Abstract
Travel to procure deceased donor organs is associated with risk to transplant personnel. In many instances, multiple teams are present for a given operation. We studied our statewide experience to determine how much excess travel this redundancy entails, and generated alternate models for organ recovery. We reviewed our organ procurement organization’s experience with deceased donor operations between 2002 and 2008. Travel was expressed as cumulative person-miles between procurement team origin and donor hospital. A model of minimal travel was created, using thoracic and abdominal teams from the closest in-state center. A second model involved transporting donors to a dedicated procurement facility. Travel distance was recalculated using these models, and mode and cost of travel extrapolated from current practices. In 654 thoracic and 1469 abdominal donors studied, mean travel for thoracic teams was 1066 person-miles, and for abdominal teams was 550 person-miles. The mean distance traveled by thoracic and abdominal organs was 223 miles and 142 miles, respectively. Both hypothetical models showed reductions in team travel and reliance on air transport, with favorable costs and organ transport times compared to historical data. In summary, we found significant inefficiency in current practice, which may be alleviated using new paradigms for donor procurement.
Introduction
Procurement of deceased donor organs for transplantation is unique in the field of modern surgery, as the technical expertise and required materials are transported to the patient’s location, rather than vice versa. In the state of Michigan, as in most regions of the United States, donor operations (excluding donor nephrectomy) are typically performed by teams from the institutions planning on using the organs. Reasons for sending individual teams vary, but commonly cited advantages include the chance to visualize the organ in situ, the ability to advocate for certain anatomic approach or demarcation (i.e., point of transection of suprahepatic cava), and avoidance of graft injury during explantation (1).
Following the loss of 6 transplant personnel in a fixed wing aircraft accident in June 2007, we have undertaken a critical reassessment of the safety and efficiency of organ procurement travel practices in the state of Michigan. With an increasing appreciation of the risks associated with travel for organ procurement, efforts to reduce unnecessary trips are gaining ground (2,3). Beyond the safety risk, current procurement practices impart a heavy financial and logistical burden on transplant centers. The donor hospital setting is also significantly affected by the time committed to donor medical management and organ allocation in a critical care setting, as well as surgery scheduling conflicts that may occur between previously scheduled cases and the emergent needs of the donor recovery teams. Productivity is lost on either side of a donor procedure as a result of transit to the donor hospital and idle time around the actual operation. Overall, there may be significant opportunities to improve both the safety and efficiency of organ procurement practices in Michigan and throughout the United States.
Within this context, we first sought to better understand organ procurement travel practices in the state of Michigan. We retrospectively reviewed data on all organ procurement operations facilitated by Gift of Life Michigan over the last seven years, as well as internal travel records for University of Michigan transplant surgeons. Based on this data, we then generated hypothetical models for organ procurement practices in Michigan. The first model involved minimal donor team travel, with surgeons from the transplant center closest to the donor hospital procuring the thoracic and abdominal organs. The second model involved transportation of the donor to a theoretical organ procurement facility at Gift of Life Michigan. These models were compared to the historical data, with analysis of effects on amount, type, and costs of travel, as well as impact on organ ischemic time. We introduce these theoretical models as a starting point for discussion of improvements to organ procurement practices at a national level.
Methods
Data collection
Approval for data collection and analysis was obtained through the University of Michigan Institutional Review Board and Gift of Life Michigan. Records of all deceased donor operations involving Gift of Life Michigan between January 1, 2002 and July 22, 2008 were obtained. Each record included the donor hospital name, as well as origin of the surgeon, assistant, and perfusionist for each of the following organs: heart, left and right lung, liver, pancreas, and intestine. The ultimate destination of each procured organ was also listed. The thoracic and abdominal domains were considered separately. In cases where multiple organs from the same body cavity (thoracic or abdominal) were procured by the same institution, one team was taken to be responsible for both procedures. To assess changes in practice over time, comparisons were made between donor operations occurring before and after July 1, 2005. This date was chosen to approximate the midpoint of the sample in number of donor procedures.
As our organ procurement organization’s records related to kidney procurement were not as complete or detailed as those related to other solid organs, we compiled information on kidney travel practices from internal records at the University of Michigan. This data was used to assess the frequency with which a surgeon traveling to procure a liver or pancreas also performed a donor nephrectomy.
