Abstract
Background and objectives
Living donor guidelines—both national and international—either do not address or are vague about what information can be shared between prospective living donors and transplant candidates, as well as when to make such disclosures and who should make them. This study explored the attitudes of donors and recipients regarding how much information they believe should be shared.
Design, setting, participants, & measurements
Two Email invitations were sent by the National Kidney Foundation (national headquarters) to its Email listservs, inviting members to participate in an online survey to assess the attitudes of kidney transplant stakeholders regarding the disclosure of health and health risk behavior information.
Results
From approximately 4200 unique Email addresses, 392 (9.3%) respondents completed part or all of the survey. The analyses were limited to the 236 respondents who self-identified as either donors (potential and actual, n=160) or recipients (candidates and actual, n=76). Overall, 79% (186 of 234) of respondents supported disclosure of general recipient health information that would affect post-transplant outcome to donors, and 88% (207 of 235) supported disclosure of general donor health information to recipients. Recipients and donors were also supportive of sharing donor and recipient information, particularly information relevant to graft and patient survival. There is some reticence, however, about sharing social information. The closer the relationship, the more information they are willing to share. Both donors and recipients wanted the transplant team involved in the information disclosure. Over three quarters of donors (79%) and recipients (78%) did not think the recipient had a right to know why a donor was excluded from donating.
Conclusions
Both donors and recipients want a significant amount of health information to be disclosed. The opinions of other stakeholders need to be surveyed to determine whether a revision of current policies and practices is warranted.
Keywords: kidney transplantation, risk factors, living donors, disclosure, privacy
Introduction
Living donor guidelines—both national and international—either do not address or are vague about what information can be shared between prospective living donors and transplant candidates, as well as when to make such disclosures and who should make them (1–5). Information about the donor may be of significant interest to the recipient to decide whether to accept the organ. Likewise, a potential donor may want information about an intended recipient to decide whether to offer the organ. How much information should be shared with each party and by whom are controversial questions.
Potential living donors undergo extensive screening both to try to ensure that they are physically, psychologically, and socially healthy enough to safely undergo unilateral nephrectomy and to identify their risk of transmitting certain infectious diseases or cancers. In some cases, donors may be excluded because of the disease transmission risk they pose to their recipient candidates. Although potential donors are usually provided with specific information about why they are excluded, recipients are only told that the potential donor was excluded.
Some potential donors may participate in high-risk activities that expose them to the risk of being infected with HIV, hepatitis B, or hepatitis C, even if they are negative at screening. Transplant professionals want to identify these donors because these infections can be transmitted in the graft (6). For deceased donor organs, the United Network for Organ Sharing (UNOS)/Organ Procurement and Transplantation Network (OPTN) has a policy that requires that candidates be informed whether their deceased donor meets the Centers for Disease Control and Prevention increased risk classification for infection transmission (15.3 bullet 2), even if the donor tests negative (7). Whether this classification must be disclosed for living donors is not clearly articulated. What the policy handbook states is that recipients should be told that living donors are required to undergo screening for a list of transmissible diseases (15.3.2) but that “there is no comprehensive way to screen potential deceased and living donors for all transmissible diseases” (15.3.3) (7).
Recipient candidate health, by contrast, does not pose any medical risk to the donor and therefore UNOS/OPTN guidance is to not share any health information. Rather, the transplant team is instructed to tell living donors that “any transplant candidate might have risk factors for increased morbidity or mortality that are not disclosed to the potential donor” (Table 14.1) (7). Given that donors expose themselves to the short- and long-term risks of unilateral nephrectomy, some believe that donors should have access to recipient health and health risk behavior information that may affect their decision on whether the benefit of donation outweighs these risks (5).
We designed a survey to assess the attitudes of living kidney transplant stakeholders regarding the disclosure of health information and information about social behaviors related to health. We had four hypotheses: First, both donors and recipients would want more information shared than currently is required to be shared. Second, the closer donors and recipients are emotionally, the more willing they would be to share information. Third, both donors and recipients would want the transplant team involved in the sharing of this information. Fourth, donors would believe that recipients do not have a right to know why a donor was excluded, but recipients would believe that they do.
