Abstract
Background
Suicidality risk-factors between countries with similar economic and religious background have been rarely compared, especially within genders.
Methods
Lifetime prevalence of suicide ideation, plans, and attempts in the ESEMeD surveys were stratified on four separate groups: French women, Spanish women, French men, Spanish men. Outcome odds-ratios (OR) were modelled within each group using logistic regression including demographic characteristics, lifetime mood/anxiety disorders, parental bonding, marital status, and health service-use.
Results
Lifetime prevalence of suicide attempts was 3.4% in France (1.1% men, 5.4% women) and 1.5% in Spain (1.2% men, 1.7% women), with a significantly greater gender difference in France (p=0.001). Regarding risk-factors, French women reported suicide attempt more commonly with authoritarian mothers (OR=1.51; 95%CI=1.04–2.18), unlike Spanish women (OR=0.77; 95%CI=0.51–1.15) (p<0.001). Spanish men showed more than eight-times higher odds of suicide attempt with overprotecting mothers than French men (p=0.03). General practitioner-(GP)-use was significantly protective of suicide attempt among Spanish women (OR=0.08; 95%CI=0.02–0.35) with no effect in French women (OR=1.03; 95%CI=0.54–2.00) (p=0.01). No significant differences in the effect of marital status, any lifetime antidepressant use, mental disorders, or religiosity on suicide attempt were observed between France and Spain within gender-stratum.
Limitations
Parental bonding is retrospective and potentially influenced by mental state. Response rate was considerably lower in France than in Spain.
Conclusions
Suicidality risk-factors play different roles across genders between France and Spain. Parental bonding dimensions may be interpreted differently according to country, underlining cultural importance. As recommended by WHO, mental health decisions must involve GPs in conjunction with psychiatrists or psychologists.
Keywords: suicide, suicidal attempt, suicidal thought, epidemiology, survey, mental health
INTRODUCTION
When suicide rates are compared within Europe, and more specifically within the European Union (EU) member states (WHO, 2005), large between-country variation is observed with rates ranging from as high as 37.0 per 100,000 in Lithuania to as low as 3.1 in Greece. Although some inconsistencies between countries as to how suicides are recognized, collected and classified from death certificates are suspected, this alone does not explain such large differences in suicide rates.
Suicide has been usually studied and compared cross-culturally using risk-factors at the macro-level; such as religion, economic conditions, historical traditions, and access to mental health care. For instance, some religions, mainly Catholic and Muslim faiths, strongly prohibit suicidal behaviour and suicide. For Muslim countries, it has been suggested that reports of suicide could be concealed under other violent deaths. (Pritchard and Amanullah, 2007) For catholic countries, mostly in Southern European, some of the lowest suicide rates in Europe have been reported (Gearing and Lizardi, 2009), notwithstanding notable exceptions in Portugal and Poland (WHO, 2005). Another study claims that certain cultural elements, such as alcohol use and ancestral production of alcohol, also influence suicide rates. (Marusic and Farmer, 2001) Increasing access to preventative measures, such as health care and suicide prevention programs, and decreasing access to lethal means have led to significant reduction in suicide. (Mann et al., 2005)
Within a different context, many risk-factors at the individual-level have been identified with suicide. Psychological autopsies found that the major underlying cause of suicide was mental health disorders, including depressive disorders, substance use disorders, and impulsivity. (Bernal et al., 2007, Hawton and van Heeringen, 2009) Family adversity and physical illness are also events that have been associated with suicide-related death. (Cavanagh et al., 1999) Finally, it should be noted that religious practice itself has been strongly linked to other protective factors against suicide, namely lower divorce rates and less likely being alcoholic. (Berggren, 1997, Lambert et al., 2010)
The aim of the study herein was to compare the prevalence and correlates of suicidality at the individual level and to contrast these correlates with macro-level trends. In order to limit large macro-level differences, we selected two neighbouring countries – Spain and France – based on their similar religious, Catholic backgrounds and economic environments. Despite these similarities, all-cause suicide mortality rates were substantially different between Spain and France in 2005, at 9.6 and 22.9 per 100 000, respectively. (WHO, 2005) These differences were parallel among both females (Spain: 4.5 vs France: 11.8) and males (Spain: 14.8 vs France: 35.1), with a higher relative rate of suicide among women than men. Moreover, other causes of death, under which suicide could be hidden, were unable to provide an explanation for these discrepancies, with higher deaths rates in France than Spain, respectively, for injury or poison by external causes (48.1 vs 31.7), undetermined intention (0.8 vs 0.2), accidental falls (11.5 vs 5.0), and undetermined cause (32.7 vs 12.4). (WHO, 2005) These countries also have remarkable suicide rate trends from 1974/1976 to 1999/2000, in which rates for both countries exhibited increases in not only absolute values, but also rank among developed countries by three places. (Hansen and Pritchard, 2008) Highly refined comparisons are then required to determine risk-factors that shed light on these differences at the micro-level through the careful study of suicidal behaviours. This was possible using the European Study of the Epidemiology of Mental Disorders (ESEMeD), a part of the World Mental Health Surveys, which comprises of several population-based surveys including structured psychiatric interviews in six European countries, measuring, among others, the presence of mental disorders, suicidal behaviour, religious affiliation, social factors, use of case, and parental-bonding. The last being of recent importance, as our study group has demonstrated an increased risk of suicidality to the quality of parental bonding, such as low maternal and paternal care. (Heider et al., 2007)
In order to study risk-factors related to suicide, we used the endpoints of suicidal attempt, plans and thoughts, as is the case for most psychiatric epidemiological surveys. Indeed, there is gender paradox in suicidality, in which suicidal ideation is higher in women than men while mortality from suicide is lower in women than men. Regardless, these outcomes have been associated with a number of mental health disorders, such as depression for ideation and anxiety or poor impulse control for attempts (Nock et al., 2008), thereby rendering such data suitable to study suicide.
METHODS
Study sample
The European study of the Epidemiology of Mental Disorders (ESEMeD) was a cross-sectional, population-based, household survey in a representative sample of adults from 6 European countries (Belgium, France, Germany, Italy, the Netherlands, and Spain). As a part of the WHO World Mental Health (WMH) Surveys Initiative (http://www.hcp.med.harvard.edu/wmh/), the survey’s aim was to assess the prevalence of common mental disorders as well as their correlates and use of services. Respondents underwent a face-to-face, computer-assisted personal interview, conducted by a trained interviewer, speaking in lay terms. A stratified multi-stage random sample without replacement was drawn in each country. The sampling frame and the number of sampling stages used to obtain the final sample differed across countries. The target population was represented by non-institutionalized adults (aged 18 years or older) identified from a national household list or a list of residents in each country. This list was obtained from the census, local postal registries, or in the case of France from telephone lists. Additional details about sampling are provided elsewhere. (Alonso et al., 2004)
After receiving a complete description of the study, all respondents provided written informed consent. Questions were administered at home by trained interviewers who used a computer-assisted personal interview (Robins et al., 1988). The interview was conducted in two phases. In the first phase, all respondents were screened for the most common mood and anxiety disorders. Only those who presented symptoms of specific mood and anxiety disorders, and a random sample of 25% of respondents who did not, entered the second phase of the interview, which included in-depth questions about additional mental disorders, mental health service use, as well as demographic, lifestyle features, and religious beliefs. Data were obtained from 21,425 respondents between January 2001 and July 2003. The overall response rate was 78.6% in Spain and 45.9% in France. The sample was weighted to take into account different selection probabilities within countries, specific age and gender distributions of the general population in each country, and the relative population sizes between countries. In this study, we report data from the sample in Part II only (including 2,121 respondents from Spain and 1,434 from France), which is referred to as “the overall sample” in the text.
