 2006); Russia (November 2004 / November 2007) and Taiwan (May 2006 / in progress). The ExAblate device also has the CE mark in Europe for MRgHIFU treatment of essential tremor, Parkinson disease, and neuropathic pain (December 2012), and a clinical trial is currently underway in the United States and Canada under both Health Canada and the FDA.
Regulatory approvals for the Philips Sonalleve MRgHIFU system for treatment of uterine fibroids has been obtained in Canada and 15 other jurisdictions and are in progress for 2 countries: China, for uterine fibroids, and the United States, for uterine fibroids and bony metastases. (Personal Communication, Thomas Andreae, PhD, Director, Marketing MR-Therapy, Philips Healthcare, July 2014) As of May 2014, these other jurisdictions and their dates of regulatory approval for uterine fibroids and for bone metastases were as follows (fibroids / bony metastases): Europe (December 2009 / February 2011); Switzerland, Norway, Iceland, Liechtenstein, Turkey (October 2011 / in progress); Argentina (July 2012 for both indications); Brazil (February 2013 for both indications); Mexico (August 2013 for both indications); Kazakhstan (May 2013 for both indications); Russia (March 2013 for both indications); Saudi Arabia (July 2013 for both indications); Jordan (December 2009 / February 2011); Australia (December 2012 for both indications); India (December 2009 / February 2011); Indonesia (October 2012 for both indications); Malaysia (December 2009/ February 2011); New Zealand (December 2013 for both indications); South Korea (October 2010 / in progress); Vietnam (December 2009 / February 2011).
Health Canada has approved both the ExAblate HIFU device (License 91830, issued on August 15, 2013) and the Sonalleve HIFU device (License 87439, issued on November 7, 2013) both as Class III devices. The ExAblate HIFU device is approved for indications of symptomatic uterine fibroids and palliation of painful bony metastases. The indications for fibroid treatment are for symptom relief in pre- or perimenopausal women who desire a uterine-sparing procedure and whose uterine size is less than a 24-week pregnancy. Patients should also have completed child-bearing. The Sonalleve HIFU device has approval for treatment of symptomatic uterine fibroids, with the same indications as for the ExAblate device except that women planning future pregnancy are advised to consult with their physician. The FDA's initial approval of ExAblate treatment for uterine fibroids included a condition that patients “must have” completed child-bearing. The FDA implemented less restrictive commercial treatment guidelines in 2004, (43) and a premarket approval supplement in 2009 softened the position on fertility with the statement that patients “should have” completed child-bearing. (44)
In Ontario, 2 sites are currently investigating the use of MRgHIFU (the Sonalleve HIFU device) for treating symptomatic uterine fibroids: Sunnybrook Health Sciences Centre in Toronto and Thunder Bay Regional Research Institute. (Personal Communication, Thomas Andreae, PhD, Director, Marketing MR-Therapy, Philips Healthcare, July 2014) MRgHIFU services are not provided in any other province and it is not an insured service in any province for any indication.
EVIDENCE-BASED ANALYSIS
Research Questions
What are the patient eligibility criteria, technical success, safety, effectiveness, and durability of magnetic resonance–guided high-intensity focused ultrasound (MRgHIFU) for treatment of symptomatic uterine fibroids?
What is the comparative safety and effectiveness of MRgHIFU in the treatment of symptomatic uterine fibroids, versus other uterine-preserving procedures and versus hysterectomy?
Research Methods
Literature Search
Search Strategy
A literature search was performed on March 27, 2014, using Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid EMBASE, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), and EBM Reviews, for studies published from January 1, 2000, to March 27, 2014. (Appendix 1 provides details of the search strategies.) Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search.
Inclusion Criteria
English-language full-text publications
published between January 1, 2000, and March 27, 2014
randomized controlled trials (RCTs), systematic reviews (SRs), meta-analyses, and observational studies including case reports
clinical studies including technical and clinical outcomes on any of the following: safety, eligibility, technical success, safety, fibroid reduction, symptom relief, reinterventions, heath-related quality of life (HRQOL)
any comparative studies involving MRgHIFU and an alternative treatment including other uterine-preserving treatments or hysterectomy.
Exclusion Criteria
experimental or animal studies involving evaluations of technology performance
studies not involving technical or clinical outcomes
Outcomes of Interest
eligibility for treatment
technical success
fibroid shrinkage
symptom relief
durability of symptom relief
reintervention rates
adverse events
reproductive outcomes
Quality of Evidence
The quality of the body of evidence for each outcome was examined according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria. (45) The overall quality was determined to be high, moderate, low, or very low using a step-wise, structural methodology.
Study design was the first consideration; the starting assumption was that RCTs are high quality, whereas observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias—were then taken into account. Limitations in these areas resulted in downgrading the quality of evidence. Finally, 3 main factors that may raise the quality of evidence were considered: the large magnitude of effect, the dose-response gradient, and any residual confounding factors. For more detailed information, please refer to the latest series of GRADE articles. (45)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | High confidence in the effect estimate—the true effect lies close to the estimate of the effect |
| Moderate | Moderate confidence in the effect estimate—the true effect is likely to be close to the estimate of the effect, but may be substantially different |
| Low | Low confidence in the effect estimate—the true effect may be substantially different from the estimate of the effect |
| Very Low | Very low confidence in the effect estimate—the true effect is likely to be substantially different from the estimate of the effect |
Results of Evidence-Based Analysis
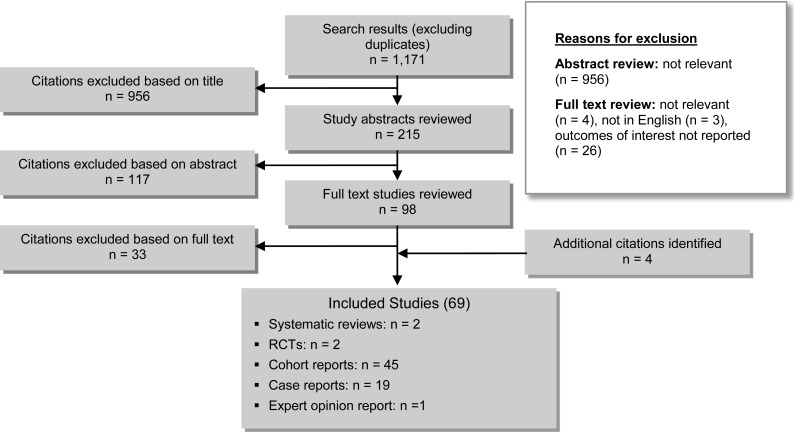
The database search performed on March 27, 2014, and yielded 1,171 citations published between January 1, 2000, and March 27, 2014 (with duplicates removed). Articles were excluded based on information in the title and abstract. The full texts of potentially relevant articles were obtained for further assessment. Figure 3 shows the breakdown of when and for what reason citations were excluded from the analysis.
Figure 3: Citation Flow Chart.
For each included study, the study design was identified and is summarized below in Table 2, a modified version of a hierarchy of study design by Goodman, 1996. (46)
Table 2:
Body of Evidence Examined According to Study Design
| Study Design | Number of Eligible Studies |
|---|---|
| RCTs | |
| Systematic review | |
| Large RCT | |
| Small RCT | 2 |
| Observational Studies | |
| Systematic review | 2 |
| Controlled cohort clinical studies | |
| Uncontrolled cohort clinical studies | 45 |
| Database, registry, or cross-sectional study | |
| Case series | 19 |
| Retrospective review, modelling | |
| Studies presented at an international conference | |
| Expert opinion | 1 |
Abbreviations: RCT, Randomized controlled trial.
The systematic evidence search on MRgHIFU for uterine fibroids identified 2 systematic reviews (47;48) that were used to identify any additional relevant citations. This review also identified 2 RCT reports, 45 cohort study reports, and 19 case reports involving HIFU for treatment of systematic uterine fibroids. Investigators from 29 institutes in 12 countries have reported on their clinical results of MRgHIFU treatment of symptomatic uterine fibroids (Table 3). The 16 reports from American sites involved 7 reports that included overlapping patient groups with different follow-up periods and study objectives. The summary details of these clinical reports are further listed in Appendix 2, Table A1. The GRADE evidence profile for this body of evidence is summarized in Table A2.
Table 3:
Reports of HIFU Treatment of Uterine Fibroids by Country, Institute, and Study Type
| Country | Technology | Number of Institutions | Total Reports | Case Reports | Cohort Study Reports | RCT Reports |
|---|---|---|---|---|---|---|
| Australia | ExAblate 2000 – 1.5T MR | 1 | 1 | 1 | ||
| Brazil | ExAblate 2000 – 1.5T MR | 1 | 1 | 1 | ||
| China | JC-HIFU Ultrasound | 2 | 5 | 1 | 1 | 3 |
| Germany | ExAblate 2100 – 1.5T MR | 1 | 3 | 3 | ||
| India | ExAblate 2000 – 1.5T MR | 2 | 3 | 1 | 2 | |
| Israel | ExAblate 2000 – 1.5T MR | 2 | 3 | 2 | 1 | |
| Japan | ExAblate 2000 – 1.5T MR | 5 | 9 | 2 | 7 | |
| Korea | ExAblate 2000 – 1.5T MR Sonalleve 1.5T MR | 3 | 12 | 4 | 8 | |
| Netherlands | Sonalleve 1.5T MR | 1 | 3 | 1 | 2 | |
| Norway | Sonalleve 1.5T MR | 1 | 1 | 1 | ||
| United Kingdom | ExAblate 2000 – 1.5T MR | 1 | 6 | 3 | 3 | |
| United States | ExAblate 2000 – 1.5T MR | 9 | 20 | 3 | 17 | |
| Total | 29 | 67 | 19 | 45 | 3 |
Abbreviations: RCT, randomized controlled trial; T MR, Tesla magnetic resonance.
The clinical reports on MRgHIFU treatment for symptomatic uterine fibroids involved 2 HIFU devices, the ExAblate and the Sonalleve. Almost all countries had clinical reports with the ExAblate device. Three countries (Korea, Netherlands, and Norway) had clinical reports involving the Sonalleve device, and Korea was the only country to have clinical reports for both devices. Both devices involved reports on their first- or second-generation hardware and/or software enhancements. The technical performance of these devices, however, was restricted in several ways by initial regulatory controls of the FDA that aimed to balance safety with effectiveness. In general, the restrictions included limiting the degree of ablation of the target fibroid, only treating 1 fibroid, restricting the procedure time to 3 hours, and not permitting repeat procedures. (49) As well, due to the uncertainty of the effect of HIFU on fertility, it was also an absolute requirement that women have completed their child-bearing.
The FDA gradually relaxed the technical restrictions, particularly with respect to the fibroid volume that could be treated. Prior to 2004, the FDA only allowed ablation of 33% of the fibroid, to a maximum of 100 ml for a single fibroid, limited the maximum procedure time to 120 minutes, and did not allow second procedures. After April 2004, the FDA allowed second or staged procedures, increased the maximum procedure time to 180 minutes, and increased the ablation limits to 50% and 150 ml of the fibroid volume. In April 2009, the FDA lifted these restrictions allowing for 100% ablation of the target. (49) The FDA in 2009 also revised the contraindication on child-bearing and stated that women “should be family complete” rather than “must be family complete.” (44) For those reasons, evaluations of safety and effectiveness in this review were, where possible, stratified by the degree of intended ablation stated by the investigators.
Several reports on ultrasound-guided HIFU (USgHIFU) were identified in the literature review. (50–62) We included 5 of these reports (52;54;56;58;59) in this evidence review for several reasons. One of these studies included a large cohort (54) that contributed information on reproductive outcomes after HIFU. There were also no RCTs for MR-guided HIFU and the only RCTs identified involved ultrasound-guided HIFU. One of these RCTs compared HIFU to abdominal myomectomy (59) and the other compared HIFU to radiofrequency ablation, another form of thermal ablation therapy. (52) An additional comparative cohort study compared USgHIFU with laparoscopic myomectomy. (56) All of this evidence derives from studies in China. At this point, no ultrasound-guided HIFU devices have been approved for treatment of symptomatic uterine fibroids in Canada or the United States. Regulatory agencies have been concerned about the safety of ultrasound guidance for HIFU as it does not provide imaging or real-time thermal monitoring as efficiently as MR-guidance. At least 1 clinical trial involving ultrasound guidance for uterine fibroids, however, is currently underway in the United States (ClinicalTrials.gov identifier NCT01946178).
The evidence for MRgHIFU treatment of symptomatic uterine fibroids will be evaluated in the following 6 sections: Section A. Patient Eligibility; Section B. Technical Success; Section C. Safety; Section D. Treatment Effectiveness; Section E. Reproductive Outcomes; and Section F. Comparative Effectiveness.
Section A. Patient Eligibility
Women seeking consultations for MRgHIFU are initially assessed through a medical history and clinical exams to document their age, body mass index, hormonal status, the extent and severity of fibroid symptoms, and the relevance of symptoms to fibroids. If appropriate, they are then referred for a screening pelvic MR exam to determine their anatomic and technical eligibility. Screening with MR is not the standard of care but it is the best modality to document fibroid characteristics and presence of additional uterine pathology. (63) All clinical studies in this evidence review had MR prescreening exams to determine patient eligibility. Treatment eligibility, however, has a variable threshold governed by a series of relative and absolute contraindications from regulatory agencies, manufacturers, institutional review boards, and individual treating or referring physicians.
A survey of the opinions of physicians providing MRgHIFU and attending the first international symposium in 2008 dedicated to MRgHIFU reported various clinical and technical contraindications to this treatment. Factors limiting the use of HIFU for fibroid treatment included comorbid severe adenomyosis, abdominal scarring, pedunculated fibroids (attached to the uterus by a stalk) or fibroids larger than 10 cm in diameter, gadolinium non-enhancement (already non-perfused), and postmenopausal status. (64) A general list of clinical and technical criteria cited in MRgHIFU clinical trials involving contraindications, more relative than absolute criteria, are outlined in Table 4.
Table 4:
Clinical and Technical Factors Limiting MRgHIFU Treatment for Uterine Fibroids
| Clinical Ineligibility | Technical Ineligibility |
|---|---|
| Fibroids not symptomatic, large (> 10 cm), multiple, pedunculated, high vascular index, or degenerated | Unable to remain still in a prone position for long periods of time (> 3 hours) |
| Postmenopausal | Severe claustrophobia |
| Desiring fertilitya | Obesity (≥ 250 lbs., or unable to fit in scanner) |
| Active pelvic inflammatory disease, local or systemic infection | Unable to respond to simple commands |
| Known or suspected pelvic carcinoma or premalignant conditions | Metallic implants incompatible with MR imaging |
| Undiagnosed vaginal bleeding | Sensitivity to MR imaging contrast |
| Concurrent uterine pathology (adenomyosisb) | Fibroids inaccessible to the device (shielded by bone or bowel or deeper than 12 cm from the skin) |
Abbreviations: lbs., pounds; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound.
The FDA requirement is that the patient should not desire future pregnancy and that the physician should be consulted.
Adenomyosis is an approved treatment indication based on the European CE but not the FDA.
Patient selection guidelines are extensive for MRgHIFU and, in summary, include relevant symptoms, fibroid characteristics (particularly distance to the skin or to the sacral bone), obstacles to the ultrasound beam, beam aberration, or other uterine pathology. (65) Patient-related factors such as the correct pathology or the presence of other uterine pathology (e.g., adenomyosis), the relevance of the symptoms to the uterine pathology, and the degree of fibroid-related symptoms are all seen as qualifying criteria. There are many other limiting factors associated with the fibroid characteristics themselves. As noted, fibroids that are too big (> 10 cm) will likely need more than one session to ablate and extended periods of immobilization increase the risk of deep venous thrombosis (DVT). Fibroids that are too numerous pose a different problem, increasing the probability that one or more fibroids will not be appropriate or related to symptoms or may be in a location inaccessible to the ultrasound beam. Pedunculated fibroids pose a potential risk of dislodgement into the peritoneal cavity. Other fibroid characteristics, such as the degree of necrotic degenerative changes already underway or the degree of fibroid vascularity, potentially limit the success of the treatment. Fibroids that are too vascular (usually indicated by a hyperintense signal on MR T2-weighted imaging) act like heat sinks, limiting the degree of thermal energy that can be generated to ablate tissue.
There are also several potential technical restrictions having different implications. A target fibroid positioned too deeply in the body may exceed the depth of the ultrasound beam; 12 cm from the skin is usually the maximum vertical distance. Fibroids are located too close to other vital structures, such as the bladder, bowel, or sacral bone, may pose a risk of non-target ablation to these structures. In addition, anatomic variations such as an irregularly shaped layer of rectus muscle or a large layer of subcutaneous fat may distort, alter, or attenuate the beam or sonication's thermal energy, limiting the degree of tissue ablation.
Mitigation Strategies to Improve Safety or Technical Success
In view of these numerous restrictions and limitations on the use of MRgHIFU, many mitigation strategies have been developed or attempted to increase patient eligibility for the procedure or increase treatment success. (66) Bowel obstruction in the beam pathway has been dealt with in several ways. In some cases, structures can be moved out of the sonication pathway by inflating or deflating Foley catheters with distilled water. (60;67) In the Zhang et al study (60) of 21 patients, all had bowel positioning anterior to the uterus and, in all cases, a degassed water balloon was used to successfully compress the bowel. Careful bowel preparation 3 days prior to the procedure had also been employed for the study group, including a liquid diet, milk restriction, 12-hour fasting prior to the procedure, and an enema in the early morning on the day of the procedure. No bowel injuries were reported. In the Park et al study, (67) a bowel manipulation technique involving sequential applications of urinary bladder filling, rectal filling, and urinary bladder emptying was employed. In their consecutive series, the 33.3% (30/90) screening failure rate due to bowel interference was reduced to 10.7% (15/140) after they employed these bowel-manipulation strategies. The ability to mitigate the interference of bowel loops was also one of the intended technical advances for the second-generation ExAblate device. In that design, selective transducer elements can be disabled, thereby reshaping the sonication beam to avoid passage through critical structures. (Personal Communication, Doris Schechter, MD, Medical Director, InSightec Ltd., July 2014).
Abdominal scars, such as those from Caesarean section, have a fibrotic rather than vascular nature which can attenuate the ultrasound beam when it passes through. Various surface patches and films have been applied to the skin to address this limitation. (68;69) In the Zaher et al study, (69) 25 women had their transverse abdominal scars painted with a solution mixture of nail varnish and MR-certified intravenous contrast agent containing paramagnetic iron oxide particles which then enabled marking on the MR image by the ExAblate software. Patients were either positioned on the table to avoid the beam having to pass through the scar or the beam was altered or angled. All patients successfully underwent MRgHIFU treatment, and an average non-perfused volume (NPV) ratio of 64% ± 16% was achieved. None of the sonications passed through the scars, no patients reported skin pain during the procedure, and after the procedure there were no incidences of skin changes or redness.
In the Yoon et al study, (68) abdominal scars in 20 consecutive premenopausal women were covered by a patch consisting of polyethylene foam covered with a double-sided medical tape on one side. The patch was water resistant, visible on MR images, easily attached to various scar shapes, and did not result in skin heating beyond 39°C. Thermal ablation was achieved if the patch did not block more than 20% of the ultrasound beam. In this study, an average NPV ratio of 54% ± 3.5% was achieved and all cases needed only 1 procedure. The average number of sonications per treatment was 74 ± 25 and only 1 patient was treated without any sonication through the patch. On average, 57% of the sonications passed through the scar patch. In 2 cases, first-degree skin burns were detected but disappeared without intervention within 1 week. The scar patch, however, is not FDA approved but can be used in countries where CE (European Commission) approval is accepted. (Personal Communication, Doris Schechter, MD, Medical Director, InSightec Ltd., September 2014)
At the beginning of MRgHIFU use, because of safety concerns for unintentional heating outside the targeted fibroids, limits were placed on the margins of the planned treatment area: a 5-mm margin from the fibroid capsule and 15-mm margins from the endometrium (inner uterine layer) and the serosal surface (outer uterine layer). These restrictions often resulted in a large surface of the fibroid being untreated, increasing the need for a retreatment. Currently, only a 10-mm margin from the serosa must be preserved. (Personal Communication, Doris Schechter, MD, Medical Director, InSightec Ltd., September 2014) At one centre, the institutional review board did not specify the safety margins and left the decision to the discretion of the treating physician. (70) The actual distance between the serosal lining and the sonication edge was measured in 83 patients treated at that institution. A total number of 8,231 sonications (94 per treatment, on average) were examined and on average 79% were less than 15 mm from the serosa and 37% were less than 10 mm. The authors also stressed that during the procedure, real-time continual MR thermal and anatomical images were carefully examined to identify movement by the patient or organs that might increase risk and to ensure that adequate distances between the uterus and other sensitive structures were maintained with the reduced thermal safety margins. No serious adverse events occurred, although 1 patient had transient sciatic neuralgia resulting from a disc herniation that was determined to be unrelated to MRgHIFU.
Some effort has been directed at changing the characteristics of the fibroid—reducing the size and/or vascularity of the tumour—through the prior use of gonadotropin-releasing hormone analogue (GnRHa) therapy. Funaki et al (71–73) demonstrated in earlier studies that the effectiveness of MRgHIFU was related to the vascularity of the fibroid, determined at baseline by the T2-weighted MR signal characteristics of fibroids. The authors defined 3 classes of fibroids, based on signal intensities: type 1, low signal intensity comparable to skeletal muscle; type 2, lower intensity than myometrium and higher than skeletal muscle; and type 3, equal or higher intensity than myometrium. (72) A type 3 fibroid (high-intensity signal) indicates vascularization, fluid rich tissues, or degeneration of the tumour. It is more difficult to obtain sufficiently high temperatures to ablate tissues in vascular tumours as blood flow tends to transport energy. In these studies, type 1 and type 2 fibroids had significantly larger treated areas compared to type 3 fibroids, and all of the fibroids that had decreased markedly in size on follow-up were types 1 or 2. The reintervention rate was higher for type 3 compared to type 1 or 2 fibroids at 12-month (21.6% vs. 2.9%) and 24-month (21.6% vs. 14.0%) follow-up. (73)
GnRHa, which induces a hypogonadotropic state, has often been used to shrink fibroids, but the therapy has generally been used as an adjunct to surgery rather than a stand-alone therapy because fibroids typically re-grow to their original size after the injections stop. (74;75) Pretreatment with GnRHa has been shown to decrease the diameter of fibroid arterioles and induce arteriosclerotic fibrotic changes, essentially reducing the vascularity of the fibroid. (76) In a study by Smart et al, (77) 27 women with large fibroids in excess of 10 cm in diameter were pretreated over 3 months with 3 courses of GnRHa injections prior to MRgHIFU. The pretreatment resulted in an average uterine volume reduction of 45% and an average target fibroid reduction of 36%. All but 8 women were successfully treated with MRgHIFU treatment. Compared to a control group not receiving GnRHa, the intervention group required the delivery of less mean energy to produce a greater mean NPV; the mean NPV per joule in the treated group was half that of the control group.
Clinical Trials Investigating MRgHIFU Eligibility
Investigators from 3 countries—the United States, (78;79) Germany, (80) and the United Kingdom (81)— performed studies to evaluate the degree of eligibility of women with symptomatic uterine fibroids referred to their centres for MRgHIFU treatment. Their estimates of the proportion of women eligible for MRgHIFU ranged from 14% to 74% (Table 5).
