Abstract
Objective
To evaluate the prevalence of deltoid ligament and distal tibiofibular syndesmosis injury on 3T magnetic resonance imaging (MRI) in patients with chronic lateral ankle instability (CLAI).
Materials and Methods
Fifty patients (mean age, 35 years) who had undergone preoperative 3T MRI and surgical treatment for CLAI were enrolled. The prevalence of deltoid ligament and syndesmosis injury were assessed. The complexity of lateral collateral ligament complex (LCLC) injury was correlated with prevalence of deltoid or syndesmosis injuries. The diagnostic accuracy of ankle ligament imaging at 3T MRI was analyzed using arthroscopy as a reference standard.
Results
On MRI, deltoid ligament injury was identified in 18 (36%) patients as follows: superficial ligament alone, 9 (50%); deep ligament alone 2 (11%); and both ligaments 7 (39%). Syndesmosis abnormality was found in 21 (42%) patients as follows: anterior inferior tibiofibular ligament (AITFL) alone, 19 (90%); and AITFL and interosseous ligament, 2 (10%). There was no correlation between LCLC injury complexity and the prevalence of an accompanying deltoid or syndesmosis injury on both MRI and arthroscopic findings. MRI sensitivity and specificity for detection of deltoid ligament injury were 84% and 93.5%, and those for detection of syndesmosis injury were 91% and 100%, respectively.
Conclusion
Deltoid ligament or syndesmosis injuries were common in patients undergoing surgery for CLAI, regardless of the LCLC injury complexity. 3T MRI is helpful for the detection of all types of ankle ligament injury. Therefore, careful interpretation of pre-operative MRI is essential.
Keywords: Chronic ankle instability, Lateral collateral ligament, Deltoid ligament, Syndesmosis, Magnetic resonance imaging, 3T
INTRODUCTION
Three-quarters of ankle injuries involve the lateral collateral ligament complex (LCLC) (1,2). Of these, 20-40% patients complain of chronic lateral ankle instability (CLAI) (2,3). CLAI is defined as the development of recurrent ankle sprains and persistent symptoms after an initial lateral ankle sprain. The diagnosis of ankle instability is usually established following a careful history, physical examination, and radiographic assessment (3,4). Surgical treatment in CLAI patients may be indicated in the context of persistent symptoms that do not respond to non-operative management (4). However, according to previous reports, between 13% and 35% of patients continue to experience ankle symptoms after surgical intervention, despite the success of the original procedure (5). These results may be due to the presence of undetected and therefore untreated injury to the combined other ligamentous complex. In most cases, surgical intervention in patients with CLAI is focused on the LCLC injury; however, forceful, repetitive ankle sprains can also cause injuries to other ankle ligaments. Accurate preoperative evaluation of injured ankle ligaments can be helpful for appropriate treatment and can derive better prognosis. In previous studies, the incidence of deltoid ligament injury in CLAI patients varies from 4.2% on a 1T magnetic resonance imaging (MRI) system (6) to 25.3-72% on a 1.5T MRI system (6,7). A combined syndesmosis injury was present in 45% of CLAI patients on a 0.2T MRI system (8). These reports, however, are limited by the use of low field MRI systems, and a lack of surgically corroborated data. In the present study, we used 3T MRI to evaluate the prevalence of deltoid ligament and distal tibiofibular syndesmosis injury in patients with CLAI.
MATERIALS AND METHODS
Patients
This study was approved by our Institutional Review Board, and was therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all patients. The study population comprised 56 patients who had undergone pre-operative MRI for a surgical reconstruction of CLAI at our institution between July 2011 and April 2014. All patients had experienced recurrent ankle sprains and chronic lateral ankle pain with grade 3 on anterior drawer test, and had not responded to conservative treatment. Five patients also complained of medial ankle pain. All patients who accepted both the modified Broström procedure and ankle arthroscopy were included in the study. We excluded 6 patients who had a previous history of surgery to the affected ankle, a recent ankle fracture, a comorbid infection, or an underlying systemic pathology, such as inflammatory arthritis. A total of 50 eligible patients (33 males, 17 females) aged between 15 and 58 years (mean age, 35 years) were enrolled. CLAI involved the left ankle in 29 patients, and the right ankle in 21 patients. Clinical and surgical data were reviewed.