Amount and mode of travel
For each organ procured, the one-way distances from donor hospital to the hospital where the transplant occurred were calculated. For personnel traveling for procurement, the sum of round-trip distance for each individual was computed. Straight-line distance calculations were made using zip code data for each hospital. Final values were expressed as ‘person-miles’ for comparison between total organ and team travel. Estimates of the most likely means of transport used by procurement teams were made on straight line distance guidelines at our centers. One-way distances less than 60 miles are traveled by ground transport, distances of 60 to 120 miles are covered by helicopter, and greater than 120 miles necessitate fixed wing aircraft. These travel practice patterns were determined as a composite of current practices use by the University of Michigan and Henry Ford Hospital. We also performed a sensitivity analysis using travel practices that represent current practices in other regions of the United States. Comparisons of travel practices in Michigan with national data showed the principal difference across donor service areas to be reliance on helicopters for mid-range distances (3). We repeated our models under the assumption that travel less than 100 miles would be by ground and greater than 100 miles would be by fixed wing aircraft, and again with a distance cutoff of 150 miles. We determined these thresholds based on our previous work in which we surveyed transplant surgeons and OPO directors (3).
Average total transport costs were assigned to each mode of travel based on FY 2006 total cost data at $1104 per team for ground transport, $4742 per team for helicopter flights, and $7558 per team for fixed wing aircraft. These costs were determined using financial data from the internal cost-accounting system at the University of Michigan (TSI Systems, Lakewood, CO), and are inclusive of direct and indirect costs for driver/pilot payment and vehicle use and maintenance, but do not include compensation for surgeons and perfusionists. Cold time in transit for individual organs was calculated based on distance to the destination and likely means of travel, assuming a mean speed of 70 mph for ground transport, 150 mph for helicopter flights, and 350 mph for fixed wing aircraft.
In order to gauge the environmental impact of each trip, the same assumptions regarding mode of transport were used to estimate the CO2 footprint associated with each organ procurement trip. Average ground vehicle (ambulance, SUV, town car) CO2 production was estimated at 1.6 lb/mile, helicopter (Bell 212 or comparable) at 10 lb/mile, and fixed-wing aircraft (Gulfstream or comparable) at 16 lb/mile (4).
As practices related to kidney procurement travel were not available through the organ procurement organization’s records, we reviewed internal billing records for donor procurements by four University of Michigan transplant surgeons to assess the frequency with which they procured kidneys when traveling to obtain livers or pancreata from extramural donors.
Minimal team travel model
A model of minimal travel was applied to historical data. For each thoracic or abdominal procurement from a donor hospital in Michigan, one team from the closest in-state center (University of Michigan or Henry Ford Hospital) with a compatible program would be responsible for explanting all organs in the body cavity. Using this approach, a maximum of two teams, each consisting of surgeon, assistant, and perfusionist, would carry out the donor procedure. Organ destinations, packaged travel distance, and mode of travel were unchanged, and medical team travel was calculated as described above. Comparisons were made between historical and model data with regard to cumulative travel distance, persons traveling, reliance on fixed-wing aircraft, and total costs and CO2 footprint.
Donor transport model
In this scenario, organ procurement would be procured in a dedicated facility, with donor operations staffed by surgeons from the two in-state multivisceral organ transplant centers (University of Michigan and Henry Ford Hospital). Donors from hospitals around the state would be transported by ambulance, with two medical personnel in attendance, to the procurement center. Organs would be explanted by the facility’s team, packaged, and delivered to the transplanting institution. For each donor case, team travel was calculated as the sum of the round-trip ground distance between the donor hospital and hypothetical facility, as well as a fixed distance representing travel for the surgical team to the donor facility. To account for inability to transport some donors, data was generated using 30%, 70%, and 100% compliance, and using historical practice data in instances where the donor was not transported. As with the minimal travel model, the total cost and CO2 production figures include donor organ shipping (unaccompanied by medical personnel).
Statistical analysis
Student’s t-test was used to assess the statistical significance of comparisons between historical and model data were made for aggregate person-miles traveled, number of fixed-wing flights by transplant personnel, and transport costs and CO2 production.
