Abstract
An exigent need exists for HIV prevention intervention research targeting young men who have sex with men (MSM) – a group of young adults that, despite composing the highest and most racially disproportionate rates of HIV incidence, has been least often the focus of behavioral intervention research. This pilot study tested a group-based HIV primary prevention intervention for young MSM to evaluate its initial efficacy, feasibility, and acceptability. Participants were randomized (N=101; aged 16-20 years) to one of two group-level, HIV and STI education programs: controls participated in a non-interactive, lecture-based program while intervention participants took part in a highly interactive program tailored to young MSM aged 16-20. Sexual risk and social cognitive outcomes were assessed at baseline, and 6- and 12 weeks post-intervention. Over the entire follow-up period, intervention participants were less likely than controls to engage in any sexual behavior while under the influence of substances (p<0.05), and also observed in this group was a decreasing trend of unprotected anal sex while under the influence of substances (p=.08). Follow-up differences between groups on social cognitive outcomes favored the intervention group, though these differences were non-significant. Acceptability ratings were modest. A 6-session behavioral intervention tailored to young MSM, aged 16-20, is feasible, acceptable, and demonstrates evidence of preliminary efficacy in reducing sexual risk, specifically sexual risk while under the influence of substances.
Keywords: adolescents, sexual risk, homosexuality, sexually transmitted infection, substance use
Introduction
Annually in the United States, one in four (or 12,200) new HIV infections are among youth aged 13 to 24 (CDC, 2012a, 2012b). The majority of these infections (72%) are acquired by young men who have sex with men (MSM) with African American and Latinos particularly burdened by disproportionately high infection rates (CDC, 2012a, 2012b, 2013). Annual rates of HIV infection in young MSM continue to rise (by 22% from 2008-2010), indicating a need for primary prevention with increasingly younger groups of MSM (CDC, 2012a, 2012b).
In young MSM, HIV risk behavior has been linked to social cognitive and skills-based factors, namely low knowledge and self-efficacy regarding safer sex, ineffective condom use skills, and ineffective sexual health-related communication with sexual partners. A recent comprehensive review outlines these and other factors contributing to HIV risk in young MSM (Mustanski, Newcomb, Du Bois, Garcia, & Grov, 2011). Additionally, substance use during sex is documented as highly prevalent in young MSM (Garofalo, Wolf, Kessel, Palfrey, & DuRant, 1998; Newcomb, 2013; Thiede et al., 2003) and, compared to both heterosexual young men and MSM over age 25, some evidence suggests that young MSM who use alcohol, marijuana, and stimulants during sex are more likely to engage in unprotected sex (Celentano et al., 2006; Salomon et al., 2009) (for contradictory evidence see (Mustanski, 2008)).
Regardless of their sexual identity label, young MSM may experience overt or implied forms of social discrimination in their family systems, ethnic/cultural communities, educational settings, and other social institutions (Harper, Jernewall, & Zea, 2004; Harper & Schneider, 2003; Meyer, 1995; Nadal et al., 2011). These experiences contribute to internalized negative attitudes regarding homosexuality (Meyer, 1995), which can predict sexual risk behavior in MSM (Huebner, Davis, Nemeroff, & Aiken, 2002; Meyer & Dean, 1995) – although this effect may be declining over time (Newcomb & Mustanski, 2011). Family and school-based discrimination, including family rejection, violence and peer victimization, are associated with homelessness in young MSM, and homelessness may precipitate various safety and health risks including increased sexual risk behavior (Bontempo & D'Augelli, 2002; Ryan, Huebner, Diaz, & Sanchez, 2009).
Several evidence-based interventions (EBI) have demonstrated effectiveness in reducing HIV risk behavior among ethnically-diverse samples of MSM, aged 18-65 (Jones et al., 2008; Kegeles, Hays, & Coates, 1996; Koblin, Chesney, & Coates, 2004; Wilton et al., 2009). These EBI often rely on group-level approaches (as opposed to community- or individual-level approaches) with narrow inclusion criteria and usually employed in clinics, HIV testing sites, and other health venues that attract individuals with histories of sexual risk behavior (Elford & Hart, 2003; Warner et al., 2003). In addition, group-level interventions are cost-effective and reach a greater number of participants than individual-level interventions, and they likely increase odds of condom use in MSM compared to both individual- and community-level interventions (Herbst et al., 2007). While no existing EBI have yet to address HIV risk in MSM under age 18 (Harper, 2007), at least one has been effective at reducing HIV risk among a younger group of MSM (those aged 18-27) (Kegeles et al., 1996). The protracted absence of EBI for MSM under age 18 grows more pronounced with documented increases in HIV incidence among these MSM and evidence indicating their earlier sexual initiation compared to years past (Garofalo et al., 1998).
This pilot study sought to determine initial efficacy, feasibility and acceptability of a group-based, primary prevention intervention designed to reduce HIV risk behavior in ethnically-diverse groups of young MSM aged 16-20. It was hypothesized that, compared to controls, (1) participation in the intervention condition would result in reduced sexual risk behaviors at follow-up and (2) that intervention participation would positively influence intermediate, social cognitive and skills-based factors that contribute to HIV risk behavior in young MSM.
Method
Participants
Participants were young MSM, aged 16-20, who reported having anal intercourse with another male in the past 12 months, were HIV-negative (by self-report), and who resided in a large Midwestern city. Recruitment efforts spanned 18 months, concluding in December 2010, and consisted of 2-3 study recruitment staff members approaching all adolescent and young adult males at public events frequented by lesbian, gay, bisexual, and transgender (LGBT) youth (e.g., dances, LGBT community festivals), in LGBT youth-serving community-based organizations, at high school gay-straight alliances and college student groups throughout the greater metropolitan area. The 6 study recruitment staff members were males and females in their early to mid-twenties, 5 identified as lesbian or gay, and all had experience conducting venue-based community sampling with LGBT youth populations. During these interactions, recruitment staff introduced themselves, shared information about the study aim and its procedures, conducted a 10-item eligibility screener in cases when individuals agreed to be screened, and scheduled the initial baseline visit (conducted at one of two study locations) for individuals who screened eligible. The eligibility screener, based on study inclusion criteria, included items such as “How old are you?” and “Have you been sexually active with a male in the past 12 months?” Approximately two-thirds (N=187) of the total 280 individuals approached by study staff agreed to be screened. Study promotional materials, which provided study telephone and email contact, were distributed in recruitment settings, restaurants and businesses frequented by youth, and on social networking websites (e.g, Twitter, Facebook). Individuals who contacted the study were then scheduled to undergo eligibility screening conducted either in person or by phone. To confirm eligibility status, individuals deemed eligible via phone screening were re-screened in person at the start of their initial baseline visit.
