Abstract
Background and objectives
CD14 plays a key role in the innate immunity as pattern-recognition receptor of endotoxin. Higher levels of soluble CD14 (sCD14) are associated with overall mortality in hemodialysis patients. The influence of kidney function on plasma sCD14 levels and its relationship with adverse outcomes in patients with CKD not yet on dialysis is unknown. This study examines the associations between plasma levels of sCD14 and endotoxin with adverse outcomes in patients with CKD.
Design, setting, participants, & measurements
We measured plasma levels of sCD14 and endotoxin in 495 Leuven Mild-to-Moderate CKD Study participants. Mild-to-moderate CKD was defined as presence of kidney damage or eGFR<60 ml/min per 1.73 m2 for ≥3 months, with exclusion of patients on RRT. Study participants were enrolled between November 2005 and September 2006.
Results
Plasma sCD14 was negatively associated with eGFR (ρ=–0.34, P<0.001). During a median follow-up of 54 (interquartile range, 23–58) months, 53 patients died. Plasma sCD14 was predictive of mortality, even after adjustment for renal function, Framingham risk factors, markers of mineral bone metabolism, and nutritional and inflammatory parameters (hazard ratio [HR] per SD higher of 1.90; 95% confidence interval [95% CI],1.32 to 2.74; P<0.001). After adjustment for the same risk factors, plasma sCD14 was also a predictor of cardiovascular disease (HR, 1.30; 95% CI, 1.00 to 1.69; P=0.05). Although plasma sCD14 was associated with progression of CKD, defined as reaching ESRD or doubling of serum creatinine in models adjusted for CKD-specific risk factors (HR, 1.24; 95% CI, 1.01 to 1.52; P=0.04), significance was lost when adjusted for proteinuria (HR, 1.19; 95% CI, 0.96 to 1.48; P=0.11). There was neither correlation between plasma endotoxin and sCD14 (ρ=–0.06, P=0.20) nor was endotoxin independently associated with adverse outcome during follow-up.
Conclusions
Plasma sCD14 is elevated in patients with decreased kidney function and associated with mortality and cardiovascular disease in patients with CKD not yet on dialysis.
Keywords: soluble CD14, endotoxin, inflammation, microbiome, CKD
Introduction
CKD is an important and independent risk factor for cardiovascular disease (CVD) and death (1). In an ongoing search for determinants underlying the increased incidence of adverse outcomes in CKD, subclinical endotoxemia may be an attractive factor to explore. The human gut is host to 100 trillion commensal organisms, which contributes to an enteric reservoir of about 1 g of endotoxin (2). Impaired gut barrier function in CKD could permit translocation of gut-derived endotoxin into the systemic circulation (3–5). The Bruneck Study showed that elevated plasma levels of endotoxin are associated with CVD in the general population (6). Endotoxemia has also been shown to be related to inflammation and atherosclerosis in peritoneal dialysis patients (7). However, the effect of subclinical endotoxemia in patients with CKD has not been fully elucidated.
Actions of endotoxin or LPS are mediated by interaction with the Toll-like receptor 4/MD-2 complex and its coreceptor CD14 on monocytic cells, initiating an innate immune response and proinflammatory signaling (Supplemental Figure 1) (8,9). CD14 is either membrane-bound with a glycosylphosphatidylinositol anchor or present as a soluble molecule (soluble CD14 [sCD14]) after secretion or enzymatically cleavage (10). sCD14 can participate in cell activation indirectly by promoting transfer of LPS to membrane-bound CD14 (11) or directly by transferring LPS to Toll-like receptor 4/MD-2 complex on cells that do not express membrane-bound CD14 (12). The level of sCD14 increases in response to an LPS challenge (13).
We previously reported that plasma sCD14, but not endotoxin, is a predictor of mortality in maintenance hemodialysis patients (14,15). However, endotoxemia in hemodialysis patients may be caused by translocation from dialysate into the blood compartment (16). Therefore, it is important to understand the determinants of circulating endotoxin and plasma sCD14 in patients with CKD. In this study we tested the hypothesis that elevated plasma sCD14 and endotoxin are associated with CVD, mortality, and loss of kidney function in patients with CKD not yet on dialysis.
Materials and Methods
Study Population
This was an ancillary study of the Leuven Mild-to-Moderate CKD cohort, a prospective cohort to investigate the role of uremic retention solutes in patients with CKD not yet on dialysis (clinicaltrials.gov NCT00441623) (17). Prevalent CKD patients, followed at the nephrology outpatient clinic of the University Hospitals Leuven, were eligible for inclusion, with enrollment between November 2005 and September 2006. Mild-to-moderate CKD was defined as presence of kidney damage (i.e., pathologic abnormalities, abnormalities in urine or imaging tests) or eGFR by CKD Epidemiology Collaboration (CKD-EPI) equation <60 ml/min per 1.73 m2 for ≥3 months, with exclusion of patients on RRT. The study was performed according to the Declaration of Helsinki and approved by the ethics committee of the University Hospitals Leuven. Informed consent was obtained from all patients.
Laboratory Measurements
At inclusion, blood was taken for measurement of hemoglobin (g/dl), albumin (g/l), C-reactive protein (CRP; mg/l), cholesterol (mg/dl), calcium (mg/dl), phosphate (mg/dl), biointact parathyroid hormone (PTH) (ng/L), creatinine (mg/dl), urea (mg/dl), sCD14 (µg/ml), and endotoxin (EU/ml). Hemoglobin, albumin, CRP, cholesterol, calcium, phosphate, biointact PTH, creatinine, and urea were all measured using standard laboratory techniques. The eGFR was calculated using the CKD-EPI equation (18). Plasma sCD14 concentration was determined using ELISA (sCD14 Quantikine ELISA Kit; R&D Systems, MN; minimum detectable level of 125 pg/ml). The inter- and intra-assay coefficients of variations are <7.5% and <6.5%, respectively. Plasma levels of endotoxin were quantified by kinetic chromogenic limulus amebocyte lysate (LAL) assay (Kinetic-QCL; Lonza, MD; sensitivity range, 0.005–50 EU/ml). The coefficient of variation was 3%–9%. For sCD14 and endotoxin, all samples were tested in duplicate, and mean values were reported.