Results
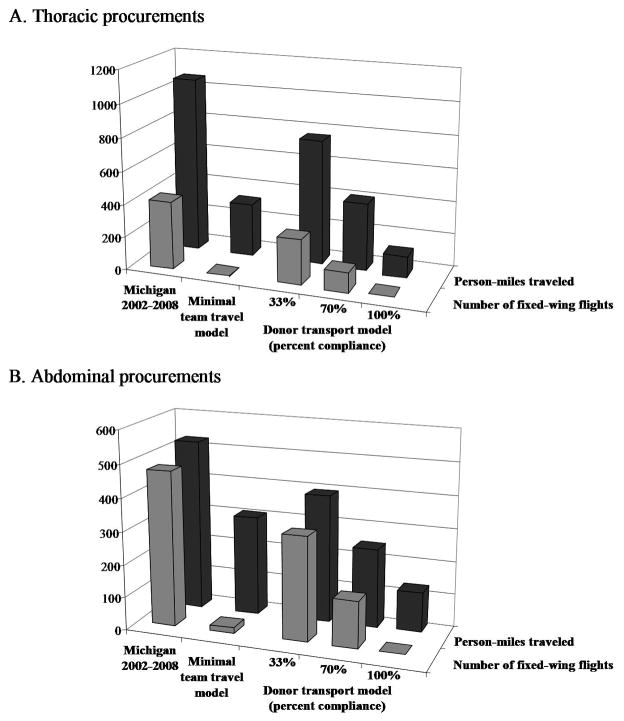
Over the course of the study period, Gift of Life Michigan facilitated 2196 organ procurement operations. From these, a total of 2018 in-state organ donors were identified. Among these, 492 donors were used for kidney-only procurement. The remaining 1526 donors had a total of 654 thoracic operations, with explantation of 855 organs. The same group had 1469 abdominal operations, resulting in explantation of 1862 organs (kidneys excluded). The distribution of numbers of organs obtained per donor is shown in Figure 1A. The average number of organs (non-kidney) obtained per donor operation was 1.77 in 2002–2005, and decreased to 1.22 in the period 2005–2008. This drop correlates with an increase in the proportion of kidney-alone donors over the same period. The numbers of separate teams present for donor procurements is shown in Figure 1B. The average number of teams per donor decreased from 1.51 in 2002–2005 to 1.47 in 2005–2008.
Figure 1.
(A) Number of non-renal organs procured per donor in deceased-donor procurements in Michigan, 2002–2008. Though not included in this analysis, kidney only procurements represented 33% (N = 592) procures over the study period. (B) Number of organ procurement teams present per deceased donor operation in Michigan, 2002–2008. Participation of the nephrectomist was not counted.
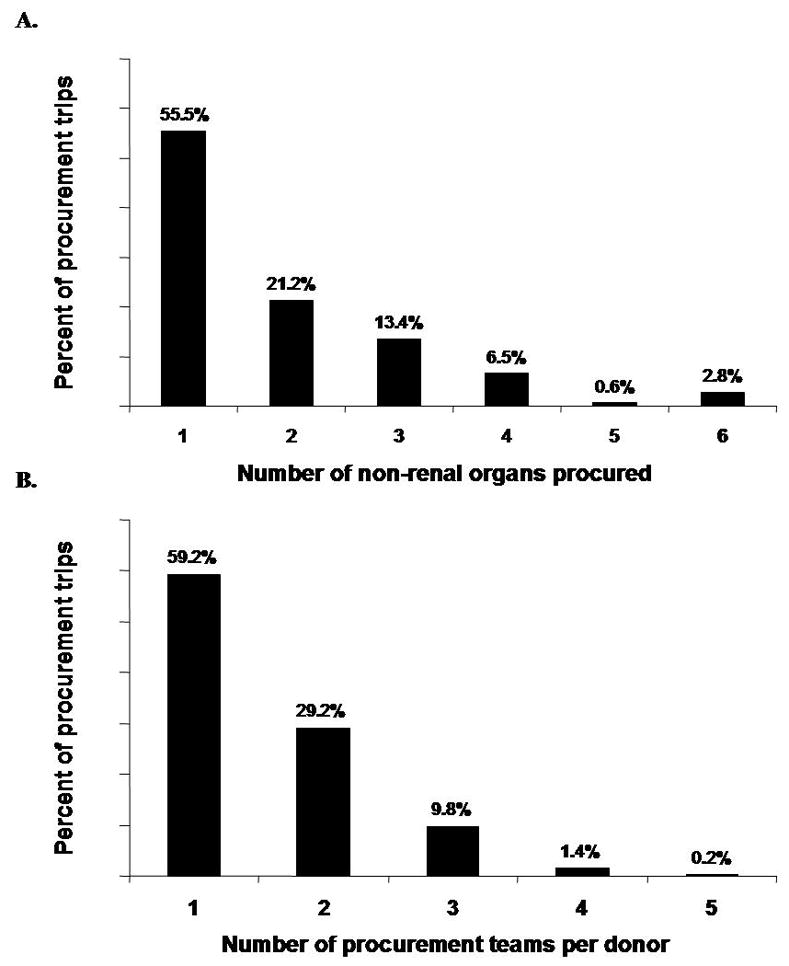
Data gathered from OPO and University of Michigan data systems on the identity of kidney procurement surgeons is shown in Figure 2. For 233 donors at which a University of Michigan surgeon was present, that surgeon removed the kidneys in only 156 cases. In 12 instances (5.2%), the kidney was the only organ procured by the university surgeon. In the remaining 77 cases, the kidney was procured by a second surgeon, most likely a local nephrectomist.
