Abstract
Background
China is one of the countries with the highest prevalence of diabetes in the world. We analysed all the death certificates mentioning diabetes from 2002 to 2012 in Songjiang District of Shanghai to estimate morality rates and examine cause of death patterns.
Methods
Mortality data of 2654 diabetics were collected from the database of local CDC. The data set comprises all causes of death, contributing causes and the underlying cause, thereby the mortality rates of diabetes and its specified complications were analysed.
Results
The leading underlying causes of death were various cardiovascular diseases (CVD), which collectively accounted for about 30 % of the collected death certificates. Diabetes was determined as the underlying cause of death on 28.7 %. The trends in mortality showed that the diabetes related death rate increased about 1.78 fold in the total population during the 11-year period, and the death rate of diabetes and CVD comorbidity increased 2.66 fold. In all the diabetes related deaths, the proportion of people dying of ischaemic heart disease or cerebrovascular disease increased from 18.0 % in 2002 to 30.5 % in 2012. But the proportions attributed directly to diabetes showed a downtrend, from 46.7–22.0 %.
Conclusions
The increasing diabetes related mortality could be chiefly due to the expanding prevalence of CVD, but has nothing to do with diabetes as the underlying cause. Policy makers should pay more attention to primary prevention of diabetes and on the prevention of cardiovascular complications to reduce the burden of diabetes on survival.
Electronic supplementary material
The online version of this article (doi:10.1186/s12902-015-0042-1) contains supplementary material, which is available to authorized users.
Background
Diabetes is a global epidemic with nearly 350 million cases [1]. According to the data from the World Health Organization (WHO), over 3 million people die worldwide from diabetes and its related complications every year [2]. China is the country with the second highest diabetes rate in the world [3]. The development and expansion of China’s economy over the past decade, has led to dramatic changes in people’s lifestyle and an increase in life expectancy, not only in cities but also in rural areas. But changes in lifestyle and diet associated with an improvements in socioeconomic status may contribute to an increasing diabetes burden in China [4, 5]. A national survey conducted in 2009 estimated age-standardized prevalences of 9.7 and 15.5 % for diabetes and prediabetes, which accounted for 92.4 million and 148.2 million adults, respectively [6]. These estimates are approximately tripled and quintupled, respectively, from earlier estimates from survey data collected in early 1990s [7].
Many people with diabetes do not die from hyperglycaemia itself; the top causes of death are various complications, among which cardiovascular diseases and nephropathy are the most common [8–10]. This results in a difficulty for estimating the burden of diabetes on survival. There are normally two measures estimating the burden of diabetes, diabetes related death and diabetes as the underlying cause of death. For the diabetes related death, underreporting in death certificate is very common worldwide. It was found that only about 40 % diabetes had been recorded on the death certificates of decedents with known diabetes [11–18]. On the other hand, the state of existing routine vital statistics worldwide may omit mention of diabetes as an underlying cause of death [19]. The recording cause of death can also be affected by subjective judgement of physicians and different coding systems among countries [20, 21].
In 1980s, China’s Ministry of Health established the vital registration system (MOH-VR) to record the fact and cause of death. However, the accuracy and representativeness of data from the system are biased due to some limitations such as variability in quality control measures and coverage between different areas [22]. Therefore, the Ministry of Health instructed departments of health at the province and county levels to establish the Chinese Disease Surveillance Points System (DSP) from which cause specific mortalities are monitored for a nationally representative sample. In 2013, there were 605 DSP sites nationwide covering over 1 % of the national population [22]. Shanghai Songjiang District is one of the DSP sites since 1990s.
In the present study, a file of coded death certificate data was supplied by the Songjiang Center for Disease Control and Prevention (CDC). The data set comprises all causes of death including the contributing causes and the underlying cause associated with diabetes mellitus between January 2002 and December 2012. From these data, we described the changing patterns of mortalities related to diabetes, and analysed its health burden for the last decade. To the best of our knowledge, this is the first study reporting epidemiological data concerning mortalities related to diabetes in China.
