Abstract
Background Surgery is increasingly recognized as an important driver for health systems strengthening, especially in developing countries. To facilitate quality improvement initiatives, baseline knowledge of capacity for surgical, anaesthetic, emergency and obstetric care is critical. In partnership with the Malawi Ministry of Health, we quantified government hospitals’ surgical capacity through workforce, infrastructure and health service delivery components.
Methods From November 2012 to January 2013, we surveyed district and mission hospital administrators and clinical staff onsite using a modified version of the Personnel, Infrastructure, Procedures, Equipment and Supplies (PIPES) tool from Surgeons OverSeas. We calculated percentage of facilities demonstrating adequacy of the assessed components, surgical case rates, operating theatre density and surgical workforce density.
Results Twenty-seven government hospitals were surveyed (90% of the district hospitals, all central hospitals). Of the surgical workforce surveyed (n = 370), 92.7% were non-surgeons and 77% were clinical officers (COs). Of the 109 anaesthesia providers, 95.4% were non-physician anaesthetists (anaesthesia COs or ACOs). Non-surgeons and ACOs were the only providers of surgical services and anaesthetic services in 85% and 88.9% of hospitals, respectively. No specialists served the district hospitals. All of the hospitals experienced periods without external electricity. Most did not always have a functioning generator (78.3% district, 25% central) or running water (82.6%, 50%). None of the district hospitals had an Intensive Care Unit (ICU). Cricothyroidotomy, bowel resection and cholecystectomy were not done in over two-thirds of hospitals. Every hospital provided general anaesthesia but some did not always have a functioning anaesthesia machine (52.2%, 50%). Surgical rate, operating theatre density and surgical workforce density per 100 000 population was 289.48–747.38 procedures, 0.98 and 5.41 and 3.68 surgical providers, respectively.
Conclusion COs form the backbone of Malawi’s surgical and anaesthetic workforce and should be supported with improvements in infrastructure as well as training and mentorship by specialist surgeons and anaesthetists.
Keywords: Anaesthesia, clinical officers, global health, global surgery, Malawi, surgical capacity, surgery, surgical care, surgical burden
KEY MESSAGES.
Understanding a country’s baseline surgical and anaesthetic capacity with appropriate metrics is critical to improving the quality of services and outcomes.
Non-physician surgical and anaesthetic clinical officers provide care at the majority of hospitals in Malawi. Ongoing support and mentorship and incremental skills training by specialist physicians should be a priority.
Surgical and anaesthetic infrastructure in Malawi requires improvements to provide safe, reliable surgical care across all hospitals.
Introduction
Surgery is an essential part of a health system and the recognition of critical service, workforce and infrastructure deficiencies in surgical care in low- and middle-income countries (LMICs) has gained global attention (Hsia et al. 2012; Hoyler et al. 2014). Conditions requiring surgical care account for an estimated 19.2% of the global burden of disease (Murray et al. 2012), yet 2 billion people still lack access to the most basic, essential surgical services (Funk et al. 2010). Surgery is simply not being done in certain areas. Weiser et al. (2008) demonstrated the paucity of surgical care in the poorest one third of the world (<$100 per capita) with only 3.5% of all recorded operations undertaken in those areas.
Contributing to this global crisis is the staunch lack of comprehensive data to begin the process of health systems strengthening (Dubowitz et al. 2010; Hoyler et al. 2014). In a recent systematic review of published literature on number of surgeons, obstetricians and anaesthetists in LMICs, only 6 of 42 countries described relevant countrywide statistics (Hoyler et al. 2014). To date, numbers of surgical providers or surgical infrastructure have not been recorded or published in national health sector reviews or official country reports to the World Health Organization (WHO) (WHO 2012). Data fields on basic and comprehensive surgical services, infrastructure and workforce have only recently been included in the WHO Service Availability and Readiness Assessment (SARA) questionnaire (WHO 2014a) and the Demographic and Health Surveys (DHS) and will take several years before information becomes available (DHS 2014).
The need for country-level information on surgical capacity with appropriate epidemiologic indicators is evident for appropriate health care planning and management. Although no consensus currently exists, it has been suggested that metrics such as surgeon density (surgeons per 100 000 people) (Hoyler et al. 2014), annual case rate (annual number of major operations per 100 hospital beds, the number per 1000 inpatient admissions, the number per 10 000 new outpatient consultations, or the annual number per 100 000 catchment area population) (Nordberg et al. 2002), number of operating theatres, and 30-day perioperative mortality rate (Weiser et al. 2009) could potentially be routine indicators of the quality of surgical care or the ability of the health system to provide adequate safe surgery. These metrics could provide the foundation of quality improvement initiatives in increasing surgical capacity, and hence, bring countries closer to meeting the burden of surgical disease, particularly in rural areas.
To address the gap in knowledge of a comprehensive, countrywide assessment of surgical care capacity in Malawi, utilize surgical metrics as potential quality improvement indicators, and provide a baseline understanding of critical workforce, infrastructure and service delivery challenges that must be overcome at the national level, we collaborated with the Malawi School of Anaesthesia, Ministry of Health (SoA MOH) to quantify government hospitals’ capacity to provide surgical care. The result of this study provides detailed insight into the surgical system of Malawi, can be utilized to supplement large databases such as the DHS and SARA survey, and can form the basis of a countrywide effort to expand access to essential surgical services.
