Abstract
Objectives:
Treatment of choice at stable burst fracture is still a matter of debate. The aim of this study is assessment of health-related quality of life (HRQOL) regarding short form-36 (SF-36) and its correlation with kyphosis in patients affected by thoracolumbar burst fracture without neurological deficit undergoing posterior short segment pedicular screw fixation.
Materials and Methods:
Twenty patients with thoracolumbar burst fractures without neurological deficits, meeting our criteria were enrolled in this study. The patients underwent short segment pedicular screw fixation. After 2 years of follow-up, the outcome assessment was performed with evaluating HRQOL; SF-36. The mean ± standard deviation was measured at each eight category of SF-36 and compared with normative values of Iran. The correlation of Cobb angle and body pain was analyzed by linear regression.
Results:
The study detected reduced quality of life (QOL), with total mean of 49.7 ± 14 and physical function grade of 61.2 ± 22 which was significantly lower than Iran normative reported as 85.9 ± 19. Fifty percent still suffered from moderate to severe pain and Cobb angle had no statistically significant correlation with body pain.
Conclusions:
It seems that surgical treatment could not improve pain related disability of patients with stable thoracolumbar burst fracture at long term follow up.
Keywords: Burst, fracture, kyphosis, quality of life, thoracolumbar
Introduction
Thoracolumbar junction is the most common area of the spine involved in burst fractures.[1,2,3] Burst fractures are divided into several subtypes regarding neurological status and morphology.[2,3,4] Treatment of choice at stable burst fracture without neurological deficit is still a matter of debate and there is a lack of evidence on the superiority of operative treatment at long-term follow-up.[1,5,6]
Considering the outcome, besides pain relief, patient's subjective perception increasingly became aim in medicine.[3,7,8] Therefore, the postoperative quality of life (QOL) occupies an important position in trauma surgery. Short form-36 (SF-36) is one of the tools for assessment of health-related quality of life (HRQOL).
The aim of this study is assessment of HRQOL in patients affected by thoracolumbar burst fracture without neurological deficit undergoing posterior short segment pedicular screw fixation. This is the first norm-based analysis to compare pathologic and normal values of HRQOL in Iran, which could evaluate the patients at the same population of their origin. Besides, long-term follow-up is considered.
Materials and Methods
Twenty patients with thoracolumbar burst fractures without neurological deficits, meeting our criteria were enrolled in this study. X-ray, computed tomography scan, and magnetic resonance imaging study of the whole spine were performed. The inclusion criteria were as follows: burst fracture at anterior and middle column, intact posterior ligamentous complex (PLC), intact facet and decreased height <50%. The patients underwent posterior short segment pedicular screw fixation. After 2 years of follow-up, the outcome assessment was performed with evaluating HRQOL; SF-36. The mean ± standard deviation (SD) was measured at each eight category of SF-36 and compared with normative values of Iran. Analysis was performed with Chi-square test. Statistical significance was considered as P < 0.05.
Kyphosis was measured as Cobb angle. The correlation of Cobb angle and body pain was analyzed by linear regression. IBM SPSS software version 17.0 was used for data analysis. The whole study was approved by the local ethics committee and informed consents were signed by all of the patients before surgery.
Results
Male to female ratio was 2/1 with a mean age of 44.5 ± 7.6 (mean ± SD). The level of fracture was equally divided between L1 and T12.
The assessment showed reduced QOL, with total mean of 49.7 ± 14 and physical function grade of 61.2 ± 22 which was significantly lower than Iran normative reported as 85.9 ± 19 (P < 0.05). Bodily pain (BP) was 34 ± 29 comparing to the normal value of 78.9 ± 26 (P < 0.05). The detail result of each category is reported at Table 1. Fifty percent of patients still suffered from moderate to severe pain, 2 years after surgical intervention [Figure 1]. Cobb angle had no statistically significant correlation with body pain score (P > 0.05) as indicated at [Figure 2]. Low scores of BP (more disabilities) were found at some cases with minimal kyphosis.
Table 1.