Methods
Songjiang District is one of the administrative regions of the Shanghai municipality located to the South of the city centre, covering 15 communities including rural and urban areas. According to the data from the government, the population of Songjiang District was approximately 500,000 in 2002. With a natural population growth rate of about 15 per thousand, the registered permanent residents increased to 583,000 in 2012.
Data on mortality status were ascertained through death certificates completed by local physicians, validated by specific staff, and archived (electronic data) with the local CDC. The detailed working procedure for mortality registration and surveillance is described elsewhere [22, 23]. The information in the death certificate includes demographic variables for each decedent, such as sex, date of birth and date of death, all causes of death (related and underlying), as well as some other death status such as death place, diagnostic basis of death, the level of the institute providing diagnosis etc. By considering ethical issues, we used anonymized death registration data with hiding personal identification, so that no individual could be identified. Therefore individual institutional approval was unnecessary. The dataset can be found in Additional file 1.
The present study includes data for all deaths related to diabetes (ICD-10 E10-E14) among the permanent residents, during the 11-year period from 2002 to 2012. The fourth character subdivisions under ICD-10 E10-E14 were used to analyse diabetic complications.
Statistical analysis was performed using the PASW statistics version 18 (SPSS) for Windows. Values of p < 0.05 were deemed as statistically significant. Normally distributed continuous clinical data were presented as means ± SD, whereas non-normally distributed continuous data were presented as median and interquartile range (IQR; P25–P75), unless otherwise stated. To test temporal trends, we performed the Spearman rank correlations of mortalities and time. Interval estimations (95 % confidence interval, 95 % CI) were used to analyse statistical significances of proportion differences between 2002 and 2012.
Results
Description of total sample
There were 2654 diabetes related deaths in the period 2002–2012 (1269 men, 1385 women). This represents 6.6 % (2654/40059) of all deaths in Songjiang District. The age of the deceased ranged between 18 and 101 years, median 76 (IQR: 68 – 82) years. Of these deaths, there were 21 (0.8 %) type 1 diabetics, 1168 (44.0 %) type 2 diabetics, 1462 (55.1 %) cases with unspecified diabetes (ICD-10 E14), and 3 cases that were allocated to other specified diabetes (ICD-10 E13). Overall, diabetes was determined as the underlying cause of death on 28.7 % (762 cases) of the collected death certificates.
For 2332 deceased, the diagnosis of the cause of death was based on medical records, which accounts for 87.9 % of all the involved subjects; 268 (10.1 %) deaths were diagnosed based on pathologic findings; 36 (1.4 %) deaths were determined in surgical operations; and 14 (0.5 %) deaths were determined by executed autopsy. There were 1495 (56.3 %) home deaths and 1045 (39.4 %) deaths occurred in health facilities. The remaining 114 (4.3 %) deaths died on the way to hospital or somewhere else.
Table 1 shows all of the underlying causes of death for the subjects with diabetes from 2002 to 2012. The leading causes of death were cardiovascular diseases, diabetes mellitus, neoplasms, and respiratory diseases. These accounted for 88.4 % of all the causes of death. Women more frequently died from unspecified diabetes, cerebrovascular diseases and injury than men; whereas the cause of death for men was more frequently attributed to tumour, hypertension and respiratory disease than women (p < 0.05, Chi-square test).
Table 1.