Table 5:
Patient Eligibility for MRgHIFU Treatment of Uterine Fibroids
| Author, Year | Country, Institute | Enrolment Period | Study Group | Clinically and Technically Eligible, % (n) |
|---|---|---|---|---|
| Arleo E et al, 2007 (78) | United States, New York Presbyterian Hospital | April to December 2005 | 333 women inquiring about minimally invasive treatment options for uterine fibroids | 14% (47/333) |
| Behera M et al, 2010 (79) | United States, Duke University Medical Center | November 2007 to February 2009 | 169 women referred for requesting HIFU for uterine fibroids | 16% (27/169) |
| Froling V et al, 2014 (80) | Germany, Charite University Hospital | July 2001 to July 2012 | 783 women applying for UAE and evaluated for MRgHIFU as well as UAE | 39% (276/710) |
| Zaher S et al, 2009 (81) | United Kingdom, St Mary's Hospital | September 2005 to December 2006 | 100 who chose MRgHIFU, of 144 women attending a fibroid clinic in search of minimally invasive treatment options | 74% (74/100) |
Abbreviations: HIFU, high-intensity focused ultrasound; MRgHIFU, magnetic resonance-guided high-intensity focused ultrasound; UAE, uterine artery embolization.
The 14% (78) and 16% (79) treatment eligibility rates reported for the American sites were much lower than for the European sites. The Arleo E et al (78) study was subjected to additional institutional restrictions, which limited treatment to women over 40 and under 60 years of age. Their centre also did not consider any mitigation strategies for anatomical restrictions.
The Froling et al study (80) in Germany reported on the comparative eligibility of women with symptomatic uterine fibroids for either MRgHIFU or uterine artery embolization (UAE), a minimally invasive treatment option for uterine fibroids. The few exclusions for UAE included infarcted fibroids, pedunculated fibroids, and aberrant blood vessel supply. For MRgHIFU, a broad range of technical criteria were used, although the most common were bowel interference in the pathway of the ultrasound beam, high numbers of fibroids, and proximity of fibroids to other critical anatomy. Almost all of the women (99%) were eligible for UAE treatment, whereas only 39% were found to be eligible for MRgHIFU.
The United Kingdom centre reporting the highest eligibility (74%) employed mitigation strategies to decrease the screening failure rate. (81) The high eligibility rate was achieved by pretreating patients (88%; 65/74) with GnRHa for 3 months to both reduce the fibroid size and decrease its vascularity, thereby potentially improving responses to thermal ablation. In addition, the patient's desire for future fertility was not a contraindication to MRgHIFU in Europe at that time and therefore was not an exclusion criterion for treatment. The only indications for exclusion were reported to be abdominal scarring, other uterine pathology (adenomyosis), and bowel occlusion of the acoustic window.
Section B. Technical Success
The technical success of MRgHIFU relates to the ability of the operator to deliver the degree or number of sonications in order to deliver the intended amount of thermal energy to the target region. This process also depends on continual real-time monitoring and accurate feedback control to produce consistency in the ablation zone. Interrupting or terminating the procedure, either due to a signal by the patient or overrides by the operator or the device, is considered a technical failure. Completing a procedure in 2 scheduled sessions due to fibroid size is not considered a failure. The non-perfused volume (NPV) of the fibroid, an automated measurement taken by MR imaging immediately before and after the procedure, is cited as a measure of the degree of ablation of the fibroid and is used as a measure of technical success.
At the end of the procedure, T1-weighted contrast-enhanced MR images are used to inspect the non-enhancing regions, which correspond to an absence of blood perfusion in the regions. The actual amount of tissue ablation needed to result in cell death and coagulative necrosis is unknown, but based on experience with other ablation techniques, as close to 100% would be desirable due to the potential for regrowth and the need for reintervention with partial ablation. The optimal NPV for MRgHIFU has been variably defined. Park et al (82) cite an NPV of 80% as a practical and achievable goal of HIFU treatment, whereas others (83) have cited a 60% NPV as a measure of technical success, as this outcome was linked with a less than 15% need for reintervention within a 24-month follow-up.
Several early reports evaluated technical proof-of-concept with the ExAblate MRgHIFU device, (84) which uses a point-by-point ablation technique, as well as the Sonalleve MRgHIFU device, (85) which employs a volumetric-based ablation strategy. The study objective and protocol were intended to evaluate the ability of operators to successfully ablate only the target areas without damaging non-target areas. The multicentre regulatory trial in the United States initially evaluated MRgHIFU with the ExAblate device at 5 different sites; 3 sites involved a hysterectomy protocol where hysterectomy was to be performed within a month following MRgHIFU, and 2 sites involved an observation protocol where hysterectomy was an elective decision made a month after MRgHIFU. (84) HIFU treatment protocols were restricted by the regulatory agency and involved restricting the size of fibroids (< 10 cm), limiting procedure duration to 2 hours or less, and limiting the degree of the ablation; as well, typically only 1 fibroid, the suspected symptomatic one, was targeted.
The proof-of-concept results were presented in 2 reports, 1 for the 9 women receiving MRgHIFU in the hysterectomy protocol group at Brigham and Women's Hospital (86) and 1 for the 35 women at the Sheba and the Hadassah Medical Centers in Israel (87) where an observation protocol followed MRgHIFU. In the hysterectomy protocol group, 6 of the 9 patients received focused ultrasound, and in 3 patients the treatment plan could not be fully executed. Eight of the 9 women underwent hysterectomy. (86) In general, focal necrotic lesions were demonstrated by MR in all cases and pathologically confirmed. The MR images of necrosis and hemorrhage, when compared with gross histopathological changes, tended to underestimate the actual pathologic volumes. In the observation protocol study group, 83% (29/35) of the symptomatic women scheduled for hysterectomy and followed up by expectant management for 6 months chose not to undergo hysterectomy because their symptoms abated. (87) Six of the women (17%) underwent hysterectomy because their symptoms did not improve.
The tumour-targeting accuracy of another MRgHIFU device, the Sonalleve, was also investigated with protocols involving MRgHIFU followed by hysterectomy within 1 month at 2 American sites (11 women in total): the NIH Center for Interventional Oncology in Maryland and St Luke's Episcopal Hospital in Houston. (85) The Sonalleve also uses a different ablation technique, known as volumetric ablation, which purports to be a more energy efficient mechanism than the point-by-point ablation technique of the ExAblate device. Of the 11 women, 9 underwent hysterectomy and, in 8 of these cases, coagulative necrosis in the targeted location was verified at histology. In 1 patient there was an additional focus of hemorrhagic necrosis within the myometrium and adjacent to a small submucosal fibroid. During that procedure, patient movement was noted on MR and the patient, experiencing pain, pressed the stop button. However, in general, comparisons between MR and pathology are limited by challenges associated with matching imaging to gross pathology planes and relating observed volumes of transected fibroids at pathology to volumes based on estimates from MR imaging.
Technical Success in Clinical Trials
The degree of technical success for MRgHIFU was reported in 13 clinical cohort studies, 6 involving restricted ablation strategies and 7 involving protocols that allowed complete or near-complete ablation strategies. Three of the reports (42;88;89) involved the Sonalleve device; 10 studied the ExAblate device. Table 6 lists the technical success rates, reasons for failures, and the mitigation strategies employed to decrease technical failures for studies, grouped by ablation protocols (restricted or near complete).
Table 6:
Technical Success of MRgHIFU Treatment for Uterine Fibroids
| Country, Institute, Author, Year | NPV, % Mean ± SD,(range) | Mitigation Strategies | Technical Success, % (n) | Reasons for Technical Failure |
|---|---|---|---|---|
| Restricted Ablation Protocols | ||||
| Israel, Sheba Medical Center, Machtinger R et al, 2012 (92) | 41 ± 21 (10–100) | None reported | 92 (80/87) | Bowel obstructing sonications (n = 2); patient discomfort (n = 2); menopausal: treated but excluded (n = 1) |
| Israel, Sheba Medical Center, Rabinovici J et al, 2007 (87) | 31 ± 23 (2–92) | None reported | 89 (31/35) | Early cessation of treatment (n = 4) |
| Korea, Samsung Medical Center, Park MJ et al, 2013 (89) | 57 ± 26 (0.6–100) | Bladder filling (saline) to avoid scars or small bowel loops (n = 7), bladder and rectal filling (ultrasound gel) to move small bowel loops out of sonication field (n = 1) | 98 (42/43) | Early cessation due to unexpected and severe pelvic pain (n = 1) |
| Netherlands, University Medical Center Utrecht, Voogt M et al, 2012 (42) | 22 (0–66) | None reported | 94 (31/33) | Insufficient heating of fibroid and underwent UAE within 1 week (n=1); underwent surgical removal of fibroid for unknown reason (n = 1) |
| United States, Mayo Clinic, Hesley G et al, 2006 (93) | NR | None reported | 95 (40/42) | Inadequate number of sonications due to discomfort (n=2) |
| Multinational, 5 sites (United States, Germany, United Kingdom, Israel), Stewart E et al, 2003 (84) | 25 | None reported | 76 (42/55) | Presence of bowel in sonication pathway (n=3); less energy delivered than intended, due to inability to visualize the low energy test pulse, resulting in no sonication (related to tissue aberrations of abdominal wall such as surgical scars or inhomogeneous fat and muscle deposition in abdominal wall) (n = 10) |
| Near-Complete Ablation Protocols | ||||
| Australia, Royal Women's Hospital, Dobrotwir A and Pun E, 2012 (94) | 67 ± 25 (0–100) | Patients pretreated with GnRHa (n = 7) | 100 (100/100) | No failures |
| Germany, Klinikum der Ludwig-Maximilians, Trumm C et al, 2013 (91) | 88 ± 15 (38–100) | Patient positioning: rectal filling (ultrasound gel) (n = 64), temporary filling of bladder (sterile water) (n = 51), or both (n = 48), scar patch or tilting transducer to avoid abdominal scars | 93 (115/123) | Bowel in beam pathway (could not be mitigated by modifying the transducer or patient positioning either by bladder and/or rectal filling (n = 6); continuous patient movement (n = 1); system malfunction (n = 1) |
| India, Jaslok Hospital and Research Center, Desai S et al, 2012 (95) | 88 ± 6 | None used; patients with bowel in beam excluded | 100 (50/50) | No failures, excluded risk cases; noted that 20 patients had a second treatment and 1 patient had 3 treatments. |
| Korea, Samsung Medical Center, Kim YS et al, 2014 (88) | 68 ± 26 | Prior GnRHa administration (n = 6), bladder filling (n = 15), rectal filling (n = 14), or both bladder and rectal filling | 94 (67/71) | Inability to achieve high temperature even with highest acoustic power (n = 3); complication (n = 1) |
| Japan, Tokyo, Itabashi Chuo Medical Center, Morita Y et al, 2008 (96) | 60 ± 18 (22–100) | None reported | 100 (48/48) | Required a second procedure because of large fibroids (n = 5) |
| Japan, Osaka, Osaka Kinki University School of Medicine Mikami K et al, 2008 (90) | 47 (25–72) | None reported | 67 (32/48) | Incomplete ablation due to severe pain during sonication (n = 16) |
| United States, Mayo Clinic, Gorny K et al, 2011 (97) | 45 ± 23 (0–100) | None reported | 96 (130/136) | 6 failures: 3 failed in the first procedure (incomplete due to pain) and 3 failed in the second treatment (could not tolerate another 3-hour prone position); 59 patients had 2 sessions on consecutive days |
Abbreviations: GnRHa, gonadotropin-releasing hormone analogue; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NPV, non-perfused volume; UAE, uterine artery embolization.
The mean technical success was 93.3% in the studies involving restricted ablation and 94.1% in those involving near-complete ablation. Without the 1 outlier report in each group, the technical success was generally higher in the near-complete ablation group, ranging from 93% to 100%, compared to 89% to 95% in the restricted ablation group. The 2 outlier studies reporting low technical results involved different reasons for technical failures. In the Stewart et al report, (84) the study was based on their early experience with MRgHIFU in which they report a range of anatomic limitations involving bowel obstruction in the ultrasound beam pathway and aberrations in the abdominal wall. In addition, few if any mitigation strategies were employed at that time. In the report by Mikami et al, (90) also based on early experience but without a restriction on the degree of intended ablation, the main reason for their 33% rate of technical failure was the unmanaged skin pain experienced by the patients during the sonication procedure. They noted that all of the 32 patients in the technical success group had fibroids with baseline low MR signal intensity, whereas 9 of the 16 patients in the failure group had fibroids with high MR signal intensity, reflecting more vascular tumors.
One of the studies involved the use of the second-generation ExAblate 2100 device. (91) Some of the advanced features with this device include elevation of the transducer closer to the skin, thereby reducing energy density in the near and far field; decreased average focal distance with an increase in maximum energy to allow for greater spot sizes and potentially quicker treatment; automatic disabling of selective transducer elements by the operating system in case risk structures are in the beam pathway; and automatic detection of patient movement and subsequent treatment correction (Personal Communication, Doris Schechter, MD, Medical Director, InSightec Ltd., July 2014) Despite these advances and even with mitigation strategies, the procedure remained technically unsuccessful in 7% (8/123) of the patients.
Section C. Safety
This safety review considered multiple sources of information including case reports of adverse events and incident reports published on-line in national safety databases such as the FDA's Manufacturer and User Facility Device Experience Database (MAUDE) in the United States and Health Canada's Medical Device Problem Reports. We also reviewed adverse events reported in 2008 by physicians providing MRgHIFU and attending the first international symposium dedicated to MRgHIFU. (64) Complications reported in any clinical cohort or comparative cohort studies were also reviewed and were evaluated as minor or major based on the standards defined by the Society of Interventional Radiology (SIR) Standards of Practice Committee Classification of Outcomes. (98) Major complications were defined as those requiring therapy or minor hospitalization (< 48 hours); requiring major therapy, unplanned increase in the level of care, or prolonged hospitalization (> 48 hours); having permanent adverse sequelae; or resulting in death.
Three case reports involving complications following MRgHIFU were identified (Table 7). (99–101) One of these events, (100) the discharge of ablated fibroid tissue, has not always been classified as a complication after an embolization or ablative process but more as a natural consequence of the procedure (the body expelling ablated or dead tissue). The second report involved the treatment of unsuspected leiomyosarcoma, which was detected at laparoscopic myomectomy after the fibroid symptoms did not adequately resolve with HIFU. (99) This report raises several issues. First, the risk that the target fibroid is an unsuspected malignant tumour has been estimated to be low: 1 in 352 surgeries for uterine sarcoma and 1 in 498 surgeries for leiomyosarcoma. (102) Even though the risk is low, patients failing ablation therapies should be followed closely not only to ensure timely treatment but also to investigate for potential malignancy. Second, the FDA has recently raised concerns with the surgical treatment of uterine fibroids, namely the use of power morcellation either with myomectomy or hysterectomy, as there is a potential seeding or spreading of an unsuspected leiomyosarcoma or sarcoma. On April 17, 2014, the FDA issued a safety warning discouraging the use of laparoscopic power morcellation for uterine fibroids. (103)
Table 7:
Case Reports of Complications Following MRgHIFU Treatment for Uterine Fibroids
| Author, Year, Country | Adverse Event | Case Detail |
|---|---|---|
| Kim KA et al, 2011 (100) Korea | Spontaneous vaginal expulsion of uterine fibroid | 38-year-old woman with severe menorrhagia and resultant anemia underwent HIFU with an NPV ratio of 80%, and 2 weeks post underwent hysteroscopic resection for an incompletely discharged fibroid mass without adverse events. |
| Fukunishi H et al, 2007 (99) Japan | Unsuspected uterine leiomyosarcoma treated | 40-year-old woman with menorrhagia and a 9-cm mass on the anterior uterine wall underwent HIFU with an NPV of 25%, after which symptoms resolved for a time but returned within 6 months. The tumour was morcellated by laparoscopic myomectomy, and leiomyosarcoma coexistent with degenerated fibroid was confirmed at histology. Subsequently the patient underwent definitive surgery (Wertheim operation with lymphadenectomy) without adjuvant chemotherapy and remained in good health 16 months following HIFU. |
| Leon-Villapolis J et al, 2005 (101) United Kingdom | Full thickness abdominal skin burn | 39-year-old woman underwent HIFU and 2 weeks post developed a small area of hyperintensity close to the abdominal skin burn sites within the left rectus muscle initially treated with Flamazine dressing. No MR abnormalities were reported for the subcutaneous fat or muscle fascia. After the patient was referred to a burn centre, a full-thickness skin burn down to the abdominal fascia causing localized areas of subcutaneous fat necrosis was identified. The patient was hospitalized for a day and underwent surgery in which the burn areas were treated by excision as an ellipse and direct closure. |
Abbreviations: HIFU, high-intensity focused ultrasound; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NPV, non-perfusion volume
The third case report involved a full-thickness abdominal skin burn, a unique complication directly related to HIFU technology. (101) Third-degree burns are considered a major adverse event of MRgHIFU, unlike first- and second-degree skin burns, which are more common. The authors also noted that the degree of the burn in the case reported was unappreciated on MR, suggesting that any skin burn should be closely followed.
Adverse event reports from the FDA's MAUDE database for January 1, 2004, to October 31, 2008, were accessed on April 24, 2014. None were reported in Health Canada's Medical Device Problem Reporting database for the same period, likely reflecting the limited use of HIFU interventions for uterine fibroids in clinical trials or commercial settings in Canada. In the MAUDE database, 8 major adverse events (7 reported by company medical personnel) were reported over a 7-year period, 2007 to 2013 (2007, n = 1; 2008, n = 2; 2009, n = 3; 2012, n = 1; 2013, n = 1) (Table 8).
Table 8:
Adverse Events With MRgHIFU Treatment for Uterine Fibroids, From FDA MAUDE Database
| Event Date | Report Source, Reporter | Event | Outcome | Causation |
|---|---|---|---|---|
| Dec 12, 2012 | Manufacturer, physician | First- or second-degree abdominal skin burn | Hospitalization and uneventful surgical resection of burned abdominal tissue | Physician error |
| Nov 20, 2009 | Manufacturer, biomedical engineer | Failure of the console stop-sonication mechanism | Not an adverse event but the manufacturer sent an application note to all sites to test the stop-sonication button during power-up as a routine QA activity | Potential device malfunction |
| Sep 17, 2013 | Manufacturer, physician | Patient death | Cardiac arrest immediately following the procedure and successfully resuscitated. Her hemoglobin dropped from 10.8 gm/dl before treatment to approx. 3 gm/dl and improved following blood expanders, but a second cardiac arrest occurred and resuscitation was unsuccessful. | Uncertain; device technically intact and functioning within specifications and no device malfunctions; treatment appropriate. The institution did not have next-of-kin authorization to share medical records. |
| Sep 15, 2009 | Manufacturer, company representative | Potential issue detected in-house where certain modified ExAblate 2000 units could malfunction in that the system fails to correctly display the frequency spectrum during sonication | No adverse events occurred but instructions on maintaining safety margins of 10 mm from the serosa were repeated. | Potential device malfunction |
| Jan 1, 2009 | Voluntary, patient | Uterine carcinoma diagnosed within 1 year of HIFU | Patient had a hysterectomy and cancer was at an early stage. | Unrelated |
| Jul, 29, 2008 | Manufacturer, physician | 2 weeks after HIFU a bladder wall ulceration was diagnosed by a urologist | Patient was discharged after a 2-day hospitalization in which she received hemostatic interventions which stopped the bleeding. | Physician error |
| Jan 24, 2008 | Manufacturer, physician | Due to considerable undetected uterine motion during a large part of the treatment, sonication of structures outside the uterus resulted in nerve injury (14 and 15 nerve roots) in the right lumbosacral plexus and a bowel perforation: 2 in the ileum region and 1 in the sigmoid colon. | Hospitalized emergently for 9 days and, due to right foot weakness, was unable to walk without an aid; a rehabilitation assessment projected a 3-month recovery period. The patient underwent successful surgery for bowel perforations at another hospital. | Physician error |
| Jan 19, 2007 | Manufacturer, physician | Patient movement during sonication was undetected due to the inadequate use of fiducials (markers), leading to sonication of the bowel | Patient was hospitalized and underwent successful surgery for bowel repair. | Physician error |
Abbreviations: FDA, Food and Drug Administration; HIFU, high-intensity focused ultrasound; MAUDE, Manufacturer and User Facility Device Experience Database; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; QA, quality assurance.
One of the reports was from a patient and involved the detection of an unsuspected uterine carcinoma following HIFU. (This event was discussed earlier in a case report.) Two other reports involved potential device malfunctions that were reviewed by the company, which responded by mitigation activities and forwarding of application (voluntary advisory) letters to clients. Three other reports involved thermal injuries (all requiring hospitalization and interventions) to the abdominal skin, bladder, or bowel, and 1 case involved multiple thermal injuries to the 14 and 15 nerve roots and multiple perforations in the bowel and bladder. One death, occurring in 2013, was reported in the database. In that case, the patient experienced a rapid decline in hemoglobin and a cardiac arrest immediately following MRgHIFU; unfortunately the institute did not have next-of-kin authority to release medical records, and therefore more complete clinical information on this case was not available.
Physicians (interventional radiologists and gynecologists) providing MRgHIFU and attending the first international symposium in 2008 dedicated to MRgHIFU reported on their experiences of adverse events in their practices. Six were in academic settings and 7 in private practices. (64) The majority reported using MRgHIFU for more than 2 years and treating 3 patients per month, on average. The symposium participants reported 17 adverse events including neuropathies (n = 5), first- or second-degree skin burns (n = 4), emergency hysterectomy (n = 2), abdominal wall edemas (n = 2), bowel injury (n = 1), bladder injury (n = 1), DVT (n = 1), and fat necrosis (n = 1). No deaths were reported.
