Abstract
Background:
Insulin resistance (IR) is the key pathophysiological defect that leads to the development of type 2 diabetes mellitus. The purpose of this study was to estimate serum magnesium level and insulin sensitivity indices among type 2 diabetes mellitus patients and to see an association between them.
Methods:
This study was carried out among 38 type 2 diabetic patients and forty age and sex matched controls. Serum fasting glucose, magnesium, insulin, urea, and creatinine levels were estimated. Insulin sensitivity indices, homeostasis model assessment for insulin resistance (HOMA-IR) and quantitative insulin sensitivity check index (QUICKI) levels were calculated as per formulae.
Results:
A highly significant low serum magnesium level was found in diabetic subjects as compared to the controls. Statistically significant high HOMA levels (>2.6) and low QUICKI levels (<0.33) were found among the case group. An inverse, statistically significant correlation was found between serum magnesium and fasting insulin level. A highly statistically significant inverse correlation was found between serum magnesium and HOMA level, and a positive correlation was found between serum magnesium and QUICKI level, that is, serum magnesium level decreases with increase in IR. A strong association was also found between fasting serum insulin level and insulin sensitivity indices.
Conclusion:
This study showed a lower serum magnesium level in diabetic patients compared to control. A strong association was also found between serum magnesium level and insulin sensitivity indices. For proper management of type 2 diabetes, it may, therefore, be necessary to treat hypomagnesemia in these patients.
Keywords: Diabetes mellitus, homeostasis model assessment for insulin resistance, insulin resistance, magnesium, quantitative insulin sensitivity check index
INTRODUCTION
Type 2 diabetes mellitus, previously referred to as noninsulin-dependent diabetes, or adult-onset diabetes, encompasses individuals who have insulin resistance (IR) and usually have relative (rather than absolute) insulin deficiency.[1] Number of people with diabetes in India is 40.9 million and is expected to rise to 69.9 million by 2025.[2] The two main pathophysiological defects, IR and beta-cell dysfunction which lead to hyperglycemia may precede the development of type 2 diabetes mellitus for many years.[3] Therefore most of the type 2 diabetes patients remain undiagnosed and are often diagnosed late. IR is a pathological situation characterized by a lack of physiological response of peripheral tissues to insulin action, leading to the metabolic and hemodynamic disturbances known as the metabolic syndrome.[3] The concept of IR in type-2 diabetes mellitus was first advanced by Himsworth of the university college hospital medical centre in London in 1936.[4]
Though euglycemic hyperinsulinemic glucose clamp is the gold standard to detect IR, it is difficult to perform it in daily clinical practice. Therefore, homeostasis model assessment for insulin resistance (HOMA-IR) and quantitative insulin sensitivity check index (QUICKI) are frequently used as indirect insulin sensitivity indices which correlates well with the gold standard method.[5,6,7]
Due to lack of standardization of insulin assay procedure, use of fasting insulin level for measurement of IR is limited. Moreover estimation of fasting insulin level does not cover the inappropriately low insulin secretion seen in diabetic subjects or in glucose-intolerant subjects.[8]
As research continues for better understanding of body's glucose management, IR, metabolic syndrome and diabetes, role of minerals like, magnesium in glucose metabolism has been revealed. Magnesium is the second most abundant intracellular cation in our body. Cellular magnesium helps in glucose metabolism by mediating insulin secretion, insulin receptor interaction, and signaling (involving tyrosine kinase mediated phosphorylation) and acting as a cofactor for various key enzymatic reactions in the metabolism of glucose.[9,10]
There are studies which suggest that magnesium deficiency is common in diabetic people, and it may be a preceding factor in IR and hyperinsulinemia.[11]
This study was therefore undertaken to estimate the serum level of magnesium and insulin sensitivity indices in type 2 diabetes mellitus patients and to evaluate the association between them.
METHODS
This study was carried out in North East Indira Gandhi Institute of Health and Medical Science, among 38 recently diagnosed type 2 diabetes mellitus patients above the age of 20 years and forty age and sex matched nondiabetic controls. Diabetes status was determined as per American Diabetes Association criteria. Patients suffering from chronic inflammatory diseases and infections, hypothyroidism, liver disease, kidney disease, heart failure, ascites, abdominal hernias, tumors and pregnant ladies were excluded from the study.
