Abstract
BACKGROUND
Little is known regarding youth perceptions of tap water and school water fountains and how these relate to water and sugar-sweetened beverage (SSB) intake.
METHODS
We used national 2010 YouthStyles data to assess perceptions of tap water and school water fountains and associations with water and SSB intake.
RESULTS
Nearly 1 in 5 participants disagreed their tap water was safe and nearly 2 in 5 disagreed school water fountains were clean and safe. Perceived tap water risk was more prevalent among non-Hispanic (NH) blacks (26.4%) and Hispanics (28.3%) compared to NH whites (14.7%, p < .001) and more prevalent among lower income youth. Negative water fountain perceptions were more common among high school age youth. Perceived tap water risk was not associated with SSB intake (odds ratio (OR) = 1.0, 95% CI: 0.6, 1.5) or water intake (OR = 1.4, 95% CI: 0.9, 2.1). Negative water fountain perceptions were associated with SSB intake only among Hispanics (race/ethnicity interaction p < .001; OR = 2.9, 95% CI: 1.3, 6.6) but were not associated with water intake.
CONCLUSION
Negative perceptions of tap water and water fountains among youth are common and should be considered in efforts to provide water in schools.
Sugar-sweetened beverages (SSB), defined by the 2010 Dietary Guidelines for Americans as liquids that are sweetened with various forms of sugars that add calories,1 are a leading source of calories in the diets of children in the United States.2 Among adults and children, high consumption of SSB has been associated with weight gain,3 diabetes,4 elevated triglycerides,5 cardiovascular disease,6 and dental caries.7 During 2005–2008, the average energy intake from SSB was 273 kcal/day for boys and 171 kcal/day for girls aged 12–19 years.8 In 2010, 62.8% of high school students reported drinking regular soda, sports drinks, or fruit flavored drinks daily, and 32.9% reported drinking these beverages two or more times per day.9 Furthermore, non-Hispanic (NH) black and Hispanic students were less likely than white students to drink milk and water daily but more likely to report daily consumption of sports drinks.9 Research suggests that daily energy consumption can be substantially reduced if children replace SSB with plain water10 and greater plain water intake has been associated with lower SSB intake among youth.11, 12 Indeed, an intervention encouraging consumption of plain water in schools has shown promising results in prevention of weight gain among German elementary school students.13 In an effort to increase access to plain water, the Healthy, Hunger-Free Kids Act of 2010 requires schools that participate in the National School Lunch Program to provide plain drinking water to students at no charge during meal times in the locations where lunch meals are served beginning at the start of the 2011/2012 school year.14
One potential barrier to encouraging youth to drink water at school may be the perception that tap water is not safe. Qualitative research in a California school district suggests that concerns about tap-water safety and contextual elements such as the cleanliness and overall condition of water fountains might be issues affecting water intake in schools.15 Evidence among adults suggests that negative perceptions of tap water safety are common, particularly among minority and lower socioeconomic status populations,16–20 and may be associated with lower intake of water and greater intake of SSB among some racial ethnic groups.20 Research suggests that those who agree that their tap water is safe are more likely to be NH white race, older, have higher income and more education.20 Among youth however, perceptions regarding tap water and school water fountain safety and their potential association with SSB or plain water intake have not been examined. Examination of children’s perceptions, both of tap water in general and of water fountains, would help to inform school-based and public health efforts to reduce intake of SSB through promotion of drinking water. Therefore, the aim of our study will be to examine cognitive evaluations of tap water safety and school water fountains among youth and how these evaluations relate to consumption of plain water and SSB. We will also assess whether the relationship between tap water and water fountain perceptions with SSB and water intake differs according to race/ethnicity.
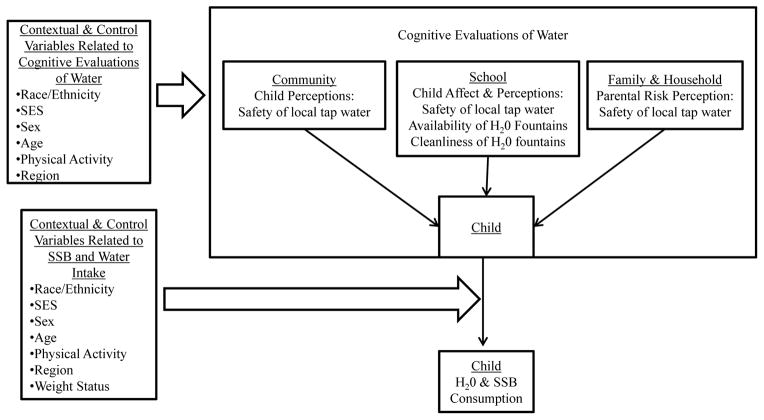
Conceptual Model of the Relationship of Water Perceptions with Plain Water and SSB Consumption
The conceptual model in Figure 1 is based upon current evidence and describes plausible factors that may explain the relationship between perceptions of drinking water with water and SSB intake among youth. We understand water perceptions among school age children to be influenced by factors within the family and household, the school, and the larger community. These include perceived risk21–24 of water safety and contextual elements such as the affective evaluation of the cleanliness of school fountains. Variables known to be associated with perceiving water consumption as risky behavior are shown in the box labeled “Contextual & Control Variables Related to Cognitive Evaluations of Water” and include race/ethnicity, socio-economic status, sex, age, physical activity, and geographic region. Specifically, concerns regarding the safety of tap water may be more common among Black and Hispanic populations,20 lower-income populations,16, 20 women,25 and physically inactive persons.20 Age has also been associated with perceived risk of tap water consumption with younger adults more likely to have concerns regarding tap water safety.20 Finally, large regional differences in water perceptions have also been noted.20
Figure 1.