Adverse events reported by investigators in 21 clinical cohort studies of MRgHIFU for uterine fibroids are detailed in Table 9, grouped by ablation strategies that were restricted and generally involved early experiences (Table 9A) and ablation strategies that involved complete or near-complete protocols (Table 9B). Minor procedural complications were commonly reported in these clinical cohort studies and included abdominal skin irritation, redness, burns or ulceration, and discomfort or pain in various regions such as the abdomen, leg, and back. Generalized constitutional symptoms involving low-grade fevers, chills, fatigue, or malaise were reported in 2 studies (42;82) and were similar to symptoms following UAE, a self-limiting condition referred to as post-embolization syndrome. (104) Spontaneous abnormal vaginal discharge of fibroid materials was also reported to occur after MRgHIFU (82;105;106) and was similar to the events of fibroid discharge reported after UAE. (104) As noted above, this event has generally not been characterized as a complication but as a natural reaction of the body to expel necrotic tissue. However, if the tissue does not discharge naturally or cannot be easily removed but requires additional surgeries, or if the product resulted in infection, then the event would be considered a complication. One study reported that a patient was admitted to the emergency department for hysteroscopic myomectomy for a discharged fibroid after MRgHIFU. (92)
Table 9A:
Adverse Events Reported in Clinical Studies of MRgHIFU With Restricted Ablation Protocols for Uterine Fibroids
| Country, Author, Year | Study Size, Follow-up | NPV, % Mean ± SD, (range) | Minor Complications | Major Complications |
|---|---|---|---|---|
| Israel, Machtinger | 81 women | 41 ± 21 | N = 8 | N = 2 |
| R et al, 2012 (92) | 6 months | (10–100) | First-degree burn (n = 3), fever >38° C (n = 1), back pain (n = 2), leg pain (n = 2) | Fever, abdominal pain, leukocytosis, and hospitalized for antibiotics (n = 1); fibroid discharge and admitted to ED for hysteroscopic myomectomy (n = 1) |
| Israel, Rabinovici | 35 women | 31 ± 23 | N = 2+ | None reported |
| J et al, 2007 (87) | 6 months | (2–92) | Abdominal skin burn subsiding in 2 weeks (n = 1), sciatica pain subsiding within a week (n = 1), lower abdominal pain subsiding shortly after HIFU (several women, number not specified) | |
| Korea, Yoon S-W | 60 women | 40 ± 20 | N = 3 | None reported |
| et al, 2013 (111) | 12 months | (0–92) | Skin burn resolving within 2 weeks (n = 2), pelvic pain lasting up to 1 month possible exacerbation of thoracic spinal fusion from prolonged immobilization (n = 1) | |
| Korea, Park MJ et | 43 women | 57 ± 26 | N = 2 | N = 5 |
| al, 2013 (89) | 3 months | (1–100) | First-degree burn (n = 1), Foley catheterization-related cystitis symptoms (n = 1) | Unexplained severe pelvic pain terminating the procedure (n = 1), thermal injury to abdominal wall muscle and subcutaneous fat by increased contrast enhancement (n = 3), leg numbness persisting up to 1 month (n = 1) |
| Netherlands, | 33 women | 22 | N = 85 (31 patients; mean AE, 2.6) | N = 3 |
| Voogt M et al, 2012 (42) | 1 month | (0–66) | Pain (abdominal [n = 17], positional-related [n = 10], sonication-related [n = 7], sciatic nerve [n=1], abdominal discomfort [n = 13], urinary pain/difficulty [n=7]), post-HIFU vaginal bleeding (n = 3), hematuria (n = 1), vaginal irritation (n = 1), generalized system (fatigue [n = 6], headache [n = 4], fever > 38°C [n = 3], nausea [n = 3], skin irritation [n = 3], other unspecified [n = 6]) | Sciatic nerve pain resolving after 139 days (n = 1), leg pain resolving after 93 days (n = 1), surgical removal of fibroids at another site within 1 week post-HIFU for unknown reason (n = 1) |
| Netherlands, Ikink | 51 women | 40 ± 22 | N = 2+ | None reported |
| M et al, 2013 (112) | 6 months | Common (numbers not specified) symptoms during procedure included lower abdominal heat, back pain, and referred leg pain. First-degree skin burns adequately treated with conservative treatment (n = 2) | ||
| United States, | 42 women | NR | N = 6 | N = 2 |
| Mayo Clinic, Hesley G et al, 2006 (93) | 6 months | Diarrhea (n = 3), passage blood/mucus (n = 2), sciatic nerve-related pain gradually resolving over 12 months (n = 1) | DVT in right common femoral vein after repeat HIFU, treated by anti-coagulation therapy (n = 1), sciatic nerve-related pain gradually resolving over 12 months (n = 1) | |
| United States, | 109 women | 25 | N = 57 | N = 8 |
| Brigham and Women's Hospital (7 sites), Hindley J et al, 2004 (109) | 6 months | Moderate or severe pain during the procedure (n = 49), moderate or severe pain after the procedure (n = 8), overall moderate or severe discomfort during the procedure (n = 37) | Overnight hospital admission for severe nausea (n = 1), continued heavy menses following treatment requiring blood transfusions (n = 5), urinary tract infection requiring hospitalization 2 weeks after treatment (n = 1), sciatic nerve palsy with numbness and weakness resolving by 12-month follow-up (n = 1) | |
| United States, Brigham and Women's Hospital (5 sites), Fennessy F et al, 2007 (49) | 88 women, (early protocol) 44 women, (later protocol) | 17 ± 16 26 ± 22 | Overall, 87% reported AEs. Pain or discomfort related to position or sonication (54%) Overall 75% reported AEs. Pain or discomfort related to position or sonication (47%) | N = 2 Parasthesia at the site of intravenous cannula resolving within 6 weeks (n = 1), sonication-related leg pain resolving within 2 days and reported to the FDA (n=1) None reported |
| United States, | 122 women | 41 ± 25 | N = 128 | None reported |
| Brigham and Women's Hospital (9 sites) Machtinger R et al, 2013 (107) | (63 African American [AA] and 59 non-AA) 12 months | (AA) 30 ± 24 (non-AA) | Back/leg pain (21.9%), abdominal cramping (21.1%), urinary tract infection/irritation (11.7%), gastrointestinal complaints (11.7%), skin irritation (7.0%), vaginal bleeding or discharge (6.3%) |
Abbreviations: AE, adverse event; DVT, deep venous thrombosis; ED, emergency department; FDA, Food and Drug Administration; HIFU, high-intensity focused ultrasound; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NPV, non-perfused volume; SD, standard deviation.
Table 9B:
Adverse Events Reported in Clinical Studies of MRgHIFU With Complete or Near-Complete Ablation Protocols for Uterine Fibroids
| Country, Author, Year | Study Size, Follow-Up | NPV, % Mean ± SD, (range) | Minor Complications | Major Complications |
|---|---|---|---|---|
| Australia, Dobrotwir A et al, 2012 (94) | 100 women 2 years | 67 ± 25 (0–100) | N (unspecified) Pain 1 to 2 weeks following HIFU, minor vaginal bleeding or spotting | None reported (no overnight admissions required) |
| Germany, Trumm C et al, 2013 (91) | 115 women 6 months | 88 ± 15 (38–100) | N = 2 First-degree skin burn, skin erythema and blistering, with 4,600 joules, well under 7,100 joules maximum limit (n = 2) | None reported |
| India, Desai S et al, 2012 (95) | 50 women 6 months | 88 ± 6 | N = 14 Leg pain (n = 10, 9 resolving and 1 unresolved at 6 month follow-up), urinary tract infection (n = 1), urine retention (n = 1), skin blister (n = 1), abdominal pain (n = 1) | None reported |
| India, Himabindu Y et al, 2014 (105) | 32 women 6 months | 70 | N = 5 Blisters in abdominal wall subsiding within a week (n = 1), leukorrhea (vaginal discharge) subsiding within 2 weeks (n = 4) | None reported |
| Korea, Park MJ et al, 2014 (82) | 79 women 3 months | 63 ± 26 (1–100) | N = 45 Non-target ablation as indicated by abnormally increased contrast enhancement of abdominal wall muscle or subcutaneous fat layer (n = 9), abnormal vaginal discharge and abdominal bloating (n = 2), nausea lasting for < 1 hour (n = 1), mild pelvic pain resolving within 3 days (n = 19), constitutional symptoms (low-grade fevers, chills and/or malaise) regarded as post-ablation syndrome (n = 12), first-degree skin burns (n = 2), Foley catheterization-related cystitis (n = 1) | N = 1 Sciatic nerve-related leg numbness resolving within 30 days |
| Korea, Kim Y-S et al, 2014 (88) | 71 women 3 months | 68 ± 26 (2–100) | N = 7 Abdominal wall thermal injury (n = 5), cystitis (n = 1), transient gross hematuria (n = 1) | N = 1 Second-degree burn in right inguinal area |
| Japan, Okada A et al, 2009 (106) | 144 women (early protocol) | 39 ± 24 (1–91) | N = 55 Abdominal pain (n = 17), lower back or leg pain (n = 9), vaginal discharge or bleeding (n = 12), fever (n = 7), skin burns (n = 10) | None reported |
| 143 women (later protocol) | 54 ± 19 (4–100) | N = 49 Abdominal pain (n = 16), lower back or leg pain (n = 11), vaginal discharge or bleeding (n = 11), fever (n = 9), skin burns (n = 2) | None reported | |
| Japan, Tokyo, Morita Y et al, 2008 (96) | 48 women 12 months | 60 ± 18 (22–100) | N = 8 Skin redness (n = 4), transient sciatica neuralgia related to underlying disc herniation at L4-L5 and L5-S1 resolving within a month (n = 1), procedural pain (n = 3) | None reported |
| Japan, Osaka, Mikami K et al, 2008 (90) | 48 women 12 months | 47 (25–72) | N = 6 Skin burns: first-degree (n=3), second-degree (n = 3) | None reported |
| United States, Mayo Clinic, Gorny K et al, 2011 (97) | 150 women 12 months | 45 ± 23 (0–100) | N = 22 (17 women) Edema in various regions in 11 women (mild abdominal edema [n = 11], subcutaneous fat edema [n = 8], subcutaneous and abdominal muscle edema [n = 2], subcutaneous fat edema and skin erythema [n = 1]), lower back discomfort (n = 5) with 3 reporting pain and 2 reporting sciatica involving numbness and temporary decrease in strength | N = 1 DVT treated with anti-coagulation therapy |
| United States, University Imaging-Guidance Center, Florida, LeBlang S et al, 2010 (43) | 80 women 6 months | 55 ± 25 | N = 3 First-degree skin burns (n = 2), mild sciatica (n = 1), all resolving within 6 weeks | N = 1 Endometritis and yeast infection 6 weeks following HIFU, managed by hysterectomy |
Abbreviations: DVT, deep venous thrombosis; HIFU, high-intensity focused ultrasound; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NPV, non-perfused volume; SD, standard deviation.
The safety experiences reported in the clinical trials represent women from many countries. The Machtinger et al (107) report was the only one to compare outcomes between different racial groups (African American and non–African American women) undergoing HIFU within the same study. In that study, non–African American women reported more complications (80% reported at least 1 complication; 47/59) than African American women (29%; 18/63), although all adverse events were minor. No major complications were reported in the study for either group.
HIFU treatments require a combination of conscious sedation and analgesia. (108) The effect of the procedure is to destroy fibroid tissue by inducing coagulative necrosis, which creates edema, swelling, and immediate mild to severe pain. The need to manage pain during the procedure, however, must be balanced by the need for patients to be able to communicate with the operator and to use stop buttons to abort the procedure if pain is intolerable. This action by patients may reflect individual pain tolerances but may also indicate unintended, non-target thermal effects. In the clinical cohort studies, the protocols for pain management during the HIFU procedure were varied and in general also involved different regimens for conscious sedation.
In 1 report, the majority of patients received intravenous opioids (88%; 38/43) to control pain in various regions: abdomen or pelvis (n = 23), sacrococcygeal or lower back (n = 9), or leg (n = 6). (89) In a multicentre trial involving practices in 4 countries (England, Germany, Israel, and the United States), pain and discomfort were systematically assessed for patients undergoing MRgHIFU. (109) During the procedure, 49% of patients (53/109) reported experiencing moderate (n = 36) or severe (n=17) pain, and 34% (37/109) reported overall discomfort at moderate (n = 29) or severe (n = 8) levels. Both pain and overall discomfort were significantly reduced immediately after the procedure, but 8% of patients experienced moderate or severe pain after the procedure and 7% reported overall moderate or severe discomfort.
Major complications, as defined by SIR guidelines, were rarely reported in the clinical cohort studies. In the 21 studies involving 1,594 patients, 26 major complications (1.6%) were reported. The rate was found to be higher in the earlier experience where restricted ablation strategies were employed (4.1%; 22/534) (Table 9A) compared to later experience where complete or near-complete ablation strategies were employed (0.4%; 4/1,060) (Table 9B). The major adverse events included deep venous thrombosis; non-target thermal injury such as sciatic nerve palsy or skin burn; transfusions; and rehospitalizations for various conditions including fever, removal of discharging ablated fibroid products, urinary tract infection, endometritis, and yeast infection. Rehospitalization or need for additional care are both criteria for major adverse events; 1 study reported both rates for a 6-month follow-up of 109 women in a multicentre trial: 7% were rehospitalized and 3% required transfusion. (110)
Section D. Treatment Effectiveness
Treatment effectiveness of MRgHIFU is evaluated by the degree of fibroid reduction, subsequent symptom resolution, rate of reintervention for persistent or recurrent symptoms, and the impact on HRQOL. To balance safety with efficacy for MRgHIFU, the FDA initially restricted the duration of the procedure and the degree of ablation that could be targeted, and many of the cohort studies evaluated outcomes under those restrictions, including the pivotal international multicentre trial that gained regulatory approval for the procedure. (83) As discussed previously, the amount of tissue destruction required to relieve symptoms is unknown and the therapeutic intent is generally to reduce mass sufficiently that symptoms are relieved. Measuring fibroids in longitudinal follow-up is also problematic because generally only 1 fibroid is treated and identifying it can be difficult when there are multiple fibroids. For the measure of treatment achieved, most studies reported the NPV value immediately following HIFU, which represents the degree of coagulative necrosis. Only a few studies reported fibroid volume reductions, and those that did reported modest reductions over baseline with short-term follow-up (Table 10). All clinical cohort studies reported symptom reductions; these outcomes are summarized in Tables 11A and 11B.
Table 10:
Fibroid Reduction After MRgHIFU
| Country, Author, Year | Study Size, N | Fibroid Volume, cc, Mean ± SD (range) | ||||
|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | 36 months | ||
| Korea, Yoon S-W et al, 2013 (111) | 60 | 200 ± 16 (17–650) | NR | 150 ± 130 (16–607) | 140 ± 130 (8–524) | |
| Korea, Park M et al, 2013 (89) | 43 | 373 ± 325 | 326 ± 221 | |||
| Netherlands, Ikink M et al, 2013 (112) | 46 | 353 ± 269 | 289 ± 232 | 271 ± 225 | ||
| United States, Brigham and Women's Hospital, Lenard Z et al, 2008 (113) | 66 | 256 ± 202 | NR | 12.6% reduction over baseline | 9.3% reduction over baseline | |
| United States, Johns Hopkins University School of Medicine, Kim H et al, 2011 (114) | 40 | 337 (295–379) | NR | 274 (229–318) | 250 (208–292) | 228 (172–285) |
Abbreviations: MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NR, not reported; SD, standard deviation.
Table 11A:
Fibroid-Related Symptom Reduction With Restricted MRgHIFU Ablation Protocols
| Country, Site, Author, Year | Study Size, N | Symptom Measures | Symptom Reduction at Follow-Up Points | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | 24 months | 36 months | |||
| Korea, CHA Bundang Medical Center, Yoon S-W et al, 2013 (111) | 60 | UFS-QOL (SSS) Mean ± SD | 50 ± 22 | 33 ± 16 P < 0.0001 | NR | 19 ± 12 P < 0.0001 | ||
| Korea, Samsung Medical Center, Park M et al, 2013 (89) | 43 | UFS-QOL (SSS) Mean ± SD (range) | 43 ± 18 (9–81) | 26 ± 12 (6–50) P < 0.001 | ||||
| Netherlands, University Medical Center, Utrecht, Ikink M et al, 2013 (112) | 46 | UFS-QOL (SSS) Mean ± SD (range) | 51 ± 18 | NR | 35 ± 20 P < 0.001 | |||
| United States Mayo Clinic, Hesley G et al 2006 (93) | 42 | Self-reported symptom improvement | See summary in text | |||||
| United States, MCT, Fennessy F et al, 2007 (49) | 160 | UFS-QOL (SSS) Mean ± SD (range) | 62 ± 16 | 36 ± 20 P < 0.001 | 33 ± 20 P < 0.001 | 33 ± 21 P < 0.001 | ||
| United States, Johns Hopkins University School of Medicine, Kim H et al, 2011 (114) | 40 | UFS-QOL (SSS) Mean (95% CI) | 65 (59–71) | 35 (29–41) | 32 (26–38) | 41 (33–49) | 18 (8–28) | 17 (9–25) |
| United States, Brigham and Women's Hospital, Lenard Z et al, 2008 (113) | 66 | UFS-QOL (SSS) Mean ± SD | 62 ± 15 | NR | 34 ± 17 | 38 ± 18 P < 0.001 | ||
| United States, MCT, Machtinger R et al, 2013 (107) | 63 (AA) | UFS-QOL (SSS) Median (IQR) | 69 (50–81) | NR | NR | 33 (13–47) P < 0.0001 | 28 (9–44) | 13 (6–38) |
| 59 (Non-AA) | UFS-QOL (SSS) Median (IQR) | 59 (50–78) | NR | NR | 31 (19–44) P < 0.0001 | 27 (9–44) | 19 (13–41) | |
| United States, Brigham and Women's Hospital (MCT), Stewart E et al, 2006 (110) | 176 | UFS-QOL (SSS) Mean ± SD | 62 ± 15 | 41 ± 22 P < 0.001 | 38 ± 21 P < 0.001 | |||
Abbreviations: AA, African-American; CI, confidence interval; IQR, inter-quartile range; MCT, multicentre trial; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NR, not reported; SD, standard deviation; SSS; symptom severity score; UFS-QOL, Uterine Fibroid Symptom and Quality of Life questionnaire.
Table 11B:
Fibroid-Related Symptom Reduction With Complete or Near-Complete MRgHIFU Ablation Protocols
| Country, Author, Year | Study Size, N | Symptom Measures | Symptom Reduction at Follow-Up Points | |||
|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |||
| Australia, Dobrotwir A et al, 2012 (94) | 100 | UFS-QOL (SSS) Mean ± SD | 59 ± 21 | 37 ± 22 P < 0.001 | 34 ± 22 P < 0.001 | 29 ± 17 P < 0.001 |
| Germany, Trumm C et al, 2013 (91) | 115 | UFS-QOL (SSS) Median (IQR) | 63 (38–73) | NR | 38 (25–44) | |
| India, Desai S et al, 2012 (95) | 50 | UFS-QOL (SSS) Mean ± SD | 57 ± 5 | NR | 29 ± 6 P < 0.001 | |
| India, Himabindu Y et al, 2014 (105) | 32 | UFS-QOL (SSS) Mean ± SD | 68 ± 7 | 30 ± 5 P < 0.01 | 27 ± 6 P < 0.01 | |
| Korea, Park M et al, 2014 (82) | 79 | UFS-QOL (SSS) Mean ± SD (range) | 43 ± 16 (13–81) | 28 ± 15 (6–59) P < 0.001 | ||
| Japan, Mikami et al 2008 (90) | 48 | Self-reported symptom improvement | NR | See summary in text | See summary in text | |
| United States, Gorny K et al 2011 (97) | 150 | See summary in text | See summary in text | See summary in text | ||
Abbreviations: IQR, inter-quartile range; MRgHIFU, magnetic resonance-guided high-intensity focused ultrasound; NR, not reported; SD, standard deviation; SSS; symptom severity score; UFS-QOL, Uterine Fibroid Symptom and Quality of Life questionnaire.
Fibroid-Related Symptom Relief
Sixteen clinical cohort studies reported on fibroid-related symptom reduction with MRgHIFU treatment: 9 studies involving restricted MRgHIFU ablation protocols (Table 11A) and 7 studies involving protocols that allowed complete or near-complete ablation (Table 11B). In all but 3 of the studies (90;93;97), the Uterine Fibroid Symptom and Quality of Life questionnaire (UFS-QOL), a specifically designed and validated instrument, was employed to measure symptom reduction. (22) The other 3 studies used general measures of individual symptom improvements.
Symptom Reduction in Studies With Restricted MRgHIFU Ablation Protocols
Of the 9 reports in this group, listed in Table 11A, 4 studies involved overlapping patients from different institutes participating in a multicentre trial with different follow-up points. (49;107;110;113) All studies reported significant reductions in mean symptom severity scores (SSS), a subscale on the UFS-QOL, over baseline values at 3-month follow-up. Symptom severity scores continued to improve over the study follow-ups. In all cases, the mean change in symptom severity scores was more than a clinically significant symptom reduction (at least a 10-point reduction) on the SSS-UFS-QOL. Two studies reported symptom scores at longer than 1-year follow-up: Kim et al (114) and Machtinger et al (107) followed patients for 3 years. In both of these studies, mean symptom scores approached values in control populations without uterine fibroids (15.3 ± 14.5). (24) The Machtinger et al (107) study was the only study to evaluate and compare the response of different racial groups (African American and non–African American women) to MRgHIFU treatment. In this comparison, African American women, despite their heavier fibroid burden at baseline, also experienced significant reductions in their fibroid symptoms, and reductions occurred early, at 3 months, and continued with longer follow-up.
In the Hesley et al report, (93) the UFS-QOL was not used and changes in menstrual symptoms and mass or pressure effects were evaluated based on individual self-reports. Before treatment, 42 women reported a mean and median menstrual period duration of 6.1 days and 5.3 days (range, 1.5–14 days). After HIFU, although the range of 1 to 14 days was unaffected, the mean and median duration were reduced to 4.9 and 4.5 days. Inter-menstrual bleeding was not affected: 6 of the 7 women initially reporting this symptom continued to experience it after treatment. Of the 37 patients reporting a range of pressure symptoms prior to treatment, only 1 woman reported no improvement in these symptoms following treatment. Nocturia, reported by 25 patients, resolved completely in 17 of them.
The impact of MRgHIFU on fibroid-related symptoms, in 4 studies in this ablation group, was also evaluated as the proportion of patients experiencing clinically relevant improvement, defined as at least a 10-point reduction in symptom severity scores. (49;110;112;113) Three of these studies (49;110;113) involved overlapping participants, so the report with the largest study group and follow-up is detailed here. (49) In that report, in the overall population the percentage of patients achieving a clinically relevant improvement in their SSS-UFS-QOL scores was 79% (118/149) at 3 months, 79% (114/144) at 6 months, and 78% (59/76) at 12-month follow-up. The results also included a comparison between 96 women undergoing MRgHIFU with the original treatment restrictions and 64 treated under subsequently modified MRgHIFU protocols. The proportion achieving improvement of 10 points or better in their symptom severity scores was higher in the modified versus the original treatment group, at all follow-up points: at 3 months, 85% versus 76%; at 6 months, 88% versus 74%; and at 12 months, 91% versus 72%. The report by Ikink et al (112) only reported on the 6-month follow-up and, in that study, 54% (25/46) of the patients achieved at least a 10-point improvement in their symptom scores.
Symptom Reduction in Studies With Complete or Near-Complete MRgHIFU Ablation Protocols
In the 7 studies involving MRgHIFU with complete or near-complete ablation protocols, statistically and clinically significant reductions in fibroid-related symptoms assessed by the UFS-QOL were also reported as early as the 3-month follow-up point (Table 11B). Paralleling the responses in the restricted ablation group, fibroid symptoms continued to improve with time and approached normal values at the 12-month follow-up. None of the studies in this group reported long-term follow-up greater than 12 months.
Two studies (90;97) involving complete or near-complete ablation protocols also reported on changes in individual symptoms. In the Gorny et al study, (97) a 4-point overall symptom improvement rating was reported for the 3-month, 6-month, and 12-month follow-up: 86% (90/105), 93% (92/99), and 88% (78/89) of women reported an overall symptom improvement in those respective follow-up periods. In the Mikami et al study (90), at 6-month follow-up 51% of participants (15/29) reported that their menstrual symptoms were alleviated and 60% (15/25) reported that their pressure or bulk-related symptoms had improved. At 12-month follow-up, although improvements in bulk-related symptoms were maintained, menstrual symptoms were reported to have worsened in 33% of the women (5/15).
Health-Related Quality of Life
Health-related quality of life, based on the UFS-QOL, was reported in 2 studies (110;114), both involving restricted MRgHIFU ablation treatment protocols (Table 12). Each study reported increasing (improving) HRQOL measures at follow-up. In the Stewart et al study, (110) HRQOL was reported to 6-month follow-up, and the Kim et al study (114) reported on HRQOL measures for longer follow-up terms, at 2 years and 3 years.