Study Design
This study employed a randomized controlled trial design approved by the Institutional Review Boards of the participating institutions and registered with ClinicalTrials.gov (ClinicalTrials.gov number: NCT01771237). After obtaining informed consent/assent, a baseline assessment was administered and participants were randomized to either (a) the 6-session intervention or (b) a 6-session, safer sex education group (time-matched, active control).
Intervention Methods
MyPEEPS (Male Youth Pursuing Empowerment, Education and Prevention around Sexuality) is a group-level intervention to reduce sexual risk behaviors among young MSM aged 16-20. Informed by social cognitive theory (Bandura, 1994), MyPEEPS aims to educate participants about modes of HIV transmission, increase self-efficacy for condom use, increase assertive safer sex-related communication, generate situation-specific risk reduction strategies, and increase awareness about the influence of substance use on sexual risk (Table 1). MyPEEPS was developed by this investigative team based on semi-structured, qualitative interviews they conducted among a multiethnic sample of 21 young MSM. Given the ultimate aim to develop a HIV primary prevention intervention for young MSM aged 16-20, qualitative interviews collected retrospective accounts of HIV risk in young MSM, aged 18-24, all of whom acquired HIV through male-male sexual activity between ages 16-20 (Hidalgo, Cotten, Johnson, Kuhns, & Garofalo, 2013). These qualitative findings indicated the importance of addressing homophobia and racism in primary prevention efforts; therefore, integrated into MyPEEPS are theories of sexual minority stress, racial identity development, and stigma management (Diaz, Ayala, & Bein, 2004; Hatzenbuehler, 2009; Helms, 1990; Meyer, 2003). Qualitative findings also included testimonies in which respondents explicitly requested the implementation of intervention groups by gay/bisexual males, and in a setting that was affirming of young MSM; therefore, MyPEEPS ran in a lesbian, gay, bisexual, and transgender community health center, and two gay/bisexual male facilitators, both of whom had extensive experience leading group-based interventions among LGBT youth, delivered the intervention to optimize its relevance and cultural competence (Berkel, Mauricio, Schoenfelder, & Sandler, 2011; Wilson & Miller, 2003).
Table 1. Group Session Content by Condition.
| Intervention Condition | Control Condition | |||
|---|---|---|---|---|
| Session | Subject | Activities | Subject | Activities |
| 1 | Intro and Communication | Provide intervention overview, and discuss effective interpersonal communication and HIV/STI epidemiology in YMSM. | Sexually Transmitted Infections (STIs) | Present distinctions between viral, bacterial, and parasitic STIs, and information regarding the course and symptomology of STIs. |
| 2 | HIV/AIDS and STIs | Discuss safer sex specific to YMSM, effective condom use, and distinctions between viral, bacterial, and parasitic STIs. | HIV Myths and Facts | Distinguish factual information from common misconceptions and beliefs about HIV transmission and treatment. |
| 3 | Managing Minority Stress | Discuss minority stress, its influence on motivation to practice safer sex, and role-play safer sex strategies in situations involving minority stress. | What are HIV and AIDS? | Define HIV and AIDS, and describe the biological and behavioral modes of HIV transmission. |
| 4 | Affect and Emotion Regulation | Discuss the influence of emotion regulation on motivation to practice safer sex, and role-play safer sex strategies related to session content. | Who's Most at Risk for HIV Infection? | Highlight populations most vulnerable to HIV infection, including YMSM. Present HIV/AIDS epidemiology in YMSM. |
| 5 | Interpersonal and Substance-related Risk Factors | Discuss the influence of partner communication and substance use on motivation to practice safer sex, and role-play safer sex strategies related to session content. | HIV Prevention | Describe abstinence and methods of safer sex behavior, including condom use, and the effectiveness of each method at preventing HIV transmission. |
| 6 | Goal-making and Wrap Up | Review intervention content, develop personal risk reduction plans, and identify strategies to overcome barriers to success. | HIV Treatment Options | Describe treatment options for HIV and notable side effects of medications to treat HIV. |
The MyPEEPS intervention is a manualized curriculum consisting of 6 modular, interactive, group sessions (2 hours each), delivered twice weekly for three weeks. Adolescent behavior is highly peer influenced (Gardner & Steinberg, 2005; Steinberg, 2008); therefore, group census was kept between 5-10 young men to enhance opportunities for prosocial, peer feedback regarding sexual health behavior (Goodenow, Szalacha, & Westheimer, 2006; Herbst et al., 2007). Intervention sessions incorporated developmentally-appropriate, didactic approaches that have been linked with salubrious sexual health behavior in adolescents (Pedlow & Carey, 2004). Therefore, session content was concretely presented with each session consisting of brief lectures, demonstrations, group exercises, small and large group discussions, and role-plays. Each session was introduced through a cartoon vignette in which a fictitious young MSM managed his sexual health against a backdrop of personal, family-based, and relational challenges. These characters and scenarios were composites developed from our qualitative findings.
The time-matched control condition consisted of a group-level intervention also focused on HIV risk reduction, located in the same building as MyPEEPS, and comprised of 5-10 young MSM. The control relied entirely on a lecture format led by one facilitator and thus was largely didactic. Although the lecture slideshow content was not tailored to sexual situations pertaining to male-male sex it did feature information on HIV/STI transmission and effective condom use (Table 1).
Data Collection
Computer-assisted self-interviewing (CASI) was utilized to evaluate participants at three time points: baseline, 6-week post-intervention and 12-week post-intervention. CASI assessed primary and intermediate outcomes, intervention acceptability, and sociodemographic characteristics. Prior to implementation CASI was piloted among young MSM (n=9) to ensure its comprehension.