Blood samples for glucose, magnesium, insulin, urea, and creatinine estimation were collected after 10–12 h fast. A postprandial sample was also collected for glucose estimation. Blood chemistry analysis was done with the Beckman coulter autoanalyzer AU2700. Serum fasting insulin level was assayed by chemiluminiscence method (Access 2, Beckman Coulter).
Indices of IR, HOMA and QUICKI were calculated using following formulae:
HOMA = (fasting insulin [µIU/ml] × fasting glucose [mg/dl])/405
QUICKI = 1/log (fasting insulin [µIU/ml] + log fasting glucose [mg/dl])
Patients were considered as insulin resistant when, HOMA was ≥2.6 and QUICKI was ≤0.337.[5,6,7]
A database was constructed on Microsoft Excel (Office 2007, Microsoft Corporation, Redmond, Washington, USA), and statistical analysis was done using Statistical Package for Social Sciences (SPSS) Windows version 20 (IBM, Armonk, New York, USA).
RESULTS AND DISCUSSION
In this study comprising 38 patients, 23 (60.5%) were men and 15 (39.5%) were women.
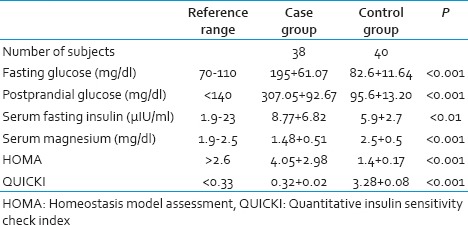
Mean ± standard deviation of serum fasting glucose, postprandial glucose, urea, creatinine, magnesium, fasting insulin, HOMA-IR and QUICKI levels for patients, were 195 + 61.07 mg/dl, 307.05 + 92.67 mg/dl, 26.61 + 9.33 mg/dl, 1.23+.53 mg/dl, 1.48 + 0.51 mg/dl, 8.77 + 6.10 µIU/ml, 4.05 + 2.98, and 0.32 + 0.02 respectively. For control subjects these parameters were within the reference range. Twenty-six (68.4%) patients (10 women, 16 men), out of 38 showed IR according to HOMA and QUICKI.
A highly significant lower serum magnesium level was found in diabetic subjects as compared to the control individuals (P < 0.001). Statistically significant higher HOMA levels (>2.6) and lower QUICKI levels (<0.33) were found among the case group as compared to the control group (P < 0.001) [Table 1].
Table 1.
Biochemical parameters of the study group
Though an association was found between serum fasting glucose and magnesium level but the correlation is not statistically significant (r = −0.29, P > 0.05). Similarly an association between serum fasting glucose and HOMA level (r = 0.252, P > 0.05) and between serum fasting glucose and QUCIKI level (r = −0.255, P > 0.05) were found which was not statistically significant.
An inverse, statistically significant correlation was found between serum magnesium and fasting insulin level (r = -0.396, P < 0.01). A highly statistically significant inverse correlation was found between serum magnesium and HOMA-IR level (r = −0.518, P < 0.001) [Figure 1] and a positive correlation was found between serum magnesium and QUICKI level (r = 0.55, P < 0.001) [Figure 2], that is, serum magnesium level decreases with increase in IR.
Figure 1.
