Abstract
Context:
Functional reach on the Star Excursion Balance Test is decreased in participants with chronic ankle instability (CAI). However, comprehensive 3-dimensional kinematics associated with these deficits have not been reported.
Objective:
To determine if lower extremity kinematics differed in CAI participants during anteromedial, medial, and posteromedial reach on the Star Excursion Balance Test.
Design:
Case-control study.
Setting:
Sports medicine research laboratory.
Patients or Other Participants:
Twenty CAI participants (age = 24.15 ± 3.84 years, height = 168.95 ± 11.57 cm, mass = 68.95 ± 16.29 kg) and 20 uninjured participants (age = 25.65 ± 5.58 years, height = 170.14 ± 8.75 cm, mass = 69.89 ± 10.51 kg) with no history of ankle sprain. We operationally defined CAI as repeated episodes of ankle “giving way” or “rolling over” or both, regardless of neuromuscular deficits or pathologic laxity. All CAI participants scored ≤26 on the Cumberland Ankle Instability Tool.
Intervention(s):
Star Excursion Balance Test reaches in the anteromedial, medial, and posteromedial directions. The CAI participants used the unstable side as the stance leg. Control participants were sex, height, mass, and side matched to the CAI group. The 3-dimensional kinematics were assessed with a motion-capture system.
Main Outcome Measure(s):
Group differences on normalized reach distance, trunk, pelvis, and hip-, knee-, and ankle-joint angles at maximum Star Excursion Balance Test reach.
Results:
No reach-distance differences were detected between CAI and uninjured participants in any of the 3 reach directions. With anteromedial reach, trunk rotation (t1,38 = 3.06, P = .004), pelvic rotation (t1,38 = 3.17, P = .003), and hip flexion (t1,38 = 2.40, P = .002) were greater in CAI participants. With medial reach, trunk flexion (t1,38 = 6.39, P = .05) was greater than for uninjured participants. No differences were seen with posteromedial reach.
Conclusions:
We did not detect reach-distance differences in any direction. However, participants with CAI rotated the trunk and pelvis more toward the stance leg than did stable-ankle participants during anteromedial and medial reach, possibly to help maintain a proximal stable posture and compensate for distal instability. These joint-angle differences with Star Excursion Balance Test performance may represent unique compensatory patterns for those with CAI.
Key Words: ankle injuries, dynamic balance, dynamic postural control
Key Points
Movement-pattern differences at the trunk and hip were present in those with chronic ankle instability for selected directions of the Star Excursion Balance Test.
Altered movement strategies may contribute to the long-lasting sequelae of chronic ankle instability after ankle sprain.
Chronic ankle instability (CAI) is a frustrating and potentially debilitating condition. Up to 30% of those who sustain a single ankle sprain will go on to develop CAI, which may include chronic pain, feelings of “giving way,” and diminished self-reported function in their daily lives.1 Those with CAI exhibit balance deficits in many tasks, and a recent meta-analysis showed that foot center-of-pressure measures, balance errors, time to stabilization, and the Star Excursion Balance Test (SEBT) were all sensitive to these balance deficits.2 Although static-balance tests can detect impairments in those with CAI, dynamic-balance tasks may better represent lower extremity function during activity.3 The SEBT is a valid and reliable dynamic-balance test that accurately quantifies lower extremity functional performance and has been reported to detect functional deficits associated with CAI.4–8 Stability limits are challenged as participants perform a maximal reach task with 1 foot in a prescribed direction while maintaining single-legged balance on the other leg.3 Functional performance is quantified as the maximal normalized reach distance in each direction, with greater distances equaling better functional performance.
Dynamic balance can be characterized as maintaining one's center of mass within the base of support during a movement task. Such tasks require simultaneous stabilizing movements from the entire lower extremity throughout the exercise. In healthy participants, Robinson and Gribble9 determined that hip and knee flexion accounted for most of the reach-distance variance in all 8 directions of the SEBT. Gribble et al4,5 found that CAI participants, in addition to demonstrating decreased reach in the selected directions of the SEBT, also displayed altered hip and knee flexion under normal and fatigued conditions compared with uninjured participants. Although a large amount of lower extremity motion has been demonstrated in the sagittal plane with CAI, trunk and lower extremity kinematics have not been investigated during SEBT performance except with fatiguing conditions.4,5 Transverse- and frontal-plane motions in CAI participants have yet to be examined.
Based on factor analyses of all 8 reach directions of the original SEBT, Hertel et al10 supported the use of the anteromedial (AM), medial (M), and posteromedial (PM) reach directions for CAI detection, with the PM reach direction being the most representative. However, theirs was not a hypothesis-driven study, and they recommended a priori testing. Therefore, the purpose of our research study was to (1) identify reach-distance differences in the AM, M, and PM directions of the SEBT in CAI participants in a hypothesis-driven manner and (2) detect particular reach-strategy differences in the frontal, sagittal, and transverse planes of the trunk, pelvis, and lower extremity in CAI participants during maximal reach of the SEBT. We hypothesized that CAI participants would demonstrate decreased reach-distance differences and altered kinematic movement strategies during the A, M, and PM directions of the SEBT compared with uninjured participants. Understanding full lower extremity and spinal kinematic differences may allow us to better identify abnormal movement patterns that should be addressed in rehabilitation programs for CAI.
