Abstract
Background
Transient ischemic attack (TIA) is a brief episode of dysfunction in a confined area of the brain. The risk of stroke following TIA is approximately 4% within the first 2 days and 9% within the first month. Therefore, early diagnosis and treatment is critical to reduce mortality and risk of stroke in patients who have experienced a TIA.
Objectives
This systematic review aimed to investigate the impact of the urgent evaluation and initiation of treatment of patients with TIA on the risk of subsequent stroke and death.
Data Sources
A literature search was performed for studies published from January 1, 2007, until December 21, 2012. The search was updated monthly to April 1, 2013.
Results
All identified studies showed that urgent assessment and initiation of treatment of TIA is an effective strategy in reducing the incidence of stroke. Among these, a large observational study found a large effect in that the risk of stroke was reduced by 80%, and a Canadian study found that providing urgent care significantly reduced the rate of stroke in high-risk patients. Another Canadian study reported a significant reduction in the rate of death among patients referred to stroke prevention clinics, compared to patients not referred to such services. One study showed that patients discharged from an emergency department with standard care had significantly higher rates of stroke and subsequent TIA in the first month, compared to those who were hospitalized. However, another study showed that for patients at low to moderate risk, rate of stroke was similar between inpatients and those managed in a TIA clinic.
Limitations
Our analysis was restricted to the effect of the combined interventions. The magnitude of benefit of each individual component of the intervention cannot be determined through this review.
Conclusions
The results of this systematic review have important clinical and health system implications. Urgent management of TIA patients in specialized TIA clinics rather than regular practice results in a lower rate of stroke and disability.
Plain Language Summary
Transient ischemic attack (TIA) is a temporary dysfunction in the brain that occurs when the blood supply to one part of the brain is briefly interrupted. Patients may experience sudden weakness or numbness in their arms or legs on one side of the body, confusion, difficulty talking, vision troubles, dizziness, or loss of balance. Although symptoms may disappear, TIA is known to be a signal that the patient is at risk for a full-blown stroke. TIA precedes approximately 23% of strokes, which often occur within 48 hours of the TIA. Therefore, early diagnosis and treatment of TIA is considered to be critical to reduce mortality and risk of stroke.
This study analyzed what is known from published research about the importance of quickly treating patients who have had a TIA to prevent a full-blown stroke. Specifically, we investigated whether the risk of stroke and death following TIA is lower for patients who are rapidly evaluated and treated, compared to patients who receive standard care. Our review found multiple studies showing that patients assessed and treated in a TIA clinic with rapid access to specialist services had significantly lower risk of subsequent stroke. We concluded that most patients can be managed through outpatient clinics or specialized observation units in emergency departments. However, some will need treatment requiring hospitalization.
Our review of the research in this area also looked at the use of a tool called ABCD2 that helps to identify patients at high risk of stroke, based on their symptoms and medical history. While this tool can be helpful, some studies showed that other investigations, such as diagnostic imaging of the brain and blood vessels, can add critical information about a patient's risk of stroke after a TIA.
Background
Objective of Analysis
This analysis aimed to investigate the impact of rapid evaluation and initiation of treatment of patients with transient ischemic attack (TIA) on the risk of subsequent stroke and death.
Clinical Need and Target Population
Description of Disease/Condition
TIA and stroke are events associated with the sudden onset of neurological dysfunction, caused by reduction in blood flow in confined areas of the brain. TIA is characterized by the transient nature of symptoms, which resolve within minutes or hours, but it is strongly associated with the risk of subsequent stroke. Therefore, early diagnosis and treatment of TIAs is considered to be critical to reduce disability and mortality from stroke.
TIAs often precede a stroke within hours or days. Johnston et al (1) determined the following risks of stroke after TIA:
3.9% within the first 2 days
5.5% within 7 days
7.5% within 30 days
9.2% within 90 days
Of approximately 300,000 patients presenting to clinics and emergency departments with TIA symptoms, 21% were classified as high risk for subsequent stroke, 45% as moderate risk, and 34% as low risk. (1)
Prevalence and Incidence of TIA and Stroke
TIAs are believed to often go undiagnosed and are likely underreported. (2) The 2008/2009 Ontario Stroke Audit showed that among patients who were hospitalized or had an emergency department visit for acute stroke or TIA, 61% had a final diagnosis of stroke and 30% had a final diagnosis of TIA. In 9% of these patients the diagnosis was uncertain. (3) Of 8,548 first-ever stroke events in 2007/2008 in British Columbia, about 30% were classified as TIA, 60% were acute ischemic stroke, and 10% were hemorrhagic events. (4) The incidence of all types of stroke for hospitalized patients in Canada in 1999/2000 was 14.4 per 10,000 population in Canada, and the mean length of stay was 21 days (95% confidence interval [CI], 20.0–21.4). (5)
Changes in the Definition of Transient Ischemic Attack
Conventionally, TIA and stroke have been differentiated by the duration of symptoms, with TIA defined as symptoms resolving within 24 hours. However, concerns arose that this definition might result in delayed treatment and higher risk to patients, if practitioners waited to see whether symptoms would spontaneously resolve.
In 2009, the American Heart Association and the American Stroke Association adopted a new tissue-based definition to distinguish TIA and stroke. (6) It defines TIA as a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retina ischemia, without evidence of acute infarction. Implementing this definition requires resources such as diffusion-weighted magnetic resonance imaging (DWI) to diagnose the presence or absence of an acute infarct.
Defining TIA in a way that will correctly identify patients at high risk of stroke continues to be challenging. The new definition may be difficult to implement in rural areas, where diagnostic imaging may not be available. Some investigators have suggested that the earlier, time-based definition be revised, with the cut-off for TIA reduced to 1 hour and stroke defined as symptoms lasting for 24 hours. (6)
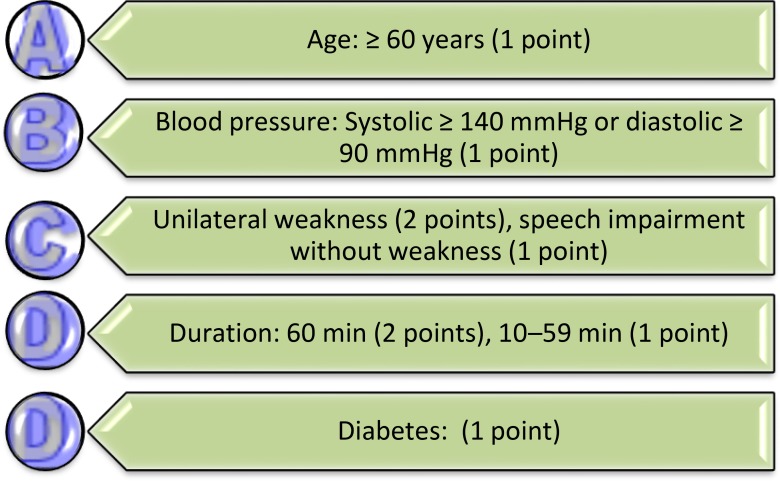
Risk Prediction Score
Clinical risk prediction scores can help to classify patients for urgent diagnosis and possible treatment. The ABCD2 scale scores patients with TIA according to age, blood pressure, clinical features, duration of symptoms, and diabetes status. Higher scores indicate higher risk of stroke in the next 2 to 90 days (Figure 1). (1)
Figure 1: ABCD2 Scale for Risk of Stroke Following Transient Ischemic Attack.
Source: Johnson et al, 2007. (1)
More recently, imaging data have been added (ABCD2-I), and the most recent version includes both brain and vascular imaging (ABCD3-I). The combination of neuroimaging and vascular information has resulted in an improvement in the prognostic accuracy of the risk algorithm for patients with TIA. (7)
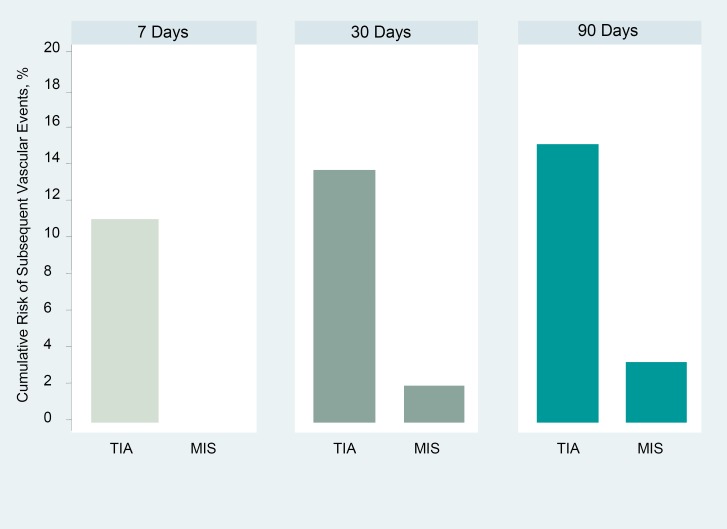
Differences between Transient Ischemic Attack and Minor Ischemic Stroke
In some epidemiological studies, TIA is often combined with minor ischemic stroke (MIS), a longer-lasting condition in which the symptoms persist. This has created some confusion. Although the 2 conditions share common risk factors and symptoms, and both indicate high risk of subsequent full-blown stroke, studies have shown that the early risk of subsequent stroke is significantly higher after a TIA than that after MIS. A prospective observational study by Lin et al (8) compared patients with TIA and with MIS (and scores of 3 or less on the National Institute of Health stroke scale) who presented to hospital within 48 hours after the onset of symptoms. The risk of a major vascular event (MVE) was significantly higher after TIA than after MIS (hazard ratio [HR], 4.6; 95% CI, 2.3–9.3), and the difference was essentially due to the first 7 days after the initial event. Even at 3 months, risk was 5 times higher following TIA than after MIS (Figure 2).
Figure 2: Cumulative Risk of Subsequent Vascular Events: Transient Ischemic Attach Versus Minor Ischemic Stroke.
Abbreviations: MIS, minor ischemic stroke; TIA, transient ischemic stroke.
Source: Lin et al, 2007 (8)
The investigators also showed that differences in the etiology of TIA and MIS had a significant impact on the risk of subsequent vascular events. MIS patients had a higher rate of small-vessel occlusion, while TIA patients had more large-artery atherosclerosis which was associated with much higher probability of vascular events compared to other underlying factors.
The risk difference between TIA and MIS appears to shift over time. At 3 years of follow-up, TIA patients have been found to have lower risk of MVE than MIS patients (odds ratio [OR], 0.75; 95% CI, 0.43–1.32). However, TIA patients had higher MVE fatality compared to MIS patients (OR, 1.43; 95% CI, 0.53–3.90). (9)
Evidence-Based Analysis
Research Questions
Do rapid diagnosis and initiation of therapy reduce the risk of death and major vascular events in patients with transient ischemic attack (TIA)?
