Abstract
Background: A key aspect of any intervention to improve obesity is to better understand the environment in which decisions are being made related to health behaviors, including the food environment.
Methods: Our aim was to examine the extent to which proximity to six types of food establishments is associated with BMI z-score and explore potential effect modification of this relationship. We used geographical information software to determine proximity from 49,770 pediatric patients' residences to six types of food establishments. BMI z-score obtained from the electronic health record was the primary outcome.
Results: In multivariable analyses, living in closest proximity to large (β, −0.09 units; 95% confidence interval [CI], −0.13, −0.05) and small supermarkets (−0.08 units; 95% CI, −0.11, −0.04) was associated with lower BMI z-score; living in closest proximity to fast food (0.09 units; 95% CI, 0.03, 0.15) and full-service restaurants (0.07 units; 95% CI, 0.01, 0.14) was associated with a higher BMI z-score versus those living farthest away. Neighborhood median income was an effect modifier of the relationships of convenience stores and full-service restaurants with BMI z-score. In both cases, closest proximity to these establishments had more of an adverse effect on BMI z-score in lower-income neighborhoods.
Conclusions: Living closer to supermarkets and farther from fast food and full-service restaurants was associated with lower BMI z-score. Neighborhood median income was an effect modifier; convenience stores and full-service restaurants had a stronger adverse effect on BMI z-score in lower-income neighborhoods.
Introduction
Although several individual-level behavior change interventions have been tested to prevent and manage obesity, federal and international organizations, such as the World Health Organization, suggest that among the most promising approaches for childhood obesity prevention are sustainable, multisector strategies that support change at both individual and neighborhood levels.1
A key aspect of any intervention to improve obesity is to better understand the socioecological context in which decisions are being made related to health behaviors, including within neighborhoods. There is evidence that the obesity epidemic has been driven by an increase in availability of processed, affordable, and highly marketed food, leading to overconsumption.2 Previous studies have examined the association of weight status in children and proximity to food establishments. A few of these studies have shown a protective effect of “healthy” food establishments, such as supermarkets,3,4 and adverse effects of “unhealthy” food establishments, such as fast food and convenience stores.5,6 Others have found no association.7,8 Characterizing adverse and protective effects of varying food establishments on weight status can assist policy makers in creating more convenient and healthier options for communities.
Although informative, previous studies examining associations between food establishments and child weight status have often lacked information about multiple types of food establishments, objective weight and height measures, and have had not had diverse and large sample sizes allowing for the ability to examine sources of effect modification. As such, the aim of this study was to examine the associations of proximity to six types of food establishments (large supermarkets [supermarkets with ≥50 employees], small supermarkets [food stores with <50 employees], fast food restaurants, full-service restaurants, convenience stores, and bakeries, coffee shops, and candy stores) with BMI z-score and examine weight status category, neighborhood median income, and age as potential effect modifiers. We hypothesized that pediatric patients living closer to large and small supermarkets would have a lower BMI z-score, compared to those living farthest away, and that those pediatric patients living closest to fast food and full-service restaurants would have a higher BMI z-score.
Methods
Study Design and Participants
From 14 pediatrics practices in a large multisite, multispecialty physician group practice in eastern Massachusetts, we extracted electronic health record (EHR) data on height, weight, age, sex, race/ethnicity, date and location of well-child visits, and most recent residential address for 49,770 pediatric patients ages 4–18 years observed for well-child care with a height and weight measurement between August 2011 and August 2012. We excluded patients with (1) a residential address outside of Massachusetts, (2) any history of medical diagnoses affecting growth and nutrition (i.e., pregnancy, leukemia, and inflammatory bowel disease), and (3) any outlier BMI z-score values (less than −6 and greater than 6) based on US 2000 reference data.9 This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and our institutional review board approved all procedures involving human subjects/patients. A waiver of informed consent was obtained for this study given the use of existing EHR data.
Main Exposures
Our main exposures were proximity of the family's residential address to the following neighborhood food establishments, as defined by the North American Industry Classification System: (1) large supermarkets (supermarkets with ≥50 employees); (2) small supermarkets (food stores with <50 employees); (3) fast food restaurants; (4) full-service restaurants; (5) convenience stores (not including gas stations); and (6) bakeries, coffee shops, and candy stores. We used geographical information systems (GIS) software to map addresses of food establishments and the most recent residential address for each subject. We collected food establishment information from the InfoUSA database (2009) and categorized food establishments into the six categories as listed above.