MRI Techniques
MRI studies were performed using a 3T imaging system (Skyra; Siemens Healthcare, Erlangen, Germany). The patients were examined in the supine position with a neutral ankle position, using phased-array foot-and-ankle coil (16 channels). A sagittal T2-weighted fat suppression image was obtained using the Dixon technique with a repetition time of 4100 ms, an echo time of 73 ms, a turbo factor of 19, and a slice thickness of 3 mm with no interslice gap. Sagittal, axial, coronal oblique, and coronal fat-suppression proton-weighted turbo spin-echo (TSE) images were obtained with a repetition time of 3160-3500 ms, an effective echo time of 22-33 ms, a turbo factor of 6 or 7, a slice thickness of 3 mm with no interslice gap, and a field of view of 11-16 cm. A 512 × 410 matrix was obtained with a number of excitations of 1 or 2. A coronal oblique image was scanned perpendicular to the long axis of the navicular bone. An axial fat suppression T2-weighted TSE image was also obtained with a repetition time of 3130 ms, an effective echo time of 78 ms, a turbo factor of 11, and a matrix of 384 × 230. Axial oblique (syndesmotic view) proton-weighted TSE images were also obtained in 45 patients.
MRI Analysis
All MR images were retrospectively reviewed, first independently and then in consensus, by 2 radiologists who had 11 years and 3 years of experience in musculoskeletal imaging. The radiologists were unaware of the patient's clinical symptoms or the surgical records during their evaluation. The LCLC was classified into anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL); the deltoid ligament was divided into superficial and deep ligaments; the distal tibiofibular syndesmosis was divided into the anterior inferior tibiofibular ligament (AITFL), distal interosseous ligament (IOL), posterior inferior tibiofibular ligament, and transverse ligament. Radiologists evaluated which subdivided ligament of LCLC, deltoid ligament, and distal tibiofibular syndesmosis were injured. Even if one of the subdivided ligaments presented as injured, we assessed deltoid ligament or syndesmosis as injured when analyzing the prevalence. For the purpose of this study, chronic injury to these ligaments was defined as thickening, thinning, irregularities, discontinuity, nonvisualization, signal alteration, loosening or elongation of the ligaments on MRI (9,10). Additionally, the relationship between the LCLC injury complexity (ATFL alone, both ATFL and CFL, all ligaments) (Table 1) and the prevalence of accompanying deltoid or syndesmosis ligament injury was also evaluated. The sensitivity and specificity of MRI evaluation of ankle ligament injury was assessed using arthroscopic findings as a reference standard according to the established procedure for the diagnosis and treatment of disorders of the ankle joint (11,12).
Table 1. Complexity of Lateral Collateral Ligament Complex Injury in Chronic Lateral Ankle Instability.
| Injured Ligament | Total Number on MRI | Total Number on Arthroscopy |
|---|---|---|
| Only ATFL | 21 | 23 |
| ATFL and CFL | 23 | 22 |
| ATFL, CFL, and PTFL | 5 | 5 |
| Unremarkable | 1 | 0 |
| Total | 50 | 50 |
ATFL = anterior talofibular ligament, CFL = calcaneofibular ligament, PTFL = posterior talofibular ligament
Surgery
The mean interval between the MRI examination and surgery was 21 days (range: 0-89 days). Two orthopedic surgeons, who were specialized in foot and ankle surgery, performed all surgical procedures using arthroscopic evaluation of the LCLC, deltoid ligament, and distal tibiofibular syndesmosis. Arthroscopic evaluation of the ankle allowed inspection of the ATFL and PTFL, the capsular reflection of the CFL, the deltoid ligament, the syndesmotic ligament complex (7,13). CFL and superficial deltoid ligament injury could be evaluated when severe laxity or defect was present in the joint capsule or deep deltoid ligament. In the present study, chronic medial ligament abnormality was defined as enough to introduce a 2.9-mm arthroscope probe into medial mortise due to tibionavicular laxity without using a traction device, based on Hintermann's classification (14,15). Chronic syndesmotic abnormality was considered present when the distal tibiofibular diastasis was ≥ 4 mm, permitting arthroscopic insertion and swinging of an obturator (2.9 mm) between the tibiofibular diastasis (16). The IOL was generally difficult to evaluate at arthroscopy because it is attached approximately ≥ 1 cm above the joint line (17). But, IOL could be seen in the lateral portal and with probe in the medial portal, the degree of instability between the fibula and the tibia could be demonstrated (18). The modified Broström procedure for ATFL injury was performed in all patients after arthroscopy. Additionally, 2 patients underwent a CFL repair, 3 patients underwent a superficial deltoid ligament repair, 2 patients underwent an AITFL reconstruction with anchors, and 1 patient had a tibiofibular syndesmotic screw fixation. Two orthopedic surgeons retrospectively reviewed operation records. Two radiologists analyzed the prevalence and complexity of LCLC, deltoid ligament, and syndesmotic ligament. The relationship between the LCLC injury complexity and the prevalence of accompanying deltoid or syndesmosis ligament injury was also evaluated.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics version 20.0 (IBM Corp, Armonk, NY, USA). Linear-by-linear association was conducted for evaluation of the relationship between LCLC injury complexity and the prevalence of deltoid ligament or syndesmosis injury on both MRI and arthroscopic findings. The diagnostic accuracy (sensitivity and specificity) of ankle ligament imaging at 3T MRI was analyzed using arthroscopy as a reference standard.