Does inpatient admission result in a significantly better outcomes as compared with rapid outpatient care?
Research Methods
Literature Search
Search Strategy
A literature search was performed on December 21, 2012, using OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), the Wiley Cochrane Library, and the Centre for Reviews and Dissemination database, for studies published from January 1, 2007, until December 21, 2012. Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search. The search was updated on a monthly basis through AutoAlert function of the search up to April 1, 2013.
Inclusion Criteria
English language full-reports
studies published between January 1, 2007, and April 1, 2013
studies that included adult patients presenting with symptoms of TIA
studies comparing outcomes of patients with TIA who were managed urgently in specialized outpatient services with those who were managed in routine clinical practice
studies comparing outcomes of patients with TIA who were managed urgently in specialized outpatient centres with those who were hospitalized
single-arm studies reporting on outcomes achieved through rapid assessment of patients in TIA clinics or other specialized services for patients with TIA
Exclusion Criteria
studies that did not report patient outcomes
studies comparing outcomes within in-hospital units
studies on the effect of clinics opening hours (weekend plus weekdays versus weekdays)
studies comparing risk of stroke by sex and race
studies using local audit data
studies on adherence to treatment or adherence to evidence-based guidelines
Outcomes of Interest
Primary outcomes
risk of stroke and death at the following time points: 48 hours, 1 week, 4 weeks, 3 months, 1 year
Secondary outcomes
hospital costs and length of stay
-
measures of process of care
-
–
percentage of tests completed and time to completion:
neuroimaging (computed tomography [CT], magnetic resonance imaging [MRI])
vascular imaging
echocardiography
electrocardiography (ECG)
-
–
time to carotid intervention
-
–
percentage of treatment completed and time to administration/prescription of medications:
antiplatelet
anticoagulant
antihypertensive
lipid-lowering
-
–
Statistical Analysis
A descriptive analysis was carried out and comparative graphs were created to demonstrate the risk of stroke and death in TIA patients who were treated urgently in specialized TIA clinics and those who received care in regular clinical practice. For single-arm studies, the observed risk was compared to the risk predicted by ABCD2 score.
Within stratified data, the associations between categories of ABCD2 scores and risk of stroke were examined. Where brain and vascular imaging data were available, these associations were re-examined to determine the effect of adding the additional data to the risk score.
Quality of Evidence
The quality of the body of evidence for each outcome was examined according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group criteria. (10) The overall quality was determined to be high, moderate, low, or very low using a step-wise, structural methodology.
Study design was the first consideration; the starting assumption was that randomized controlled trials (RCTs) are high quality, whereas observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias—were then taken into account. Limitations in these areas resulted in downgrading the quality of evidence. Finally, 3 main factors that may raise the quality of evidence were considered: large magnitude of effect, dose-response gradient, and accounting for all residual confounding factors. (10) For more detailed information, please refer to the latest series of GRADE articles. (10)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | High confidence in the effect estimate—the true effect lies close to the estimate of the effect |
| Moderate | Moderate confidence in the effect estimate—the true effect is likely to be close to the estimate of the effect, but may be substantially different |
| Low | Low confidence in the effect estimate—the true effect may be substantially different from the estimate of the effect |
| Very Low | Very low confidence in the effect estimate—the true effect is likely to be substantially different from the estimate of effect |
Results of Evidence-Based Analysis
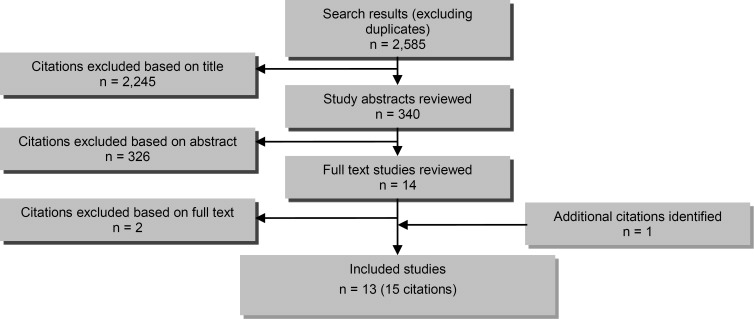
The database search yielded 2,585 citations published between January 1, 2007, and December 21, 2012 (with duplicates removed). Articles were excluded based on information in the title and abstract. The full texts of potentially relevant articles were obtained for further assessment. Figure 3 shows the breakdown of when and for what reason citations were excluded in the analysis.
Figure 3: Citation Flow Chart.
Twelve studies (14 citations) met the inclusion criteria. The references lists of the included studies were hand-searched to identify any additional potentially relevant studies. One study was identified through the AutoAlert monthly updates of the search, which continued up to April 1, 2013, and this study was included in the review.
For each included study, the study design was identified and is summarized in Table 1, a modified version of a hierarchy of study design by Goodman. (11)
Table 1:
Body of Evidence Examined According to Study Design
| Study Design | Number of Eligible Studies | |
|---|---|---|
| RCT Studies | ||
| Systematic review of RCTs | ||
| Large RCT | ||
| Small RCT | 1 | |
| Observational Studies | ||
| Systematic review of non-RCTs with contemporaneous controls | ||
| Non-RCT with non-contemporaneous controls | 2 (3 citations) | |
| Systematic review of non-RCTs with historical controls | ||
| Non-RCT with historical controls | 1 | |
| Database, registry, or cross-sectional study | 2 | |
| Case series | 7 (8 citations) | |
| Retrospective review, modelling | ||
| Studies presented at an international conference | ||
| Expert opinion | ||
| Total | 13 (15 citations) | |
Abbreviation: RCT, randomized controlled trial.
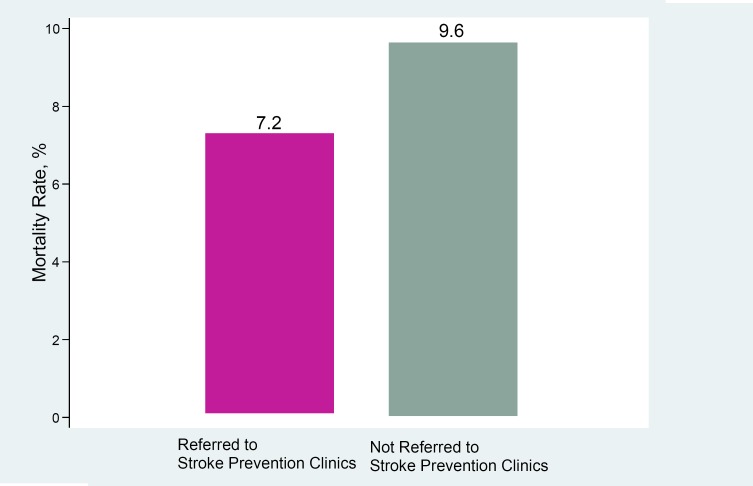
Urgent Care Provided in Specialized Clinics
A Canadian study (12) investigated risk of death following TIA or ischemic stroke, using data from the Canadian Stroke Network registry, which contained detailed information on all patients seen in the ED or admitted to a hospital in Ontario. The study compared 1-year, all-cause mortality in patients referred to stroke prevention clinics (SPCs) with those not referred to such services between 2003 and 2008. The study sample included 16,468 patients; however, due to significant differences in baseline characteristics of the 2 groups, a propensity-score matching of the baseline variables was performed, resulting in 5,531 matched pairs with a mean age of 70.2 years (standard deviation [SD], 13.7) for patients referred to an SPC and, for the not-referred group, 72.6 years (SD, 14.2).
Crude 1-year mortality was significantly lower in patients referred to SPCs compared with those not referred (7.2% vs. 9.6%; hazard ratio [HR], 0.74; 95% confidence interval [CI], 0.65–0.84; P < 0.0001) (Figure 4). When TIA and ischemic stroke patients were analyzed separately, 1-year mortality was also lower in those referred to SPCs than in those not referred (for ischemic stroke: 8.0% for referred to SPCs vs. 10.6% for not referred; HR, 0.74; 95% CI, 0.64–0.86; P < 0.001; for TIA: 4.8% vs. 6.7%; HR, 0.71; 95% CI, 0.54–0.93; P = 0.014).
Figure 4: One-Year Mortality After Transient Ischemic Attack or Ischemic Stroke: Patients Referred Versus not Referred to Stroke Prevention Clinics.
Source: Webster et al, 2011. (12)
Six-month follow-up showed that patients referred to SPCs received significantly more diagnostic evaluations and treatments, except for computed tomography [CT] neuroimaging, warfarin for atrial fibrillation, and antihypertensive medications (Table 2).
Table 2:
Measures of Process of Care Within 6 Months After Transient Ischemic Attack
| Referred to Stroke Prevention Clinic | Not Referred to Stroke Prevention Clinic | P Value | |
|---|---|---|---|
| Diagnostic Evaluations Performed, % of Patients | |||
| Carotid imaging | 42.1 | 34.5 | < 0.001 |
| Echocardiography | 34.3 | 26.4 | < 0.001 |
| CT scan | 25.0 | 24.8 | 0.82 |
| MRI scan | 15.2 | 10.4 | < 0.001 |
| Holter monitoring | 22.2 | 12.1 | < 0.001 |
| Treatments Provided, % of Patientsa | |||
| BP-lowering agents | 84.3 | 82.8 | 0.074 |
| Warfarin | 78.9 | 79.2 | 0.89 |
| Lipid-lowering agents | 73.1 | 67.6 | < 0.001 |
| Antiplatelet agents | 49.2 | 45.2 | < 0.001 |
| Carotid procedures | 29.0 | 37.0 | 0.02 |
Abbreviations: BP, blood pressure; CT, computed tomography; MRI, magnetic resonance imaging.
For medications, outcomes were reported only for patients over age 65 years.