Conceptual Model for the Relationship of Water Perceptions with SSB and Water Intake Among Youth
As shown in the lower right box titled “Contextual & Control Variables Related to SSB and Water Intake“, race/ethnicity, socio-economic status, sex, age, physical activity, weight status and geographic region are also known determinants of SSB and/or water intake among youth. Both water and SSB intake is higher in teens than among younger children8, 11, 12 and higher among boys as compared to girls.8, 12 Although overall plain water intake doesn’t differ according to race/ethnicity,12 SSB intake is greater among Black youth as compared to white and Hispanic youth.8 Physically active youth tend to drink more water and sports drinks but less soda than inactive youth.8, 11, 26 Obese youth drink more water11, 12 and although SSB intake has been associated with weight gain,3 obese youth do not necessarily drink more SSB than normal weight youth26. Regarding geographic variation, wide variations in youth soda intake have been noted by state27 although differences in water intake and other SSB have not been reported.
METHODS
Participants
Data were collected through the 2010 YouthStyles mail survey administered by Synovate, Inc., a market research firm. This national survey was designed to assess health-related attitudes and behaviors among children. Participants were selected from among respondents to the ConsumerStyles survey, a consumer mail survey. ConsumerStyles participants are sampled from a consumer mail panel of approximately 200,000 potential respondents using a sampling design stratified on region, household income, population density, age, and household size, and includes an oversample of low-income/minority participants and households-with-children to ensure adequate representation of these groups.
In 2010, a total of 10,328 people completed the ConsumerStyles survey, with a response rate of 51.6%. Subsequently, 2401 YouthStyles surveys were sent to a stratified sample of ConsumerStyles survey respondents who had indicated that they had children aged 9 through 19 living in their home; survey instructions stated that a child or teen should complete the survey. Responses were received from 1197 YouthStyles participants, yielding a response rate of 49.9%. Responders did not differ from non-responders in parental income, home ownership, household size, or sex of child participant. However, response rates differed somewhat by child age (Chi-Square test, p = .001) with higher response rates seen among high school aged youth as compared to middle school and elementary school (55% response rate vs. 50% and 48%, respectively. Response rates also differed by parent race/ethnicity (p < .001) with Hispanics having a lower response rate (37%) as compared to non-Hispanic white (55%) and non-Hispanic black (52%).
The YouthStyles survey is weighted to match the U.S. Current Population Survey28, with individuals in the final sample assigned sample weights according to the age and sex of the child, household size, household income, head of household age, and race/ethnicity of the adult included in the ConsumerStyles survey. Additional data on parent perceptions of tap water safety were obtained in a separate adult survey (HealthStyles) and linked to YouthStyles child data using a common identifier variable. For the present analysis, 27 YouthStyles participants were excluded because they had missing data on SSB intake, 5 were excluded for missing data on plain water intake, 25 were excluded for missing data on water safety perceptions, 12 were excluded because they were more than 18 years of age at the time of the survey, and 84 were excluded because of race/ethnicity other than NH white, NH black, or Hispanic. This left a final analytic sample of 1044 participants (43.5% of sampled youth). Participants included in the final analytic sample did not differ significantly from excluded participants in regards to age, sex, or distribution of NH white, NH black, or Hispanic race/ethnicity.
Instruments
Exposure variables for tap water and school water fountain perceptions
Participants were asked to rate their agreement with the following statements: “My local tap water is safe to drink” and “Water fountains at school are clean and safe to drink from.” Response choices available for both of these items were “strongly disagree,” “somewhat disagree,” “neither agree nor disagree,” “somewhat agree,” and “strongly agree.” For bivariate analysis, 3 categories were created for each water perception variable: strongly/somewhat agree, neutral, and strongly/somewhat disagree. For logistic regression analysis, water perception variables were dichotomized. Participants were classified as perceiving tap water as unsafe if they responded “strongly disagree” or “somewhat disagree” that their local tap water was safe to drink and were classified as perceiving tap water as safe if they responded “neither agree nor disagree,” “somewhat agree,” and “strongly agree.” Participants were classified as evaluating water fountains as unsafe and unclean if they responded “strongly disagree” or “somewhat disagree” that their school water fountains were clean and safe to drink and were classified as evaluating water fountains as safe and clean if they responded “neither agree nor disagree,” “somewhat agree,” and “strongly agree.”
Additionally, a parent or caregiver of each YouthStyles participant was also asked in the HealthStyles Survey to rate their agreement with the statement: “My local tap water is safe to drink” with the same response options as above. Parent/caregiver responses for tap water perceptions were categorized for bivariate analysis in the same manner as for youth.