Demographic variables
Respondents were asked questions on several demographic variables, including age at interview and the total years of schooling. Respondents were also asked if they were currently working and if not, for what reason(s). Unemployment was then defined as any person not working, excluding persons on sick-leave or with any other health condition preventing them to work.
Assessment of mental disorders
The lifetime presence of mood, anxiety, and alcohol use disorders was determined by diagnostic criteria defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 1994). Organic exclusion rules were imposed in making all diagnoses. The WHO CIDI 3.0 Field Trials and later clinical calibration studies have shown that all these disorders could be assessed with acceptable reliability and validity using the CIDI (Wittchen, 1994). More recent reappraisals carried out in four WMH countries (US, Italy, Spain, and France, with total N=468) have demonstrated good agreement between CIDI-3.0 diagnoses and diagnoses based on blinded re-interviews, with the area under the receiver operator characteristics curve ranging between 0.73 – 0.93 for lifetime mood/anxiety disorders, and 0.83 – 0.88 for 12-month mood/anxiety disorders (Haro et al., 2006).
Religiosity
Subjects were asked five questions on religiousness. These covered the presence or absence of religious beliefs and, for subjects who claimed a religion, extent of religious practice and intrinsic religiosity (Pickard, 2006). Three variables were computed: attending religious services weekly (“weekly practice” dimension), often using religion as problem solving tool (“problem solving” dimension), and if religion is very important in daily life (“importance” dimension). A more complete description of these dimensions is provided in a previous publication. (Kovess-Masfety et al., 2010)
Parental bonding
The Parental Bonding Instrument (PBI) measures fundamental parental styles according to the scales of control and overprotection. (Cox et al., 2000) The original PBI (Heider et al., 2008) was intended to measure the perceived parental rearing styles of overprotection and care as remembered by the respondents during their first 16 years of life. It consists of 25 items to be assessed separately for mother and father. In a number of studies, the PBI proved to be a reliable and valid measure of actual, and not merely perceived, parenting. In a previous study, the authors were also able to confirm this three-factor structure for the nine-item short-form of the PBI used in the ESEMeD (Heider et al., 2008): maternal/paternal care, overprotection and authoritarianism
Antidepressant use
All respondents were asked in a face-to-face interview about the use of antidepressants (tricyclic antidepressants, selective serotonine reuptake inhibitors, monoamine oxidase A inhibitors, non-selective monoamine oxidase inhibitors, non-selective monoamine reuptake inhibitors, etc.) during the last 12 months. A full list of antidepressants is available in another publication. (Demyttenaere et al., 2008) A standardized booklet containing pictures of each antidepressant was provided as a reference to assist recalling use.
Suicidality
Specific questions were asked on any lifetime ideation, plans and attempts of suicide. Among those who attempted suicide, three questions assessed the severity of the attempt: (1) I made a serious attempt to kill myself and it was only luck that I did not succeed; (2) I tried to kill myself, but knew that the method was not full-proof; (3) My attempt was a cry for help. I did not intend to die. Based on evidence that reports of such embarrassing behaviours are higher in self-administered than interviewer-administered surveys (Turner et al. 1998), these questions were printed in a self-administered booklet and referred to by letter. Interviewers asked respondents to report whether the experiences ever happened to them and if so, to report the age of onset and their recency.
Statistical Analysis
Analyses were stratified on four separate gender and country groups: 1) French women, 2) Spanish women, 3) French men, and 4) Spanish men. Prevalence of each suicide variable (ideation, plan, and attempt) was reported with 95% CI according to gender and country group. In order to test our research questions, we built three different logistic regression models. First, a bivariate logistic regression model (accounting for survey design) was build, including country, gender, and the interaction term between gender and country as independent variables and each suicide variable as a dependent variable. Statistical significance of 2nd order interactions was then tested using a t-test based on the linearized standard error of the interaction effect. Second, a multivariable logistic model was estimated including lifetime mood or anxiety disorders, parental bonding, marital status, and service-use variables (general practitioner, psychiatrist, or other health service use) as covariables. ORs and 95% CI for reporting suicide ideation and attempts were then calculated for each gender and country group. Differences between countries were then compared within gender-stratum by including an interaction term of the risk-factors and country in the multivariable model and testing its significance using a t-test. Sensitivity analysis of the suicide attempt variables was performed in which only serious suicide attempts were used as the dependent variable. Similar results were obtained, yet power was substantially lowered due to the reduced prevalence (2-times decrease for all gender and country groups). Third, religion was added as a risk-factor to the above multivariable logistic model and county differences were then compared within gender strata. Since data on religiosity are available on a smaller proportion of persons, separate multivariable logistic models were estimated and were adjusted for any lifetime mood or anxiety disorder, parental bonding, marital status, and service-use variables. Differences between countries within each gender stratum were then tested as above.
Age at first suicide attempt was summarized for each country within gender-stratum using median and interquartile range (IQR) and weighted by survey selection probability. Distributions of age at first suicide attempt were then examined using a kernel density plot for each country and gender group.
A multivariable logistic model accounting for survey design was estimated using age (≤ 35 or >35), year of education, unemployment status, any lifetime mood or anxiety disorder, parental bonding index, marital status, any lifetime use of antidepressants, and psychiatrist, general practitioner or other health service use. All analyses were performed using STATA statistical software (v11.0, College Station, TX, USA) and significance was defined as a p-value < 0.05.
RESULTS
Suicidality prevalence in France and Spain from the ESEMeD study
The prevalence of suicide ideation, plan, and attempt are reported for each country and gender group in Table 1. In France, lifetime prevalence of suicide ideation was estimated at 12.4% (95%CI: 11.0–13.9), with 9.6% occurring among men and 14.9% among women. The prevalence of suicide ideation was significantly (p<0.0001) lower in Spain (4.4%, 95%CI: 3.7–5.1), with 3.4% occurring among men and 5.2% among women. No interaction between gender and country was observed for the prevalence of suicide ideation (p=0.8).
Table 1.