Source: Webster et al, 2011. (12)
Eight studies reported on the rate of stroke at 90 days following TIA. Table 3 shows study design and patient characteristics of these studies. Two were comparative and 6 were single-arm studies in which the observed risk of stroke was compared with the predicted risk based on ABCD2 scores. Two of these studies had 1 year of follow-up. (13;14)
Table 3:
Characteristics of Studies Comparing Urgent Care for Transient Ischemic Attack and Conventional Care or Predicted Rate
| Author, Year | Country | Study Design | Number of Patients | Age, Years | Follow-Up, Months |
|---|---|---|---|---|---|
| Rothwell et al, 2007 (15) | United Kingdom | Prospective cohort (Comparative) | 591 Phase 1: 310 Phase 2: 281 |
In both phases, 67% of patients were < 80 years old | 3 |
| Wu et al, 2009 (16) | Canada (Alberta) | Retrospective cohort (Comparative) | 581 Rapid evaluation: 189 Standard care: 392 |
Rapid evaluation unit: Mean, 67.5 (range, 14–93) Standard care: Mean, 71 (range, 19–98) |
3 |
| Wasserman et al, 2010 (17) | Canada (Ontario) | Prospective cohort (Single arm) | 982 | Mean, 67 (range, 19–97) | 3 |
| Olivot et al, 2011 (18) | United States | Prospective cohort (Single-arm study of ED-based TIA triage system) | 224 TIA clinic: 157 Hospitalized: 67 |
TIA clinic: Mean, 67 (SD, 16) Hospitalized: Mean, 71 (SD, 15) |
3 |
| Lavellee et al, 2007 (13) | France | Prospective cohort (Single arm) | 1,085 | TIA with no new lesion: Median, 66.1 (IQR, 51.5–80.7) TIA with new lesion: Median, 65.8 (IQR, 51.2–80.4) Possible TIA: Median, 57.3 (IQR, 41.4–73.2) MIS: Median, 68.3 (IQR, 53.6–83) Other: Median, 53 (IQR, 35.8–70.2) |
12 |
| von Weitzel-Mudersbach et al, 2011 (14) | Denmark | Prospective cohort (Single arm) | 306 | Median, 65.8 (range, 19–93) | 12 |
| Torres Macho et al, 2011 (19) | Spain | Prospective cohort (Single arm) | 97 | Mean, 72.5 (SD, 9.1) | 3 |
| Horer et al. 2011 (20) | Germany | Prospective cohort (Single arm) | 123 | Mean, 59 (SD, 17.2) | 3 |
Abbreviations: ED, emergency department; IQR, interquartile range; MIS, minor ischemic stroke; SD, standard deviation; TIA, transient ischemia attack.
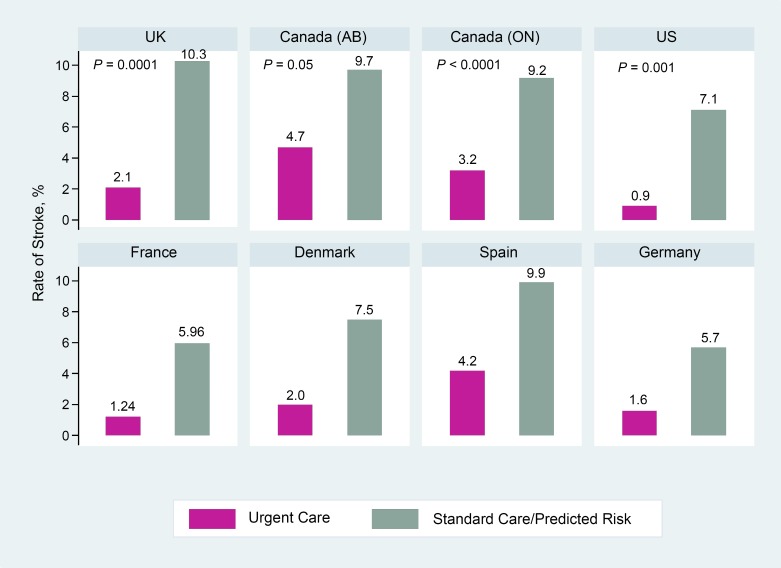
The results of all studies showed that patients managed in outpatient TIA clinics had lower rates of stroke at 90 days compared to those managed in regular clinical practices or compared to patients’ predicted risk scores (Figure 5).
Figure 5: Rate of Stroke in 90 Days Following Transient Ischemic Attack: TIA Clinic Versus Regular Clinical Practice or Predicted Risk.
Abbreviations: AB, Alberta; ON, Ontario; UK, United Kingdom; US, United States.
P values are shown where reported.
UK and Canada: Urgent care versus regular clinical practice.
USA, France, Denmark, Spain, Germany: Urgent care versus predicted risk score.
Sources: Rothwell et al, 2007 (15); Wu et al, 2009 (16); Wasserman et al, 2010 (17); Olivot et al, 2011 (18); Lavellee et al, 2007 (13); von Weitzel-Mudersbach et al, 2011 (14); Torres Macho et al, 2011 (19); Horer et al. 2011 (20).
The EXPRESS Study
The EXPRESS study (15), conducted in the UK, was an observational study and consisted of 2 phases distinguished by speed of initiation of therapy (Table 4). In both phases, the collaborating primary care physicians referred patients with suspected TIA or minor ischemic stroke to a daily TIA clinic. In phase 1 (n = 310), following referral the clinic contacted the patients to arrange an appointment as soon as possible. However, there were inherent delays in receiving referrals and contacting patients. Patients were seen at the clinic on weekdays only or were seen at home if the patient was too frail to come to the clinic. Brain imaging and ECG were usually performed the same day as the appointment or shortly after. If carotid ultrasound and echocardiography were necessary, they were performed during the following week. The clinic did not initiate any treatment; instead, a report consisting of the initial assessment and specific treatment recommendations was faxed to the primary care provider, usually within 24 hours of the evaluation, and patients were instructed to contact their primary care provider as soon as possible for follow-up. In phase 2 (n = 281), patients were referred by their primary care provider to the TIA clinic, but no appointment was necessary and treatment was initiated by the TIA clinic immediately following investigation.
Table 4:
Characteristics of the 2 Study Periods in the EXPRESS Study
| Time-Related Variables | Phase 1 | Phase 2 | P Value |
|---|---|---|---|
| Percentage of patients seen in TIA clinic ≤ 6 hours | 1.7 | 29 | < 0.001 |
| Percentage of patients seen in TIA clinic ≤ 24 hours | 23.4 | 59.1 | < 0.001 |
| Median (IQR) time from seeking medical attention to assessment in clinic, days | 3 (2–5) | < 1 (0–3) | < 0.001 |
| Median (IQR) time from seeking medical attention to first prescription of 1 of the treatments recommended in fax to primary care provider, days | 20 (8–53) | 1 (0–3) | < 0.001 |
Abbreviations: IQR; interquartile range; TIA, transient ischemic attack.
Source: Rothwell et al, 2007. (15)
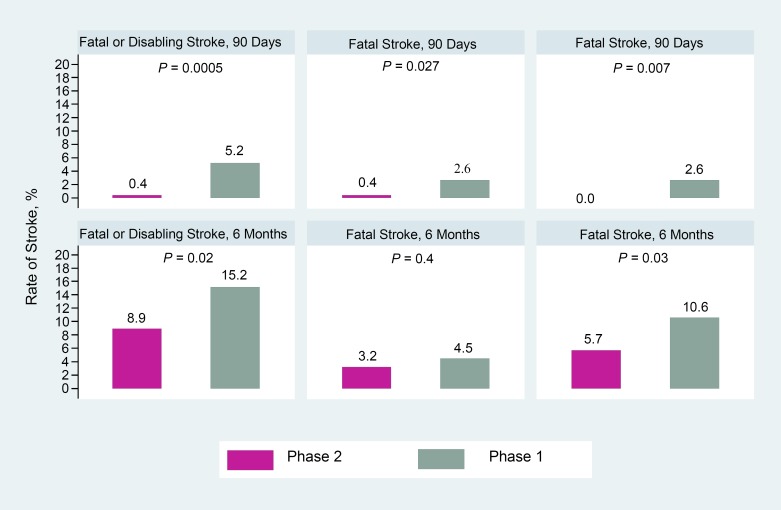
At 90 days of follow-up, patients in phase 2 had a significantly lower rate of any stroke compared to patients in phase 1 (2.1% vs. 10.3%; adjusted HR, 0.2; 95% CI, 0.08–0.49; P = 0.0001). In addition, the overall rate of fatal or disabling strokes was significantly lower in phase 2 than in phase 1. In each phase, one-quarter to one-fifth of all recurrent strokes were fatal. In phase 2, no subsequent strokes were disabling compared to one-quarter of strokes in phase 1 (Figure 6).
Figure 6: Rate of Stroke at 6 Months and 90 Days Following Transient Ischemic Attack in the EXPRESS Study.
Source: Luengo-Fernandez et al, 2009. (21)
A separate publication reported the 6-month stroke outcomes, as well as rates and costs of hospitalization. (21) At 6 months, rates of fatal or disabling stroke were still significantly lower in phase 2 than in phase 1 (8.9% vs. 15.2%; OR, 0.51; 85% CI, 0.3–0.85; P = 0.022). Rate of disabling stroke was 10.6% in phase 1 and 5.7% in phase 2 (unadjusted OR, 0.46; 95% CI, 0.25–0.86; P = 0.031). The rate of fatal stroke, however, did not differ at 6 months of follow-up (Figure 6).
The proportion of patients who had undergone carotid procedure by 1 month did not differ significantly in phase 1 (5.6%) and phase 2 (5.4%). However, this procedure was performed more quickly in phase 2 than in phase 1 (40% during the first week versus 0%, respectively; P = 0.006). Similarly, 67% of carotid procedures were performed during the first month in phase 2, compared to only 12% in phase 1 (P = 0.001), and significantly more patients in phase 2 than in phase 1 were on aspirin, lipid-lowering, and antihypertensive medications at 1-month follow-up (Table 5).
Table 5:
Percentage of Patients on Preventive Treatment at 1 Month Following Transient Ischemic Attack, the EXPRESS Study
| Medication | Phase 1, % of Patients | Phase 2, % of Patients | P Value |
|---|---|---|---|
| Antiplatelet/anticoagulant | 97 | 97 | 1.0 |
| Aspirin and 30 days of clopidogrel | 10 | 49 | < 0.0001 |
| Statin | 65 | 84 | < 0.001 |
| 1 or more blood pressure lowering drug | 62 | 83 | < 0.001 |
| 2 or more blood pressure lowering drugs | 34 | 60 | < 0.001 |
Source: Rothwell et al, 2007. (15)
All-cause hospitalization was similar in both phases, but admission rates due to recurrent stroke were significantly lower in phase 2 than in phase 1. Patients in phase 2 also had significantly fewer total days in hospital due to any vascular cause or to recurrent stroke, compared to phase 1; however, total days in hospital due to other vascular causes were not different between the 2 phases. The mean length of stay was 18 days shorter for all admitted patients in phase 2 and 17 days shorter for admissions due to recurrent stroke (Table 6). At 90 days, total and mean costs were lower in phase 2 than in phase 1, mainly due to reductions in costs due to recurrent stroke. The mean cost per patient was £624 less in phase 2 than in phase 1 (Table 7).