Causes of death for diabetics in Songjiang District 2002–2012
| Total no. (%) | Male | Female | P value† | |
|---|---|---|---|---|
| All causes | 2654 (100) | 1269 (100) | 1385 (100) | - |
| Diabetes as the underlying cause | 762 (28.7) | 323 (25.5) | 439 (31.7) | <0.01 |
| Type 1 diabetes (E10) | 15 (0.6) | 7 (0.6) | 8 (0.6) | 0.93 |
| Type 2 diabetes (E11) | 306 (11.5) | 134 (10.6) | 172 (12.4) | 0.13 |
| Unspecified diabetes (E14) | 441 (16.6) | 182 (14.3) | 259 (18.7) | <0.01 |
| Infections (A00-B99) | 68 (2.6) | 32 (2.5) | 36 (2.6) | 0.90 |
| Neoplasms (C00-D48) | 612 (23.1) | 339 (26.7) | 273 (19.7) | <0.01 |
| Mental and behavioural disorders (F00-F99) | 9 (0.3) | 4 (0.3) | 5 (0.4) | 1.00‡ |
| Neuropathies (G00-G99) | 15 (0.6) | 8 (0.6) | 7 (0.5) | 0.67 |
| Cardiovascular diseases (CVD) (I00-I99)a | 793 (29.9) | 362 (28.5) | 431 (31.1) | 0.15 |
| Hypertension (I10-I15) | 25 (0.9) | 17 (1.3) | 8 (0.6) | 0.04 |
| Ischaemic heart diseases (I20-I25) | 232 (8.7) | 112 (8.8) | 120 (8.7) | 0.88 |
| Cerebrovascular diseases (I60-I69) | 522 (19.7) | 226 (17.8) | 296 (21.4) | 0.02 |
| Other CVDsa | 14 (0.5) | 7 (0.6) | 7 (0.5) | 0.86 |
| Respiratory diseases (J00-J99) | 178 (6.7) | 113 (8.9) | 65 (4.7) | <0.01 |
| Diseases of the digestive system (K25-K93) | 63 (2.4) | 33 (2.6) | 30 (2.2) | 0.46 |
| Diseases of the musculoskeletal system and connective tissue (M00-M99) | 14 (0.5) | 4 (0.3) | 10 (0.7) | 0.18‡ |
| Nephropathy (N00-N19) | 16 (0.6) | 8 (0.6) | 8 (0.6) | 0.86 |
| Other disorders of the genitourinary system (N20-N99) | 6 (0.2) | 4 (0.3) | 2 (0.1) | 0.43‡ |
| External causes (V01-Y98) | 111 (4.2) | 38 (3.0) | 73 (5.3) | <0.01 |
| Othersa | 7 (0.3) | 1 (0.1) | 6 (0.4) | 0.13‡ |
Data are shown as frequencies and percentages
†Chi-square test, unless otherwise stated
‡Fisher’s exact test
aThe ICD-10 code I46 is not included in CVD category but in the category of others, since it is not a cause of death referring to CVD
The burden of diabetic complications
Of the 2654 diabetes related deaths, 1943 (73.2 %) deceased were diagnosed with comorbidity of diabetes and circulatory system diseases (ICD-10 I00–I99, excluding I46); and no statistical difference was shown by gender (p = 0.10, Chi-square test). Diabetes specified complications were determined according to the fourth character subdivisions under ICD-10 codes E10–E14. The distribution of complications in the deceased with diabetes as underlying cause of death is shown in Fig. 1. In addition to the circa 38 % deceased without complications, the leading causes were renal complications, other specified complications, multiple complications, and peripheral circulatory complications, which collectively accounted for over 45 % of deaths where diabetes was the underlying cause.
Fig. 1.
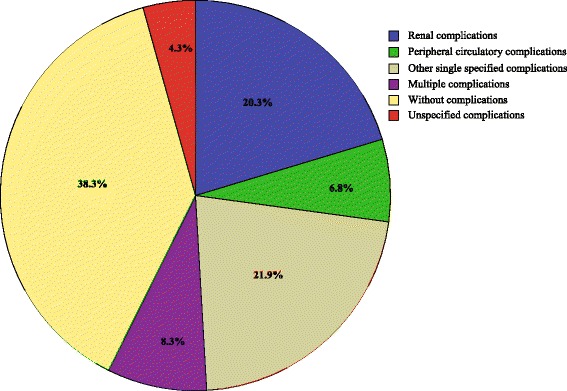
The distribution of diabetes specified complications in the decedents with diabetes as underlying cause of death in 11 years
Trends in mortality and proportion during the 11-year period
Of all the diabetes related deaths, type 2 diabetes and the unspecified diabetes (ICD-10 E14) accounted for over 97 % of cases in each of every year from 2002 to 2012. However, there were divergent trends: the proportion of unspecified diabetes declined, whereas the proportion of type 2 diabetes presented an ascendant pattern. For more detail please find in Additional file 2: Figure S1.