Outcome variables for water and SSB intake
Plain water intake was based upon the following question: “On a typical day, how many times do you drink a glass or bottle of plain water? Count tap, water fountain, bottled, and unflavored sparking water.” Response choices for water intake were “none,” “1 time per day,” “2 times per day,” “3 times per day,” “4 times per day,” or “5 times or more per day.” Participants were classified as having low intake of plain water if they responded “none,” “1 time per day,” or “2 times per day.” This definition of low water intake was based upon previous research among high school students using data from the 2010 National Physical Activity and Nutrition Study that showed an association of low water intake with other dietary and physical activity behaviors.11 SSB intake was based upon the following question: “During the past 7 days, how many times did you drink sodas, fruit drinks, sports or energy drinks, or other sugar-sweetened drinks? Do not include 100% fruit juice, diet drinks, or artificially sweetened drinks.” Response choices for SSB intake were “none,” “1 to 6 times per week,” “1 time per day,” “2 times per day,” “3 times per day,” or “4 or more times per day.” Participants were classified as daily SSB consumers if they responded that they consumed SSB “1 time per day” or more.
Sociodemographic variables
Race/ethnicity was classified as “NH white,” “NH black,” or “Hispanic” according to the self-reported race/ethnicity of children’s parent who completed the ConsumerStyles survey. Participants were classified into 3 age categories approximately corresponding to school level: 9–10 (elementary school), 11–13 (middle school), and 14–18 years of age (high school). Household income was classified into 3 categories based upon parent report: <$25,000, $25,000-$59,999, and >$59,999 with cutpoints approximately corresponding to 100% and 250% income to poverty level ratios for a family of four. Geographic regions of the country were classified according to the following 9 U.S Census Regions: New England, Middle Atlantic, South Atlantic, East North Central, East South Central, West North Central, West South Central, Mountain, and Pacific.
Physical activity was measured by asking participants the number of days during the past 7 days on which they exercised or participated in physical activity for at least 20 minutes. Participants were classified into 3 categories according to the number of days they reported: 0 days, 1–4 days, or ≥5 days. Weight status was classified according sex-specific body mass index (BMI) percentiles published by the Centers for Disease Control and Prevention using the participant’s self-reported height and weight.29 Children were classified as overweight if their BMI was equal to or greater than the 85th percentile for children their age and obese if their BMI was equal to or greater than the 95th percentile.29 For the purpose of determining a participant’s BMI percentile, each child was assumed to be at the midpoint of their current year of age (6 months after their last birthday) because age data were only available in whole years.
Data analysis/procedure
Analysis was conducted using SURVEYFREQ and SURVEYLOGISTIC procedures in SAS 9.2 (SAS Institute, Inc., Cary, North Carolina). Weighted frequencies of tap water and water fountain perceptions were compared to each other and to participant age, sex, race/ethnicity, family income, physical activity level, weight status, region, parental tap water perceptions, daily SSB intake, and low plain water intake using Chi-Square tests. Weighted multivariable logistic regression was used to assess the association of tap water and water fountain perceptions with daily SSB intake and low plain water intake.
Two separate models were fit to assess the association of tap and water fountain perceptions with each outcome (low water intake and daily SSB intake). Both models included perception of tap water and perception of school water fountains as the primary exposure variables along with covariables for age, sex, family income, race/ethnicity, region of country, physical activity level, and weight status. Model covariates were selected because they have been associated with water perceptions as well as water and/or SSB intake in previous research or in the current analysis. Because previous studies have observed racial/ethnic differences in perceptions of tap water safety and interactions on SSB and water intake among adults20, we assessed the interactions between race/ethnicity and the perceptions of tap water and water fountains. Likelihood ratio tests with alpha levels of.05 were used to assess the significance of interaction terms. To assess the appropriateness of the dichotomous classification of water perception variables in logistic models, sensitivity analysis was performed by refitting the models with separate variables corresponding to neutral and negative water perceptions as compared to positive water perceptions. The resulting race/ethnicity–specific odds ratios corresponding to negative water perceptions were then compared to original estimates where neutral perceptions were included in the reference categories.
RESULTS
Descriptive and Bivariate Analysis of Tap Water and Water Fountain Perceptions
Overall, 19.2% of youth disagreed that their local tap water was safe and 38.1% disagreed that their school water fountains were clean and safe. In addition, 43.6% of participants drank plain water twice per day or less often and 47.2% of participants drank SSB 1 time per day or more.
Bivariate associations of tap water and water fountain perceptions with sociodemographic characteristics are shown in Table 1. Perceptions of tap water safety differed significantly by race/ethnicity, family income, weight status, and parental perceptions of tap water safety. The perception that tap water was unsafe was more common among NH black and Hispanic youth, youth from lower-income families, and obese youth. Evaluations of school water fountain safety and cleanliness differed only according to age and physical activity level, with more middle and high school age youth and physically inactive youth disagreeing that fountains were clean and safe. Tap water perceptions and water fountain perceptions were also associated with each other; 75.2% of those who perceived tap water to be unsafe also evaluated water fountain as unsafe and unclean compared to only 27.8% of those who perceived tap water as safe. Youth tap water perceptions were also significantly associated with parent tap water perceptions: 56.7% of youth whose parent disagreed that tap water was safe also disagreed that tap water was safe.
Table 1.
