Abstract
Salmonella typhi is a true pathogen, which is capable of causing both intestinal and extraintestinal infections. Unusual presentations of Salmonella should always be kept in mind as this organism can cause disease in almost any organ of the body. S. typhi has been reported to cause the life-threatening infections such as meningitis, endocarditis, myocarditis, empyema, and hepatic abscess. Renal involvement by S. typhi is a relatively rare presentation. We report a case of renal abscess caused by S. typhi in an afebrile, 10-year-old child who did not have any clinical history of enteric fever. To our knowledge, this is the first reported case of isolation of S. typhi from the renal abscess, and interestingly this isolate was found to be resistant to quinolones.
Keywords: Fluoroquinolones, renal abscess, Salmonella typhi
INTRODUCTION
Typhoid fever caused by Salmonella typhi is endemic in many parts of India. Less commonly, extraintestinal infections can occur with S. typhi. These extraintestinal infections can involve liver, spleen, lung, bones, joints, endocardium, or central nervous system.[1,2,3,4,5,6,7,8,9] Genitourinary infections by S. typhi are relatively rare. A renal abscess is commonly caused by Staphylococci, Escherichia coli, Klebsiella, and Proteus. There are documented reports of renal abscess caused by Salmonella virchow, Salmonella enteritidis, Salmonella Typhimurium, and Salmonella paratyphi A.[10,11,12,13] We report a case of renal abscess caused by S. typhi. In a PubMed/PubMed Central search of reported cases, there is no case of isolation of S. typhi from renal abscess so far. Interestingly, the isolate was found to be resistant to ciprofloxacin (minimum inhibitory concentration [MIC] ≥1 µg/ml).
CASE REPORT
A 10-year-old male child, a known case of congenital atrophy of left kidney presented with complaints of mild pain in the right lumbar area of 3 days. He did not have any urinary symptoms, vomiting, jaundice, bladder, or bowel disturbance. The patient was afebrile and hemodynamically stable. General physical and systemic examinations were unremarkable except for flank tenderness on the right side. Laboratory investigations revealed hemoglobin: 11.1 g/dl and a total leukocyte count: 16.51 × 103/µl. Renal function tests were normal with blood urea: 33 mg/dl and serum creatinine: 0.7 mg/dl. Ultrasound kidney, ureter, bladder regions on the right side showed enlarged kidney (11.7 × 5.6) with hydronephrosis of the mid and lower poles with hydroureter. A cystic lesion was seen in mid pole with sedimenting hyperechoic contents. An ill-defined hypoechoic area was seen in the upper pole measuring 4.2 cm × 3.1 cm, causing capsular bulge with upper pole hypertrophy, with a possible diagnosis of lobar nephronia. On the left side, it showed a small kidney (5.3 cm × 2.3 cm) with dilated ureter in its entire length. Computed tomography urography revealed enlarged right kidney (11.2 cm × 6 cm) with the irregular contour. There was decreased nephrographic density in the anterior-mid and lower parenchyma probably due to focal nephronia. Calyceal cut off and hydronephrosis were noted in the anterior-mid and lower pole calyces on the right side with no excretion of contrast even on delayed scans. Two of the cut off calyces in the anterior mid pole and one in the lower pole showed a high density contents and mild wall thickening on delayed scans, which was likely due to exudative fluid or pus. On the left side, it showed atrophic kidney [Figure 1]. No organism was isolated from urine culture. Based on these investigations, the patient was planned for ultrasound guided aspiration of the right renal abscess under local anesthesia. He underwent the procedure well, and the aspirate was sent to the microbiology lab for culture and sensitivity. Postprocedure, he was started empirically on cefoperazone-sulbactam 1g intravenous (IV) 3 times a day. Aspirate culture grew nonlactose fermenting Gram-negative Bacilli, which was identified as S. typhi by VITEK 2 compact. Serotyping was done to confirm the isolate. This isolate was found to be sensitive to ceftriaxone (MIC ≤ 1 µg/ml), cefoperazone-sulbactam (MIC ≤ 8 µg/ml), trimethoprim/sulfamethoxazole (MIC ≤ 20 µg/ml) but resistant to ciprofloxacin (MIC ≥ 1 µg/ml). As the patient was afebrile and clinically there was no suspicion of enteric fever at presentation, his blood culture was not sent. However, we managed to do the Widal test on his serum sample, which was stored in the lab following renal function tests. Widal came out to be positive for S. typhi (O and H antigens in the titer of 1:320). Treatment was continued with IV cefoperazone-sulbactam till the 4th day of his hospitalization as the isolate was sensitive to third generation cephalosporins. Pain and flank tenderness subsided, and the patient was discharged with an advice to take cefixime 200 mg twice daily for 7 days. The patient was asymptomatic on subsequent follow-up visits.