Table 6:
Hospitalization Within 90 Days Following Transient Ischemic Attack, the EXPRESS Study
| Event | Phase 1 | Phase 2 | Effect |
|---|---|---|---|
| All cause admission to hospital | 18% | 18% | P = 0.85 |
| Admission due to recurrent stroke | 8% | 2% | OR, 0.21 (0.88–0.55); P = 0.001 |
| Total days in hospital due to any vascular causes, n | 1,365 | 427 | Mean reduction of 3 (– 6 to – 1) days per patient (P = 0.02) |
| Total days in hospital due to recurrent stroke, n | 1,147 | 90 | P = 0.005 |
| Total days in hospital due to other vascular causes, n | 218 | 337 | P = 0.31 |
| Length of stay for admitted patients, mean days (SD) | 29 (52) | 11 (11) | Reduction of 18 days (– 36 to – 4); P = 0.02 |
| Length of stay for those who had recurrent stroke, mean days(SD) | 32 (60) | 15 (29) | Reduction of 17 days (– 46 to 20); P = 0.37 |
Abbreviations: OR, odds ratio; SD, standard deviation.
Source: Luengo-Fernandez et al, 2009. (21)
Table 7:
90-Day Costs Following Transient Ischemic Attack, the EXPRESS Study
| Cost, £ | Phase 1 | Phase 2 | Effect |
|---|---|---|---|
| Total cost | 327,474 | 121,506 | Saving of £205,968 |
| Mean cost (SD) for recurrent stroke | 866 (4,788) | 76 (998) | P = 0.003 |
| Mean cost (SD) | 1,056 (4,879) | 432 (2,277) | Saving of £624 (95% CI, 1,370–104) per patient referred to the TIA clinic (P = 0.03) |
Abbreviations: SD, standard deviation.
Source: Luengo-Fernandez et al, 2009. (21)
Alberta Study
A study in Alberta compared high-risk TIA patients receiving urgent care in a rapid evaluation unit (n = 189) with high-risk TIA patients receiving standard care in emergency departments (ED) (n = 392). (16) The Calgary Stroke Program had initiated the rapid evaluation unit for TIA patients who presented in less than 24 hours and who were at high risk of stroke.
The 90-day risk of stroke among patients in the rapid evaluation unit was 4.7% compared with 9.7% in the standard care cohort. One-year median cost was significantly higher for the rapid evaluation cohort than for standard ED care ($8,360 vs. $4,820, respectively; P < 0.001).
Significantly more patients in the rapid evaluation unit underwent carotid procedures within 90 days than in the standard care cohort (11.1% vs. 2.6%, respectively; P < 0.001). In standard care, half of the patients received their carotid surgery after they developed stroke, compared with none in the rapid evaluation group. No patient in the standard care group developed stroke following endarterectomy, versus 5% in the rapid evaluation group.
Significantly more patients in the rapid evaluation cohort received MRI, carotid Doppler, Holter monitoring, echocardiogram, CT angiogram, and MR angiogram, and this group was also more likely to be newly prescribed antihypertensives and statins. However, significantly more patients in standard are cohort had ECG.
Ontario Study
A study by Wasserman et al (17), conducted in Ontario, prospectively identified patients with symptoms of TIA who were seen at 2 tertiary care EDs and referred to a stroke clinic. The clinic provided rapid, standardized assessment and treatment for patients at risk for stroke. Of 1,093 patients diagnosed with TIA in ED, 1,004 were referred to the stroke clinic and 982 completed 90 days of follow-up.
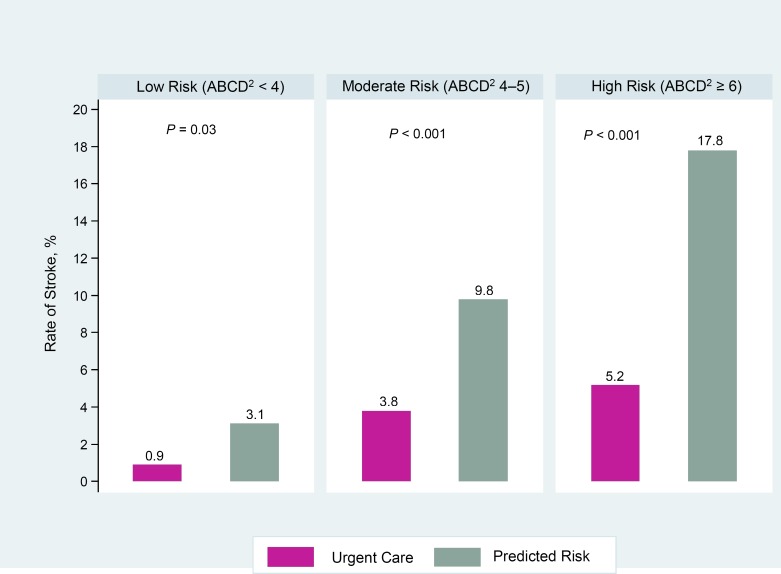
Patients were stratified into 3 groups according to their ABCD2 risk scores: 32% were classified as low risk (ABCD2 < 4), 49% were moderate risk (ABCD2 4–5), and 19% were high risk (ABCD2 ≥ 6). All groups received the same care. The primary outcome was risk of stroke at 90 days from symptom onset. Secondary outcomes were subsequent TIA, myocardial infarction (MI), or death.
At 90 days, the overall rate of stoke was 3.2%, while predicted risk was 9.2% (P < 0.001). Across all 3 risk strata, the observed rate of stroke was significantly lower than the predicted risk (Figure 7). Rate of subsequent TIA was 5.5%, rate of MI was 0.1%, and all-cause mortality was 1.7%, including 3 patients who died from stroke.
Figure 7: Rate of Stroke Following Transient Ischemic Attack at 90 Days in Ontario Study According to Risk Category.
Source: Wasserman et al, 2010 (17)
On arrival at the ED, 41% of the patients had previously been prescribed blood pressure lowering medications, 27% were on statins, and 35% were on antiplatelet therapy. Carotid Doppler identified carotid stenosis in 45% of patients, but less than 1% of patients underwent carotid endarterectomy. The mean times (SD) between presentation to ED and carotid Doppler, echocardiography, and Holter monitoring were 12.5 (14.1) days, 16.8 (18.6) days, and 30.7 (18.2) days, respectively.
Two Aces Study
A study conducted in United States evaluated the outcomes of an ED-based triage system for patients presenting with symptoms of TIA. (18) Patients with ABCD2 scores of 3 or less were eligible to be discharged directly from the ED to an outpatient TIA clinic. For ABCD2 scores of 4 to 5, the protocol recommended cervical and intracranial vessel imaging, with hospitalization if imaging identified symptomatic vessel stenosis of 50% or greater and referral to the TIA clinic in the absence of significant stenosis. Patients with an ABCD2 score greater than 5 were hospitalized. Efforts were made to manage patients in the TIA clinic within 1 to 2 business days. It was assumed that the triage system would result in reduced hospitalization and that outcomes of hospitalized patients and those managed in the outpatient clinic would not differ.
Of 224 patients evaluated in the ED, 157 (70%) were referred to TIA clinic and 67 (30%) were hospitalized. Rate of stroke at 90 days was 0.6% (IQR, 0.1%–3.5%) for patients referred to TIA clinic and 1.5% (IQR, 0.3%–8.0%) for those who were hospitalized. For both groups combined, the rate of stroke was 0.9% (IQR, 0.3%–3.2%), which was significantly less than the predicted rate of 7.1% (P = 0.001). All stroke events occurred during the first 7 days.
The median time from symptom onset to evaluation at ED was 0 days, and 206 patients (92%) were seen at ED within 24 hours after onset of the symptoms. The median time between presentation at ED and TIA clinic was 3 days (IQR, 2–5) and 4 days from symptom onset (IQR, 2–6). Before going to the TIA clinic, 119 patients (76%) underwent an MRI and 144 patients (92%) had vascular imaging.
SOS-TIA Study
The SOS-TIA study, conducted in France, was a prospective study evaluating the effectiveness of a TIA clinic with round-the-clock access. (13) All assessments in this clinic were completed within 4 hours of admission, and treatment was then initiated. Leaflets about the clinic were sent to 15,000 family physicians, neurologists, ophthalmologists, and cardiologists in Paris and the administrative region. Of 1,085 patients with suspected TIA seen in the clinic from 2003 to 2005, about 53% were seen within 24 hours of symptom onset. Three-quarters of the patients were sent home on the same day. Among patients who required carotid revascularization, most received the procedure within 8 days.
At 90 days, the overall observed rate of stroke was 1.24%, whereas predicted risk based on ABCD2 scores was 5.96%. Patients whose brain imaging showed a new lesion had subsequent stroke at a rate 3.5 times higher than those who did not have a new lesion (4.76 vs. 1.34). At 1 year, the same pattern was still observed and patients with new lesions had the highest rate of stroke (Figure 8). The combined outcome of stroke, MI, and vascular death was also highest in patients who had a new lesion.
Figure 8: Rate of Stroke Following Transient Ischemic Attack at 90 Days and 1 Year in the SOS-TIA Study.
Abbreviations: TIA, transient ischemic attack.
Source: Lavallee et al, 2007. (13)
Within 15 days of symptoms onset, 82% of patients had CT scans, 78% had MRI, and 27% had diffusion-weighted imaging (DWI). Also within 15 days, 99% of patients had brain imaging performed, 82% had CT scans, 78% had MRI, and 27% had DWI. Patients also received the following procedures (no time period reported): intracranial and extracranial MR angiography, 71%; transthoracic echocardiography, 69%; transthoracic and transesophageal echocardiography, 61% each. Antithrombotic medication was given to 98% of patients who had minor stroke, definite TIA, or possible TIA. Among patients with atrial fibrillation, 76% were given oral anticoagulants. Blood pressure lowering medications were started or modified in 20.7% of patients, and lipid lowering medications were prescribed or modified in 45% of patients. Urgent carotid revascularization was performed in 5.7% of patients, with a median delay from initial examination of 6 days (IQR, 4–10).