End Point Evaluation
Patients were prospectively followed at 3- to 6-month intervals until December 31, 2010, with recording of predefined end points (i.e., overall mortality, first cardiovascular [CV] event, progression of CKD). Cause of death was classified as either CV, infectious, malignancy, or other. CV deaths included fatal myocardial infarction, sudden death, and death caused by congestive heart failure. Out-of-hospital deaths were coded after consultation of the general practitioner. First CV event was a composite of cardiac death, nonlethal cardiac event, ischemic stroke, or peripheral vascular disease, whichever occurred first. Nonlethal cardiac events included myocardial infarction, diagnosed on the basis of elevated levels of cardiac enzymes and/or typical electrocardiography changes, myocardial ischemia with typical electrocardiography changes without elevated cardiac enzymes, coronary intervention (thrombolysis, percutaneous coronary intervention, or coronary artery bypass grafting), and ventricular arrhythmia. Ischemic stroke was defined as a neurologic deficit lasting >24 hours. Peripheral vascular disease included new-onset ischemic lower-limb pain, with abnormal ankle brachial pressure index or radiologic evidence of peripheral vascular disease, new-onset ischemic necrotic lesions, or surgical arterial intervention. Progression of CKD was defined as reaching ESRD or doubling of serum creatinine during follow-up.
Statistical Analyses
Data are expressed as mean (SD) for normally distributed variables or median (interquartile range [IQR]) for non-normally distributed variables. Differences between baseline variables according to tertiles of plasma sCD14 were tested using parametric ANOVA, Kruskal–Wallis test, or chi-squared test as appropriate. Spearman rank correlation coefficients were used to calculate correlations between plasma sCD14 and other variables. Independent determinants of plasma sCD14 were identified using multivariate linear regression analysis. For this purpose, prespecified demographic (i.e., age, sex, presence of diabetes mellitus, smoking status, body mass index) and biochemical (i.e., hemoglobin, CRP, albumin, eGFR, 24-hour proteinuria, endotoxin) parameters were subjected to a first backward elimination procedure on P<0.2 and a final backward elimination step on P<0.05. Cumulative incidence of the end point was estimated with the Kaplan–Meier method using the log-rank test to compare differences between tertiles of plasma sCD14. Time to first event analysis was performed using Cox proportional hazards analysis. For multivariate analysis, a double backward elimination approach was used with inclusion of all variables at P<0.20 for secondary backward elimination at P<0.05. To test the proportionality assumption, each model was tested against log (time) with the use of time-dependent covariates when the proportionality assumption was violated. With respect to overall mortality, for both Kaplan–Meier and Cox proportional hazard analysis, data were censored at start of RRT, loss to follow-up, or at the end of the study observation period. For analysis of the first CV event, censoring was performed at the start of RRT, death other than CV, loss to follow-up, or study end, whereas for progression of CKD, data were censored at death, loss to follow-up, or end of the study period. For all statistical analysis, P<0.05 was considered significant. Statistical analysis was performed using SAS (version 9.3; SAS Institute, Cary, NC).
Results
Study Population
Between November 2005 and September 2006, 495 prevalent patients with CKD Kidney Disease Outcomes Quality Initiative stages 1–5 followed at the nephrology outpatient clinic of the University Hospitals Leuven, Belgium, were included in the Leuven Mild-to-Moderate CKD Study (clinicaltrials.gov NCT00441623) (17). Measurements of sCD14 and endotoxin were available in a total of 495 patients (Supplemental Figure 2). Baseline characteristics of the study population are presented in Table 1. Glomerular disease was the most prevalent underlying renal disease (27.9%), followed by vascular disease (10.1%), diabetic nephropathy (8.7%), autosomal dominant polycystic disease (8.7%), and tubulointerstitial disease (4.0%).
Table 1.