RESULTS
Pre-operative MRI showed 49 patients of ATFL injury, 28 patients of CFL injury and 5 patients of PTFL injury. Injury confined to the ATFL alone in 21 (42%) patients, injury to both ATFL and CFL in 23 (46%) patients, and injury to all 3 ligamentous structures (the ATFL, CFL, and PTFL) in 5 (10%) patients. In 1 patient, the LCLC had a normal MRI appearance (Table 1). All CFL injuries were accompanied by ATFL injuries. PTFL injuries were observed only in the presence of concomitant ATFL and CFL injuries. The complexity of deltoid ligament and syndesmosis injuries on MRI was documented in Table 2. MRI showed deltoid ligament injury in 18 patients (36%) (superficial ligament alone, 9; deep ligament alone, 2; both ligaments, 7) (Fig. 1). Superficial deltoid ligament injury was more common than deep ligament injury. Syndesmosis injury were found in 21 patients (42%) (Fig. 2) and the majority of the syndesmosis injuries were confined to the AITFL. Nine patients showed abnormalities consistent with injury to both the deltoid ligament and the syndesmosis (Fig. 3). Based on both MRI and arthroscopic findings, there was no clear relationship between the LCLC injury complexity and the prevalence of accompanying deltoid or syndesmosis injuries (MRI, p = 0.29-0.83; arthroscopy, p = 0.16-0.71) (Table 3). MRI sensitivities for detection of deltoid ligament and syndesmosis injury were 84% and 91%, respectively, and specificities were 93.5% and 100%, respectively (Table 2).
Table 2. Complexity of Deltoid Ligament and Syndesmosis Injuries in Chronic Lateral Ankle Instability: MRI vs. Arthroscopy.
| Injured Ligament | MRI (Number of Ankles) | Arthroscopy (Number of Ankles) | Sensitivity of MRI (%) | Specificity of MRI (%) | |
|---|---|---|---|---|---|
| Deltoid ligament | Superficial | 9 | 11 | 84 (16 of 19 ankles) | 93.5 (29 of 31 ankles) |
| Deep | 2 | 2 | |||
| Superficial and deep | 7 | 6 | |||
| Syndesmosis | AITFL | 19 | 21 | 91 (21 of 23 ankles) | 100 (27 of 27 ankles) |
| AITFL and IOL | 2 | 2 | |||
AITFL = anterior inferior tibiofibular ligament, IOL = distal interosseous ligament
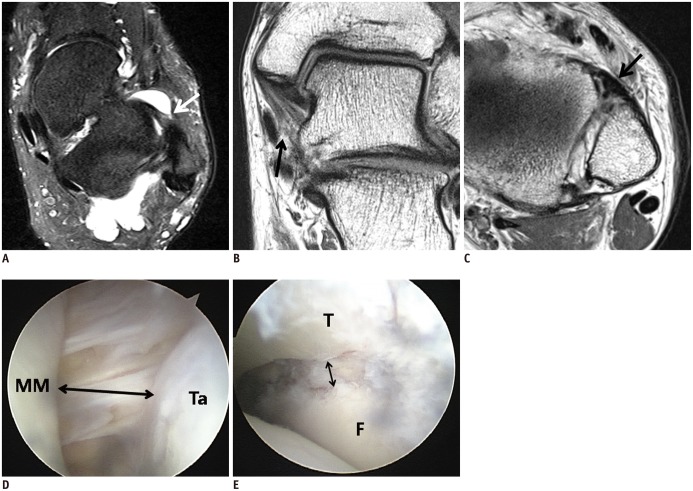
Fig. 1. 21-year-old man with chronic tear of anterior talofibular ligament (ATFL) and deltoid ligament.