Figure 1.
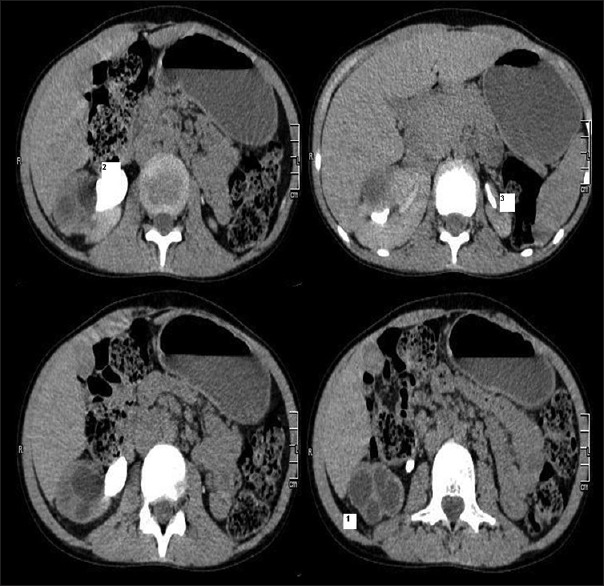
Computed tomography urography showing: (1) Enlarged right kidney with multiple round hypodense lesions (2) Right sided dilated ureter (3) Small left kidney
DISCUSSION
Typhoid is a major health problem, especially in developing countries with poor sanitation where fecal contamination of food and water is common. The most common infections caused by S. typhi in humans are gastrointestinal infections, but it is also capable of causing the extra-intestinal infections. It can involve almost any organ in the body producing different manifestations. Salmonella can affect the central nervous system, cardiovascular system, pulmonary system, bone, joints, hepatobiliary system, and genitourinary system. There are few reported cases from India on these extra-intestinal infections. In a study by Gokul et al., 27 cases of central nervous system infection by Salmonella were reported.[9] This organism can also cause myocarditis, endocarditis, and less commonly pericarditis.[8] It has also been reported to cause pleural empyema in an 83-year-old male diabetic patient who presented with fever, productive cough, and difficulty in swallowing.[4] S. typhi can cause osteomyelitis by hematogenous spread, contiguous source, or as a result of vascular insufficiency. An association between S. typhi osteomyelitis and sickle cell anemia has been seen.[6] S. typhi can involve a hepatobiliary system and cases of S. typhi liver abscess have been reported in the literature.[1,2]
Genitourinary infection by S. typhi is a relatively rare event, even in endemic areas. Predisposing factors for genitourinary involvement include underlying structural or functional abnormalities, calculi, pyelonephritis, dermoid cyst, and renal transplant. S. typhi has never been implicated in renal abscess, although renal involvement has been reported.[14] Diagnosis is confirmed by culture of the aspirated pus from the abscess.