Using the ArcGIS (version 10) Network Analyst Extension Closest Facility tool and StreetMap USA detailed streets (ESRI, Redlands CA), we calculated distances along the street network from each pediatric patient's residence to the closest food establishment of each type. We categorized closest proximity to each of the six food establishment types as: ≤0.5 mile; >0.5–1.0 mile; >1– 2 miles; and >2 miles.
Outcomes: BMI z-Score
The outcome measure for our analyses was the patient's age- and sex-specific BMI z-score derived from height and weight measured and recorded in the EHR at their most recent well-care visit between August 2011 and August 2012. At each well-child visit, medical assistants measured height and weight following a written standardized protocol, which are consistent with the standard of care in pediatric primary care described in detail in previously published work.10 We calculated BMI as kg/m2 and used the CDC growth curves to define the participants' BMI z-score.9
Covariates
We obtained the patient's sex and age from the EHR. Pediatric patients' race/ethnicity was based on parent report on a written card completed during the patient registration process as part of previously implemented quality improvement efforts to improve race/ethnicity documentation at these practices. We recoded the original categories into non-Hispanic white, non-Hispanic black, Hispanic, Asian, and other race/ethnicity. We obtained neighborhood median income by linking the child's geocoded residential addresses with 2006–2010 American Community Survey data at the US census tract level.
Statistical Analysis
We first examined descriptive and bivariate associations of neighborhood food establishments with our main outcomes and covariates. We then used separate multivariable linear regression models to assess associations of proximity to each of the six types of food establishments with child BMI z-score. Model 1 was adjusted for patient age, sex, and race/ethnicity. In model 2, we additionally adjusted for neighborhood household income. In the fully adjusted model (model 3), we also controlled for proximity to the five other food establishment categories. To assess for effect modification, in separate models we examined stratified models and interaction terms by: (1) dichotomizing neighborhood median income into <$50,000 and ≥$50,000; (2) creating age categories, including 4–<6, 6–<13, and 13–18 years; and (3) weight status as: <85th percentile (normal weight), 85–<95th percentile (overweight), and ≥95th percentile (obese). We conducted statistical analyses using SAS software (version 9.3; SAS Institute Inc., Cary, NC).
Results
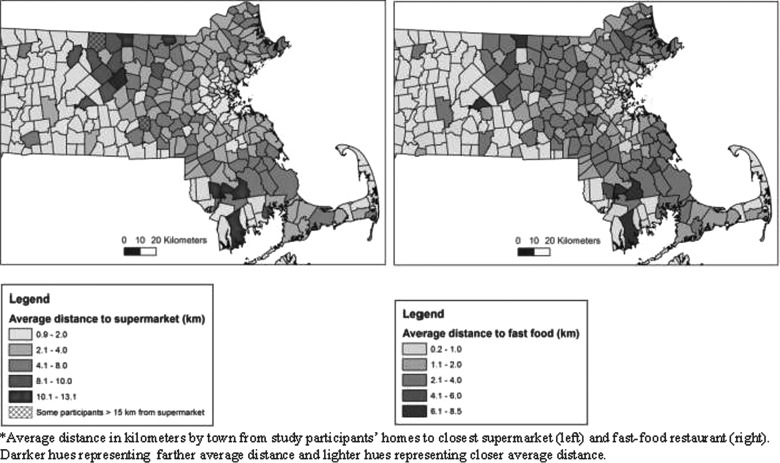
At the most recent well-child care visit in 2011–2012, mean (standard deviation; SD) age of pediatric patients was 11.3 (4.4), and mean (SD) BMI z-score was 0.42 units (1.04; Table 1). Approximately half were female and two thirds were non-Hispanic White. Mean (SD) median neighborhood household income for pediatric patients' census tract was $86,577 ($33,196). Median neighborhood household income in Massachusetts from 2007 to 2011 was $65,981.11 Mean (SD) network distance from pediatric patients' residence to the closest large supermarket and fast food restaurant was 1.57 (1.1) and 0.86 miles (0.74). Spearman's correlation coefficients among the different types of food establishments show that proximity to all food establishment types was highly correlated (r=≥ 0.5 and p<0.0001 for all correlations). Figure 1 shows the mean distance to large supermarkets and fast food restaurants by town. Towns with the largest mean distances from both large supermarkets and fast food restaurants are generally farther away from Boston.
Table 1.