Materials and Methods
With permission and help from the National Kidney Foundation (NKF) (national office), two invitations (July and August 2013) were sent to NKF-maintained listservs (approximately 2500 transAction Council members; approximately 1500 living donation members, which includes some family and professionals; and approximately 200 living donor advocate professionals), inviting them to participate in an online survey (Supplemental Appendix). Individuals aged <18 years were excluded.
The survey focused on attitudes regarding disclosure of information between living donors and recipients: what general information should be given, what specific information should be given, and who should be involved in the disclosure process. The content was developed based on a study by Rodrigue et al. (8). Questions were asked about both scenarios: sharing donor information with the recipient and sharing recipient information with the donor. Respondents were also asked how information about donors and recipients should be obtained (e.g., through friends, the Internet, etc.), whether a recipient had the right to know why a donor was excluded from donating, and how long a kidney should function after transplantation to make living donation worthwhile. Demographic questions included age, sex, race, ethnicity, and education level. Respondents were also asked to self-identify as a donor (prospective or actual), recipient (deceased donor recipients, living donor recipients, and candidates awaiting a transplant), health care provider (mainly living donor advocates), or other (which included family of donors and recipients, friends, individuals with kidney disease, and interested public). Of the donors, we asked them what their relationship is with their recipient, how well they know each other, and what personal information about themselves they have shared or intend to share with their recipient. Recipients were asked the same questions about their donor.
Statistical analysis was performed using SPSS software (version 21.0; SPSS Inc., Chicago, IL). Results were compared using chi-squared tests and t tests of independence. Approval from the University of Chicago Institutional Review Board was obtained and the requirement for written consent was waived. The research adheres to the requirements stipulated in the Declaration of Helsinki, and the clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
Results
Approximately 4200 Email addresses received two Emails from the NKF (national headquarters), inviting them to participate in an online survey. Of the 396 (9.4%) NKF stakeholders who opened the survey, 392 (9.3%) answered the age screening question, and 287 (6.9%) completed the demographics questions at the end of the survey. One hundred and sixty (56%) self-classified as donors, 76 (27%) as recipients, 13 (5%) as health care providers, and 13 (5%) as other. For the purpose of this article, we only focused on the 236 donors and recipients.
Of the 160 donor respondents, 146 (91%) had already donated and 14 (9%) were considering donating. Of the 76 recipient respondents, 44 (58%) received a living donor graft, 19 (25%) received a deceased donor graft, five (6.6%) had received both, five (6.6%) were waiting for a living donor graft, and three (4%) were on the deceased donor waitlist. Table 1 provides additional demographics. Most respondents were aged ≤50 years, female, white, non-Hispanic, with some form of higher education (2-year degree or higher). Compared with recipients, donors were more likely to be aged <50 years (101 of 154 donors versus 27 of 76 recipients, P<0.001), non-Hispanic (153 of 154 versus 65 of 70, P<0.02), and female (127 of 158 donors versus 43 of 75 recipients, P<0.001).
Table 1.
Demographics
| Characteristic | Donors (n=160) | Recipients (n=76) |
|---|---|---|
| Age, yr (n=230)a | ||
| ≤50 | 101 (66) | 27 (36) |
| >50 | 53 (34) | 49 (64) |
| Sex (n=233)a | ||
| Men | 31 (20) | 32 (43) |
| Women | 127 (80) | 43 (57) |
| Ethnicity (n=228)b | ||
| Hispanic | 1 (1) | 5 (7) |
| Non-Hispanic | 153 (99) | 65 (93) |
| Race (n=230) | ||
| Black | 11 (7) | 5 (7) |
| Asian or Southeast Asian | 3 (2) | 3 (4) |
| White | 138 (89) | 65 (87) |
| Native American, Pacific Islander, or Eskimo | 1 (1) | 0 (0) |
| Multiracial | 0 (0) | 1 (1) |
| Other | 2 (1) | 1 (1) |
| Education (n=234) | ||
| Graduated high school/GED | 9 (6) | 6 (8) |
| Some college studies (no degree) | 29 (18) | 14 (18) |
| Two-year degree | 17 (11) | 4 (5) |
| Four-year degree | 34 (22) | 20 (26) |
| Some graduate studies (no graduate degree) | 16 (10) | 10 (13) |
| Graduate degree (Master’s degree) | 46 (29) | 19 (25) |
| Graduate degree (doctoral degree) | 7 (4) | 3 (4) |
Data are presented as n (%). Percentages do not always add up to 100% due to rounding.