Baseline characteristics of the study population
| Variable | Overall: 1.92–7.29 µg/ml (N=495) | sCD14 | P Value | ||
|---|---|---|---|---|---|
| Tertile 1: 1.918–3.318 µg/ml (n=165) | Tertile 2: 3.319–4.106 µg/ml (n=165) | Tertile 3: 4.122–7.291 µg/ml (n=165) | |||
| Age (y) | 64 (50–75) | 58 (46–72) | 70 (52–77) | 64 (53–74) | <0.001 |
| Sex, male (%) | 271 (54.7) | 105 (63.6) | 84 (50.9) | 82 (49.7) | 0.01 |
| Prior CVD, yes (%) | 137 (27.7) | 33 (20.0) | 51 (30.9) | 53 (32.1) | 0.01 |
| Diabetes, yes (%) | 89 (18.0) | 25 (15.2) | 34 (20.6) | 30 (18.2) | 0.47 |
| Current smoker, yes (%) | 90 (18.2) | 30 (18.2) | 27 (16.4) | 33 (20.0) | 0.67 |
| Body mass index (kg/m2) | 25.69 (22.99–29.06) | 25.96 (23.41–30.02) | 25.51 (22.49–29.45) | 24.91 (22.86–28.34) | 0.12 |
| Systolic BP (mmHg) | 135 (120–150) | 130 (120–150) | 140 (125–160) | 135 (120–150) | 0.02 |
| Diastolic BP (mmHg) | 80 (70–85) | 80 (70–88) | 80 (70–85) | 80 (70–80) | 0.26 |
| Hemoglobin (g/dl) | 13.4±1.8 | 14.0±1.8 | 13.3±1.8 | 12.8±1.5 | <0.001 |
| Albumin (g/dl) | 4.48 (4.24–4.68) | 4.56 (4.24–4.74) | 4.45 (4.16–4.67) | 4.47 (4.29–4.64) | 0.01 |
| C-reactive protein (mg/L) | 2 (1–6) | 1 (1–3) | 2 (1–5) | 3 (1–7) | <0.001 |
| Cholesterol (mg/dl) | 178 (152–205) | 179 (156–207) | 178 (156–201) | 176 (148–205) | 0.45 |
| LDL (mg/dl) | 85 (67–112) | 89 (68–115) | 88 (69–114) | 81 (61–104) | 0.07 |
| HDL (mg/dl) | 57 (48–72) | 55 (48–70) | 58 (49–71) | 58 (47–74) | 0.67 |
| Calcium (mg/dl) | 9.6 (9.2–9.9) | 9.6 (9.3–9.9) | 9.6 (9.2–9.9) | 9.5 (9.2–9.9) | 0.85 |
| Phosphate (mg/dl) | 3.3 (2.9–3.8) | 3.2 (2.8–3.6) | 3.4 (3.0–3.8) | 3.5 (3.1–4.0) | <0.001 |
| Parathormone (pg/ml) | 23.8 (12.7–52.0) | 17.5 (9.3–37.4) | 27.1 (16.2–58.9) | 30.2 (14.3–57.9) | <0.001 |
| Creatinine (mg/dl) | 1.79 (1.27–2.47) | 1.51 (1.09–1.97) | 1.83 (1.34–2.56) | 2.00 (1.46–2.86) | <0.001 |
| eGFR (ml/min per 1.73 m2) | 34 (23–55) | 46 (31–72) | 32 (22–50) | 28 (18–41) | <0.001 |
| 24-hour proteinuria (g) | 0.28 (0.11–0.88) | 0.19 (0.10–0.59) | 0.29 (0.11–1.08) | 0.43 (0.12–1.01) | 0.04 |
| Therapy with ACEI/ARB, yes (%) | 349 (70.5) | 118 (71.5) | 116 (70.3) | 115 (69.7) | 0.72 |
| Therapy with statins, yes (%) | 238 (48.1) | 75 (45.5) | 82 (49.7) | 81 (49.1) | 0.51 |
| Therapy with 25-OH-vitamin D, yes (%) | 92 (18.6) | 23 (13.9) | 26 (15.8) | 43 (26.1) | <0.01 |
| Therapy with phosphate binder, yes (%) | 136 (27.5) | 31 (18.1) | 50 (30.3) | 55 (33.3) | 0.003 |
| sCD14 (µg/ml) | 3.72 (3.15–4.40) | 2.93 (2.65–3.15) | 3.72 (3.52–3.89) | 4.69 (4.40–5.22) | <0.001 |
| Endotoxin (EU/ml) | 0.71 (0.38–1.3) | 0.82 (0.45–1.49) | 0.64 (0.34–1.23) | 0.71 (0.38–1.3) | 0.05 |
Data are expressed as mean±SD, median (interquartile range), n (%), or as otherwise indicated. Differences between tertiles were tested using parametric ANOVA, Kruskal–Wallis test, or chi-squared test, as appropriate. CVD, cardiovascular disease; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; 25-OH-vitamin D, 25-hydroxy-vitamin D; sCD14, soluble CD14.
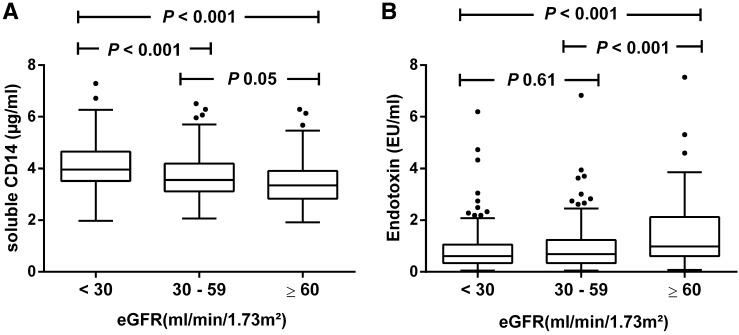
Determinants of Plasma sCD14
The median level of sCD14 was 3.72 µg/ml (IQR, 3.15–4.40). There was a significant and graded inverse relationship between plasma sCD14 and eGFR (Spearman rank correlation ρ=–0.34, P<0.001) (Figure 1A). A higher level of plasma sCD14 was also significantly correlated with older age (ρ=0.13, P=0.003), female sex (ρ=0.12, P<0.01), and prior CVD (ρ=0.12, P<0.01). sCD14 was also associated with lower levels of hemoglobin (ρ=–0.31, P<0.001), LDL (ρ=–0.09, P=0.04), and serum albumin (ρ=–0.10, P=0.03). CRP (ρ=0.20, P<0.001), phosphate (ρ=0.22, P<0.001), PTH (ρ=0.18, P<0.001), and 24-hour proteinuria (ρ=0.12, P=0.02) were positively associated with sCD14 (Supplemental Table 1). There was no correlation between plasma sCD14 and endotoxin (ρ=–0.06, P=0.20). Plasma endotoxin was significantly correlated with eGFR (ρ=0.21, P<0.001), with higher levels present in patients with eGFR>60 ml/min per 1.73 m2 (Figure 1B).
Figure 1.
Plasma soluble CD14, endotoxin, and renal function. Distribution of plasma soluble CD14 (A) and endotoxin (B) levels as a function of eGFR. Between-group comparisons are Bonferroni-corrected.
