Abstract
Context:
Whereas static lower extremity alignment (LEA) has been identified as a risk factor for anterior cruciate ligament injury, little is known about its influence on joint motion and moments commonly associated with anterior cruciate ligament injury.
Objective:
To cluster participants according to combinations of LEA variables and compare these clusters in hip- and knee-joint kinematics and kinetics during the landing phase of a drop-jump task.
Design:
Descriptive laboratory study.
Setting:
Research laboratory.
Patients or Other Participants:
A total of 141 participants (50 men: age = 22.2 ± 2.8 years, height = 177.9 ± 9.3 cm, weight = 80.9 ± 13.3 kg; 91 women: age = 21.2 ± 2.6 years, height = 163.9 ± 6.6 cm, weight = 61.1 ± 8.7 kg).
Main Outcome Measure(s):
Static LEA included pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, genu recurvatum, tibial torsion, and navicular drop. Cluster analysis grouped participants according to their static LEA profiles, and these groups were compared on their hip- and knee-joint kinematics and external moments during the landing phase of a double-legged drop jump.
Results:
Three distinct clusters (C1–C3) were identified based on their static LEAs. Participants in clusters characterized with static internally rotated hip and valgus knee posture (C1) and externally rotated knee and valgus knee posture (C3) alignments demonstrated greater knee-valgus motion and smaller hip-flexion moments than the cluster with more neutral static alignment (C2). Participants in C1 also experienced greater hip internal-rotation and knee external-rotation moments than those in C2 and C3.
Conclusions:
Static LEA clusters that are positioned anatomically with a more rotated and valgus knee posture experienced greater dynamic valgus along with hip and knee moments during landing. Whereas static LEA contributes to differences in hip and knee rotational moments, sex may influence the differences in frontal-plane knee kinematics and sagittal-plane hip moments.
Key Words: anterior cruciate ligament injury risk factors, lower extremity posture, anatomical alignment
Key Points
The direction and magnitude of frontal-plane hip and knee biomechanics during landing differed among participants clustered by lower extremity posture.
Participants with rotational alignments that contribute to a static knee-valgus posture tended to demonstrate joint kinematic and kinetic patterns thought to increase anterior cruciate ligament injury risk.
Differences in the static alignment of the proximal structures of the hip and pelvis appeared to influence rotational moments about the hip and knee, regardless of sex.
Faulty dynamic alignment during landing activities, or functional valgus collapse, has been described as one of the mechanisms associated with noncontact anterior cruciate ligament (ACL) injury.1,2 Functional valgus collapse, which is characterized by increased hip adduction and internal rotation along with knee valgus and either internal or external rotation, has been observed more often in females than in males during landing activities.3–7 Females also have demonstrated greater frontal- and transverse-plane knee moments than males during dynamic activities that potentially place the ACL at greatest risk of injury.3,8–10 Whereas these differences in lower extremity kinematics and kinetics have been proposed to increase the risk of ACL injury in females,6 much is still unknown about the factors contributing to these high-risk lower extremity joint biomechanics.
Differences in static lower extremity alignment (LEA) have been suggested to be an intrinsic risk factor for ACL injury,2,11–15 and in some cases, authors of retrospective studies have identified associations between ACL injury status and greater pronation,16–18 pelvic angle,19 and genu recurvatum.17 Limitations of these studies were that only 1 or a few LEA variable(s) were examined, and the mechanism by which static LEA contributes to ACL injury was not investigated. Specifically, static LEAs along the lower kinetic chain that structurally position the lower extremity in a more inwardly rotated hip and valgus knee position may contribute to dynamic alignments and increased moments thought to increase the risk of ACL injury. Nguyen et al20 reported that greater femoral anteversion and navicular drop predicted greater hip internal-rotation motion and that greater femoral anteversion and genu recurvatum predicted greater knee external-rotation motion during a controlled single-legged squat.
Examining discrete LEA variables may not sufficiently describe the interaction among multiple LEA variables along the kinetic chain. Evaluating the influence of static LEA by grouping people based on similarities in LEA characteristics may be a more appropriate approach to understanding the role of lower extremity posture in the expression of dynamic motion and joint moments. The rationale for this approach is based on evidence that static LEA variables are not independent of one another but rather interact along the lower extremity kinetic chain.21,22 Therefore, the first purpose of our study was to measure static LEA characteristics along the kinetic chain and cluster participants into lower extremity profile groups based on the similarities and differences in their LEA characteristics. Our expectation was that the clusters would be defined by similarities in static alignments of the proximal anatomical structures (pelvis or femur) versus the distal anatomical structures (tibia or foot). This expectation was based on previous work in which investigators21 identified an LEA posture characterized by a relationship between the pelvis and knee and another LEA posture characterized by a relationship among the alignment of the knee, tibia, and foot. Our second purpose was to compare hip- and knee-joint kinematics and kinetics during the initial landing phase of a drop-jump task among clusters with different LEA profiles. Our hypothesis was that participants who were structurally aligned with hips more inwardly rotated and greater knee-valgus postures would land with greater frontal- and transverse-plane hip and knee motions and moments.