Prevalence of Tap Water and School Water Fountain Perceptions According to Survey Respondent Characteristics
| Local Tap Water Perceptions | School Water Fountain Perceptions | |||||||
|---|---|---|---|---|---|---|---|---|
| “My local tap water is safe to drink” | “Water fountains in my school are clean and safe to drink from” | |||||||
| Disagree | Neutral | Agree | Chi-square p-value | Disagree | Neutral | Agree | Chi-square p-value | |
| N (weighted %*) | 179 (19.2) | 120 (13.2) | 745 (67.6) | 385 (38.1) | 150(14.8) | 509 (47.1) | ||
| Age (years) | .844 | .017 | ||||||
| 9–10 | 18.6 | 11.7 | 69.7 | 28.3 | 11.4 | 60.4 | ||
| 11–13 | 19.9 | 15.4 | 64.9 | 38.4 | 16.0 | 45.6 | ||
| 14–18 | 19.1 | 12.5 | 68.4 | 41.4 | 15.3 | 43.3 | ||
| Sex | .923 | .090 | ||||||
| Male | 18.7 | 13.2 | 68.2 | 34.3 | 15.8 | 50.0 | ||
| Female | 19.9 | 13.2 | 66.9 | 42.2 | 13.8 | 44.0 | ||
| Race/ethnicity | < .001 | .567 | ||||||
| White | 14.7 | 10.9 | 74.5 | 38.9 | 13.1 | 48.1 | ||
| Black | 26.4 | 13.9 | 59.7 | 36.6 | 16.5 | 46.9 | ||
| Hispanic | 28.3 | 20.4 | 51.3 | 36.8 | 19.2 | 44.0 | ||
| Annual household family income | .001 | .248 | ||||||
| <$25,000 | 24.3 | 22.7 | 53.1 | 34.7 | 21.8 | 43.5 | ||
| $25,000–$59,999 | 23.2 | 13.2 | 63.6 | 41.2 | 12.8 | 46.0 | ||
| >$59,999 | 15.3 | 10.7 | 74.0 | 37.0 | 14.2 | 48.8 | ||
| Weight status | < .001 | .917 | ||||||
| Missing | 17.5 | 15.6 | 66.9 | 32.2 | 16.0 | 51.8 | ||
| Normal/underweight | 17.2 | 12.5 | 70.3 | 39.5 | 14.6 | 45.9 | ||
| Overweight | 12.1 | 10.1 | 77.7 | 37.6 | 13.6 | 48.8 | ||
| Obese | 38.1 | 17.2 | 44.8 | 37.7 | 16.0 | 46.3 | ||
| Physical activity days/week | .113 | .027 | ||||||
| 0 days | 18.2 | 21.5 | 60.4 | 44.0 | 21.3 | 34.6 | ||
| 1–4 days | 20.3 | 12.2 | 66.4 | 40.1 | 14.4 | 45.5 | ||
| ≥ 5 days | 18.3 | 10.5 | 71.2 | 33.8 | 13.3 | 52.9 | ||
| Region | .087 | .279 | ||||||
| New England | 20.6 | 10.9 | 68.6 | 33.0 | 25.2 | 41.8 | ||
| Middle Atlantic | 17.2 | 15.2 | 67.6 | 44.8 | 12.9 | 42.3 | ||
| South Atlantic | 17.7 | 13.1 | 69.2 | 37.8 | 14.2 | 51.1 | ||
| East North Central | 12.0 | 9.5 | 78.5 | 28.2 | 12.5 | 59.3 | ||
| East South Central | 17.3 | 16.2 | 66.4 | 40.7 | 19.7 | 39.6 | ||
| West North Central | 13.7 | 10.8 | 75.6 | 30.6 | 18.2 | 51.1 | ||
| West South Central | 24.8 | 13.3 | 61.9 | 39.5 | 13.9 | 46.6 | ||
| Mountain | 29.6 | 8.4 | 62.0 | 40.2 | 16.4 | 43.4 | ||
| Pacific | 30.3 | 18.2 | 51.5 | 46.8 | 14.2 | 39.0 | ||
| Water fountain perceptions | < .001 | - | ||||||
| Agree school water fountains are clean and safe | 7.6 | 7.2 | 85.2 | - | - | - | ||
| Neutral school water fountains are clean and safe | 8.1 | 33.6 | 58.3 | - | - | - | ||
| Disagree school water fountains are clean and safe | 38.0 | 12.6 | 49.4 | - | - | - | ||
| Tap water perceptions | - | <.001 | ||||||
| Agree home tap water is safe | - | - | - | 27.8 | 12.8 | 59.4 | ||
| Neutral home tap water is safe | - | - | - | 36.5 | 37.8 | 25.7 | ||
| Disagree home tap water is safe | - | - | - | 75.2 | 6.2 | 18.6 | ||
| Parent tap water perceptions | < .001 | .019 | ||||||
| Parent agrees home tap water is safe | 9.1 | 9.4 | 81.6 | 34.0 | 14.9 | 51.2 | ||
| Parent neutral home tap water is safe | 27.3 | 25.9 | 46.9 | 46.8 | 12.9 | 40.4 | ||
| Parent disagrees home tap water is safe | 56.7 | 12.4 | 30.8 | 45.1 | 17.5 | 37.4 | ||
Because of rounding, weighted percentages may not add up to 100%.