Individual and Neighborhood Characteristics of 49,770 Pediatric Patients Ages 4–18 Years Living in Eastern Massachusetts
| Individual characteristics | N (%) or mean (SD) |
|---|---|
| Gender | |
| Male | 25,153 (50.5) |
| Female | 24,617 (49.5) |
| Race/ethnicity | |
| White | 29,206 (65.2) |
| Black | 5943 (13.3) |
| Hispanic | 2549 (5.7) |
| Asian | 4166 (9.3) |
| Other | 2946 (6.6) |
| Most recent well-child visit | |
| Age, years (SD) | 11.3 (4.4) |
| BMI, z-score (SD) | 0.42 (1.04) |
| Neighborhood characteristics | Mean (SD) |
|---|---|
| Neighborhood household median income (SD) | 86,577 (33,196) |
SD, standard deviation.
Figure 1.
Average distance to a large supermarket and fast food restaurant by town. Data from 49,770 children.*
In bivariate analyses of neighborhood-level covariates, we found that those living closer to large supermarkets and fast food restaurants were more likely to live in a neighborhood where median household income was lower and where a larger proportion of the pediatric patients were black or Hispanic (Table 2). We observed a negative relationship between proximity to fast food restaurants and BMI z-score (p for trend, <0.001). The farther pediatric patients lived from a fast food restaurant, the lower their BMI z-score. Mean (SD) BMI z-score at the most recent visit was 0.50 (1.08) units among patients living ≤0.5 miles from a fast food restaurant and 0.25 (0.94) units among those living >2 miles away from a fast food restaurant.
Table 2.
Characteristics of 49,770 Pediatric Patients, According to Category of Networked Distance to Large Supermarkets and Fast Food Restaurants
| Category of networked distance to large supermarkets | |||||
|---|---|---|---|---|---|
| ≤0.5 miles | >0.5–1.0 mile | >1–2 miles | >2 miles | Trend p value | |
| Individual characteristics | N (%) | ||||
| Gender | 0.89 | ||||
| Male | 2649 (50.1) | 6340 (50.8) | 9746 (50.5) | 6416 (50.5) | |
| Female | 2639 (49.9) | 6143 (49.2) | 9549 (49.5) | 6282 (49.5) | |
| Race/ethnicity | <0.0001 | ||||
| White | 2410 (51.4) | 6256 (56.2) | 11,146 (63.6) | 9391 (81.9) | |
| Black | 946 (20.2) | 2197 (19.7) | 2334 (13.3) | 466 (4.1) | |
| Hispanic | 424 (9.0) | 835 (7.5) | 1040 (5.9) | 248 (2.2) | |
| Asian | 484 (10.3) | 974 (8.7) | 1793 (10.2) | 915 (8.0) | |
| Other | 426 (9.1) | 878 (7.9) | 1201 (6.9) | 441 (3.8) | |
| Most recent well-child visit | Mean (SD) | ||||
|---|---|---|---|---|---|
| Age, years | 10.9 (4.5) | 11.1 (4.5) | 11.2 (4.4) | 11.7 (4.3) | <0.0001 |
| BMI, z-score | 0.44 (1.08) | 0.46 (1.06) | 0.44 (1.04) | 0.34 (0.99) | <0.0001 |
| Neighborhood characteristics | Mean (SD) | ||||
|---|---|---|---|---|---|
| Percent white | 66.5 (25.2) | 67.5 (26.5) | 75.5 (22.7) | 86.2 (12.4) | <0.0001 |
| Percent without high school diploma | 10 (8.4) | 10.2 (8.6) | 8.6 (7.5) | 5.5 (5.6) | <0.0001 |
| Neighborhood household median income ($) | 73,067 (29,888) | 75,866 (31,122) | 84,687 (31,359) | 106,000 (30,731) | <0.0001 |
| Category of networked distance to fast food restaurants | |||||
|---|---|---|---|---|---|
| ≤0.5 miles | >0.5–1.0 mile | >1–2 miles | >2 miles | Trend p value | |
| Individual characteristics | N (%) | ||||
| Gender | 0.76 | ||||
| Male | 10,466 (50.8) | 7015 (50.1) | 5396 (50.5) | 2276 (50.7) | |
| Female | 10,144 (49.2) | 6980 (49.9) | 5283 (49.5) | 2210 (49.3) | |