Mean values of different aspects of SF-36 in comparison to Iran normative
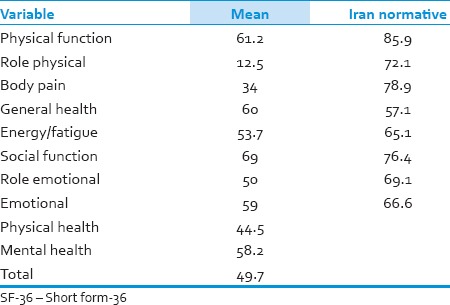
Figure 1.
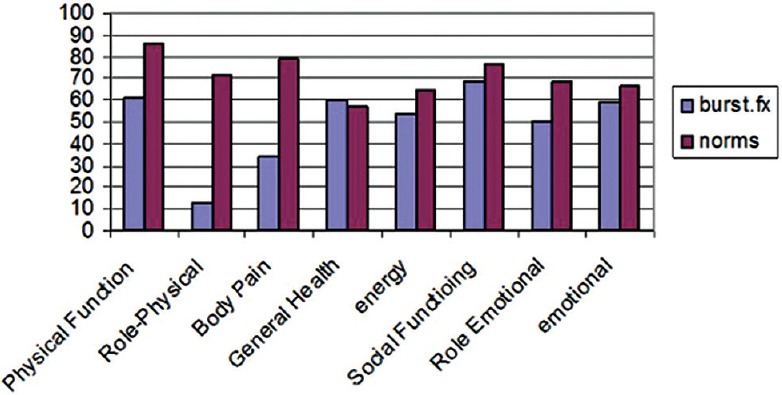
Comparison of short form-36 results between patients and normal persons
Figure 2.
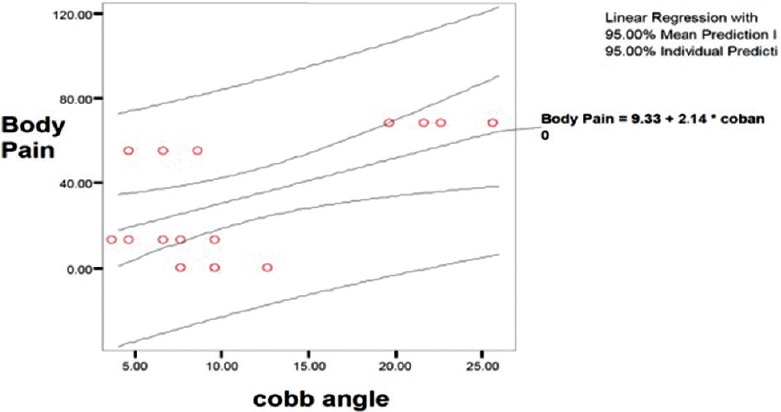
Correlation of body pain and Cobb angle
Discussion
Burst fractures constitute 30–60% of thoracolumbar fractures and about 50% or more have no neurologic deficit.[8,9,10] Burst fractures were first reported by Holdsworth and different classifications exist based on morphology, stability, and mechanism of injury since that time.[8] Thoracolumbar injury classification and severity score (TLICS) considers neurological status, morphology and integrity of PLC.[5] According to this classification, burst fracture with intact PLC and neurological status is categorized as one subgroup. In these cases, operative treatment is not necessary.[8,11,12,13]
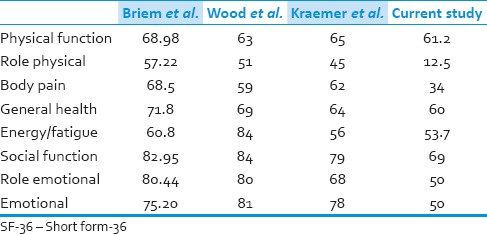
This is the first norm-based evaluation of HRQOL with long-term follow-up in Iran. The current study revealed significant decreased QOL and BP score, which did not correlate with the degree of progressive kyphosis, at stable burst fractures. This would be partly due to the nature of primary trauma insult. Other studies have reported similar values for SF-36 [Table 2]. Several reasons exist for poor grades of HRQOL and pain scale, including the injury to the motion segment, method of treatment (nonoperative versus operative), and surgical technique.[3,6,7,8]
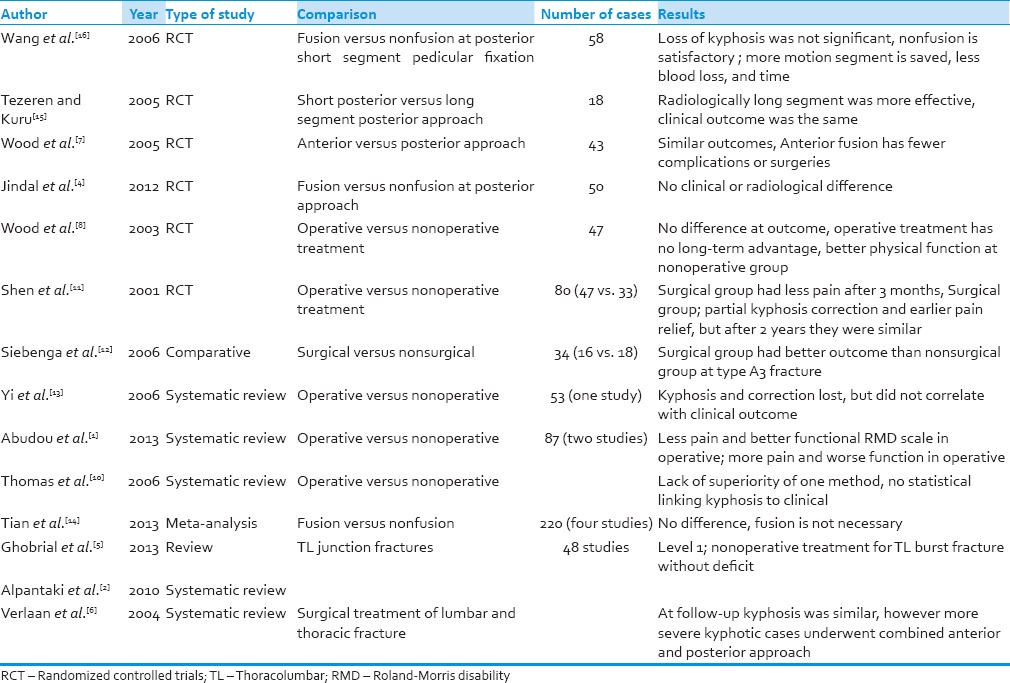
Table 2.
Values of SF-36 categories reported at other studies
Bone deformity is corrected with surgery. However, it is unclear if this correction is clinically important since patients with residual kyphosis improve neurologically[6,14,15,16] and some of the operated cases may be stable before surgery. Surgery causes earlier mobilization and discharge, less initial pain and faster return to work.