Table 12:
Impact of MRgHIFU Treatment for Uterine Fibroids on Health-Related Quality of Life
| Country, Author, Year | Study Size, N | HRQOL Measure | Impact at Follow-Up Points | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | 24 months | 36 months | |||
| United States, Johns Hopkins University School of Medicine, Kim H et al 2011 (114) | 40 | UFS-QOL, Mean (95% CI) | 44.1 (37.7–50.6) | 68.8 (62.1–75.6) | 68.6 (61.9–75.4) | 68.7 (59.6–77.9) | 86.1 (74.8–97.5) | 83.9 (74.5–93.3) |
| United States, Brigham and Women's Hospital (7 sites), Stewart E et al, 2006 (110) | 176 | UFS-QOL, Mean ± SD | 47.0 ± 18.6 | 65.9 ± 22.4 P < 0.001 | 67.9 ± 21.7 P < 0.001 | |||
Abbreviations: CI, confidence interval; HRQOL, health-related quality of life; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; SD, standard deviation; UFS-QOL, Uterine Fibroid Symptom and Quality of Life.
Additional Treatments for Persistent or Recurrent Symptoms Following MRgHIFU
An important end point for evaluating the treatment effectiveness of MRgHIFU for uterine fibroids is an assessment of the need for additional treatments for persistent or recurring symptoms. The decision regarding which alternative or additional treatments are provided reflects a complex process involving several factors. These include the patients’ desires and willingness to continue to avoid surgery and their ability to achieve a benefit with further minimally invasive therapies. The preferences of the treating physicians or their ability to provide alternative treatment options at their institute is also a factor.
Retreatment rates for MRgHIFU with follow-up are detailed in Table 13A for strategies that involved restricted ablation and in Table 13B for strategies that involve complete or near-complete ablation protocols. All of the retreatments were elective except for 1 reported case (97) involving emergent hysterectomy following an infarcted fibroid 6 weeks after the MRgHIFU procedure. The most common retreatments in the restricted ablation group were hysterectomy (52.7%; 29/55), myomectomy (18.2%; 10/55), or UAE (14.5%; 8/55), and in the near-complete ablation group, hysterectomy (46.1%; 18/39) or myomectomy (25.6%; 10/39).
Table 13A:
Retreatment After MRgHIFU With Restricted Ablation Protocols for Uterine Fibroids
| Country, Author, Year | NPV, % Mean ± SD (range) | Follow-Up Period | Retreatment Rate, % (n/Eligible) [Original Cohort] | Alternative Treatments | Comments |
|---|---|---|---|---|---|
| Israel, Machtinger R et al, 2012 (92) | 41 ± 21 (10– 100) | 33 months | 23.8 (19/80) [81] | 13 HY + 4 MY + 2 UAE | 1 surgery was a hysteroscopic myomectomy for an incompletely expelled fibroid. 6 women having surgeries had a prior repeat HIFU. All surgeries were performed within 2 years. |
| Israel, Rabinovici J et al, 2007 (87) | 31 ± 23 (2–92) | 6 months | 17.1 6/35 [35] | 6 HY | All surgeries were within 6 months (proof-of-principle hysterectomy observation cohort). |
| Japan, Okada A et al, 2009 (106) | 39 ± 24 (early protocol) | 6 months 12 months | 4.8 (5/105) 12.4 (13/105) [144] | NR | Overall, 8/228 (4%) had alternative surgeries up to 6 months and an additional 5% between 6 and 12 months. Cumulative 12-month reintervention rate was 8.3% (19/228). |
| 54 ± 19 (amended protocol) | 6 months | 2.4 (3/123) | |||
| 12 months | 4.9 (6/123) [143] | ||||
| Korea, Yoon S-W et al, 2013 (111) | 40 ± 20 (0–90) | 12 months | 11.5 (6/52) [60] | NR | 6 women elected to undergo additional surgeries, which were not reported; 8 patients were lost to follow-up. |
| Netherlands, Ikink M et al, 2013 (112) | 40 ± 22 | 6 months | 9.8 (4/41) [51] | 2 HY + 2 UAE | 5 women were not satisfied with treatment result; of these, 4 had retreatments and 1 withdrew from follow-up and her treatment was unknown; 5 other women were lost to follow-up. |
| United States, Mayo Clinic, Hesley G et al, 2006 (93) | NR | 6 months | 42.5 (17/40) [42] | 6 HY + 2 MY + 1 UAE + 2 EA + 6 rHIFU | Of the 2 women lost to follow-up, 1 had unresolved significant symptoms and 1 was satisfied with treatment. Of the women having hysterectomy, 1 had only 3 sonications due to pain and 2 had hysterectomy for unrelated causes (enlarging complex adrenal mass and progressive pelvic organ collapse). Time to additional treatment ranged from 1 week to 35 months. |
| United States, Johns Hopkins University School of Medicine, Kim H et al, 2011 (114) | 32 | 36 months | 31.0 (9/29) [40] | 2 HY + 2 MY + 5 UAE | All of the additional treatments were elective. Kaplan-Meier analysis showed that, at 2.5 years, 31% had received additional treatments; 11 patients were lost to follow-up. |
| United States, Brigham and Women's Hospital (7 sites), Stewart E et al, 2006 (110) (1 of 3 reports) | 25 | 12 months | 28.0 (23/82) [109] | NR | Of the 27 women not evaluated, 9 declined further follow-up, 9 withdrew from the study or were lost to follow-up, and 9 were non-evaluable. |
| Brigham and Women's Hospital (7 sites), Fennessy F et al, 2007 (49) (2 of 3 reports) | 17 ± 16 (restricted protocol) 26 ± 22 (amended protocol) | 12 months 12 months | 33.3 (32/96) 12.5 (8/64) | NR | 24 of the 64 women in the amended treatment group underwent a second HIFU within 2 weeks under the modified guidelines; 6 were lost to follow-up at 6 months. |
| Brigham and Women's Hospital (7 sites), Machtinger R et al, 2013 (107) (3 of 3 reports) | 41 ± 25 | 12 months 24 months | 11.7 (12/103) 33.3 (32/96) [122] | NR | The 137 women in the study were divided into 2 groups: African-American (AA) (n = 63) and non-AA (n = 59). The need for additional treatment did not differ between the study groups. |
Abbreviations: AA; African-American; EA, endometrial ablation; HY, hysterectomy; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; MY, myomectomy; NPV, non-perfused volume; NR, not reported; rHIFU, repeat high-intensity focused ultrasound; SD, standard deviation; UAE, uterine artery embolization.
Table 13B:
Retreatment After MRgHIFU With Complete or Near-Complete Ablation Protocols for Uterine Fibroids
| Country, Author, Year | NPV, % Mean ± SD, (range) | Follow-Up Period | Retreatment Rates, % (N/Eligible [Original Cohort] | Alternative Treatments | Comment |
|---|---|---|---|---|---|
| Australia, Dobrotwir A et al, 2012 (94) | 67 ± 25 (0–100) | 12 months | 13.7 (7/ 51) [100] | 2 HY + 4 MY + 1 UAE | Of the 51 patients due for their 12-month follow-up, 1 withdrew from the study and 7 elected not to have an MRI scan but reported no further intervention. 5 of the 7 who had additional treatments had NPV < 50%. The hysterectomies were both at 8 months, the myomectomies were at 4, 5, 8, and 11 months, and the UAE was at 12 months after HIFU. |
| Japan, Kobe, Funaki K et al, 2009 (73) | 39 ± 24 (0–91) | 12 months 24 months | 3.8 (12/ 65) 11.1 (5/45) [91] | 1 HY + 5 MY + 1TR + 5 rHIFU | 12 patients underwent additional treatments: 2 within 12 months, 5 between 12 and 24 months, and 5 after 24 months. None of the hysterectomies were emergent. The additional treatment rate was higher for type 3 tumours (highly vascular) (2/11) compared to type 1, and for 2 less vascular tumours (12/80). 19 were lost to 12-month follow-up; 12 were lost between 12- and 24-month follow-up. |
| Japan, Tokyo, Morita Y et al, 2008 (96) | 60 ± 18 (22–100) | 12 months | 8.3 (4/48) [48] | 1 MY + 1 UAE + 2 DT | 7 women were not satisfied with treatment and 3 did not seek additional therapy; of these 3, 1 resumed pain killers, 1 continued anemia treatment, and the third was not prescribed therapy. The other 4 underwent additional treatment: 2 had surgical intervention and 2 underwent drug therapy involving GnRHa until onset of natural menopause. |
| Japan, Osaka, Mikami K et al, 2008 (90) | 47 (25–72) | 12 months | 50 (16/32) [48] | NR | 32 of the 48 were evaluated as technical success and, at 6-month follow-up, all 32 women were followed. Alternative treatments (hysterectomy, myomectomy, or UAE) were recommended for 16 women not having symptom relief. |
| United States, Mayo Clinic, Gorny K et al, 2011, 2014 (97;115) | 45 ± 23 (0–100) | 12 months | 5.9 (8/136) [150] | 7 HY + 1 EA | 14 of the original 150 women completing treatment denied use of their data for research. Treatment was not completed in 6 patients and completed in 130 patients: 71 women in 1 session, 59 women in 2 sessions on consecutive days. 8 patients had additional treatments within 12 months, and 3 had surgeries for other indications: hysterectomy during ovarian cyst surgery, myomectomy during surgery for a pancreatic tumour, and hysterectomy when Pap test was unsuccessful. Cumulative additional treatment rates were estimated with Kaplan-Meir analysis and were 0% at 6 months, 2.6% at 9 months, and 7.4% at 12 months. |
| United States, LeBlang S et al, 2010 (43) | 55 ± 25 | 12 months | 10 (8/80) [80] | 8 HY | HIFU was performed in more than 1 session for 20 of the 80 women: 2 sessions for 18 women, 3 sessions for 1 woman, and 4 sessions for 1 woman. The NPV ratio was < 15% for 6 of the women having hysterectomy. 1 woman underwent surgery for bladder prolapse and had a concurrent hysterectomy. Among the 49 women having an NPV > 50%, only 1 needed a hysterectomy for inadequate symptom relief. |
Abbreviations: DT, drug therapy; EA, endometrial ablation; GnRHa; gonadotropin-releasing hormone analogue; HY, hysterectomy; MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; MY, myomectomy; NPV, non-perfused volume; NR, not reported; rHIFU, repeat high-intensity focused ultrasound; SD, standard deviation; UAE, uterine artery embolization.
Reintervention rates reported for the restricted ablation group at 12-month follow-up were higher and more variable, ranging from 4.9% to 33%, than for the near-complete ablation protocol group, which ranged from 3.8% to 13.7% (except for the 50% in the Mikami et al (90) study). Two reports allowed for a direct comparison of retreatment rates between the restricted and near-complete ablation strategies within their study sites. (49;106) In both comparisons, the 12-month reintervention rates were higher for the restricted ablation strategies: in the Fennesy et al (49) report, the rates were 33.3% versus 12.5%, and in the Okada et al (106) report, the rates were 12.4% versus 4.8%.
Two studies—1 in the restricted ablation group (114) and 1 in the near-complete ablation group (97)—more appropriately reported on retreatment rates using survival analysis to account for follow-up durations. The Kim et al (114) report on their 3-year MRgHIFU experience at the Johns Hopkins University School of Medicine showed, using Kaplan-Meier analysis, that at approximately 2.5 years, 31% of the patients had undergone retreatments, all of them electively. In the Gorny et al (97) first report on their MRgHIFU follow-up experience at the Mayo Clinic, cumulative retreatment rates based on Kaplan-Meier analysis were 0% at 6 months, 2.6% at 9 months, and 7.4% at 12 months. In their second report on the Mayo experience involving a larger cohort (138 patients) and a longer follow-up (median 2.6 years), the cumulative retreatment rates, again based on Kaplan-Meier analysis, at 12 months, 24 months, 36 months, and 48 months were 4%, 13%, 19%, and 23% respectively. (115)
Section E. Reproductive Outcomes
When MRgHIFU was initially evaluated in regulatory trials as an alternative treatment to hysterectomy, a major restriction was that women must have completed their child-bearing because of uncertainty on the impact of HIFU on reproductive outcomes. However, many young women successfully underwent the procedure and, because their uterus was preserved, further pregnancies were possible. In 2006, the FDA loosened the contraindication related to child-bearing and stated that women “should” have completed their families to be eligible for the procedure. (44)
We obtained information on pregnancies occurring after MRgHIFU for uterine fibroids from several sources including case reports and reports from clinical cohort trials. A trial employing ultrasound-guided HIFU was also reviewed because of the large number of pregnancies occurring in the trial and the consequences of unintended pregnancies. (54) In addition, we reviewed a summary report by Rabinovici et al (116) on pregnancies occurring in clinical trials sites (in the United States, Israel, the United Kingdom, Germany, and Japan) and commercial treatment sites (in the United States, Russia, Japan, and Germany). The manufacturer (InSightec Ltd., Haifa, Israel) was required to report these occurrences as part of post-approval monitoring by the FDA. A systematic review by Clark et al (47) on the reproductive impact of MRgHIFU was used as an additional source of references. In none of the studies they reviewed was evaluation of reproductive outcomes a stated study objective, and in most cases a desire for fertility was stated as a study exclusion. The FIRSTT study (Fibroid Interventions: Reducing Symptoms Today and Tomorrow), an RCT currently underway comparing MRgHIFU with UAE, is the only study so far in which reproductive potential is a stated study objective. (117) Recruitment for the trial is now closed and data analysis is currently underway. (Personal Communication, Elizabeth Stewart, MD, FIRSTT Investigator, April 2014)
Eight case reports of pregnancies were reported (Table 14): 3 in the United States, (118–120) 2 in the United Kingdom, (121;122) and 1 each in Japan, (123) Korea, (124) and Israel. (125) All pregnancies except for 2 (118;122) were conceived spontaneously. In one case, a 37-year-old woman conceived after undergoing a cycle of clomiphene citrate and, in the other, a 45-year-old woman successfully conceived after 1 cycle of in vitro fertilization. Pregnancy courses were uneventful with normal fetal development, and fibroids remained stable in size or were absent. Deliveries were generally at term with uneventful labour and postpartum recoveries.
Table 14:
Pregnancy Case Reports After MRgHIFU Treatment of Uterine Fibroids
| Country, Author, Year | Case Detail | Pregnancy Outcomes |
|---|---|---|
| United States, Bouwsma E et al, 2011 (118) | 37-year-old Asian woman having had a prior miscarriage at 6 weeks underwent clomiphene citrate cycles following successful MRgHIFU and spontaneously conceived. | Fetal growth was normal and uterine fibroids remained stable in size and at 40 weeks after uneventful labour, she delivered a 3,450-g baby girl with Apgar scores of 7 and 9. |
| United States, Gavrilova-Jordan L et al, 2007 (119) | 38-year-old nulligravid woman conceived 18 months following MRgHIFU treatment for a single uterine fibroid. | At 39 weeks she underwent labour induction for gestational hypertension with vacuum-assisted vaginal delivery of a healthy baby boy. Postpartum recovery of both mother and neonate was uneventful. |
| United States, Hanstede M et al, 2007 (120) | 40-year-old woman with 3 full-term deliveries, a history of secondary infertility, and a 10-year history of uterine fibroids underwent MRgHIFU for treatment of symptomatic uterine fibroids. | Conception occurred a year and a half following MRgHIFU treatment. Pregnancy was complicated with first-trimester vaginal bleeding until 16 weeks gestation and diagnosed with diabetes mellitus type 1. The uterine fibroids remained stable and normal fetal development occurred. Labour was induced at 39 weeks and she delivered a full-term 3,170-g baby boy after an uneventful labour and vaginal delivery. |
| Japan, Morita Y et al, 2007 (123) | 29-year-old nulligravid woman underwent MRgHIFU rather than myomectomy for a single large (6.8 × 8.0 × 7.9 cm) fibroid | She conceived 3 months following HIFU; repeated ultrasounds throughout pregnancy showed normal fetal development, normal placental insertion in the posterior uterine wall, and no change in size of the treated fibroid. At 39 weeks she had an uneventful labour and vaginal delivery of a healthy baby boy with normal weight (3,212 g) and Apgar scores of 8 and 9. Postpartum recovery was uneventful. |
| Israel, Rabinovici J et al, 2006 (125) | 36-year-old woman gravida 1 without prior miscarriages was initially diagnosed with uterine fibroids, later diagnosed by MRI as having focal adenomyosis with infertility secondary to menometrorrhagia; she successfully underwent MRgHIFU rather than myomectomy. | She conceived spontaneously 3 months following MRgHIFU with an uneventful pregnancy course with normal fetal development, normal placental insertion in posterior uterine wall, and normal uterine anatomy. Birth was a full-term 3,050-g healthy baby girl after an uneventful labour and vaginal delivery. Placental separation was delayed and the placenta was manually extracted. Postpartum recovery was uneventful. |
| Korea, Yoon S-W et al, 2010 (124) | 31-year-old woman with 2 intramural fibroids underwent 2 separate MRgHIFU treatments for frequent urination and bulk symptoms. | Spontaneous conception occurred 4 months following HIFU and pregnancy was carried to term. At 39 weeks, a 3,190-g baby girl was born through a vaginal delivery. Labour and postpartum recovery were uneventful. |
| United Kingdom, Zaher S et al, 2010 (121) | 39-year-old woman with 1 prior pregnancy resulting in a premature delivery at 28 weeks, attributed to fibroids, presented with menorraghia and urinary pressure symptoms including frequency and nocturia. 5 fibroids were identified, the largest being a fundal intramural fibroid, and she underwent a successful MRgHIFU treatment after a pretreatment course of GnRHa injections. | Spontaneous conception occurred 10 months following HIFU. Repeated ultrasounds throughout pregnancy revealed normal fetal growth with cephalic presentation and an anterior placenta which was not low lying. No fibroids were visible at the 40-week scan. Delivery was induced at 41-weeks and a healthy 3,589-g baby girl was born with Apgar scores of 8 and 9 after an uncomplicated vaginal delivery. |
| United Kingdom, Zaher S et al, 2011 (122) | 45-year-old woman para 0+1 with a known history of fibroids had undergone 4 prior IVF cycles, 3 with egg donations and 1 with her own egg. 2 years prior to presenting with fibroid-related menorrhagia, she had 1 pregnancy resulting in a first-trimester miscarriage. An infertility work-up identified the fibroid as the likely obstacle to pregnancy. She underwent HIFU for a single large (9 × 6.2 × 7.1 cm) intramural fibroid. | 10 months following HIFU the patient underwent IVF treatment and became pregnant after the first cycle. Repeated ultrasound scans revealed normal fetal development with cephalic presentation. At 39 weeks the patient presented in spontaneous labour but due to persistently suboptimal cardiotocograph, delivery was by emergency Caesarean section which was uncomplicated and involved a blood loss of 100 ml. A healthy 3,050-g baby boy with Apgar scores of 9 and 10 was delivered without placental delivery problems. Postpartum recovery was uneventful. |
Abbreviations: GnRHa; gonadotropin-releasing hormone analogue; HIFU; high-intensity focused ultrasound; IVF, in vitro fertilization; MRgHIFU, MR-guided high-intensity focused ultrasound; MRI, magnetic resonance imaging.
Pregnancies were reported in longitudinal follow-up in 5 clinical cohort studies (Table 15), 1 involving ultrasound guidance rather than MR guidance. (54) The pregnancies reported in the Morita et al (96) and the Yoon et al (111) cohort studies have been documented more fully in earlier case reports. (123;124). The clinical studies were not intended to evaluate reproductive outcomes, and desire for fertility preservation was usually a study exclusion criteria. The low number of pregnancies occurring after HIFU is to be expected given that women treated were generally aged 40 or older and that cautionary advice on pregnancy was provided to patients. In addition, the reproductive histories and fertility or infertility status of the women in the studies were generally not known.
Table 15:
Pregnancy Reports in Cohort Studies After MRgHIFU Treatment of Uterine Fibroids
| Country, Author, Year, | Cohort Size, Age, Mean ± SD (range) | Follow-Up Duration | Pregnancies | Pregnancy Outcomes |
|---|---|---|---|---|
| Germany, Froeling V et al, 2013 (126) | 50 women 36.1 years (27–41 years) | 24 months | 9 women had 10 pregnancies | Pregnancies occurred on average 16.1 months (range, 8.5–23.8) after MRgHIFU. There were 7 live births and 3 miscarriages. |
| Japan, Funaki K et al, 2009 (73) | 91 women 40.4 ± 4.6 years | 24 months | 4 pregnancies | 1 pregnancy occurred 3 months after MRgHIFU, 2 at 12 months, and 1 within 24 months. There were 2 live full-term births and 2 first-trimester miscarriages. |
| Japan, Morita Y et al, 2008 (96) | 48 women 42.2 ± 5.8 years (24–51 years) | 12 months | 1 pregnancy | 1 pregnancy occurred 4 months after MRgHIFU in a 29-year-old women with no previous pregnancy. There was a 39-week vaginal delivery of a normal 3,212-g baby with Apgar scores of 8 and 9 and an uneventful postpartum course. |
| Chinaa, Qin J et al, 2012 (54) | 435 women 34.5 ± 4.5 years (25–42 years) | 12 months | 24 women had 24 pregnancies | Of the 24 women, 8 had desired pregnancy while remaining 16 had not. Only 1 woman had been diagnosed with secondary infertility. Conception occurred following USgHIFU at < 3 months (n = 4), 3–6 months (n = 13), and > 7 months (n = 7). Of the 8 desiring pregnancy, 7 continued to elective Caesarean section at full term with birth weights at least 2,500-g and Apgar scores within normal ranges (8–9) in all cases. |
| Korea, Yoon S-W et al, 2013 (111) | 60 women 41.3 ± 6.3 years (30–52 years) | 12 months | 1 pregnancy | 1 pregnancy occurred 4 months following MRgHIFU and resulted in a successful delivery. |
Abbreviations: MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; SD, standard deviation; USgHIFU, ultrasound-guided high-intensity focused ultrasound.
Women in this study underwent ultrasound-guided HIFU.
Rabinovici et al (116) reported on a series of pregnancies occurring in clinical trials and commercial treatment and reported to the FDA. Overall, 54 pregnancies occurred in 51 women who underwent MRgHIFU. Eight of these pregnancies occurred in clinical trials for women who had completed their families, 26 occurred in commercial treatments, and 20 occurred in 17 women in the trial designed for women who were trying to conceive. The mean age of the women was 37.2 years (range, 28–49 years) and 39% were at least 40 years old. More than one-third of the women (38%) had never been pregnant and almost two-thirds had never delivered. The mean time to pregnancy following MRgHIFU was 8 months.
Of the 54 pregnancies, 22 resulted in deliveries, 11 were reported to be ongoing beyond 20 weeks, 7 were electively terminated, and 14 resulted in spontaneous miscarriage, the majority occurring by the tenth week. Fibroid growth was a concern in 2 of the pregnancies. Four women were hospitalized antepartum, and 2 women had placenta previa. One patient experienced serious complications in each of 2 pregnancies that occurred after MRgHIFU. In the first pregnancy, she required an elective Caesarean section due to a breech presentation and an intramural fibroid obstructing the pelvic outlet. Although a healthy child was delivered, the mother underwent a myomectomy for a low-lying fibroid, bled vaginally due to persistent uterine atony, and subsequently developed disseminated intravascular coagulation. After recovering from this, she developed adult respiratory distress syndrome and recovered after 3 days in the intensive care unit. Her second pregnancy was complicated by a placenta previa resulting in hospitalization in the third trimester. A healthy infant was delivered again after a repeat Caesarean delivery.