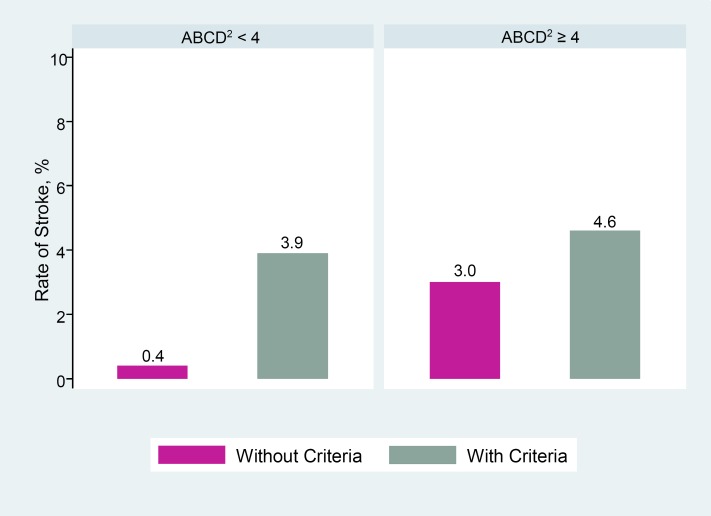
Amarenco et al (22) provided a new perspective on the risk of stroke using data from the SOS-TIA study. This second study (N = 1,679) included patients from the original SOS-TIA study plus additional patients who came to the clinic up to December 2008 with a definite or possible TIA and had 90 days of follow-up and complete information on ABCD2 scores. The study also defined criteria for emergency treatment as symptomatic carotid artery stenosis at 50% or greater (n = 157), symptomatic intracranial artery stenosis at 50% or greater (n = 85), or a major source of cardiac embolism (n = 169). These criteria were found in 18% of patients with scores of less than 4 and 28% of patients who scored 4 or greater.
By 90 days, 34 patients had subsequent strokes, including 3 that were fatal. Among 701 patients with ABCD2 scores of 4 or greater, stroke occurred in 24 (3.4%). However, among 180 patients with ABCD2 scores of less than 4 but who met any of the criteria for emergency treatment, 7 had subsequent stroke (3.9%). The risk of stroke was lowest among patients with scores of less than 4 who did not meet the criteria for emergency treatment (0.4%).
Using patients with ABCD2 scores of 4 or greater as a reference group, the study found that risk of stroke was significantly lower in patients with scores of less than 4 and no criteria for emergency treatment (P < 0.0001). However, patients with ABCD2 scores of less than 4 but who met the criteria for emergency treatment had similar risk of stroke as the reference group (P = 0.82) (Figure 9).
Figure 9: Rate of Stroke Following Transient Ischemic Attack, by Risk Scores and Criteria for Emergency Treatment.
Patients with criteria for emergency treatment had one of the following characteristics: symptomatic carotid artery stenosis ≥ 50%, symptomatic intracranial artery stenosis ≥ 50%, or a major source of cardiac embolism. Patients without criteria did not have any of these characteristics.
Source: Amarenco et al, 2012. (22)
Study From Denmark
In a study conducted in Denmark, a hospital-based TIA team was established to serve patients with TIA in the hospital's stroke unit and its TIA clinic. (14) Patients suspected of having TIA were referred to this team by primary care providers or the ambulances, bypassing the ED. All patients included in this study (n = 306) fulfilled diagnostic criteria of TIA lasting less than 24 hours and had a modified Rankin score of 2 or less. The primary outcome was a combination of stroke, MI, or vascular death within 1 year.
The cumulative stroke rate at 7 days, 90 days, and 1 year (1.6%, 2%, and 4.4%, respectively) was much less than the predicted rate for 7 days and 90 days (4.5% and 7.5%, respectively). Recurrent TIA occurred in 10.2% of patients. At 1-year follow-up, the cumulative mortality rate was 2.9%.
Preventive treatment was initiated immediately including fast track for carotid surgery. All patients underwent diagnostic work-up including neurologic examination, CT/MRI of the brain, ECG, laboratory tests, duplex ultrasound of the intra- and extracranial vessels. These examinations were performed during the first visit to the outpatient clinic and within 24 hours for patients admitted to the stroke unit. All patients with possible diagnosis of cardioembolism and all patients under 65 years of age and without a major cardiovascular risk factor were examined with Holter and/or transthoracic echocardiography. Transthoracic and transesophageal echocardiography were performed in 59.5% and 16.0% of patients, respectively. Holter monitoring was performed in 19.8% of the patients. Secondary prevention included treatments for vessel stenosis, atrial fibrillation, hypertension, and high lipid level. Carotid surgery was performed in 8.1% of patients, with a median time to operation of 11 days after first contact with the TIA team.
Study From Spain
A study conducted in Spain evaluated outcomes of TIA patients managed in an ED. (19) All consecutive patients with a diagnosis of TIA or MIS were assessed for eligibility. All patients were evaluated by an emergency physician without the aid of a neurologist, following a standardized protocol that had been in operation for more than 5 years before the start of the study. Patients (n = 97) were followed for 90 days.
At 90 days, the incidence of moderate to severe stroke was 4.2%, compared with the predicted rate of 9.9% based on ABCD2 scores. The overall incidence of moderate to severe stroke at 24 hours, 1 week, and 90 days was 0%, 1%, and 5%, respectively.
All patients underwent brain CT and electrocardiogram. Extracranial supra-aortic Doppler testing was performed in 94.5% of patients.
Study From Germany
A study conducted in Germany investigated the effectiveness of an outpatient TIA clinic in reducing the risk of stroke. (20) The clinic received referrals from family doctors (48.8%), neurologists (16.3%), ophthalmologists (0.8%), and other specialties (8.1%). The TIA clinic was open on weekdays and was comprised of a senior neurologist and a team of 3 nurses. Patients who were diagnosed with stroke were sent to the emergency department and stroke unit and those whose neurological dysfunction completely resolved in less than 24 hours were evaluated and treated in the TIA clinic.
The median time from symptom onset to presentation at the TIA clinic was 48 hours (range, 1 hour to 3 months). The median time from presentation to TIA clinic to the first cerebral imaging was 123 minutes (range, 12–72 minutes). MRI was performed in 79.7% of the patients, and 37.4% received a CT scan. Extracranial and transcranial duplex sonography were performed in 95.1% and 48% of the patients, respectively. Screening for patent foramen ovale was performed in 56.1%, an ECG in 91.9%, echocardiography in 12.2%, and other examinations were performed in 38.2% of the patients. TIA patients received secondary prevention treatments immediately.
Twelve patients (9.8%) were admitted to the stroke unit because they had ABCD2 scores of 4 or greater or had experienced TIA within 72 hours, symptomatic arterial stenosis, a newly detected atrial fibrillation, or recurrent TIA. The remaining patients were discharged home. During a 3-month follow-up, 2 ischemic strokes occurred. The rate of stroke was 1.6% among all patients referred to the TIA clinic with suspected TIA, and 2.9% among those with confirmed TIA or minor stroke. These rates were much lower than the 90-day predicted risk of 5.7%, based on ABCD2 score.
Urgent Care Provided in Hospital Settings
Four studies reported on the outcomes of TIA patients after hospitalization. Three studies were comparative and 1 was a single-arm study. Table 8 shows study design and patient characteristics.
Table 8:
Characteristics of Studies Reporting on Urgent Care Provided in Hospital Settings Following Transient Ischemic Attack
| Author, Year | Country | Study design | Number of Patients | Mean Age, Years (SD) | Follow-Up, Months |
|---|---|---|---|---|---|
| Ross et al, 2007 (23) | United States | RCT | 149 | ED: 68.4 (15.3) Inpatient: 67.7 (15.4) |
3 |
| Martinez-Martinez et al, 2013 (24) | Spain | Prospective cohort (Comparative) | 211 | TIA clinic: 65.73 (15.8) In-hospital: 67.91 (15.2) |
3 |
| Kehdi et al, 2008 (25) | Australia | Registry (Comparative) | 2,535 | Admitted: 70 (14.1) Discharged: 67.9 (15.8) |
12 |
| Calvet et al, 2007 (26) | France | Prospective cohort (Single arm) | 203 | 61.2 (16) | 3 |
Abbreviations: ED, emergency department; RCT, randomized controlled trial; SD, standard deviation; TIA, transient ischemic attack.
Urgent Care Provided in Emergency Department Observation Unit Versus Urgent Care Provided in Hospital
A prospective randomized controlled trial compared ED diagnostic protocol with hospitalization. (23) Patients who came to the ED and were diagnosed with TIA by a board-certified ED physician were screened according to eligibility criteria of the study. Patients were excluded if they had acute infarction, mass, or bleeding on their initial CT scan, an embolic source including a history of atrial fibrillation, or carotid stenosis greater than 50%. Patients were observed and treated in an adjacent ED observation unit by attending ED physician assistants using specific guidelines and protocols. Screening was available 24 hours, 7 days a week, and patients who met the eligibility criteria and gave informed consent were randomized to either an accelerated diagnostic protocol (ADP) (n = 75) or admission to hospital (n = 74). Fifteen percent of those in the ADP arm were admitted to hospital during their stay in observation unit. The ADP program had been operational for more than 1 year before the start of the study. On completion of the protocol, patients were discharged home if they had no recurrent deficits, had negative tests results, and were clinically stable.
The primary outcome of the study was length of stay of the index visit. Secondary outcomes were 90-day total direct cost and clinical outcomes including rate of stroke. The sample size estimate was based on the primary end point. All patients completed 90 days of follow-up.
Index visit length of stay was 61.2 hours (IQR, 41.6–92.2) for those admitted to hospital and 25.6 hours (IQR, 21.9–28.7) for those in observation unit (P < 0.001). ADP patients who were hospitalized had longer stays (mean, 100 hours) and higher costs ($2,737) than the inpatient arm. However, both index visit total direct cost and 90-day total direct cost were significantly lower in the ADP arm overall (Table 9).
Table 9:
Costs Within 90 Days Following Transient Ischemic Attack, Inpatient Care Versus Emergency Department Observation Unit
| 90-Day Total Direct Cost, $US | ||||
|---|---|---|---|---|
| Inpatient | ED Observation Unit With ADP | Difference, Median | P Value | |
| Index visit total direct cost, median (IQR) | 1,529 (1,091–2,306) | 864 (726–1,076) | 617 (413–842) | < 0.001 |
| 90-day total direct cost, median (IQR) | 1,548 (1,091–2,474) | 890 (768–1,510) | 540 (312–810) | < 0.001 |
Abbreviations: ADP, accelerated diagnostic protocol; ED, emergency department; IQR, interquartile range.
Source: Ross et al, 2007. (23)
Index visit stroke occurred in 5 patients (6.8%) in the inpatient arm and in 7 (9.3%) in the ADP arm. All 7 strokes in ADP arm occurred when patients were in the ED observation unit, and all were subsequently admitted to the hospital. Rate of subsequent stroke to 90 days was also lower among patients originally admitted to hospital, but it was not significantly different from those in the ADP arm (2.7% vs. 4%). The study did not report the significance of the difference between the two groups with respect to the overall rate of stroke (Figure 10). Patients in the ADP arm who were later hospitalized had much higher rates of limb weakness and diabetes at baseline than those who were originally randomized to the inpatient arm.