| Race/ethnicity | <0.0001 | ||||
| White | 9729 (52.7) | 8438 (66.6) | 7523 (77.7) | 3516 (87.8) | |
| Black | 3683 (20.0) | 1647 (13.0) | 536 (5.5) | 77 (1.9) | |
| Hispanic | 1674 (9.1) | 615 (4.9) | 213 (2.2) | 47 (1.2) | |
| Asian | 1807 (9.8) | 1165 (9.2) | 937 (9.7) | 257 (6.4) | |
| Other | 1562 (8.5) | 805 (6.4) | 470 (4.9) | 109 (2.7) | |
| Most recent well-child visit | Mean (SD) | ||||
|---|---|---|---|---|---|
| Age, years | 10.9 (4.5) | 11.3 (4.4) | 11.5 (4.4) | 12 (4.3) | <0.0001 |
| BMI, z-score | 0.5 (1.08) | 0.42 (1.04) | 0.34 (0.99) | 0.25 (0.94) | <0.0001 |
| Neighborhood characteristics | Mean (SD) | ||||
|---|---|---|---|---|---|
| Percent white | 66.1 (26.6) | 76.8 (22.2) | 85.4 (11.3) | 88.9 (6.4) | <0.0001 |
| Percent without high school diploma | 11.6 (9.2) | 7.4 (6.2) | 5.1 (4.2) | 3.9 (3.2) | <0.0001 |
| Neighborhood household median income | 70,285 (28,375) | 85,861 (29,014) | 104,000 (29,220) | 122,000 (26,065) | <0.0001 |
SD, standard deviation.
In models adjusted for patient age, sex, and race/ethnicity only, we found that living ≤0.5 miles (vs. >2 miles) to each food establishment, with the exception of large supermarkets, was associated with a higher BMI z-score in our cross-sectional analyses (Table 3). Adjustment for neighborhood household income in model 2 resulted in attenuation of observed BMI z-score differences and also a reversal of the direction of the associations for large and small supermarkets as well as bakeries, coffee shops, and candy stores. For example, in model 1 living ≤0.5 miles from a large supermarket demonstrated a null relationship with BMI z-score (0.02 units; 95% confidence interval [CI], −0.01, 0.05). However, after adjustment for neighborhood median income, living ≤0.5 miles from a large (−0.07 units; 95% CI, −0.10, −0.03) supermarket was associated with a lower BMI z-score, compared to those living >2 miles from a large supermarket. Therefore, taking into account patient age, sex, race/ethnicity, and neighborhood median income, pediatric patients living closer to large supermarkets had a lower BMI z-score than those living farther away. A similar reversal was found for small supermarkets. Living ≤0.5 miles from a fast food restaurant was associated with a 0.03-unit (95% CI, 0.00, 0.07) higher BMI z-score than those living >2 miles away (model 2). Those pediatric patients who lived closer to fast food restaurants had a higher BMI z-score than those living farther away after taking into account patient age, sex, race/ethnicity, and neighborhood median income. Further adjustment for distance to all other food establishments strengthened the effect estimates for large and small supermarkets and for fast food restaurants. In addition, after adjusting for all other food establishments, living ≤0.5 miles from a full-service restaurant was associated with a 0.07-unit (95% CI, 0.01, 0.14) higher BMI z-score than those living >2 miles. Pediatric patients who lived closer to full-service restaurants had a higher BMI z-score than those living farther away after taking into account child age, sex, race/ethnicity, and neighborhood median income. We did not observe an association between BMI z-score and proximity to convenience stores or bakeries, coffee shops, and candy stores.
Table 3.