Primary Outcome Measure
Male-male sexual risk in the prior 6-week period was evaluated at all time points using the AIDS-Risk Behavior Assessment (ARBA) adapted for young MSM (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001; Garofalo, Herrick, Mustanski, & Donenberg, 2007; Garofalo, Mustanski, McKirnan, Herrick, & Donenberg, 2007). Variables of interest included total number of sex partners and total number of unprotected anal sex partners, and frequencies for unprotected sex acts (anal or oral), sex (oral or anal) under the influence of alcohol/drugs, and unprotected anal intercourse under the influence of alcohol/drugs. Respondents rated frequency items on a 5-point Likert scale (0=Never, 5=Always). A sample item is “In the last 6 weeks, when you had anal sex, how often did you or your partner use a condom?”
Intermediate Outcome Measures
Behavior change is moderated and mediated by intermediate personal and social factors including knowledge (e.g., how to use a condom), self-efficacy, and inter-personal communication skills (Bandura, 1994). Internalized homophobia has also been associated with sexual risk behavior in young MSM (Meyer & Dean, 1995). These intermediate factors were assessed using measures psychometrically validated among youth and, in some cases, young MSM. All measures were scored by summing across items. While this study was not powered for tests of moderation and mediation, the purpose of the inclusion of these factors was to measure the impact of the intervention on them as intermediate targets given their potential role in behavior change.
Self-efficacy for safer sex and situational temptation for unsafe sex
The 10-item Self-efficacy for Safer Sex (Parsons, Halkitis, Borkowski, & Bimbi, 2000) scale (SSS) (alpha = 0.72) was used to assess self-efficacy in practicing condom use and safer sex communication with a partner. Respondents rated items on a 5-point Likert scale (1=strongly agree, 5=strongly disagree) with a lower scale score indicating greater safer sex self-efficacy. A sample item is “If I didn't want to have sex with my partner, I would be able to say ‘no.’” Included as a companion measure was the 7-item Situational Temptation for Unsafe Sex scale (Parsons et al., 2000) (STUS) (alpha= 0.74) in which respondents rate hypothetical situation-based influences for unsafe sex (e.g., pressure from a sex partner) on a 5-point likelihood scale (1=much more likely, 5= much less likely). A higher scale score indicates greater situational temptation. A sample item is “How likely would you be to use condoms if condoms are not readily available and you (or your partner) have to go out and get them?” SSS was assessed at baseline and 6-week post-intervention, and STUS at baseline and at 6- and 12-week post-intervention.
Condom errors
The 12-item Condom Use Errors and Problems Questionnaire (Crosby, Sanders, Yarber, Graham, & Dodge, 2002) was adapted to reflect a 6-week recall period (alpha = .60). Respondents rated items on a 5-point frequency scale (1 = always to 5 = never) representing the sum of the frequency of total reported errors. A higher scale score indicates increased HIV transmission potential through condom errors (e.g., condom breakage, slippage, etc.) among participants who reported condom use in the past 6 weeks and completed the measure at baseline, 6- and 12-weeks follow-up (Sanders, Graham, Yarber, & Crosby, 2003). A sample from the scale is “When you used condoms during the last 6 weeks, how often was the condom put on the wrong side up so that it had to be flipped over?”
Health-related partner verbal communication
The 9-item Health Protective Communication scale (Catania, 1998) (alpha= 0.71) assessed the quality of safer sex verbal communication between partners. Respondents rated items on a 4-point frequency scale (1=always, 4=never), with a low scale score indicating good communication quality. A sample item is “How often in the past 6 weeks have you told a new sex partner that you won't have sex unless a condom is used?” Health protective communication was assessed at baseline, 6-week and 12-week post-intervention. Only participants who reported a new sex partner in the past 6 weeks completed this measure.
Internalized Homophobia
The 23-item Homosexual Attitudes Inventory (Rosario, Hunter, Maguen, Gwadz, & Smith, 2001) (alpha=.86) was adapted to assess participants' attitudes toward and comfort with homosexuality, two constructs associated with internalized homophobia. Respondents rated items on a 4-point response scale (1= disagree strongly, 4=agree strongly) with high mean scores indicating positive attitudes regarding homosexuality. A sample item is “Homosexuality is not as good as heterosexuality.” Changes in this outcome were assessed at baseline, and 6- and 12-week follow-up.
Intervention acceptability
Intervention acceptability was assessed using the 8-item Abbreviated Acceptability Rating profile (Tarnowski & Simonian, 1992) (alpha= 0.91) adapted to reflect this intervention, and including 3 additional open-ended items. Respondents rated closed-ended items on a 6-point response scale (1 = strongly disagree, 6 = strongly agree), with higher scores indicating greater acceptability. Sample items include “This program has helped me change my behavior to keep myself safe from HIV and other STDs” and “Overall, I found this program helpful.” Acceptability was assessed at 12-week follow-up.
Sociodemographic characteristics
Sociodemographic data of study participants were collected at baseline, including age, race/ethnicity, sexual orientation, highest level of education, and history of incarceration. Also collected were data concerning age of sexual initiation and history of HIV testing.
Statistical Analyses
The descriptive analysis included an examination of frequencies, variable distributions, and measures of central tendency for sociodemographic characteristics, and cognitive and behavioral variables. Cronbach's alpha was used to assess internal consistency of multi-item scales. Comparisons between baseline characteristics of intervention and control groups were conducted using Chi-square tests for categorical variables and t-tests and Wilcoxon tests for parametric and non-parametric continuous variables, respectively. Multivariable analyses were used to control variables for which differences of p<0.15 at baseline existed, or that were considered potential confounders based on empirical evidence and prior literature. To control for baseline differences between groups, the baseline value of the outcome was controlled for in all analyses.