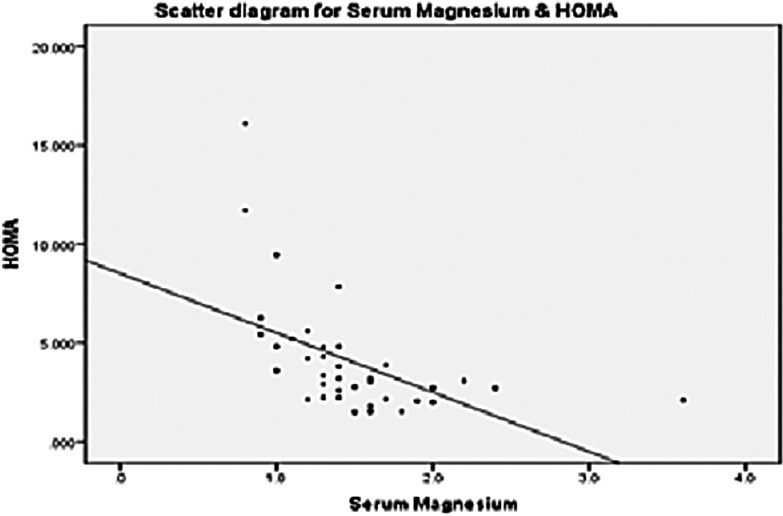
Scatter diagram for serum magnesium and homeostasis model assessment for insulin resistance in case group
Figure 2.
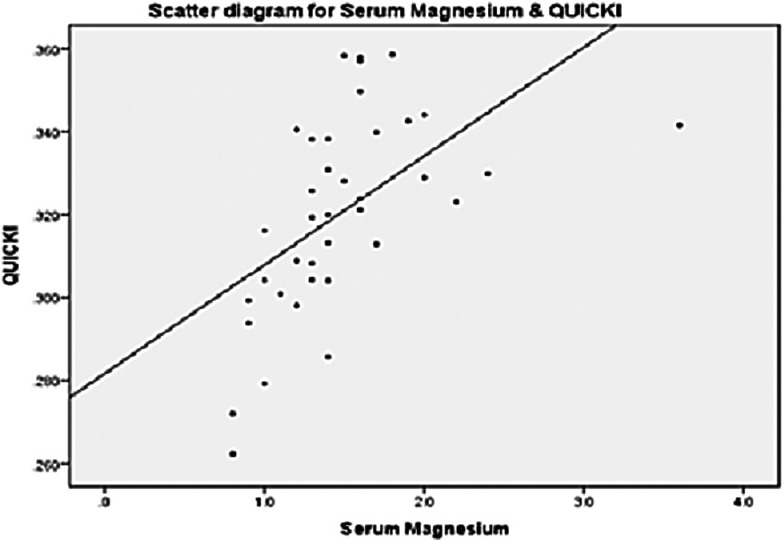
Scatter diagram for serum magnesium and quantitative insulin sensitivity check index level in case group
A strong positive correlation was found between serum fasting insulin level and HOMA level (r = 0.875, P < 0.001), and similarly a strong negative correlation was found between fasting insulin level and QUICKI level (r = −0.731, P < 0.001) which means that serum fasting insulin level increases with increase in IR.
In this study, serum magnesium level was significantly lower in diabetic patients. This finding is consistent with the studies done by Badyal et al. and Chambers et al.[11,12] A Dasgupta et al. also found poorer glycemic control in the hypomagnesemia patients as compared with the normomagnesemia patients.[13] Hereditary factors, poor dietary intake, autonomic dysfunction, altered insulin metabolism, glomerular hyperfiltration, osmotic diuresis, recurrent metabolic acidosis, hypophosphatemia and hypokalemia may all contribute to hypomagnesaemia in diabetic patients.[14] Magnesium deficiency in diabetes mellitus has also been linked to the development of the disease as well as its severity. In a study done by Hruby et al. among middle aged Americans, found that higher magnesium intake may lower the risk of progressing to diabetes among those with the highest risk of doing so, namely, those with IR or prediabetes.[15]
The lower magnesium level also correlates with the faster the deterioration of renal function in type 2 diabetics.[16] Therefore, magnesium supplementation may help in preventing the renal damage. However, care must also be taken in patients already with developed renal insufficiency as renal excretion is the major route of magnesium elimination from the body and this may cause a positive magnesium balance and hence may result in toxic concentrations of the ion in serum.[17]
An inverse correlation (P < 0.01) was found between serum magnesium and fasting insulin level. Also a highly statistically significant correlation (P < 0.001) was found between magnesium and insulin sensitivity indices, HOMA-IR and QUICKI. In a study done by Hata et al., they found that increased magnesium intake was a significant protective factor for the incidence of type 2 diabetes in the general Japanese population, especially among subjects with IR; low-grade inflammation and a drinking habit.[18]
In a study done by Lima Mde et al., a negative association was found between HOMA-IR and Intracellular magnesium level, though it was not statistically significant.[19] In a meta-analysis done in prospective cohort studies, by Dong et al., provides further evidence supporting that magnesium intake is significantly inversely associated with risk of type 2 diabetes in a dose-response manner.[20]
CONCLUSIONS
Magnesium is an important cofactor in glucose metabolism and also acts as a second messenger in insulin action. Low levels of magnesium can therefore impede reactions of many enzymes related to glucose metabolism as well as insulin receptor function through increased microviscosity of the plasma membrane and thus decreasing insulin sensitivity.[21] Hence, hypomagnesaemia found in type 2 diabetic patients in the current study may be a cause of increased IR in this group.