Background
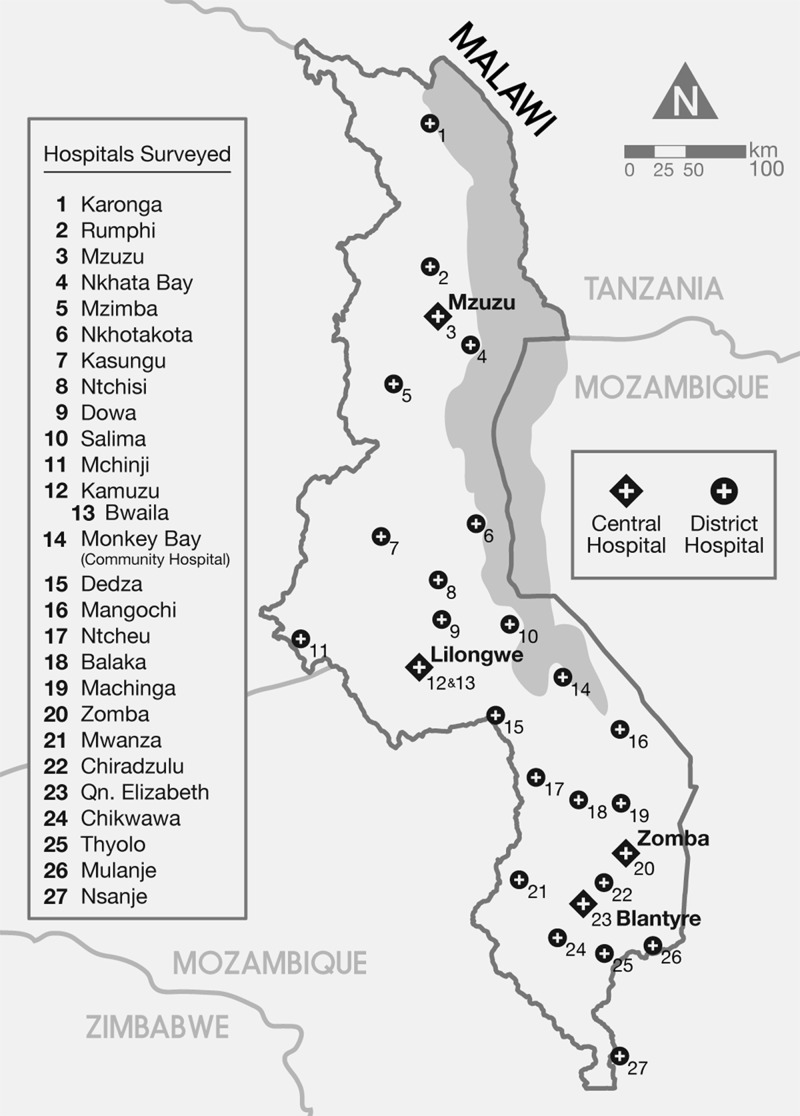
Malawi is a landlocked country that lies on the southeastern part of the African continent (Figure 1), spanning 118 484 km2 (population = 14 000 000) with Zambia to the west, Tanzania to the northeast and Mozambique forming its southwest, south and southeastern border. The eastern half of Malawi is taken up by Lake Malawi, which has a surface area of ∼29 600 km2. Classified as a ‘low-income country’ by the World Bank, the country’s Gross domestic product (GDP) per capita is US Dollar (USD) 900, which ranks 220 out of 229 countries. About 65% of the population lives on less than United States (US)$ 1 per day (Malawi NSO 2004).
Figure 1.
Map of Malawi showing distribution of government hospitals.
Malawi’s human development index (HDI) ranking of 170 out of 186 countries reflects the challenging health landscape in the country. Life expectancy (52.78 years), infant mortality (77 deaths per 1000 live births; global average 43/1000), and under five mortality rate (110 deaths per 1000 live births; global average 48/1000) are among some of the worst health rankings in the world. As of 2010, Malawi had the 22nd highest maternal mortality ratio (MMR) in the world with 460 deaths per 100 000 live births, much higher than the global average of 260 per 100 000 live births. As of 2008, there were 0.02 physicians per 1000 population (recommended: 2.3/1000) (CIA 2012).
Malawi is a Democratic Republic formally divided into three administrative regions (North, Central and South), further subdivided into 28 administrative districts (CIA 2012). Three main agencies provide formal health care services in the country: 60% from the Malawi Ministry of Health, 37% from the Christian Health Association of Malawi and the rest by the local government, private practitioners, commercial companies, the Army, and the Police (Phiri 2007). Health care is divided into primary, secondary and tertiary levels of care. Primary care is generally composed of 68 dispensaries, 328 health centres each with 5–10 beds and 16 maternity clinics. About 10–15 health centres feed into a district hospital, or mission hospital, which form the secondary level of care in Malawi. Not all districts have a government hospital and such gaps are met by faith-based mission hospitals. Each district or mission hospital has 100–200 beds and offer basic surgical services such as trauma management and obstetric emergencies. Four central hospitals, each with capacity of 600–1500 beds, form the tertiary level of care and offer more specialized medical and surgical treatment. The health care workforce in Malawi is extremely limited and insufficient to fully address the needs of the population, an issue we discuss below.
Overview of surgical training in Malawi
The first medical school in Malawi was built in 1991, graduating 20 doctors per year in the first 15 years. In 2003, an increase in student intake resulted in an increase in 2008 of ∼50 doctors per year. In 2005, the medical school introduced MMed postgraduate programmes in general surgery, ophthalmology, orthopaedics and anaesthesia with a tuition fee of USD 3000 per student per annum. Candidates must have completed 2 years of public service work post-internship before they can be eligible for government funding. They continue to enjoy full salaries and other benefits and are required to work for the government after training. As of 2013, three have completed surgical training (two in ophthalmology and one in general surgery) and seven are still in training. The College of Surgeons of East, Central and Southern Africa (COSECSA) has started fellowship programmes in general surgery, orthopaedics and paediatric surgery. Four surgeons have graduated (three in orthopaedics and one in general surgery), five have finished the membership programme and 12 candidates are currently in training. There are three accredited training facilities (Kakande et al. 2011).
Non-physician clinicians
General clinical officers
In 1975, to address the shortage of physicians, Malawi started a 3-year training programme for clinical officers (COs) who are awarded a Diploma in Clinical Medicine by the government-funded Malawi College of Health Sciences or the faith-based training institution Malamulo College of Health Sciences. The Medical Council of Malawi (MCM) and the MOH formally recognize both institutions. After graduating, general COs complete a 1-year internship at a district or central hospital supervised by senior COs or medical officers. They can be deployed up to central hospital level. The scope of their work is detailed in Table 1. To qualify for annual registration with the MCM, mandatory continuing professional development courses like other health workers is required. They can be promoted to more senior CO levels based on experience as a career pathway but cannot progress to more senior medical positions unless they complete a 5-year medical degree regardless of their level of experience or demonstrated expertise. COs can start their own practice after 10 years of public service but have to remain supervised by a licensed physician.
Table 1.