METHODS
Participants
We recruited 20 participants with CAI and 20 uninjured participants with no history of ankle injury. Uninjured participants were sex, height, weight, and side matched to the CAI group. All participants completed a medical history questionnaire that asked about a previous history of lower extremity injuries and the incidence of ankle giving way. Chronic ankle instability was operationally defined as repeated (more than 2) episodes of ankle giving way, ankle “rolling over,” or both, regardless of the existence of neuromuscular deficits or pathologic laxity.3 To determine CAI group eligibility, participants had to have a history of at least 1 significant ankle sprain (but not in the past 30 days) and multiple reported episodes of giving way within the past month. The inclusion criteria were being physically active (defined as a minimum of 3 hours per week of activity that required energy expenditure by skeletal muscles), having no history of lower extremity surgery, being free of any lower extremity injuries within the past month, and being free of cerebral concussion, vestibular disorder, upper respiratory infection, and ear infection at the time of study.
Additionally, all participants recorded answers on 2 ankle-instability questionnaires: (1) the Cumberland Ankle Instability Tool (CAIT),11 used to rate instability; and (2) the Foot and Ankle Disability Index–Sport (FADI–Sport),12 used to quantify disability resulting from CAI. The CAI participants averaged 18.84 ± 5.65 out of a possible 30 points on the CAIT and 89.97 ± 12.39 out of a possible 100 on the FADI–Sport. Control participants averaged 29.05 ± 1.43 points on the CAIT and 99.03 ± 2.59 on the FADI–Sport (Table 1). This study was approved by the institutional review board at Virginia Commonwealth University, and all participants read and signed an informed consent form before data collection.
Table 1.
Descriptive Statistics for Study Participants
| Group |
Sex |
Mean ± SD |
||||
| Age, y |
Height, cm |
Mass, kg |
Cumberland Ankle Instability Tool Score |
Foot and Ankle Disability Index–Sport Score, % |
||
| Uninjured | Men (n = 7) | 24.57 ± 5.56 | 178.96 ± 6.51 | 78.29 ± 6.10 | 29.14 ± 1.57 | 97 ± 6.66 |
| Women (n = 13) | 26.23 ± 5.73 | 165.39 ± 5.50 | 65.37 ± 9.64 | 29.00 ± 1.41 | 99.28 ± 2.60 | |
| Total (n = 20) | 25.65 ± 5.58 | 170.14 ± 8.75 | 69.89 ± 10.51 | 29.05 ± 1.43a | 99.03 ± 2.59a | |
| Chronic ankle instability | Men (n = 7) | 24.00 ± 5.48 | 180.63 ± 9.75 | 87.14 ± 11.48 | 21.50 ± 6.47 | 89.06 ± 13.66 |
| Women (n = 13) | 24.23 ± 2.89 | 162.66 ± 6.48 | 59.15 ± 7.58 | 17.62 ± 5.03 | 90.39 ± 12.33 | |
| Total (n = 20) | 24.15 ± 3.84 | 168.95 ± 11.57 | 68.95 ± 16.29 | 18.84 ± 5.65a | 89.97 ± 12.39a | |
Indicates significance at the .05 level.
Instrumentation and Data Processing
A 3-dimensional optical motion-capture system (Vicon Motion Systems, Centennial, CO) with accompanying force plates (Bertec Corporation, Columbus, OH) and software (Nexus version 1.3.109; Vicon Motion Systems) were used for data collection. Data were processed and filtered with Plug-in Gait modeling through the Vicon Nexus software, which uses a predefined marker set and participant measurements to create kinematic and kinetic outputs. Missing marker data (gaps) were spline filled on a frame-by-frame basis. Trunk, pelvis, and lower extremity kinematics at maximal reach were determined as described in the upcoming text.
Procedures
We tested participants in the AM, M, and PM directions of the SEBT relative to the stance leg. These 3 directions are sensitive in detecting functional performance differences in CAI participants.10 Reach lines were marked on the testing surface at 45° angles and intersected in the center. Similar to several previously published studies, the center of each participant's foot was placed over the intersection of the grid, which denoted the starting position for reach in all directions.4,5,7,10,13 Before testing began, participants drew a precounterbalanced card to determine the order of SEBT reach directions. For uninjured participants, the predetermined order of the testing leg was also included in the counterbalancing.