Associations of Proximity to Food Establishments with BMI z-Score in 2011–2012a
| Estimates of BMI z-score at most recent well-child visit, by multivariable model (effect estimate, 95% CI) | |||
|---|---|---|---|
| Exposures | Model 1 | Model 2 | Model 3 |
| Networked distance to large supermarket, miles | |||
| ≤0.5 | 0.02 (−0.01, 0.05) | −0.07 (−0.10, −0.03) | −0.09 (−0.13, −0.05) |
| >0.5–1.0 | 0.05 (0.03, 0.08) | −0.03 (−0.06, 0.00) | −0.05 (−0.08, −0.01) |
| >1–2 | 0.06 (0.04, 0.09) | 0.01 (−0.02, 0.03) | −0.01 (−0.04, 0.02) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Networked distance to small supermarket, miles | |||
| ≤0.5 | 0.08 (0.05, 0.10) | −0.05 (−0.08, −0.02) | −0.08 (−0.11, −0.04) |
| >0.5–1.0 | 0.04 (0.01, 0.07) | −0.04 (−0.07, −0.01) | −0.06 (−0.10, −0.03) |
| >1–2 | 0.02 (0.00, 0.05) | −0.02 (−0.05, 0.01) | −0.04 (−0.07, −0.01) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Networked distance to fast food restaurants, miles | |||
| ≤0.5 | 0.18 (0.14, 0.21) | 0.03 (0.00, 0.07) | 0.09 (0.03, 0.15) |
| >0.5–1.0 | 0.13 (0.09, 0.16) | 0.02 (−0.01, 0.06) | 0.07 (0.01, 0.12) |
| >1–2 | 0.08 (0.05, 0.12) | 0.03 (0.00, 0.07) | 0.06 (0.02, 0.11) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Networked distance to full-service restaurants | |||
| ≤0.5 | 0.18 (0.14, 0.21) | 0.02 (−0.02, 0.06) | 0.07 (0.01, 0.14) |
| >0.5–1.0 | 0.13 (0.09, 0.17) | 0.02 (−0.02, 0.06) | 0.06 (0.00, 0.12) |
| >1–2 | 0.08 (0.04, 0.12) | 0.01 (−0.03, 0.05) | 0.04 (−0.01, 0.09) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Networked distance to convenience stores, miles | |||
| ≤0.5 | 0.15 (0.12, 0.18) | 0.01 (−0.03, 0.05) | 0.04 (−0.01, 0.08) |
| >0.5–1.0 | 0.11 (0.07, 0.14) | 0.01 (−0.03, 0.04) | 0.03 (−0.01, 0.08) |
| >1–2 | 0.07 (0.03, 0.10) | 0.03 (−0.01, 0.06) | 0.04 (0.01, 0.08) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Networked distance to bakeries, coffee shops, candy stores, miles | |||
| ≤0.5 | 0.12 (0.09, 0.16) | −0.02 (−0.06, 0.02) | −0.04 (−0.10, 0.02) |
| >0.5–1.0 | 0.10 (0.07, 0.14) | −0.01 (−0.05, 0.03) | −0.02 (−0.08, 0.03) |
| >1–2 | 0.06 (0.02, 0.10) | 0.00 (−0.04, 0.04) | 0.00 (−0.05, 0.04) |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.0 (ref) |
Model 1: adjusted for age, sex, and race/ ethnicity. Model 2: model 1 plus neighborhood median household income. Model 3: model 2 plus five other food establishments (continuous networked distance).
N=49,770.
CI, confidence interval.
In multivariable models stratified by neighborhood median income (Table 4), we found that living in a census tract where the neighborhood median income was <$50,000 was a statistically significant effect modifier of the relationship between distance to a convenience store and full-service restaurant and BMI z-score at baseline (fully adjusted interaction: p=0.01 and p=0.001, respectively). For example, those living ≤0.5 miles from a convenience store in a census tract with a neighborhood median income <$50,000 had a BMI z-score, which was 1.28 units (95% CI, 0.37, 2.19) higher than those living >2 miles away. Those living in a census tract with a neighborhood median income ≥$50,000 had a BMI z-score, which was 0.06 units (95% CI, 0.00, 0.13) higher than those living >2 miles away. Living closer to a convenience store had a more adverse association with BMI z-score in lower- versus higher-income neighborhoods. Similarly, those living ≤0.5 miles from a full-service restaurant in a census tract with a neighborhood median income <$50,000 had a BMI z-score, which was 1.01 units (95% CI, 0.51, 1.51) higher than those living >2 miles away. Those living in a census tract with neighborhood median income ≥$50,000 had a BMI z-score, which was 0.03 units (95% CI, −0.02, 0.07) higher than those living >2 miles away. Similar to convenience stores, living closer to a full-service restaurant had a more adverse association with BMI z-score in lower- versus higher-income neighborhoods. We did not observe effect modification by neighborhood median income and the other four types of food establishments. Further, age and weight status category were not effect modifiers of the relationship between food establishments and baseline BMI z-score.
Table 4.