Clinical officer scope of work
| General surgical clinical officer | Orthopaedic clinical officer |
|---|---|
| Cyst and foreign body removal | Debridement of open fractures |
| Hernia repair | External fixation |
| Hydrocoelectomy | Management of acute pyogenic musculoskeletal infections |
| Laparotomy for acute abdominal emergencies | Manipulations of major joint dislocations |
| Caesarean section | Closed fractures |
| Ectopic pregnancy | Conservative treatment of degenerative musculoskeletal conditions |
| Tubal ligation | Management of club foot disorders |
| Dilatation and curettage | Management of developmental childhood conditions |
Specialized COs
Following the success of the generalist COs, upgrade courses for orthopaedics and anaesthesia were administered to medical assistants to become specialized COs. Orthopaedic COs have been trained and deployed to rural district hospitals since 1985 and have been managing 80–90% of the orthopaedic workload in Malawi (Table 1). Anaesthetic COs are the major providers of anaesthesia in the whole country. The Malawi School of Anaesthesia started training Anaesthetic COs in 1988. Ophthalmic COs manage acute eye emergencies and perform cataract surgery and evisceration of the globe.
General COs were deployed to district hospitals to cover the majority of the burden of surgical disease while surgeons from central hospitals periodically visited to run clinics and sometimes operate. Many patients suffering from traumatic, obstetric, abdominal and orthopaedic emergencies, however, were still referred to the overburdened central hospitals, which were located a few hours away (Jiskoot 2008). A study done in 2003 found that only 3% of major surgical procedures were performed by COs at district hospitals. On further inquiry, the COs were comfortable performing major obstetric surgeries since the procedures were fairly reliable but an acute abdomen posed challenges beyond the scope of the CO’s training and experience (Steinlechner et al. 2006). It is well established that delay in operating on abdominal emergencies increases mortality (Monod-Broca 1990). To address this problem, the College of Medicine introduced on-the-job training in surgical and gynaecologic procedures from January 2005 to December 2006 in 17 district and mission hospitals in the Southern region of Malawi. Surgeons were involved in training the COs and monitored their operative skill. A retrospective review comparing operative logs before and after the training programme showed a significant difference in CO major surgical activity (P < 0.005) (van Amelsfoort et al. 2010). A 5-year retrospective study of COs at Zomba Central Hospital from 2003 to 2007 showed that under supervision, they performed 51% of 2931 major general surgery procedures and independently performed 50% of prostatectomies, ventriculoperitoneal shunts and strangulated hernia repairs with bowel resection. Baseline parameters and perioperative outcomes of the patients who were operated by COs alone compared with a supervising surgeon assistant showed no significant difference (Wilhelm et al. 2011). An assessment of the orthopaedic CO training programme showed cost-effectiveness (Mkandawire et al. 2008).
Materials and Methods
Survey preparation, administration and data collection
We based our study on the Personnel, Infrastructure, Procedures, Equipment and Supplies (PIPES) survey adapted by Surgeons OverSeas from the WHO Situational Analysis Tool to Assess Emergency and Essential Surgical Care. We loaded the survey on an iPad using the QuickTap Survey application. PIPES seeks to assess surgical capacity of health facilities in five areas: workforce, infrastructure, skill, equipment and supplies and was previously administered in other countries (Henry et al. 2012). We obtained permission from the Malawi School of Anaesthesia, Ministry of Health (SoA MOH) prior to conducting site visits.
From November 2012 to January 2013, one investigator conducted site visits on all government hospitals (district and central) that had functional operating theatres and were accessible by land. Hospital administrators and onsite clinical staff were extensively interviewed. Onsite inspection and spot logbook queries were also conducted. The investigator subsequently visited and conducted surveys on nearby mission hospitals.
Population and surgical caseload
We gathered population data from the government of Malawi and calculated percentage population served by the district hospitals. Surgical caseload was obtained from a national survey of surgical activity in all district hospitals in 2003 (Steinlechner et al. 2006) and a prospective study in eight district hospitals in 2004 and 2005 (Phiri 2007). Surgical conditions were defined as ‘any condition that requires suture, incision, excision, manipulation or other invasive procedure that usually, but not always, requires local, regional or general anaesthesia’ (Debas et al. 2006). We excluded conditions that were not clearly defined, such as ‘other’, and minor obstetric procedures such as dilatation and curettage.
We calculated the surgical rate per 100 000 people based on the calculated population size and yearly volume of surgeries. When data on surgical caseload were only available for only a portion of the district hospitals in a given year, we calculated the surgical rate based on the total population served by the district hospitals and number of procedures noted. An average surgical rate was determined from the calculated rate.
Population and surgical workforce rates
We used the same population data and calculated percentage population served by all the government hospitals. Using original data presented in this article, we determined surgical workforce rates per 100 000 people and compared it with the recommended rate of surgeons per 100 000 people.
Data analysis
The surveyed hospitals were stratified according to whether they were government-run or mission-run and were analyzed separately. One hospital was excluded (Ngabu Rural) because the bed capacity was an outlier. One community hospital was included because it had a functional operating room that performed major surgeries. Three district hospitals were not visited because (a) Phalombe Hospital only performed minor operations, (b) Neno District Hospital did not have a functioning operating theatre at the time and (c) Chitipa Hospital was inaccessible during the study period because of road conditions.
The survey tool’s procedures section included a list of minor, major, orthopaedic, trauma and resuscitation, obstetric, paediatric and cancer surgeries. Descriptive statistics indicated frequencies and tables and graphs were drawn to illustrate the data.
Results
Of 38 hospitals surveyed, 27 (71%) were government hospitals (23 district and community, 4 central hospitals) and 11 (29%) were mission hospitals. The 27 government facilities represented 90% of the district hospitals and all of the central hospitals. Of the 27 hospitals, 5 (18.5%) were in the northern region, 8 (29.6%) in the central region and 14 (51.8%) in the southern region (Figure 1). The 27 government hospitals included in the analysis represented 74 operating theatres and 9,405 hospital beds. The average number of beds in the district and central hospitals was 250 and 913, respectively. The average operating theatre density per 100 000 people was 0.98 (Table 2).
Table 2.