Lifetime prevalence of suicidal ideation, plan, and attempts between France and Spain across gender-specific strata
| % with suicide ideation*
|
% with suicide plans*
|
% with suicide attempts*
|
% with suicide attempts among those with suicide ideation
|
|||||
|---|---|---|---|---|---|---|---|---|
| France | Spain | France | Spain | France | Spain | France | Spain | |
| n=1565 | n=3052 | n=1565 | n=3052 | n=1565 | n=3052 | n=244 | n=182 | |
| Women | 14.9 (12.8–17.3) | 5.2 (4.3–6.4) | 6.1 (4.9–7.6) | 1.8 (1.3–2.4) | 5.4 (4.0–7.3) | 1.7 (1.2–2.4) | 36.2 (28.6–4.5) | 32.4 (23.8–42.3) |
| n=1329 | n=2421 | n=1329 | n=2421 | n=1329 | n=2421 | n=147 | n=90 | |
| Men | 9.6 (8.2–11.3) | 3.4 (2.7–4.2) | 2.6 (1.9–3.5) | 1.1 (0.7–1.8) | 1.1 (0.7–1.8) | 1.2 (0.9–1.8) | 11.8 (7.7–17.7) | 36.5 (26.5–47.8) |
|
| ||||||||
| p for intx | 0.8 | 0.2 | 0.001 | |||||
| n=2894 | n=5473 | n=2894 | n=5473 | n=2894 | n=5473 | n=391 | n=272 | |
| Total | 12.4 (11.0–13.9) | 4.4 (3.7–5.1) | 4.5 (3.7–5.3) | 1.4 (1.1–1.9) | 3.4 (2.6–4.3) | 1.5 (1.1–1.9) | 27.2 (21.8–33.3) | 33.9 (28.1–40.3) |
Values in parenthesis are 95% CI of point estimates.
p-value for interaction: based on a t-test of the cross-product term between country and gender, which was estimated after fitting a logistic regression model.
Lifetime prevalence of suicide plans was 4.5% (95%CI: 3.7–5.3) in France, of which 2.6% and 6.1% were reported among men and women, respectively (Table 1). Meanwhile, prevalence of suicide plans was 1.4% (95%CI: 1.1–1.9) in Spain, of which 1.1% and 1.8% were reported among men and women, respectively. No interaction between gender and country was observed for the prevalence of suicide plans (p=0.2).
Finally, lifetime prevalence of suicide attempts was 3.4% (95%CI: 2.6–4.3) in France, of which 1.1% and 5.4% were reported among men and women, respectively. The prevalence of suicide attempts was 1.5% (95%CI: 1.1–1.9) in Spain, of which 1.2% and 1.7% were reported among men and women, respectively. Contrary to suicide ideation and plans, a significant interaction between gender and country was observed for the prevalence of suicide attempts (p=0.001), indicating that gender is an effect modifier of the country-suicide attempt relationship (Table 1).
Suicide attempts were then examined among those with suicide ideation. Suicide attempts were similar for Spanish and French women with suicide ideation (32.4% and 36.2%, respectively). Within the same subgroup, Spanish men had a higher reported suicide attempt (36.5%) when compared to French men (11.8%). However, since Spanish men have a much lower overall prevalence of suicidal thoughts, the overall prevalence of suicide attempts remains similar between countries (Table 1).
Gender-specific age at first suicide attempt between countries
Among women, median age of first suicide attempt was 19 years (IQR=14–35) in Spain and 23 years (IQR=17–34) in France. Among men, median age of first suicide attempt was 26 years (IQR=18–40) in Spain and 29 years (IQR=23–33) in France. Figure 1 represents the kernel density plot of suicide attempt with respect to age at first event for men (1a) and women (1b), thus illustrating the similarities in event distributions between countries.
Figure 1.
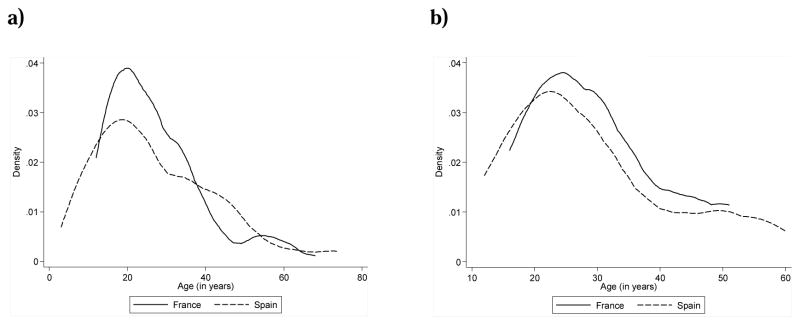
Density of suicide attempts according to age of first attempt for Spain and France among women (a) and men (b)
Country differences in risk-factors of suicide ideation within gender
Table 2 describes various risk-factors and their association with suicide ideation for each country and gender group. Persons who had any lifetime mood or anxiety disorder tended towards higher reports of suicide ideation compared to those without mental disorder, except for any lifetime anxiety disorder among Spanish men (OR=1.65, 95%CI: 0.37–7.35). No significant differences of effect were observed between countries within gender-stratum.
Table 2.
Multivariable1 risk-factors for lifetime suicide ideation between France and Spain across gender-specific strata
| Women
|
p for intx* | Men
|
p for intx* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| France n=789 |
Spain n=1222 |
France n=557 |
Spain n=781 |
|||||||
|
| ||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Sociodemographic variables
| ||||||||||
| Age ≥35 years of age | 1.23 | (0.68–2.20) | 2.14 | (1.27–3.60) | 0.2 | 0.63 | (0.25–1.61) | 1.77 | (0.51–6.18) | 0.04 |
| >12 years of education | ** | 0.55 | (0.16–1.86) | ntp | ** | 0.03 | (0.00–0.32) | ntp | ||
| Unemployed | 3.17 | (0.85–11.78) | 0.94 | (0.49–1.80) | 0.2 | 0.37 | (0.11–1.19) | 1.54 | (0.37–6.37) | 0.09 |
| Mental Disorders
| ||||||||||
| Any lifetime mood disorder | 1.71 | (0.96–3.03) | 3.85 | (1.88–7.87) | 0.07 | 4.90 | (2.06–11.65) | 4.35 | (1.01–18.81) | 0.2 |
| Any lifetime anxiety disorder | 1.91 | (1.10–3.31) | 2.75 | (1.04–7.28) | 0.2 | 3.19 | (1.52–6.69) | 1.65 | (0.37–7.35) | 0.3 |
| Parental Bonding
| ||||||||||
| Mother | ||||||||||
| Care | 0.69 | (0.51–0.93) | 0.94 | (0.62–1.42) | 0.8 | 1.38 | (0.78–2.47) | 0.27 | (0.15–0.51) | 0.005 |
| Overprotection | 1.02 | (0.60–1.75) | 0.81 | (0.55–1.20) | 0.3 | 0.82 | (0.47–1.44) | 7.67 | (2.93–20.06) | 0.03 |
| Authoritariansism | 1.14 | (0.78–1.68) | 0.83 | (0.62–1.12) | 0.03 | 0.76 | (0.49–1.18) | 0.79 | (0.50–1.25) | 0.5 |
| Father | ||||||||||
| Care | 0.91 | (0.67–1.25) | 0.58 | (0.32–1.07) | 0.09 | 1.00 | (0.73–1.37) | 0.73 | (0.41–1.30) | 0.03 |
| Overprotection | 0.89 | (0.57–1.39) | 1.05 | (0.72–1.51) | 0.2 | 0.64 | (0.32–1.28) | 0.44 | (0.24–0.83) | 0.9 |
| Authoritariansism | 1.05 | (0.73–1.52) | 1.02 | (0.71–1.48) | 0.2 | 1.29 | (0.75–2.19) | 0.92 | (0.55–1.54) | 0.3 |
| Marital Status
| ||||||||||
| Married, cohabitating | 1.00 | *** | 1.00 | *** | 0.8 | 1.00 | *** | 1.00 | *** | 0.2 |
| Separated, widowed, divorced | 0.96 | (0.55–1.68) | 1.14 | (0.60–2.17) | 1.43 | (0.39–5.32) | 1.68 | (0.42–6.66) | ||
| Never married | 1.28 | (0.50–3.27) | 1.37 | (0.51–3.66) | 2.17 | (1.14–4.15) | 1.36 | (0.44–4.19) | ||
| Use of services
| ||||||||||
| Psychiatrist | 1.89 | (1.07–3.34) | 2.17 | (1.24–3.82) | 0.6 | 6.52 | (2.83–15.04) | 1.33 | (0.31–5.62) | 0.007 |
| General practicioner | 1.44 | (0.67–3.08) | 0.72 | (0.45–1.16) | 0.7 | 1.83 | (0.39–8.64) | 1.65 | (0.27–9.92) | 0.2 |
| Other | 1.38 | (0.66–2.88) | 1.96 | (1.07–3.58) | 0.2 | 1.29 | (0.40–4.11) | 2.05 | (0.47–8.90) | 0.7 |
| Any lifetime use of antidepressants | 2.56 | (1.00–6.57) | 3.66 | (1.85–7.26) | 0.7 | 1.09 | (0.39–3.04) | 2.89 | (0.33–24.93) | 0.9 |
Models were adjusted for all variables displayed in the first column.