Adjusted Associations of Distance to Food Establishments with Most Recent BMI z-Score, Stratifieda
| Estimates of BMI z-score by multivariable model (effect estimate, 95% CI) | |||
|---|---|---|---|
| Exposures | <$50,000 | ≥$50,000 | Interaction p valuec |
| Networked distance to large supermarket, miles | |||
| ≤0.5 | −0.03 (−0.21, 0.15) | −0.10 (−0.14, −0.05) | |
| >0.5–1.0 | −0.06 (−0.23, 0.12) | −0.04 (−0.08, −0.01) | |
| >1–2 | 0.02 (−0.16, 0.19) | −0.01 (−0.04, 0.02) | |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.11 |
| Networked distance to small supermarket, miles | |||
| ≤0.5 | −0.56 (−1.17, 0.05) | −0.08 (−0.11, −0.04) | |
| >0.5–1.0 | −0.55 (−1.16, 0.06) | −0.06 (−0.10, −0.03) | |
| >1–2 | −0.59 (−1.21, 0.03) | −0.03 (−0.06, 0.00) | |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.14 |
| Networked distance to fast food restaurants, miles | |||
| ≤0.5 | 0.00 (−0.31, 0.30) | 0.09 (0.03, 0.15) | |
| >0.5–1.0 | 0.01 (−0.28, 0.30) | 0.06 (0.01, 0.12) | |
| >1–2 | 0.0 (ref) | 0.06 (0.02, 0.11) | |
| >2 | NAb | 0.0 (ref) | 0.28 |
| Networked distance to full-service restaurants, miles | |||
| ≤0.5 | 1.28 (0.37, 2.19) | 0.06 (0.00, 0.13) | |
| >0.5–1.0 | 1.21 (0.30, 2.12) | 0.05 (−0.01, 0.11) | |
| >1–2 | 1.19 (0.29, 2.10) | 0.03 (−0.02, 0.08) | |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.01 |
| Networked distance to convenience stores, miles | |||
| ≤0.5 | 1.01 (0.51, 1.51) | 0.03 (−0.02, 0.07) | |
| >0.5–1.0 | 0.98 (0.48, 1.47) | 0.02 (−0.02, 0.06) | |
| >1–2 | 0.93 (0.44, 1.43) | 0.04 (0.00, 0.07) | |
| >2 | 0.0 (ref) | 0.0 (ref) | 0.001 |
| Networked distance to bakeries, coffee shops, candy stores, miles | |||
| ≤0.5 | 0.05 (−0.15, 0.25) | −0.04 (−0.10, 0.01) | |
| >0.5–1.0 | 0.06 (−0.14, 0.25) | −0.03 (−0.08, 0.02) | |
| >1–2 | 0.0 (ref) | 0.00 (−0.05, 0.04) | |
| >2 | NAb | 0.0 (ref) | 0.17 |
Model 1. Adjusted for age, sex, and race/ethnicity, neighborhood median household income, five other food establishments (continuous networked distance).
N=49,770.
There were no participants in these categories.
Interaction p value is adjusted for age, sex, and race/ethnicity, neighborhood median household income, five other food establishments (continuous networked distance).
CI, confidence interval; NA, not applicable.
Discussion
In this analysis of over 40,000 pediatric patients living in eastern Massachusetts, we found that those living in closest proximity to a large or small supermarket had lower BMI z-scores, compared to those living farthest away. We found that pediatric patients living closest to a fast food or full-service restaurant had a higher BMI z-score by 0.09 and 0.07 units, respectively, compared to those living farthest away. A difference in BMI z-score of 0.09 units is approximately 0.5 kg for an average height 11-year-old male (our population's average age).12 All other food establishments did not have a statistically significant association with BMI z-score. Neighborhood median income was an effect modifier of the relationships of proximity to convenience stores and full-service restaurants with BMI z-score. In both cases, closest proximity to convenience stores and full-service restaurants had a stronger adverse effect in lower-income neighborhoods (p=0.01 and p=0.001, respectively).
Our study builds upon the previous food environment research and extends that research by examining exposures to multiple types of food establishments examines objectively measured weight and height, and because of our large and diverse sample size, we were able to examine effect modification by neighborhood median income, age, and weight status category (normal weight, overweight, or obese). Previous studies have shown inconsistent associations between food establishments and BMI.3–8,13–15 For example, among 2192 low-income 2- to 4-year-olds, researchers found that a higher density of grocery stores was associated with higher BMI.13 However, in a study of 13,462 children in California ages 5–18 years, no association was found between school and neighborhood food environment and consumption of fruits, vegetables, sugar-sweetened beverages (SSBs), or fast food.8 In contrast, in a study of 7334 children ages 3–18, increased distance to large supermarkets was associated with an increased risk of obesity in lower-population areas.4 Our very large and diverse sample size demonstrated that large and small supermarkets had a protective association with BMI z-score, and fast food and full-service restaurants had an adverse association. We were also able to examine whether or not neighborhood median income, age, or BMI status was an effect modifier of these relationships.