Summary of government facilities surveyed
| District hospitals | Central hospitals | Total | |
|---|---|---|---|
| Number of facilities surveyed (%, per cent of total number) | 23 (90) | 4 (10) | 27 (100) |
| Total number of beds | 5753 | 3652 | 9405 |
| Range of beds | 120–360 | 352–1500 | 120–1500 |
| Average number of beds (95% Confidence Interval, CI) | 250 (221.78–278.48) | 913 (94.56–1431.44) | |
| Number of functional operating theatres | 46 | 28 | 74 |
| Average number of functional operating theatres (95% CI) | 2 (1.83–2.17) | 7 (3.8–10.2) | |
| Functional operating theatres per 100 000 people | 0.86 | 0.37 | 0.98 |
| Average functioning pulse oximeter per operating theatre | 0.855 (0.73–0.98) | 1.045 (0.19–1.91) |
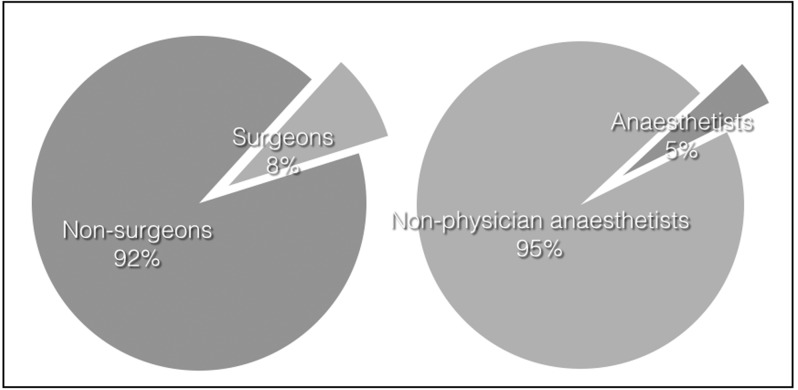
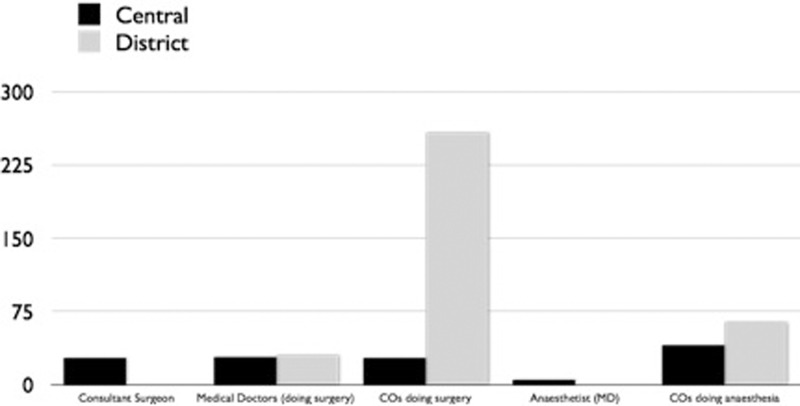
Workforce
Figure 2 illustrates the national distribution of specialist and non-specialist surgical and anaesthetic providers. Among the 27 facilities, there were 479 surgical and anaesthetic personnel. 370 people performed surgery, of whom 343 (92.7%) were non-surgeons and 285 (77%) were COs. Of the 109 anaesthesia providers, 104 (95.4%) were non-physician anaesthetists (anaesthetic COs or ACOs) (Figure 2). Non-surgeons were the only provider of surgical services at 23 (85%) of the hospitals and ACOs were the only provider of anaesthetic services at 24 (88.9%) of the hospitals. No certified surgeons were based at the district hospitals and the five anaesthetists in the country were concentrated in three of the four central hospitals (Table 2). Figure 3 shows the distribution of surgical and anaesthetic personnel across central and district hospitals. The average number of surgical providers per 100 000 in the district and central hospitals was 5.41 and 3.68, respectively.
Table 3.
Average surgeon, anaesthetist, non-physician clinician and biomedical technician distribution
| District hospitals (n = 23) Population catchment area: 5 319 315.6 |
Central hospitals (n = 4) Population catchment area: 2 225 512.2 |
Total population catchment area: 7 544 827.8 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Workforce | Total | Average | 95% CI | Density (per 100 000 people) | Total | Average | 95% CI | Density (per 100 000 people) | Total | Density (per 100 000 people) |
| General surgeon | 0 | 0 | 0 | 0 | 27 | 6.75 | (0.64–12.86) | 1.21 | 27 | 0.36 |
| Anaesthetist | 0 | 0 | 0 | 0 | 5 | 1.25 | (0.02–2.48) | 0.22 | 5 | 0.07 |
| Medical doctors (performing surgery) | 30 | 1.30 | (0.95–1.66) | 0.56 | 28 | 7 | (2.84–11.16) | 1.26 | 58 | 0.76 |
| COs performing surgery | 258 | 11.22 | (9.07–13.36) | 4.85 | 27 | 6.75 | (4.73–8.77) | 1.21 | 285 | 3.78 |
| COs providing anaesthesiaa | 64 | 2.78 | (2.39–3.17) | 1.20 | 40 | 10 | (6.5–13.49) | 1.80 | 104 | 1.38 |
| Biomedical technicians | 0 | 0 | 0 | 0 | 9 | 2.25 | (0.58–3.92) | 0.40 | 9 | 0.12 |
| Total | 352 | 136 | 488 | |||||||
aReferred to as Anaesthesia Clinical Officers (ACOs) in the text.
Figure 2.
Workforce distribution.
Figure 3.
Personnel distribution across central and district hospitals. Numbers in absolute figures. CO—clinical officers.
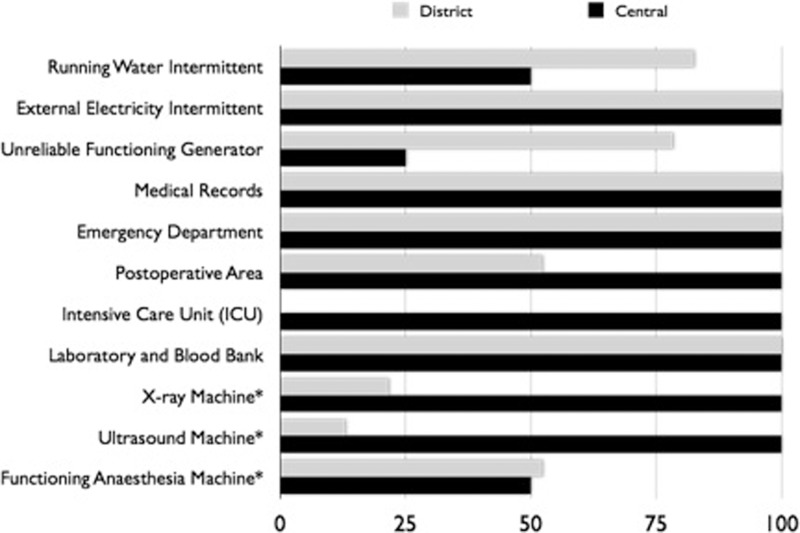
Infrastructure
Figure 4 shows the availability, distribution, and state of basic infrastructure elements critical to a well-functioning surgical service. All of the government hospitals surveyed experienced periods without external electricity. Majority of district hospitals did not always have access to a functioning generator (74% district, 25% central) or running water (70%, 50%). None of the district hospitals surveyed had an intensive care unit and only 12 (52.2%, 100%) had a post-operative/recovery area. All hospitals had an emergency department and medical record system. Availability of ancillary services varied but was largely present. All facilities surveyed had a laboratory and a blood bank. Radiological services were commonly available such as a functioning X-ray machine (81%) and ultrasound machine (89%). Nevertheless, only 14 (52.2%, 50%) could always rely on a functioning anaesthesia machine (Figure 4).
