Abstract
Respiratory viral infections, especially influenza have a potential to form a fatal association with cryptococcosis in the setting of compromised immunity. Considering the lethality of these two infections, we report an unusual case of dual infection of pandemic influenza A H1N1 and disseminated cryptococcosis in an HIV seropositive individual.
Keywords: Disseminated cryptococcosis, H1N1, pandemic influenza
INTRODUCTION
Invasive mycotic infections and respiratory viral infections are of a rising concern in HIV seropositive population.[1,2] Cryptococcus neoformans is the most common fungal infection in HIV patients, and a concurrent rise has also been seen in the number of HIV patients suffering from pandemic influenza A virus.[3] Apart from protean manifestations of upper respiratory tract symptoms and malaise, rare manifestation such as seizures, encephalopathy, Guillain-Barre syndrome, acute disseminated encephalomyelitis, transverse myelitis and aseptic meningitis are also encountered pandemic influenza.[4,5]
We describe an unusual case of concomitant pandemic influenza A and cryptococcal meningitis in an HIV-seropositive patient, who later succumbed to the dual infection.
CASE REPORT
A 34-year-old adult male presented to the emergency department with complaints of high-grade fever, breathlessness, and cough for 15 days. He was admitted to pandemic influenza intensive care unit. The patient was conscious, oriented to time, place and person, had tachypnea, tachycardia, pallor, and edema. The past history was significant for smoking and alcoholism. He had suffered from pulmonary tuberculosis (TB) 2 years back and had taken a full course of anti-tubercular therapy. Respiratory system examination revealed bilateral basal crepitations. Central nervous system examination showed a positive Babinski's sign. The hematological parameters, liver and kidney function tests were normal except low hemoglobin of 6%. Computed tomography of the chest revealing bilateral air space consolidation, ground-glass opacities, and bilateral parenchymal lesions suggestive of bilateral pneumonitis [Figure 1]. He was diagnosed with pandemic influenza A H1N1 by real-time polymerase chain reaction as per Centers for Disease Control and Prevention guidelines. A sputum pyogenic culture was positive for Escherichia coli, and it was sensitive to meropenem and ertapenem. Sputum for mycobacterial culture was negative. Patient's urine and blood cultures were sterile. A provisional diagnosis of pandemic influenza pneumonitis with adult respiratory distress syndrome was made, and patient's management initiated. The antibiotic therapy with ertapenem, oseltamivir and fluconazole was started. On the 7th day, patient's condition deteriorated. His arterial blood gas parameters were deranged and was put on a ventilator. Samples were sent for fungal and bacterial culture. India ink examination of cerebrospinal fluid (CSF) and pleural fluid demonstrated capsulated budding yeast cells [Figure 2]. Latex agglutination test was positive for the cryptococcal antigen. C. neoformans was isolated in fungal cultures of CSF, sputum, and pleural fluid. It was sensitive to amphotericin B, fluconazole, itraconazole, voriconazole and flucytosine. Injection amphotericin 1 mg/kg body weight was started. The patient was also declared positive for HIV by three different ELISA kits using three different antigens. CD 4 cell count was 39 cells/μL. His partner was also HIV positive, and she gave a history of contact in her spouse. On 14th day, no improvement was seen and patient developed respiratory acidosis. Despite the timely diagnosis, the patient died.
Figure 1.
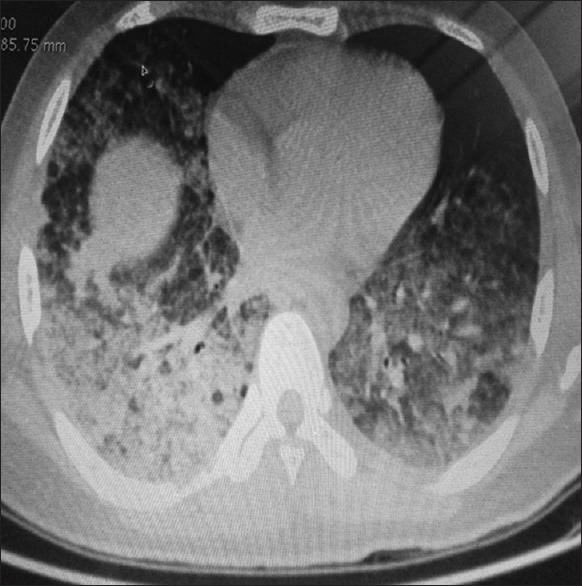
Computed tomography of chest revealing bilateral air space consolidation, ground glass opacities, bilateral parenchymal lesions suggestive of bilateral pneumonitis
Figure 2.