Association of Tap and Water Fountain Perceptions with Plain Water Intake
Intake of plain water did not differ significantly by perceptions of tap water or water fountains (Table 2). Furthermore, tests of racial/ethnic interactions with low water intake on tap water and water fountain perceptions were not significant (Table 3, p = .352 for tap interaction; p = .237 for fountain interaction).
Table 2.
Prevalence of Low Plain Water and Daily SSB Intake According to Race/Ethnicity and Tap Water and School Water Fountain Perceptions
| Local Tap Water Perceptions | School Water Fountain Perceptions | |||||||
|---|---|---|---|---|---|---|---|---|
| “My local tap water is safe to drink” | “Water fountains in my school are clean and safe to drink from” | |||||||
| Disagree | Neutral | Agree | Chi-Square p-value | Disagree | Neutral | Agree | Chi-Square p-value | |
|
| ||||||||
| Prevalence of Low Plain Water Intake* (%) | ||||||||
| Overall | 44.2 | 41.1 | 43.9 | .988 | 40.2 | 49.0 | 44.6 | .762 |
| NH White | 49.8 | 41.9 | 46.8 | .761 | 45.8 | 48.0 | 47.2 | .902 |
| NH Black | 38.9 | 31.2 | 33.2 | .817 | 27.6 | 43.2 | 38.1 | .201 |
| Hispanic | 38.7 | 43.2 | 40.3 | .741 | 31.8 | 55.7 | 41.0 | .969 |
| Prevalence of Daily SSB Intake (%) | ||||||||
| Overall | 47.6 | 50.6 | 46.3 | .771 | 46.0 | 44.0 | 49.1 | .574 |
| NH White | 41.9 | 50.2 | 43.5 | .583 | 40.7 | 38.9 | 48.0 | .178 |
| NH Black | 52.8 | 50.7 | 60.0 | .766 | 45.2 | 60.0 | 64.8 | .198 |
| Hispanic | 53.5 | 51.3 | 46.1 | .790 | 65.3 | 43.5 | 38.3 | .023 |
Because of rounding, weighted percentages may not add up to 100%.
Table 3.
Associations of Plain Water Intake and Daily Intake of Sugar-Sweetened Beverages with Negative Perceptions of Tap Water and Water Fountains
| Local tap water perceptions | School water fountains perceptions | |
|---|---|---|
| “My local tap water is safe to drink” | “Water fountains in my school are clean and safe to drink from” | |
| Disagree vs. Neutral or Agree | Disagree vs. Neutral or Agree | |
| Multivariable ORs for low plain water intake (≤ 2 time/day))*,† | ||
| All respondents | 1.4 (0.9, 2.1) | 0.7 (0.5, 1.0) |
| Non-Hispanic white | 1.3 (0.8, 2.2) | 0.9 (0.6, 1.3) |
| Non-Hispanic black | 2.6 (0.7, 9.1) | 0.4 (0.1, 1.4) |
| Hispanic | 1.2 (0.5, 3.2) | 0.5 (0.2, 1.3) |
| Multivariable ORs for daily SSB intake (≥ 1 time/day)*,† | ||
| All respondents | 1.0 (0.6, 1.5) | 1.0 (0.7, 1.4) |
| Non-Hispanic white | 0.9 (0.6, 1.6) | 0.9 (0.6, 1.3) |
| Non-Hispanic black | 1.5 (0.5, 4.8) | 0.5 (0.2, 1.2) |
| Hispanic | 0.7 (0.3, 1.9) | 2.9 (1.3, 6.6) |
Interaction between Hispanic race and drinking fountain perceptions on SSB intake significant (p < .001). All other race and water perception interactions were not significant (p > .05)
ORs in bold denote significant findings based on the 95% CI (i.e., the CI does not include 1.0). ORs are adjusted for age, sex, household income, regions of country, physical activity level, and weight status.
Association of Tap and Water Fountain Perceptions with SSB Intake
Results concerning the bivariate association of tap water and water fountain perceptions with SSB intake are shown in Table 2. The proportion of youth who consumed SSB daily did not differ according to tap water perceptions either overall or among specific racial/ethnic subgroups. This did not change after the data were fit to a multivariable logistic regression model; the race/ethnicity interaction with tap water perceptions was not significant (Table 3, p =.427). Evaluation of school water fountains as unsafe and unclean was associated with daily SSB intake only among Hispanic participants (Table 2). Specifically, 65.3% of Hispanic participants who evaluated water fountains as unsafe and unclean reported daily SSB consumption compared to 43.5% of those who were neutral and 38.3% of those who considered water fountains safe and clean (Table 2). In the multivariable logistic regression model, the association between water fountain perceptions and SSB intake differed significantly by race/ethnicity (Table 2, p <.001). In the final multivariable logistic regression model, the odds of daily SSB intake were 2.9 times greater among Hispanics who disagreed that their school water fountains were safe and clean than among Hispanics who were neutral or agreed that their water fountains were safe and clean (Table 3).
In sensitivity analysis of the classification of water perceptions, the direction and significance of race-specific ORs for SSB intake and low plain water intake were unchanged, and the magnitude of ORs was similar when neutral responses to water perception questions were removed from reference categories (results not shown).