Empiric treatment of renal abscess is started with anti-staphylococcal drugs as it is the most common causative agent. Once the culture and sensitivity reports are available, treatment is modified accordingly.[13] S. typhi, usually shows good sensitivity to fluoroquinolones, but quinolone resistance has emerged in developing countries due to the widespread availability of inexpensive fluoroquinolones. Our isolate was also resistant to ciprofloxacin. Third generation cephalosporins can be used in cases showing resistance to fluoroquinolones. Other antibiotics that have been reported to be used successfully are chloramphenicol, co-trimoxazole, and azithromycin. Chloramphenicol should be reserved for the infections caused by S. typhi when less toxic antimicrobials are ineffective or contraindicated. In case of perinephric abscess drainage procedure is also required in addition to antibiotics.[15,16] Salmonellosis continues to be a major public health problem in developing countries, therefore, unusual clinical presentations of Salmonella should be kept in mind.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jorge JF, Costa AB, Rodrigues JL, Girão ES, Luiz RS, Sousa AQ, et al. Salmonella typhi liver abscess overlying a metastatic melanoma. Am J Trop Med Hyg. 2014;90:716–8. doi: 10.4269/ajtmh.13-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soni PN, Hoosen AA, Pillay DG. Hepatic abscess caused by Salmonella typhi. A case report and review of the literature. Dig Dis Sci. 1994;39:1694–6. doi: 10.1007/BF02087778. [DOI] [PubMed] [Google Scholar]
- 3.Piplani S, Krishna R, Nandi B, Ganjoo RK, Madan R, Chander BN. Two cases of Salmonella splenic abscess. MJAFI. 2006;62:77–8. doi: 10.1016/S0377-1237(06)80167-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Afridi FI, Farooqi BJ, Hussain A. Pleural empyema due to Salmonella typhi. J Coll Physicians Surg Pak. 2012;22:803–5. [PubMed] [Google Scholar]
- 5.Aslam F, Bhaila I, Nadeem N, Fadoo Z. Salmonella typhi-infected lung hydatid cyst. Pediatr Infect Dis J. 2005;24:270–2. doi: 10.1097/01.inf.0000154331.67419.78. [DOI] [PubMed] [Google Scholar]
- 6.Declercq J, Verhaegen J, Verbist L, Lammens J, Stuyck J, Fabry G. Salmonella typhi osteomyelitis. Arch Orthop Trauma Surg. 1994;113:232–4. doi: 10.1007/BF00441839. [DOI] [PubMed] [Google Scholar]
- 7.Shanthi M, Sekar U, Sridharan KS. Septic arthritis of hip caused by Salmonella typhi: A case report. Case Rep Infect Dis. 2012;2012:464527. doi: 10.1155/2012/464527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh VP, Jain V, Sharma A, Agarwal AK. Salmonella typhi endocarditis. J Indian Acad Clin Med. 2010;11:49–50. [Google Scholar]
- 9.Gokul N, Chandramuki A, Ravikumar R, Khanna N. Salmonella infections of central nervous system. NIMHANS J. 1988;6:115–9. [Google Scholar]
- 10.Olson ES, Asmussen T, Vicca AF, Osborn DE. A case report of renal abscess caused by Salmonella virchow phage type 1 associated with a papillary renal cell carcinoma. J Infect. 1999;38:56–7. doi: 10.1016/s0163-4453(99)90035-x. [DOI] [PubMed] [Google Scholar]
- 11.Hashino S, Imamura M, Tanaka J, Noto S, Kobayashi S, Kasai M, et al. Renal Salmonella enteritidis abscess in a patient with severe aplastic anemia after allogeneic stem cell transplantation. Bone Marrow Transplant. 1996;18:807–8. [PubMed] [Google Scholar]
- 12.Dravid M, Joshi BN. Renal abscess due to Salmonella typhimurium. Indian J Pediatr. 1990;57:586–8. doi: 10.1007/BF02726778. [DOI] [PubMed] [Google Scholar]
- 13.D’Cruz S, Kochhar S, Chauhan S, Gupta V. Isolation of Salmonella paratyphi a from renal abscess. Indian J Pathol Microbiol. 2009;52:117–9. doi: 10.4103/0377-4929.44996. [DOI] [PubMed] [Google Scholar]
- 14.Duncan ME, Perine PL, Krause DW. Pelvic infection caused by Salmonella typhi. Two unusual cases. East Afr Med J. 1981;58:703–7. [PubMed] [Google Scholar]
- 15.Renuka K, Kapil A, Kabra SK, Wig N, Das BK, Prasad VV, et al. Reduced susceptibility to ciprofloxacin and gyra gene mutation in North Indian strains of Salmonella enterica serotype typhi and serotype paratyphi A. Microb Drug Resist. 2004;10:146–53. doi: 10.1089/1076629041310028. [DOI] [PubMed] [Google Scholar]
- 16.Chinh NT, Parry CM, Ly NT, Ha HD, Thong MX, Diep TS, et al. A randomized controlled comparison of azithromycin and ofloxacin for treatment of multidrug-resistant or nalidixic acid-resistant enteric fever. Antimicrob Agents Chemother. 2000;44:1855–9. doi: 10.1128/aac.44.7.1855-1859.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]