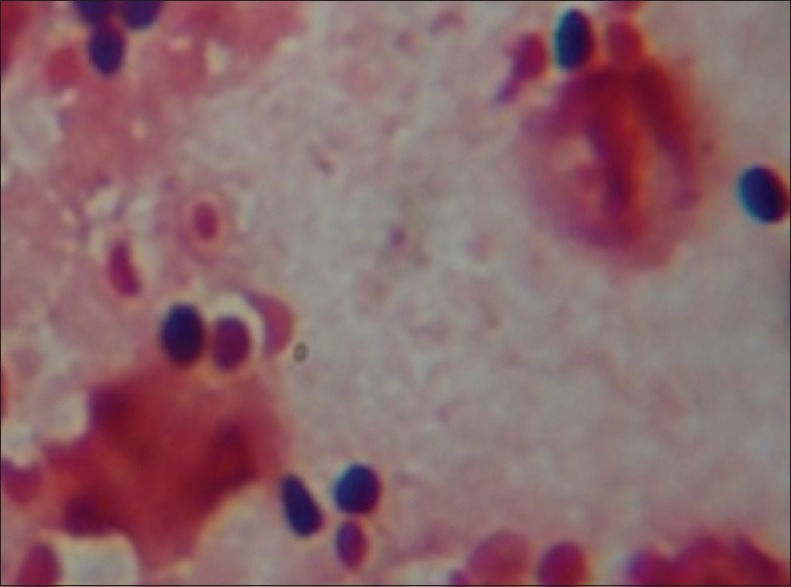
Gram's stain smear of pleural fluid sample showing broad base budding yeasts cells and exudate
DISCUSSION
HIV and other immunocompromised individuals suffer from a number of opportunistic bacterial, viral, fungal and parasitic diseases. The infections with C. neoformans spar a varied clinical spectrum in immunocompromised host, from meningitis, pneumonia, soft tissue and bone infections.[6,7] Pandemic influenza is also a major cause of morbidity and mortality in HIV-infected individuals, and also in patients undergoing treatment with highly active antiretroviral therapy. The meningeal signs and symptoms have also been attributed to pandemic influenza in a small number of cases.[4] In this case, the patient developed meningitis after being diagnosed by pandemic influenza. The compromised pulmonary functions with past history of TB in this case also provided an ideal breeding ground for a respiratory infection, e.g. influenza and cryptococcosis. HIV seropositive patients should be vaccinated for influenza annually to improve their prognosis.
In the medical literature, only one case of association between Cryptococcus and pandemic influenza virus has been reported. He was HIV seronegative, a normal CD4 count, responded to antiviral treatment with oseltamivir and survived.[8] The striking similarity between the first reported and our case was the onset of symptoms. Both the patients were immunocompromised, the first one due to prolonged influenza infection and use of corticosteroids, and our patient due to HIV infection and history of TB. Both cases developed cryptococcal meningitis after they were diagnosed with pandemic influenza A H1N1. This suggests that lungs of an immunocomprised patient can play a breeding for an opportunistic fungal or bacterial infection. Contrast to the previous case, our patient died, which could be due to oseltamivir resistance. This necessitates that the severely affected people should be screened for oseltamivir resistance.
As both C. neoformans and influenza virus can present with meningeal symptoms, it is essential to diagnose the primary pathogen so that a proper treatment in proper time can be instituted. Hence, this case highlights the fact that an AIDS patient is a microbiological zoo and all the parameters should be assessed and opportunistic infection specific treatment and anti-retroviral therapy instituted to prevent mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Englund J, Feuchtinger T, Ljungman P. Viral infections in immunocompromised patients. Biol Blood Marrow Transplant. 2011;17 1 Suppl:S2–5. doi: 10.1016/j.bbmt.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–30. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 3.Peters PJ, Skarbinski J, Louie JK, Jain S, Roland M, et al. New York City Department of Health Swine Flu Investigation Team. HIV-infected hospitalized patients with 2009 pandemic influenza A (pH1N1) – United States, spring and summer 2009. Clin Infect Dis. 2011;52 Suppl 1:S183–8. doi: 10.1093/cid/ciq036. [DOI] [PubMed] [Google Scholar]
- 4.Landau YE, Grisaru-Soen G, Reif S, Fattal-Valevski A. Pediatric neurologic complications associated with influenza A H1N1. Pediatr Neurol. 2011;44:47–51. doi: 10.1016/j.pediatrneurol.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Ozdemir H, Karbuz A, Ciftçi E, Ince E, Dogru U. Aseptic meningitis in a child due to 2009 pandemic influenza A (H1N1) infection. Turk J Pediatr. 2011;53:91–3. [PubMed] [Google Scholar]
- 6.Bratton EW, El Husseini N, Chastain CA, Lee MS, Poole C, Stürmer T, et al. Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIV-negative/non-transplant. PLoS One. 2012;7:e43582. doi: 10.1371/journal.pone.0043582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okumura A, Nakagawa S, Kawashima H, Morichi S, Muguruma T, Saito O, et al. Severe form of encephalopathy associated with 2009 pandemic influenza A (H1N1) in Japan. J Clin Virol. 2013;56:25–30. doi: 10.1016/j.jcv.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Hosseinnezhad A, Rapose A. Cryptococccal meningoencephalitis after H1N1 influenza. BMJ Case Rep 2012. 2012 doi: 10.1136/bcr.11.2011.5224. pii: Bcr1120115224. [DOI] [PMC free article] [PubMed] [Google Scholar]