A. Axial proton-weighted turbo spin echo (TSE) magnetic resonance (MR) image showing torn ATFL (arrows). B. Oblique coronal proton-weighted TSE MR image showing loose, thin superficial deltoid ligament (arrow). Deep posterior tibiotalar ligament is thickened with loss of striation. C. On arthroscopy, injury of superficial (not visible on this figure) and deep deltoid ligament (arrow) with widening of medial mortise (double arrow) were seen. Patient underwent modified Broström operation and repair of superficial deltoid ligament. MM = medial malleolus, Ta = medial talus
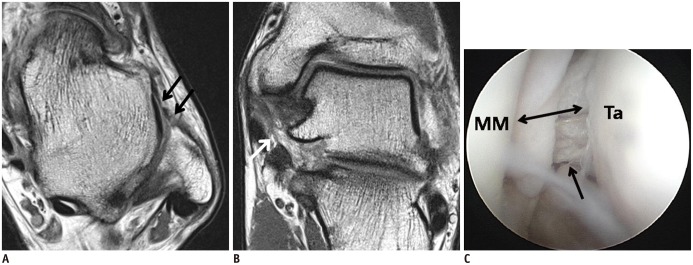
Fig. 2. 27-year-old man with chronic injuries of anterior talofibular ligament (ATFL) and anterior inferior tibiofibular ligament (AITFL).
A. Axial fat suppression T2-weighted turbo spin echo (TSE) magnetic resonance (MR) image shows very loose and irregular ATFL (arrows). B. Axial oblique proton-weighted TSE MR image shows irregular and loose AITFL (arrow). C. On arthroscopic image, there are obturator insertion and widening of distal tibiofibular joint (> 4 mm). Patient underwent modified Broström operation and reconstruction of AITFL using anchors. F = distal fibula, T = distal tibia
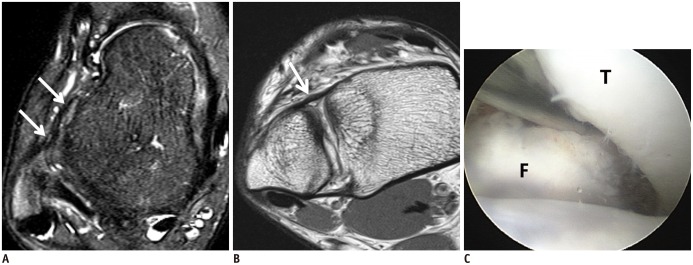
Fig. 3. 48-year-old man with chronic injuries to anterior talofibular ligament (ATFL), superficial deltoid ligament, and anterior inferior tibiofibular ligament (AITFL).
A. Axial T2-weighted fat-suppression turbo spin echo (TSE) magnetic resonance (MR) image shows hyperintensity of ATFL, with partial discontinuity (arrow). B. Coronal oblique proton-weighted TSE MR image shows hyperintensity of superficial deltoid ligament, with partial discontinuity (arrow). C. Axial proton-weighted TSE MR image shows thickened AITFL (arrow). D, E. Arthroscopic images show loose and partially torn superficial deltoid ligament, with widening of medial mortise (double arrow, D), and widening of distal tibiofibular joint (double arrow, E). Patient underwent modified Broström operation, repair of superficial deltoid ligament, and reconstruction of AITFL using anchors. F = distal fibula, MM = medial malleolus, T = distal tibia, Ta = medial talus
Table 3. Relationship between Complexity of Lateral Collateral Ligament Injury and Prevalence of Deltoid Ligament or Syndesmosis Injury in Chronic Lateral Ankle Instability on MRI and Arthroscopy.