Generalized linear models (GLM) were used to assess intervention effects on primary and intermediate outcomes at follow-up, with link functions as appropriate based on the distribution of the outcome variable (e.g., logit link for binary outcomes, negative binomial for count outcomes, and identity for continuous outcomes). The Generalized estimating equation (GEE) extension of GLM was used to assess average differences between MyPEEPS and the control group over the entire 12-week follow-up period. GEEs have the advantage of accommodating correlation between repeated measurements on the same subjects over time, and make use of all available observations for patients with missing data at one or more time points. Controlled for in GEE models were baseline values of the outcome variable as a covariate and adjusted for age, race/ethnicity, time, and number of sessions attended. For consistency with other published literature, and to account for residual confounding due to baseline differences despite lack of statistically significant differences between groups at baseline, age and race/ethnicity were controlled for. Time period was included as a covariate to control for residual confounding due to secular trends, and total sessions was included to account for differences in level of exposure to the intervention.
All GEE models were initially fit with a group-by-time interaction to assess the effectiveness of the intervention in terms of the rate of change from baseline in the intervention group compared to the control group at 6- and 12-week follow-up. However, the interaction term was not significant for any of the outcomes, so it was excluded from the final GEE models. Thus, the interpretation of the GEE coefficients represents the overall difference between intervention and control groups over the entire 6- and 12-week follow-up period for an “average” participant, controlling for the baseline value of the outcome and all covariates. GEE effect estimates represent odds ratios estimated by logistic regression for binary outcomes, rate ratios estimated by negative binomial regression for count outcomes, and mean differences estimated by linear regression for continuous variables. All analyses were conducted using SAS version 9.2.
Results
Over 9 months 187 young people were screened, 140 of whom met eligibility criteria, and 109 completed baseline assessments. Eight cases were lost to follow-up, which resulted in 101 randomized cases. Most participants (85%) were randomized using a 1:1 allocation to intervention vs. time-matched active control. However, at three randomization time-points (equating to 15% of the sample), the cohort sizes were too small to allocate a sufficient amount of participants into both group conditions. Therefore, participants were allocated at the group-level (i.e., group condition was randomly selected into which all members of the cohort were then allocated), resulting in the slightly imbalanced overall allocation between conditions: 57% to the intervention (n=58) and 43% to the control (n=43) condition. Participants were reimbursed for their time following each study visit: $20 at baseline, $10 at each group session, an additional $10 for perfect 6-session attendance, $30 at 6-week follow-up, and $30 at 12-week follow-up; a total of up to $150. The sample's mean age was 18.8 years (SD = 1.2; range: 16-20.9) with a median age of 19 (IQR 18-20); 39% African American, 23% White, 27% Hispanic/Latino, and 12% other race/ethnicity.
Baseline Comparability of Groups
With the exception of controls exhibiting greater baseline health protective communication than those in the intervention group (p<.05), no other statistically significant group differences were observed between control and intervention groups at baseline. In addition, no statistically significant between group differences were observed according to age, race, or any of the primary and intermediate outcomes (Table 2).
Table 2. Baseline Characteristics by Intervention Group Assignment.
| Total N=101 | Intervention N=58 | Control N=43 | p-value* | |
|---|---|---|---|---|
|
| ||||
| No. (%) or mean (SD) | No. (%) or mean (SD) | No. (%) or mean (SD) | ||
|
| ||||
| Age | ||||
| Mean (SD) | 18.8 (1.2) | 18.6 (1.3) | 19.0 (1.1) | 0.134 |
| Median (IQR) | 19 (18-20) | 19 (17-20) | 19 (18-20) | |
|
| ||||
| Race/ethnicity | 0.315 | |||
| White | 23 (22.8) | 16 (27.6) | 7 (16.3) | |
| Black/African American | 39 (38.6) | 20 (34.5) | 19 (44.2) | |
| Hispanic/Latino | 27 (26.7) | 17 (29.3) | 10 (23.3) | |
| Other race (including multiracial) | 12 (11.9) | 5 (8.6) | 7 (16.3) | |
|
| ||||
| Education | 0.190 | |||
| < HS | 48 (47.5) | 25 (43.1) | 23 (53.5) | |
| HS/GED | 30 (29.7) | 16 (27.6) | 14 (32.6) | |
| Some college or college degree | 23 (22.8) | 17 (29.3) | 6 (14.0) | |
|
| ||||
| Employed at baseline (yes vs. no) | 44 (43.6) | 27 (46.6) | 17 (39.5) | 0.482 |
|
| ||||
| Ever incarcerated at baseline (yes vs. no) | 11 (10.9) | 5 (8.6) | 6 (13.9) | 0.521 |
|
| ||||
| ≥2 sex partnersǂ (vs. 0-1 partner) | 24 (24.0) | 10 (17.5) | 14 (32.6) | 0.082 |
|
| ||||
| Any anal sexǂ (yes vs. no) | 67 (67.0) | 34 (59.7) | 33 (76.7) | 0.072 |
|
| ||||
| Any unprotected anal sexǂ (yes vs. no) | 36 (36.0) | 19 (33.3) | 17 (39.5) | 0.522 |
|
| ||||
| Sex under influence of alcohol/drugsǂ (yes vs. no) | 22 (22.0) | 10 (17.5) | 12 (27.9) | 0.216 |
|
| ||||
| Unprotected sex under influence of alcohol/drugsǂ (yes vs. no) | 14 (14.0) | 7 (12.3) | 7 (16.3) | 0.568 |
|
| ||||
| Self-efficacy for Safer Sex (continuous) | 45.1 (4.0) | 45.0 (3.7) | 45.3 (4.3) | 0.651 |
|
| ||||
| Situational Temptation for Safer Sex (continuous) | 18.7 (5.3) | 18.8 (5.4) | 18.5 (5.1) | 0.734 |
|
| ||||
| Condom Errors (continuous) | 0.68 (0.43) | 0.72 (0.46) | 0.66 (0.41) | 0.614 |
|
| ||||
| Health Protective Communication (continuous) | 16.4 (5.1) | 18.8 (4.6) | 14.1 (4.5) | 0.016 |
|
| ||||
| Homosexual Attitudes Inventory (continuous) | 56.1 (10.2) | 55.7 (10.4) | 56.6 (10.1) | 0.676 |
Assessed by Chi-Square tests for categorical variables and Wilcoxon tests for continuous variables.