Participant Setup
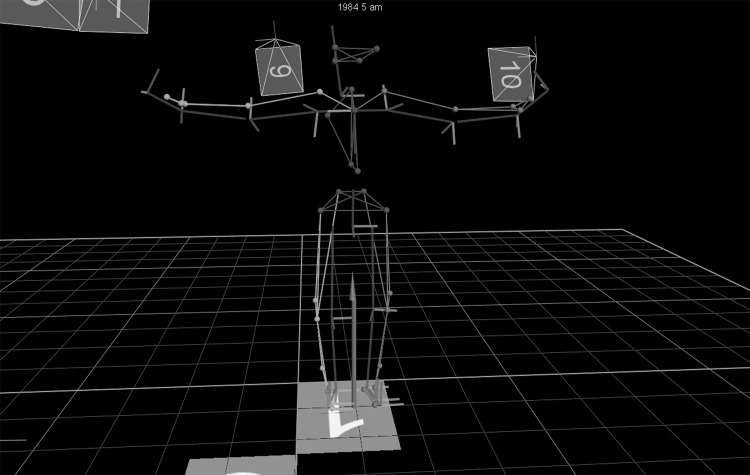
We measured participants' height (centimeters), mass (kilograms), ankle width, anterior-superior iliac spine (ASIS)–trochanter distance, knee width, inter-ASIS distance, leg length, elbow width, hand thickness, shoulder offset (vertical distance from the center of the glenohumeral joint to the acromioclavicular joint), and wrist width, which were required for running the Plug-in Gait modeling specifications. To normalize SEBT reach distance for each participant, we measured anatomical leg length (in centimeters) in the supine position from the ASIS distally to the distal tip of the medial malleolus. Thirty-five retroreflective markers were attached to the participant at predefined locations from the head to the heel. A static trial was collected with the participant in a T pose and markers manually labeled in the software. The reconstructed participant model was verified by the examiner and ensured that the participant's movement was accurately mimicked in the computer model before testing began (Figure).
Figure.
Motion-capture set-up.
Reach Performance
The examiner orally described and visually demonstrated the testing procedure before participants performed 6 practice trials in each of the 3 testing directions to become familiar with the task.7 Participants reached out along the test direction as far as possible, lightly touched the line with the most distal part of the reach foot, and returned to bilateral stance at the start position, keeping both hands on the hips at all times. For testing, reach distance was visually verified and recorded in centimeters by the principal investigator (S.dlM.) from the center of the grid along the appropriate reach vector for each reach direction. Trials were discarded and repeated if the participant (1) lost his or her balance at any point during the trial, (2) did not touch the foot down on the reach line, (3) lifted either hand off the hips, (4) lifted any part of the stance foot off the floor, or (5) placed a significant amount of weight on the reach foot so as to support the body by widening the base of support. Participants performed reach testing as instructed by the examiner, completing 6 good reach trials in each direction in the predetermined counterbalanced order. A brief rest was allowed after each reach, and participants performed the task at a self-selected pace. Uninjured participants performed testing once each on the right and left legs in a counterbalanced fashion to ensure accurate side matching with CAI participants. A significant rest period was given to uninjured participants before testing of the second leg. For CAI participants who reported more than 1 ankle with CAI, the more subjectively unstable side was tested.
Reach Kinematics
After all data had been processed through Plug-in Gait modeling software, we determined maximal reach kinematics in the Vicon computer system by visually verifying the frame at which the reach-foot marker was furthest away from the body and recorded its most negative value on the z-axis trajectory. An event marker was placed at the frame of maximum reach for each trial, signifying the spatiotemporal point of maximum reach. From this frame, frontal-, sagittal-, and transverse-plane kinematics for the trunk, pelvis, and hip-, knee-, and ankle-joint angles of the stance-leg side were extracted. All joint angles for each reach were averaged using a customized MATLAB program (The MathWorks, Inc, Natick, MA).
According to Plug-in Gait conventions, we calculated output angles for all joints from the YXZ Cardan angles derived by comparing the relative orientations of the 2 adjoining segments. The trunk was modeled as a rigid segment (running from the seventh cervical vertebra to the fifth lumbar vertebra) whose angles illustrated motion between the rigid trunk and pelvis, with the pelvis being acted upon. For the pelvis, the coordinate system was reconstructed from the surface markers on the ASIS and posterior-superior iliac spine landmarks, with pelvic tilt calculated about the laboratory's transverse axis. Finally, hip-joint centers were calculated using the Newington-Gage model,14 and hip angles represent the motion between the thigh and pelvis. For all kinematic variables, 0° represents the neutral upright anatomical position of the stance-leg side, which was collected during the static pose. For all planes, positive values indicate segmental movement of the stance-leg side toward the reach leg, and negative values indicate stance-leg–side segmental movement away from the reach leg.
Statistical Methods
For statistical analyses, we used means for reach distance and trunk, pelvis, hip, knee, and lower extremity kinematics in the 3 reach directions. Separate independent t tests for each reach direction were calculated to investigate group effects (CAI, uninjured) on normalized reach distance and on the 3-dimensional kinematics of the trunk, pelvis, hip, knee, and ankle values at SEBT maximal reach. Statistical significance was set a priori at .05.