DISCUSSION
The results of this study suggest that 1 in 5 youth perceive their tap water to be unsafe and nearly 2 in 5 youth consider their school water fountains to be unsafe and unclean. Youth perceptions of tap water safety were strongly associated with parental perceptions of tap water safety and differed by race/ethnicity, family income, and weight status, but were not associated with SSB intake. Although evaluation of school water fountain safety and cleanliness did not differ significantly by race/ethnicity or socioeconomic status, negative evaluation of school water fountains was associated with greater intake of SSB among Hispanic youth but not among NH black or NH white youth. However, neither tap water nor school water fountain perceptions were associated with low plain water intake. Nonetheless, this study reinforces the high prevalence of low plain water intake among youth with nearly half of the participants (43.6%) drinking plain water twice per day or less often, which is consistent with previous research.26
To our knowledge, this is the first quantitative study to examine perceptions of tap water and school water fountains among US youth. The racial/ethnic differences in tap water perceptions detected in this study are consistent with other studies that found that perceived risk of tap water is more common among NH black and Hispanic adults.16, 17, 20 The association of a negative evaluation of water fountain safety and cleanliness with daily SSB intake among Hispanic youth is consistent with findings by the authors suggesting an association of tap water risk perception with SSB intake among Hispanic adults.20 Furthermore, in a qualitative study conducted in California, school and public health officials, students, and parents reported that immigrant status from Latin American countries such as Mexico may be a determinant of perceived risk of tap water consumption,15 perhaps because drinking water supplies in these countries may not be considered safe. In another small focus group study, Hispanic adults from California’s rural Central Valley region reported regularly drinking SSB and juice when filtered or bottled water was not available.30 Interestingly, we did not find a similar association between tap water perceptions with SSB intake among Hispanic youth. Research suggests that Hispanic parents who do not trust their tap water serve bottled water to their children.19 Outside of the home however, where bottled water is not freely available and where youth are more independent to choose what they drink, they may choose to purchase SSB rather than bottled water. The lack of association between tap and water fountain perceptions with plain water intake in our study may also reflect the high intake of bottled water among this study population. Specifically, subsequent ad-hoc analysis of the dataset determined that 69% of the participants reported drinking bottled water at least once on the day prior to the survey and 38% reported drinking 2 or more bottled waters. With bottled water intake constituting such a major source of plain water, tap and water fountain perceptions may not necessarily impact overall water intake among this population.
Limitations
The primary limitations of this study are the sample design and the self-report of data using single item instruments. Regarding the sample design, it is possible that the findings are not generalizable nationally because of selection bias associated with the use of a mail panel convenience sample with a relatively low response rate. While HealthStyles draws its sample from a large mail panel rather than a true random sample of the population, a previous study has shown that prevalence estimates of several health conditions, attitudes, and behaviors from HealthStyles are reasonably comparable to those obtained through the Behavioral Risk Factor Surveillance System, which uses a probability-sampling technique.31 Regarding survey items, the lack of an association of tap water and water fountain perceptions with plain water intake may be caused by a measurement error of plain water intake resulting from having only 1 survey question to collect information about tap water consumption. Furthermore, dietary reporting among children in general may be subject to bias, although research suggests that children aged 9 years and above are generally capable of accurately reporting their dietary intake.32 Another data limitation is self-report of height and weight used to derive weight status; a literature review found that bias existed by weight status and sex, so we may have underestimated obesity status, particularly among girls.33 However, some research suggests that students as young as fifth graders (generally 10–11 years of age) are reasonably able to report their height and weight.34 Although our sample does include 94 children who are 9 years of age (8% of the final study sample), we feel that weight status is an important variable to include in the present analysis due to its status as a potential confounder. Specifically, weight status has been associated with water and SSB intake as well as with tap water safety perceptions. It is also possible that our finding that negative evaluation of school water fountains was associated with greater intake of SSB among Hispanic youth was due to chance because we estimated 16 separate odds ratios. Regarding race/ethnicity, because youth were not asked to report their race/ethnicity, classification of youth race/ethnicity was based upon the self-reported race/ethnicity of the participating parent and therefore, could differ from race/ethnicity that would be reported by the child. Finally, although previous research suggests that acculturation may be an important factor in water perceptions,15 it was not possible to ascertain whether racial/ethnic differences in observed associations were further modified by country of birth or acculturation because this information was not collected in the survey.
Conclusion
While perceived risk of local tap water and negative evaluation of school water fountain safety and cleanliness are both common among youth, different factors may influence each. Specifically, this study suggests that perceived risk of tap water is more common among lower income youth and youth from minority racial/ethnic groups. The evaluation of water fountains as unclean and unsafe does not differ by race/ethnicity or income but becomes more common with increasing age.
Negative evaluation of school water fountains was associated with greater intake of SSB among Hispanic youth but not among NH black or NH white youth. However, neither tap water nor school water fountain perceptions were associated with low plain water intake among youth, suggesting that youth may still not choose to drink water even when they believe that water is safe and water fountains are clean. Taken together, this information can help to inform school efforts to encourage water consumption among students and their families.
Given these potentially important racial/ethnic differences and the complexity of these findings, the role of student perceptions of tap water and water fountains may play as determinants of plain water and SSB intake among youth should be examined further. With the high prevalence of daily SSB intake and low plain water intake, public health and school professionals must find ways to promote tap water as a desirable beverage choice among American youth.