P<0.001.
P<0.02.
Overall, 79% (186 of 234) of respondents supported disclosure of general recipient health information that would affect recipient post-transplant outcome to donors, and 88% (207 of 235) of respondents supported disclosure of donor health information to recipients. Respondents also preferred that the transplant team be involved in the disclosure of this information, with or without the involvement of the individual (recipient or donor) whose information is being shared. This perspective was held similarly by both groups.
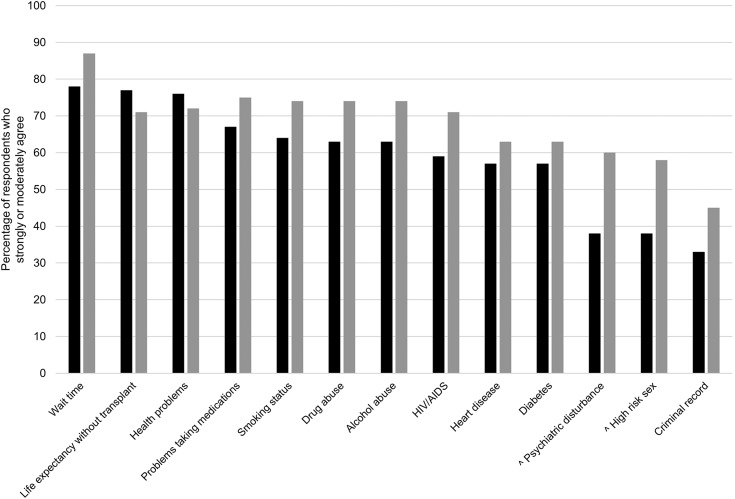
Figure 1 illustrates the attitudes of donors and recipients regarding the disclosure of specific recipient information to the donor. The majority of donors supported disclosing 10 of the 13 recipient characteristics, whereas the majority of recipients supported disclosing 12 of the 13 recipient characteristics. The only two characteristics in which the majority of donors and recipients differed were disclosure of psychiatric disturbance (P<0.005) and high-risk sex (P<0.005). In both cases, the majority of recipients were in favor of disclosure, whereas the majority of donors were against disclosure.
Figure 1.
Recipient information that should be disclosed to donor. Black bars indicate the percentage of donor respondents who strongly or moderately agree, whereas gray bars indicate the percentage of recipient respondents who strongly or moderately disagree. ^Donors versus recipients, P<0.005.
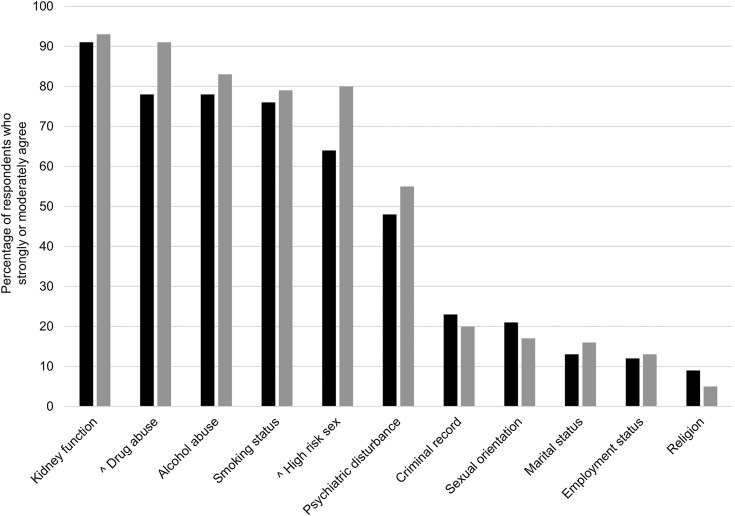
Figure 2 illustrates the attitudes of donors and recipients regarding the disclosure of specific donor information to the recipient. The majority of donors supported disclosing five of the 11 characteristics, whereas the majority of recipients supported disclosing six of the 11 characteristics. Donor and recipient attitudes differed significantly on only two characteristics: drug abuse (P<0.05) and high-risk sex (P<0.05). In both cases, however, the majority of both donors and recipients agreed that this information should be disclosed, but recipients were more emphatically in favor of disclosure than donors.