There are studies which confirm that diabetics and nondiabetics with IR who were supplemented with magnesium showed significant improvement in their IR.[22,23]
Though a number of prospective cohort studies and meta-analyses have suggested that magnesium intake reduces the risk of diabetes, but the results are still inconsistent. In addition, most cohort studies have been derived from Caucasian populations, and thus the effect of magnesium intake on diabetes risk in Asians remains to be fully elucidated. To the best of our knowledge, our study is first of its kind to be done in Indian patients to show the relation between the serum magnesium level and IR.
Limitation of this study includes small study group, lack of long term follow-up, no intervention with magnesium supplementation and study to see its outcome. Therefore a larger study group with active intervention with magnesium supplementation with long term follow up is necessary to corroborate the findings of this study.
Though hypomagnesaemia has been reported to occur with increased frequency among patients with type 2 diabetes mellitus, serum magnesium levels are not investigated in routine clinical practice. Therefore, for better management of type 2 diabetes and its complications it may be necessary to include serum magnesium estimation as a routine examination in these patients and adequate magnesium supplementation wherever required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.American Diabetes Association. Diabetes Care. 2014;37 Suppl 1:S81–90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 2.Diabetes Atlas. 3rd ed. Brussels: International Diabetes Federation; 2006. International Diabetes Federation. [Google Scholar]
- 3.Forst T, Standl E, Hohberg C, Konrad T, Schulze J, Strotmann HJ, et al. IRIS II study: The IRIS II score – Assessment of a new clinical algorithm for the classification of insulin resistance in patients with Type 2 diabetes. Diabet Med. 2004;21:1149–53. doi: 10.1111/j.1464-5491.2004.01298.x. [DOI] [PubMed] [Google Scholar]
- 4.Hanefeld M. The metabolic syndrome: Roots, myths, and facts. In: Hanefeld M, Leonhardt W, editors. The Metabolic Syndrome. Jena: Gustav Fischer; 1997. pp. 13–24. [Google Scholar]
- 5.Himsworth HP. Diabetes mellitus its differentiation into insulin sensitive and insulin insensitive types. Lancet 1936. Diabet Med. 2011;28:1440–4. doi: 10.1111/j.1464-5491.2011.3508.x. [DOI] [PubMed] [Google Scholar]
- 6.McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, et al. Diagnosing insulin resistance in the general population. Diabetes Care. 2001;24:460–4. doi: 10.2337/diacare.24.3.460. [DOI] [PubMed] [Google Scholar]
- 7.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70. doi: 10.2337/diacare.22.9.1462. [DOI] [PubMed] [Google Scholar]
- 8.Conwell LS, Trost SG, Brown WJ, Batch JA. Indexes of insulin resistance and secretion in obese children and adolescents: A validation study. Diabetes Care. 2004;27:314–9. doi: 10.2337/diacare.27.2.314. [DOI] [PubMed] [Google Scholar]
- 9.Singh B, Saxena A. Surrogate markers of insulin resistance: A review. World J Diabetes. 2010;1:36–47. doi: 10.4239/wjd.v1.i2.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendall DM. Targeting Insulin Resistance: Diabetes Prevention, Cardiovascular Disease Risk, and the Thiozolidinediones. In Medscape Coverage of American Diabetes Association. 64th Annual Scientific Sessions. 2004 [Google Scholar]