p-value for interaction: based on a t-test of the cross-product term between country and risk-factor. This term was estimated in two multivariable logistic regression models - one for women and another for men.
Variable was omitted from analysis, no parameter was estimated.
ntp: no test performed
95% CI not reported, variable used as reference group.
In terms of PBI, French women were more likely to report suicide ideation with authoritarian mothers (OR=1.14, 95%CI: 0.78–1.68), whereas Spanish women were less likely with authoritarian mothers (OR=0.83; 95%CI: 0.62–1.12). French men were more likely to report suicide ideation with caring mothers (OR=1.38, 95%CI: 0.78–2.47), whereas Spanish men were less likely with mothers of the same PBI (OR=0.27; 95%CI: 0.15–0.51). In contrast, overprotecting mothers were associated with a much higher risk of suicide ideation among Spanish men (OR=7.67, 95%CI: 2.93–20.06) than French men (OR=0.82, 95%CI: 0.47–1.44). These effect differences between countries were significantly different (p≤0.03).
No significant differences in the effect of unemployment, marital status or use of services on suicide ideation were observed between France and Spain within gender-stratum (Table 2). However, use of psychiatrist was more strongly associated with suicide ideation among French men (OR=6.52, 95%CI: 2.83–15.04) compared to Spanish men (OR=1.33, 95%CI: 0.31–5.62) (p=0.007).
Country differences in risk-factors of suicide attempt within gender
Table 3 contains various risk-factors and their association with suicide attempts for each gender and country group. Similar to suicide ideation, the presence of any lifetime mood or anxiety disorder tended to be strong risk-factors for suicide attempt across all genders and countries, except for mood disorders among Spanish men. No significant differences were found in ORs between countries within each gender stratum.
Table 3.
Multivariable1 risk-factors for lifetime suicide attempt between France and Spain across gender-specific strata
| Women
|
p for intx* | Men
|
p for intx* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| France n=789 |
Spain n=1222 |
France n=557 |
Spain n=781 |
|||||||
|
| ||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Sociodemographic variables
| ||||||||||
| Age ≥35 years of age | 0.65 | (0.31–1.36) | 1.84 | (0.68–4.96) | 0.006 | 0.55 | (0.07–4.66) | 4.55 | (1.02–20.19) | 0.009 |
| Years of education | ** | 0.57 | (0.07–5.07) | ntp | ** | ** | ntp | |||
| Unemployed | 1.46 | (0.30–6.98) | 0.65 | (0.24–1.77) | 0.7 | 0.56 | (0.09–3.54) | 2.95 | (0.22–38.70) | 0.2 |
| Mental Disorders
| ||||||||||
| Any lifetime mood disorder | 6.52 | (1.95–21.85) | 4.83 | (1.07–21.77) | 0.7 | 2.14 | (0.33–13.79) | 0.37 | (0.03–5.46) | 0.3 |
| Any lifetime anxiety disorder | 1.04 | (0.53–2.07) | 8.18 | (1.09–61.54) | 0.08 | 1.37 | (0.42–4.50) | 4.39 | (0.35–55.77) | 0.4 |
| Parental Bonding
| ||||||||||
| Mother | ||||||||||
| Care | 0.74 | (0.50–1.10) | 0.72 | (0.43–1.21) | 0.4 | 0.65 | (0.39–1.09) | 0.42 | (0.09–1.84) | 0.6 |
| Overprotection | 1.21 | (0.88–1.66) | 0.83 | (0.48–1.43) | 0.2 | 0.88 | (0.43–1.81) | 7.79 | (1.33–45.71) | 0.03 |
| Authoritariansism | 1.51 | (1.04–2.18) | 0.77 | (0.51–1.15) | <0.001 | 1.18 | (0.66–2.11) | 0.72 | (0.33–1.60) | 0.3 |
| Father | ||||||||||
| Care | 1.09 | (0.76–1.57) | 1.05 | (0.45–2.45) | 0.2 | ** | 0.56 | (0.22–1.40) | ntp | |
| Overprotection | 0.91 | (0.56–1.47) | 0.93 | (0.45–1.89) | 0.3 | ** | 0.44 | (0.17–1.16) | ntp | |
| Authoritariansism | 0.96 | (0.70–1.32) | 0.63 | (0.39–1.03) | 0.01 | 0.97 | (0.46–2.04) | 1.57 | (0.53–4.65) | 0.9 |
| Marital Status
| ||||||||||
| Married, cohabitating | 1.00 | *** | 1.00 | *** | 0.07 | 1.00 | *** | 1.00 | *** | 0.1 |
| Separated, widowed, divorced | 0.78 | (0.29–2.15) | 0.90 | (0.24–3.38) | 4.46 | (0.74–26.78) | 8.04 | (0.17–387.90) | ||
| Never married | 1.19 | (0.44–3.22) | 3.95 | (1.02–15.30) | 3.25 | (0.32–33.32) | 3.24 | (0.39–27.07) | ||
| Use of services
| ||||||||||
| Psychiatrist | 5.67 | (3.12–10.30) | 4.67 | (1.16–18.83) | 0.1 | 3.54 | (0.36–35.21) | 4.87 | (0.46–51.19) | 0.6 |
| General practicioner | 1.03 | (0.54–2.00) | 0.08 | (0.02–0.35) | 0.01 | 1.81 | (0.29–11.34) | 3.60 | (0.13–100.81) | 0.8 |
| Other | 1.52 | (0.62–3.73) | 1.69 | (0.47–6.14) | 0.9 | 3.89 | (0.87–17.36) | 3.99 | (0.35–45.98) | 0.8 |
| Any lifetime use of antidepressants | 0.63 | (0.28–1.42) | 5.86 | (1.51–22.74) | 0.3 | 3.15 | (0.78–12.71) | 6.89 | (0.63–75.88) | 0.9 |
Models were adjusted for all variables displayed in the first column.
p-value for interaction: based on a t-test of the cross-product term between country and risk-factor. This term was estimated in two multivariable logistic regression models - one for women and another for men.