Figure 2.
Donor information that should be disclosed to recipient. Black bars indicate the percentage of donor respondents who strongly or moderately agree, whereas gray bars indicate the percentage of recipient respondents who strongly or moderately disagree. ^Donors versus recipients, P<0.05.
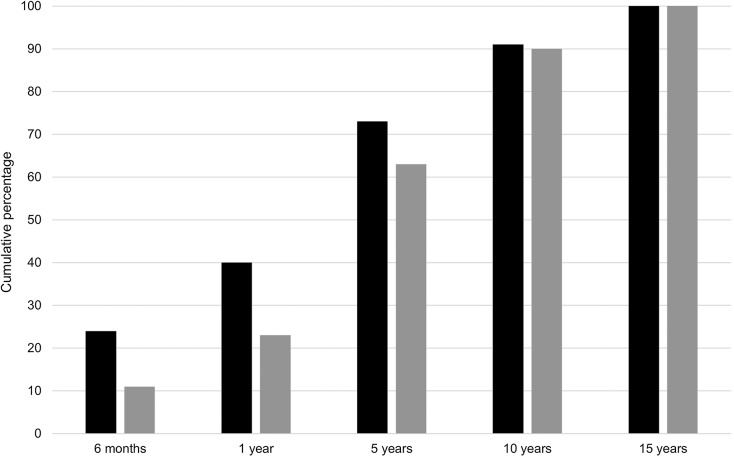
Figure 3 illustrates the attitudes of donors and recipients regarding how long a kidney graft needs to function to make donation worthwhile. If the graft were only to survive 6 months, 24% of donors but only 11% of recipients thought donation was worthwhile. The percentage of respondents who believe that donation is worthwhile increases with longer graft survival: 40% of donors and 23% of recipients believe 1-year survival is worthwhile, 73% of donors and 63% of recipients believe 5-year survival is worthwhile, and 91% of donors and 90% of recipients believe 10-year survival is worthwhile. All donors and recipients believe that donation is worthwhile if the graft survives for ≥15 years. Donors were significantly more likely to find shorter graft survival times to be worthwhile than recipients (P=0.02).
Figure 3.
How long does a kidney graft need to function to make donation worthwhile? Black bars indicate the percentage of donor respondents who believe the amount of time is worthwhile, whereas gray bars indicate the percentage of recipient respondents who believe the amount of time is worthwhile. P=0.02 determined by 2-tailed independent t test.
Table 2 shows donor and recipient attitudes regarding who should share information and how it should be obtained. With respect to who should be responsible for disclosure, the majority of donors and recipients wanted the transplant team involved. A minority of respondents (25% of donors and 30% of recipients) supported contacting a recipient’s friend, partner, or spouse for more information about the recipient. Respondents answered similarly about contacting a donor’s friend, partner, or spouse for more information about the donor. Approximately one half supported the use of the Internet to obtain more information about the donor and about the recipient. Donors and recipients did not differ significantly in their beliefs for any of these questions.
Table 2.