Figure 10: Rate of Stroke and Other Major Events at 90 Days, Inpatient Versus Emergency Department Observation Unit.
Abbreviations: ED, emergency department.
Source: Ross et al, 2007. (23)
In both arms, more than 90% of patients had carotid imaging, but it was performed faster in the ADP arm (median, 13 hours; IQR, 8.4–18) than the inpatient arm (median, 25.2 hours; IQR, 17.3–37.1). More patients in the ADP arm received echocardiography (97% vs. 73%) and also in less time (median, 19.1 hours [IQR, 16.7–22.5] vs. 43 hours [IQR, 23.8–63.8]) (Table 10). In each group, 7 patients had greater than 70% carotid artery stenosis but no carotid endarterectomy was performed in 90 days in either arm.
Table 10:
Percentage of Tests Completed and Time to Completion for Patients With Transient Ischemic Attack, Inpatient Versus Emergency Department Observation Unit
| Tests Completed, % | Hospitalized | ED Observation Unit |
| Carotid imaging completed | 91 | 97 |
| Carotid Doppler | 91 | 96 |
| Echocardiography | 73 | 97 |
| Time to Completion of Tests, Hours (Range) | ||
| Carotid imaging | 25.2 (17.3–37.1) | 13 (8.4–18) |
| Echocardiography | 43 (23.8–63.8) | 19.1 (16.7–22.5) |
Abbreviations: ED, emergency department.
Source: Ross et al, 2007. (23)
Standard Care Provided in Emergency Department Versus Urgent Care Provided in Hospital
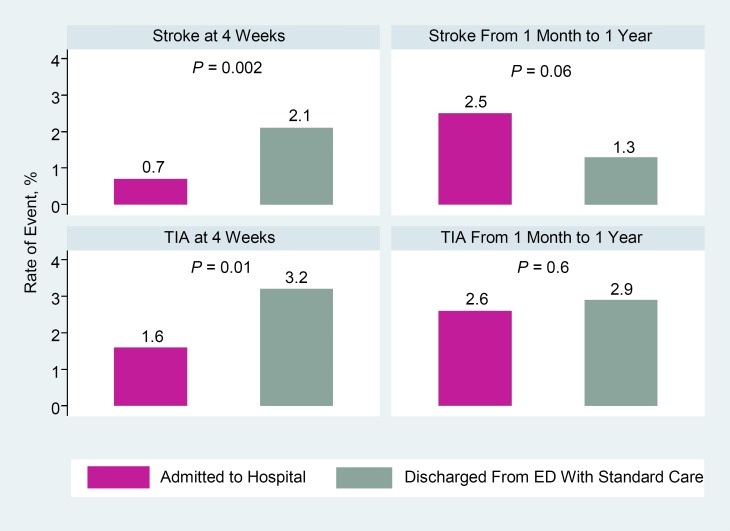
A study by Kehdi et al, (25) based on data from the Australian Stroke Registry, reported 4-week and 1-year outcomes of 2,533 TIA patients who presented to the ED in a large region of Sydney. Outcomes were compared between patients who were discharged from the ED (71.6%) and those who were hospitalized (28.4%).
At 4 weeks, the discharged group had significantly higher rate of stroke than the admitted group. Rate of a subsequent TIA was also significantly higher in the discharged group. At 1 year, however, rate of stroke was higher for admitted patients. Rate of subsequent TIA at 1 year was similar between the two groups (Figure 11).
Figure 11: Rate of Stroke and Transient Ischemic Attack Following Admission to Hospital or Discharge from Emergency Department.
Abbreviations: TIA, transient ischemic attack.
Source: Kehdi et al, 2008. (25)
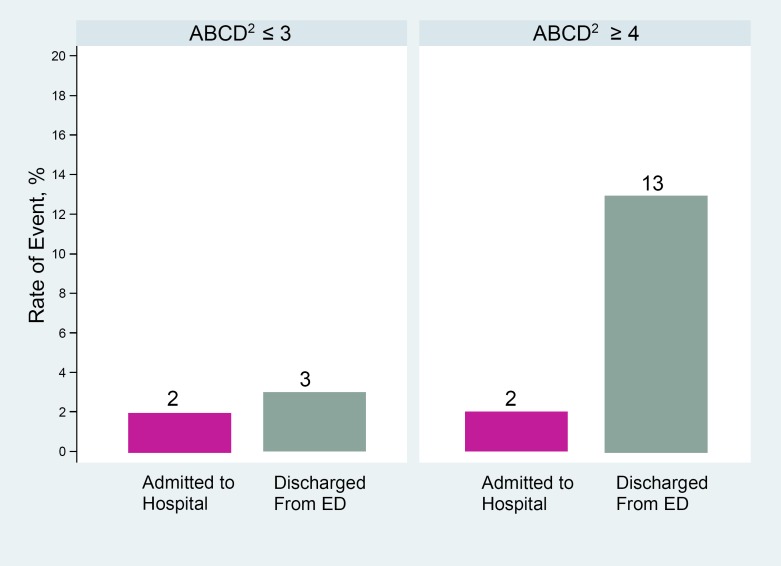
In this study, risk score was calculated for 383 patients admitted to the principal referral hospital and for 102 patients discharged from ED. The proportions of patients with low, moderate, and high risk were similar between the 2 arms. When data were stratified by risk scores, the differences at 4 weeks appeared to be mainly due to the patients who were at high risk of stroke; while rate of stroke was similar in the 2 groups for patients who had ABCD2 score of 3 or less, patients with ABCD2 scores of 4 or greater had a 6-fold higher rate of stroke if they were discharged from ED compared to admitted patients in the same risk category (Figure 12).
Figure 12: Rate of Stroke or Transient Ischemic Attack at 4 Weeks, by Risk Scores.
Abbreviations: ED, emergency department.
Subgroup analysis based on data from principal referral hospital.
Source: Kehdi et al, 2008. (25)
Urgent Care Provided in TIA Clinic Versus Urgent Care Provided in Hospital for Low- to Moderate-Risk Patients
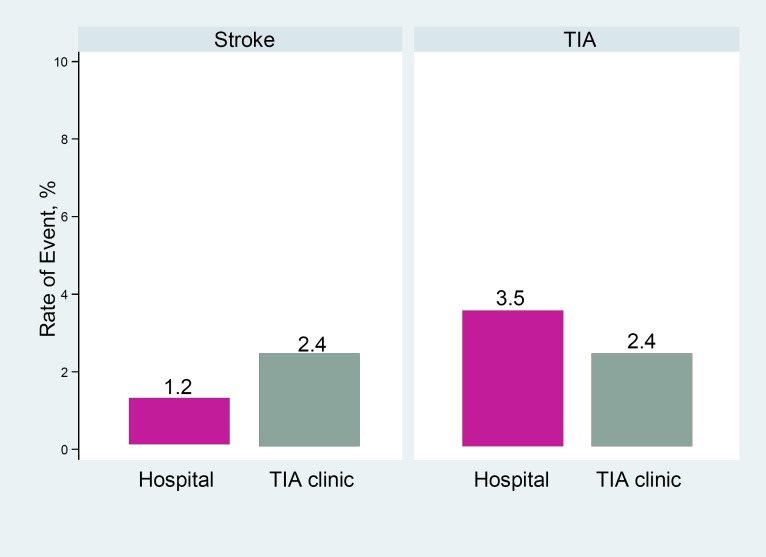
A study conducted in Spain evaluated the management of TIA patients with low to moderate risk scores, defined as ABCD2 of 5 or less, no recurrent TIA in the previous week, and no active embolic source suspected. (24) The study compared the outcomes of 211 patients managed in a TIA clinic in 2010 (n = 125) with hospitalized patients managed by the same stroke team in 2009 (n = 86).
At 90 days, rates of stroke were 1.2% in hospitalized patients and 2.4% in TIA clinic patients (P = 0.65). TIA recurred in 3.5% of hospitalized patients and 2.4% of TIA clinic patients (P = 0.69) (Figure 13).
Figure 13: Rate of Stroke and Transient Ischemic Attack in Patients Managed in TIA Clinic or Admitted to Hospital.
Abbreviations: TIA, transient ischemic attack.
Source: Martinez-Martinez et al, 2013 (24)
More patients in the TIA clinic received brain MRI (P = 0.05), but more hospitalized patients received echocardiography (P = 0.01). No significant differences were found in other measures of care (Table 11).
Table 11:
Measures of Process of Care – Hospitalized Versus TIA Clinic
| Tests Completed, % of Patients | Hospitalized | TIA Clinic |
| Brain MRI | 58.1 | 71.2 |
| Echocardiography | 70.6 | 52.8 |
| Holter monitoring | 25.9 | 35.2 |
| Medications, % of Patients | ||
| Antiplatelet agents | 83.7 | 77 |
| Anticoagulation | 16.3 | 9.6 |
| Antihypertensive agent | 16.3 | 13.6 |
| Statin | 69.8 | 65.6 |
Abbreviations: MRI, magnetic resonance imaging; TIA, transient ischemic attack.
Source: Martinez-Martinez et al, 2013 (24)
Urgent Care Provided in Stroke Unit
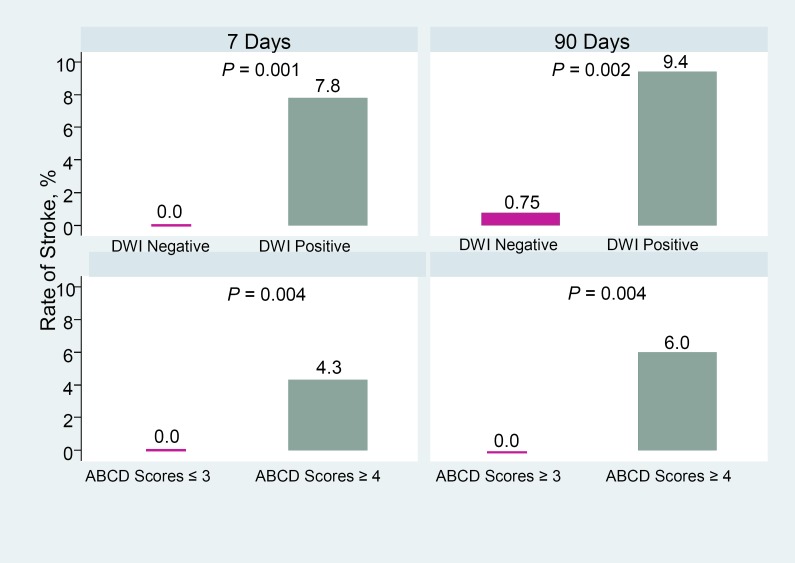
A prospective study by Calvet et al (26) investigated outcomes of 203 TIA patients admitted to a stroke unit. Patients with TIA symptoms for less than 48 hours were included and followed for 3 months.