RESULTS
Independent t tests indicated no group differences in age (t1,38 = 0.50, P = .33), height (t1,38 = 0.07, P = .72), or mass (t1,38 = 0.02, P = .83). Differences were seen between groups for both the CAIT (t1,38 = 30.62, P < .001) and FADI–Sport (t1,38 = 4.17, P = .002; Table 1) scores.
Reach Distance
We noted no statistical differences between groups in any of the 3 reach directions (AM t1,38 = 0.44, P = .66; M t1,38 = 0.94, P = .35; PM t1,38 = 0.76, P = .45; Table 2).
Table 2.
Normalized Reach Distances on Selected Directions of the Star Excursion Balance Test, %
| Normalized Reach Distance, Mean ± SD |
|||
| Group |
Anteromedial |
Medial |
Posteromedial |
| Uninjured | 73.16 ± 6.49 | 75.20 ± 8.92 | 77.48 ± 11.74 |
| Chronic ankle instability | 74.37 ± 6.32 | 77.94 ± 8.35 | 80.13 ± 10.34 |
Reach Kinematics
The means, standard deviations, significance values, and Cohen d effect sizes for reach kinematics are provided in Tables 3 and 4.
Table 3.
Spine and Pelvis Reach Kinematicsa Extended on Next Page
| Reach Direction |
Group |
Spinal Flexion |
Lateral Spinal Flexion |
Spinal Rotation |
||||||
| Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
||
| Anteromedial | Uninjured | −4.50 ± 8.50 | .15 | −0.23 | −15.18 ± 6.53 | .69 | −0.06 | −3.76 ± 10.25 | .004b | −0.44 |
| Chronic ankle instability | 0.54 ± 12.52 | −13.90 ± 12.55 | −30.35 ± 37.43 | |||||||
| Medial | Uninjured | 14.82 ± 9.15 | .05b | −0.30 | −20.69 ± 10.48 | .68 | 0.07 | −5.84 ± 18.90 | .97 | −0.01 |
| Chronic ankle instability | 21.61 ± 11.92 | −22.05 ± 9.42 | −6.03 ± 14.79 | |||||||
| Posteromedial | Uninjured | 28.60 ± 13.83 | .88 | 0.02 | −11.18 ± 8.15 | .31 | 0.16 | 2.70 ± 25.19 | .47 | 0.11 |
| Chronic ankle instability | 27.66 ± 22.65 | −14.70 ± 13.05 | −4.92 ± 39.22 | |||||||
For all variables, 0° represents the upright anatomical position during the static pose. Positive values represent segmental movement toward the reach leg, and negative values represent segmental movement away from the reach leg.
Indicates significance at the .05 level.
Table 4.
Hip, Knee, Ankle Reach Kinematicsa Extended on Next Page
| Direction |
Group |
Hip Flexion |
Hip Abduction |
Hip Rotation |
||||||
| Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
||
| Anteromedial | Uninjured | 23.36 ± 14.65 | .02b | −0.35 | 3.69 ± 7.41 | .12 | −0.27 | 31.53 ± 12.64 | .26 | 0.61 |
| Chronic ankle instability | 36.31 ± 19.23 | 7.08 ± 6.03 | 35.93 ± 11.90 | |||||||
| Medial | Uninjured | 50.28 ± 18.08 | .23 | −0.19 | −2.21 ± 6.10 | .18 | −0.21 | 29.14 ± 14.64 | .57 | −0.09 |
| Chronic ankle instability | 57.79 ± 20.81 | 0.63 ± 6.99 | 31.82 ± 14.72 | |||||||
| Posteromedial | Uninjured | 66.23 ± 17.32 | .58 | 0.43 | −4.72 ± 8.14 | .17 | −0.22 | 20.27 ± 14.40 | .88 | −0.05 |
| Chronic ankle instability | 69.81 ± 22.67 | −1.13 ± 8.05 | 20.99 ± 15.31 | |||||||
For all variables, 0° represents the upright anatomical position during the static pose. Positive values represent segmental movement toward the reach leg, and negative values represent segmental movement away from the reach leg.
Indicates significance at the .05 level.
Table 3.
Extended From Previous Page
| Anterior Pelvic Tilt |
Superior Pelvic Tilt |
Pelvic Rotation |
||||||
| Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
| 5.50 ± 8.95 | .35 | −0.15 | −4.56 ± 5.32 | .48 | 0.11 | 2.84 ± 9.66 | .003b | 0.45 |
| 8.76 ± 12.64 | −6.15 ± 8.31 | −23.96 ± 36.58b | ||||||
| 21.28 ± 11.70 | .28 | −0.17 | −11.04 ± 5.88 | .86 | 0.03 | 1.57 ± 18.75 | .88 | 0.03 |
| 25.25 ± 11.10 | −11.40 ± 6.80 | 0.74 ± 13.88 | ||||||
| 33.16 ± 13.80 | .66 | 0.07 | −3.15 ± 7.28 | .36 | 0.14 | 6.41 ± 24.27 | .62 | 0.08 |
| 31.05 ± 16.37 | −6.43 ± 14.28 | 1.61 ± 35.74 | ||||||
Table 4.