METHODS
Participants
A total of 141 participants (50 men: age = 22.2 ± 2.8 years, height = 177.9 ± 9.3 cm, weight = 80.9 ± 13.3 kg; 91 women: age = 21.2 ± 2.6 years, height = 163.9 ± 6.6 cm, weight = 61.1 ± 8.7 kg) were measured on LEA variables and knee-joint biomechanics as part of a larger study.23,24 Participants were recreationally active, which was defined as being active for 2.5 to 10 hours per week for the 3 months before the study; had a body mass index (weight/height2) ≤ 30; and had no history of ligament or cartilage injury to the knee. All measurements were made on the dominant-stance limb, which was defined as the stance extremity used when kicking a ball. All participants provided written informed consent, and the study was approved by the Institutional Review Board of the University of North Carolina at Greensboro.
Measurement of Static LEA
For this study, we assessed 6 alignment characteristics of the pelvis and lower extremity based on commonly identified variables suggested to influence dynamic motion and the risk of ACL injuries.25 All measurement procedures were performed by a single examiner (A.D.N.), who had established good to excellent test-retest reliability on all measures (intraclass correlation coefficient [2,3] ≥ 0.87)26,27 using identical techniques that have been described in detail.26–29 All standing measures were taken in a standardized stance with the feet spaced equal to the width of the left and right acromion processes and the toes facing forward. The stance was achieved by instructing participants to march in place and then take a step forward. Participants were instructed to look straight ahead during all standing measures and to distribute their weight evenly over both feet. Pelvic angle was measured in standing using an inclinometer and represented the angle formed by a line from the anterior-superior iliac spine to the posterior-superior iliac spine relative to the horizontal plane.24,30 Femoral anteversion was measured in a prone position using the Craig test, which has been highly correlated with intraoperative measurements.31 Quadriceps angle was measured in standing and represented the angle formed by a line from the anterior-superior iliac spine to the patellar center and a line from the patella center to the tibial tuberosity.24 Tibiofemoral angle was measured in standing and represented the angle formed by the anatomical axis of the femur (line from the midpoint between the anterior-superior iliac spine and the greater trochanter to the knee-joint center) and the anatomical axis of the tibia (line from the knee-joint center to the ankle-joint center) in the frontal plane.24,26 Whereas the validity of this clinical measurement to represent the frontal-plane angle of the tibiofemoral joint is unknown, the anatomical landmarks used in the clinical measurement have been suggested to approximate the anatomical axes of the femur and tibia.28 Genu recurvatum was measured in a supine position with a bolster positioned under the distal tibia and represented the sagittal-plane alignment of the femur and tibia when participants maximally extended their knees.26 Navicular drop was measured in standing and represented the difference between the height of the navicular in a subtalar-joint neutral position and a relaxed stance.24,26 Tibial torsion was measured in a supine position with the knee extended and represented the angle formed by a line bisecting the bimalleolar axis and the true vertical.26 Each measure was repeated 3 times, and the average value was entered into the cluster analysis.
Biomechanical Assessment of Drop Landings
Kinematic data for the pelvis, thigh, shank, and foot were sampled at 100 Hz using 6-degrees-of-freedom electromagnetic sensors (Flock of Birds; Ascension Technology Corp, Milton, VT) and MotionMonitor software (version 8.43; Innovative Sports Training, Inc, Chicago, IL) during a double-legged drop-landing task with previously described methods.23 Electromagnetic position sensors were attached with double-sided tape and elastic wrap over the anterior midshaft of the third metatarsal, the midshaft of the medial tibia, and the lateral aspect of the midshaft of the femur of the dominant-stance limb. An additional sensor was secured on the sacrum. The initial neutral position was established in a standardized stance with the feet spaced equal to the width of the left and right acromion processes and the toes facing forward. The knee- and ankle-joint centers were estimated using the centroid method: the knee-joint center was calculated as the midpoint between the digitized medial and lateral femoral epicondyles, and the ankle-joint center was calculated as the midpoint between the digitized medial and lateral malleoli. We used the method of Leardini and colleagues32 to determine the hip-joint center.
Participants completed 5 barefoot drop-jump landings from a 0.45-m platform placed 0.1 m behind the rear edge of the force plate (model 4060; Bertec Corp, Columbus, OH). Participants were instructed to drop off the platform onto the force plate and then perform a maximal vertical jump, keeping their hands at ear level throughout the landing to eliminate variability attributed to upper extremity swing. Participants were otherwise given no specific instructions on how to land. We allowed 3 practice trials before data collection. Kinetic data were collected simultaneously at 1000 Hz during each trial and synchronized by the software using a foot-contact threshold of 10 N to trigger data collection. Trials were repeated if participants lost their balance, did not land bilaterally, let their hands drop below ear level, or did not land on the force plate after the maximal vertical jump.