Figure 4.
Infrastructure distribution. Numbers in percentages. *denotes always being available.
Surgical procedures and case rate
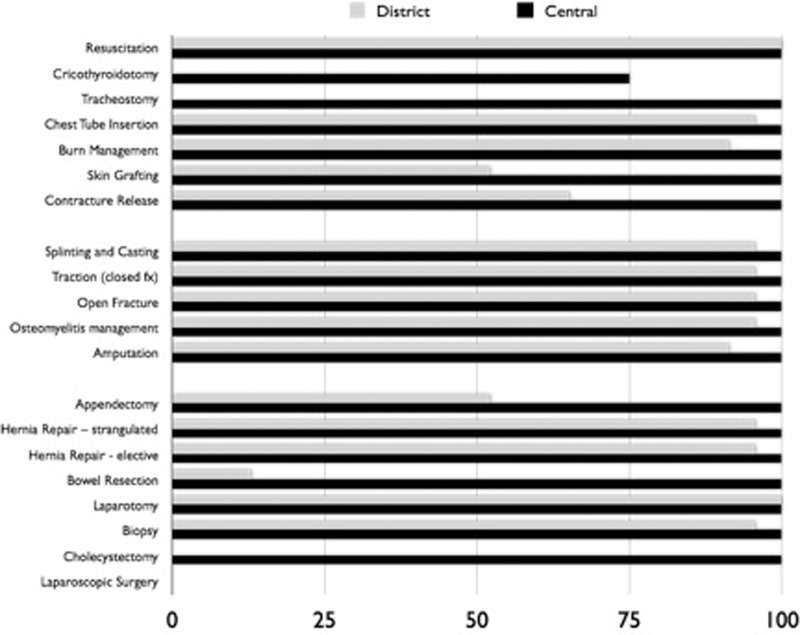
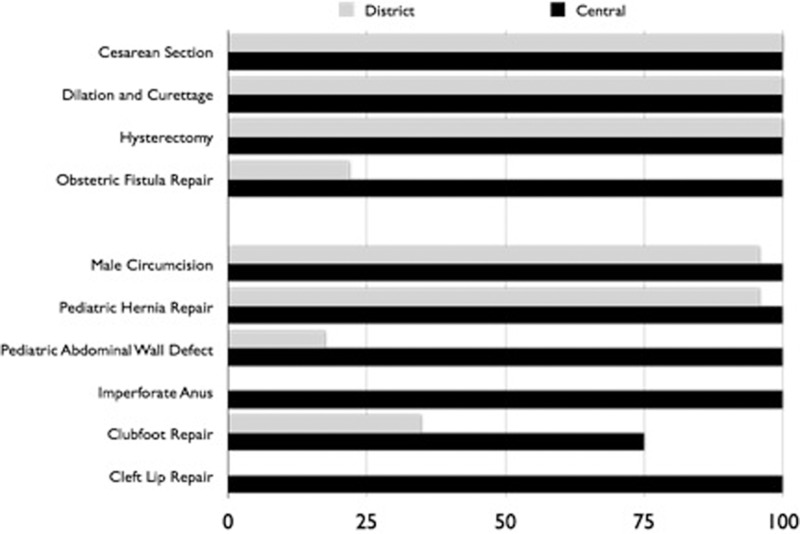
Figure 5 details the availability and distribution of select essential surgical procedures. Every facility surveyed was able to perform minor surgical procedures such as suturing, wound debridement and incision and drainage. Every facility also reported the ability to perform basic trauma resuscitation. No district hospital could perform advanced airway management procedures such as a cricothyroidotomy or tracheostomy. The vast majority (96%) were able to insert a chest tube. Likewise, almost all facilities (93%) were able to manage burns. Nevertheless, only 59% could perform skin grafts and just 19 (65.2%, 100%) performed post-burn contracture release. The majority of facilities (96%) reported being able to perform basic fracture management: splinting, casting, traction, treatment for open fractures and management of osteomyelitis. All of the facilities could perform laparotomy while none of the facilities had the capacity for laparoscopic surgery. No district hospital could perform a cholecystectomy. All of the facilities were able to perform Caesarean section, dilation and curettage, tubal ligation, and hysterectomies. Only 9 hospitals (21.7%, 100%) were able to repair obstetric fistulas. Among paediatric procedures, the most commonly performed were hydroceles (96%), hernia repair (93%) and male circumcision (96%). Over a third (41%) of all facilities could treat clubfoot, but only 15% could treat cleft lip or imperforate anus. Every facility surveyed reported the ability to provide regional, spinal, ketamine and general anaesthesia. All of hospitals were forced to deliver non-inhalational anaesthesia (locally called total intravenous anaesthesia) at times. Surgical rates ranged from 289.48 to 747.38 procedures per 100 000 people (Table 4).
Figure 5.
Percentage of facilities performing select procedures assessed (general).
Table 4.
Surgical caseload in Malawi
| Year | Number of surgeries | Total population served | Procedures/100 000 people |
|---|---|---|---|
| 2003 | 17 260 | 5 962 318.8 | 289.48 |
| 2004 | 8025 | 2 045 364 | 653.92 |
| 2005 | 9172 | 2 045 364 | 747.38 |
Equipment and supplies
Compressed cylinder oxygen was not reliably available at 17 (65.2%, 50%) of facilities, though 20 (74%, 75%) reported access to functioning oxygen concentrators. Fifty-two per cent of all facilities always could not rely on a functioning anaesthesia machine and nearly two-thirds could not rely on a functioning patient monitor (70%) or pulse oximeter (67%). None of the government hospitals had any laparoscopic equipment. Adequacy of supplies varied greatly among these facilities: 67% of the facilities had eye protection, 85% always had facemasks but only 20% had chest tubes reliably in stock.