Extended From Previous Page
| Knee Flexion |
Knee Valgus |
Knee Rotation |
||||||
| Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
| 50.11 ± 13.85 | .08 | −0.28 | 24.45 ± 11.45 | .80 | 0.04 | −8.52 ± 15.73 | .68 | 0.07 |
| 58.34 ± 14.63 | 23.51 ± 11.69 | −10.51 ± 14.68 | ||||||
| 61.07 ± 16.18 | .58 | −0.09 | 19.29 ± 12.37 | .89 | −0.02 | −2.31 ± 17.09 | .27 | 0.17 |
| 63.65 ± 13.05 | 19.84 ± 11.49 | −8.17 ± 16.16 | ||||||
| 57.93 ± 16.99 | .76 | 0.05 | 19.67 ± 12.68 | .59 | 0.09 | −2.68 ± 17.40 | .23 | 0.19 |
| 59.42 ± 13.73 | 21.86 ± 12.85 | −9.12 ± 15.67 | ||||||
Table 4.
Extended From Previous Page
| Ankle Inversion |
Ankle Internal Rotation |
Ankle Dorsiflexion |
||||||
| Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
Mean ± SD, ° |
P Value |
Effect Size |
| 5.89 ± 4.75 | .41 | 0.13 | −20.60 ± 14.02 | .20 | −0.20 | 41.00 ± 8.48 | .37 | 0.14 |
| 4.66 ± 4.55 | −14.73 ± 14.57 | 33.82 ± 34.30 | ||||||
| 5.80 ± 5.02 | .19 | 0.21 | −20.23 ± 13.89 | .08 | −0.27 | 40.18 ± 7.99 | .24 | 0.19 |
| 3.77 ± 4.60 | −12.10 ± 15.00 | 30.96 ± 33.53 | ||||||
| 6.01 ± 5.36 | .14 | 0.23 | −20.54 ± 14.63 | .07 | −0.29 | 34.60 ± 8.00 | .29 | 0.17 |
| 3.45 ± 5.40 | −11.13 ± 16.92 | 26.68 ± 32.29 | ||||||
Anteromedial Reach
Rotation of the trunk away from the reaching leg (in a backward twisting motion) was greater in CAI participants (group mean difference = 26.59, 95% confidence interval [CI] = 9.02, 44.16, P = .004; Table 3). More external pelvic rotation of the stance side (that is, the reach-side pelvis was in front) was observed with CAI (group mean difference = 26.80, 95% CI = 9.67, 43.92, P = .003). Hip flexion was greater in CAI participants (group mean difference = −12.95, 95% CI = −23.90, −2.01, P = .02; Table 4). We detected no other differences.
Medial Reach
Trunk flexion (defined as the forward tilt toward the pelvis) was greater in CAI participants in the M reach direction (21.61° versus 14.82°, P = .05), although the 95% CI for group mean difference crosses 0 (group mean difference = −6.79, 95% CI = −13.59, 0.01; Table 3). No other differences were seen for this direction.
Posteromedial Reach
We found no differences in trunk, pelvis, or lower extremity motion in this direction.
DISCUSSION
Although functional reach differences on the SEBT have been reported in participants with CAI, to our knowledge, no authors have examined the AM, M, and PM reach distances and joint angles in a 3-dimensional, whole-body manner. We undertook a thorough multiplanar examination of trunk and lower extremity joint angles at maximum reach distance on the SEBT in an attempt to characterize multiplanar movement strategy during a dynamic postural-stability task in those with CAI. Although we did not find any reach-distance differences, our results show distinct joint-angle differences between uninjured and CAI participants at the point of maximal reach, which may represent unique movements that reflect compensatory strategies associated with CAI.
Reach Distance
We did not detect any reach-distance differences between CAI participants and healthy individuals. Our finding mirrors that of Sefton et al,15 who also reported no reach differences in CAI participants in the AM, M, or PM reach directions. Reach-distance differences in these 3 directions had not been tested in a hypothesis-driven manner before our study, and it is possible that these directions may not be the most sensitive to CAI-related performance deficits. Several authors3–5,10 noted decreased functional reach deficits in CAI participants on the SEBT in multiple directions. Methodologic, statistical, and participant-selection variations may explain the different findings. Olmsted et al3 pooled reach distances from injured and contralateral limbs of CAI participants for 8 reach directions, creating an overall reach variable. More importantly, they did not normalize to leg length or height, as is recommended to account for leg-length differences (and hence potential reach differences) among participants.16 Gribble et al5 observed that CAI participants had decreased maximum reach distance (MAXD) in the M and posterior directions compared with their uninjured side. However, CAI participants had decreased MAXD versus the healthy group only for posterior reach. Conversely, in the anterior direction, CAI participants had greater MAXD than the healthy group. These findings should be viewed with caution, as statistical analyses showed significant interactions only with a repeated-measures analysis of variance with lower extremity fatiguing conditions as a within-subject factor.