Variable was omitted from analysis, no parameter was estimated.
ntp: no test performed
95% CI not reported, variable used as reference group.
In terms of sociodemographic variables, French women older than 35 years were significantly less likely to attempt suicide than Spanish women of the same age (OR=0.65 vs OR=1.84, respectively; p=0.006). The same significant difference in effect held true for French men compared to Spanish men (OR=0.55 vs. 4.55, p=0.009). The effect of unemployment status between countries within gender stratum was not significantly different.
Strong differences in direction of association were also observed between France and Spain with respect to parental bonding as a risk-factor for suicide attempt. Overprotecting mothers increased the odds by 7.8-fold of reporting suicide attempts among Spanish men versus 0.9-fold decrease among French men (p=0.03). Conversely, authoritarian mothers increased the odds by 1.5-fold of suicide attempts among French women, while a 0.8-fold decrease in odds was observed among Spanish women (p<0.001). No significant differences were found in father parental bonding index, except for French women, among whom the presence of an authoritarian father had no association on suicide attempts (OR=0.96) versus a protective association among Spanish women (OR=0.63) (p=0.01).
Concerning marital status, Spanish men and women who were never married reported significantly higher levels of suicide attempts (OR=3.24; 95%CI: 0.39–27.07 and OR=3.95; 95%CI: 1.02–15.30, respectively) when compared to those who are married or cohabitating. This effect was observed with French men, but not French women. Moreover, French women had a borderline significantly lower odds of suicide attempt when not married versus Spanish women (p=0.07).
Use of general practitioner had a significantly protective effect of suicide attempt among Spanish women (OR=0.08; 95%CI: 0.02–0.35) compared to no effect with French women (OR=1.03; 95%CI: 0.54–2.00) – the difference of effect between countries was significant (p=0.01). Overall, the odds of reporting suicide tended to be higher among both French and Spanish men who used any health service versus no use at all, yet these were not significant risk-factors (Table 3).
Religiosity as a risk-factor of suicide attempt between countries within gender
Any declared religion was also examined as a risk-factor for both suicide ideation and attempt (Table 4) and are reported for each country and gender group. A significant 3.0-fold and 11.0-fold increase in odds of reporting suicide attempts was observed among French women and Spanish men, respectively, declaring a religion when compared to those reporting no religion. However, no significant differences in ORs were observed between countries within gender-strata.
Table 4.
Religious practices and use of religion as risk-factors for lifetime suicide ideation and attempt between France and Spain across gender-specific strata
| Women
|
p for intx* | Men
|
p for intx* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| France | Spain | France | Spain | |||||||
|
|
|
|||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
|
Suicide ideation
| ||||||||||
| n=789 | n=1221 | n=557 | n=780 | |||||||
| Any declared religion | 0.74 | (0.31–1.74) | 0.53 | (0.22–1.31) | 0.7 | 0.77 | (0.32–1.87) | 1.55 | (0.52–4.65) | 0.5 |
| n=457 | n=961 | n=294 | n=491 | |||||||
| Use of religion | ||||||||||
| Weekly practice | 0.48 | (0.05–4.29) | 0.51 | (0.23–1.12) | 0.8 | 0.54 | (0.07–4.27) | 1.00 | (0.18–5.52) | 0.4 |
| Importance of religion | 0.71 | (0.13–3.77) | 0.74 | (0.25–2.20) | 0.3 | 0.39 | (0.02–6.21) | 3.03 | (0.86–10.63) | 0.5 |
| Problem solving with religion | 3.64 | (1.22–10.89) | 1.42 | (0.43–4.69) | 0.08 | 1.55 | (0.16–15.47) | 0.37 | (0.08–1.67) | 0.7 |
|
Suicide attempt
| ||||||||||
| n=789 | n=1221 | n=557 | n=780 | |||||||
| Any declared religion | 2.95 | (1.29–6.75) | 1.10 | (0.33–3.70) | 0.08 | 3.21 | (0.62–16.51) | 10.98 | (1.13–106.60) | 0.4 |
| n=457 | n=961 | |||||||||
| Use of religion1 | ||||||||||
| Weekly practice | 5.24 | (0.31–88.77) | 0.28 | (0.07–1.08) | 0.2 | |||||
| Importance of religion | 0.09 | (0.00–3.15) | 1.05 | (0.09–11.67) | 0.7 | |||||
| Problem solving with religion | 1.74 | (0.37–8.14) | 0.78 | (0.10–6.35) | 0.7 | |||||
All ORs were adjusted for age, year of education, unemployment status, any lifetime mood or anxiety disorder, parental bonding index of both mother and father, marital status, any lifetime use of antidepressants, and psychiatrist, general practitioner or other health service use.
p-value for interaction: based on a t-test of the cross-product term between country and risk-factor. This term was estimated in two multivariable logistic regression models - one for women and another for men.
Standard error estimates could not be performed for survey data; this variable was not included in the multivariable model.
Models for men in both France and Spain produced unstable estimates and were excluded from analysis.
In addition, the use of religion (weekly practice, importance of religion, and problem solving with religion) were also examined as risk-factors for both suicide ideation and attempt (Table 4). French women who used problem solving with religion were the only group with a significantly higher odds of reporting suicide ideation than those who did not (OR=3.64; 95%CI: 1.22–10.89). No differences in association of religious use on suicide ideation or attempt were observed between France and Spain among women. Due to the low number of responses and events among men, stable estimates could not be converged using religiosity variables as risk-factors for suicide ideation or attempt.
DISCUSSION
Using a population-based study, our objective was to compare two relatively similar neighbouring, mainly Catholic European countries: France and Spain. The results demonstrated that the prevalence of suicide deaths, ideation, plans and attempts were significantly higher in France compared to Spain. This mirrors WHO data from 2005 in which a substantially higher suicide rate was observed in France than Spain and whose reports were unlikely to be misclassified with other deaths, resulting in artificial differences of suicide death rates.
In the ESEMeD study, the differences in suicide attempts between France and Spain appear mainly within gender. Prevalence of suicide attempts did not significantly differ between French and Spanish men, whereas French women had a much higher prevalence than Spanish women. Interestingly, this parallels the higher prevalence of depressive and anxiety disorders, as well as higher rates of completed suicide, observed among women in France than in Spain. (Demyttenaere et al., 2004, Fernandez et al., 2007, Codony et al., 2007, Fernandez et al., 2006, Costa-Font et al., 2009) In this respect, studying suicidality is a useful means of understanding the gender-specific determinants of suicide.