Who should share information and how should the information be obtained?
| Question | Donors | Recipients |
|---|---|---|
| Who should share donor information with the recipient? | 160 | 75 |
| No one | 8 (5) | 3 (4) |
| Prospective donor/prospective recipient | 14 (9) | 9 (12) |
| Transplant team | 52 (33) | 32 (43) |
| Prospective donor and transplant team | 86 (54) | 31 (41) |
| Who should share recipient information with the donor? | 160 | 76 |
| No one | 8 (5) | 4 (5) |
| Prospective donor/ prospective recipient | 20 (13) | 12 (16) |
| Transplant team | 45 (28) | 25 (33) |
| Prospective donor and transplant team | 87 (54) | 35 (46) |
| How should donor information be obtained? | 160 | 75 |
| Contact friend, partner, or spouse | 41/157 (26) | 16/74 (22) |
| Internet (e.g., Facebook or Google) | 80/159 (50) | 35/75 (47) |
| How should recipient information be obtained? | 160 | 76 |
| Contact friend, partner, or spouse | 39/159 (25) | 23/76 (30) |
| Internet (e.g., Facebook or Google) | 82/159 (52) | 34/76 (45) |
Data are presented as n, n (%), or a proportion (%). Percentages do not always add up to 100% due to rounding.
Respondents were also asked whether they believe recipients have a right to know why a donor is excluded from donating. The majority of both donors and recipients rejected this notion, with 79% (125 of 159) of donors and 78% (59 of 76) of recipients responding no.
Finally, donors and recipients were each asked questions about who their potential recipient/donor is, how well they know each other, and what information they have shared or intend to share with them, all of which is reflected in Table 3. In our sample, recipients were most likely to be receiving a kidney from a sibling (34%), parent (15%), or close friend (13%). The vast majority of recipients (85%) know their donor very well. Donors were most likely to be donating their kidney to a sibling (18%), parent (17%), or stranger (17%) and were less likely to know their recipient very well (64%). The majority were in agreement with sharing every single characteristic with their prospective recipient/donor. For each characteristic, those who knew their intended recipient or donor very well were more likely to share information (data not shown, P<0.05).
Table 3.
Relationship of donors and recipients
| Question | Donors | Recipients |
|---|---|---|
| For donors, who is your recipient/intended recipient? For recipients, who is your donor/intended donor? | 157 | 53 |
| Parent | 26 (17) | 8 (15) |
| Sibling/half-sibling/step-sibling | 29 (18) | 18 (34) |
| Spouse | 13 (8) | 6 (11) |
| Child | 11 (7) | 3 (6) |
| Grandparent | 1 (1) | 0 (0) |
| Second-degree relative | 10 (6) | 4 (8) |
| Relative of spouse/partner | 3 (2) | 0 (0) |
| Close friend | 18 (11) | 7 (13) |
| Acquaintance (church member, colleague) | 6 (4) | 0 (0) |
| Stranger | 27 (17) | 3 (6) |
| Other (paired exchange, chain) | 13 (8) | 4 (8) |
| For donors, how well do you know your recipient/intended recipient? For recipients, how well do you know your donor/intended donor? | 157 | 52 |
| Very well | 100 (64) | 44 (85) |
| Moderately well | 21 (13) | 3 (6) |
| Not well | 12 (8) | 1 (2) |
| Not at all | 24 (15) | 4 (8) |
| For donors, what do you intend to share with your recipient/intended recipient? For recipients, what do you intend to share with your donor/intended donor? | 156–160 | 49 |
| Age | 137 (86) | 46 (94) |
| Smoking status | 125 (79) | 44 (90) |
| Drug abuse | 117 (75) | 40 (82) |
| Alcohol abuse | 118 (75) | 40 (82) |
| Psychiatric disturbance | 114 (72) | 39 (80) |
| Religion | 113 (72) | 41 (84) |
| High-risk sex | 91 (58) | 39 (80) |
| Sexual orientation | 113 (72) | 44 (90) |
| Criminal record | 103 (66) | 41 (84) |
| HIV/AIDS status | Not asked | 40 (82) |
| Trouble taking medications/keeping appointments | Not asked | 40 (82) |
Data are presented as n or n (%). Percentages do not always add up to 100% due to rounding.