[6,7,8] However, HRQOL is not superior in surgical treatment [Table 3]. According to the systematic review done by Thomas et al., there is no evidence for the superiority of surgical treatment; and kyphosis will progress at both surgical and conservative modalities.[10] Besides, the correlation of kyphosis and outcome is not clear.[6,8,10] Verlaan et al. concluded that the final degree of kyphosis was similar regardless of surgical approach.[6]
Table 3.
Results of comparative studies and systematic reviews of burst fractures at thoracolumbar junction
There is an increasing emphasis on self-reported measures of health status and HRQOL. Considering the patients’ point of view and the multidimensional nature of health, subjective measures of health status are included in epidemiological and community-based survey research. SF-36 is one of the most widely used subjective measures of health status.[3,7,8] It is a generic measure developed to meet psychometric standards for group comparisons, to enable profiling of functional health and well-being, and to quantify disease burden. The SF-36 includes 36 questions grouped into eight categories: Physical functioning, role limitations due to physical health (role physical), body pain, general health perceptions, energy/fatigue, social functioning, role limitations due to emotional problems (role emotional), and emotional. The higher scores indicate less disability. SF-36 estimates disease burden for more than 200 diseases and conditions including arthritis, back pain, spinal injuries, stroke, surgical procedures, trauma, cancer, cardiovascular disease, chronic obstructive pulmonary disease, depression, diabetes.[17] Norm-based comparison is a type of criterion-based interpretation, in which scores are evaluated in relation to typical scores (norms). This method could evaluate the patients at the same population of their origin.[17] Since the reliable Persian translation and norm-based scores of SF-36 for Iran population are available and their reliability and validity have been reported well in literature,[9] the aforementioned method was selected for analysis. However, the major limitation of our study is lack of control group as nonoperated cases.