In both countries, differences did not appear to be caused by marital status, years of education, or religion. For suicidal thoughts, employment status seemed to have a differential effect according to gender: Spanish unemployed women had lower risk than French women and the reverse applied for men. This might be attributed to a much larger gender difference in employment rates for Spain when compared to France. (Eurostat, 2010) Indeed, there is a higher dependence for Spanish men to work during situations of unemployment. French women may also be more emancipated in the sense that they undertake employment more readily than Spanish women, particularly during parenthood. (Eurostat, 2010)
Parental bonding is an important risk-factor for which maternal care has been shown to protect especially against the cumulating effect of both depressive disorder (Heider et al., 2006) and suicidality. (Heider et al., 2007) The comparison between France and Spain demonstrates that parental attitudes as a risk-factor differ within gender. Among women, maternal authoritarianism is protective in Spain while appearing to be detrimental in France (for both suicidal thoughts and suicidal attempts), with a similar, significant trend for paternal authoritarianism and suicide attempt. In contrast, the effect of other dimensions of care and overprotection on suicide attempt does not appear to be significantly different between countries within gender. However, the risk of suicide attempt with an overprotective mother increased among Spanish men, while decreased for French men.
Although an authoritative mother has been linked with positive attachment in some cultures, other settings may perceive maternal bonding differently. For example, a mother who is viewed as authoritarian may represent severe, distant and frightening traits in France, while at the same time meaning a structuring and warm relationship in Spain and the US. (Nair and Murray, 2005, Karavasilis et al., 2003) On the contrary, overprotective mothers may be more detrimental for Spanish men because the maternal relationship is perceived as very intrusive and restricting, when in France it signifies a warm relationship. (Burbach et al., 1989) This cultural influence may explain why a much smaller association of overprotection on psychiatric disorders was observed in a longitudinal study conducted in the Netherlands (Overbeek et al., 2007), compared to a national co-morbidity survey in the US. (Enns et al., 2002) The contextual interpretation of parental roles is one limitation of using such a very restricted scale, which can only measure subtle parental relationships during childhood.
The third finding, of great interest, is the role of General Practitioners (GPs) in Spain versus France. In Spain, women have a decreased risk of suicide attempt when in contact with their GP, which was not the case among French women. Does this imply that Spanish GPs more adequately meet the needs of suicidal women than French GPs? Is this because Spanish GPs have more developed training in mental health and increased support from psychiatrists than in France? We have previously found that France has the lowest amount of contact between GPs and any mental health provider among the ESEMeD countries. (Kovess-Masfety et al., 2007) Spanish GPs can also refer patients to psychologists, which does not readily occur in France, as the social security system does not reimburse patients for consultations with a psychologist. In addition, the low level of continuing education among French GPs may also contribute to the unawareness of mental health problems. Of note, the Spanish health system follows WHO recommendations in which GPs heavily rely on the support of a consulting psychiatrist for patients with mental health problems. (Kovess-Masfety et al., 2007) This system is not applied in France, where GPs and psychiatrists are working in parallel through direct-access care and with very little intra-service contact.
Finally, the use of religion as a means to resolve mental health problems does not appear to be a prominent risk-factor for suicidality. Despite this seemingly contrary finding, our results are in keeping with more recent research in which a consistent relationship between religiosity and attempted suicide was not found. (Kovess-Masfety et al., 2010, Sisask et al., 2010) Suicidal thoughts tended to be higher among French women who claimed to rely on religion for support, while no effect was observed among Spanish women. One interpretation could be that religion-reliant women in France have a higher frequency of mental health problems, although this is not the case for Spanish women.
Economically-speaking, these two countries are relatively similar, although France, when compared to Spain, has lower unemployment rates (10.0% for France, 19.3% for Spain), and a slightly higher Purchasing Power Standard per inhabitant (25,300 € in France vs 24,500 € in Spain). (Eurostat, 2009) This implies that differences in suicide rates and suicidality may not be related by economic factors, rather to either cultural elements, linked to child rearing styles and parent-child relationships, or the structure of primary health-care system. Furthermore, it appears that religion does not play a role in the attitudes toward suicide. Comparative psychiatry may be needed for future between-country comparisons, in which the aim is to study the consequences of these culture features.
Certain limitations need to be addressed in this study. First, this study was cross-sectional in nature, thus the temporality of the exposure-disease relationship cannot be established. For instance, it is uncertain as to whether suicidal behaviour preceded consultation with a GP. However, many of the risk-factors are argued to evaluate exposures occurring prior to the onset of suicidality, such as the PBI during childhood. Second, the response rate was much lower in France than in Spain, although weighted adjustments were performed to represent the target population. Third, diagnostic accuracy of mental health problems may have been affected by self-report or recall bias. Fourth, parental bonding is retrospective and could be influenced by current mental state, as discordant PBI results have occurred between patients with depression and their family members. (Parker et al., 1997) Finally, the effect of alcohol or substance abuse could not be evaluated. We examined several models including these risk-factors, yet they demonstrated no significant association with suicide attempt nor were they significant between countries within gender stratum.
In conclusion, risk-factors for suicidality play different roles across genders within these two countries and their relationship with completed suicide are parallel for women but not for men. In addition, parental bonding dimensions have different consequences, thus underlining the importance of cultural aspects when studying suicidality, an apparent advantage of the cross-cultural comparisons of the ESEMeD and WMH surveys. Potential interventions aiming to reduce suicide and suicidality may want to address parent-child relationships by underscoring supportive parental attitudes in a culturally-adapted manner. In terms of public health, the most important finding is the general practitioner’s role between the two countries, for which access to mental health care has been organised in rather different ways. Our results support WHO recommendations, which place the GP at the centre of mental health decisions with close psychiatric support and access to psychologists. This is in keeping with the seminal work of Rutz and colleagues. (Rutz et al., 1989, Rutz et al., 1992)
Acknowledgments
Role of funding support
This project was funded by the European Commission (Contract QLG5-1999-01042 and SANCO 2008/1308); the Piemont Region (Italy), Fondo de Investigacion Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia Y Tecnologia, Spain (SAF 2000-158-CE), Department de Sanitat, Generalitat de Catalunya, Spain, other local agencies and by an unrestricted educational grant from GlaxoSmithKline. ESEMeD is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey initiative. These WMH activities were supported by the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. All funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
We thank the WMH staff for assistance with instrumentation fieldwork, and data analysis. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Footnotes
Conflict of Interest
The authors report no conflict of interest.
CONTRIBUTORS
V. Kovess-Masfety partook in the design and implementation of the ESEMeD study, proposed and oversaw the statistical analysis, and wrote the majority of the paper.