Several methodologic differences may also account for variations in reach-distance results among studies. First, we had participants perform 6 reach trials in each direction in an attempt to achieve a more stable measurement of reach performance. Although most authors have included only 3 reach trials per direction, this recommendation is based on studies of healthy participants.8,17 We noted that even given the confines of “good” trials, reach distance varied greatly from 1 trial to another in both healthy and unstable participants. We chose to increase the number of trials to stabilize the measure.
Second, we required participants to keep their hands on their hips for each reach. Hand placement has varied across studies. Participants in the Hertel et al10 study were not required to keep their hands on their hips during performance but could move their arms freely. Placing the hands on the hips prevents the hands from aiding in balance, creating a more challenging task for the lower extremity and core, and was recently endorsed by the authors of a systematic review6 as a way to standardize movements outside the trunk and lower limbs.
Movement-Pattern Differences
Despite the absence of reach-distance differences, we did observe movement-pattern differences between CAI and healthy participants. Biomechanical measurement of the lower extremity kinetic chain during dynamic-balance activities has been limited to hip, knee, and ankle sagittal-plane kinematics and, to our knowledge, has not included contributions from the trunk and pelvis. Although dynamic balance requires simultaneous stabilizing movements from the entire lower extremity, the primary goal is to maintain the center of mass within the base of support. We found that CAI participants used a proximal balance strategy, manipulating the trunk, pelvis, and hip differently than healthy participants to achieve maximal reach during the SEBT reach in the AM and M directions. No differences between CAI and healthy participants were observed for the PM reach direction.
For AM reach, CAI participants rotated the trunk and pelvis posteriorly, away from the reach leg and toward the stance leg, in an almost leaning-back manner, to maintain the center of mass within the base of support. In addition to this proximal rotation, CAI participants had more hip flexion with AM reach. The combined proximal rotation and increased hip flexion appear to have enabled CAI participants to extend the reach foot to touch just as far along the AM vector as uninjured participants and still maintain balance. Although this result did not achieve significance for the M reach direction, those with CAI did display increased trunk flexion, bringing the trunk forward for maximum reach. Overall, it appears CAI participants attempted to maintain the center of gravity over the foot or as near as possible at the most unstable point—at maximum reach.
Various movement strategies during dynamic tasks have been reported. Previous authors18,19 have demonstrated altered kinematic patterns in participants with unstable ankles during more dynamic jump-landing tasks. Caulfield and Garrett19 theorized that these differences could indicate a learned adaptive strategy as a result of previous injury and may be reflected in other tasks in which CAI dysfunction is exhibited. Such learned strategies could help explain our findings in the AM and M directions. The SEBT is a closed chain exercise that allows participants to perform reaches in a self-selected manner at a self-selected pace. Thus, it is possible that our participants used a compensatory learned adaptive motor-control strategy, demonstrating kinematic alterations proximally at the trunk, pelvis, and hip—the joints closest to the base of support—during SEBT performance.
Decreased hip strength has been demonstrated in those with CAI. Several authors noted slower gluteus medius activity,20,21 less hip-flexor eccentric torque production,22 and gluteus maximus weakness during closed chain rotational exercises in participants with CAI.23 Although we did not specifically investigate it in our study, hip strength may have played a role in these kinematic changes observed at maximum reach. It is also feasible that the trunk and hip differences were related to disrupted afferent information at the unstable ankle. Such proximal movements may serve as a protective mechanism to safeguard against any undulations of the unstable ankle or as compensation for decreased degrees of freedom during reach.24,25
Alternatively, such movement strategies could be preexisting and actually contribute to ankle sprain and CAI risk. Performance in the anterior, PM, and posterolateral directions of the SEBT has prospectively identified an increased risk of ankle sprain in high school basketball players.26 Players who had side-to-side deficits or reach distances that were less than 94% of their limb length were up to 2.5 times more likely to sustain a lower extremity injury during a season. Although neither movement strategy nor a thorough injury history were documented in the Plisky et al26 study, these results are remarkable. Taken together with our findings, it is apparent that movement-pattern deficits are present before and after injury and may contribute to an individual's future injury risk. Prospective cohort studies specifically targeting preexisting movement deficits and ankle-injury outcomes should be conducted, with the goal of understanding movement and injury risk to provide further guidance for developing effective prevention strategies.
Lastly, contrary to Gribble et al,4,5 who reported sagittal-plane kinematic changes in CAI participants with SEBT M reach, we did not find any knee, ankle, or reach-distance differences in this direction. Possible explanations for this could be related to our use of an average of 6 reach attempts to stabilize the measures. Also, baseline group mean differences between healthy and CAI participants before fatigue were not reported,4 and direct comparisons between study results cannot be drawn. Methodologic differences in kinematic data capture and processing could have also been a factor. We used a 3-dimensional optical motion-capture system with 35 retroreflective markers and Plug-in Gait software to calculate joint kinematics, whereas Gribble used a digital video camera and the markerless SMART system (MGI Software Corp, Richmond Hill, ON, Canada). The agreement between these 2 systems has not been evaluated and may have influenced angle measurements.