Discussion
Our data support three of our four hypotheses. In general, both donor and recipient respondents are willing to have a significant amount of their own information disclosed, more than is currently required by UNOS/OPTN policies. The closer the relationship, the more they are willing to share. Interestingly, they want the transplant team to be involved in the disclosure. Two potential explanations include (1) the belief that health care professionals are better situated to explain medical information or (2) relief from the responsibility of leading a conversation that might involve potentially embarrassing information.
The only hypothesis that was refuted was that both donors and recipients strongly and equally supported the donor’s right to privacy regarding why a donor is excluded, when we had originally hypothesized that recipients would be less supportive of the donor’s right to privacy.
Donors and recipients expressed similar attitudes regarding disclosure of recipient information to the donor (Figure 1). The three recipient characteristics that respondents most want to be shared are all health related: estimated waiting time, estimated life expectancy without transplant, and whether the recipients have health problems that will affect the post-transplant outcome. The two recipient characteristics for which recipients were more in favor of disclosure than donors were high-risk sex and psychiatric disturbance. Two possible explanations are that (1) recipients may believe they are receiving an extraordinary gift, and that the donor has a right to know; or (2) recipients may want to show their donors that they are worthy of the donation.
Two previous studies have shown that most donors and recipients believe that information about the recipient’s health that could affect the transplant should be shared with the donor. The first study by Hizo-Abes et al. in Ontario, Canada, found that >80% of potential donors and potential recipients agreed that recipient information should be shared with donors and >89% agreed that donor information should be shared with recipients (9). The second study by Rodrigue et al. in Boston, Massachusetts, studied potential and actual living donors as well as potential and actual transplant recipients regarding what information should be disclosed to donors and what effect such information may have on willingness to donate (8). Rodrigue and colleagues examined five specific domains: waiting time, graft survival, medical comorbidity, nonadherence, and substance abuse/psychiatric conditions. They found that most donors and recipients “felt strongly that certain types of recipient information should be shared with potential donors” (8, p. 1273). As they noted, although some of the recipient risk information was consistent with published guidelines at the time, disclosure of behavioral health patterns had not been previously addressed (8). A finding of particular relevance was that most donor and recipient respondents felt that prior graft loss as a result of nonadherence as well as a history of substance abuse or current smoking should be disclosed (8). Notably, over one half of both past and potential donors thought nonadherence might change their donation decision, and approximately 40% thought other behaviors might change their decision (8).
Our study also found that the majority of donors and recipients supported disclosing recipient health information (HIV, AIDS, heart disease, and diabetes) and recipient health-related behaviors (compliance, smoking, drugs, and alcohol). One must be cautious with regard to disclosure of these health-related behaviors because data show public willingness to discriminate against individuals with these behaviors (10–13). The only statistical differences between donor and recipient respondents were that less than one half of donors thought that recipient psychiatric disturbances or high-risk sex behaviors should be disclosed, whereas the majority of recipients thought it should be disclosed (P<0.05).
Our study is different in that it used a national listserv for recruitment, although its generalizability is limited by its opt-in membership. To our knowledge, this is the first study to examine what additional donor information donors and recipients thought should be shared with potential recipients. We found that both donors and recipients thought there should be disclosure of kidney function as well as health-related behaviors, with recipients more supportive of disclosure of the latter than donors (P<0.05). There was low interest in disclosure of non–health-related social factors such as criminal record, sexual orientation, employment status, or religion.
Our finding that both donors and recipients support greater sharing of health and health behavior information challenges the current approach to disclosure in organ transplantation. The current model of health care decision-making and information disclosure assumes an isolated autonomous individual who makes private health care decisions with his or her own physician (14,15). A number of bioethics scholars have argued that the focus on individual autonomy fails to fully capture moral agency, which is often inextricably intertwined in the family (16–19). A reevaluation of current policies should be considered, given that UNOS data reveal that over two thirds of living donor kidney transplants involve first-degree relatives, with a parent, child, sibling, or spouse as the donor (20). Interestingly, although our donor sample involves a high percentage of nondirected donors, they also support greater disclosure—giving further support for a reevaluation of current policies and practices.