Annual crude mortality rates for all-causes were relatively stable during the 11-year period ranging 63.19 per ten thousand to 74.39 per ten thousand for the Songjiang population (see Additional file 3: Table S1). The diabetes related death rate was 2.44 per ten thousand in 2002, increasing to 6.78 per ten thousand in 2012. The death rates of diabetes and cardiovascular diseases comorbidity exhibited the same rising trend, from 1.52 per ten thousand in 2002 to 5.55 per ten thousand in 2012. The mortalities of diabetes as the underlying cause rose slightly from 1.14 per ten thousand in 2002 to 1.49 per ten thousand in 2012. These rates are shown in Fig. 2. The Spearman’s rho were −0.24 (p = 0.31), 0.89 (p < 0.01), 0.49 (p = 0.04), and 0.89 (p < 0.01) for the correlations between all-cause mortality and the year of death, between diabetes related death rate and the year of death, between the mortality of diabetes as the underlying cause and the year of death, between the death rate of diabetes and CVD comorbidity and the year of death, respectively.
Fig. 2.
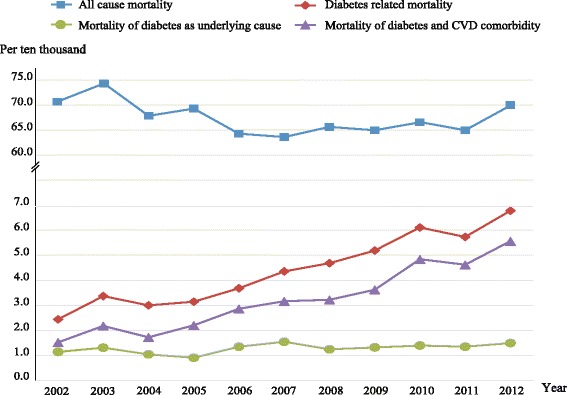
Changing patterns in crude death rates from 2002 to 2012. The denominators are the average total population in Songjiang District for every year
Of all diabetes related deaths, the proportions attributed directly to diabetes as the underlying cause decreased from 46.7 % in 2002 to 22.0 % in 2012 (95 % CI of the rate difference ranged from 15.0–34.5 %). The corresponding Spearman’s rho = −0.92 (p < 0.01). The proportions of deceased without complications followed a similar downtrend from 24.6 in 2002 to 6.3 % in 2012 (95 % CI of the rate difference ranged from 10.3–26.3 %). The Spearman’s rho = −0.93 (p < 0.01). In comparison, the proportions of deceased diabetics who died from renal complications varied within a narrow range, from 6.6 % in 2002 to 5.1 % in 2012 (95 % CI of the rate difference ranged from −3.4–6.4 %). The Spearman’s rho = −0.45 (p = 0.17). The proportions of deceased diabetic due to cardiovascular diseases showed an ascendant trend, of which ischaemic heart diseases as underlying cause of death increased from 3.3 % in 2002 to 9.8 % in 2012 (95 % CI of the rate difference ranged from −10.9–2.3 %), and cerebrovascular diseases increased from 14.8 % in 2002 to 20.7 % in 2012 (95 % CI of the rate difference ranged from −13.4–1.5 %). The values of Spearman’s rho were 0.70 (p = 0.02) and 0.60 (p = 0.05), respectively. These changing patterns are shown in Fig. 3.
Fig. 3.