Kinematic data were interpolated linearly to force-plate data and low-pass filtered at 12 Hz using a fourth-order, zero-lag Butterworth filter. A segmental reference system defined the body segments (+z-axis directed to the right, +y-axis directed superiorly, +x-axis directed anteriorly). Knee and hip motions were calculated using Euler-angle definitions with a rotational sequence of z y′ x″.33 Kinetic data were low-pass filtered at 12 Hz using a fourth-order, zero-lag Butterworth filter, and intersegmental external-moment data were normalized to the height (Ht) and body weight (BW) (Nm · BW−1 · Ht−1) of each participant. Kinematic and kinetic data for the initial landing phase (initial contact to peak knee-flexion angle) were then normalized to 101 points and averaged across the 5 drop-jump trials to yield an ensemble motion or moment curve for each variable and participant.
Statistical Analysis
We used the Ward hierarchical clustering and nonhierarchical clustering (k-means) analyses to cluster participants based on similarities in their LEA profiles. Standardized scores for each variable were used during the cluster analysis to ensure that the magnitude of any 1 variable did not overwhelm the model.34 After determining cluster membership, we used analysis of variance (ANOVA) and multiple pairwise comparisons with Bonferroni adjustment to examine differences in LEA values among the identified clusters, and then we operationally named these clusters based on their LEA characteristics.
The identified clusters were compared on the pattern of change in sagittal-, frontal-, and transverse-plane hip and knee biomechanics during the initial phase of the drop landing using 2 separate (kinematic, kinetic) 3 (clusters) × 99 (% landing) multivariate repeated-measures ANOVA procedures to control for type 1 error. When multivariate results were different, we examined univariate results and performed post hoc pairwise comparisons without adjustment to further explore main effects and interactions within each univariate model.23 We interpreted interactions with trend analyses and graphical interpretation of the 95% confidence intervals (CIs) to compare the change in landing patterns among the LEA clusters. The α level for all analyses was set at .05. Analyses were performed using the statistical software packages SAS (version 9.2; SAS Institute Inc, Cary, NC) and PASW Statistics 17.0 (SPSS Inc, Chicago, IL).
RESULTS
After preliminary cluster analysis, 1 man and 2 women were excluded because 1 woman had a very large negative femoral-anteversion angle (−14°), which was ±2 SD outside the mean, and the other 2 participants were considered outliers because they were observed visually to not fit the overall clustering pattern. The cluster analysis of the remaining participants (89 women and 49 men) identified 3 distinct clusters based on the similarities in their LEA characteristics. The descriptive statistics for each LEA variable stratified by cluster and the ANOVA model results when comparing clusters among groups are provided in Table 1. Normative adult values from a large data set (50 men and 50 women) using identical measurement methods are included for comparison.28 Based on these normative values,28 participants in cluster 1 (4 men, 45 women) had relatively high anterior pelvic tilt (Cohen d = 0.8), femoral anteversion (Cohen d = 0.4), knee-valgus angles (quadriceps [Cohen d = 0.8] and tibiofemoral angles [Cohen d = 0.8]), and genu recurvatum (Cohen d = 0.4) and had below-average tibial torsion (Cohen d = −1.1). As such, cluster 1 was named internally rotated hip and valgus knee posture (HIR-KVAL). Individuals in cluster 3 (4 men, 28 women) had relatively high anterior pelvic tilt (Cohen d = 0.7) and valgus knee angles (quadriceps [Cohen d = 1.3] and tibiofemoral [Cohen d = 1.5] angles), average femoral anteversion (Cohen d = −0.2), below-average genu recurvatum (Cohen d = −0.9), and above-average tibial torsion (Cohen d = 0.9) and were named externally rotated knee and valgus knee posture (KER-KVAL). Participants in cluster 2 (41 men, 16 women) had relatively average values in all LEA variables and were named neutral posture (NEUT). All groups had navicular-drop values that were within the average ranges that have been reported.28
Table 1.