In multivariate regression analysis, independent determinants of plasma sCD14 were body mass index (β=–0.01, P=0.01), hemoglobin (β=–0.02, P<0.001), CRP (β=0.04, P<0.001), and eGFR (β=–0.09, P<0.001) (model R2=0.18) (Supplemental Table 2). Plasma endotoxin was not associated with plasma sCD14 (P=0.24).
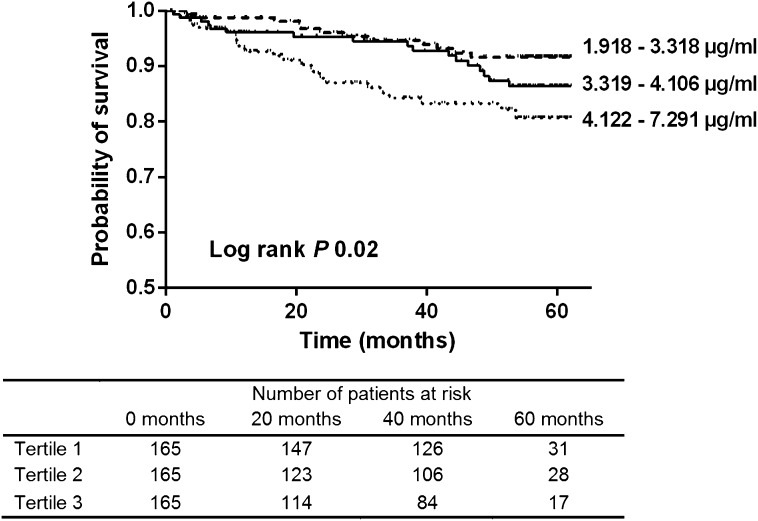
sCD14 and Mortality
During a median follow-up of 54 (IQR, 23–58) months, 53 patients died (Supplemental Table 3), with more deaths observed among patients with sCD14 in higher tertiles (tertiles 1–3: 12, 17, and 24 events, respectively; log-rank test, P=0.02) (Figure 2). In univariate Cox proportional hazard analysis, plasma sCD14 was significantly associated with mortality (hazard ratio [HR] per SD higher of 1.81; 95% confidence interval [95% CI], 1.36 to 2.41; P<0.001) (Table 2). This association remained significant in various multivariate models with adjustment for kidney function, Framingham risk factors, markers of mineral bone metabolism, CRP, and serum albumin (HR, 1.90; 95% CI, 1.32 to 2.74; P<0.001). Although we also noted a significant, albeit inverse, relationship between plasma levels of endotoxin and risk of death in univariate Cox proportional hazard analysis (HR, 0.61; 95% CI, 0.47 to 0.79; P<0.001), plasma endotoxin was not predictive of mortality after adjustment for the same risk factors as in the previous analysis (HR, 0.96; 95% CI, 0.70 to 1.32; P=0.80).
Figure 2.
Kaplan–Meier showing death by tertiles of soluble CD14 concentration. Tertiles 1–3: 12, 17, and 24 deaths, respectively. Log-rank test, P=0.02.
Table 2.
Multivariate analysis showing association of plasma soluble CD14 and mortality
| Variable | Hazard Ratio (95% CI) Per SD Higher | P Value |
|---|---|---|
| Unadjusted: sCD14 (Ln) | 1.81 (1.36 to 2.41) | <0.001 |
| Adjusted for renal function: eGFR (Ln) | 1.65 (1.21 to 2.26) | 0.002 |
| Adjusted for Framingham risk factors: age, sex, systolic BP, current smoker, diabetes mellitus, cholesterol | 1.86 (1.37 to 2.55) | <0.001 |
| Full model: adjusted for creatinine (Ln), age, sex, systolic BP, current smoker, diabetes mellitus, cholesterol, calcium, phosphate, parathyroid hormone (Ln), C-reactive protein (Ln), albumin | 1.90 (1.32 to 2.74) | <0.001 |
sCD14, soluble CD14; 95% CI, 95% confidence interval.
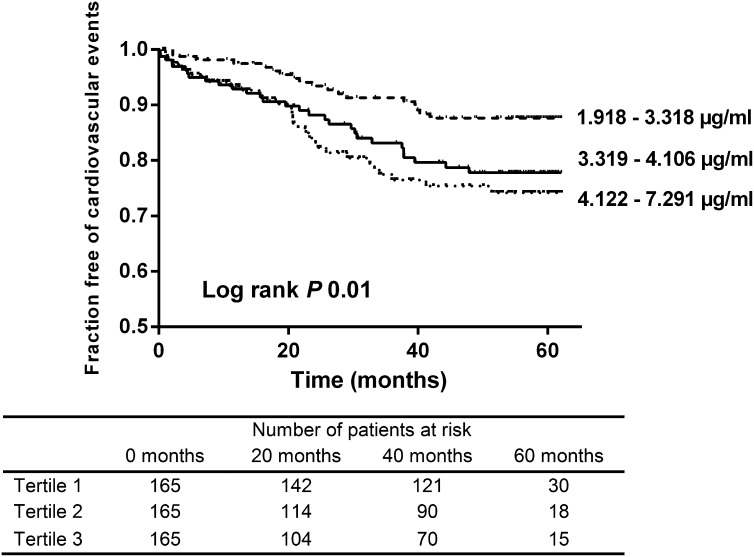
sCD14 and CVD
Next, we explored the relationship between plasma sCD14 and CVD. A total of 78 CV events were observed during follow-up (52 [17–58] months) (Supplemental Table 4). The number of events was higher among patients in higher sCD14 tertiles (tertiles 1–3: 18, 29, and 31 events, respectively; log-rank test, P=0.01) (Figure 3). In unadjusted analysis, plasma sCD14 was significantly associated with CV events during follow-up (HR, 1.43; 95% CI, 1.13 to 1.81; P=0.003) (Table 3). This association remained highly significant after adjustment for Framingham risk factors (HR, 1.44; 95% CI, 1.12 to 1.85; P=0.004). Significance was lost when adjusted for eGFR (HR, 1.22; 95 CI, 0.95 to 1.57; P=0.11). However, there was significant interaction between eGFR and plasma sCD14 in this model (P=0.03). In the full multivariate model, plasma sCD14 was a borderline significant predictor of CV events during follow-up (HR, 1.30; 95 CI, 1.00 to 1.69; P=0.05). There was a significant inverse relationship between endotoxin levels and CVD in unadjusted analysis (HR, 0.69; 95% CI, 0.56 to 0.86; P<0.001), but not in the fully adjusted model (HR, 0.99; 95 CI, 0.78 to 1.26; P=0.95).