| LCLC Injury | Unremarkable | ATFL | ATFL and CFL | ATFL, CFL, and PTFL | P | |
|---|---|---|---|---|---|---|
| MRI | Deltoid injury | 1 (100%) | 7 (33.3%) | 7 (30.4%) | 3 (60%) | 0.838 |
| Syndesmosis injury | 1 (100%) | 6 (28.6%) | 11 (47.8%) | 3 (60%) | 0.290 | |
| Arthroscopy | Deltoid injury | 0 | 8 (34.8%) | 9 (40.9%) | 2 (40%) | 0.712 |
| Syndesmosis injury | 0 | 8 (34.8%) | 12 (54.5%) | 3 (60%) | 0.160 |
Linear-by-linear association was conducted (statistically significant: p value ≤ 0.05). ATFL = anterior talofibular ligament, CFL = calcaneofibular ligament, LCLC = lateral collateral ligament complex, PTFL = posterior talofibular ligament
DISCUSSION
Chronic lateral ankle instability occurs in a significant minority of patients following single or repeated episodes of ankle sprain (7,19,20,21). CLAI can lead to early degenerative changes in the ankle due to unbalanced loading on the medial side. Therefore, appropriate treatment is important (1,22). Contemporary treatments for CLAI focus on the lateral ankle ligament complex, especially the ATFL and associated intra- or extra-articular lesions. The ATFL is the most frequently injured of the lateral ligaments, due to its lower maximal load and energy to failure value under tensile stress (23,24); it is also located parallel to the direction of ankle inversion.
The results of our study were consistent with those of previous reports (23,24). In the present study, all patients had at least 1 lateral collateral ligament injury, and the ATFL was the most frequently injured LCLC ligament, on both MRI and arthroscopy. Both MRI and arthroscopy indicated that approximately half of the patients sustained injuries to the ATFL and the CFL, the classic pattern associated with inversion instability (7).
Several studies have investigated the combined deltoid ligament injury in CLAI patients. In Lee et al.'s (25) report, 58 of 229 patients (25.3%) who had ankle instability showed deltoid ligament abnormalities on MRI. Hintermann et al. (14) found significant injuries to the deltoid ligament in 59 of 127 patients (40%) who had a clinical and arthroscopic diagnosis of lateral ankle instability. Our results indicated that 36% and 38% of patients with CLAI had deltoid ligament abnormalities on MRI and arthroscopy, respectively, consistent with the earlier reports. In our series, 9 patients (18%) had superficial deltoid abnormalities alone on MRI similar to Crim et al. (7), who reported that 23% of patients had a lone superficial deltoid injury. Injury to both superficial and deep components was observed in 7 patients (14%) in our study, substantially fewer than the 43% reported by Crim et al. Injury to the anterior superficial deltoid ligament suggests that a rotatory instability is present, at least in some patients with CAI. Rotational instability may be difficult to assess clinically, and MRI is useful for detection of anterior superficial deltoid ligament injury and raising suspicion of this pattern of instability. In the present study, only 5 of 18 patients who had a deltoid abnormality on MRI had medial ankle complaints and had no recorded physical examination results about rotatory instability. Further studies are needed to determine if rotational instability is related clinically to the MRI and surgical finding of superficial deltoid ligament injury.
A few previous studies have mentioned syndesmosis injury in CLAI patients. Syndesmosis forms the roof for the mortise of the talocrural joint, and is therefore often injured in eversion ankle injuries, resulting in the so-called "high ankle sprain" (23,26). McCollum et al. (27) have suggested that inversion tends to injury of only the AITFL component of the distal tibiofibular syndesmosis, together with injury to the ATFL; however, this study was confined to athletes. Our study in a more typical clinical population also showed that the majority of combined syndesmosis injuries in patients with CLAI affected the AITFL alone, together with chronic injury to the ATFL. Hua et al. (28), in a study of CLAI patients with ankle arthroscopy combined with a modified Broström procedure, found that 6 of 87 ankles (6.9%) had distal tibiofibular syndesmosis injuries, which was much lower than the 46% incidence on arthroscopy in the present study. A previous report has indicated that injury to the distal tibiofibular syndesmosis accounts for between 1% and 11% of all ankle injuries (29). The apparent increase in the incidence of syndesmosis injuries according to more recent reports could be attributed to an increase in knowledge, understanding, and awareness of syndesmosis injuries (30). Syndesmosis injuries have a long recovery time, and are frequently associated with CLAI, or residual symptoms (29,30). Teramoto et al. (30) reported the occurrence of multidirectional ankle instability, including inversion instability and external rotation, as a result of syndesmosis injuries.