Section F. Comparative Effectiveness
A summary of the clinical trials involving comparisons among MRgHIFU, other minimally invasive interventions that preserve the uterus, and surgical interventions for uterine fibroids is outlined in Table 16. There were no RCT studies comparing MRgHIFU to hysterectomy, myomectomy, or any other minimally invasive, uterine-sparing interventions such as UAE. There were, however, RCT studies comparing another image-guided HIFU procedure (ultrasound guidance, USgHIFU) to myomectomy and to radiofrequency ablation for the treatment of uterine fibroids.
Table 16:
Comparative Effectiveness Trials of Hysterectomy and Uterine-Preserving Fibroid Treatments
| Author, Year | Country | Study Design | Centres, Subjects | Study Outcomes |
|---|---|---|---|---|
| UAE versus hysterectomy | ||||
| Volkers N et al, 2006, 2007 (129;130) | Netherlands (EMMY trial) | Multicentre, non-inferiority RCT | 28 sites, 170 women (88 UAE, 89 hysterectomy) | Comparison of the 2-year efficacy outcomes |
| Pinto I et al, 2003 (128) | Spain, Madrid | RCT (Zelen consent): randomized to group 1 (informed choice of UAE or hysterectomy) or group 2 (assigned hysterectomy) | 1 site, 57 women (38 in group 1, 19 in group 2) | Comparison of the effectiveness of UAE for management of bleeding secondary to uterine fibroids with an additional focus on hospital stay and safety |
| Edwards R et al, 2007 (132) | United Kingdom (REST trial) | 2:1 pragmatic RCT (for surgical intervention) | 27 sites, 157 women (106 UAE, 51 surgery: myomectomy or hysterectomy) | Clinical outcomes and HRQOL at 1 year |
| Moss J et al, 2011 (127) | United Kingdom (REST trial) | 2:1 pragmatic RCT (for surgical intervention) | 27 sites, 157 women (106 UAE, 51 surgery: myomectomy or hysterectomy) | 5-year clinical and economic outcomes |
| Ananthakrishnan G et al, 2013 (131) | United Kingdom (REST trial) | 2:1 pragmatic RCT (for surgical intervention) | 27 sites, 157 women (106 UAE, 51 surgery: myomectomy or hysterectomy) | Relationship of imaging to clinical outcomes and need for reintervention |
| Spies J et al, 2010 (24) | United States | Prospective non-randomized comparative cohort study comparing 3 uterine fibroid interventions and a control group | 329 women either undergoing hysterectomy (n = 106), myomectomy (n = 61), or UAE (n = 107) recruited from 4 sites and 130 control subjects from 5 sites | Comparison of the longitudinal changes in symptoms and HRQOL in those undergoing uterine fibroid interventions with those in a control population |
| UAE versus myomectomy | ||||
| Mara M et al, 2008 (135) | Czeck Republic | RCT | 1 site, 121 women (58 UAE, 63 myomectomy) | Evaluation of midterm clinical and first reproductive outcomes |
| Manyonda I et al, (REST trial) 2012 (134;135) | United Kingdom, (FUME trial) London | RCT | 1 site, 163 women (82 UAE, 81 myomectomy) | HRQOL, measured as UFS-QOL score at 1-year was the primary outcome measure |
| Goodwin S et al, 2006 (136) | United States | Parallel contemporary prospective cohort study, assignment by physician and patient | 6 US sites, 163 women (149 UAE, 60 myomectomy) | Comparison of adverse events, recovery, clinical outcomes, and HRQOL at 6-months (both groups) and at 1-year (UAE only) |
| MRgHIFU versus hysterectomy | ||||
| Taran F et al, 2009 (133) | International study (United States, Israel, United Kingdom, Germany) | Prospective comparative cohort study with contemporaneous controls | 14 medical centers: 7 sites, 109 women for MRgHIFU; and7 separate sites, 83 women abdominal hysterectomy | Incidence of significant clinical complications and adverse events and HRQOL at 6 months |
| USgHIFU versus myomectomy | ||||
| Wang X et al, 2013 (59) | China | RCT | 1 site, 120 women (60 USgHIFU, 60 abdominal myomectomy) | Impact of treatments on immune function was the primary outcome, adverse reactions and complications were also compared |
| Wang X et al, 2013 (58) | China | RCT | 1 site, 100 premenopausal women (55 USgHIFU, 55 abdominal myomectomy) | Impact of treatments on sexual function (BISF-W); hospital stay, recovery time and complications; adverse reactions were also compared |
| Wang F et al, 2014 (56) | China | Prospective comparative cohort study | 1 site, 130 premenopausal women (83 USgHIFU, 39 laparoscopic myomectomy) | Impact of treatments on HRQOL at 1-year follow-up |
| MRgHIFU versus UAE | ||||
| Froeling V et al, 2013 (126;137) | Germany | Prospective comparative cohort study | 1 site; among women equally eligible for UAE or MRgHIFU, 30 in UAE group and 50 in MRgHIFU group | Comparison of the reintervention rate and midterm changes in symptom severity and HRQOL |
| Bouwsma E et al, 2011 (117) | United States | RCT (protocol stage, due in 2014) | 2 sites, 220 planned to randomize to MRgHIFU or UAE and a control group | Outcomes to include recovery, complications, symptom relief and fibroid reduction, reinterventions and impact on reproductive function, as well as an economic analysis with 3-year follow-up |
| USgHIFU versus radiofrequency ablation | ||||
| Meng X et al, 2010 (52) | China | RCT | 1 site, 100 premenopausal women randomized to USgHIFU (n = 50) or radiofrequency ablation (n = 50) | Comparison of ablation rates, and complications |
Abbreviations: BISF-W, Brief Index of Sexual Functioning for Women; HRQOL, health-related quality of life; MRgHIFU, magnetic resonance-guided high-intensity focused ultrasound; RCT, randomized controlled trial; UAE, uterine artery embolization; UFS-QOL, Uterine Fibroid Symptom and Quality of Life questionnaire; USgHIFU, ultrasound-guided high-intensity focused ultrasound.
Comparative Effectiveness of MRgHIFU and Hysterectomy
Hysterectomy has been the definitive treatment for symptomatic uterine fibroids. As noted, we found no RCT studies comparing MRgHIFU to hysterectomy, but 3 RCT studies (127–129) and 1 prospective cohort study (24) have compared UAE with hysterectomy for safety and effectiveness, and they are cited here as indirect evidence. Minimally invasive treatments that spare the uterus, such as UAE, have been an alternative to surgical treatment, both myomectomy and hysterectomy, for about 10 years and have been evaluated in clinical trials involving more than 8,000 women. (28) The results of these RCT studies are indirectly informative to MRgHIFU, which is an even less invasive treatment than UAE.
The RCT studies included the EMMY trial (Embolization versus Hysterectomy) in the Netherlands at 28 sites (129;130) and in Spain at 1 site. (128) Patients in the third RCT, the REST trial (Randomized Trial of Embolization versus Surgical Treatment for Fibroids) in the United Kingdom, were randomized to UAE and either hysterectomy or myomectomy. (127;131;132) In the prospective cohort study, patients were recruited from 4 sites for fibroid uterine interventions—either hysterectomy, myomectomy, or UAE—and compared with control patients without uterine fibroids, recruited from 5 sites in the United States. (24)
MRgHIFU has developed more recently than UAE, and the lack of RCT studies comparing MRgHIFU to hysterectomy may be due to the fact that the safety and effectiveness of UAE (compared to hysterectomy) have already been established. As an extracorporeal technique, MRgHIFU is even less invasive than UAE, and randomizing patients between a noninvasive procedure and hysterectomy would likely not be acceptable to patients or physicians. To date, MRgHIFU has only been compared to hysterectomy in a multicentre international prospective parallel cohort study. (133) In that study, patients undergoing MRgHIFU at 7 centres were compared with patients undergoing abdominal hysterectomy at 7 different sites. Outcomes for women undergoing MRgHIFU were reported by Stewart et al (110) for the original trial that led to FDA regulatory approval.
In that parallel cohort study, (133) fewer clinically significant complication events were reported after MRgHIFU than for hysterectomy. Recovery trajectories were significantly better for the MRgHIFU group. At 1-month follow-up there were significant differences in days lost to work and to usual activities. Women reported losing 1.2 work days and 2.7 days from usual activities after MRgHIFU compared to 19.2 and 17.4 days lost by women after hysterectomy (P < 0.0001). In addition at 1 month, women in the MRgHIFU group had significantly greater improvement in their HRQOL scores based on SF-36 scores (the 36-item Short Form Health Survey) for physical function, physical roles, and social function. At 3-month and 6-month follow-up, however, these differences were not significant.
Comparative Effectiveness of MRgHIFU and Myomectomy
There were also no RCTs comparing MRgHIFU with myomectomy by any route. One RCT with 2 reports (52;58) and 1 comparative cohort study (56) have compared ultrasound-guided HIFU with myomectomy. The comparative safety and effectiveness of UAE to myomectomy has been evaluated earlier in 2 RCTs (134;135) and 1 comparative cohort study. (136)
The RCT comparing USgHIFU to abdominal myomectomy, conducted by Wang et al (58;59) at 1 site in China, was evaluated in 2 separate reports. The first report compared the impact of HIFU ablation of fibroid tissue on the immune response of 120 patients, 60 undergoing myomectomy and 60 receiving USgHIFU. (59) Levels of peripheral blood cell subpopulations (T lymphocytes) and serum levels of cytokines (interleukins [IL] 2, 6, and 10) were used as markers of specific and non-specific immune function. Although measurements were only taken in the immediate postoperative period (up to 72 hours), there were no changes in the percentage of T lymphocyte cell counts (CD4+ and CD8+) and CD16+ (NK cell marker) in the HIFU group but all were significantly decreased in the myomectomy group and remained decreased compared to baseline values at 48 and 72 hours. Preoperative serum levels of immune-related cytokines (IL-2, IL-6, and IL-10) at baseline were similar in the 2 groups. After treatment, IL-6 and IL-10 increased in both groups but levels were significantly higher in the myomectomy group at 24-hour and 72-hour follow-up. The IL-2 levels significantly decreased in the myomectomy group compared to the HIFU group.
The second report on the RCT evaluated sexual function in 100 women using a validated sexual function questionnaire, the Brief Index of Sexual Functioning for Women (BISF-W). (58) Recovery and perioperative complications were also compared between the study groups. Prior to treatment, all women had been sexually active and, at 1 month following treatment, sexual activity decreased in both groups but the decrease was significantly smaller in the HIFU group. However, there were no significant differences between the study groups in their BISF-W scores at 3 or 6 months following treatment. The myomectomy group had significantly more postoperative complications compared to the HIFU group. No complications occurred in the HIFU group. In the myomectomy group, 1 patient required a blood transfusion and 5 developed fevers, although they recovered promptly with intravenous antibiotic therapy. There were also significant differences in recovery time between the groups, including shorter hospital stays, quicker return to ambulation (shorter time to out-of-bed activity), and to return to normal daily activities for the HIFU-treated group.
The comparative cohort study compared USgHIFU with laparoscopic myomectomy where patients were assigned to treatment groups based on their preference. (56) In the study, 89 women underwent USgHIFU and 41 underwent laparoscopic myomectomy. Two procedures in the surgery group converted to laparotomy myomectomy because of serious pelvic adhesions. HRQOL was assessed by the SF-36, and there were no significant differences between the study groups at 1-year follow-up for any subdomain of the score.
Comparative Effectiveness of MRgHIFU and UAE
MRgHIFU has only been compared with UAE in 1 prospective comparative cohort study and reported on in 2 follow-up periods. (126;137) In that study, women equally eligible for UAE or MRgHIFU underwent one of the treatments between 2002 and 2009 at a single site. A total of 121 women were judged to be eligible for either treatment, and 80 were included in the analysis, with 41 lost to follow-up. The majority (94%; 47/50) of the women in the MRgHIFU group were treated according to the modified FDA treatment guidelines which limited ablation to 50% or 150 ml of the fibroid volume. In addition the study eligibility for the 2 treatments included both general inclusion criteria that were common to both study groups and additional criteria for the MRgHIFU group that included restrictions on the size of the uterus (> 24 weeks gestation) and the size (> 10 cm diameter) and number (> 5) of fibroids. Consequently the resulting study groups in this report differed in several ways, complicating treatment comparisons. The UAE group included women with larger uteruses, more fibroids, higher symptom severity scores, and lower HRQOL scores on the UFS-QOL. The women in the UAE group were also older than those in the MRgHIFU group, with a median age of 42.7 years (range, 33.6–52.2) compared to 36.2 years (range, 29.2–41.0)
There were no complications in either study group. At mean 13-month follow-up, the symptom severity and HRQOL scores of the UFS-QOL were significantly improved over baseline in both groups. The improvement in median symptom severity scores was not significantly different between the groups, but the total median HRQOL score was significantly better after UAE than after MRgHIFU (median, 93.1 vs. 82.8; P = 0.032). The rate of reintervention was significantly higher after MRgHIFU (P = 0.002) at midterm follow-up. Within 24-month follow-up, 6.7% (2/30) in the UAE group required reinterventions, which included hysterectomy (n = 1) and endometrial ablation (n = 1). In the MRgHIFU group, 30% (15/50) required reinterventions, including repeat MRgHIFU (n = 7), myomectomy (n = 5), hysterectomy (n = 2), and UAE (n = 1).
In the second report, (126) involving longer-term follow-up of the same study group (median, 61.9 months for UAE and 60.7 months for MRgHIFU), the median symptom severity scores and HRQOL scores based on the UFS-QOL remained significantly improved in both groups. However, at follow-up the median symptom severity score (6.3 vs. 26.6; P = 0.019) and HRQOL scores (100 vs. 87.9; P = 0.049) were significantly better in the UAE than the MRgHIFU group. The reintervention rate was also significantly higher in the MRgHIFU group than the UAE group (66.7% [24/36] vs. 12.2% [5/41]; P < 0.001). The reinterventions for the 24 women in the MRgHIFU group included hysterectomy (n = 8), myomectomy (n = 7), repeat MRgHIFU (n = 7), and UAE (n = 2). The reinterventions for the 5 women in the UAE group included hysterectomy (n = 2), myomectomy (n = 2), and endometrial ablation (n = 1).
Comparative Effectiveness of MRgHIFU and Other Minimally Invasive Treatments
MRgHIFU has not been compared to any other minimally invasive treatment option for uterine fibroids. HIFU with ultrasound guidance has been compared to radiofrequency ablation, another minimally invasive, uterine-preserving intervention, in a single-site RCT. (52) Radiofrequency ablation involves the percutaneous insertion of an electrode, connected to a radiofrequency generator, directly into the fibroid under ultrasound guidance. The degree of ablation was evaluated by contrast-enhanced colour Doppler ultrasound 1 week following the procedure to assess early treatment efficacy. Complete ablation was achieved more commonly (90% vs. 58%, P < 0.05) with radiofrequency ablation than with HIFU. Minor complications such as fever, abdominal pain, and pelvic fluid occurred in each group: 18% (9/50) in the HIFU group and 34% (17/50) in the radiofrequency group. No serious postprocedural complications were reported for either group.
Conclusions
For women failing or intolerant to medical therapy and seeking alternatives to hysterectomy for symptomatic uterine fibroids, magnetic resonance-guided high-intensity focused ultrasound (MRgHIFU) provides a safe and effective, noninvasive, uterine-preserving treatment from which they rapidly recover. Treatment durability, however, for which there is more limited information, depends on the delivery of adequate thermal energy to ablate fibroid tissue which is greatly influenced by patient selection, factors, technical limitations, and treatment strategies.
There are several limitations with MRgHIFU technology. These include restricted eligibility criteria, requirement for a dedicated (and proprietary) MR device to guide the HIFU treatment, lengthy procedure time, and loss of MR opportunity time. In addition, access to the procedure is limited as few centres in Canada have interventional radiologists with the required technical expertise or have multidisciplinary team approaches to fibroid management with organized referral patterns for this condition.
Increasingly, women with uterine fibroids are seeking treatments that not only preserve their uterus but also their fertility. However, HIFU clinical studies to date have not been designed to evaluate the procedure's impact on fertility. In addition, desiring future fertility was an exclusion criterion for clinical trials evaluating HIFU. Nonetheless, spontaneous pregnancies and uneventful term delivery of healthy infants after HIFU have been reported. This suggests both that HIFU may have a role in fertility preservation and that women should be advised that pregnancy is possible following HIFU and that they should continue using contraception to ensure that unintended pregnancies do not occur.
A lack of comparative evidence between HIFU and other mainstay, uterine-preserving treatments, such as UAE or myomectomy, limits informed decision making about these treatment options. For patients and physicians considering interventions for symptomatic uterine fibroids, the decision may well depend on patient characteristics and preferences as well as technical factors, given the restrictive eligibility criteria for MRgHIFU.