Figure 3.
Kaplan–Meier curve of time to first cardiovascular event by tertiles of soluble CD14 concentration. Tertiles 1–3: 18, 29, and 31 cardiovascular events, respectively. Log-rank test, P=0.01.
Table 3.
Cox proportional hazard analysis of time to first cardiovascular event
| Variable | Hazard Ratio (95% CI) Per SD Higher | P Value |
|---|---|---|
| Unadjusted: sCD14 (Ln) | 1.43 (1.13 to 1.81) | 0.003 |
| Adjusted for renal function: eGFR (Ln) | 1.22 (0.95 to 1.57) | 0.11 |
| Adjusted for Framingham risk factors: age, sex, systolic BP, current smoker, diabetes mellitus, cholesterola | 1.44 (1.12 to 1.85) | 0.004 |
| Full model: adjusted for creatinine (Ln), age, sex, systolic BP, current smoker, diabetes mellitus, cholesterol, calcium, phosphate, parathyroid hormone (Ln), C-reactive protein (Ln), albumina | 1.30 (1.00 to 1.69) | 0.05 |
sCD14, soluble CD14; 95% CI, 95% confidence interval.
Age and cholesterol entered as time-dependent covariate.
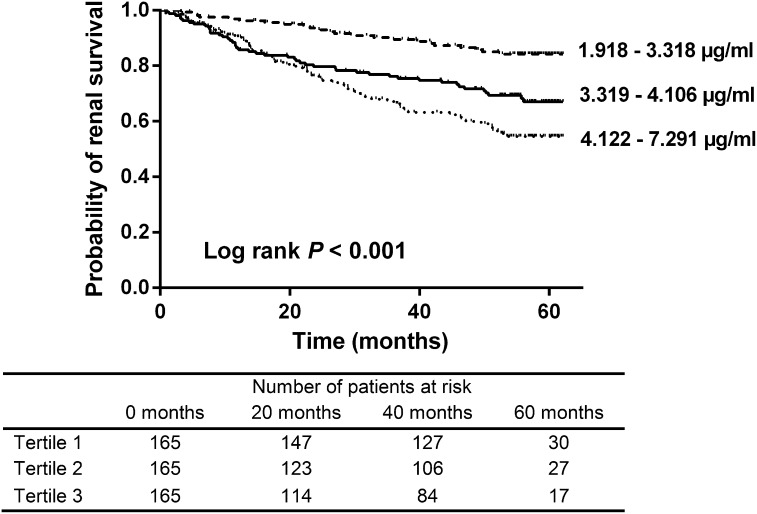
sCD14 and Progression of CKD
We also examined the potential associations between plasma sCD14 and progression of CKD, defined as reaching ESRD or doubling of serum creatinine. During a median follow-up of 53 (IQR, 22–58) months, 132 patients were classified as having progressive CKD. We observed more CKD progressors among patients in higher tertiles of sCD14 (tertiles 1–3: 23, 47, and 62 events, respectively; log-rank test, P<0.001) (Figure 4). Plasma sCD14 was a significant predictor of CKD progression in the unadjusted analysis (HR, 1.66; 95% CI, 1.39 to 1.99; P<0.001) (Table 4). When adjusted for eGFR, this association was no longer significant (HR, 1.20; 95% CI, 0.99 to 1.47; P=0.06). In the full model, including CKD-specific and Framingham risk factors and CRP and serum albumin, plasma sCD14 remained a significant predictor of CKD progression (HR, 1.24; 95% CI, 1.01 to 1.52; P=0.04). However, when proteinuria was added in the model, the significance was lost (HR, 1.19; 95% CI, 0.96 to 1.48; P=0.11). Plasma endotoxin was not significantly associated with progression of CKD in both unadjusted (HR, 0.84; 95% CI, 0.71 to 1.00; P=0.06) and full multivariate (HR, 1.08; 95% CI, 0.88 to 1.33; P=0.44) models.
Figure 4.
Kaplan–Meier renal survival curve by tertiles of soluble CD14 concentration. Tertiles 1–3: 23, 47, and 62 renal progressors, respectively. Log-rank test, P<0.001.
Table 4.
Multivariable Cox proportional hazard model showing association between soluble CD14 and progression of CKDa
| Variable | Hazard Ratio (95% CI) Per SD Higher | P Value |
|---|---|---|
| Unadjusted: sCD14 (Ln) | 1.66 (1.39 to 1.99) | <0.001 |
| Adjusted for renal function: eGFR (Ln) | 1.20 (0.99 to 1.47) | 0.06 |
| Adjusted for Framingham risk factors: age, sex, systolic BP, current smoker, diabetes mellitus, cholesterol | 1.65 (1.37 to 1.98) | <0.001 |
| Full model: adjusted for creatinine (Ln), hemoglobin, bicarbonate, calcium, phosphate, parathyroid hormone (Ln), urea (Ln), therapy with ACE/ARB, age, sex, systolic BP, current smoker, diabetes mellitus, cholesterol, C-reactive protein (Ln), albumin | 1.24 (1.01 to 1.52) | 0.04 |
| Full model + 24-h proteinuria (n=412) | 1.19 (0.96 to 1.48) | 0.11 |
sCD14, soluble CD14; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; 95% CI, 95% confidence interval.