The overall rate of stroke was 2.5% at 7 days and 3.5% at 90 days and, at both periods, the presence of brain abnormality and higher ABCD risk scores were independent predictors of subsequent stroke (Figure 14). Patients who had a positive DWI had significantly higher rate of stroke at 7 days and 90 days, compared to patients with negative imaging, and most of those strokes occurred within 7 days. The same pattern was seen when data were stratified by risk category. For patients with risk scores of 4 or greater, rate of stroke was 4.3% at 7 days and 6% at 90 days, while no patients with risk scores of 3 or less developed stroke within 90 days. Risk of stroke for patients with ABCD scores of 4 was 1.7% at 7 days and 3.3% at 90 days. The risk was much higher for scores of 5 to 6 (7% at 7 days and 8.8% at 90 days).
Figure 14: Risk of Stroke in Patients Admitted to Stroke Unit, by Brain Status and Risk Scores.
Abbreviations: DWI, diffusion-weighted imaging.
Source: Calvet et al, 2007. (26)
All patients had their initial assessment and treatment within 48 hours. The time from TIA onset to initial assessment and treatment was 6 hours or less for 105 patients (53%) and 12 or less for 153 patients (78%). Although all patients received brain imaging within 48 hours, about one-fifth received echocardiography within this time (Table 12). However, cardiac monitoring resulted in the diagnosis of 10 cases of previously unknown atrial fibrillation. Overall, 147 (72%) patients received antiplatelet therapy only, 56 (28%) received anticoagulation with full-dose heparin, and 7 (3%) had a carotid procedure.
Table 12:
Tests Completed in Stroke Unit Within 48 Hours After Onset of Transient Ischemic Attack
| Diagnostic Evaluation | 12 Hours, % of Patients | 24 Hours, % of Patients | 48 Hours, % of Patients |
|---|---|---|---|
| Brain imaging | 82 | 90 | 100 |
| Cervical artery imaging | 12 | 40 | 82 |
| Echocardiography | 2 | 7 | 21 |
Abbreviations: TIA, transient ischemic attack.
Source: Calvet et al, 2007. (26)
Summary of Results
Rapid Evaluation and Treatment Versus Standard Care
One large observational study (the EXPRESS study, N = 591) showed that urgent assessment of patients with TIA and minor ischemic stroke significantly reduces the risk of subsequent stroke, by 80% (GRADE: Moderate), and reduces the total days in hospital due to recurrent stroke (GRADE: Low) and associated costs (GRADE: Very low) (15) Seven other studies (13;14;16–20) supported the findings of the EXPRESS study (GRADE: Low). No adverse effects associated with early assessment and treatment of these patients were reported.
A study from Alberta (N = 581) found that urgent evaluation and treatment of high-risk TIA patients in a specialized clinic can reduce the risk of stroke by half, but with higher costs. (16) (GRADE: Low)
A study based on the registry of the Canadian Stroke Network showed a significantly lower rate of death among patients referred to stroke prevention clinics following TIA or minor stroke, compared to patients who were not referred to such services. (12)
Two studies showed that brain imaging can inform both diagnosis and prognosis. (13;26) In 1 study (N = 1,085), patients found to have acute lesions had a significantly higher risk of stroke following TIA, compared to patients whose imaging found no new lesions. (13) In the other study (N = 203), the presence of abnormality on DWI was associated with a higher risk of stroke. (26) (GRADE: Low)
A study based on data from the SOS-TIA study in France (N = 1,679) reported that ABCD2 risk score does not reflect the presence of conditions that require immediate treatment (symptomatic internal carotid or intracranial artery stenosis greater than 50% or a major cardiac source of embolism). (22) Therefore, relying on ABCD2 risk score alone may result in missed opportunities to treat patients with these conditions. (GRADE: Low)
An Ontario study (N = 982) showed that rapid access to a specialized clinic for evaluation of TIA and minor ischemic stroke can result in lower rates of subsequent stroke, even in high-risk patients. (17) (GRADE: Low)
Inpatient Versus Outpatient Care
An RCT (N = 149) showed that index visit length of stay, index visit total direct cost, and 90-day total direct cost were significantly shorter for TIA patients treated urgently in an ED-based observation unit than for patients seen in the ED and then admitted to the hospital. (23) (GRADE: Low)
A study on low- to moderate-risk TIA patients (N = 211) showed that the risk of subsequent stroke was low and was similar whether patients were managed in a TIA clinic or hospitalized. The cost per patient was about 5 times less for patients managed in TIA clinic than for hospitalized patients. (24) (GRADE: Low)
A study based on Australian registry data (N = 2,535) showed that the rate of subsequent stroke at 4 weeks after TIA was significantly higher in patients who received regular care and were discharged from the ED, compared to TIA patients who were hospitalized. (25) (GRADE: Low) In patients with ABCD2 risk scores of 4 or greater, the rate of stroke was 6 times higher for those who received standard care, compared to hospitalized patients.
A study of TIA patients hospitalized in a stroke unit (N = 203) showed that rate of stroke was 6 times higher in patients with ABCD2 scores of 5 or greater (8.8%), compared with patients with risk scores of 4 or less (1.4%). (26) (GRADE: Low)
Conclusion
The results of this systematic review, based on low to moderate quality of evidence, have important clinical implications.
Emergency investigation and initiation of treatment of patients with signs and symptoms of transient ischemic attack (TIA) is an effective strategy in reducing the incidence of subsequent stroke. Management in TIA clinics, where patients can be evaluated and treated urgently, results in lower rates of stroke and disability than conventional treatment. About half of strokes following TIA occur within the first 48 hours; therefore, patients with TIA should be evaluated as early as possible within 24 hours of first call to medical attention.
Patients at high risk of stroke may require admission to a stroke unit for further evaluation and appropriate treatment. This review showed that patients with an ABCD2 score of 4 or higher have significantly higher rates of stroke or recurrent TIA if they receive standard treatment and are discharged from an emergency department, compared to patients who are hospitalized. This may indicate that higher-risk patients need more comprehensive, intensive investigation and management than lower-risk patients.
At the same time, this analysis identified limitations to the use of ABCD2 risk scores in assessing which patients are at higher risk of stroke. ABCD2 risk scores do not reflect the absence or presence of conditions that require immediate treatment (i.e., symptomatic internal carotid or intracranial artery stenosis of 50% or greater or a major cardiac source of embolism). Therefore, imaging data can improve both diagnosis and prognosis for patients at particularly high risk for stroke. The diagnosis of TIA should be based on all available information including history, clinical examination, and laboratory tests supplemented with imaging.
For patients with ABCD2 score of 5 or less, no recurrent TIA in the previous week, and no active embolic source, no significant differences were found in rates of stroke or subsequent TIA between those managed in a TIA clinic and those admitted to hospital. The cost of initial assessment of these patients at a TIA clinic is less than the cost of hospital admission. No studies compared the outcomes of care in a TIA clinic and care via hospital admission for high-risk patients.
Acknowledgements
Editorial Staff
Amy Zierler, BA
Medical Information Services
Corinne Holubowich, BEd, MLIS
Kellee Kaulback, BA(H), MISt
Consulting Experts
| Name | Affiliation(s) | Appointment(s) |
|---|---|---|
| Panel Co-Chairs | ||
| Dr. Mark Bayley | Toronto Rehabilitation Institute; University of Toronto | Medical Director of the Neuro-rehabilitation Program; Associate Professor |
| Dr. Leanne K. Casaubon∗ | Toronto Western Hospital; University of Toronto | Assistant Professor-Division of Neurology, Stroke Program |
Appendices
Appendix 1: Literature Search Strategies
Search date: December 21, 2012
Databases searched: OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE; Cochrane Library; CRD
Database: Ovid MEDLINE(R) 〈1946 to November Week 3 2012〉, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations 〈December 20, 2012〉, Embase 〈1980 to 2012 Week 50〉
Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp Ischemic Attack, Transient/ use mesz | 17143 |
| 2 | exp transient ischemic attack/ use emez | 21887 |
| 3 | (tia? or transient isch?emic attack∗).ti,ab. | 28687 |
| 4 | or/1-3 | 53587 |
| 5 | exp Time Factors/ use mesz or exp Delayed Diagnosis/ or exp time/ use emez | 1452869 |
| 6 | exp Emergency Medical Services/ use mesz or exp emergency health service/ use emez | 147818 |
| 7 | exp Hospitalization/ | 328591 |
| 8 | exp Outpatient Clinics, Hospital/ use mesz or exp outpatient department/ use emez | 50440 |
| 9 | (tia? clinic∗ or transient isch?emic attack∗ clinic∗).ti,ab. | 235 |
| 10 | (special∗ adj4 (tia or transient isch?emic attack∗)).ti,ab. | 64 |
| 11 | ((immediate or rapid or early or urgent or delay∗ or prompt) adj2 (evaluation or diagnosis or treatment or assessment or access or care)).ti,ab. | 294344 |
| 12 | exp Risk Assessment/ | 462483 |
| 13 | or/5-12 | 2610144 |
| 14 | 4 and 13 | 8090 |
| 15 | limit 14 to english language | 7139 |
| 16 | limit 15 to human | 5443 |
| 17 | limit 16 to yr=“2007 -Current” | 2830 |
| 18 | exp Case Reports/ use mesz or exp case report/ use emez | 3480048 |
| 19 | exp letter/ or exp editorial/ | 2342573 |
| 20 | exp Comment/ use mesz | 493546 |
| 21 | or/18-20 | 5580626 |
| 22 | 17 not 21 | 2610 |
| 23 | remove duplicates from 22 | 2051 |
Cochrane
| ID | Search | Hits |
|---|---|---|
| #1 | MeSH descriptor: [Ischemic Attack, Transient] explode all trees | 471 |
| #2 | tia? or transient isch?emic attack∗:ti (Word variations have been searched) | 130 |
| #3 | #1 or #2 | 563 |
| #4 | MeSH descriptor: [Time Factors] explode all trees | 44941 |
| #5 | MeSH descriptor: [Delayed Diagnosis] explode all trees | 7 |
| #6 | MeSH descriptor: [Emergency Medical Services] explode all trees | 2416 |
| #7 | MeSH descriptor: [Hospitalization] explode all trees | 10365 |
| #8 | MeSH descriptor: [Outpatient Clinics, Hospital] explode all trees | 588 |
| #9 | tia? clinic∗ or transient isch?emic attack∗ clinic∗:ti (Word variations have been searched) | 14 |
| #10 | (special∗ near/4 (tia or transient isch?emic attack∗)):ti,ab,kw (Word variations have been searched) | 1 |
| #11 | ((immediate or rapid or early or urgent or delay∗ or prompt) near/2 (evaluation or diagnosis or treatment or assessment or access or care)):ti (Word variations have been searched) | 1655 |
| #12 | MeSH descriptor: [Risk Assessment] explode all trees | 6034 |
| #13 | #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 | 61997 |
| #14 | #3 and #13 from 2007 to 2012 | 35 |
CRD
| Search Hits | ||
|---|---|---|
| 1 | MeSH DESCRIPTOR Ischemic Attack, Transient EXPLODE ALL TREES | 45 |
| 2 | (tia? or transient isch?emic attack):TI | 9 |
| 3 | #1 OR #2 | 46 |
| 4 | MeSH DESCRIPTOR Time Factors EXPLODE ALL TREES | 1821 |
| 5 | MeSH DESCRIPTOR Delayed Diagnosis EXPLODE ALL TREES | 1 |
| 6 | MeSH DESCRIPTOR Emergency Medical Services EXPLODE ALL TREES | 529 |
| 7 | MeSH DESCRIPTOR Hospitalization EXPLODE ALL TREES | 2395 |
| 8 | MeSH DESCRIPTOR Outpatient Clinics, Hospital EXPLODE ALL TREES | 72 |
| 9 | (tia? clinic∗ or transient isch?emic attack∗ clinic∗) | 1 |
| 10 | (special∗ adj4 (tia or transient isch?emic attack∗)) | 0 |
| 11 | ((immediate or rapid or early or urgent or delay∗ or prompt) adj2 (evaluation or diagnosis or treatment or assessment or access or care)):TI | 208 |
| 12 | MeSH DESCRIPTOR risk assessment EXPLODE ALL TREES | 1150 |
| 13 | #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 | 5395 |
| 14 | #3 AND #13 | 14 |
| 15 | (#14):TI FROM 2007 TO 2012 | 9 |
Appendix 2: GRADE Tables
Table A1:
GRADE Evidence Profile for Comparison of Urgent Care and Standard Care for Transient Ischemic Attack
| Number of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Death | |||||||
| 1 large observational study | Serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Risk of Stroke | |||||||
| 1 large observational study | Serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | +1a | ⊕⊕⊕ Moderate |
| 1 observational comparative and 6 single-arm studies | Serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Length of Stay | |||||||
| 1 large observational study | Serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Cost | |||||||
| 1 large observational study | Serious limitations | No serious limitations | No serious limitations | Serious limitations | Undetected | −1b | ⊕ Very low |
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation.