Figure 2.
Identity of kidney-procurement surgeon in donor cases attended by an abdominal team from the University of Michigan.
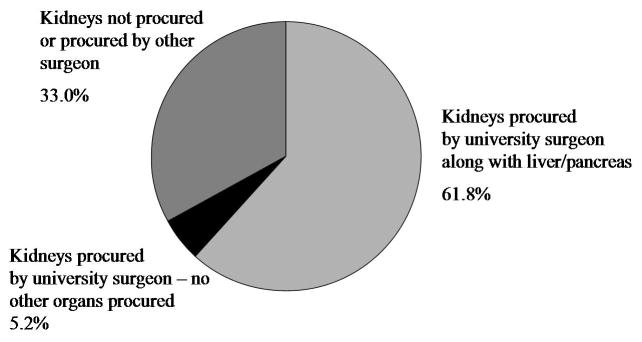
The fate of non-renal organs from the donor pool was assessed between the two time periods. Third-party use of organs was defined as transplantation at a center other than the institution responsible for the procurement. As shown in Figure 3, use of third party teams decreased in every category between 2005 and 2008. This difference was most apparent with regard to heart transplant, with a 14-fold drop between the two periods reviewed. To assess whether decreased reliance on third party organs was associated with changes in organ utilization, the proportion of discarded organs was compared between 2002–2005 and 2005–2008. These data represent organs from donors where a team was dispatched for a planned procurement, but the organ was ultimately not used. The overall discard rate of organs was 8.1% in the period 2002–2005, and 8.3% in 2005–2008. There was no obvious relationship between the use of third-party procurement teams and organ discard rates.
Figure 3.
Organ procurement by non-recipient institutions and rates of non-renal organ discard in Michigan, 2002–2008.
The relative distance traveled by members of procurement teams and the organs they explanted are shown in Figure 4. In this comparison, distances are expressed in person-miles. Organ travel is the one-way, straight line distance between the donor and recipient hospitals. Donor team travel represents the sum of the round-trip distance covered by all medical personnel responsible for the donor procedure. Heart, lung, and intestine procurements had proportionately greater team travel relative to organ transport distance than did liver and pancreas procurements. Measurement of person-miles covered for various organ types showed no significant change over time between 2002 and 2008. The percentage of donor teams traveling from outside Michigan to procure organs in Michigan for differing organ types was: heart 45%, lung 42%, liver 17%, pancreas 9%, and intestine 95%.
Figure 4.
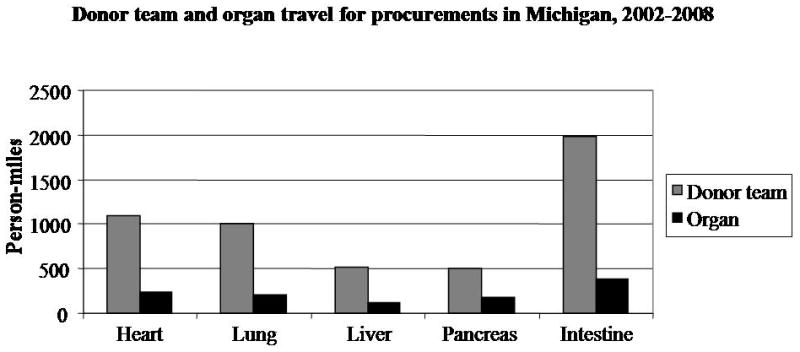
Donor team and organ travel in Michigan, 2002–2008. Person-miles represent the sum of the distances traveled by each individual on the procurement team.