Timeframe for sexual behavior variables is past 6 weeks
Attrition
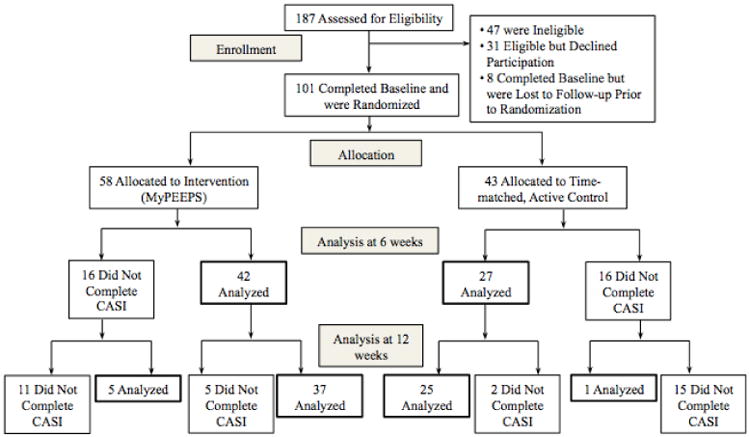
On average, 62% of MyPEEPS participants attended 3 or more sessions (compared to 42% of controls). Randomization and follow-up are illustrated in Figure 1. No statistically significant proportional differences were observed between intervention and control group participants that completed 6-week (72.4% vs. 62.8%, p=0.31) and 12-week follow-up (72.4% vs. 60.5%, p=0.21). Overall, 61.4% (62/101) of the sample was assessed at both 6 and 12 weeks, and 74.3% (75/101) had any follow-up.
Figure 1. Randomization and Follow-up Diagram.
Feasibility and Acceptability
Participants rated MyPEEPS as moderately acceptable (mean= 24.7; SD=13.6; range: 8-48). Slightly over half the sample (52%) indicated the program was a “good way to learn about HIV and STDs and how to prevent them,” 55% found the program helpful, and half agreed that the program positively influenced their safer sex behavior. In spite of moderate acceptability ratings, the majority of responses to open-ended acceptability items was positive and generally highlighted relational aspects of the intervention (e.g., “meeting other people,” “friendly” facilitators), and described the intervention as “informative” and “entertaining; 6 cases shared disliking the intervention due to its far distance from their home, its “long questionnaire,” and the “small” cohort sizes.
Primary Outcomes
Compared to the active control at 12-week follow-up, MyPEEPS participants reported lower odds of any sex under the influence of alcohol or drugs (OR=0.35; 95% CI 0.10-1.19, p=0.093), and unprotected sex under the influence of alcohol or drugs (OR=0.21; 95% CI 0.04-1.13, p=0.069) though the associations were statistical trends. When both follow-up periods were collapsed, these outcomes persisted in favoring MyPEEPS: sex under the influence of alcohol or drugs (aOR=0.35; 95% CI 0.12-0.99, p=0.048), and unprotected sex under the influence of alcohol or drugs (aOR=0.23; 95% CI 0.05-1.15, p=0.075), controlling for age, race/ethnicity, time, number of sessions attended, and baseline outcome value. Results were virtually unchanged when number of sessions was excluded from the model: for sex under the influence (aOR=0.35, 95% CI 0.12-1.02; p=0.055), and for unprotected sex under the influence (aOR=0.24, 95% CI 0.05-1.18; p=0.079). No intervention effects were observed on unprotected anal sex, total number of sex partners, or total number of unprotected anal sex acts with male partners at 6-, 12-week, or overall follow-up periods (Table 3).
Table 3. Effects of the Intervention on Primary and Intermediate Outcomes at 6 and 12 weeks.
| Intervention, N=58 | Control, N=43 | Effect Estimates | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted No. (%) or Mean (SD) | Unadjusted No. (%) or Mean (SD) | 6-weeks vs. Baseline | 12-weeks vs. Baseline | Overall follow-up period | |||||
| Baseline | 6 week | 12 week | Baseline | 6 week | 12 week | Estimateǂ (95% CI) | Estimateǂ (95% CI) | Estimateǂǂ (95% CI) | |
| n | 58 | 42 | 43 | 43 | 33 | 31 | |||
| Unprotected anal sex | 19 (33.3) | 9 (21.4) | 11 (25.6) | 16 (37.2) | 7 (21.2) | 8 (25.8) | 1.09 (0.35-3.41) | 1.06 (0.36-3.10) | 1.11 (0.42-2.91) |
| No. unprotected anal sex acts with male partners (count)¶ | 0.96 (2.4) | 0.52 (1.5) | 1.12 (2.9) | 1.5 (3.6) | 0.91 (2.9) | 1.2 (2.3) | 0.48 (0.10-2.18) | 0.61 (0.13-2.96) | 0.37 (0.10-1.44) |
| Total no. sex partners | 1.0 (1.8) | 0.98 (1.6) | 0.90 (1.3) | 1.4 (1.5) | 1.1 (1.9) | 1.1 (1.7) | 0.91 (0.48-1.70) | 0.84 (0.45-1.55) | 0.96 (0.52-1.79) |
| Sex under the influence of alcohol/drugs | 10 (17.5) | 5 (11.9) | 5 (11.6) | 12 (27.9) | 8 (24.2) | 9 (29.0) | 0.55 (0.15-2.04) | 0.35 (0.10-1.19)ǂ | 0.35 (0.12-0.99)* |
| Unprotected sex under the influence of alcohol/drugs | 7 (12.3) | 2 (4.8) | 2 (4.7) | 7 (16.3) | 4 (12.1) | 6 (19.4) | 0.33 (0.04-2.43) | 0.21 (0.04-1.13)ǂ | 0.23 (0.05-1.15)ǂ |
| Intermediate Outcomes | |||||||||
| Self-efficacy for Safer Sex | 45.0 (3.7) | 46.6 (3.5) | n/a | 45.3 (4.3) | 45.5 (4.7) | n/a | 1.17 (-0.51-2.86) | n/a | n/a |
| Situational Temptation for Safer Sex | 18.8 (5.4) | 16.8 (5.9) | 15.8 (6.2) | 18.5 (5.1) | 16.7 (6.4) | 16.7 (6.0) | 0.31 (-2.33-2.95) | -0.78 (-3.39-1.84) | -0.92 (-3.27-1.44) |
| Condom Errors | 0.72 (0.46) | 0.55 (0.50) | 0.56 (0.52) | 0.66 (0.41) | 0.58 (0.43) | 0.74 (0.48) | -0.08 (-0.27-0.11) | -0.21 (-0.54-0.13) | -0.10 (-0.32-0.11) |
| Health Protective Communication | 18.8 (4.6) | 19.4 (5.0) | 17.3 (5.9) | 14.1 (4.5) | 17.3 (4.3) | 18.8 (4.7) | 5.42 (-2.04-12.9) | -4.40 (-16.6-7.77) | 0.09 (-4.92-5.11) |
| Homosexual Attitudes Inventory | 55.7 (10.4) | 71.1 (16.4) | 73.5 (15.4) | 56.6 (10.1) | 69.8 (16.6) | 72.7 (15.3) | 1.81 (-5.55-9.18) | 0.97 (-6.09-8.03) | -0.44 (-6.39-5.51) |
p<0.05;
p<0.10
Effects estimates represent odds ratios estimated by logistic regression for binary outcomes, rate ratios estimated by negative binomial regression for count outcomes, and mean differences estimated by linear regression for continuous variables. All models include the baseline value of the outcome as a covariate.