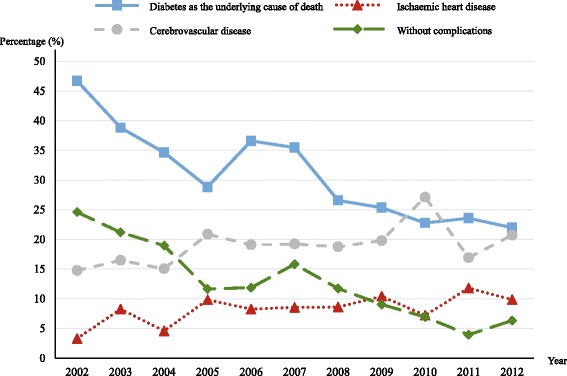
Changing patterns in proportions of the underlying cause of death for diabetes, cardiovascular diseases, and diabetes without complications. The denominators are the number of diabetes related deaths for every year
Discussion
Trends in mortalities tend to reflect the level of economic development and the changing pattern of health services of a country or region [24, 25]. In the present study, it showed an increased trends in diabetes related mortality with growing proportions of CVD prevalence and mortality in a Chinese population. In the first decade of the 21st century, China has been one of the most rapidly developing countries in the world with an increase in life expectancy and changes in lifestyle [4]. The crude death rates for China, including for Shanghai [26] and Songjiang have varied only slightly during this decade, but the diabetes mortality (diabetes related death) increased about 1.78 fold (see Fig. 2) in Songjiang District. Similarly, the prevalence of diabetes has increased dramatically during a similar period in China, from 5.5 % in 2001 [27] to 11.6 % in 2010[28]. This reveals that the increased diabetics should be owed to the growth of incidence, which should be faster than the growth of mortality. Certainly, the development of medical techniques should help to detect more and more individuals with undiagnosed diabetes since last decades, which could led to a pseudo increase of incidence. In spite of the striking increase of diabetes related death (by 178 %), the mortality of diabetes as the underlying cause increased only 30 %. In addition, the proportion of diabetes as the underlying cause reduced significantly, of which especially the proportion of subject without complications (Fig. 3). This may reflect improvement of health service like effective treatment of hyperglycaemia and efforts to prevent diabetic complications (not counting CVD) by local health care systems. On the other hand, it suggests that the central and local governments should pay more attention to primary preventions aimed at lowering the incidence and ultimately to reduce the burden of diabetes. Moreover, the descending proportion of unspecified type may be attributable to improvements in proper diagnosis by clinicians. That is, the types of diabetes for a large amount of decedents had been already clarified and/or recorded before death. This is in conformity with the progress of local health service (Data from “Statistic Yearbook of Songjiang” 2004 – 2013,published by local government).
People with type 2 diabetes have an increased risk of developing CVD. In the present study, 73.6 % of deceased diabetics had suffered from CVD, and about 30 % died directly of CVD, which is higher than India (13.7 %) [29] and Taiwan (19.8 %) [30], and is lower than the western countries (49.4 % for the U.S. and 49.1 % for U.K.) [31]. But this comparison is not totally appropriate because it can be biased by many factors including the difference of coding system among countries, the habits of recording physicians, the subjective judgement of them, and so on [20, 21]. We used continuous data to describe the variation of mortality of CVD, which is more informative than a static observation and helpful to assess the CVD burden. The changing pattern during the 11-year period manifests that the increasing deaths associated with diabetes should chiefly be owed to cardiovascular diseases but have nothing to do with diabetes as the underlying cause, that is, other diabetic complications and diabetes without complications. As shown in Fig. 2, the curve of death rate for people with diabetes and CVD comorbidity shows nearly parallel to the curve of diabetes related mortality. In fact, the mortality for people with comorbidity increases faster than the mortality for all diabetics, that is, the proportion of deceased diabetics with CVD comorbidity increased from 62–82 % during the 11 years. However, the mortality rate for people with other complications varied very slightly; even the proportion of deaths without complications decreased more than three fold in the same period.
Mortality statistics are an important source of health information for analysing the burden of diseases and are often used to assign priorities in health policy [2]. In China, there are two sets of mortality registration systems, the MOH-VR and the DSP. In general, the DSP provides more representative and more accurate data than the MOH-VR, especially in rural areas [22]. Songjiang District is one of the national DSP sites since the last decades, where the non-agricultural population accounted for 46 % in 2003 and 83 % in 2012 (Data from “Statistic Yearbook of Songjiang” 2004 – 2013). Considering that Songjiang locates in the most developed area in China, the number of hospital beds per thousand people was 6.5 in 2003 and 8.0 in 2012, that is, the local health service are quantitatively and qualitatively in the forefront of the country [26], thus the accuracy of the data should be in a higher level comparing with other areas of the country.