Reaching ESRD or doubling of serum creatinine during follow-up.
Discussion
In this study we examined the role of plasma sCD14 and endotoxin in patients with CKD not yet on dialysis. The key findings are as follows: (1) there is a graded relationship between plasma sCD14 and renal function, with higher levels of plasma sCD14 present in patients with more advanced CKD; (2) plasma sCD14 is a strong and independent predictor of mortality; (3) an elevated level of sCD14 is associated with CV events during follow-up; and (4) there is no significant association between plasma endotoxin and adverse outcomes in patients with CKD.
Endotoxin refers to the biologically active LPS complex associated with the outer membrane of gram-negative bacteria. Endotoxin provokes an array of host responses by binding to the CD14 receptor (19). Endotoxin concentrations as low as 1 pg/ml could induce cellular activation and expression of CD14 (20,21). Recent evidence indicates that sCD14 may be derived by enzymatic cleavage of glycosylphosphatidylinositol-anchored cell membrane–bound CD14 or secreted by liver in response to inflammation or infection (22). Interestingly, sCD14 can both potentiate and downregulate responses to LPS by transfer of LPS to lipoproteins for subsequent removal (23). Therefore, higher levels of sCD14 can reduce the amount of monocyte-bound LPS and attenuate the inflammatory response.
In multivariate regression analysis, kidney function, body mass index, hemoglobin, and CRP were all associated with plasma sCD14. Renal function was the strongest determinant of plasma sCD14, with higher levels of sCD14 observed in patients with lower eGFR. Reduced renal excretion might also be responsible for accumulation of plasma sCD14 in CKD (24). On the other hand, elevated sCD14 could be a response to subclinical endotoxemia. In this study, we did not observe a significant association between plasma sCD14 and endotoxin levels. Other investigators have also reported lack of association between endotoxin and sCD14 (25). Interestingly, we noted higher levels of endotoxin in patients with eGFR>60 ml/min per 1.73 m2. Previous studies have reported elevated or unchanged endotoxin levels in patients with more advanced CKD (7,26–29). This apparent discrepancy may be explained by several factors. First, the half-life of endotoxin is very short, with approximately 90% of LPS being removed within 5 minutes after entrance in the systemic circulation (30). Therefore, it may be questioned whether measurement of systemic LPS is representative of the actual exposure to endotoxin. In this regard, it may also be more logical to consider the host response to endotoxemia, of which plasma sCD14 may be a good surrogate. Second, the LAL test assay for endotoxin may be inaccurate. It has been reported that various plasma components may interfere with detection of LPS by the LAL test (31,32). Finally, CD14 is a multifunctional receptor molecule that responds to endotoxin from gram-negative bacteria and multiple other ligands (19,33), possibly confounding the relationship between plasma endotoxin and sCD14, in which sCD14 may be better considered a general marker of monocyte activation (34).
We found that higher plasma levels of sCD14 are predictive of overall mortality, even after adjustment for renal function, CV risk factors, markers of mineral bone metabolism, and inflammatory and nutritional parameters. Investigators have reported that higher levels of plasma sCD14 are associated with increased mortality in patients with HIV infection (25) and those with gram-negative sepsis (35). We also explored the relationship between sCD14 and CV events, again demonstrating the prognostic role of sCD14 with respect to CVD in CKD. In patients without CKD, an elevated sCD14 level is associated with aortic stiffness, carotid plaque formation, and unstable angina (36,37). In a CV health study, sCD14 levels were associated with both subclinical vascular disease and risk of future clinical CVD (38). sCD14 is capable of mediating LPS activation of membrane–bound negative cells, such as endothelial and smooth muscle cells, which is important in atherogenesis (12).
The relationship between plasma sCD14 and CKD progression has not been explored. We noted that sCD14 was associated with progression of CKD after adjustment for CKD-specific and CV risk factors and inflammatory and nutritional parameters. However, when adjusted for proteinuria, the significance of the association was lost. Assuming that sCD14 is a marker of endotoxin burden, this finding may expand the spectrum of renal disease caused by endotoxemia from sepsis-related AKI to CKD (39). Even low concentrations of endotoxin are capable of inducing tubular cell injury because sCD14 largely enhances sensitivity to endotoxin (24). Urine sCD14 may also be increased in patients with proteinuria (24), which either may be a consequence or a cause of proximal tubulopathy. Furthermore, CD14 is upregulated in tubular cells after kidney injury, probably mediating apoptosis (40). In a small study in patients with autosomal dominant polycystic disease, expression of CD14 in the kidney, urine sCD14, and plasma sCD14 were also related to progression of polycystic disease (41). Further research is necessary to identify the role of plasma sCD14 with respect to CKD progression.
It remains to be elucidated why plasma sCD14 associates with adverse outcomes in patients with renal dysfunction. Although plasma levels of sCD14 have been linked to exposure to endotoxin (13,21), we did not observe a correlation between endotoxin and sCD14 levels. Furthermore, plasma sCD14, but not endotoxin levels, was predictive of adverse outcomes in our cohort, a finding also noted in previous studies (14,25). This does not, however, preclude a pathophysiologic role of endotoxemia in CKD as previously explained. Whatever the cause may be, higher plasma sCD14 is indicative of a persistent activation of monocytic cells, which may contribute to microinflammation in CKD and associated adverse outcomes (42).