- 11.Badyal A, Sodhi KS, Pandey R, Singh J. Serum magnesium levels: A key issue for diabetes mellitus. Jk Science. 2011;13:3. Available from: www.jkscience.org . [Google Scholar]
- 12.Chambers EC, Heshka S, Gallagher D, Wang J, Pi-Sunyer FX, Pierson RN., Jr Serum magnesium and type-2 diabetes in African Americans and Hispanics: A New York cohort. J Am Coll Nutr. 2006;25:509–13. doi: 10.1080/07315724.2006.10719566. [DOI] [PubMed] [Google Scholar]
- 13.Dasgupta A, Sarma D, Saikia UK. Hypomagnesemia in type 2 diabetes mellitus. Indian J Endocrinol Metab. 2012;16:1000–3. doi: 10.4103/2230-8210.103020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pham PC, Pham PM, Pham SV, Miller JM, Pham PT. Hypomagnesemia in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2007;2:366–73. doi: 10.2215/CJN.02960906. [DOI] [PubMed] [Google Scholar]
- 15.Hruby A, Meigs JB, O’Donnell CJ, Jacques PF, McKeown NM. Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged Americans. Diabetes Care. 2014;37:419–27. doi: 10.2337/dc13-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pham PC, Pham PM, Pham PA, Pham SV, Pham HV, Miller JM, et al. Lower serum magnesium levels are associated with more rapid decline of renal function in patients with diabetes mellitus type 2. Clin Nephrol. 2005;63:429–36. doi: 10.5414/cnp63429. [DOI] [PubMed] [Google Scholar]
- 17.Mountokalakis TD. Magnesium metabolism in chronic renal failure. Magnes Res. 1990;3:121–7. [PubMed] [Google Scholar]
- 18.Hata A, Doi Y, Ninomiya T, Mukai N, Hirakawa Y, Hata J, et al. Magnesium intake decreases Type 2 diabetes risk through the improvement of insulin resistance and inflammation: The Hisayama Study. Diabet Med. 2013;30:1487–94. doi: 10.1111/dme.12250. [DOI] [PubMed] [Google Scholar]
- 19.Lima Mde L, Pousada J, Barbosa C, Cruz T. Magnesium deficiency and insulin resistance in patients with type 2 diabetes mellitus. Arq Bras Endocrinol Metabol. 2005;49:959–63. doi: 10.1590/s0004-27302005000600016. [DOI] [PubMed] [Google Scholar]
- 20.Dong JY, Xun P, He K, Qin LQ. Magnesium intake and risk of type 2 diabetes: Meta-analysis of prospective cohort studies. Diabetes Care. 2011;34:2116–22. doi: 10.2337/dc11-0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barbagallo M, Dominguez LJ, Galioto A, Ferlisi A, Cani C, Malfa L, et al. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol Aspects Med. 2003;24:39–52. doi: 10.1016/s0098-2997(02)00090-0. [DOI] [PubMed] [Google Scholar]
- 22.Guerrero-Romero F, Tamez-Perez HE, González-González G, Salinas-Martínez AM, Montes-Villarreal J, Treviño-Ortiz JH, et al. Oral magnesium supplementation improves insulin sensitivity in non-diabetic subjects with insulin resistance. A double-blind placebo-controlled randomized trial. Diabetes Metab. 2004;30:253–8. doi: 10.1016/s1262-3636(07)70116-7. [DOI] [PubMed] [Google Scholar]
- 23.Mooren FC, Krüger K, Völker K, Golf SW, Wadepuhl M, Kraus A. Oral magnesium supplementation reduces insulin resistance in non-diabetic subjects – A double-blind, placebo-controlled, randomized trial. Diabetes Obes Metab. 2011;13:281–4. doi: 10.1111/j.1463-1326.2010.01332.x. [DOI] [PubMed] [Google Scholar]