In general, estimation of diabetes mortality is challenging due to various reasons. For example, these challenges stem from people with diabetes most frequently dying of cardiovascular diseases or renal failure, and the physicians who record and determine the causes of death may miss and underestimate the contributions of diabetes on death [11–19, 32]. In the present study, the death certification in Songjiang listed up to seven causes contributing to death, of which the underlying causes were determined by certified doctors. We collected all records mentioning diabetes in the certificates to assess contributions of diabetes on death; thus the estimate we calculated could be very similar to a mortality statistic for the people with diabetes.
Although we are confident of the higher quality of data, data from death certificates have potential to distort mortality rates because of the ineluctability of incorrect reporting. One possible explanation for the steep increase in diabetes related deaths could be increased awareness of the disorder. Since the Center for Non-communicable Disease of the Chinese Center for Disease Control and Prevention (China CDC) was established in 2002, surveillance on chronic diseases, such as hypertension and diabetes etc., was gradually highlighted by local CDCs. Therefore, an underestimation of mortality should be taken into account, especially in the earlier stage of the investigation. Furthermore, the International Statistical Classification of Diseases and Related Health Problems (known as ICD) facilitates mortality statistics by standardizing causes of death [33], and also request the capacities of certifying doctors in the correct ICD procedures [34]. But even in developed countries there was often substantial use of ICD codes for unknown and ill-defined causes [33]. Also ill-defined causes (ICD-10 codes R00-R99) existed in our data (230 cases for the contributing causes, but none was in the underlying cause), that would also affect the validity of our estimates. Death certificate is one of the most important sources of data regarding people health, but the data quality is often concerned. There were few studies concerning the accuracy of recorded cause of death of diabetic decedents in China. Therefore, assessment and further improvement of death certificate should become a key emphasis in work of the health care system in the future, which would help us to correctly understand the burden of diabetes on survival [35].
Another limitation relates to the representativeness of local population. Due to China’s household registration system, only permanent residents were recorded by local CDCs. People who lived in Songjiang but were registered in other regions were not included in the present study. Because the majority of these people were young adults who worked in Songjiang, the diabetes related mortalities for the total population would be smaller than the data in the present study. Moreover, though the data of the study cannot represent the characteristics of entire Chinese population, it should be also meaningful and suggestive for policymakers. Since Shanghai is one of the most developed area of China and has a very higher proportion (>20 %) of old people (60 years or older, permanent residents) [36]. This is and will be a similar situation in other areas of China.
The present survey provides only information restricted in deceased diabetics, therefore the results should be explained carefully. For example, although the proportions of those who died from CVD rose rapidly from 2002 to 2012, we cannot attribute the increase of CVD mortality only to the prevalence of diabetes. Because we did not collect mortality data of people who did not have diabetes, we do not know the situation of CVD mortality for them [37]. In contrast, from the changing proportions it could be clearly determined that CVD contributed more and more on diabetes deaths from 2002 to 2012.
Conclusions
There was an increase in diabetes related mortality over the past decade. The increased mortality appears mostly attributed to the prevalence of cardiovascular diseases. Therefore, policy makers should pay more attentions to diabetes primary prevention to reduce the incidence rate while also placing a priority on the prevention of cardiovascular diseases to reduce the burden of diabetes on survival.
Acknowledgements
We would like to thank all the staffs of Songjiang CDC and the certifying physicians for their active collaboration and support.
Funding sources
Georgia State University CITIES internal grant 2012–2014,the World Health Organization Center for Health Development (the WHO Kobe Center), the National Institute of Minority Health and Health Disparities of the National Institutes of Health under award number 1P20MD004806.