There are limitations to our study. First, the observational study design precludes causal inferences. Second, unavailability of urine sCD14 measurements does not allow for the gain of more insights in the renal handling of sCD14. Third, our study population mainly consists of patients who are white. Care must be taken when extrapolating our data to other patient populations. Finally, our analyses are on the basis of single baseline biochemical measurements that are potentially subjected to certain variability over time.
In conclusion, levels of plasma sCD14 are elevated in patients with more advanced CKD. In addition, elevated plasma sCD14 is associated with mortality and CVD. The association between sCD14 and CKD progression was significantly attenuated by addition of proteinuria in the model. The plasma endotoxin level was not associated with any clinical outcome in our study. The potential utility of sCD14 as a prognostic and therapeutic target in CKD requires further investigation.
Disclosures
None.
Supplementary Material
Acknowledgments
RP is the recipient of a fellowship of the Research Foundation - Flanders (FWO) (grant 11E9813N). Part of the research has been funded by the Research Foundation - Flanders (FWO) (grant G077514N). DR is supported by the National Institutes of Health Grants 1R01-DK073665-01A1, 1U01-DK099924-01, and 1U01-DK099914-01.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03100315/-/DCSupplemental.
References
- 1.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 2.Berg RD: The indigenous gastrointestinal microflora. Trends Microbiol 4: 430–435, 1996 [DOI] [PubMed] [Google Scholar]
- 3.Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, Desantis TZ, Ni Z, Nguyen TH, Andersen GL: Chronic kidney disease alters intestinal microbial flora. Kidney Int 83: 308–315, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Vaziri ND, Yuan J, Rahimi A, Ni Z, Said H, Subramanian VS: Disintegration of colonic epithelial tight junction in uremia: A likely cause of CKD-associated inflammation. Nephrol Dial Transplant 27: 2686–2693, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magnusson M, Magnusson KE, Sundqvist T, Denneberg T: Impaired intestinal barrier function measured by differently sized polyethylene glycols in patients with chronic renal failure. Gut 32: 754–759, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiedermann CJ, Kiechl S, Dunzendorfer S, Schratzberger P, Egger G, Oberhollenzer F, Willeit J: Association of endotoxemia with carotid atherosclerosis and cardiovascular disease: Prospective results from the Bruneck Study. J Am Coll Cardiol 34: 1975–1981, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Szeto CC, Kwan BC, Chow KM, Lai KB, Chung KY, Leung CB, Li PK: Endotoxemia is related to systemic inflammation and atherosclerosis in peritoneal dialysis patients. Clin J Am Soc Nephrol 3: 431–436, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyake K: Innate recognition of lipopolysaccharide by Toll-like receptor 4-MD-2. Trends Microbiol 12: 186–192, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC: CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science 249: 1431–1433, 1990 [DOI] [PubMed] [Google Scholar]
- 10.Ulevitch RJ, Tobias PS: Receptor-dependent mechanisms of cell stimulation by bacterial endotoxin. Annu Rev Immunol 13: 437–457, 1995 [DOI] [PubMed] [Google Scholar]
- 11.Hailman E, Vasselon T, Kelley M, Busse LA, Hu MC, Lichenstein HS, Detmers PA, Wright SD: Stimulation of macrophages and neutrophils by complexes of lipopolysaccharide and soluble CD14. J Immunol 156: 4384–4390, 1996 [PubMed] [Google Scholar]
- 12.Pugin J, Schürer-Maly CC, Leturcq D, Moriarty A, Ulevitch RJ, Tobias PS: Lipopolysaccharide activation of human endothelial and epithelial cells is mediated by lipopolysaccharide-binding protein and soluble CD14. Proc Natl Acad Sci U S A 90: 2744–2748, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schütt C, Schilling T, Grunwald U, Schönfeld W, Krüger C: Endotoxin-neutralizing capacity of soluble CD14. Res Immunol 143: 71–78, 1992 [DOI] [PubMed] [Google Scholar]
- 14.Raj DS, Carrero JJ, Shah VO, Qureshi AR, Bárány P, Heimbürger O, Lindholm B, Ferguson J, Moseley PL, Stenvinkel P: Soluble CD14 levels, interleukin 6, and mortality among prevalent hemodialysis patients. Am J Kidney Dis 54: 1072–1080, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raj DS, Shah VO, Rambod M, Kovesdy CP, Kalantar-Zadeh K: Association of soluble endotoxin receptor CD14 and mortality among patients undergoing hemodialysis. Am J Kidney Dis 54: 1062–1071, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coulliette AD, Arduino MJ: Hemodialysis and water quality. Semin Dial 26: 427–438, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meijers BK, Claes K, Bammens B, de Loor H, Viaene L, Verbeke K, Kuypers D, Vanrenterghem Y, Evenepoel P: p-Cresol and cardiovascular risk in mild-to-moderate kidney disease. Clin J Am Soc Nephrol 5: 1182–1189, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pugin J, Heumann ID, Tomasz A, Kravchenko VV, Akamatsu Y, Nishijima M, Glauser MP, Tobias PS, Ulevitch RJ: CD14 is a pattern recognition receptor. Immunity 1: 509–516, 1994 [DOI] [PubMed] [Google Scholar]