Figure 6.
Percentage of facilities performing select procedures assessed (obstetric and paediatric).
Discussion
Our results showed important deficiencies in five major areas: workforce, infrastructure, supplies, equipment, and service delivery. These categories are vital to a well-functioning health system. Our results did not differ from previous surgical capacity studies conducted in the region (Galukande et al. 2010; Iddriss et al. 2011; Petroze et al. 2012) although this study is one of two nationally representative surveys of government hospitals in which data for every district and referral hospital is available (Petroze et al. 2012).
There are measurable inadequacies and disparities in the number and distribution of surgical care specialists in the country. The average general surgeon density is 1.21 per 100 000 people compared with the recommended 4.7 per 100 000 people in the US (ACS 2010). The average anaesthesia workforce density is even more dire with 0.22 per 100 000 people. All specialists are found in urban areas. More than 93% of the surgical and anaesthetic workforce in the country are non-physicians (e.g. COs and ACOs) with variable levels of training and only serve the districts.
Critical deficiencies in basic infrastructure required to provide surgical services, well documented in previous studies, were also noted. More than 75% of district hospitals surveyed had unreliable running water, electricity or a functioning back-up generator. The availability of functioning essential equipment and supplies relies on a planning and procurement process inherent in a functioning health care system (Hsia et al. 2012). Pulse oximeters and anaesthesia machines were not always functional or available in more than half of facilities. A previous study estimated that about 58.4–70.4% of operating theatres in Sub-Saharan Africa (SSA) lacked a pulse oximeter (Funk et al. 2010). These results indicate that the safety of the patients while surgery is being conducted may be compromised by lack of available essential equipment. However, ACOs, while being technically skilled, often lack a thorough understanding of the relevant pathophysiology needed to anticipate or troubleshoot difficulties.(WHO 2014b) The WHO Patient Safety Pulse Oximetry project aims to improve the safety of operating theatres worldwide by providing a high standard low-cost pulse oximeter and a training toolkit. The programme also supports legislation to increase the training of medical officers in anaesthesia (WHO 2014c).
Our calculated hospital operating theatre density (0.98 per 100 000 people) was 84% less than the global average of 6.2 per 100 000 people. This number is comparable with the SSA average of 1.0–1.2 per 100 000 people and may explain the high unmet need for surgery (Funk et al. 2010) and low surgical output in the region. Major surgery rates in East Africa in the early 1990s was from 70 to 500 per 100 000 population compared with 5000–9000 in highly industrialized nations (Nordberg et al. 2002). Malawi’s annual surgical rate (289.48–747.38 procedures per 100 000 people) is disproportionately low compared with high-income settings (11 110 procedures per 100 000 people; Weiser et al. 2008). Moreover, essential life-saving and disability-preventing interventions in the district hospitals were lacking. No district hospital could perform cricothyroidotomy or tracheostomy while slightly more than half could provide skin grafting, contracture release and appendectomy. Bowel resection, important for major abdominal trauma cases, obstruction or cancer, was only done in slightly more than 10% of district hospitals. These procedures, if available at point of care, can avert potentially disastrous complications and premature mortality and significantly decrease morbidity. Exorbitant transportation costs will be avoided since average transport times from rural to urban areas is 4–8 h (Husum et al. 2003).
The Malawi MOH began training COs and general practitioners in the late 1980s to provide surgical care as a strategy to combat the severely depleted surgical workforce. Retention of doctors who were sponsored and trained in developed countries was a significant challenge. Physician-level Specialization is concentrated in the central hospitals, where the majority of intensive care units are located. The range and scope of expertise varies greatly among non-physician clinicians and is a limitation on their comparability. The result of this article has shown that other sources of human capital (apart from surgical and anaesthetic physicians) who are already present and in the current medical workforce can provide surgical and anaesthetic care. In addition, previous studies have shown that this cadre, with appropriate training, had comparable surgical outcomes (Jiskoot 2008; Mkandawire et al. 2008). An evaluation of the impact of a CO training programme in district hospitals (before–after prospective study, n = 22) showed that the majority of the procedures was performed by COs (90% of 10 934–12 171 surgical procedures) with a 31% decrease in referral rates, 96.5% increase in laparotomy rates, significant improvement in antibiotic use and decrease in hernia infection rates and length of hospital stay after the training programme (Phiri 2007). Until countries with severely depleted health workforce can build up a critical mass of surgical and anaesthetic specialists to adequately take care of the basic surgical needs of their population, COs can be a viable option to fill the labour gap. We recommend investment in further training of the surgical and anaesthetic COs located at the district hospital in essential surgical procedures. These COs should build competence and confidence in performing emergency resuscitation and abdominal surgeries, obviating the need to refer patients to the central hospitals. Furthermore, surgeons and anaesthesiologists from the central hospitals should be invested in the training of COs with continued supervision.
Advances in maternal and child health have hinged on the ability to learn from and document programmatic success with the aid of specific benchmarks such as infant and maternal mortality rates. Improvements in surgical care cannot be achieved without a focus on specific quality indicators whether it be on structural, process or outcome measures. The WHO and its Patient Safety Programme have proposed six surgical metrics designed specifically to capture facility-level data on structural (number of operating rooms, number of accredited surgeons, number of accredited anaesthesia professionals), process (volume of surgery) and outcome (post-operative death ratios) (Weiser et al. 2009; Table 5). Based on the findings of this study, these metrics, calibrated to the population catchment area (per 100 000 people) since the uneven geographic distribution of workforce and infrastructure will not provide an accurate representation of the country, can be proposed as benchmarks for improving surgical care capacity globally. Moreover, accredited non-physician clinicians (e.g. COs and ACOs) providing perioperative care should be accounted for since this cadre is responsible for majority of the surgical workload especially in countries with the greatest need. Table 5 lists proposed surgical metrics in the literature with corresponding definitions and limitations. Results from this study along with defined benchmarks could contribute to the WHO SARA survey as well as the DHS survey to provide countrywide information and thus aid the completion of a global database of surgical capacity.
Table 5.