Table 1 shows how travel for thoracic and abdominal procurements would have differed had surgeons relied solely on automobiles and fixed-wing aircraft, with a cutoff distance for air travel at either 100 or 150 miles one-way. As shown, the number of flights would increase with a reduction of the threshold distance for air travel to 100 miles, and would decrease with a threshold of 150 miles. Because the bulk of travel would be reassigned from helicopter to automobile travel, modest benefits would be realized in cost and carbon emissions in comparison to historical practice.
Table 1.
Effect of changes in travel practice in Michigan to a ground travel/fixed-wing aircraft only model.
| Michigan 2002–2008 | 100 mile auto/fixed-wing cutoff | 150 mile auto/fixed-wing cutoff | |
|---|---|---|---|
|
| |||
| Number of fixed-wing flights | 408 | 425 | 390 |
| Total travel (vehicle) costs | $4,694,596 | $4,564,206 | $4,338,316 |
| Total CO2 footprint (lbs.) | 6,049,813 | 5,955,206 | 5,828,900 |
|
| |||
| Number of fixed-wing flights | 494 | 538* | 422* |
| Total travel (vehicle) costs | $8,962,938 | $8,617,540 | $7,868,876* |
| Total CO2 footprint (lbs.) | 4,489,576 | 4,325,656 | 3,991,576* |
denotes P < 0.05 when compared with historical values (Michigan 2002–2008)
Alternative practice models for organ procurement
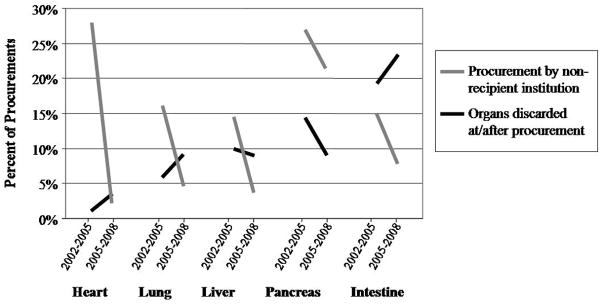
The results of alternative models for donor team travel are given in Figure 5. In the minimal team travel model, a maximum of one team would travel for each abdominal or thoracic procurement. The organ destination would not change, but donor teams would travel from the nearest in state center. Of the 145 potential donor acute care hospitals in Michigan, the University of Michigan would be the closest abdominal or thoracic transplant center for 91, with the remainder closer to Henry Ford Hospitals in Detroit. Using this model, the number of persons traveling for thoracic procurements would be reduced by 31%, and those needed for abdominal operations would decrease by 18%. As shown in Figures 5A and B, the model would reduce travel in person-miles by 70% for thoracic procedures, and by 42% for abdominal procurements. The minimal travel model would reduce dependence on fixed wing aircraft for thoracic operations by 99%, with a corresponding 69% increase in ground travel. Abdominal organ procurement would change less dramatically, but the model would still reduce fixed wing flights by 87% and helicopter flights by 14%.
Figure 5.
Impact of alternate models of thoracic (A) and abdominal (B) donor organ procurement on cumulative team travel and dependence on fixed-wing aircraft.
Also shown in Figures 5A and B is the expected amount and type of travel if the donor was transported to a dedicated donor procurement facility. The 30% and 70% models of compliance still incorporate some historical practices, but with increasing utilization of the donor facility, the requirement for air travel of donor teams could theoretically drop to zero. At 70% compliance, the number of person-miles travel for thoracic and abdominal procurements would drop by 61% and 54%, respectively.
Table 2 summarizes expected changes to travel-associated costs of donor procurement using either the minimal travel or donor transport models. Use of the minimal travel model would decrease travel costs by 25% for abdominal cases and 27% for thoracic cases. Increased compliance with a donor transport model would improve cost savings, with an overall reduction of 42% for abdominal cases and 34% for thoracic cases at 70% utilization of a dedicated donor facility.
Table 2.