To our knowledge, no previous studies have reported the association between deltoid ligament and syndesmosis injuries, and the complexity of LCLC injury, defined as the number of involved ligaments. In the present study, we found that there was no clear relationship between the complexity of LCLC injury and the prevalence of accompanying deltoid or syndesmosis injuries. Therefore, even those patients who have a single ATFL injury might have concomitant injuries to the deltoid ligament or syndesmosis.
In the present study, we also evaluated the diagnostic value of the 3T MRI for LCLC, deltoid ligament and syndesmosis injuries in CLAI patients. 3T MRI of the ankle was highly sensitive and specific for the detection of ligament injury, as compared with arthroscopy. These results were far superior to previous results obtained using 1.5T MRI, and MR arthrography. Chandnani et al. (31) reported a sensitivity of 50% and a specificity of 100% for the evaluation of the ATFL, and a sensitivity of 50% and a specificity of 83% for the evaluation of the CFL, when using MR arthrography. Cha et al. (32), in a study of CLAI patients, found the sensitivity of 1.5T MRI to be 60% for ATFL injuries, and 21% for distal tibiofibular ligament injuries. MRI allows improved visualization of the syndesmosis, in the form of syndesmotic images, which might account for the higher rate of detection of chronic distal tibiofibular syndesmosis injury on MRI, as compared with arthroscopy. In the present study, syndesmotic MR images were not observed in the 2 patients with normal AITFL on MRI but abnormal appearance on arthroscopy.
The present study was limited by several factors. The study included only a small number of patients, all of whom received surgical treatment for CLAI. Given that surgically treated patients with CLAI tend to have severe and complex injuries, the choice of study population may introduce selection bias. Inter- and intra-observer reliability was not assessed. According to the biomechanism of patients' ankle injuries, the incidence of combined deltoid ligament or syndesmosis injury in CLAI patients has been varied in some studies; future studies would benefit from the inclusion of a larger number of CLAI patients.
In conclusion, injury to the deltoid ligament or syndesmosis in patients undergoing surgical treatment of an LCLC injury was frequently observed. The presence of these additional injuries was not associated with the LCLC injury complexity. 3T MRI was helpful for the detection of all types of ankle ligament injury. Thus, careful interpretation of pre-operative MRI must be emphasized, because the treatment plan for CLAI can only be made based on a precise description of all associated lesions.
References
- 1.Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69:17–26. [PubMed] [Google Scholar]
- 2.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 3.Cass JR, Morrey BF. Ankle instability: current concepts, diagnosis, and treatment. Mayo Clin Proc. 1984;59:165–170. doi: 10.1016/s0025-6196(12)60769-1. [DOI] [PubMed] [Google Scholar]
- 4.Alparslan L, Chiodo CP. Lateral ankle instability: MR imaging of associated injuries and surgical treatment procedures. Semin Musculoskelet Radiol. 2008;12:346–358. doi: 10.1055/s-0028-1100641. [DOI] [PubMed] [Google Scholar]
- 5.Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007;28:24–31. doi: 10.3113/FAI.2007.0005. [DOI] [PubMed] [Google Scholar]
- 6.Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010;16:78–80. doi: 10.1016/j.fas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Crim JR, Beals TC, Nickisch F, Schannen A, Saltzman CL. Deltoid ligament abnormalities in chronic lateral ankle instability. Foot Ankle Int. 2011;32:873–878. doi: 10.3113/FAI.2011.0873. [DOI] [PubMed] [Google Scholar]
- 8.Milz P, Milz S, Steinborn M, Mittlmeier T, Putz R, Reiser M. Lateral ankle ligaments and tibiofibular syndesmosis. 13-MHz high-frequency sonography and MRI compared in 20 patients. Acta Orthop Scand. 1998;69:51–55. doi: 10.3109/17453679809002357. [DOI] [PubMed] [Google Scholar]