IMPLICATIONS FOR SCHOOL HEALTH
Tap water is an inexpensive35 and calorie free beverage that can reduce the intake of excess calories and added sugars when substituted for other beverages among youth.10 Given the recent mandate in the Healthy, Hunger-Free Kids Act of 2010 for schools participating in the National School Lunch Program to provide free drinking water to students during lunch times in places where meals are served, the findings of this study suggest that school efforts to provide drinking water to children should acknowledge that perceived risk of tap water is common, especially among minority and low income children. Nonetheless, since nearly 70% of youth agree that local tap water is safe to drink, there is hope that creative promotion and marketing of tap water in schools settings could lead to successful efforts to increase water intake among youth. Furthermore, negative evaluation of water fountain safety and cleanliness was nearly twice as common as negative perceptions of tap water safety, suggesting that much of students’ negative perceptions concerning school water fountains may pertain to cleanliness, which might be easier to address than concerns around the safety of tap water itself. Schools with existing water fountains should ensure that they are cleaned and maintained regularly. Given the increasing prevalence of negative water fountain perceptions with age, efforts to clean and maintain water fountains are of particular importance in middle and high schools. Future studies should further examine water intake in school settings and also seek to separate the effects of tap water safety and dispenser cleanliness on water and SSB intake by students.
Finally, since the present study did not find an association between tap water or water fountain perceptions with water intake, our research suggests that schools must find ways to effectively promote tap water as an attractive beverage choice among youth. Schools might look to college campuses, where environmental concerns have motivated successful campaigns to promote tap water on campuses throughout the country.36 Other ways schools can promote water consumption might be through promotional activities around water or by allowing youth to utilize refillable water bottles. Considering that the vast majority of SSB are consumed by youth outside of school,37 successful school efforts to encourage youth to choose water as a beverage at school should also aim to influence youth to drink more water and less SSB in other settings as well. Although this study suggests that negative perceptions of tap water and school drinking fountains are common, promising research is emerging to show that water can be presented to youth in an attractive manner that encourages them to drink it.13, 38
Footnotes
HUMAN SUBJECTS APPROVAL
This analysis was exempt from the CDC Institutional Review Board process because personal identifiers were not included in the data provided to the Centers for Disease Control and Prevention.
Conflict of interest statement: None of the authors has conflicts of interest to declare.
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Stephen J Onufrak, Email: seo5@cdc.gov, Epidemiologist, Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, Atlanta, Georgia.
Sohyun Park, Email: geo7@cdc.gov, Epidemiologist, Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, Atlanta, Georgia.
Joseph R Sharkey, Email: jrsharkey@srph.tamhsc.edu, Professor, Texas A&M Health Science Center, School of Rural Public Health, Department of Health Promotion and Community Health Sciences, College Station, Texas.
Caitlin Merlo, Email: ihb7@cdc.gov, Health Scientist, Centers for Disease Control and Prevention, Division of Division of Population Health, Atlanta, Georgia.
Wesley R. Dean, Email: wdean@srph.tamhsc.edu, Assistant Professor, Texas A&M Health Science Center, School of Rural Public Health, Department of Health Promotion and Community Health Sciences, College Station, Texas.
Bettylou Sherry, Email: bls6@cdc.gov, Lead Epidemiologist, Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, Atlanta, Georgia.
References
- 1.U.S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7. Washington, DC: U.S. Government Printing Office; Dec, 2010. http://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf. [Google Scholar]
- 2.Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc. 2010;110(10):1477–1484. doi: 10.1016/j.jada.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu F, Malik V. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100(1):47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apovian CM. Sugar-sweetened soft drinks, obesity, and type 2 diabetes. J Am Med Assoc. 2004;292(8):978–979. doi: 10.1001/jama.292.8.978. [DOI] [PubMed] [Google Scholar]
- 5.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs, et al. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation. 2007;116(5):480–488. doi: 10.1161/CIRCULATIONAHA.107.689935. [DOI] [PubMed] [Google Scholar]
- 6.Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89(4):1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohn W, Burt BA, Sowers MR. Carbonated soft drinks and dental caries in the primary dentition. J Dent Res. 2006;85(3):262–266. doi: 10.1177/154405910608500311. [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Kit BK, Carroll MD, Park S. NCHS Data Brief. 71. Hyattsville, MD: National Center for Health Statistics; 2011. Consumption of sugar drinks in the United States, 2005–2008; pp. 1–8. [PubMed] [Google Scholar]
- 9.Brener N, Merlo C, Eaton D, Kann L, Park S, Blanck HM. Beverage consumption among high school students — United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(23):778–780. [PubMed] [Google Scholar]
- 10.Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163(4):336–343. doi: 10.1001/archpediatrics.2009.23. [DOI] [PubMed] [Google Scholar]
- 11.Park S, Blanck HM, Sherry B, Brener N, O’Toole T. Factors associated with low water intake among US high school students-National Youth Physical Activity and Nutrition Study, 2010. J Acad Nutr Diet. 2012;112:1421–1427. doi: 10.1016/j.jand.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kant AK, Graubard BI. Contributors of water intake in US children and adolescents: associations with dietary and meal characteristics--National Health and Nutrition Examination Survey 2005–2006. Am J Clin Nutr. 2010;92(4):887–896. doi: 10.3945/ajcn.2010.29708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled Cluster trial. Pediatrics. 2009;123(4):E661–E667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Agriculture. [Accessed November 1, 2012];Healthy Hunger-Free Kids Act of 2010. Available at: http://www.fns.usda.gov/cnd/Governance/Legislation/CNR_2010.htm.