GEE estimates represent the average effect over the entire evaluation period and account for correlation between observations within subjects over time. All models adjusted for baseline value of outcome, time, age at baseline, race/ethnicity, and total number of sessions attended.
Among those reporting any anal sex at baseline, n=67
Intermediate Outcomes
No statistically significant differences were found between conditions on intermediate outcome variables, though trends tended to be in the expected direction (Table 3). For example, compared to controls, intervention group participants had greater self-efficacy for safer sex at 6 weeks, and both lower situational temptation for safer sex and fewer condom errors at 12 weeks, adjusted for baseline values of these outcomes.
Discussion
This pilot study is the first to develop and evaluate initial efficacy, feasibility, and acceptability of a group-level behavioral intervention designed to address HIV risk behavior in an ethnically-diverse sample of MSM younger than those sampled in previous intervention trials (i.e., aged 16-20). This was also the first known pilot to include young MSM under age 18 using a randomized controlled design with an active, time matched control group that provided sexual health education (i.e., in a didactic, less interactive and culturally-tailored manner than the intervention condition).
Intervention acceptability measures were only administered at 12-week follow-up and satisfaction data are missing from 16 participants who did not complete the final assessment. The MyPEEPS intervention appeared feasible to run among young MSM as evidenced by the recruitment and enrollment of 101 participants over a 9 month period, a fair degree of session attendance (62% attending at least 3 sessions), and retention at follow-up (over 60%).
Primary and intermediate outcomes were measured at 6- and 12-week post-intervention follow-up. In comparison to controls, MyPEEPS intervention participants reported a significant reduction in any sex (e.g., anal or oral) under the influence of substances, and a marginal reduction in unprotected anal intercourse while under the influence of substances. Though non-significant, also observed were adaptive changes to intermediate risk factors that favored the intervention. These adaptive trends suggest promise for the intervention components included in MyPEEPS. Greater between-group differences were likely attenuated by the time-matched active control also related to safer sex education.
As previously described, the MyPEEPS pilot intervention curriculum was developed largely from qualitative interview data of HIV-positive young MSM. These data informed key aspects of the intervention including its content and activities, its modular design, and its format and delivery. Therefore, the effects of this intervention also illustrate advantages of utilizing qualitative approaches to develop EBI for young MSM.
Limitations
Several limitations to this study should be noted. First, the validity of these findings is contingent upon the accuracy of participant retrospective self-report, which is an unavoidable concern in most research on sexual behavior. Also, this study was limited in detecting intervention effects on risk behaviors linked to HIV infection (e.g., unprotective receptive anal intercourse, use of certain substances during sex) as other studies have done (Celentano et al., 2006). This was due to the questionnaire not including items that examined various sexual behaviors (e.g., insertive versus receptive anal intercourse) or inquiring about specific substances used during sex (e.g., marijuana versus cocaine use).
Furthermore, the non-probabilistic method of sampling in LGBT community venues limits this pilot's results from generalizing to all 16 to 20 year-old, young MSM, especially those whom may not partake in activities organized by LGBT community venues (Meyer & Wilson, 2009). Another limitation is the pilot's relatively short period between two follow-up assessments (i.e., 6 weeks), which prevented the measurement of long-term intervention effects. Last, it can be surmised that varying degrees of housing and financial instability present in this young population, and somewhat reflected in this sample (e.g., 10% reported a history of incarceration), may have contributed to one in four enrollees not completing both of the pilot's follow-up assessments. Significant differences were not observed among those with complete vs. incomplete follow-up data on factors related to treatment group assignment, participant demographics, or baseline risk behaviors; however, the significant attrition observed across assessment points may limit the study's generalizability.
Future Research
These results suggest areas of further development of MyPEEPS. First, a future trial of MyPEEPS should examine risk behavior with greater dimensionality (e.g., insertive vs. receptive anal sex, itemization of substances used during sex, etc.) (Celentano et al., 2006). Another priority should be to improve MyPEEPS acceptability using formative techniques (e.g., focus groups) involving young MSM, aged 16-20, from whom qualitative data can inform the increased acceptability and refinement of the intervention – an effective method recently employed to refine a behavioral intervention involving young MSM (Pachankis, Lelutiu-Weinberger, Golub, & Parsons, 2013).
Given the exploratory mechanism by which this pilot was funded, it did not include an individual post-intervention counseling component (i.e., “booster” visit), which can assist participants in reviewing relevant health protective information (Mustanski, Garofalo, Monahan, Gratzer, & Andrews, 2013). This study's findings support the compulsory inclusion of booster visits in a future iteration of MyPEEPS given slight increases in rates of unprotected anal intercourse reported between follow-up visits.