Comparison of historical and model data for donor travel practices in Michigan
| Michigan 2002–2008 | minimal team travel1 | transport of donors2 (percent compliance) | |||||
|---|---|---|---|---|---|---|---|
| 33% | 70% | 100% | |||||
|
| |||||||
| Thoracic | organ | Miles traveled | 212 | 212 | 198 | 183* | 170* |
| Cold time in transit (hrs) | 0.87 | 0.87 | 0.80 | 0.72* | 0.65** | ||
| team | Person miles traveled | 1066 | 323* | 757 | 410** | 129** | |
| # fixed wing flights | 408 | 3** | 273* | 122** | 0** | ||
| Total travel (vehicle) costs | $4,694,596 | $3,438,412* | $ 3,929,797* | $ 3,072,294** | $ 2,377,022** | ||
| Total CO2 footprint (lbs.) | 6,049,813 | 2,166,968* | 4,554,091* | 2,877,070** | 1,517,323** | ||
|
| |||||||
| Abdominal | organ | Miles traveled | 137 | 137 | 121* | 103** | 89** |
| Cold time in transit (hrs) | 0.65 | 0.65 | 0.58 | 0.50* | 0.43** | ||
| team | Person miles traveled | 550 | 318* | 410* | 253** | 125** | |
| # fixed wing flights | 494 | 18** | 331* | 148** | 0** | ||
| Total travel (vehicle) costs | $8,962,938 | $6,684,606* | $7,194,045 | $ 5,210,741** | $ 3,602,656** | ||
| Total CO2 footprint (lbs.) | 4,489,576 | 3,321,431* | 3,509,276* | 2,410,152** | 1,518,971** | ||
denotes P < 0.01 when compared to historical values
denotes P < 0.001 when compared to historical values
minimal travel model assumes a maximum of one thoracic and one abdominal team per donor, from nearest in-state center
donor transport model utilizes a facility in Ann Arbor, MI, with shared duty between UMMC and HFH transplant surgeons for procurements. Percent compliance assumes non-transported donors have procurements as per historical data
The effect of changes to donor travel practice on organ ischemic time in transit is also shown in Table 2. The minimal team travel would not affect the distance between organ and destination, and so there would be no change in preservation time. Because the organs would travel to their ultimate destinations from a central location in the donor transport model, the transit time would change. As shown, at a compliance level of 70%, the donor transport model would decrease cold time in transit by approximately 10 minutes for both abdominal and thoracic organs.
Finally, Table 2 shows estimates of greenhouse gas generation with donor procurement travel for historical data and each model. As expected based on the disproportionate carbon dioxide footprint of small fixed wing aircraft, the reductions in flights in the minimal team travel model and higher utilization levels of a donor transport model are associated with large reductions in CO2 output.
Discussion
In this report, we examined organ procurement travel practices within the state of Michigan. We found that the majority of in-state donors are operated on by one or two teams, but that in 12% of cases, more than one team is present for each body cavity. Over the course of the study period, there was a trend toward decreased utilization of third-party donor teams to procure organs. This increased reliance on institutional, rather than shared, donor responsibilities corresponded to a rise in the mean number of teams present for each procurement. Analysis of the relative amount of travel by donor teams and the organs they procured showed heart, lung, and intestinal procurements to have the most travel by personnel. This parallels our finding that organs from these categories are more commonly procured by out of state teams. Finally, we created hypothetical models for organ procurement which would significantly reduce the costs of travel and the need for transplant personnel to travel long distances or travel by air transport. These models suggest that the greatest potential benefits could be realized with increasing utilization of donor transport to a central donor facility.
Measurement of optimal utilization of deceased donor organs is a complex problem (5), with multiple measures of success, including organs recovered per donor, organs transplanted per donor, as well as the Caldes procurement and transplant indices (6). The relative efficiency of organ procurement practices is less-well understood. Several European efforts focused on streamlining donor procedures with regional procurement teams (7–9), with favorable cold ischemia times and short-term graft function compared to standard methods. Other work has added support for alternate procurement strategies, including the finding that lungs shipped from third party procurements have equivalent outcome to extramural procurements by the institution’s own team (10).