Proposed global surgical care metrics
| Category | Description | Metric | Rationaleb | Comments/limitations |
|---|---|---|---|---|
| Surgical workforce | The number of trained surgical provider with the capacity to provide surgical care servicesa | Surgical provider per 100 000 peoplea | Availability and composition of the health workforce is an important indicator of the strength of the health system | Definition of ‘surgical provider’ varies with each country, has to take into account different levels of surgical expertise as well as presence of distinct health cadre providing surgical services |
| Accredited surgeons are physicians who have achieved certification in a surgical specialty as recognized by the accepted national standards of the member state or national professional organizationsb | Absolute number of accredited surgeonsb | |||
| Anaesthetic workforce | The number of trained health providers with the capacity to provide anaesthesia care services | Anaesthesia provider per 100 000 people | Availability and composition of the health workforce is an important indicator of the strength of the health system | Definition of ‘anaesthesia provider’ varies with each country, has to take into account different levels of anaesthetic expertise |
| Accredited surgeons are physicians who have achieved certification in a surgical specialty as recognized by the accepted national standards of the member state or national professional organizationsb | Absolute number of accredited anaesthesiologistsb | |||
| Operating theatre | The number of functional operating theatres available to a catchment population. | Operating theatre per 100 000 people | Structural indicator of the ability to provide surgical interventions | Needs a standard recommended number. Global average: 6.2 per 100 000 people |
| The absolute number of operating theatres used specifically for surgical procedures and equipped to deliver anaesthesiab | Absolute number of operating theatresb | |||
| Surgical output | The average annual major surgery output in a defined population catchment areac | Major surgery output per 100 000 catchment population areac | Indication of the access to and use of health care, particularly surgical services | Needs a defined basic package of surgical care enumerating major surgical procedures being measured |
| The absolute number of all surgical procedures, defined as the incision, excision, or manipulation of tissue that requires regional or general anaesthesia, or profound sedation to control pain, undertaken in an operating roomb | Number of surgical procedures done in an operating room per yearb | |||
| Day-of-surgery death ratio | Number of deaths on the day of surgery, irrespective of cause, divided by the number of surgical procedures in a given year or periodb | Deaths on day of surgery/total annual surgical procedures (%)b | Allow the health system to assess its performance and the state of health of the population | Challenging to collect the information due to poor record keeping |
| Postoperative in-hospital death ratio | Number of deaths in the hospital following surgery, irrespective of cause and limited to 30 days, divided by the number of surgical procedures done in a given year or periodb | A 30-day in-hospital deaths/total annual surgical procedures (%)b | Provides insight into the risks associated with surgical intervention | Challenging to collect the information due to poor record keeping |
Adapted from: aHoyler et al. 2014; bWeiser et al. 2009; cNordberg et al. 2002.
Several limitations of this study deserve mention. The PIPES tool is simple and provides a brief snapshot of the capacity of hospitals to provide surgical care. The survey does not provide insight on other components of service delivery including quality, accessibility, co-ordination of stakeholders, supply chain practices and hospital planning and efficiency. Nevertheless, data on availability of workforce, essential surgical interventions, infrastructure, equipment and supplies is important for MOHs and stakeholders to plan efforts to increase capacity in those critical areas. The survey also does not cover other aspects of health system evaluation such as infection control, waste management, communications, emergency transport, medicine availability and supervision. Another limitation was obtaining clear information from facilities due to the phrasing of the questions in the survey. For the categories infrastructure, equipment and supplies the questions were posed as ‘which of the following are NOT always available?’ which means that we could not distinguish between those that are never available or are only sometimes available. Furthermore, certain items (e.g. generator, anaesthesia machine) may always be available but not always functioning. To address this, where possible we specified ‘functioning’ before the item assessed. For the category of procedures, the questions were posed as ‘which of the following procedures ARE performed at this facility?’ While these answers were cross-checked with logbooks, this phrasing shows a clear binary answer when, in reality, some procedures may be performed but only rarely. Another limitation is a lack of a population-based study on the need for surgery, which could help guide the planning of service availability in specific regions. We used existing information from an audit of procedures done at different hospitals in different points in time (2003–2005) to calculate the average surgical caseload, which limits its comparability. To offset this, we calculated surgical rates according to the population catchment area served by the district hospital where the study was done assuming the data was well-captured. Post-operative mortality rates in Malawi were not available in the literature and thus limits our ability to compare Malawi’s surgical safety profile with the pilot study on surgical metrics conducted by the WHO (Weiser et al. 2009). This data is important to further inform the MOH of the urgency of increasing funds for essential equipment and training of surgical providers.
Overall, the study uncovered significant deficiencies in workforce, infrastructure and service delivery in order to provide safe, adequate surgical care for the population. It is hoped that these barriers can be overcome through systematic collection of relevant data with appropriate metrics to begin quality improvement initiatives. Incorporating the result of this study in national and international databases is critical to raise awareness and subsequent funding for this often overlooked and neglected aspect of the health system.
Conclusion
Growing awareness on the large burden of surgical disease, unmet need, disparities in access to surgical care, and critical gaps in workforce, basic infrastructure and service delivery need a push to systematize collection of relevant surgical metrics and appropriate indicators to begin large-scale quality improvement initiatives. Until global data on surgical surveillance is available, unco-ordinated efforts with unclear impact will continue.
This study represents the first survey that encompasses all government hospitals, including both district and central hospitals, that had some form of surgical capacity in Malawi. The results of the study have enabled us to make recommendations to the Malawi MOH and to highlight areas of severe deficiency. We recommend further attention to training and professionalizing non-physician clinicians and their scope of work and increased involvement of surgeons and anaesthesiologists in training and working with this cadre as a way to extend their expertise. Moreover, documenting a defined set of surgical metrics is critical to providing a baseline by which improvements in the health system and subsequently in health outcomes for surgery can be made.
Funding
This work was supported by the Malawi School of Anaesthesia, Ministry of Health and Gradian Health Systems.
Conflict of interest statement. None declared.