A. Boyd did the data analysis, drafted and corrected the methods, results, tables, and figure sections.
J.M. Haro, J.P. Lépine, I. Gasquet, and R. Bruffaerts partook in the design and implementation of the ESEMeD study, provided substantial advice on specific measurement tools, and whose revisions added valuable insight and to the paper.
G. Villgut partook in the design and implementation of the ESEMeD study, verified the statistical analysis, and whose revision added valuable insight to the paper.
J. Alonso is the principle investigator and leader of the data management and analysis center for the ESEMeD study, partook in the design and implementation of the study, and whose revision contributed valuable insight to the paper
All authors have approved of the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ALONSO J, ANGERMEYER MC, BERNERT S, BRUFFAERTS R, BRUGHA TS, BRYSON H, DE GIROLAMO G, GRAAF R, DEMYTTENAERE K, GASQUET I, HARO JM, KATZ SJ, KESSLER RC, KOVESS V, LEPINE JP, ORMEL J, POLIDORI G, RUSSO LJ, VILAGUT G, ALMANSA J, ARBABZADEH-BOUCHEZ S, AUTONELL J, BERNAL M, BUIST-BOUWMAN MA, CODONY M, DOMINGO-SALVANY A, FERRER M, JOO SS, MARTINEZ-ALONSO M, MATSCHINGER H, MAZZI F, MORGAN Z, MOROSINI P, PALACIN C, ROMERA B, TAUB N, VOLLEBERGH WA. Sampling and methods of the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004:8–20. doi: 10.1111/j.1600-0047.2004.00326. [DOI] [PubMed] [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION. Diagnostic and statistical manual of mental disorders. 4. Washington DC: 1994. (DSM IV) 1995. [Google Scholar]
- BERGGREN N. Rhetoric or reality? An economic analysis of the effects of religion in Sweden. Journal of Socio-Economics. 1997;26:571–596. [Google Scholar]
- BERNAL M, HARO JM, BERNERT S, BRUGHA T, DE GRAAF R, BRUFFAERTS R, LEPINE JP, DE GIROLAMO G, VILAGUT G, GASQUET I, TORRES JV, KOVESS V, HEIDER D, NEELEMAN J, KESSLER R, ALONSO J. Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord. 2007;101:27–34. doi: 10.1016/j.jad.2006.09.018. [DOI] [PubMed] [Google Scholar]
- BURBACH DJ, KASHANI JH, ROSENBERG TK. Parental bonding and depressive disorders in adolescents. J Child Psychol Psychiatry. 1989;30:417–29. doi: 10.1111/j.1469-7610.1989.tb00255.x. [DOI] [PubMed] [Google Scholar]
- CAVANAGH JT, OWENS DG, JOHNSTONE EC. Life events in suicide and undetermined death in south-east Scotland: a case-control study using the method of psychological autopsy. Soc Psychiatry Psychiatr Epidemiol. 1999;34:645–50. doi: 10.1007/s001270050187. [DOI] [PubMed] [Google Scholar]
- CODONY M, ALONSO J, ALMANSA J, VILAGUT G, DOMINGO A, PINTO-MEZA A, FERNANDEZ A, SERRANO-BLANCO A, MARQUEZ M, HARO JM. Psychotropic medications use in Spain. Results of the ESEMeD-Spain study. Actas Esp Psiquiatr. 2007;35(Suppl 2):29–36. [PubMed] [Google Scholar]
- COSTA-FONT J, CABASES J, ALONSO J, SALVADOR-CARULLA L, MCDAID D. New and old challenges in the reform of mental health systems in Spain. Eurohealth. 2009;14:14–18. [Google Scholar]
- COX BJ, ENNS MW, CLARA IP. The Parental Bonding Instrument: confirmatory evidence for a three-factor model in a psychiatric clinical sample and in the National Comorbidity Survey. Soc Psychiatry Psychiatr Epidemiol. 2000;35:353–7. doi: 10.1007/s001270050250. [DOI] [PubMed] [Google Scholar]
- DEMYTTENAERE K, BONNEWYN A, BRUFFAERTS R, DE GIROLAMO G, GASQUET I, KOVESS V, HARO JM, ALONSO J. Clinical factors influencing the prescription of antidepressants and benzodiazepines: results from the European study of the epidemiology of mental disorders (ESEMeD) J Affect Disord. 2008;110:84–93. doi: 10.1016/j.jad.2008.01.011. [DOI] [PubMed] [Google Scholar]
- DEMYTTENAERE K, BRUFFAERTS R, POSADA-VILLA J, GASQUET I, KOVESS V, LEPINE JP, ANGERMEYER MC, BERNERT S, DE GIROLAMO G, MOROSINI P, POLIDORI G, KIKKAWA T, KAWAKAMI N, ONO Y, TAKESHIMA T, UDA H, KARAM EG, FAYYAD JA, KARAM AN, MNEIMNEH ZN, MEDINA-MORA ME, BORGES G, LARA C, DE GRAAF R, ORMEL J, GUREJE O, SHEN Y, HUANG Y, ZHANG M, ALONSO J, HARO JM, VILAGUT G, BROMET EJ, GLUZMAN S, WEBB C, KESSLER RC, MERIKANGAS KR, ANTHONY JC, VON KORFF MR, WANG PS, BRUGHA TS, AGUILAR-GAXIOLA S, LEE S, HEERINGA S, PENNELL BE, ZASLAVSKY AM, USTUN TB, CHATTERJI S. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- ENNS MW, COX BJ, CLARA I. Parental bonding and adult psychopathology: results from the US National Comorbidity Survey. Psychol Med. 2002;32:997–1008. doi: 10.1017/s0033291702005937. [DOI] [PubMed] [Google Scholar]
- EUROSTAT. [Accessed October 20, 2010];National Accounts (including GDP) 2009 [Online]. Available: http://epp.eurostat.ec.europa.eu/portal/page/portal/national_accounts/data/main_tables.