Abbreviations
- CVD
Cardiovascular disease
- WHO
World Health Organization
- MOH-VR
Ministry of Health –vital system
- DSP
Disease Surveillance Points System
- CDC
Center for Disease Control and Prevention
- IQR
Interquartile range
- ICD
International Statistical Classification of Diseases
Additional files
Dataset. This Excel dataset was used for all the analysis of the present study. (XLS 602 kb)
The Proportion of diabetes types in the diabetes related deaths from 2002 to 2012. The blocks indicate the proportions of type 2 diabetes, unspecified type, and other specified types (including type 1 diabetes) in each year, respectively. (PDF 154 kb)
Annual number of deaths according to different sub-groups from 2002 to 2012. (PDF 43 kb)
Footnotes
Meiying Zhu and Jiang Li contributed equally to this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MZ constructed the study, and took charge of the data collection, management and interpretation. JL designed the study, and did the data analysis, and interpretation, literature searches, and wrote the first draft of the report. DD constructed the study, and contribute to study design. ZL, WL gathered, interpreted, and analysed the data, SRW, CS and RL contributed to study design, writing of the draft and review and critique of the manuscript. All authors have fulfilled authorship criteria per ICMJE guidelines and have approved the manuscript and this submission. JL is guarantor for the study, had full access to the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011. 1980;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. [Google Scholar]
- 3.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 4.He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–34. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 5.Cheng TO. Diabetes epidemic in China and its economic impact. International journal of cardiology. 2011;149(1):1–3. doi: 10.1016/j.ijcard.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 7.Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care 1997. 1994;20(11):1664–9. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 8.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control: World Health Organization; 2011.
- 9.Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S14–21. doi: 10.1007/PL00002934. [DOI] [PubMed] [Google Scholar]
- 10.Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64) Kidney international. 2003;63(1):225–32. doi: 10.1046/j.1523-1755.2003.00712.x. [DOI] [PubMed] [Google Scholar]
- 11.McEwen LN, Pomeroy NE, Onyemere K, Herman WH. Are primary care physicians more likely to record diabetes on death certificates? Diabetes Care. 2008;31(3):508–10. doi: 10.2337/dc07-1994. [DOI] [PubMed] [Google Scholar]
- 12.McEwen LN, Kim C, Haan M, Ghosh D, Lantz PM, Mangione CM, et al. Diabetes reporting as a cause of death: results from the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2006;29(2):247–53. doi: 10.2337/diacare.29.02.06.dc05-0998. [DOI] [PubMed] [Google Scholar]
- 13.Evans JM, Barnett KN, McMurdo ME, Morris AD. Reporting of diabetes on death certificates of 1872 people with type 2 diabetes in Tayside, Scotland. European journal of public health. 2008;18(2):201–3. doi: 10.1093/eurpub/ckm113. [DOI] [PubMed] [Google Scholar]
- 14.Will JC, Vinicor F, Stevenson J. Recording of diabetes on death certificates. Has it improved? Journal of clinical epidemiology. 2001;54(3):239–44. doi: 10.1016/S0895-4356(00)00303-6. [DOI] [PubMed] [Google Scholar]
- 15.Thomason MJ, Biddulph JP, Cull CA, Holman RR. Reporting of diabetes on death certificates using data from the UK Prospective Diabetes Study. Diabet Med. 2005;22(8):1031–6. doi: 10.1111/j.1464-5491.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- 16.Cheng WS, Wingard DL, Kritz-Silverstein D, Barrett-Connor E. Sensitivity and specificity of death certificates for diabetes: as good as it gets? Diabetes Care. 2008;31(2):279–84. doi: 10.2337/dc07-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McEwen LN, Karter AJ, Curb JD, Marrero DG, Crosson JC, Herman WH. Temporal trends in recording of diabetes on death certificates: results from Translating Research Into Action for Diabetes (TRIAD) Diabetes Care. 2011;34(7):1529–33. doi: 10.2337/dc10-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saydah SH, Geiss LS, Tierney E, Benjamin SM, Engelgau M, Brancati F. Review of the performance of methods to identify diabetes cases among vital statistics, administrative, and survey data. Annals of epidemiology. 