References
- American College of Surgeons (ACS) 2010. Health Policy Research Institute. The Supply of Surgeons in the United States: Mapping the 50 States. http://mcacs.org/files/2010/Massachusetts-Surgeon-Map.pdf, accessed 23 April 2014. [Google Scholar]
- Central Intelligence Agency (CIA) The World Factbook. 2013–14. https://www.cia.gov/library/publications/the-world-factbook/index.html, accessed 19 June 2013. [Google Scholar]
- Debas HT, et al. Surgery. In: Jamison DT, et al., editors. Disease Control Priorities in Developing Countries. 2nd. New York: Oxford University Press; 2006. pp. 1245–60. [Google Scholar]
- The Demographic and Health Surveys (DHS) 2014. http://www.dhsprogram.com/pubs/pdf/SPAQ5/Service_Readiness_Indicators_042012.pdf, accessed 23 April 2014. [Google Scholar]
- Dubowitz G, Detlefs S, McQueen KA. Global anaesthesia workforce crisis: a preliminary survey revealing shortages contributing to undesirable outcomes and unsafe practices. World Journal of Surgery. 2010;34:438–44. doi: 10.1007/s00268-009-0229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk LM, Weiser TG, Berry WR, Lipsitz SR, Merry AF, Enright AC, et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet. 2010 Sep 25 doi: 10.1016/S0140-6736(10)60392-3. 376(9746):1055–61. PubMed PMID: 20598365. [DOI] [PubMed] [Google Scholar]
- Galukande M, von Schreeb J, Wladis A, et al. Essential surgery at the district hospital: a retrospective descriptive analysis in three African countries. PLoS medicine. 2010;7:e1000243. doi: 10.1371/journal.pmed.1000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JA, Windapo O, Kushner AL, Groen RS, Nwomeh BC. A survey of surgical capacity in rural southern Nigeria: opportunities for change. World Journal of Surgery. 2012;36:2811–8. doi: 10.1007/s00268-012-1764-0. [DOI] [PubMed] [Google Scholar]
- Hoyler M, Finlayson SR, McClain CD, Meara JG, Hagander L. Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anaesthesia workforce literature. World Journal of Surgery. 2014;38:269–80. doi: 10.1007/s00268-013-2324-y. [DOI] [PubMed] [Google Scholar]
- Hsia RY, Mbembati NA, Macfarlane S, Kruk ME. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy and Planning. 2012;27:234–44. doi: 10.1093/heapol/czr023. [DOI] [PubMed] [Google Scholar]
- Husum H, Gilbert M, Wisborg T, Van Heng Y, Murad M. Rural prehospital trauma systems improve trauma outcome in low-income countries: a prospective study from North Iraq and Cambodia. The Journal of Trauma. 2003;54:1188–96. doi: 10.1097/01.TA.0000073609.12530.19. [DOI] [PubMed] [Google Scholar]
- Iddriss A, Shivute N, Bickler S, et al. Emergency, anaesthetic and essential surgical capacity in the Gambia. Bulletin of the World Health Organization. 2011;89:565–72. doi: 10.2471/BLT.11.086892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiskoot P. On-the-job training of clinical officers in Malawi. Malawi Medical Journal. 2008;20:74–7. doi: 10.4314/mmj.v20i3.10969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakande I, Mkandawire N, Thompson M. A review of surgical capacity and surgical education programmes in The COSECSA Region. East and Central African Journal of Surgery. 2011;16:6–34. [Google Scholar]
- Mkandawire N, Ngulube C, Lavy C. Orthopaedic clinical officer program in Malawi: a model for providing orthopaedic care. Clinical Orthopaedics and Related Research. 2008;466:2385–91. doi: 10.1007/s11999-008-0366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monod-Broca P. Mortality in emergency abdominal surgery. 304 cases. A plea for better clinical practice. Annals of Gastroenterology and Hepatology. 1990;26:184–6. [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Nordberg E, Mwobobia I, Muniu E. Major and minor surgery output at district level in Kenya: review and issues in need of further research. African journal of health sciences. 2002;9:17–25. doi: 10.4314/ajhs.v9i1.30752. [DOI] [PubMed] [Google Scholar]
- National Statistics Office of Malawi (NSO) 2004. Demographic and Health survey. http://www.nsomalawi.mw/index.php/publications/malawi-demographic-and-health-survey/2004-malawi-demographic-and-health-survey.html, accessed 19 June 2013. [Google Scholar]
- Petroze RT, Nzayisenga A, Rusanganwa V, Ntakiyiruta G, Calland JF. Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. The British Journal of Surgery. 2012;99:436–43. doi: 10.1002/bjs.7816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phiri NA. Malawi: University of Malawi College of Medicine; 2007. Does training in surgical skills of Clinical Officers in the Southern Region of Malawi reduce the number of surgical referrals from district government and CHAM hospitals to central hospitals? MPH. [Google Scholar]
- Steinlechner C, Tindall A, Lavy C, Mkandawire N, Chimangeni S. A national survey of surgical activity in hospitals in Malawi. Tropical Doctor. 2006;36:158–60. doi: 10.1258/004947506777978208. [DOI] [PubMed] [Google Scholar]
- van Amelsfoort JJ, van Leeuwen PA, Jiskoot P, Ratsma YE. Surgery in Malawi–the training of clinical officers. Tropical Doctor. 2010;40:74–6. doi: 10.1258/td.2009.090068. [DOI] [PubMed] [Google Scholar]
- Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. The Lancet. 2008;372:139–44. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- Weiser TG, Makary MA, Haynes AB, et al. Standardised metrics for global surgical surveillance. Lancet. 2009;374:1113–7. doi: 10.1016/S0140-6736(09)61161-2. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Rio de Janeiro: World Health Organization; 2009. Global Forum on Trauma Care: Meeting Report. http://www.who.int/violence_injury_prevention/services/traumacare/global_forum_meeting_report.pdf, accessed 10 July 2013. [Google Scholar]
- World Health Organization (WHO) 2012. Global Health Observatory data repository 2012. http://apps.who.int/gho/data/node.main.A1443?lang=en, accessed 12 April 2014. [Google Scholar]
- World Health Organization (WHO) 2014a. 2013 Service Availability and Readiness Assessment (SARA): an annual monitoring system for service delivery: Reference Manual Geneva, Switzerland: World Health Organization. http://www.who.int/healthinfo/systems/sara_reference_manual/en/, accessed 12 April 2014. [Google Scholar]
- World Health Organization (WHO) 2014b. Challenges to achieving universal pulse oximetry: World Health Organization. http://www.who.int/patientsafety/safesurgery/pulse_oximetry/challenges_to_achieving_universal_pulse_oximetry.pdf, accessed 27 April 2014. [Google Scholar]
- World Health Organization (WHO) 2014c. WHO Patient Safety Pulse Oximetry Project 2014. http://www.who.int/patientsafety/safesurgery/pulse_oximetry/en/, accessed 27 April 2014. [Google Scholar]
- Wilhelm TJ, Thawe IK, Mwatibu B, Mothes H, Post S. Efficacy of major general surgery performed by non-physician clinicians at a central hospital in Malawi. Tropical Doctor. 2011;41:71–5. doi: 10.1258/td.2010.100272. [DOI] [PubMed] [Google Scholar]