- 20.Erridge C, Attina T, Spickett CM, Webb DJ: A high-fat meal induces low-grade endotoxemia: Evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 86: 1286–1292, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Nockher WA, Scherberich JE: Monocyte cell-surface CD14 expression and soluble CD14 antigen in hemodialysis: Evidence for chronic exposure to LPS. Kidney Int 48: 1469–1476, 1995 [DOI] [PubMed] [Google Scholar]
- 22.Bas S, Gauthier BR, Spenato U, Stingelin S, Gabay C: CD14 is an acute-phase protein. J Immunol 172: 4470–4479, 2004 [DOI] [PubMed] [Google Scholar]
- 23.Kitchens RL, Thompson PA, Viriyakosol S, O’Keefe GE, Munford RS: Plasma CD14 decreases monocyte responses to LPS by transferring cell-bound LPS to plasma lipoproteins. J Clin Invest 108: 485–493, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bussolati B, David S, Cambi V, Tobias PS, Camussi G: Urinary soluble CD14 mediates human proximal tubular epithelial cell injury induced by LPS. Int J Mol Med 10: 441–449, 2002 [PubMed] [Google Scholar]
- 25.Sandler NG, Wand H, Roque A, Law M, Nason MC, Nixon DE, Pedersen C, Ruxrungtham K, Lewin SR, Emery S, Neaton JD, Brenchley JM, Deeks SG, Sereti I, Douek DC, INSIGHT SMART Study Group : Plasma levels of soluble CD14 independently predict mortality in HIV infection. J Infect Dis 203: 780–790, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nisbeth U, Hällgren R, Eriksson O, Danielson BG: Endotoxemia in chronic renal failure. Nephron 45: 93–97, 1987 [DOI] [PubMed] [Google Scholar]
- 27.Gonçalves S, Pecoits-Filho R, Perreto S, Barberato SH, Stinghen AE, Lima EG, Fuerbringer R, Sauthier SM, Riella MC: Associations between renal function, volume status and endotoxaemia in chronic kidney disease patients. Nephrol Dial Transplant 21: 2788–2794, 2006 [DOI] [PubMed] [Google Scholar]
- 28.McIntyre CW, Harrison LE, Eldehni MT, Jefferies HJ, Szeto CC, John SG, Sigrist MK, Burton JO, Hothi D, Korsheed S, Owen PJ, Lai KB, Li PK: Circulating endotoxemia: A novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol 6: 133–141, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taniguchi T, Katsushima S, Lee K, Hidaka A, Konishi J, Ideguchi H, Kawaguchi Y: Endotoxemia in patients on hemodialysis. Nephron 56: 44–49, 1990 [DOI] [PubMed] [Google Scholar]
- 30.Herring WB, Herion JC, Walker RI, Palmer JG: Distribution and clearance of circulating endotoxin. J Clin Invest 42: 79–87, 1963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen J: The detection and interpretation of endotoxaemia. Intensive Care Med 26[Suppl 1]: S51–S56, 2000 [DOI] [PubMed] [Google Scholar]
- 32.Mattsby-Baltzer I, Lindgren K, Lindholm B, Edebo L: Endotoxin shedding by enterobacteria: Free and cell-bound endotoxin differ in Limulus activity. Infect Immun 59: 689–695, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Devitt A, Moffatt OD, Raykundalia C, Capra JD, Simmons DL, Gregory CD: Human CD14 mediates recognition and phagocytosis of apoptotic cells. Nature 392: 505–509, 1998 [DOI] [PubMed] [Google Scholar]
- 34.Nockher WA, Wigand R, Schoeppe W, Scherberich JE: Elevated levels of soluble CD14 in serum of patients with systemic lupus erythematosus. Clin Exp Immunol 96: 15–19, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Landmann R, Zimmerli W, Sansano S, Link S, Hahn A, Glauser MP, Calandra T: Increased circulating soluble CD14 is associated with high mortality in gram-negative septic shock. J Infect Dis 171: 639–644, 1995 [DOI] [PubMed] [Google Scholar]
- 36.Zalai CV, Kolodziejczyk MD, Pilarski L, Christov A, Nation PN, Lundstrom-Hobman M, Tymchak W, Dzavik V, Humen DP, Kostuk WJ, Jablonsky G, Pflugfelder PW, Brown JE, Lucas A: Increased circulating monocyte activation in patients with unstable coronary syndromes. J Am Coll Cardiol 38: 1340–1347, 2001 [DOI] [PubMed] [Google Scholar]
- 37.Amar J, Ruidavets JB, Bal Dit Sollier C, Bongard V, Boccalon H, Chamontin B, Drouet L, Ferrières J: Soluble CD14 and aortic stiffness in a population-based study. J Hypertens 21: 1869–1877, 2003 [DOI] [PubMed] [Google Scholar]
- 38.Reiner AP, Lange EM, Jenny NS, Chaves PH, Ellis J, Li J, Walston J, Lange LA, Cushman M, Tracy RP: Soluble CD14: Genomewide association analysis and relationship to cardiovascular risk and mortality in older adults. Arterioscler Thromb Vasc Biol 33: 158–164, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schrier RW, Wang W: Acute renal failure and sepsis. N Engl J Med 351: 159–169, 2004 [DOI] [PubMed] [Google Scholar]
- 40.Morrissey J, Guo G, McCracken R, Tolley T, Klahr S: Induction of CD14 in tubular epithelial cells during kidney disease. J Am Soc Nephrol 11: 1681–1690, 2000 [DOI] [PubMed] [Google Scholar]
- 41.Zhou J, Ouyang X, Cui X, Schoeb TR, Smythies LE, Johnson MR, Guay-Woodford LM, Chapman AB, Mrug M: Renal CD14 expression correlates with the progression of cystic kidney disease. Kidney Int 78: 550–560, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kato S, Chmielewski M, Honda H, Pecoits-Filho R, Matsuo S, Yuzawa Y, Tranaeus A, Stenvinkel P, Lindholm B: Aspects of immune dysfunction in end-stage renal disease. Clin J Am Soc Nephrol 3: 1526–1533, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.