Because most donors and recipients know each other well and their lives are intertwined, they may share health information and health-related behavior information with each other separate from their transplant interactions, and they may also choose to obtain information from other sources, again, not related to their transplant interactions. Our data suggest that many donors and recipients support such opportunities. Although our respondents showed reluctance in asking friends, spouses, and partners for information about prospective donors and recipients, approximately one half would browse the Internet to get additional information. Many preferred the participation of health care professionals when sharing information. It may behoove transplant programs to assess whether individual donor-recipient pairs want to share more information and if so, to offer to help facilitate this. In our current system, this would require permission and consensus of what is shared by the donor, the recipient, and the transplant team, with any party able to veto additional disclosure. Whether the presumption of strict privacy should be the norm needs further discussion and analysis.
There are four limitations of our results. First is the low response rate, which is typical for Internet surveys sent to a mailing list (21). Second, the survey offered discrete-choice responses to facilitate completion, but this may not capture the complexity and nuances of the respondents’ attitudes. Third, respondents were at different stages in the donation and transplant process, and attitudes and disclosure practices may change with time and with changes in the legal and regulatory climate. Fourth, although the NKF listserv is a national listserv, its members self-select to join, and our respondents do not reflect the national demographics of living donors nor of individuals with ESRD. Rather, our respondents are more likely to self-identify as female or white and are more likely to have achieved higher educational status than is representative of the living donor and ESRD communities. Our sample was also not representative based on donor-recipient relationship. UNOS national data show that more than two thirds of donors and recipients are parents, siblings, children, or spouses. Our recipient respondents’ demographics were aligned with national data; however, nondirected donors were heavily overrepresented in our sample (17% versus <2% in the national sample) (20). This may mean that the donors who responded to our survey do not know their intended recipient as well as a more typical donor. Because a closer relationship correlates with greater willingness to share information, our data may underestimate actual donor interest in sharing of information.
In living donor transplantation, most donors and recipients want a significant amount of health information to be disclosed. The closer the relationship, the more they are willing to share. There is some reticence, however, about sharing social information. Additional stakeholders need to be surveyed to understand the public’s attitude toward the relative merits of privacy versus the right to know.
Disclosures
None.
Supplementary Material
Acknowledgments
The authors thank Jennifer Martin of the NKF for help in distributing the survey.
L.M. and J.M. were supported by funding from the University of Chicago Summer Research Program and the National Institutes of Health (Grant 2T35D062719-26 to Principal Investigator Eugene Chang). J.R.T. and L.F.R. were supported by Robert Wood Johnson Investigator Awards in Health Policy. L.F.R. is also supported by the National Library of Medicine (Ethical and Policy Issues in Living Donor Transplantation Grant 1G13LM009096).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.02280215/-/DCSupplemental.