Upon first consideration, transporting donors away from the donor hospital might seem unorthodox and impractical. However, Mid-America Transplant Services has piloted such a program with reported success. More specifically, their report on use of a dedicated donor facility to centralize procurement noted reductions in time from brain death to crossclamping and thoracic organ cold ischemic times (11). The centralized donor procurement process also may reduce organ acquisition costs for the donor service area, especially if the diagnostic tests and procedures as a part of donor workup are offloaded to the facility rather than occurring in the donor hospital. Finally, surgeon satisfaction will undoubtedly improve with reduced travel burdens. Overall, our findings add to the discussion on procurement practice by providing data on existing donor systems in a busy donor service area, and showing the degree to which sharing donor duties between transplant centers could reduce travel requirements and associated costs.
One limitation of our study is the lack of OPO-level data on kidney procurement practices. Kidneys have traditionally been procured and handled differently than other organs, with many procurements handled by local (non-transplant) surgeons serving as nephrectomists. Some understanding of kidney procurement practice can be gained from review of University of Michigan records over the same period as our statewide data gathering. We found that only 5% of procurements by our surgeons involved kidney-only operations, and that in only 62% of cases where we traveled to procure a liver and/or pancreas did we also perform the donor nephrectomy. As the overwhelming majority of liver and pancreas donors are also kidney donors, we calculate that local surgeons performed approximately 1000 procurements within Michigan over the study period. These surgeons almost universally live close to the donor hospital, and the organs they procure are shipped by courier service. Recipient surgeon satisfaction with this model is high, and as the personnel travel distances are short, kidney-only procurement does not represent an area in which travel policy changes are as pressing as with procurement of other organs.
Other limitations of our dataset include absence of information on donor age or type (ie, deceased cardiac death or extended criteria donors), so that analyses of more or less favorable donor groups are not possible. In addition, information of type of vehicle used is based on straight-line distance assumptions, rather than historical data, and does not account for circumstances such as physician preference and weather conditions. These assumptions also apply to cost and organ ischemic time calculations. In order to expand the applicability of our results to other organ procurement organizations whose travel practices differ from our own, we recalculated our estimates of numbers of fixed wing aircraft flights and travel costs and carbon emissions using two sets of distance cutoffs for ground vs. air transport, and eliminating helicopter travel. These models showed modest differences from our practice, but overall estimates of other OPO travel policy were still much more similar to our historical data than to any of the models proposed to increase travel efficiency.
Finally, the models of more efficient procurement travel are rudimentary. The minimal travel model excludes out of state centers that may be considerably closer to donor hospitals than either Henry Ford Hospital or the University of Michigan. A more accurate representation of least-distance procurement would require national data to correctly link each potential donor hospitals to the nearest transplant center. Ultimately, any such proposal would likely require regional adjustments to ensure parity of donor duties among transplant programs. Finally, the alternative models for organ procurement practices require that transplant surgeons surgeon allow third-party donor teams to procure organs on their behalf. Though this happens rarely in the United States at this time, the majority of abdominal and thoracic transplant surgeons have self-reported willingness to transplant organs procured by a third party donor team. (3) Such donor procurement relationships will require oversight and an infrastructure of exceptional communication in order to be successful.
Despite these shortcomings, we believe that these data are an accurate representation of organ donation in Michigan, and that their reporting and analysis can aid in future policy discussions. Information on the amount and costs of travel associated with deceased donor operations will be vital to planning future procurement strategies. The continued practice of transplantation depends on its financial viability, and as such, efforts to eliminate waste in procurement practice must be considered by the transplant community. In addition, ACGME regulations and the realities of the 80 hour workweek are already reducing the extent of resident involvement in donor operations. Public opinion strongly supports this movement, and limitations on fellow and staff level work hours may not be far off. These changes will further increase pressure to avoid redundancy of surgical personnel at donor operations. Finally, surgeons and the healthcare system as a whole have a responsibility to practice environmental stewardship. If excess travel can be curtailed without compromising patient outcomes, it will afford considerable reductions in greenhouse gas generation. We believe that these challenges can best be met with an integrated approach, using cooperation between transplant centers and organ procurement organizations, open dialog with private and federal payers, exploitation of emergent technologies such as EISOR (extracorporeal interval support for organ retrieval) (12), and partnership with industry to streamline the donation process.
Long-distance travel of procurement teams is resource-intensive and exposes transplant personnel to accident risks. The desire to ensure organ quality drives many decisions to travel to organ procurements, but this consideration does not necessarily require the resources and risk to personnel inherent in the current system. The discussion on procurement practice should remain open, and efforts to improve the safety and efficiency of organ procurement should take their place alongside initiatives to maximize clinical outcomes.