2004;14(7):507–16. doi: 10.1016/j.annepidem.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Roglic G, Unwin N. Mortality attributable to diabetes: estimates for the year 2010. Diabetes Res Clin Pract. 2010;87(1):15–9. doi: 10.1016/j.diabres.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Lu TH, Kwok CF, Ho LT. Whether to report diabetes as the underlying cause-of-death? a survey of internists of different sub-specialties. BMC endocrine disorders. 2010;10:13. doi: 10.1186/1472-6823-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu TH, Walker S, Johansson LA, Huang CN. An international comparison study indicated physicians’ habits in reporting diabetes in part I of death certificate affected reported national diabetes mortality. Journal of clinical epidemiology. 2005;58(11):1150–7. doi: 10.1016/j.jclinepi.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: history, current situation and challenges. Population health metrics. 2005;3(1):3. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dai Z, Zheng X, Qi X, Yang G. Guidebook on disease surveillance. Beijing: Hua Xia Press; 1993. [Google Scholar]
- 24.Preston SH. The changing relation between mortality and level of economic development. Population studies. 1975;29(2):231–48. doi: 10.1080/00324728.1975.10410201. [DOI] [PubMed] [Google Scholar]
- 25.Seale C. Changing patterns of death and dying. Soc Sci Med. 2000;51(6):917–30. doi: 10.1016/S0277-9536(00)00071-X. [DOI] [PubMed] [Google Scholar]
- 26.Zhongguo weisheng tongji nianjian . China health statistical yearbook. Beijing: China NHaFPCotPsRo; 2013. [Google Scholar]
- 27.Gu D, Reynolds K, Duan X, Xin X, Chen J, Wu X, et al. Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA) Diabetologia. 2003;46(9):1190–8. doi: 10.1007/s00125-003-1167-8. [DOI] [PubMed] [Google Scholar]
- 28.Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. Jama. 2013;310(9):948–59. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 29.Zargar AH, Wani AI, Masoodi SR, Bashir MI, Laway BA, Gupta VK, et al. Causes of mortality in diabetes mellitus: data from a tertiary teaching hospital in India. Postgraduate medical journal. 2009;85(1003):227–32. doi: 10.1136/pgmj.2008.067975. [DOI] [PubMed] [Google Scholar]
- 30.Tseng CH. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care. 2004;27(7):1605–9. doi: 10.2337/diacare.27.7.1605. [DOI] [PubMed] [Google Scholar]
- 31.Lu TH, Hsu PY, Anderson RN, Huang CN. Mortality and causes of death in a national sample of diabetic patients in Taiwan: response to Tseng. Diabetes Care. 2005;28(5):1266–7. doi: 10.2337/diacare.28.5.1266-a. [DOI] [PubMed] [Google Scholar]
- 32.Chen F, Florkowski CM, Dever M, Beaven DW. Death Certification and New Zealand Health Information Service (NZHIS) statistics for diabetes mellitus: an under-recognised health problem. Diabetes Res Clin Pract. 2004;63(2):113–8. doi: 10.1016/j.diabres.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bulletin of the World Health Organization. 2005;83(3):171–7. [PMC free article] [PubMed] [Google Scholar]
- 34.Stausberg J, Lehmann N, Kaczmarek D, Stein M. Reliability of diagnoses coding with ICD-10. International journal of medical informatics. 2008;77(1):50–7. doi: 10.1016/j.ijmedinf.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 35.Lu TH, Hsu PY, Bjorkenstam C, Anderson RN. Certifying diabetes-related cause-of-death: a comparison of inappropriate certification statements in Sweden. Taiwan and the USA. Diabetologia. 2006;49(12):2878–81. doi: 10.1007/s00125-006-0470-6. [DOI] [PubMed] [Google Scholar]
- 36.Sixth National Population Census Office of State Council . Major figures on population census of China. Beijing: China Statistics Press; 2011. [Google Scholar]
- 37.Paula AA, Schechter M, Tuboi SH, Faulhaber JC, Luz PM, Veloso VG, et al. Continuous increase of cardiovascular diseases, diabetes, and non-HIV related cancers as causes of death in HIV-infected individuals in Brazil: an analysis of nationwide data. PloS one. 2014;9(4) doi: 10.1371/journal.pone.0094636. [DOI] [PMC free article] [PubMed] [Google Scholar]