- 15.Patel AI, Bogart LM, Uyeda KE, Rabin A, Schuster MA. Perceptions about availability and adequacy of drinking water in a large California school district. Prev Chronic Dis. 2010;7(2):A39. [PMC free article] [PubMed] [Google Scholar]
- 16.Gorelick MH, Gould L, Nimmer M, Wagner D, Heath M, Bashir H, et al. Perceptions about water and increased use of bottled water in minority children. Arch Pediatr Adolesc Med. 2011;165(10):928–932. doi: 10.1001/archpediatrics.2011.83. [DOI] [PubMed] [Google Scholar]
- 17.Hobson W, Knochel M, Byington C, Young P, Hoff C, Buchi K. Bottled, filtered, and tap water use in Latino and non-Latino children. Arch Pediatr Adolesc Med. 2007;161(5):457–461. doi: 10.1001/archpedi.161.5.457. [DOI] [PubMed] [Google Scholar]
- 18.Hu Z, Morton LW, Mahler RL. Bottled water: United States consumers and their perceptions of water quality. Int J Environ Res Public Health. 2011;8(2):565–578. doi: 10.3390/ijerph8020565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huerta-Saenz L, Irigoyen M, Benavides J, Mendoza M. Tap or bottled water: Drinking preferences among urban minority children and adolescents. J Community Health. 2012;37(1):54–58. doi: 10.1007/s10900-011-9415-1. [DOI] [PubMed] [Google Scholar]
- 20.Onufrak SJ, Park S, Sharkey JR, Sherry B. The relationship of perceptions of tap water safety with intake of sugar-sweetened beverages and plain water among US adults. Public Health Nutr. 2013;113(1):112–9. doi: 10.1017/S1368980012004600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- 22.Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 23.Poortinga W, Pidgeon NF. Trust in risk regulation: cause or consequence of the acceptability of GM food? Risk Anal. 2005;25(1):199–209. doi: 10.1111/j.0272-4332.2005.00579.x. [DOI] [PubMed] [Google Scholar]
- 24.de Franca Doria M, Pidgeon N, Hunter P. Perception of tap water risks and quality: a structural equation model approach. Water Sci Technol. 2005;52(8):143–149. [PubMed] [Google Scholar]
- 25.Saylor A, Prokopy LS, Amberg S. What’s wrong with the tap? Examining perceptions of tap water and bottled water at Purdue University. Environ Manage. 2011;48(3):588–601. doi: 10.1007/s00267-011-9692-6. [DOI] [PubMed] [Google Scholar]
- 26.Park S, Blanck HM, Sherry B, Brener N, O’Toole T. Factors associated with sugar-sweetened beverage intake among United States high school students. J Nutr. 2012;142(2):306–312. doi: 10.3945/jn.111.148536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 28.United States Census Bureau. [Accesed August 31, 2012];Current Population Survey (CPS) 2012 Available at: http://www.census.gov/cps/
- 29.Centers for Disease Control and Prevention. [Accessed September 5, 2012];About BMI for Children and Teens. Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- 30.Scherzer T, Barker JC, Pollick H, Weintraub JA. Water consumption beliefs and practices in a rural Latino community: implications for fluoridation. J Public Health Dent. 2010;70(4):337–343. doi: 10.1111/j.1752-7325.2010.00193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollard WE. Use of a consumer panel survey for public health communication planning: An evaluation of survey results. Proceedings of the American Statistical Association, Section on Health Policy Statistics; New York. 2002. pp. 2120–2124. [Google Scholar]
- 32.Livingstone MB, Robson PJ. Measurement of dietary intake in children. Proc Nutr Soc. 2000;59(2):279–293. doi: 10.1017/s0029665100000318. [DOI] [PubMed] [Google Scholar]
- 33.Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Arch Pediatr Adolesc Med. 2007;161(12):1154–1161. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- 34.Beck J, Schaefer CA, Nace H, Steffen AD, Nigg C, Brink L, et al. Accuracy of self-reported height and weight in children aged 6 to 11 years. Prev Chronic Dis. 2012;9:E119. doi: 10.5888/pcd9.120021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Environmental Protection Agency. [Accessed November 15, 2012];Drinking Water Costs & Federal Funding. 2004 Available at: http://water.epa.gov/lawsregs/guidance/sdwa/upload/2009_08_28_sdwa_fs_30ann_dwsrf_web.pdf.
- 36.Koch W, Marohn K. Hydration stations sweep colleges to promote tap water. [Accessed December 15, 2012];USA Today. 2011 Available at: http://usatoday30.usatoday.com/news/education/story/2011-09-14/water-bottle-college/50403454/1.
- 37.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 38.Patel AI, Bogart LM, Elliott MN, Lamb S, Uyeda KE, Hawes-Dawson J, et al. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Prev Chronic Dis. 2011;8(3):A60. [PMC free article] [PubMed] [Google Scholar]