- 9.Schneck CD, Mesgarzadeh M, Bonakdarpour A. MR imaging of the most commonly injured ankle ligaments. Part II. Ligament injuries. Radiology. 1992;184:507–512. doi: 10.1148/radiology.184.2.1620856. [DOI] [PubMed] [Google Scholar]
- 10.Kanamoto T, Shiozaki Y, Tanaka Y, Yonetani Y, Horibe S. The use of MRI in pre-operative evaluation of anterior talofibular ligament in chronic ankle instability. Bone Joint Res. 2014;3:241–245. doi: 10.1302/2046-3758.38.2000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010;39:41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 12.Parisien JS, Shereff MJ. The role of arthroscopy in the diagnosis and treatment of disorders of the ankle. Foot Ankle. 1981;2:144–149. doi: 10.1177/107110078100200304. [DOI] [PubMed] [Google Scholar]
- 13.James PT, Peter DL. Recent advances in ankle arthroscopic techniques. In: Parisien JS, editor. Current Techniques in Arthroscopy. 3rd ed. New York: Thieme; 1998. pp. 182–194. [Google Scholar]
- 14.Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30:402–409. doi: 10.1177/03635465020300031601. [DOI] [PubMed] [Google Scholar]
- 15.Hintermann B, Valderrabano V, Boss A, Trouillier HH, Dick W. Medial ankle instability: an exploratory, prospective study of fifty-two cases. Am J Sports Med. 2004;32:183–190. doi: 10.1177/0095399703258789. [DOI] [PubMed] [Google Scholar]
- 16.Han SH, Lee JW, Kim S, Suh JS, Choi YR. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28:336–342. doi: 10.3113/FAI.2007.0336. [DOI] [PubMed] [Google Scholar]
- 17.Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324–329. doi: 10.1302/0301-620x.85b3.13174. [DOI] [PubMed] [Google Scholar]
- 18.Ogilvie-Harris DJ, Reed SC. Disruption of the ankle syndesmosis: diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10:561–568. doi: 10.1016/s0749-8063(05)80015-5. [DOI] [PubMed] [Google Scholar]
- 19.Ferran NA, Oliva F, Maffulli N. Ankle instability. Sports Med Arthrosc. 2009;17:139–145. doi: 10.1097/JSA.0b013e3181a3d790. [DOI] [PubMed] [Google Scholar]
- 20.Karlsson J, Lansinger O. Lateral instability of the ankle joint. Clin Orthop Relat Res. 1992;276:253–261. [PubMed] [Google Scholar]
- 21.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324–331.e6. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61:354–361. [PubMed] [Google Scholar]
- 23.Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train. 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- 24.Attarian DE, McCrackin HJ, DeVito DP, McElhaney JH, Garrett WE., Jr Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985;6:54–58. doi: 10.1177/107110078500600202. [DOI] [PubMed] [Google Scholar]
- 25.Lee KM, Chung CY, Kwon SS, Chung MK, Won SH, Lee SY, et al. Relationship between stress ankle radiographs and injured ligaments on MRI. Skeletal Radiol. 2013;42:1537–1542. doi: 10.1007/s00256-013-1704-6. [DOI] [PubMed] [Google Scholar]
- 26.Miller CD, Shelton WR, Barrett GR, Savoie FH, Dukes AD. Deltoid and syndesmosis ligament injury of the ankle without fracture. Am J Sports Med. 1995;23:746–750. doi: 10.1177/036354659502300618. [DOI] [PubMed] [Google Scholar]
- 27.McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1328–1337. doi: 10.1007/s00167-012-2205-1. [DOI] [PubMed] [Google Scholar]
- 28.Hua Y, Chen S, Li Y, Chen J, Li H. Combination of modified Broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy. 2010;26:524–528. doi: 10.1016/j.arthro.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325–330. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 30.Teramoto A, Kura H, Uchiyama E, Suzuki D, Yamashita T. Three-dimensional analysis of ankle instability after tibiofibular syndesmosis injuries: a biomechanical experimental study. Am J Sports Med. 2008;36:348–352. doi: 10.1177/0363546507308235. [DOI] [PubMed] [Google Scholar]
- 31.Chandnani VP, Harper MT, Ficke JR, Gagliardi JA, Rolling L, Christensen KP, et al. Chronic ankle instability: evaluation with MR arthrography, MR imaging, and stress radiography. Radiology. 1994;192:189–194. doi: 10.1148/radiology.192.1.8208935. [DOI] [PubMed] [Google Scholar]
- 32.Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, et al. Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg. 2012;4:293–299. doi: 10.4055/cios.2012.4.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]