ACKNOWLEDGEMENTS
Editorial Staff
Amy Zierler, BA
Medical Information Services
Corinne Holubowich, BEd, MLIS
Expert Consultants on MRgHIFU
Dr Bijah Boran, Assistant Professor, Mayo Clinic College of Medicine, Rochester, Minnesota
Dr Jennifer Blake, Chief Executive Officer, Society of Obstetricians and Gynaecologists of Canada, Ottawa, Ontario
Dr Andrew Common, Department of Medical Imaging, St Michael's Hospital, Toronto, Ontario
Dr Elizabeth David, Department of Medical Imaging, Sunnybrook Health Sciences Centre, Toronto
Dr Alan Matsumoto, Chair, Department Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, Virginia
Dr Elizabeth Stewart, Chair, Division of Reproductive Endocrinology, Mayo Clinic College of Medicine, Rochester, Minnesota
Dr Togas Tulandi, Vice Chair, Department of Obstetrics and Gynecology, and Chair in Reproductive Medicine, McGill University, Montreal, Quebec
APPENDICES
Appendix 1: Literature Search Strategies
Search date: March 27, 2014
Databases searched: Ovid MEDLINE, Ovid MEDLINE In-Process, EMBASE, all EBM Databases (see below)
Q: MR-Guided High Intensity Focused Ultrasound for Uterine Fibroids
Limits: 2000-current; English
Filters: none
Databases: EBM Reviews - Cochrane Database of Systematic Reviews <2005 to February 2014>, EBM Reviews - ACP Journal Club <1991 to March 2014>, EBM Reviews - Database of Abstracts of Reviews of Effects <1st Quarter 2014>, EBM Reviews - Cochrane Central Register of Controlled Trials <January 2014>, EBM Reviews - Cochrane Methodology Register <3rd Quarter 2012>, EBM Reviews - Health Technology Assessment <1st Quarter 2014>, EBM Reviews - NHS Economic Evaluation Database <1st Quarter 2014>, EMBASE <1980 to 2014 Week 12>, Ovid MEDLINE(R) <1946 to March Week 3 2014>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <March 26, 2014>
Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp Leiomyoma/ | 30271 |
| 2 | Myoma/ | 3158 |
| 3 | Uterus/ | 95762 |
| 4 | Myometrium/ | 15359 |
| 5 | or/3–4 | 107631 |
| 6 | and/2,5 | 570 |
| 7 | Uterine Myomectomy/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed | 97 |
| 8 | Uterus Myoma/ use emez | 9297 |
| 9 | Myomectomy/ use emez | 3246 |
| 10 | (((uterine or uterus) adj2 fibro*) or fibromyoma* or (fibroid adj2 tumo?r*) or angioleiomyoma* or angiomyoma* or elastomyofibroma* or hemangioleiomyoma* or hemangiomyoma* or leimyoma* or leiomyoma* or leyomyoma* or myofibroma* or myofibromatosis or myoma*).ti,ab. | 39005 |
| 11 | or/1,6–10 | 51805 |
| 12 | exp High-Intensity Focused Ultrasound Ablation/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed | 895 |
| 13 | exp High Intensity Focused Ultrasound/ use emez | 2521 |
| 14 | “Magnetic Resonance Guided Focused Ultrasound Surgery”/ use emez | 24 |
| 15 | Magnetic Resonance Imaging, Interventional/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed | 768 |
| 16 | Interventional Magnetic Resonance Imaging/ use emez | 758 |
| 17 | Ultrasonic Therapy/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed | 8510 |
| 18 | Ultrasonography, Interventional/ use mesz,acp,cctr,coch,clcmr,dare,clhta,cleed | 14883 |
| 19 | Ultrasound/ use emez or Ultrasound Surgery/ use emez or Ultrasound Therapy/ use emez | 105154 |
| 20 | ((MR or MRI or magnetic resonance imag* or magnetic resonance) adj2 (guide* or ultrasound* or ultrasonograph*)).ti,ab. | 18151 |
| 21 | (ExAblate or Sonalleve or high intensity focused ultrasound* or HIFU* or focused ultrasound* or MRgFUS).ti,ab,dv. | 6557 |
| 22 | or/12–21 | 149158 |
| 23 | 11 and 22 | 1728 |
| 24 | limit 23 to (english language and yr=“2000 -Current”) [Limit not valid in CDSR,ACP Journal Club,DARE,CCTR,CLCMR; records were retained] | 1449 |
| 25 | remove duplicates from 24 | 1171 |
Appendix 2: Evidence Base
Table A1:
Characteristics of Reports on MRgHIFU Treatment of Uterine Fibroids
| Country, Device | Author, Year | Hospital(s) Source | Report Type | Recruitment Period | Study Size (Age) | Study Objective |
|---|---|---|---|---|---|---|
| Australia | ||||||
| ExAblate 2000 (InSightec Ltd., Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Dobrotwir A and Pun E, 2012 (94) | The Royal Women's Hospital, Melbourne, Victoria | Single site prospective longitudinal cohort study | May 2009 to April 2011 | 100 women (mean age 42 ± 7 years) | Treatment effectiveness; outcomes, 24-months follow-up |
| Brazil | ||||||
| ExAblate 2000 (InSightec Ltd., Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | De Melo F et al, 2009 (138) | LABS-D'OR Hospital Network, Rio de Janeiro | Case report | NR | 41-year-old woman | Technical report; treatment success with ablation focused only at tumour periphery at 12-month follow-up |
| China | ||||||
| HIFU 9000 (Shanghai Aishen Technology, Shanghai, China) and Valleylab Cool-Tip (Valleylab/Tyco Healthcare Group, Boulder, CO, US) | Meng X et al, 2010 (52) | Xijing Hospital, Shaanxi | RCT, USgHIFU versus radiofrequency ablation | March 2009 to August 2009 | 100 women: USgHIFU 50 women (mean age 35.6 ± 6.0 years; range, 26–47)) vs. RF 50 women (mean age 39.2 ± 5.7 years; range, 24–48) | Comparative study; RCT to compare the efficacy of USgHIFU with radiofrequency ablation |
| JC-HIFU (Chongqing Haifu Technology Co. Ltd, Chongqing, China) | Qin J et al, 2012 (54) | Chongquing University Medical Center, Chongquing | Case series nested within a cohort study | October 1, 2006, to October 1, 2009 | USgHIFU 435 women: 24 women (mean age 34.5 ± 4.5 years; range, 25–42) achieving unplanned pregnancy within 1 year of treatment | Reproductive report to review outcomes of unplanned pregnancies occurring in a cohort of women undergoing USgHIFU |
| JC-HIFU (Chongqing Haifu Technology Co. Ltd., Chongqing, China) | Wang X et al, 2013 (59) | Chongquing University Medical Center, Chongquing | RCT, USgHIFU versus abdominal myomectomy | NR | 120 women: USgHIFU 60 women (mean age 39.9 ± 5.2 years) and myomectomy 60 women (mean age 38.6 ± 4.4 years) | Comparative study; RCT to evaluate the effect of USgHIFU compared to myomectomy on immune function |
| JC-HIFU (Chongqing Haifu Technology Co. Ltd., Chongqing, China) | Wang X et al, 2013 (58) | Chongquing University Medical Center, Chongquing | RCT, USgHIFU versus abdominal myomectomy | NR | 110 premenopausal women: HIFU 55 women (mean age 39.2 ± 5.2 years) vs. myomectomy 55 women (mean age 38.1 ± 4.6 years) | Comparative study; RCT to evaluate the effect of USgHIFU compared to myomectomy on sexual function |
| JC-HIFU (Chongqing Haifu Technology Co. Ltd., Chongqing, China) | Wang F et al, 2014 (56) | Chongquing University Medical Center, Chongquing | Comparative prospective longitudinal cohort study, USgHIFU versus laparoscopic myomectomy | January 2010 to December 2011 | 130 premenopausal women: HIFU 89 women (mean age 37.9 ± 5.5 years) vs. myomectomy 41 women (mean age 38.4 ± 5.0 years) | Comparative cohort study to evaluate the effect of USgHIFU compared to laparoscopic myomectomy on complications, symptom relief, hospital stay, recovery, treatment satisfaction, QOL, and 12-month outcomes |
| Germany | ||||||
| ExAblate 2000 (InSightec Ltd, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Froling V et al, 2014 (80) | Charite-Universitatsmedizin, Berlin | Single site cohort study | July 2001 to July 2012 | 783 premenopausal women (median age 44.2 years) | Technical report to evaluate technical eligibility for UAE and MRgHIFU |
| ExAblate 2000 (InSightec Ltd, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Froling V et al, 2013, 2013 (126;137) | Charite-Universitatsmedizin, Berlin | Comparative prospective longitudinal cohort study, MRgHIFU versus UAE | 2002 to 2009 | 121 women: MRgHIFU 57 women (mean age 36.2 years; range, 29.2–41.0 years) vs. UAE 64 women (mean age 42.7; range, 33.6–52.2 years) | Comparative cohort study to evaluate eligibility and compare reintervention rates, symptom relief, HRQOL between MRgHIFU and UAE |
| ExAblate 2100 UF V2 (InSightec Ltd, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Trumm C et al, 2013 (91) | Klinikum der Lugwig-Maximilians-Universitat Munchen- Grobhadern, Munich | Single site prospective cohort follow-up study | November 2010 to June 2011 | 115 women (mean age 42 years; range, 25–54) | Treatment effectiveness; to evaluate safety and technical success of the second-generation ExAblate 2100 UF V2 system |
| India | ||||||
| ExAblate 2000 (InSightec Ltd) 1.5T MR (Signa; GE Healthcare | Desai S et al, 2012 (95) | Jaslok Hospital and Research Center, Mumbai | Single site prospective longitudinal cohort study | July 2010 to December 2010 | 50 women (mean age 36.2 ± 8.3 years; range, 21–53) | Treatment effectiveness; to evaluate safety and treatment success at 6-month follow-up |
| ExAblate 2010 (InSightec Ltd) −1.5T MR (Signa; GE Healthcarel | Himabindu Y et al, 2014 (105) | GSL General Hospital, Andhra Pradesh | Single site prospective longitudinal cohort study | February 2011 to October 2011 | 32 consecutive women (mean age 36.6 ± 6.23 years; range, 21–48) | Treatment effectiveness; to evaluate safety and treatment success at 6-month follow-up |
| ExAblate 2000 (InSightec Ltd., Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Nyapathy V et al, 2012 (139) | GSL General Hospital, Andhra Pradesh | Case report | NR | 44-year-old nulliparous woman | Technical report; to evaluate treatment success of MRgHIFU for fibroids with hyperintense signalling characteristics on MR T2WI fibroids and associated with urinary retention |
| Israel | ||||||
| ExAblate 2000 (InSightec Ltd., Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Machtinger R et al, 2012 (92) | Sheba Medical Center, Tel Hashomer | Single site prospective longitudinal cohort study | 2003 to 2008 | 87 premenopausal women (mean age 45.6 years ± 4.1; range, 36–53 | Treatment effectiveness; to evaluate factors associated with long-term success |
| ExAblate 2000 (InSightec Ltd, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Rabinovici J et al, 2010 (140) | 13 sites in 7 countries -reports from trials in and outside the US where desire for future pregnancy was an exclusion criteria; from 4 international sites where trial was designed for women specifically trying to conceive; and on pregnancies occurring in commercial treatment | Case series, regulatory reporting requirement | NR | 54 pregnancies in 51 women (mean age 37.2 ± 4.6 years; range, 28–49) | Reproductive report to evaluate pregnancy and obstetrical outcomes after HIFU |
| ExAblate 2000 (InSightec Ltd, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, US) | Rabinovici J et al, 2006 (125) | Sheba Medical Center, Tel Hashomer | Case report from ongoing study of MRgHIFU for benign uterine conditions | NR | 36-year-old woman | Reproductive report; a pregnancy and live birth report following MRgHIFU for adenomyotic uterus |
| Japan | ||||||
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (Signa; GE Healthcare Milwaukee, WI) | Funaki K et al, 2007 (72) | Shinsuma Hospital, Kobe | Single site prospective longitudinal cohort study | June 2004 to October 2005 | 63 women (mean age 40.5 years; range, 30–47) | Technical report to evaluate the relationship of fibroid reduction at 6-month follow-up to baseline signal intensity on pretreatment T2-weighted MR imaging of fibroids |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (Signa; GE Healthcare, Milwaukee, WI) | Funaki K et al, 2007 (72) | Shinsuma Hospital, Kobe | Single site prospective longitudinal cohort study | Beginning in 2004 | 35 women (median age 41 years; range, 30–48) | Technical report to evaluate the relationship of fibroid reduction at 12-month follow-up to baseline signal intensity on pretreatment T2-weighted MR imaging of fibroids |
| ExAblate 2000 version 4.1 or version 4.2 (InSightec, Haifa, Israel) 1.5T MR (Signa; GE Healthcare Milwaukee, WI) | Funaki K et al, 2009 (73) | Shinsuma Hospital, Kobe | Single site prospective longitudinal cohort study | June 2004 to June 2008 | 91 premenopausal women (mean age 40.4 ± 4.6 years) | Treatment effectiveness; to evaluate symptom improvement and fibroid volume change at 24-month follow-up |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (Signa; GE Healthcare Milwaukee, WI) | Fukunishi H et al, 2007 (99) | Shinsuma Hospital, Kobe | Case report | NR | 40-year-old woman (gravida 0) | Safety report; detection of unsuspected leiomyosarcoma |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Mikami K et al, 2008 (90) | Osaka University Graduate School of Medicine, Osaka | Single site retrospective cohort study | April 2003 to March 2004 | 48 women (mean age 44 years; range, 30–49) | Treatment effectiveness; to assess feasibility and effectiveness of MRgHIFU treatment at 12-month follow-up |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcarel Systems, Milwaukee, WI) | Morita Y et al, 2008 (96) | Itabashi Chuo Medical Center, Tokyo | Single site prospective longitudinal cohort study | January 2005 to February 2006 | 48 premenopausal women (mean age 42.6 ± 5.8 years; range, 24–51) | Technical report; to evaluate the relationship between the degree of uterine fibroid reduction and the degree of ablation by non-perfused volume |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare Milwaukee, WI) | Morita Y et al, 2009 (70) | Itabashi Chuo Medical Center, Tokyo | Single site prospective longitudinal cohort study | January 2005 to March 2006 | 83 premenopausal women (mean age 43 ± 5 years; range, 24–51) | Technical report; to evaluate the safety of MRgHIFU in relation to distance between treatment zone and uterine serosa at 12-month follow-up |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Morita Y et al, 2007 (123) | Itabashi Chuo Medical Center, Tokyo | Case report | NR | 29-year-old woman | Reproductive report; pregnancy outcome following MRgHIFU |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Okada A et al, 2009 (106) | 4 sites: Iseikai Hospital, Osaka; Itabashi Chuo Medical Center, Tokyo; Shinsuma General Hospital, Kobe; Aizu Chuo Hospital, Aizuwakamatsu | Multicentre prospective longitudinal cohort study | April 2003 to May 2006 | 287 women (mean age 42.5 ± 5.3 years; range, 24–60) | Technical report; to describe the learning curve effect of MRgHIFU for uterine fibroids over 12-month follow-up |
| Korea | ||||||
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI | Kim KA et al, 2011 (100) | CHA Gangnam Medical Center, Seoul | Case report | NR | 38-year-old woman | Safety report; spontaneous vaginal expulsion of ablated uterine fibroid |
| Sonalleve (Philips Healthcare, 1.5T MR (Achieva, Philips Healthcare, US) | Kim YS et al, 2012 (141;142) | Samsung Medical Center, Seoul | Retrospective cohort study | December 2010 to June 2011 | 27 women (mean age 44.5 ± 3.8 years; range, 35–50) | Technical report to evaluate initial clinical outcomes of HIFU one-layer strategy to treat large (> 10 cm in diameter) fibroids |
| Sonalleve (Philips Healthcare 1.5T MR (Achieva, Philips Healthcare, US) | Kim YS et al, 2012 (143) | 4 sites: Samsung Medical Center, Seoul, Korea; University Hospital Bordeaux, Segalen, France; University Medical Center, Utrech, Netherlands; University Hospital Schleswig-Holstein, Lubeck, Germany | Multicentre prospective cohort study | March 2009 to March 2010 | 33 pre- or peri-menopausal women (mean age 44.8 ± 5.2 years; range, 33–59) | Technical report to assess the accuracy and safety margin of volumetric HIFU based on MR thermometric analysis and effects of a feedback control technique |
| Sonalleve (Philips Healthcare 1.5T MR (Achieva, Philips Healthcare, US) | Kim YS et al, 2014 (88) | Samsung Medical Center, Seoul | Single site retrospective cohort study | December 2010 to August 2012 | 71 pre- or peri-menopausal women (mean age 43.3 years; range, 25–52) | Technical report to evaluate the relationship between intra-procedural thermal parameters and immediate or delayed therapeutic response |
| Sonalleve (Philips Healthcare,) 1.5T MR (Achieva, Philips Healthcare, US | Park MJ et al, 2013 (89) | Samsung Medical Center, Seoul | Single site retrospective cohort study | August 2009 to August 2011 | 43 women (mean age 43.7 ± 3.8 years; range, 35–50) | Technical report to examine factors affecting treatment speed of volumetric ablation including learning curve effects |
| Sonalleve (Philips Healthcare 1.5T MR (Achieva, Philips Healthcare, US) | Park MJ et al, 2013 (67) | Samsung Medical Center, Seoul | Single site retrospective case series | August 2010 to August 2012 | 13 women (mean age 40.5 ± 5.2 years; range, 34–52) | Technical report to evaluate a bowel manipulation technique to decrease screening failure rate |
| Sonalleve (Philips Healthcare,) 1.5T MR (Achieva, Philips Healthcare, US) | Park MJ et al, 2014 (82) | Samsung Medical Center, Seoul | Single site retrospective longitudinal cohort study | January 2011 to April 2012 | 79 women (mean age 43.6 ± 4.4 years; range, 34–52) | Treatment effectiveness; to evaluate the safety of complete or near-complete ablation and therapeutic efficacy at 3-month follow-up |
| ExAblate ExAblate 2000 (InSightec, Haifa, Israel) 3.0T MR (Signa HD, GE Healthcare, Milwaukee, WI) | Park H et al, 2012 (144) | CHA Bundang Medical center, Gyunggi-do | Case series | March 2007 to March 2009 | 135 women: 9 with pedunculated subserosal fibroid (mean age 39 years; range 25–47) | Treatment effectiveness; to evaluate outcomes of HIFU for pedunculated subserosal fibroids at 6-month follow-up |
| ExAblate ExAblate 2000 (InSightec, Haifa, Israel) 3.0T MR (Signa HD, GE Healthcare, Milwaukee, WI) | Yoon SW et al, 2010 (145) | CHA Bundang Medical Center, Gyunggi-do | Case report | In 2009, HIFU 9 years after a prior UAE | 45-year-old premenopausal woman | Technical report to evaluate the safety and effectiveness of HIFU after previous UAE treatment |
| ExAblate 2000 (InSightec, Haifa, Israel) 3.0T MR (Signa HD, GE Healthcare, Milwaukee, WI) | Yoon SW et al, 2011 (68) | CHA Bundang Medical Center, Gyunggi-do | Single site prospective cohort study | April 2008 to December 2008 | 20 consecutive premenopausal women (mean age 41.1 ± 4.0 years; range, 33–51) | Technical report; safety and effectiveness of HIFU using a custom patch to cover abdominal scars |
| ExAblate 2000 (InSightec, Haifa, Israel) 3.0T MR (Signa HD, GE Healthcare, Milwaukee, WI) | Yoon SW et al, 2013 (111) | CHA Bundang Medical Center, Gyunggi-do | Single centre prospective longitudinal cohort study | August 2006 to May 2007 | 60 consecutive women (mean age 41.3 ± 6.3 years, range 30–52) | Technical report to evaluate the relationship between the degree of ablation and the safety and treatment outcomes at 12-month follow-up |
| ExAblate 2000 (InSightec, Haifa, Israel) 3.0T MR (Signa HD, GE Healthcare, Milwaukee, WI) | Yoon SW et al, 2010 (124) | CHA Bundang Medical Center, Seongnam | Case report | NR | 31-year-old woman G0, P0 | Reproductive report; pregnancy following MRgHIFU |
| Netherlands | ||||||
| Sonalleve (Philips Healthcare) 1.5T MR (Achieva, Philips Healthcare, US) | Voogt M et al, 2012 (146) | University Medical Center, Utrech | Case reports | March 2010 to May 2012 | 2 women (37 years, 48 years) | Technical report to evaluate safety and effectiveness of targeted uterine artery ablation along with HIFU of uterine fibroid |
| Sonalleve (Philips Healthcare) 1.5T MR (Achieva, Philips Healthcare, US) | Voogt M et al, 2012 (42) | 4 sites: University Medical Center, Utrech Netherlands; Hospital St. Andre Bordeaux, France; Samsung Medical Center, Seoul, Korea; University Hospital Schleswig-Holstein, Lubeck, Germany | Multicentre prospective cohort study | NR | 33 pre- or perimenopausal women (mean age 44.8 ± 5.2 years) | Technical report to assess safety and technical feasibility of volumetric MRgHIFU ablation |
| Sonalleve (Philips Healthcare,) 1.5T MR (Achieva, Philips Healthcare, US) | Ikink M et al, 2013 (112) | University Medical Center, Utrech | Single centre prospective longitudinal cohort study | March 2010 to May 2012 | 51 pre- or perimenopausal women (mean age 45.3 ± 4.1 years) | Treatment effectiveness; to assess treatment efficacy of volumetric MRgHIFU ablation at 6-month follow-up |
| Norway | ||||||
| Sonalleve (Philips Healthcare) 3.0T MR (Achieva, Philips Healthcare, US) | Dorenberg E et al, 2013 (147) | Oslo University Hospital, Oslo | Case series | January 2010 to March 2011 | 7 women (mean age 44.6 years; range, 39–51) | Technical report to assess the safety and technical success of the Sonalleve system with 3T MR imaging |
| United Kingdom | ||||||
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Medical Systems, Milwaukee, WI) | Smart O et al, 2006 (77) | St Mary's Hospital, London | Single site prospective cohort study | NR | 50 premenopausal women (mean age 42 ± 4.9 years; range, 35–53) | Comparative study to evaluate the effects of GnRH fibroid pretreatment in 27 women compared to 23 age-matched women without fibroid pretreatment prior to HIFU |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Zaher S et al, 2009 (81) | St Mary's Hospital, London | Single site prospective cohort study | September 2005 to December 2006 | 144 women (mean age 42.8 years; range, 22–57) | Technical report to evaluate patient eligibility or suitability |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Zaher S et al, 2010 (69) | St Mary's Hospital, London | Single site prospective cohort study | March 2006 to May 2008 | 25 women (mean age 37 years; range, 29–52) | Technical report to evaluate a technique to treat patients with abdominal scars |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Zaher S et al, 2010 (121) | St Mary's Hospital, London | Case report | February 2007 | 39-year-old woman | Reproductive report; pregnancy and delivery outcome following MRgHIFU |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Zaher S et al, 2011 (122) | St Mary's Hospital, London | Case report | January 2008 | 45-year-old woman | Reproductive report; in vitro fertilization pregnancy after MRgHIFU |
| NR | Leon-Villapalos J et al, 2005 (101) | St Andrew's Centre for Plastic Surgery and Burns, Essex | Case report | NR | 39-year-old woman | Safety report; full thickness abdominal burn |
| United States | ||||||
| ExAblate 2000 version 4.2 (InSightec, Dallas, Texas) 3.0T MR (GE Healthcare, Milwaukee, WI) | Arleo E et al, 2007 (78) | New York Presbyterian Hospital, New York | Single site retrospective cohort review | April 2005 to December 2005 | 333 women | Technical report to assess the clinical and technical eligibility for MRgHIFU |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Behera M et al, 2010 (79) | Duke University Medical Center, North Carolina | Single site retrospective cohort review | November 2007 to February 2009 | 169 women | Technical report to assess the clinical and technical eligibility of patients for MRgHIFU |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Bouwsma E et al, 2011 (118) | NR | Case report | August 2009 | 37-year-old Asian woman | Reproductive report; pregnancy outcome after MRgHIFU |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Fennessy F et al, 2007 (49) | 5 sites: Brigham and Women's Hospital Boston MA; Mayo Clinic, Rochester MN, Johns Hopkins University School of Medicine, Baltimore MD; RadNet Management, Los Angeles CA; Lahey Clinic, Burlington MA | Multicentre prospective longitudinal cohort phase 3 clinical trial | April 2003 to December 2004 (original treatment guidelines); post 2004 (modified guidelines) | 160 consecutive women (mean age 46 years ± 4.3; range, 35–58 years) | Comparative study to compare the clinical outcomes at 12 months comparing 2 treatment protocols |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Gavrilova-Jordan LP et al, 2007 (119) | Mayo Clinic, Rochester MN | Case report | NR | 38-year-old woman | Reproductive report; pregnancy case report after MRgHIFU |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Gorny K et al, 2011 (97) | Mayo Clinic, Rochester MN | Single site prospective longitudinal cohort study | March 2005 to December 2009 | 150 women (mean age 45.6 ± 5.5 years; range, 31.9–58.5) | Treatment effectiveness; to evaluate the clinical and safety outcomes at 12 month follow-up |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Gorny K et al, 2014 (115) | Mayo Clinic, Rochester MN | Single site prospective longitudinal cohort study | March 2005 to November 2011 | 211 women (mean age 45.6 ± 5.8 years; range, 30–58) | Treatment effectiveness; to evaluate the reintervention rates in long-term follow-up |
| ExAblate 2000 (InSightec, Dallas, Texas) 1.5T MR (GE Healthcare, Milwaukee, WI) | Hanstede M et al, 2007 (120) | Brigham and Women's Hospital, Boston MA | Case report | January 2005 | 40-year-old woman | Reproductive report; pregnancy case report after MRgHIFU |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Hesley G et al, 2006 (93) | Mayo Clinic, Rochester MN | Single site (part of multicentre trial) prospective cohort study | Beginning in July 2002 | 42 women (mean age 46 years; range, 38–54) | Treatment effectiveness; to describe early clinical experience at Mayo clinic |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Hindley J et al, 2004 (109) | 7 sites: Brigham and Women's Hospital, Boston, MA; Johns Hopkins School of Medicine, Baltimore MD; Mayo Clinic, Rochester MN; Sheba Medical Center, Tel Hashomer, Israel; Hadassah Medical Center, Jerusalem, Israel; Charite Medical Center, Berlin | International multicentre phase 3 clinical trial | NR | 107 women (mean age 44.8 ± 4.9 years; range, 30–58) | Treatment effectiveness; to evaluate the early treatment results and post-treatment fibroid changes at 6-month follow-up |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Kim HS et al, 2011 (114) | Johns Hopkins University School of Medicine, Baltimore MD | Single site prospective longitudinal cohort clinical study | NR | 40 consecutive pre- and peri-menopausal women (mean age 46 ± 4.5 years) | Treatment effectiveness; to evaluate the long-term (up to 3 years) safety and clinical efficacy of MRgHIFU |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | LeBlang S et al, 2010 (43) | University Image-Guided Therapy Center, Boca Raton FL | Single site retrospective cohort clinical study | October 2004 to February 2007 | 80 consecutively treated women (mean age 46 years; range, 34–55) | Technical report to assess degree ablation and shrinkage after FDA protocol for commercial trials |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Lenard Z et al, 2008 (113) | Brigham and Women's Hospital, Boston MA | Single centre prospective longitudinal cohort clinical study | February 2002 and December 2005 | 66 women (mean age 45.4 ± 4.4 years) | Technical report to evaluate MR predictors of treatment success defined by fibroid reduction and symptom relief at 12 months |
| ExAblate 2000 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Machtinger R et al, 2013 (107) | 9 US sites: Brigham and Women's Hospital, Boston MA; Johns Hopkins University School of Medicine, Baltimore MD; Mayo Clinic, Rochester MN; Radnet Beverley Hills CA; Lahey, Burlington MA; Sightline Houston, TX; North Texas Uterine Fibroid Institute, Dallas TX; UMRI Boca Raton FL; Virtua, Voorhees NJ | Phase 2/4 prospective multicentre cohort clinical trial | January 2005 to April 2006 | 137 women (mean age 44.8 ± 4.8 years; range, 34–53); includes 64 women from the phase 3 study and 73 women from the phase 4 study of African American women | Comparative study to compare the safety and effectiveness of MRgHIFU in African American versus non–African American women |
| ExAblate 2000 (InSightec, Haifa., Israel) 1.5T MR (GE Healthcare, Milwaukee, WI | Stewart E et al, 2003 (84) | 5 sites: Brigham and Women's Hospital, Boston MA; St Mary's Hospital, London; Sheba Medical Center, Tel Hashomer, Israel; Hadassah Medical Center, Jerusalem, Israel; Charite Medical Center, Berlin | Multicentre prospective clinical trial; patients at 3 sites underwent planned hysterectomy after MRgHIFU | NR | 55 pre- or perimenopausal women (mean age 46.3 ± 0.7 years; range, 36–57) | Technical report to evaluate the safety of MRgHIFU and the degree of induced necrosis in uterine fibroids under real-time thermal monitoring with MRI |
| ExAblate 2000 version 2.3 or 2.4 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Stewart E et al, 2007 (83) | 5 sites (MRgHIFU for Uterine Fibroid Group): Brigham and Women's Hospital, Boston MA; Johns Hopkins Hospital, Baltimore MD; Mayo Clinic, Rochester MN; St Mary's Hospital, London; Sheba Medical Center, Tel Hashomer, Israel | Multicentre prospective clinical trial; pooled data from 4 separate trials with treatment protocols reported to or mandated by FDA to assess 24-month clinical end points | February 2002 to March 2006 | 359 women from 4 study groups. Group 1: phase 3 pivotal study (109 women, mean age 45.3 ± 4.8 years); Group 2: phase 3 study continued access in Europe (65 women mean age 43.9 ± 6.4 years); Group 3: phase 3 continued access in the United States (160 women mean age 46.4 ± 4.4 years); Group 4: post-market African American study in the United States (82 women, mean age 44.1 ± 5 years) | Treatment effectiveness; to evaluate long-term (3-year follow-up) outcomes of MRgHIFU treatment |
| NR | Taran F et al, 2009 (133) | 14 sites. 7 sites for MRgHIFU: Brigham and Women's Hospital, Boston MA; Johns Hopkins Hospital, Baltimore MD; Mayo Clinic, Rochester MN, St Mary's Hospital, London; Sheba Medical Center, Tel Hashomer, Israel; Hadassah Medical Center, Jerusalem, Israel; Charite Medical Center, Berlin; 7 separate sites for hysterectomy | Comparative study MRgHIFU versus hysterectomy | NR | MRgHIFU 109 women (mean age 44.8 ± 4.9 years); hysterectomy 83 women (mean age 44.4 ± 5.6 years) | Comparative study to compare MRgHIFU with hysterectomy for complications, adverse events, and HRQOL |
| NA | Taran F et al, 2010 (64) | The first international symposium on FUS surgery in Washington, DC | Survey of conference participants | October 6–7, 2008 | 13 symposium participants (5 gynecologists, 8 radiologists) | Opinion survey to evaluate participants reported patient selection criteria for HIFU |
| ExAblate 2000 version 2.3 or 2.4 (InSightec, Haifa, Israel) 1.5T MR (GE Healthcare, Milwaukee, WI) | Tempany C et al, 2003 (86) | Brigham and Women's Hospital, Boston MA | Single site prospective phase 1/2 study | NR | 9 premenopausal women (mean age 43.3 years; range, 39–51) | Technical report to test the feasibility and safety of MRgHIFU and evaluate the degree of target ablation with histopathological correlation (HIFU was followed by hysterectomy within 30 days) |
| Sonalleve (Philips Medical Systems,) 1.5T MR (Achieva, Philips Healthcare, US) | Venkatesan A et al, 2012 (85) | 2 sites: NIH Center Interventional Oncology, Bethesda MD and St Luke's Episcopal Hospital, Houston TX | Multicentre phase 1 clinical trial | NR | 11 pre- or perimenopausal women (mean age 46 years; range, 30–55) | Technical report to evaluate the safety and targeting accuracy of Sonalleve HIFU and review the imaging to histopathological correlation of target ablation (HIFU was followed by hysterectomy within 30 days) |
Abbreviations: GnRH, gonadotropin-releasing hormone analogue; HRQOL, health-related quality of life; MR, magnetic resonance; MRgHIFU, magnetic resonance-guided high-intensity focused ultrasound; NA, not appropriate; NR, not reported; QOL, quality of life; RF, radiofrequency; UAE, uterine artery embolization; US, United States; USgHIFU, ultrasound-guided high-intensity focused ultrasound.; vs., versus.