This exploratory pilot represents an important step toward filling a void in current EBI targeting young MSM. The Centers for Disease Control and Prevention (CDC) endorse a four-tiered conceptual framework outlining criteria for highly rigorous EBI (i.e., Tiers I and II). None of the relatively few MSM-focused Tier I and II EBI included in CDC's compendium of EBI targets young MSM under age 18 (CDC, 1999; Kay et al., 2003). MyPEEPS shows promise toward meeting Tier II criteria although one shortcoming involved statistical significance, which can be attributed to inadequate power in the sample. It is estimated that a sample size of at least 160 (n=80 per condition) would ensure 80% probability of detecting significant intervention effects in outcomes similar to those examined in this pilot.
Conclusions
High rates of HIV infection in young MSM under 18, especially in African Americans, Latinos and Whites, underscore the need for efficacious group-level EBI developed for this population. Participation in the MyPEEPS intervention contributed to a decline in sexual activity while under the influence of alcohol or drugs, and while non-significant, other intermediate risk factors favored the intervention (over a time-matched active control) and suggested its ability to reduce HIV risk in young MSM aged 16-20. The MyPEEPS intervention also demonstrated modest acceptability. Future studies should examine intervention efficacy on a larger sample of young MSM aged 16-20.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the contributions of Mr. Roger Fierro, Mr. John Thompson, and Drs. Christopher Cotten and Geri Donenberg. The project described was supported by Award Number R34 MH079707 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
References
- Bandura A. Social cognitive theory and exercise control of HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and methods of behavioral interventions. New York: Plenum Press; 1994. [Google Scholar]
- Berkel C, Mauricio AM, Schoenfelder E, Sandler IN. Putting the pieces together: An integrated model of program implementation. Prevention Science. 2011;12(1):23–33. doi: 10.1007/s11121-010-0186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempo DE, D'Augelli AR. Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths' health risk behaviors. Journal of Adolescent Health. 2002;30:364–374. doi: 10.1016/s1054-139x(01)00415-3. [DOI] [PubMed] [Google Scholar]
- Catania JA. The health protective communication scale. In: Davis CM, Yarber WL, Bauserman R, Schreer G, Davis SL, editors. Handbook of sexuality-related measures. Thousand Oaks, CA: Sage Publications; 1998. pp. 544–546. [Google Scholar]
- CDC. Compendium of HIV prevention intervenions with evidence of effectiveness. 1999 Retrieved from Centers for Disease Control and Prevention website: http://www.cdc.gov/hiv/pdf/prevention_research_compendium.pdf.
- CDC. Estimated HIV incidence in the United States, 2007-2010. HIV Surveillance Supplemental Report. 2012a;17(4) Retrieved from Centers for Disease Control and Prevention website: http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. [Google Scholar]
- CDC. Vital Signs: HIV infection, testing, and risk behaviors among youths - United States. MMWR. 2012b;61(47):971–976. Retrieved from Centers for Disease Control and Prevention website: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6147a5.htm. [PubMed] [Google Scholar]
- CDC. HIV among gay, bisexual, and other men who have sex with men. 2013 Retrieved from Centers for Disease Control and Prevention website: http://www.cdc.gov/hiv/pdf/risk_HIV_among_AA_Gay_other.pdf.
- Celentano DD, Valleroy LA, Sifakis F, MacKellar DA, Hylton J, Thiede H, et al. Torian LV. Associations between substance use and sexual risk among very young men who have sex with men. Sexually Transmitted Diseases. 2006;33(4):265–271. doi: 10.1097/01.olq.0000187207.10992.4e. [DOI] [PubMed] [Google Scholar]
- Crosby RA, Sanders SA, Yarber WL, Graham CA, Dodge B. Condom use errors and problems among college men. Sexually Transmitted Diseases. 2002;29(9):552–557. doi: 10.1097/00007435-200209000-00010. [DOI] [PubMed] [Google Scholar]
- Diaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: Data from a probability sample of Latino gay men in three U.S. cities. Cultural Diversity and Ethnic Minority Psychology. 2004;10:255–267. doi: 10.1037/1099-9809.10.3.255. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(6):642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elford J, Hart G. If HIV prevention works, why are rates of high risk sexual behavior increasing among MSM? AIDS Education and Prevention. 2003;15(4):294–308. doi: 10.1521/aeap.15.5.294.23825. [DOI] [PubMed] [Google Scholar]
- Gardner M, Steinberg L. Peer influence on risk taking, risk preference, and risky decision maknig in adolescence and adulthood: An experimental study. Developmental Psychology. 2005;41(4):625–635. doi: 10.1037/0012-1649.41.4.625. [DOI] [PubMed] [Google Scholar]
- Garofalo R, Herrick A, Mustanski B, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health. 2007;97:1113–1117. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Mustanski B, McKirnan DJ, Herrick A, Donenberg GR. Methamphetamine and young men who have sex with men: Understanding patterns and correlates of use and the association with HIV-related sexual risk. Archives of Pediatrics & Adolescent Medicine. 2007;161:591–596. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Wolf CR, Kessel S, Palfrey J, DuRant RH. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101:895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- Goodenow C, Szalacha L, Westheimer K. School support groups, other school factors, and the safety of sexual minority adolescents. Psychology in the Schools. 2006;43(5):573–589. [Google Scholar]
- Harper GW. Sex isn't that simple: culture and context in HIV prevention interventions for gay and bisexual male adolescents. American Psychologist. 2007;62(8):803–819. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]
- Harper GW, Jernewall N, Zea MC. Giving voice to emerging science and theory for lesbian, gay, and bisexual people of color. Cultural Diversity and Ethnic Minority Psychology. 2004;10(3):187–199. doi: 10.1037/1099-9809.10.3.187. [DOI] [PubMed] [Google Scholar]
- Harper GW, Schneider M. Oppression and discrimination among lesbian, gay, bisexual, and Transgendered people and communities: a challenge for community psychology. American Journal of Community Psychology. 2003;31(3-4):243–252. doi: 10.1023/a:1023906620085. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms JE. Black and White racial identity: Theory, research, and practice. Westport, CT: Greenwood Press; 1990. [Google Scholar]