Large magnitude of effect.
Very wide confidence interval.
Table A2:
GRADE Evidence Profile for Comparison of TIA Care Provided in Hospital and Other Settings
| Number of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Risk of Stroke | |||||||
| 1 RCT | Very serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Undetected | – 2 | ⊕⊕ Low |
| 3 observational studies | Serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Length of Stay | |||||||
| 1 RCT | Serious limitationsb | No serious limitations | No serious limitations | No serious limitations | Undetected | – 1 | ⊕⊕⊕ Moderate |
| Cost | |||||||
| 1 RCT | Serious limitationsb | No serious limitations | No serious limitations | No serious limitations | Undetected | – 1 | ⊕⊕⊕ Moderate |
| 1 observational study | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; RCT, randomized controlled trial; TIA, transient ischemic attack.
Inadequate power
Blinding of the patients and the investigators was not possible.
References
- (1).Johnston SC, Rothwell PM, Nguyen-Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007. Jan 27; 369 (9558):283–92. [DOI] [PubMed] [Google Scholar]
- (2).Gorelick PB. The burden and management of TIA and stroke in government-funded healthcare programs. Am J Manag Care. 2009. Jun; 15 (6 Suppl): S177–S184. [PubMed] [Google Scholar]
- (3).Kapral MK, Hall R, Stamplecoski M, Meyer S, Asllani E, Fang J, Richards J, O'Callaghan C, Silver FL. Registry of the Canadian Stroke Network – report on the 2008/09 Ontario Stroke Audit [Internet]. Toronto, ON: Institute for Clinical Evaluative Sciences; 2011. [cited: 2014 Dec 18]. 4 p. Available from: http://ontariostrokenetwork.ca/pdf/ICES_Stroke_Report_Final_2011_March.pdf [Google Scholar]
- (4).Guidelines and protocols advisory committee. Stroke and transient ischemic attack management and prevention [Internet]. Vancouver, BC: British Columbia Medical Association, Joint publication of the British Columbia Ministry of Health; 2012. Apr 29 [cited: 2012 Nov]. 8 p. Available from: http://www.bcguidelines.ca/pdf/stroke.pdf [Google Scholar]
- (5).Johansen HL, Wielgosz AT, Nguyen K, Fry RN. Incidence, comorbidity, case fatality and readmission of hospitalized stroke patients in Canada. Can J Cardiol. 2006. Jan; 22 (1):65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009. Jun; 40 (6):2276–93. [DOI] [PubMed] [Google Scholar]
- (7).Purroy F, Jimenez-Caballero PE, Mauri-Capdevila G, Torres MJ, Gorospe A, Ramirez Moreno JM, et al. Predictive value of brain and vascular imaging including intracranial vessels in transient ischaemic attack patients: external validation of the ABCD3-I score. Eur J Neurol. 2013. Jul; 20 (7):1088–93. [DOI] [PubMed] [Google Scholar]
- (8).Lin HJ, Yeh PS, Tsai TC, Cheng TJ, Ke D, Lin KC, et al. Differential risks of subsequent vascular events for transient ischaemic attack and minor ischaemic stroke. J Clin Neurosci. 2007. Jan; 14 (1):17–21. [DOI] [PubMed] [Google Scholar]
- (9).Atanassova PA, Chalakova NT, Dimitrov BD. Major vascular events after transient ischaemic attack and minor ischaemic stroke: post hoc modelling of incidence dynamics. Cerebrovasc Dis. 2008; 25 (3): 225–33. [DOI] [PubMed] [Google Scholar]
- (10).Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011. Apr; 64 (4):380–2. [DOI] [PubMed] [Google Scholar]
- (11).Goodman C. Literature searching and evidence interpretation for assessing health care practices. Stockholm, Sweden: Swedish Council on Technology Assessment in Health Care; 1996. 81 p. SBU Report No. 119E. [DOI] [PubMed]
- (12).Webster F, Saposnik G, Kapral MK, Fang J, O'Callaghan C, Hachinski V. Organized outpatient care: Stroke prevention clinic referrals are associated with reduced mortality after transient ischemic attack and ischemic stroke. Stroke 42 (11) ()(pp 3176–3182), 2011 Date of Publication: November 2011. 2011;(11):3176–82. [DOI] [PubMed] [Google Scholar]
- (13).Lavallee PC, Meseguer E, Abboud H, Cabrejo L, Olivot JM, Simon O, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007. Nov; 6 (11):953–60. [DOI] [PubMed] [Google Scholar]
- (14).von Weitzel-Mudersbach P, Johnsen SP, Andersen G. Low risk of vascular events following urgent treatment of transient ischaemic attack: the Aarhus TIA study. Eur J Neurol. 2011. Nov; 18 (11):1285–90. [DOI] [PubMed] [Google Scholar]
- (15).Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JN, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007. Oct 20; 370 (9596):1432–42. [DOI] [PubMed] [Google Scholar]
- (16).Wu CM, Manns BJ, Hill MD, Ghali WA, Donaldson C, Buchan AM. Rapid evaluation after high-risk TIA is associated with lower stroke risk. Can J Neurol Sci. 2009. Jul; 36 (4):450–5. [DOI] [PubMed] [Google Scholar]
- (17).Wasserman J, Perry J, Dowlatshahi D, Stotts G, Stiell I, Sutherland J, et al. Stratified, urgent care for transient ischemic attack results in low stroke rates. Stroke. 2010. Nov; 41 (11):2601–5. [DOI] [PubMed] [Google Scholar]
- (18).Olivot JM, Wolford C, Castle J, Mlynash M, Schwartz NE, Lansberg MG, et al. Two aces: transient ischemic attack work-up as outpatient assessment of clinical evaluation and safety. Stroke. 2011. Jul; 42 (7):1839–43. [DOI] [PubMed] [Google Scholar]
- (19).Torres MJ, Pena LG, Perez MD, Gonzalez MA, Gamez DS, Mateo AS, et al. Outcomes of atherothrombotic transient ischemic attack and minor stroke in an emergency department: results of an outpatient management program. Ann Emerg Med. 2011. May; 57 (5):510–6. [DOI] [PubMed] [Google Scholar]
- (20).Horer S, Schulte-Altedorneburg G, Haberl RL. Management of patients with transient ischemic attack is safe in an outpatient clinic based on rapid diagnosis and risk stratification. Cerebrovasc Dis. 2011; 32 (5): 504–10. [DOI] [PubMed] [Google Scholar]
- (21).Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol. 2009. Mar; 8 (3):235–43. [DOI] [PubMed] [Google Scholar]
- (22).Amarenco P, Labreuche J, Lavallee PC. Patients with transient ischemic attack with ABCD2 <4 can have similar 90-day stroke risk as patients with transient ischemic attack with ABCD2 >/=4. Stroke. 2012. Mar; 43 (3):863–5. [DOI] [PubMed] [Google Scholar]
- (23).Ross MA, Compton S, Medado P, Fitzgerald M, Kilanowski P, O'Neil BJ. An emergency department diagnostic protocol for patients with transient ischemic attack: a randomized controlled trial. Ann Emerg Med. 2007. Aug; 50 (2):109–19. [DOI] [PubMed] [Google Scholar]
- (24).Martinez-Martinez MM, Martinez-Sanchez P, Fuentes B, Cazorla-Garcia R, Ruiz-Ares G, Correas-Callero E, et al. Transient ischaemic attacks clinics provide equivalent and more efficient care than early in-hospital assessment. Eur J Neurol. 2013. Feb; 20 (2):338–43. [DOI] [PubMed] [Google Scholar]
- (25).Kehdi EE, Cordato DJ, Thomas PR, Beran RG, Cappelen-Smith C, Griffith NC, et al. Outcomes of patients with transient ischaemic attack after hospital admission or discharge from the emergency department. Med J Aust. 2008. Jul 7; 189 (1):9–12. [DOI] [PubMed] [Google Scholar]
- (26).Calvet D, Lamy C, Touze E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis. 2007; 24 (1): 80–5. [DOI] [PubMed] [Google Scholar]