Several potential mechanisms can help to explain our observed associations of large and small supermarkets and pediatric patient weight status. One potential mechanism is that pediatric patients who live near to supermarkets have more access to fruits and vegetables and other healthful foods, decreasing their overall calorie consumption and allowing them to maintain a lower BMI. Previous research has shown that access to low-priced fresh fruit and vegetables is associated with lower BMI among 2- to 9-year-old children.16 Supermarkets tend to have the most diverse, low-priced produce, compared to the four other categories of food establishments we examined. Because parents and families face both budget and time constraints, by living closer to supermarkets, it is likely more convenient for parents and children to purchase and consume produce on a more frequent basis and, as a result, foster a lower BMI z-score.
On the other hand, when fast food and full-service restaurants are more conveniently located to one's home, parents and families are more likely to purchase food at these locations owing to the same time and budget constraints. Fast food or full-service restaurants tend to offer higher-calorie foods, leading to increased caloric intake and a higher BMI z-score. In a national survey, those children who consumed fast food consumed 187 kcal more per day than those who did not consume fast food.17 Fast food consumers in this study ate more total fat, saturated fat, total carbohydrates, added sugars, and SSBs as well as less milk, fruit, or vegetables.17
In our study, we found that adjusting for neighborhood median household income led to reversal of the direction of the associations of BMI z-score with some of the food establishments. Another study also found differing effects of food establishments on weight status, depending on income status of the neighborhood. In higher-income neighborhoods, BMI and obesity risk were not associated with the presence of a grocery store or fast food restaurant. However, those in low-income neighborhoods had a significantly lower BMI and risk of being obese if there was one or more grocery stores in their neighborhood versus low-income areas without retail food options.18 In our stratified analyses, we found that those living in lower neighborhood median income census tracts had much higher BMI z-scores if they lived in closer proximity to convenience stores and full-service restaurants. Neighborhood median income was not an effect modifier of the relationship between BMI z-score and proximity to large or small supermarkets, fast food restaurants, or bakeries, coffee shops, and candy stores. We hypothesize that there is less variability in the products offered in large and small supermarkets as well as fast food restaurants across neighborhood median incomes given that they tend to be franchises. However, convenience stores and full-service restaurants are likely to vary in their products offered in low- and high-income areas. Further, low-income families may lack access to a car and may purchase food at the closest food establishment, which may be a convenience store or full-service restaurant. Finally, many studies have shown that there are a higher number of convenience stores in low-income neighborhoods, potentially adding to a stronger effect.19,20 As the prevalence of obesity among low-income populations continues to disproportionately rise, we believe creating policies or subsidies to increase healthier options in these establishments in low-income neighborhoods could be an effective way to reduce obesity.10,21
This study has a number of strengths, including having a large sample size, the ability to adjust for potential individual- and neighborhood-level confounders, and use of objective BMI measures from an electronic medical record. This study also has limitations. First, data quality of commercial business listings, such as InfoUSA, can be a concern in this type of research. For example, in previously published articles, InfoUSA correctly classified 69% of grocers and 81% of supermarkets.22 This imprecision of our exposure data could have attenuated our associations toward the null. This may explain why convenience stores and full-service restaurants did not have an association with BMI z-score in unstratified models. Second, we could not examine whether subjects in our study actually shopped or purchased food at nearby establishments, so we cannot assume causality. Previous studies have shown that adults do not always shop at the closest food store, traveling up to a mean distance of 6.3 miles to go to a supermarket despite the availability of a closer one.23 Third, residential selection bias could be a limitation; previous research has shown that this would attenuate associations, rather than reverse associations, as we found in this study.24 Fourth, because we only had access to the most recent address of the pediatric patients, we could not account for moving during the study period, and for 18-year-olds, we did not know whether the address in the EHR was their own or their parents. This could lead to misclassification of the exposures. Fifth, we used data from InfoUSA, which were from 2009, and we were unable to account for food establishments closing or opening from 2009 to 2011. With more up-to-date business information, this could have attenuated or strengthened our results. Sixth, because the study took place in Massachusetts, where nearly all children are insured, our findings may not be generalizable to uninsured populations. Finally, given that our study population is of higher income, it may not be generalizable to lower-income groups.