Table A2:
GRADE Evidence Profile for MRgHIFU Treatment of Uterine Fibroids
| Number of Studies (Initial Grade) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Technical success | |||||||
| 14 observational cohort studies (Low) | No serious limitations | No serious inconsistency | No serious limitations | No serious limitations | Unevaluated | (+1)a (dose-response) | Moderate |
| Safety (major adverse events) | |||||||
| 20 observational cohort studies (Low) | No serious limitations | No serious inconsistency | No serious limitations | No serious limitations | Unevaluated | (+1)b | Moderate |
| Symptom reduction (short term) | |||||||
| 12 observational cohort studies (Low) | Serious limitations (–1)c | No serious inconsistency | No serious limitations | No serious limitations | Unevaluated | (+2)d (large magnitude effect) | Moderate |
| Durability of symptom reduction (> 1 year) | |||||||
| 3 cohort studies (Low) | Serious limitations (–1)e | No serious inconsistency | No serious limitations | No serious limitations | Unevaluated | NA | Low |
| Fertility (pregnancy) | |||||||
| 5 cohort studies (Low) | Serious limitations (–1)e | Serious inconsistency (–1)e | Serious limitations (–1)e | Serious limitations (–1)e | Unevaluated | NA | Very low |
| Comparative effectiveness | |||||||
| Comparative studies with MRgHIFU are limited (no RCTs, few small selected groups) and insufficient for any meaningful comparisons between HIFU with different methods of guidance, other uterine-preserving options (UAE, myomectomy), or hysterectomy, other than comparisons of recovery trajectories which are related to the invasiveness of the treatment and their related protocols. | |||||||
Abbreviations: MRgHIFU, magnetic resonance–guided high-intensity focused ultrasound; NA, not available; RCT, randomized controlled trial; UAE, uterine artery embolization.
The degree of technical success is directly related to the ability to select appropriate patients, manage patients during the procedure, and utilize appropriate mitigation strategies.
Safety is directly related to adherence to the extensive technical safeguards, targeting, and real-time MR thermal monitoring.
Fibroid-related symptoms were evaluated by a validated disease-specific instrument at numerous institutes and in many countries, all consistently reporting statistically and clinically significant improvements over known control reference values.
The durability of symptom relief was only evaluated in a few studies and generally only for 2 or 3 years. There is convincing evidence that the symptom durability is dependent on the degree of initially induced thermal coagulative necrosis.
None of the cohort studies were designed to evaluate reproductive outcomes, and reproductive intent or history of the women was unknown.
References
- (1).Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril. 2007. Apr; 87 (4):725–36. [DOI] [PubMed] [Google Scholar]
- (2).Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009. Apr; 91 (4):1215–23. [DOI] [PubMed] [Google Scholar]
- (3).Johnson JA, Tough S. Delayed child-bearing. J Obstet Gynaecol Can. 2012. Jan; 34 (1):80–93. [DOI] [PubMed] [Google Scholar]
- (4).Flynn M, Jamison M, Datta S, Myers E. Health care resource use for uterine fibroid tumors in the United States. Am J Obstet Gynecol. 2006. Oct; 195 (4):955–64. [DOI] [PubMed] [Google Scholar]
- (5).Hartmann KE, Birnbaum H, Ben-Hamadi R, Wu EQ, Farrell MH, Spalding J, et al. Annual costs associated with diagnosis of uterine leiomyomata. Obstet Gynecol. 2006. Oct; 108 (4):930–7. [DOI] [PubMed] [Google Scholar]
- (6).Lee DW, Ozminkowski RJ, Carls GS, Wang S, Gibson TB, Stewart EA. The direct and indirect cost burden of clinically significant and symptomatic uterine fibroids. J Occup Environ Med. 2007. May; 49 (5):493–506. [DOI] [PubMed] [Google Scholar]
- (7).Rein MS, Barbieri RL, Friedman AJ. Progesterone: a critical role in the pathogenesis of uterine myomas. Am J Obstet Gynecol. 1995. Jan; 172 (1 Pt 1):14–8. [DOI] [PubMed] [Google Scholar]
- (8).Sozen I, Arici A. Cellular biology of myomas: interaction of sex steroids with cytokines and growth factors. Obstet Gynecol Clin North Am. 2006. Mar; 33 (1):41–58. [DOI] [PubMed] [Google Scholar]
- (9).Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Intl J Womens Health. 2013; 6 (1): 95–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Munro MG, Critchley HO, Fraser IS. The FIGO systems for nomenclature and classification of causes of abnormal uterine bleeding in the reproductive years: who needs them? Am J Obstet Gynecol. 2012. Oct; 207 (4):259–65. [DOI] [PubMed] [Google Scholar]
- (11).Chen YH, Lin HC, Chen SF, Lin HC. Increased risk of preterm births among women with uterine leiomyoma: a nationwide population-based study. Hum Reprod. 2009. Dec; 24 (12):3049–56. [DOI] [PubMed] [Google Scholar]
- (12).Ciavattini A, Clemente N, Delli CG, Di GJ, Giannubilo SR, Tranquilli AL. Number and size of uterine fibroids and obstetric outcomes. J Matern Fetal Neonatal Med. 2014. Jun 5;1–5. [DOI] [PubMed] [Google Scholar]
- (13).Jaques AM, Amor DJ, Baker HW, Healy DL, Ukoumunne OC, Breheny S, et al. Adverse obstetric and perinatal outcomes in subfertile women conceiving without assisted reproductive technologies. Fertil Steril. 2010. Dec; 94 (7):2674–9. [DOI] [PubMed] [Google Scholar]
- (14).Lai J, Caughey AB, Qidwai GI, Jacoby AF. Neonatal outcomes in women with sonographically identified uterine leiomyomata. J Matern Fetal Neonatal Med. 2012. Jun; 25 (6):710–3. [DOI] [PubMed] [Google Scholar]
- (15).Shavell VI, Thakur M, Sawant A, Kruger ML, Jones TB, Singh M, et al. Adverse obstetric outcomes associated with sonographically identified large uterine fibroids. Fertil Steril. 2012. Jan; 97 (1):107–10. [DOI] [PubMed] [Google Scholar]
- (16).Uterine leiomyomata. Number 192–May 1994. ACOG technical bulletin. Int J Gynaecol Obstet. 1994. Jul; 46 (1):73–82. [PubMed] [Google Scholar]
- (17).Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003. Jan; 188 (1):100–7. [DOI] [PubMed] [Google Scholar]
- (18).Eltoukhi HM, Modi MN, Weston M, Armstrong AY, Stewart EA. The health disparities of uterine fibroid tumors for African American women: a public health issue. Am J Obstet Gynecol. 2014. Mar; 210 (3):194–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Kjerulff KH, Langenberg P, Seidman JD, Stolley PD, Guzinski GM. Uterine leiomyomas. racial differences in severity, symptoms and age at diagnosis. J Reprod Med. 1996. Jul; 41 (7):483–90. [PubMed] [Google Scholar]
- (20).Wechter ME, Stewart EA, Myers ER, Kho RM, Wu JM. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011. Nov; 205 (5):492–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (21).Borah BJ, Nicholson WK, Bradley L, Stewart EA. The impact of uterine leiomyomas: a national survey of affected women. Am J Obstet Gynecol. 2013. Oct; 209 (4): 319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Spies JB, Coyne K, Guaou GN, Boyle D, Skyrnarz-Murphy K, Gonzalves SM. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002. Feb; 99 (2):290–300. [DOI] [PubMed] [Google Scholar]
- (23).Harding G, Coyne KS, Thompson CL, Spies JB. The responsiveness of the uterine fibroid symptom and health-related quality of life questionnaire (UFS-QOL). Health Qual Life Outcomes. 2008; 6 (99): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Spies JB, Bradley LD, Guido R, Maxwell GL, Levine BA, Coyne K. Outcomes from leiomyoma therapies: comparison with normal controls. Obstet Gynecol. 2010. Sep; 116 (3):641–52. [DOI] [PubMed] [Google Scholar]
- (25).Lefebvre G, Vilos G, Allaire C, Jeffrey J, Arneja J, Birch C, et al. The management of uterine leiomyomas. J Obstet Gynaecol Can. 2003. May; 25 (5):396–418. [PubMed] [Google Scholar]
- (26).Talaulikar VS, Manyonda IT. Ulipristal acetate: a novel option for the medical management of symptomatic uterine fibroids. Adv Ther. 2012; 29 (8): 655–63. [DOI] [PubMed] [Google Scholar]
- (27).Stovall DW. Alternatives to hysterectomy: focus on global endometrial ablation, uterine fibroid embolization, and magnetic resonance-guided focused ultrasound. Menopause. 2011; 18 (4): 437–44. [DOI] [PubMed] [Google Scholar]
- (28).Toor SS, Jaberi A, Macdonald DB, McInnes MD, Schweitzer ME, Rasuli P. Complication rates and effectiveness of uterine artery embolization in the treatment of symptomatic leiomyomas: a systematic review and meta-analysis. Am J Roentgenol. 2012. Nov; 199 (5):1153–63. [DOI] [PubMed] [Google Scholar]
- (29).Iversen H, Lenz S, Dueholm M. Ultrasound-guided radiofrequency ablation of symptomatic uterine fibroids: short-term evaluation of effect of treatment on quality of life and symptom severity. Ultrasound Obstet Gynecol. 2012. Oct; 40 (4):445–51. [DOI] [PubMed] [Google Scholar]
- (30).Law P, Gedroyc WMW, Regan L. Magnetic resonance-guided percutaneous laser ablation of uterine fibroids. J Magn Reson Imaging. 2000; 12 (4): 565–70. [DOI] [PubMed] [Google Scholar]
- (31).Wang F, Zhang J, Han ZY, Cheng ZG, Zhou HY, Feng L, et al. Imaging manifestation of conventional and contrast-enhanced ultrasonography in percutaneous microwave ablation for the treatment of uterine fibroids. Eur J Radiol. 2012. Nov; 81 (11):2947–52. [DOI] [PubMed] [Google Scholar]
- (32).Dunn S, Wise MR, Johnson LM, Anderson G, Ferris LE, Yeritsyan N, and et al. Ontario Women's Health Equity Report: Improving Health and Promoting Health Equity in Ontario. Bierman AS, editor. Toronto: Ontario Ministry of Health and Long-Term Care; 2011.. Chapter 10, Reproductive and Gynaecological Health; 1–164. [Google Scholar]
- (33).Dicker RC, Greenspan JR, Strauss LT, Cowart MR, Scally MJ, Peterson HB, et al. Complications of abdominal and vaginal hysterectomy among women of reproductive age in the United States. the collaborative review of sterilization. Am J Obstet Gynecol. 1982. Dec 1; 144 (7):841–8. [DOI] [PubMed] [Google Scholar]
- (34).Kafy S, Huang JY, Al-Sunaidi M, Wiener D, Tulandi T. Audit of morbidity and mortality rates of 1792 hysterectomies. J Minim Invasive Gynecol. 2006. Jan; 13 (1):55–9. [DOI] [PubMed] [Google Scholar]
- (35).Makinen J, Johansson J, Tomas C, Tomas E, Heinonen PK, Laatikainen T, et al. Morbidity of 10,110 hysterectomies by type of approach. Hum Reprod. 2001. Jul; 16 (7):1473–8. [DOI] [PubMed] [Google Scholar]
- (36).Tan N, McClure T, Tarnay C, Johnson M., Lu D, et al. Women seeking second opinion for symptomatic uterine leiomyoma: role of comprehensive fibroid center. J Ther Ultrasound. 2014; 2 (2): 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Ankem K. Information-seeking behavior of women in their path to an innovative alternate treatment for symptomatic uterine fibroids. J Med Libr Assoc. 2007. Apr; 95 (2):164–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Tyshlek D, Auby JF, Haar G, Ananel A, Foley J, Eames M, et al. Focused ultrasound development and clinical adoption: 2013 update on the growth of the field. J Ther Ultrasound. 2014; 2 (0): 2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (39).Ellis S, Rieke V, Kohi M, Westphalen AC. Clinical applications for magnetic resonance guided high intensity focused ultrasound (MRgHIFU): present and future. J Med Imaging Radiat Oncol. 2013; 57 (4): 391–9. [DOI] [PubMed] [Google Scholar]
- (40).Hesley GK, Gorny KR, Henrichsen TL, Woodrum DA, Brown DL. A clinical review of focused ultrasound ablation with magnetic resonance guidance: an option for treating uterine fibroids. Ultrasound Q. 2008; 24 (2): 131–9. [DOI] [PubMed] [Google Scholar]
- (41).Roberts A. Magnetic resonance-guided focused ultrasound for uterine fibroids. Semin Interven Radiol. 2008; 25 (4): 394–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Voogt MJ, Trillaud H, Kim YS, Mali WPTM, Barkhausen J, Bartels LW, et al. Volumetric feedback ablation of uterine fibroids using magnetic resonance-guided high intensity focused ultrasound therapy. Eur Radiol. 2012; 22 (2): 411–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Leblang SD, Hoctor K, Steinberg FL. Leiomyoma shrinkage after MRI-guided focused ultrasound treatment: report of 80 patients. Am J Roentgenol. 2010; 194 (1): 274–80. [DOI] [PubMed] [Google Scholar]
- (44).Coakley FV, Foster BR, Farsad K, Hung AY, Wilder KJ, Amling CL, et al. Pelvic applications of MR-guided high intensity focused ultrasound. Abdom Imaging. 2013; 38 (5): 1120–9. [DOI] [PubMed] [Google Scholar]
- (45).Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso-Coello P, et al. GRADE guidelines: 9. rating up the quality of evidence. J Clin Epidemiol. 2011. Dec; 64 (12):1311–6. [DOI] [PubMed] [Google Scholar]
- (46).Goodman C. Report from the Swedish Council on Technology Assessment in Health Care (SBU). literature searching and evidence interpretation for assessing health care practices. Int J Technol Assess Health Care. 1994; 10 (4): 714–5. [DOI] [PubMed] [Google Scholar]
- (47).Clark NA, Mumford SL, Segars JH. Reproductive impact of MRI-guided focused ultrasound surgery for fibroids: a systematic review of the evidence. Curr Opin Obstet Gynecol. 2014. Jun; 26 (3):151–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (48).Gizzo S, Saccardi C, Patrelli TS, Ancona E, Noventa M, Fagherazzi S, et al. Magnetic resonance-guided focused ultrasound myomectomy: safety, efficacy, subsequent fertility and quality-of-life improvements, a systematic review. Reprod Sci. 2014; 21 (4): 465–76. [DOI] [PubMed] [Google Scholar]
- (49).Fennessy FM, Tempany CM, McDannold NJ, So MJ, Hesley G, Gostout B, et al. Uterine leiomyomas: MR imaging-guided focused ultrasound surgery - results of different treatment protocols. Radiology. 2007; 243 (3): 885–93. [DOI] [PubMed] [Google Scholar]
- (50).Cho JY, Kim SH, Kim SY, Moon SK, Li J. Efficacy and safety of daily repeated sonographically guided high-intensity focused ultrasound treatment of uterine fibroids: preliminary study. J Ultrasound Med. 2013; 32 (3): 397–406. [DOI] [PubMed] [Google Scholar]
- (51).Li Q, Xiao YB, Liang ZG, Chen JY, Wang ZB. Ablation of leiomyomas using a combination of HIFU and iodized oil in vitro. Ultrasound Med Biol. 2012; 38 (9): 1576–81. [DOI] [PubMed] [Google Scholar]
- (52).Meng X, He G, Zhang J, Han Z, Yu M, Zhang M, et al. A comparative study of fibroid ablation rates using radio frequency or high-intensity focused ultrasound. Cardiovasc Intervent Radiol. 2010; 33 (4): 794–9. [DOI] [PubMed] [Google Scholar]
- (53).Peng S, Xiong Y, Li K, He M, Deng Y, Chen L, et al. Clinical utility of a microbubble-enhancing contrast (“SonoVue”) in treatment of uterine fibroids with high intensity focused ultrasound: a retrospective study. Eur J Radiol. 2012; 81 (12): 3832–8. [DOI] [PubMed] [Google Scholar]
- (54).Qin J, Chen J-Y, Zhao W-P, Hu L, Chen W-Z, Wang Z-B. Outcome of unintended pregnancy after ultrasound-guided high-intensity focused ultrasound ablation of uterine fibroids. Int J Gynaecol Obstet. 2012; 117 (3): 273–7. [DOI] [PubMed] [Google Scholar]
- (55).Ren X-L, Zhou X-D, Yan R-L, Liu D, Zhang J, He G-B, et al. Sonographically guided extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: midterm results. J Ultrasound Med. 2009; 28 (1): 100–3. [DOI] [PubMed] [Google Scholar]
- (56).Wang F, Tang L, Wang L, Wang X, Chen J, Liu X, et al. Ultrasound-guided high-intensity focused ultrasound vs laparoscopic myomectomy for symptomatic uterine myomas. J Minim Invasive Gynecol. 2014; 21 (2): 279–84. [DOI] [PubMed] [Google Scholar]
- (57).Wang W, Wang Y, Wang T, Wang J, Wang L, Tang J. Safety and efficacy of US-guided high-intensity focused ultrasound for treatment of submucosal fibroids. Eur Radiol. 2012; 22 (11): 2553–8. [DOI] [PubMed] [Google Scholar]
- (58).Wang X, Qin J, Wang L, Chen J, Chen W, Tang L. Effect of high-intensity focused ultrasound on sexual function in the treatment of uterine fibroids: comparison to conventional myomectomy. Arch Gynecol Obstet. 2013; 288 (4): 851–8. [DOI] [PubMed] [Google Scholar]
- (59).Wang X, Qin J, Chen J, Wang L, Chen W, Tang L. The effect of high-intensity focused ultrasound treatment on immune function in patients with uterine fibroids. Int J Hyperthermia. 2013; 29 (3): 225–33. [DOI] [PubMed] [Google Scholar]
- (60).Zhang L, Chen W-Z, Liu Y-J, Hu X, Zhou K, Chen L, et al. Feasibility of magnetic resonance imaging-guided high intensity focused ultrasound therapy for ablating uterine fibroids in patients with bowel lies anterior to uterus. Eur J Radiol. 2010; 73 (2): 396–403. [DOI] [PubMed] [Google Scholar]
- (61).Zhao W-P, Chen J-Y, Zhang L, Li Q, Qin J, Peng S, et al. Feasibility of ultrasound-guided high intensity focused ultrasound ablating uterine fibroids with hyperintense on T2-weighted MR imaging. Eur J Radiol. 2013; 82 (1): e43–e49. [DOI] [PubMed] [Google Scholar]
- (62).Zhou XD, Ren XL, Zhang J, He GB, Zheng MJ, Tian X, et al. Therapeutic response assessment of high intensity focused ultrasound therapy for uterine fibroid: utility of contrast-enhanced ultrasonography. Eur J Radiol. 2007; 62 (2): 289–94. [DOI] [PubMed] [Google Scholar]
- (63).Park SB. Features of the hypointense solid lesions in the female pelvis on T2-weighted MRI. J Magn Reson Imaging. 2014; 39 (3): 493–503. [DOI] [PubMed] [Google Scholar]
- (64).Taran FA, Hesley GK, Gorny KR, Stewart EA. What factors currently limit magnetic resonance-guided focused ultrasound of leiomyomas? a survey conducted at the first international symposium devoted to clinical magnetic resonance-guided focused ultrasound. Fertil Steril. 2010; 94 (1): 331–4. [DOI] [PubMed] [Google Scholar]
- (65).Yoon S-W, Lee C, Cha SH, Yu J-S, Na Y-J, Kim KA, et al. Patient selection guidelines in MR-guided focused ultrasound surgery of uterine fibroids: a pictorial guide to relevant findings in screening pelvic MRI. Eur Radiol. 2008; 18 (12): 2997–3006. [DOI] [PubMed] [Google Scholar]
- (66).Kim Y-S, Bae D-S, Park MJ, Viitala A, Keserci B, Rhim H, et al. Techniques to expand patient selection for MRI-guided high-intensity focused ultrasound ablation of uterine fibroids. Am J Roentgenol. 2014; 202 (2): 443–51. [DOI] [PubMed] [Google Scholar]
- (67).Park MJ, Kim Y-S, Rhim H, Lim HK. Technique to displace bowel loops in MRI-guided high-intensity focused ultrasound ablation of fibroids in the anteverted or anteflexed uterus. Am J Roentgenol. 2013; 201 (5): W761–W764. [DOI] [PubMed] [Google Scholar]
- (68).Yoon S-W, Seong SJ, Jung S-G, Lee SY, Jun HS, Lee JT. Mitigation of abdominal scars during MR-guided focused ultrasound treatment of uterine leiomyomas with the use of an energy-blocking scar patch. J Vasc Interv Radiol. 2011; 22 (12): 1747–50. [DOI] [PubMed] [Google Scholar]
- (69).Zaher S, Gedroyc W, Lyons D, Regan L. A novel method to aid in the visualisation and treatment of uterine fibroids with MRgFUS in patients with abdominal scars. Eur J Radiol. 2010; 76 (2): 269–73. [DOI] [PubMed] [Google Scholar]
- (70).Morita Y, Takeuchi S, Hikida H, Ohashi H, Ito N. Decreasing margins to the uterine serosa as a method for increasing the volume of fibroids ablated with magnetic resonance-guided focused ultrasound surgery. Eur J Obstet Gynecol and Reprod Biol. 2009; 146 (1): 92–5. [DOI] [PubMed] [Google Scholar]
- (71).Funaki K, Fukunishi H, Funaki T, Kawakami C. Mid-term outcome of magnetic resonance-guided focused ultrasound surgery for uterine myomas: from six to twelve months after volume reduction. J Minim Invasive Gynecol. 2007; 14 (5): 616–21. [DOI] [PubMed] [Google Scholar]
- (72).Funaki K, Fukunishi H, Funaki T, Sawada K, Kaji Y, Maruo T. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol. 2007; 196 (2): 184. [DOI] [PubMed] [Google Scholar]