Conclusions
Patients in this study showed a reduced QOL, esp. pain scale, without significant correlation with kyphosis. No evidence exists on linking kyphosis to clinical outcome. Other etiologies of poor pain scale such as weight, occupation, education, and treatment approach should be assessed as well. It seems that surgical treatment could not improve pain related disability of patients with stable thoracolumbar burst fracture at long term follow up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Abudou M, Chen X, Kong X, Wu T. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2013;6:CD005079. doi: 10.1002/14651858.CD005079.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Alpantaki K, Bano A, Pasku D, Mavrogenis AF, Papagelopoulos PJ, Sapkas GS, et al. Thoracolumbar burst fractures: A systematic review of management. Orthopedics. 2010;33:422–9. doi: 10.3928/01477447-20100429-24. [DOI] [PubMed] [Google Scholar]
- 3.Dai LY, Jiang SD, Wang XY, Jiang LS. A review of the management of thoracolumbar burst fractures. Surg Neurol. 2007;67:221–31. doi: 10.1016/j.surneu.2006.08.081. [DOI] [PubMed] [Google Scholar]
- 4.Jindal N, Sankhala SS, Bachhal V. The role of fusion in the management of burst fractures of the thoracolumbar spine treated by short segment pedicle screw fixation: A prospective randomised trial. J Bone Joint Surg Br. 2012;94:1101–6. doi: 10.1302/0301-620X.94B8.28311. [DOI] [PubMed] [Google Scholar]
- 5.Ghobrial GM, Maulucci CM, Maltenfort M, Dalyai RT, Vaccaro AR, Fehlings MG, et al. Operative and nonoperative adverse events in the management of traumatic fractures of the thoracolumbar spine: Asystematic review. Neurosurg Focus. 2014;37:E8. doi: 10.3171/2014.4.FOCUS1467. [DOI] [PubMed] [Google Scholar]
- 6.Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: A systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976) 2004;29:803–14. doi: 10.1097/01.brs.0000116990.31984.a9. [DOI] [PubMed] [Google Scholar]
- 7.Wood KB, Bohn D, Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures without neurologic deficit: A prospective, randomized study. J Spinal Disord Tech. 2005;18(Suppl):S15–23. doi: 10.1097/01.bsd.0000132287.65702.8a. [DOI] [PubMed] [Google Scholar]
- 8.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773–81. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Motamed N, Ayatollahi AR, Zare N, Sadeghi-Hassanabadi A. Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East Mediterr Health J. 2005;11:349–57. [PubMed] [Google Scholar]
- 10.Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: A systematic review. J Neurosurg Spine. 2006;4:351–8. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 11.Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976) 2001;26:1038–45. doi: 10.1097/00007632-200105010-00010. [DOI] [PubMed] [Google Scholar]
- 12.Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures: A multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006;31:2881–90. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 13.Yi L, Jingping B, Gele J, Baoleri X, Taixiang W. Operative versus non-operative treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2006;4:CD005079. doi: 10.1002/14651858.CD005079.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Tian NF, Wu YS, Zhang XL, Wu XL, Chi YL, Mao FM. Fusion versus nonfusion for surgically treated thoracolumbar burst fractures: A meta-analysis. PLoS One. 2013;8:e63995. doi: 10.1371/journal.pone.0063995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: Short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18:485–8. doi: 10.1097/01.bsd.0000149874.61397.38. [DOI] [PubMed] [Google Scholar]
- 16.Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?. A prospective, randomized study. Spine (Phila Pa 1976) 2006;31:2646–52. doi: 10.1097/01.brs.0000244555.28310.40. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36.item short.form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]