- Herbst JH, Beeker C, Mathew A, McNally T, Passin WF, Kay LS, et al. Services, Task Force on Community Preventive. The effectiveness of individual-, group-, and community-level HIV behavioral risk-reduction interventions for adult men who have sex with men: A systematic review. American Journal of Preventive Medicine. 2007;32(4S):S38–S67. doi: 10.1016/j.amepre.2006.12.006. [DOI] [PubMed] [Google Scholar]
- Hidalgo MA, Cotten C, Johnson AK, Kuhns L, Garofalo R. “Yes, I am more than just that”: Gay/bisexual young men residing in the US discuss the influence of minority stress on their sexual risk behavior prior to HIV infection. International Journal of Sexual Health. 2013;25(4):291–304. doi: 10.1080/19317611.2013.818086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner DM, Davis MC, Nemeroff CJ, Aiken LS. The impact of internalized homophobia on HIV preventive interventions. American Journal of Community Psychology. 2002;30(3):327–348. doi: 10.1023/A:1015325303002. [DOI] [PubMed] [Google Scholar]
- Jones KT, Gray P, Whiteside YO, Wang T, Bost D, Dunbar E, et al. Johnson WD. Evaluation of an HIV prevention intervention adapted for Black men who have sex with men. American Journal of Public Health. 2008;98(6):1043–1050. doi: 10.2105/AJPH.2007.120337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay LS, Crepaz N, Lyles CM, Griffin T, Patterson J, Sherba T. Update of the compendium of HIV prevention interventions with evidence of effectiveness; Paper presented at the National HIV Prevention Conference; Atlanta, GA. 2003. [Google Scholar]
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: A community-level HIV prevention intervention for young gay men. American Journal of Public Health. 1996;86(8):1129–1136. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Chesney M, Coates T. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. The Lancet. 2004;364(9428):41–50. doi: 10.1016/S0140-6736(04)16588-4. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36:38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress and mental health in Lesbian, Gay and Bisexual Populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dean L. Patterns of sexual behavior and risk taking among young New York City gay men. AIDS Education and Prevention. 1995;7(Supple):13–23. [PubMed] [Google Scholar]
- Meyer IH, Wilson PA. Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology. 2009;56(1):23–31. doi: 10.1037/a0012844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS and Behavior. 2008;12:118–126. doi: 10.1007/s10461-007-9335-3. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Monahan C, Gratzer B, Andrews K. Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: the Keep It Up! intervention. AIDS and Behavior. 2013;17(9):2999–3012. doi: 10.1007/s10461-013-0507-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: A review of epidemiological, risk and protective factors, and interventions. Journal of Sex Research. 2011;48(2):218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadal KL, Issa M, Leon J, Meterko V, Wideman M, Wong Y. Sexual orientation microaggressions: “Death by a thougsands cuts” for lesbian, gay, and bisexual youth. Journal of LGBT Youth. 2011;8(3):234–259. [Google Scholar]
- Newcomb ME. Moderating effect of age on the assocation between alcohol use and sexual risk in MSM: Evidence for elevated risk among younger MSM. AIDS and Behavior. 2013:1–9. doi: 10.1007/s10461-013-0470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sexual Behavior. 2011;40(1):189–199. doi: 10.1007/s10508-009-9573-8. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Lelutiu-Weinberger C, Golub SA, Parsons JT. Developing an online health invervention for young gay and bisexual men. AIDS and Behavior. 2013;17:2986–2998. doi: 10.1007/s10461-013-0499-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Borkowski T, Bimbi D. Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. Journal of Adolescence. 2000;23:377–391. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- Pedlow CT, Carey MP. Developmentally-appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Annals of Behavioral Medicine. 2004;27(3):172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Hunter J, Maguen S, Gwadz M, Smith R. The coming-out process and its adaptational and health-related associations among gay, lesbian and bisexual youths: Stipulation and exploration of a model. American Journal of Community Psychology. 2001;29:133–160. doi: 10.1023/A:1005205630978. [DOI] [PubMed] [Google Scholar]
- Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123:346–352. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, et al. Mayer KH. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: IMplications for age-specific interventions. AIDS and Behavior. 2009;13(811-821):811. doi: 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders SA, Graham CA, Yarber WL, Crosby RA. Condom use errors and problems among young women who put condoms on their male partners. Journal of the American Medical Women's Association. 2003;58(2):95–98. [PubMed] [Google Scholar]
- Steinberg L. A social neuroscience perspective on adolescent risk-taking. Developmental Review. 2008;28(1):78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarnowski KJ, Simonian SJ. Accessing treatment acceptability: The abbreviated acceptability rating profile. Journal of Behavior Therapy and Experimental Psychiatry. 1992;23:101–106. doi: 10.1016/0005-7916(92)90007-6. [DOI] [PubMed] [Google Scholar]
- Thiede H, Valleroy LA, MacKellar DA, Celentano DD, Ford WL, Hagan H, et al. Torian LV. Regional patterns and correlates of substance use among young men who have sex with men in 7 US urban areas. American Journal of Public Health. 2003;93(11):1915–1921. doi: 10.2105/ajph.93.11.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner L, Klausner JD, Rietmeijer CA, Malotte CK, O'Donnell L, Margolis AD, et al. O'DOnnell CR. Effects of a brief video intervention on incident infection among patients attending sexually transmitted disease clinics. PLoS Medicine. 2003;5(6):0919–0927. doi: 10.1371/journal.pmed.0050135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson BDM, Miller RL. Examining strategies for culturally grounded HIV prevention: A review. AIDS Education and Prevention. 2003;15(2):184–202. doi: 10.1521/aeap.15.3.184.23838. [DOI] [PubMed] [Google Scholar]
- Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, et al. Carey JW. Efficacy of an HIV/STI prevention intervention for Black men who have sex with men: Findings from the Many Men, Many Voices (3MV) Project. AIDS and Behavior. 2009;13:532–544. doi: 10.1007/s10461-009-9529-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