Acknowledgments
Funding sources: Raymond Lynch is supported by an award from the American Society of Transplant Surgeons. Amit Mathur is supported by an NIH/NRSA T32 institutional training grant in surgical oncology. Michael Englesbe is supported in part by a grant from the American Surgical Association.
References
- 1.Nijkamp DM, Slooff MJ, van der Hilst CS, Ijtsma AJ, de Jong KP, Peeters PM, et al. Surgical injuries of postmortem donor livers: incidence and impact on outcome after adult liver transplantation. Liver Transpl. 2006;12:1365–70. doi: 10.1002/lt.20809. [DOI] [PubMed] [Google Scholar]
- 2.Merion RM. In Memoriam – University of Michigan Transplant Flight Team, June 4, 2007. Am J Transplant. 2007;7:2060–1. [Google Scholar]
- 3.Englesbe MJ, Merion R, Sinibaldi J, Berge E, Pelletier S, Sonnenday C, et al. Organ Procurement Travel Practices and Risks: A Survery of Members of American Society of Transplant Surgeons (ASTS). Presented at The American Transplant Congress; Toronto, Canada. May 2008. [Google Scholar]
- 4.Bloch M. Carbon dioxide emissions calculator. 2008 [Online] [cited 2009 May 12]; Available from: URL: http://www.carbonify.com/carbon-calculator.htm.
- 5.Porta FK, Merion RM, Roys EC, Wolf RA. Trends in Organ Donation and Transplantationin the United States, 1997–2006. Am J Transplant. 2008;8:911–21. doi: 10.1111/j.1600-6143.2008.02170.x. [DOI] [PubMed] [Google Scholar]
- 6.Ghirardini A, Nanni Costa A, Venturi S, Ridolfi L, Petrini F, Taddei S, et al. Evaluation of the efficiency of the organ procurement and transplantation program. Transplant Proc. 2000;32:100–3. doi: 10.1016/s0041-1345(99)00894-5. [DOI] [PubMed] [Google Scholar]
- 7.Gubernatis G, Oldhafer K, Rohwer K, Fieguth HG, Korner MM, Vogelsang F, et al. Regional organ procurement teams for abdominal and thoracic organs provide a rapid and personal service for organ donation in peripheral hospitals. Transplant Proc. 1997;29:1484–6. doi: 10.1016/s0041-1345(96)00698-7. [DOI] [PubMed] [Google Scholar]
- 8.van Wezel HBM, van der Vliet JA, Hordijk W, Haase-Kromwijk B, Barendregt WB, Boll APM, et al. A regional explantation team: a big step forward in the organisation of organ procurement. Transplant Proc. 1997;29:1487–8. doi: 10.1016/s0041-1345(96)00000-0. [DOI] [PubMed] [Google Scholar]
- 9.Signori S, Boggi U, Vistoli F, Del Chiaro M, Pietrabissa A, Costa A, et al. Regional procurement team for abdominal organs. Transplant Proc. 2004;36:435–6. doi: 10.1016/j.transproceed.2004.02.060. [DOI] [PubMed] [Google Scholar]
- 10.Shiraishi Y, Ochoa L, Richardson G, Semenkovich JR, Trulock EP, Sundaresan S, et al. Retrieval by other procurement teams provides favorable lung transplantation outcome. Ann Thorac Surg. 1997;64:203–6. doi: 10.1016/s0003-4975(97)00129-x. [DOI] [PubMed] [Google Scholar]
- 11.Moazami N, Javadi OH, Kappel DF, Wagner J, Jendrisak MD. The feasibility of organ procurement at a hospital-independent facility: a working model of efficiency. J Thorac Cardiovasc Surg. 2007;133:1389–90. doi: 10.1016/j.jtcvs.2006.12.038. [DOI] [PubMed] [Google Scholar]
- 12.Hundley J, Lynch RJ, Pelletier SJ, Abbas AA, Kazimi M, Yoshida A, et al. Biliary complications following liver transplantation from donation after cardiac death donors using extra-corporeal interval support for organ retrieval (EISOR). Presented at the ASTS Winter Meeting; Marco Island, FL. January 2009. [Google Scholar]