References
- 1.US Department of Health and Human Services, Advisory Committee on Transplantation: Summary Recommendations to the Secretary. Available at http://organdonor.gov/legislation/advisory.html#recommendations. Accessed May 19, 2015
- 2.Joint Working Party of the British Transplantation Society and the Renal Association: United Kingdom guidelines for living donor kidney transplantation, 3rd Ed., 2011. Available at https://www.bts.org.uk/Documents/Guidelines/Active/UK%20Guidelines%20for%20Living%20Donor%20Kidney%20July%202011.pdf. Accessed May 19, 2015
- 3.Ethics Committee of the Transplantation Society : The consensus statement of the Amsterdam forum on the care of the live kidney donor. Transplantation 78: 491–492, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Abecassis M, Adams M, Adams P, Arnold RM, Atkins CR, Barr ML, Bennett WM, Bia M, Briscoe DM, Burdick J, Corry RJ, Davis J, Delmonico FL, Gaston RS, Harmon W, Jacobs CL, Kahn J, Leichtman A, Miller C, Moss D, Newmann JM, Rosen LS, Siminoff L, Spital A, Starnes VA, Thomas C, Tyler LS, Williams L, Wright FH, Youngner S, Live Organ Donor Consensus Group : Consensus statement on the live organ donor. JAMA 284: 2919–2926, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Adams PL, Cohen DJ, Danovitch GM, Edington RM, Gaston RS, Jacobs CL, Luskin RS, Metzger RA, Peters TG, Siminoff LA, Veatch RM, Rothberg-Wegman L, Bartlett ST, Brigham L, Burdick J, Gunderson S, Harmon W, Matas AJ, Thistlethwaite JR, Delmonico FL: The nondirected live-kidney donor: Ethical considerations and practice guidelines: A National Conference Report. Transplantation 74: 582–589, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Seem DL, Lee I, Umscheid CA, Kuehnert MJ, United States Public Health Service : PHS guideline for reducing human immunodeficiency virus, hepatitis B virus, and hepatitis C virus transmission through organ transplantation. Public Health Rep 128: 247–343, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Organ Procurement and Transplantation Network (OPTN): OPTN Policies: Policy 15: Identification of Transmissible Diseases, 15.3 Informed Consent of Transmissible Disease Risk, 2015. Available at http://optn.transplant.hrsa.gov/ContentDocuments/OPTN_Policies.pdf. Accessed May 19, 2015
- 8.Rodrigue JR, Ladin K, Pavlakis M, Mandelbrot DA: Disclosing recipient information to potential living donors: Preferences of donors and recipients, before and after surgery. Am J Transplant 11: 1270–1278, 2011 [DOI] [PubMed] [Google Scholar]
- 9.Hizo-Abes P, Young A, Reese PP, McFarlane P, Wright L, Cuerden M, Garg AX, Donor Nephrectomy Outcomes Research (DONOR) Network : Attitudes to sharing personal health information in living kidney donation. Clin J Am Soc Nephrol 5: 717–722, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neuberger J: Public and professional attitudes to transplanting alcoholic patients. Liver Transpl 13[Suppl 2]: S65–S68, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Sears SF, Jr, Marhefka SL, Rodrigue JR, Campbell C: The role of patients’ ability to pay, gender, and smoking history on public attitudes toward cardiac transplant allocation: An experimental investigation. Health Psychol 19: 192–196, 2000 [PubMed] [Google Scholar]
- 12.Johri M, Ubel PA: Setting organ allocation priorities: Should we care what the public cares about? Liver Transpl 9: 878–880, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Ubel PA, Baron J, Asch DA: Social responsibility, personal responsibility, and prognosis in public judgments about transplant allocation. Bioethics 13: 57–68, 1999 [DOI] [PubMed] [Google Scholar]
- 14.Beauchamp TL, Childress JF: Principles of Biomedical Ethics, 4th Ed., New York, Oxford University Press, 1994 [Google Scholar]
- 15.Jonsen AR, Siegler M, Winslade WJ: Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine, 7th Ed., New York, McGraw Hill Medical, 2010 [Google Scholar]
- 16.Elliott C: Doing harm: Living organ donors, clinical research and The Tenth Man. J Med Ethics 21: 91–96, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crouch RA, Elliott C: Moral agency and the family: The case of living related organ transplantation. Camb Q Healthc Ethics 8: 275–287, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Blustein J: The family in medical decisionmaking. Hastings Cent Rep 23: 6–13, 1993 [PubMed] [Google Scholar]
- 19.Hardwig J: What about the family? Hastings Cent Rep 20: 5–10, 1990 [PubMed] [Google Scholar]
- 20.Organ Procurement and Transplantation Network (OPTN): OPTN National Data Reports. Available at: http://optn.transplant.hrsa.gov/converge/latestData/step2.asp. Accessed May 19, 2015
- 21.Constant Contact: Knowledge base. Available at http://support2.constantcontact.com/articles/FAQ/2344. Accessed May 19, 2015
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.