- EUROSTAT. [Accessed May 16, 2010];Eurostat Labour Force Survey. 2010 [Online]. Available: http://epp.eurostat.ec.europa.eu/portal/page/portal/eurostat/home/
- FERNANDEZ A, HARO JM, CODONY M, VILAGUT G, MARTINEZ-ALONSO M, AUTONELL J, SALVADOR-CARULLA L, AYUSO-MATEOS JL, FULLANA MA, ALONSO J. Treatment adequacy of anxiety and depressive disorders: primary versus specialised care in Spain. J Affect Disord. 2006;96:9–20. doi: 10.1016/j.jad.2006.05.005. [DOI] [PubMed] [Google Scholar]
- FERNANDEZ A, HARO JM, MARTINEZ-ALONSO M, DEMYTTENAERE K, BRUGHA TS, AUTONELL J, DE GIROLAMO G, BERNERT S, LEPINE JP, ALONSO J. Treatment adequacy for anxiety and depressive disorders in six European countries. Br J Psychiatry. 2007;190:172–3. doi: 10.1192/bjp.bp.106.023507. [DOI] [PubMed] [Google Scholar]
- GEARING RE, LIZARDI D. Religion and suicide. J Relig Health. 2009;48:332–41. doi: 10.1007/s10943-008-9181-2. [DOI] [PubMed] [Google Scholar]
- HANSEN L, PRITCHARD C. Consistency in suicide rates in twenty-two developed countries by gender over time 1874--78, 1974--76, and 1998--2000. Arch Suicide Res. 2008;12:251–62. doi: 10.1080/13811110802101153. [DOI] [PubMed] [Google Scholar]
- HARO JM, ARBABZADEH-BOUCHEZ S, BRUGHA TS, DE GIROLAMO G, GUYER ME, JIN R, LEPINE JP, MAZZI F, RENESES B, VILAGUT G, SAMPSON NA, KESSLER RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–80. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAWTON K, VAN HEERINGEN K. Suicide. Lancet. 2009;373:1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- HEIDER D, BERNERT S, MATSCHINGER H, HARO JM, ALONSO J, ANGERMEYER MC. Parental bonding and suicidality in adulthood. Aust N Z J Psychiatry. 2007;41:66–73. doi: 10.1080/00048670601057742. [DOI] [PubMed] [Google Scholar]
- HEIDER D, MATSCHINGER H, BERNERT S, ALONSO J, ANGERMEYER MC. Relationship between parental bonding and mood disorder in six European countries. Psychiatry Res. 2006;143:89–98. doi: 10.1016/j.psychres.2005.08.015. [DOI] [PubMed] [Google Scholar]
- HEIDER D, MATSCHINGER H, BERNERT S, ALONSO J, BRUGHA TS, BRUFFAERTS R, DE GIROLAMO G, DIETRICH S, ANGERMEYER MC. Adverse parenting as a risk factor in the occurrence of anxiety disorders: a study in six European countries. Soc Psychiatry Psychiatr Epidemiol. 2008;43:266–72. doi: 10.1007/s00127-007-0302-0. [DOI] [PubMed] [Google Scholar]
- KARAVASILIS L, DOYLE AB, MARKIEWICZ D. Associations between parenting style and attachment to mother in middle childhood and adolescence. International Journal of Behavioral Development. 2003;27:153–164. [Google Scholar]
- KOVESS-MASFETY V, ALONSO J, BRUGHA TS, ANGERMEYER MC, HARO JM, SEVILLA-DEDIEU C. Differences in lifetime use of services for mental health problems in six European countries. Psychiatr Serv. 2007;58:213–20. doi: 10.1176/ps.2007.58.2.213. [DOI] [PubMed] [Google Scholar]
- KOVESS-MASFETY V, DEZETTER A, DE GRAAF R, HARO JM, BRUFFAERTS R, BRIFFAULT X, GILBERT F, CODONY M, ALONSO J. Religious advisors’ role in mental health care in the European Study of the Epidemiology of Mental Disorders survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45:989–98. doi: 10.1007/s00127-009-0143-0. [DOI] [PubMed] [Google Scholar]
- LAMBERT NM, FINCHAM FD, MARKS LD, STILLMAN TF. Invocations and intoxication: does prayer decrease alcohol consumption? Psychol Addict Behav. 2010;24:209–19. doi: 10.1037/a0018746. [DOI] [PubMed] [Google Scholar]
- MANN JJ, APTER A, BERTOLOTE J, BEAUTRAIS A, CURRIER D, HAAS A, HEGERL U, LONNQVIST J, MALONE K, MARUSIC A, MEHLUM L, PATTON G, PHILLIPS M, RUTZ W, RIHMER Z, SCHMIDTKE A, SHAFFER D, SILVERMAN M, TAKAHASHI Y, VARNIK A, WASSERMAN D, YIP P, HENDIN H. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- MARUSIC A, FARMER A. Genetic risk factors as possible causes of the variation in European suicide rates. Br J Psychiatry. 2001;179:194–6. doi: 10.1192/bjp.179.3.194. [DOI] [PubMed] [Google Scholar]
- NAIR H, MURRAY AD. Predictors of attachment security in preschool children from intact and divorced families. J Genet Psychol. 2005;166:245–63. doi: 10.3200/GNTP.166.3.245-263. [DOI] [PubMed] [Google Scholar]
- NOCK MK, BORGES G, BROMET EJ, ALONSO J, ANGERMEYER M, BEAUTRAIS A, BRUFFAERTS R, CHIU WT, DE GIROLAMO G, GLUZMAN S, DE GRAAF R, GUREJE O, HARO JM, HUANG Y, KARAM E, KESSLER RC, LEPINE JP, LEVINSON D, MEDINA-MORA ME, ONO Y, POSADA-VILLA J, WILLIAMS D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OVERBEEK G, TEN HAVE M, VOLLEBERGH W, DE GRAAF R. Parental lack of care and overprotection. Longitudinal associations with DSM-III-R disorders. Soc Psychiatry Psychiatr Epidemiol. 2007;42:87–93. doi: 10.1007/s00127-006-0115-6. [DOI] [PubMed] [Google Scholar]
- PARKER G, GLADSTONE G, WILHELM K, MITCHELL P, HADZI-PAVLOVIC D, AUSTIN MP. Dysfunctional parenting: over-representation in non-melancholic depression and capacity of such specificity to refine sub-typing depression measures. Psychiatry Res. 1997;73:57–71. doi: 10.1016/s0165-1781(97)00113-3. [DOI] [PubMed] [Google Scholar]
- PICKARD JG. The relationship of religiosity to older adults’ mental health service use. Aging Ment Health. 2006;10:290–7. doi: 10.1080/13607860500409641. [DOI] [PubMed] [Google Scholar]
- PRITCHARD C, AMANULLAH S. An analysis of suicide and undetermined deaths in 17 predominantly Islamic countries contrasted with the UK. Psychol Med. 2007;37:421–30. doi: 10.1017/S0033291706009159. [DOI] [PubMed] [Google Scholar]
- ROBINS LN, WING J, WITTCHEN HU, HELZER JE, BABOR TF, BURKE J, FARMER A, JABLENSKI A, PICKENS R, REGIER DA, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of general psychiatry. 1988;45:1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- RUTZ W, VON KNORRING L, WALINDER J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80:151–4. doi: 10.1111/j.1600-0447.1989.tb01318.x. [DOI] [PubMed] [Google Scholar]
- RUTZ W, VON KNORRING L, WALINDER J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992;85:83–8. doi: 10.1111/j.1600-0447.1992.tb01448.x. [DOI] [PubMed] [Google Scholar]
- SISASK M, VARNIK A, KOLVES K, BERTOLOTE JM, BOLHARI J, BOTEGA NJ, FLEISCHMANN A, VIJAYAKUMAR L, WASSERMAN D. Is religiosity a protective factor against attempted suicide: a cross-cultural case-control study. Arch Suicide Res. 2010;14:44–55. doi: 10.1080/13811110903479052. [DOI] [PubMed] [Google Scholar]
- WHO. [Accessed April 9, 2010];European Health for All Database (HFA-DB) 2005 [Online]. Available: http://www.euro.who.int/en/what-we-do/data-and-evidence/databases/european-health-for-all-database-hfa-db2.
- WITTCHEN HU. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]