- (73).Funaki K, Fukunishi H, Sawada K. Clinical outcomes of magnetic resonance-guided focused ultrasound surgery for uterine myomas: 24-month follow-up. Ultrasound Obstet Gynecol. 2009; 34 (5): 584–9. [DOI] [PubMed] [Google Scholar]
- (74).Lethaby A, Vollenhoven B, Sowter M. Efficacy of pre-operative gonadotrophin hormone releasing analogues for women with uterine fibroids undergoing hysterectomy or myomectomy: a systematic review. BJOG. 2002. Oct; 109 (10):1097–108. [DOI] [PubMed] [Google Scholar]
- (75).Matta WH, Shaw RW, Nye M. Long-term follow-up of patients with uterine fibroids after treatment with the LHRH agonist buserelin. Br J Obstet Gynaecol. 1989. Feb; 96 (2):200–6. [DOI] [PubMed] [Google Scholar]
- (76).Rutgers JL, Spong CY, Sinow R, Heiner J. Leuprolide acetate treatment and myoma arterial size. Obstet Gynecol. 1995. Sep; 86 (3):386–8. [DOI] [PubMed] [Google Scholar]
- (77).Smart OC, Hindley JT, Regan L, Gedroyc WG. Gonadotrophin-releasing hormone and magnetic-resonance-guided ultrasound surgery for uterine leiomyomata. Obstet Gynecol. 2006; 108 (1): 49–54. [DOI] [PubMed] [Google Scholar]
- (78).Arleo EK, Khilnani NM, Ng A, Min RJ. Features influencing patient selection for fibroid treatment with magnetic resonance-guided focused ultrasound. J Vasc Interv Radiol. 2007; 18 (5): 681–5. [DOI] [PubMed] [Google Scholar]
- (79).Behera MA, Leong M, Johnson L, Brown H. Eligibility and accessibility of magnetic resonance-guided focused ultrasound (MRgFUS) for the treatment of uterine leiomyomas. Fertil Steril. 2010; 94 (5): 1864–8. [DOI] [PubMed] [Google Scholar]
- (80).Froling V, Kroncke TJ, Schreiter NF, Scheurig-Muenkler C, Collettini F, Hamm B, et al. Technical eligibility for treatment of magnetic resonance-guided focused ultrasound surgery. Cardiovasc Intervent Radiol. 2014. Apr; 37 (2):445–50. [DOI] [PubMed] [Google Scholar]
- (81).Zaher S, Gedroyc WM, Regan L. Patient suitability for magnetic resonance guided focused ultrasound surgery of uterine fibroids. Eur J Obstet Gynecol Reprod Biol. 2009; 143 (2): 98–102. [DOI] [PubMed] [Google Scholar]
- (82).Park MJ, Kim Y-S, Rhim H, Lim HK. Safety and therapeutic efficacy of complete or near-complete ablation of symptomatic uterine fibroid tumors by MR imaging-guided high-intensity focused US therapy. J Vasc Interv Radiol. 2014; 25 (2): 231–9. [DOI] [PubMed] [Google Scholar]
- (83).Stewart EA, Gostout B, Rabinovici J, Kim HS, Regan L, Tempany CMC. Sustained relief of leiomyoma symptoms by using focused ultrasound surgery. Obstet Gynecol. 2007; 110 (2 I): 279–87. [DOI] [PubMed] [Google Scholar]
- (84).Stewart EA, Gedroyc WMW, Tempany CMC, Quade BJ, Inbar Y, Ehrenstein T, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol. 2003; 189 (1): 48–54. [DOI] [PubMed] [Google Scholar]
- (85).Venkatesan AM, Partanen A, Pulanic TK, Dreher MR, Fischer J, Zurawin RK, et al. Magnetic resonance imaging-guided volumetric ablation of symptomatic leiomyomata: correlation of imaging with histology. J Vasc Interv Radiol. 2012; 23 (6): 786–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (86).Tempany CMC, Stewart EA, McDannold N, Quade BJ, Jolesz FA, Hynynen K. MR imaging-guided focused ultrasound surgery of uterine leiomyomas: a feasibility study. Radiology. 2003; 226 (3): 897–905. [DOI] [PubMed] [Google Scholar]
- (87).Rabinovici J, Inbar Y, Revel A, Zalel Y, Gomori JM, Itzchak Y, et al. Clinical improvement and shrinkage of uterine fibroids after thermal ablation by magnetic resonance-guided focused ultrasound surgery. Ultrasound Obstet Gynecol. 2007; 30 (5): 771–7. [DOI] [PubMed] [Google Scholar]
- (88).Kim Y-S, Park MJ, Keserci B, Nurmilaukas K, Kohler MO, Rhim H, et al. Uterine fibroids: postsonication temperature decay rate enables prediction of therapeutic responses to MR imaging-guided high-intensity focused ultrasound ablation. Radiology. 2014; 270 (2): 589–600. [DOI] [PubMed] [Google Scholar]
- (89).Park MJ, Kim Y-S, Keserci B, Rhim H, Lim HK. Volumetric MR-guided high-intensity focused ultrasound ablation of uterine fibroids: treatment speed and factors influencing speed. Eur Radiol. 2013; 23 (4): 943–50. [DOI] [PubMed] [Google Scholar]
- (90).Mikami K, Murakami T, Okada A, Osuga K, Tomoda K, Nakamura H. Magnetic resonance imaging-guided focused ultrasound ablation of uterine fibroids: early clinical experience. Radiat Med. 2008; 26 (4): 198–205. [DOI] [PubMed] [Google Scholar]
- (91).Trumm CG, Stahl R, Clevert D-A, Herzog P, Mindjuk I, Kornprobst S, et al. Magnetic resonance imaging-guided focused ultrasound treatment of symptomatic uterine fibroids: impact of technology advancement on ablation volumes in 115 patients. Invest Radiol. 2013; 48 (6): 359–65. [DOI] [PubMed] [Google Scholar]
- (92).Machtinger R, Inbar Y, Cohen-Eylon S, Admon D, Alagem-Mizrachi A, Rabinovici J. MR-guided focus ultrasound (MRgFUS) for symptomatic uterine fibroids: predictors of treatment success. Hum Reprod. 2012; 27 (12): 3425–31. [DOI] [PubMed] [Google Scholar]
- (93).Hesley GK, Felmlee JP, Gebhart JB, Dunagan KT, Gorny KR, Kesler JB, et al. Noninvasive treatment of uterine fibroids: early mayo clinic experience with magnetic resonance imaging-guided focused ultrasound. Mayo Clin Proc. 2006; 81 (7): 936–42. [DOI] [PubMed] [Google Scholar]
- (94).Dobrotwir A, Pun E. Clinical 24 month experience of the first MRgFUS unit for treatment of uterine fibroids in Australia. J Med Imag Radiat Oncol. 2012; 56 (4): 409–16. [DOI] [PubMed] [Google Scholar]
- (95).Desai SB, Patil AA, Nikam R, Desai AS, Bachhav V. Magnetic resonance-guided focused ultrasound treatment for uterine fibroids: first study in Indian women. J Clin Imaging Sci. 2012; 2 (1): 74–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (96).Morita Y, Ito N, Hikida H, Takeuchi S, Nakamura K, Ohashi H. Non-invasive magnetic resonance imaging-guided focused ultrasound treatment for uterine fibroids - early experience. Eur J Obstet Gynecol Reprod Biol. 2008; 139 (2): 199–203. [DOI] [PubMed] [Google Scholar]
- (97).Gorny KR, Woodrum DA, Brown DL, Henrichsen TL, Weaver AL, Amrami KK, et al. Magnetic resonance-guided focused ultrasound of uterine leiomyomas: review of a 12-month outcome of 130 clinical patients. J Vasc Interv Radiol. 2011; 22 (6): 857–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (98).Hovsepian DM, Siskin GP, Bonn J, Cardella JF, Clark TW, Lampmann LE, et al. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. Cardiovasc Intervent Radiol. 2004. Jul; 27 (4):307–13. [DOI] [PubMed] [Google Scholar]
- (99).Fukunishi H, Funaki K, Ikuma K, Kaji Y, Sugimura K, Kitazawa R, et al. Unsuspected uterine leiomyosarcoma: magnetic resonance imaging findings before and after focused ultrasound surgery. Int J of Gynecol Cancer. 2007; 17 (3): 724–8. [DOI] [PubMed] [Google Scholar]
- (100).Kim KA, Yoon S-W, Yoon BS, Park CT, Kim SH, Lee JT. Spontaneous vaginal expulsion of uterine myoma after magnetic resonance-guided focused ultrasound surgery. J Minim Invasive Gynecol. 2011; 18 (1): 131–4. [DOI] [PubMed] [Google Scholar]
- (101).Leon-Villapalos J, Kaniorou-Larai M, Dziewulski P. Full thickness abdominal burn following magnetic resonance guided focused ultrasound therapy. Burns. 2005; 31 (8): 1054–5. [DOI] [PubMed] [Google Scholar]
- (102).US Food and Drug Administration. Quantitative assessment of the prevalence of unsuspected uterine sarcoma in women undergoing treatment of uterine fibroids: summary and key findings [Internet]. [updated 2014; cited 2014 Aug 15]. Available from: http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM393589.pdf [Google Scholar]
- (103).US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA Safety Communication [Internet]. [updated 2014; cited 2014 Jun 30]. Available from: http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM393589.pdf [Google Scholar]
- (104).Goodwin SC, Bonilla SM, Sacks D, Reed RA, Spies JB, Landow WJ, et al. Reporting standards for uterine artery embolization for the treatment of uterine leiomyomata. J Vasc Interv Radiol. 2001. Sep; 12 (9):1011–20. [DOI] [PubMed] [Google Scholar]
- (105).Himabindu Y, Sriharibabu M, Nyapathy V, Mishra A. Early evaluation of magnetic resonance imaging guided focused ultrasound sonication in the treatment of uterine fibroids. Indian J Med Res. 2014. Feb; 139: 267–72. [PMC free article] [PubMed] [Google Scholar]
- (106).Okada A, Morita Y, Fukunishi H, Takeichi K, Murakami T. Non-invasive magnetic resonance-guided focused ultrasound treatment of uterine fibroids in a large Japanese population: impact of the learning curve on patient outcome. Ultrasound Obstet Gynecol. 2009; 34 (5): 579–83. [DOI] [PubMed] [Google Scholar]
- (107).Machtinger R, Fennessy F, Stewart E, Missmer SA, Correia K., Tempany. MR-guided focused ultrasound (MRgFUS) is effective for the distinct pattern of uterine fibroids seen in African-American women: data from phase III/IV, non-randomized, multicenter clinical trials. J Ther Ultrasound. 2013; 1 (1): 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (108).Yao C-L, Trinh T, Wong GTC, Irwin MG. Anaesthesia for high intensity focused ultrasound (HIFU) therapy. Anaesthesia. 2008; 63 (8): 865–72. [DOI] [PubMed] [Google Scholar]
- (109).Hindley J, Gedroyc WM, Regan L, Stewart E, Tempany C, Hynyen K, et al. MRI guidance of focused ultrasound therapy of uterine fibroids: early results. Amer J Roentgenol. 2004; 183 (6): 1713–9. [DOI] [PubMed] [Google Scholar]
- (110).Stewart EA, Rabinovici J, Tempany CMC, Inbar Y, Regan L, Gastout B, et al. Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril. 2006; 85 (1): 22–9. [DOI] [PubMed] [Google Scholar]
- (111).Yoon S-W, Cha SH, Ji YG, Kim HC, Lee MH, Cho JH. Magnetic resonance imaging-guided focused ultrasound surgery for symptomatic uterine fibroids: estimation of treatment efficacy using thermal dose calculations. Eur J Obstet Gynecol Reprod Biol. 2013; 169 (2): 304–8. [DOI] [PubMed] [Google Scholar]
- (112).Ikink ME, Voogt MJ, Verkooijen HM, Lohle PNM, Schweitzer KJ, Franx A, et al. Mid-term clinical efficacy of a volumetric magnetic resonance-guided high-intensity focused ultrasound technique for treatment of symptomatic uterine fibroids. Eur Radiol. 2013; 23 (11): 3054–61. [DOI] [PubMed] [Google Scholar]
- (113).Lenard ZM, McDannold NJ, Fennessy FM, Stewart EA, Jolesz FA, Hynynen K, et al. Uterine leiomyomas: MR imaging-guided focused ultrasound surgery – imaging predictors of success. Radiology. 2008. Oct; 249 (1):187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (114).Kim HS, Baik J-H, Pham LD, Jacobs MA. MR-guided high-intensity focused ultrasound treatment for symptomatic uterine leiomyomata. long-term outcomes. Acad Radiol. 2011; 18 (8): 970–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (115).Gorny KR, Borah BJ, Brown DL, Woodrum DA, Stewart EA, Hesley GK. Incidence of additional treatments in women treated with MR-guided focused US for symptomatic uterine fibroids: review of 138 patients with an average follow-up of 2.8 years. J Vasc Interv Radiol. 2014. Jul 2; 25 (10):1506–12. [DOI] [PubMed] [Google Scholar]
- (116).Rabinovici J, David M, Fukunishi H, Morita Y, Gostout BS, Stewart EA. Pregnancy outcome after magnetic resonance-guided focused ultrasound surgery (MRgFUS) for conservative treatment of uterine fibroids. Fertil Steril. 2010; 93 (1): 199–209. [DOI] [PubMed] [Google Scholar]
- (117).Bouwsma EVA, Hesley GK, Woodrum DA, Weaver AL, Leppert PC, Peterson LG, et al. Comparing focused ultrasound and uterine artery embolization for uterine fibroids - rationale and design of the Fibroid Interventions: Reducing Symptoms Today and Tomorrow (FIRSTT) trial. Fertil Steril. 2011; 96 (3): 704–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (118).Bouwsma EVA, Gorny KR, Hesley GK, Jensen JR, Peterson LG, Stewart EA. Magnetic resonance-guided focused ultrasound surgery for leiomyoma-associated infertility. Fertil Steril. 2011; 96 (1): e9–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (119).Gavrilova-Jordan LP, Rose CH, Traynor KD, Brost BC, Gostout BS. Successful term pregnancy following MR-guided focused ultrasound treatment of uterine leiomyoma. J Perinatol. 2007; 27 (1): 59–61. [DOI] [PubMed] [Google Scholar]
- (120).Hanstede MMF, Tempany CMC, Stewart EA. Focused ultrasound surgery of intramural leiomyomas may facilitate fertility: a case report. Fertil Steril. 2007; 88 (2): 497. [DOI] [PubMed] [Google Scholar]
- (121).Zaher S, Lyons D, Regan L. Uncomplicated term vaginal delivery following magnetic resonance-guided focused ultrasound surgery for uterine fibroids. Biomed Imaging and Interv J. 2010; 6 (2):e28-June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (122).Zaher S, Lyons D, Regan L. Successful in vitro fertilization pregnancy following magnetic resonance-guided focused ultrasound surgery for uterine fibroids. J Obstet Gynaecol Res. 2011; 37 (4): 370–3. [DOI] [PubMed] [Google Scholar]
- (123).Morita Y, Ito N, Ohashi H. Pregnancy following MR-guided focused ultrasound surgery for a uterine fibroid. Int J Gynaecol Obstet. 2007; 99 (1): 56–7. [DOI] [PubMed] [Google Scholar]
- (124).Yoon S-W, Kim KA, Kim SH, Ha DH, Lee C, Lee SY, et al. Pregnancy and natural delivery following magnetic resonance imaging-guided focused ultrasound surgery of uterine myomas. Yonsei Med J. 2010; 51 (3): 451–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (125).Rabinovici J, Inbar Y, Eylon SC, Schiff E, Hananel A, Freundlich D. Pregnancy and live birth after focused ultrasound surgery for symptomatic focal adenomyosis: a case report. Hum Reprod. 2006; 21 (5): 1255–9. [DOI] [PubMed] [Google Scholar]
- (126).Froeling V, Meckelburg K, Schreiter NF, Scheurig-Muenkler C, Kamp J, Maurer MH, et al. Outcome of uterine artery embolization versus MR-guided high-intensity focused ultrasound treatment for uterine fibroids:long-term results. Eur J Radiol. 2013; 82 (12): 2265–9. [DOI] [PubMed] [Google Scholar]
- (127).Moss JG, Cooper KG, Khaund A, Murray LS, Murray GD, Wu O, et al. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011. Jul; 118 (8):936–44. [DOI] [PubMed] [Google Scholar]
- (128).Pinto I, Chimeno P, Romo A, Paul L, Haya J, de la Cal MA, et al. Uterine fibroids: uterine artery embolization versus abdominal hysterectomy for treatment– a prospective, randomized, and controlled clinical trial. Radiology. 2003. Feb; 226 (2):425–31. [DOI] [PubMed] [Google Scholar]
- (129).Volkers NA, Hehenkamp WJ, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids: 2 years' outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2007. Jun; 196 (6):519–11. [DOI] [PubMed] [Google Scholar]
- (130).Volkers NA, Hehenkamp WJ, Birnie E, de VC, Holt C, Ankum WM, et al. Uterine artery embolization in the treatment of symptomatic uterine fibroid tumors (EMMY trial): periprocedural results and complications. J Vasc Interv Radiol. 2006. Mar; 17 (3):471–80. [DOI] [PubMed] [Google Scholar]
- (131).Ananthakrishnan G, Murray L, Ritchie M, Murray G, Bryden F, Lassman S, et al. Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): subanalysis of 5-year MRI findings. Cardiovasc Intervent Radiol. 2013. Jun; 36 (3):676–81. [DOI] [PubMed] [Google Scholar]
- (132).Edwards RD, Moss JG, Lumsden MA, Wu O, Murray LS, Twaddle S, et al. Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med. 2007. Jan 25; 356 (4):360–70. [DOI] [PubMed] [Google Scholar]
- (133).Taran FA, Tempany CMC, Regan L, Inbar Y, Revel A, Stewart EA. Magnetic resonance-guided focused ultrasound (MRgFUS) compared with abdominal hysterectomy for treatment of uterine leiomyomas. Ultrasound Obstet Gynecol. 2009; 34 (5): 572–8. [DOI] [PubMed] [Google Scholar]
- (134).Manyonda IT, Bratby M, Horst JS, Banu N, Gorti M, Belli A-M. Uterine artery embolization versus myomectomy: impact on quality of life - results of the FUME (Fibroids of the uterus: Myomectomy versus embolization) trial. Cardiovasc Intervent Radiol. 2012; 35 (3): 530–6. [DOI] [PubMed] [Google Scholar]
- (135).Mara M, Maskova J, Fucikova Z, Kuzel D, Belsan T, Sosna O. Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Cardiovasc Intervent Radiol. 2008; 31 (1): 73–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (136).Goodwin SC, Bradley LD, Lipman JC, Stewart EA, Nosher JL, Sterling KM, et al. Uterine artery embolization versus myomectomy: a multicenter comparative study. Fertil Steril. 2006. Jan; 85 (1):14–21. [DOI] [PubMed] [Google Scholar]
- (137).Froeling V, Meckelburg K, Scheurig-Muenkler C, Schreiter NF, Kamp J, Maurer MH, et al. Midterm results after uterine artery embolization versus MR-guided high-intensity focused ultrasound treatment for symptomatic uterine fibroids. Cardiovasc Interv Radiol. 2013; 36 (6): 1508–13. [DOI] [PubMed] [Google Scholar]
- (138).de Melo FCM, Diacoyannis L, Moll A, Tovar-Moll F. Reduction by 98% in uterine myoma volume associated with significant symptom relief after peripheral treatment with magnetic resonance imaging-guided focused ultrasound surgery. J Min Invasive Gynecol. 2009; 16 (4): 501–3. [DOI] [PubMed] [Google Scholar]
- (139).Nyapathy V, Polina L. MRgFUS treatment of uterine fibroid in a nulliparous woman with acute retention of urine. J Radiol Case Rep. 2012; 6 (2): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (140).Rabinovici J, David M, Fukunishi H, Morita Y, Gostout BS, Stewart EA. Pregnancy outcome after magnetic resonance-guided focused ultrasound surgery for conservative treatment of uterine fibroids. Obstet Gynecol Surv. 2010; 65 (5): 316–8. [DOI] [PubMed] [Google Scholar]
- (141).Kim Y-S, Keserci B, Partanen A, Rhim H, Lim HK, Park MJ, et al. Volumetric MR-HIFU ablation of uterine fibroids: role of treatment cell size in the improvement of energy efficiency. Eur J Radiol. 2012; 81 (11): 3652–9. [DOI] [PubMed] [Google Scholar]
- (142).Kim Y-S, Kim J-H, Rhim H, Lim HK, Keserci B, Bae D-S, et al. Volumetric MR-guided high-intensity focused ultrasound ablation with a one-layer strategy to treat large uterine fibroids: initial clinical outcomes. Radiology. 2012; 263 (2): 600–9. [DOI] [PubMed] [Google Scholar]
- (143).Kim Y-S, Trillaud H, Rhim H, Lim HK, Mali W, Voogt M, et al. MR thermometry analysis of sonication accuracy and safety margin of volumetric MR imaging-guided high-intensity focused ultrasound ablation of symptomatic uterine fibroids. Radiology. 2012; 265 (2): 627–37. [DOI] [PubMed] [Google Scholar]
- (144).Park H, Yoon S-W, Kim K-A, Jung KD, Jung S-G. Magnetic resonance imaging-guided focused ultrasound treatment of pedunculated subserosal uterine fibroids: a preliminary report. J Vasc Interv Radiol. 2012; 23 (12): 1589–93. [DOI] [PubMed] [Google Scholar]
- (145).Yoon SW, Kim KA, Kim SH, Lee JT. Successful magnetic resonance imaging-guided focused ultrasound surgery for recurrent uterine fibroid previously treated with uterine artery embolization. Obstet Gynecol Int. 2010; 2010, (2010):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (146).Voogt MJ, Van SM, Ikink ME, Deckers R, Vincken KL, Bartels LW, et al. Targeted vessel ablation for more efficient magnetic resonance-guided high-intensity focused ultrasound ablation of uterine fibroids. Cardiovasc Intervent Radiol. 2012; 35 (5): 1205–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (147).Dorenberg EJ, Courivaud F, Ring E, Hald K, Jakobsen JA, Fosse E, et al. Volumetric ablation of uterine fibroids using Sonalleve high-intensity focused ultrasound in a 3 Tesla scanner-first clinical assessment. Minim Invasive Ther Allied Technol. 2013; 22 (2): 73–9. [DOI] [PubMed] [Google Scholar]