Chronic Ankle Instability and Participant Selection
Participant-selection methods for CAI studies have not been consistent. Even though all researchers have reported criteria to classify participants, different levels of dysfunction and disability due to CAI and various scoring ranges of healthy participants may have led to inconsistent results across studies. The Internal Ankle Consortium (IAC) released a position statement in August 2013, recommending standardized selection criteria for CAI participants.27 Our participants met most of the group's recommended inclusion criteria and all of the recommended exclusion criteria, but our study was conducted before the position statement was published. Because of this timing, we feel justified in our use of instruments to assess self-reported function (CAIT and FADI–Sport), but we did not require participants to attain a specific score for inclusion in either the CAI or uninjured group. Furthermore, our results highlight the continued difficulty of participant-selection criteria despite these best practice recommendations.
The CAIT was administered to all participants and used to classify CAI disability in our study. The CAIT is an objective pencil-and-paper tool that quantifies pain and instability during common daily activities and athletic maneuvers and is scored on a scale of 32 points. As established by Hiller et al11 in high-level dancers, a score of 27 or below indicates the presence of CAI, but this cutoff may not represent ankle dysfunction in other active populations. The IAC recommendation places this cutoff at 24, yet this value was not empirically determined. Though CAIT scores were different between the injured and uninjured groups in our study, CAIT scores of the CAI group ranged from 10 to 27 and reach distances may have been affected by various levels of ankle-related dysfunction.
We also used a second measure, the FADI–Sport, which asks participants to rate difficulty with particular sport-related activities due to their ankle. The FADI–Sport has often been used in previous literature either to classify disability or as an inclusion criterion.4,5,12,15,23,28 For our CAI group, the mean FADI–Sport was 89.97% ± 12.39%, slightly higher than in some published reports but similar to Hale and Hertel's12 study (89.6% ± 9.1%), establishing the reliability and sensitivity of the FADI–Sport in CAI participants. Additionally, all CAI participants in our study reported 1 of the strongest defining characteristics of CAI: a recurrent sense of giving way that occurred multiple times per month.27 Although the FADI–Sport has been established as sensitive and reliable for CAI, it should be noted that several participants in our study had CAIT scores as low as 12 but reported 100% function on the FADI–Sport, highlighting the difficulty in accurately classifying disability related to CAI. Newer measures such as the Identification of Functional Ankle Instability29 and the Foot and Ankle Ability Measure30 show promise in appropriately classifying participants and should continue to be investigated.
Finally, difficulty also exists in determining acceptable ranges for healthy, uninjured participants. Despite no history of ankle sprain or reported ankle problems, our healthy group reported less-than-perfect ankle ability on the FADI–Sport (99.03% ± 2.59%), but this is not unusual. We found only 1 study31 whose authors reported 100% ± 0.0% scores in their healthy group; others have reported similar less-than-perfect scores.15,23 Unfortunately, some investigators did not report raw group means4,28 or listed FADI–Sport scores only for CAI participants.32 In addition to adhering to the IAC participant-selection recommendations, future researchers should perform advanced statistical analyses, including receiving operating characteristic analyses, to determine optimal cutoffs for screening test scores for both uninjured and CAI groups.
Clinical Relevance
Fully understanding lower extremity and trunk kinematic differences in participants with CAI may allow us to better identify abnormal movement patterns that should be addressed in rehabilitation programs. Additionally, identifying preexisting movement patterns, such as altered trunk and hip movements, may help to identify those at high risk of sustaining a future injury.
Limitations
We caution that our results obtained from a recreationally active population may not be transferable to other active or nonactive populations. Future authors should focus on the proper identification and classification of CAI, including copers and noncopers, different levels of disability, and performance on functional-balance tasks. Although the Y Balance Test has gained momentum in recent studies,6,33,34 Coughlan et al33 argued that different postural-control strategies may be used to execute these tests, and thus, our findings cannot be directly compared with those using the Y Balance Test. Continued research on baseline movement patterns, ankle-sprain outcomes, CAI development, and rehabilitation is also warranted.
CONCLUSIONS
Movement-pattern differences at the trunk and hip were present in those with CAI on selected directions of the SEBT. Dynamic balance differed in these selected reach directions, but altered movement strategies may contribute to the long-lasting sequelae of CAI after ankle sprain. Future investigators should more fully examine these differences in a prospective manner.