Conclusions
In conclusion, among a large sample of pediatric patients, we found associations between closer proximity to small and large supermarkets and farther distance from fast food and full-service restaurants with lower BMI z-scores. We found that neighborhood median income was an effect modifier of the relationship between convenience stores and full-service restaurants and BMI z-score. As the nation strives to find effective ways to help families make healthier choices and curtail the obesity epidemic, policy makers should look to create opportunities to create healthier food environments for children.
Acknowledgments
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and the Harvard Pilgrim Health Care Institutional Review Board approved all procedures involving human subjects/patients. A waiver of informed consent was obtained for this study given the use of existing electronic health record data.
This study was supported by a grant from Harvard Clinical and Translational Science Center (UL1 RR 025758). Dr. Fiechtner was supported through a National Institute of Diabetes and Digestive and Kidney Diseases training grant to the Division of Gastroenterology and Nutrition (T32 DK 007747).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.World Health Organization. WHO global strategy on diet, physical activity and health. World Health Organization: Geneva Switzerland, 2006, pp. 1–19 [Google Scholar]
- 2.Swinburn BA, Sacks G, Hall KD, et al. . The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011;378:804–814 [DOI] [PubMed] [Google Scholar]
- 3.Powell LM, Auld MC, Chaloupka FJ, et al. . Associations between access to food stores and adolescent body mass index. Am J Prev Med 2007;33(4 Suppl):S301–S307 [DOI] [PubMed] [Google Scholar]
- 4.Liu GC, Wilson JS, Qi R, et al. . Green neighborhoods, food retail and childhood overweight: Differences by population density. Am J Heal Promot 2007;21:317–325 [DOI] [PubMed] [Google Scholar]
- 5.Leung CW, Laraia BA, Kelly M, et al. . The influence of neighborhood food stores on change in young girls' body mass index. Am J Prev Med 2011;41:43–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mellor JM, Dolan CB, Rapoport RB. Child body mass index, obesity, and proximity to fast food restaurants. Int J Pediatr Obes 2011;6:60–68 [DOI] [PubMed] [Google Scholar]
- 7.Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health 2012;126:723–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med 2012;42:129–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat 11 2002;(246):1–190 [PubMed] [Google Scholar]
- 10.Wen X, Gillman MW, Rifas-Shiman SL, et al. . Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics 2012;129:823–831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Census Bureau. Massachusetts quick facts. 2008. Available at http://quickfacts.census.gov/qfd/states/25000.html Last accessed November15, 2013
- 12.The Children's Hospital of Philadelphia Research Institute. Pediatric Z-score calculator. 2013. Available at http://stokes.chop.edu/web/zscore/result.php Last accessed September11, 2013
- 13.Salois MJ. The built environment and obesity among low-income preschool children. Heal Place 2012;18:520–527 [DOI] [PubMed] [Google Scholar]
- 14.Fiechtner L, Block J, Duncan DT, et al. . Proximity to supermarkets associated with higher body mass index among overweight and obese preschool-age children. Prev Med 2013;56:218–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park S, Choi BY, Wang Y, et al. . School and neighborhood nutrition environment and their association with students' nutrition behaviors and weight status in Seoul, South Korea. J Adolesc Health 2013;53:655–662.e12 [DOI] [PubMed] [Google Scholar]
- 16.Beydoun MA, Powell LM, Chen X, et al. . Food prices are associated with dietary quality, fast food consumption, and body mass index among U.S. children and adolescents. J Nutr 2011;141:304–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bowman SA, Gortmaker SL, Ebbeling CB, et al. . Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics 2004;113(1 Pt 1):112–118 [DOI] [PubMed] [Google Scholar]
- 18.Zick CD, Smith KR, Fan JX, et al. . Running to the store? The relationship between neighborhood environments and the risk of obesity. Soc Sci Med 2009;69:1493–1500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bower KM, Thorpe RJ, Rohde C, et al. . The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med 2014;58:33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health 2012;102:1644–1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci U S A 2014;111:1338–1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han E, Powell LM, Zenk SN, et al. . Classification bias in commercial business lists for retail food stores in the U.S. Int J Behav Nutr Phys Act 2012;9:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kerr J, Frank L, Sallis JF, et al. . Predictors of trips to food desintations. Int J Behav Nutr Phys Act 2012;9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boone-Heinonen J, Guilkey DK, Evenson KR, et al. . Residential self-selection bias in the estimation of built environment effects on physical activity between adolescence and young adulthood. Int J Behav Nutr Phys Act 2010;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]