REFERENCES
- 1.Donovan L, Hertel J. A new paradigm for rehabilitation of patients with chronic ankle instability. Phys Sportsmed. 2012;40(4):41–51. doi: 10.3810/psm.2012.11.1987. [DOI] [PubMed] [Google Scholar]
- 2.Arnold BL, De La Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41(5):1048–1062. doi: 10.1249/MSS.0b013e318192d044. [DOI] [PubMed] [Google Scholar]
- 3.Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PMC free article] [PubMed] [Google Scholar]
- 4.Gribble PA, Hertel J, Denegar CR. Chronic ankle instability and fatigue create proximal joint alterations during performance of the Star Excursion Balance Test. Int J Sports Med. 2007;28(3):236–242. doi: 10.1055/s-2006-924289. [DOI] [PubMed] [Google Scholar]
- 5.Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PMC free article] [PubMed] [Google Scholar]
- 6.Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the Star Excursion Balance Tests. J Sport Rehabil. 2000;9(2):104–116. [Google Scholar]
- 8.Kinzey SJ, Armstrong CW. The reliability of the Star-Excursion Test in assessing dynamic balance. J Orthop Sports Phys Ther. 1998;27(5):356–360. doi: 10.2519/jospt.1998.27.5.356. [DOI] [PubMed] [Google Scholar]
- 9.Robinson RH, Gribble PA. Kinematic predictors of performance on the Star Excursion Balance Test. J Sport Rehabil. 2008;17(4):347–357. doi: 10.1123/jsr.17.4.347. [DOI] [PubMed] [Google Scholar]
- 10.Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 11.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 12.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 13.Cote KP, Brunet ME, Gansneder BM, Shultz SJ. Effects of pronated and supinated foot postures on static and dynamic postural stability. J Athl Train. 2005;40(1):41–46. [PMC free article] [PubMed] [Google Scholar]
- 14.Ounpuu S, Gage JR, Davis RB. Three-dimensional lower extremity joint kinetics in normal pediatric gait. J Pediatr Orthop. 1991;11(3):341–349. [PubMed] [Google Scholar]
- 15.Sefton JM, Hicks-Little CA, Hubbard TJ, et al. Sensorimotor function as a predictor of chronic ankle instability. Clin Biomech (Bristol, Avon) 2009;24(5):451–458. doi: 10.1016/j.clinbiomech.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. [Google Scholar]
- 17.Robinson RH, Gribble PA. Support for a reduction in the number of trials needed for the Star Excursion Balance Test. Arch Phys Med Rehabil. 2008;89(2):364–370. doi: 10.1016/j.apmr.2007.08.139. [DOI] [PubMed] [Google Scholar]
- 18.Brown CN, Padua DA, Marshall SW, Guskiewicz KM. Hip kinematics during a stop-jump task in patients with chronic ankle instability. J Athl Train. 2011;46(5):461–467. doi: 10.4085/1062-6050-46.5.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caulfield BM, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23(1):64–68. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 20.Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74(1):17–28. doi: 10.1093/ptj/74.1.17. [DOI] [PubMed] [Google Scholar]
- 21.Bullock-Saxton JE, Janda V, Bullock MI. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med. 1994;15(6):330–334. doi: 10.1055/s-2007-1021069. [DOI] [PubMed] [Google Scholar]
- 22.Negahban H, Moradi-Bousari A, Naghibi S, et al. The eccentric torque production capacity of the ankle, knee, and hip muscle groups in patients with unilateral chronic ankle instability. Asian J Sports Med. 2013;4(2):144–152. doi: 10.5812/asjsm.34515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webster KA, Gribble PA. A comparison of electromyography of gluteus medius and maximus in subjects with and without chronic ankle instability during two functional exercises. Phys Ther Sport. 2013;14(1):17–22. doi: 10.1016/j.ptsp.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Brown CN, Padua DA, Marshall SW, Guskiewicz KM. Variability of motion in individuals with mechanical or functional ankle instability during a stop jump maneuver. Clin Biomech (Bristol, Avon) 2009;24(9):762–768. doi: 10.1016/j.clinbiomech.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 25.McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. doi: 10.1186/1471-2474-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. doi: 10.2519/jospt.2006.2244. [DOI] [PubMed] [Google Scholar]
- 27.Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Orthop Sports Phys Ther. 2013;43(8):585–591. doi: 10.2519/jospt.2013.0303. [DOI] [PubMed] [Google Scholar]
- 28.Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Correlations among multiple measures of functional and mechanical instability in subjects with chronic ankle instability. J Athl Train. 2007;42(3):361–366. [PMC free article] [PubMed] [Google Scholar]
- 29.Simon J, Donahue M, Docherty C. Development of the Identification of Functional Ankle Instability (IdFAI) Foot Ankle Int. 2012;33(9):755–763. doi: 10.3113/FAI.2012.0755. [DOI] [PubMed] [Google Scholar]
- 30.Carcia CR, Martin RL, Drouin JM. Validity of the foot and ankle ability measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–355. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 33.Coughlan GF, Fullam K, Delahunt E, Gissane C, Caulfield BM. A comparison between performance on selected directions of the star excursion balance test and the Y balance test. J Athl Train. 2012;47(4):366–371. doi: 10.4085/1062-6050-47.4.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4(2):92–99. [PMC free article] [PubMed] [Google Scholar]