Comparative Normative Values (Mean ± SD) in Lower Extremity Alignment Clusters
| Lower Extremity Alignment Variable |
Our Study |
||||
| Cluster 1: Internally Rotated Hip and Valgus Knee Posture (4 men, 45 women) |
Cluster 2: Neutral Posture (41 men, 16 women) |
Cluster 3: Externally Rotated Knee and Valgus Knee Posture (4 men, 28 women) |
|||
| Nguyen and Shultz28,a | |||||
| Men (n = 50) |
Women (n = 50) |
||||
| Pelvic angle, ° | 13.9 ± 3.8b | 9.7 ± 3.6c | 13.5 ± 4.9b | 8.7 ± 4.1 | 12.0 ± 4.9 |
| Femoral anteversion, ° | 15.3 ± 5.2d | 8.4 ± 4.5c | 11.9 ± 5.1e | 8.8 ± 5.2 | 17.6 ± 6.7 |
| Quadriceps angle, ° | 14.1 ± 3.4d | 9.2 ± 3.2c | 17.4 ± 5.6e | 9.0 ± 4.1 | 12.9 ± 4.6 |
| Tibiofemoral angle, ° | 11.8 ± 2.3d | 9.5 ± 2.2c | 13.2 ± 2.0e | 8.9 ± 2.5 | 10.7 ± 2.5 |
| Genu recurvatum, ° | 5.5 ± 3.7f | 4.0 ± 3.3f | 1.4 ± 2.7e | 2.3 ± 2.1 | 6.1 ± 4.2 |
| Tibial torsion, ° | 13.1 ± 4.5d | 16.4 ± 5.5c | 25.9 ± 6.7e | 20.5 ± 7.3 | 18.6 ± 6.3 |
| Navicular drop, mm | 5.1 ± 2.8 | 6.0 ± 3.4 | 6.6 ± 4.4 | 6.3 ± 3.0 | 7.3 ± 3.6 |
Normative values represent overall mean values of right and left limbs.
Mean is different from the mean of cluster 2.
Mean is different from the means of clusters 1 and 3.
Mean is different from the means of clusters 2 and 3.
Mean is different from the means of clusters 1 and 2.
Mean is different from the mean of cluster 3.
Kinematic Differences During Landing
The means ± SDs for kinematic and kinetic variables across the entire landing phase stratified by LEA group are shown in Table 2. Multivariate tests examining hip and knee kinematics across the entire landing phase identified a main effect for cluster (P < .001) and a cluster × percentage landing-phase interaction (P < .001). Follow-up univariate tests revealed that these differences were primarily isolated to knee varus and valgus motion (F2,135 = 5.92, P = .003), with participants in the static NEUT cluster maintaining a varus knee position (−1.06° ± 6.17°) across the entire landing phase. This finding differed from both the HIR-KVAL cluster (3.09° ± 6.81°, P = .002) and the KER-KVAL cluster (2.48° ± 7.01°, P = .02), with both demonstrating valgus knee positions throughout the landing phase.
Table 2.
Average Joint Position and External Joint Moments Across Entire Landing Phase Stratified by Static Lower Extremity Alignment Cluster
| Variable |
Cluster 1: Internally Rotated Hip and Valgus Knee Posture |
Cluster 2: Neutral Posture |
Cluster 3: Externally Rotated Knee and Valgus Knee Posture |
| Average joint position, ° | |||
| Hip flexion (+) | 46.68 ± 10.09 | 49.38 ± 13.83 | 49.55 ± 12.04 |
| Hip adduction (−) | −0.91 ± 7.28 | 2.08 ± 6.68 | −0.47 ± 8.43 |
| Hip internal rotation (−) | 1.03 ± 6.22 | 0.14 ± 7.14 | −1.60 ± 7.20 |
| Knee flexion (−) | −57.84 ± 10.88 | −59.27 ± 10.88 | −60.09 ± 10.22 |
| Knee valgus (+)a | 3.09 ± 6.81 | −1.06 ± 6.17 | 2.48 ± 7.01 |
| Knee external rotation (+) | −0.01 ± 9.08 | 0.84 ± 9.13 | 1.82 ± 7.81 |
| Average external joint moments, (Nm · BW−1 · Ht−1) × 10−2 | |||
| Hip flexion (−)b | −10.19 ± 3.27 | −11.52 ± 3.44 | −9.29 ± 2.85 |
| Hip adduction (+) | −5.00 ± 4.06 | −4.03 ± 3.72 | −3.84 ± 2.71 |
| Hip internal rotation (−) | 4.81 ± 1.74 | 4.20 ± 2.32 | 4.12 ± 1.43 |
| Knee flexion (+) | 2.23 ± 2.23 | 2.19 ± 2.02 | 3.09 ± 2.12 |
| Knee valgus (−) | −6.85 ± 2.93 | −5.62 ± 3.25 | −5.60 ± 2.15 |
| Knee external rotation (−)c | −2.69 ± 1.11 | −1.98 ± 1.64 | −1.87 ± 0.79 |
Abbreviations: BW, body weight; Ht, height.
Main effect: cluster 2 < clusters 1 and 3 (P ≤ .02).
Main effect: cluster 2 > clusters 1 and 3 (P ≤ .03).
Main effect: cluster 1 > clusters 2 and 3 (P = .006).
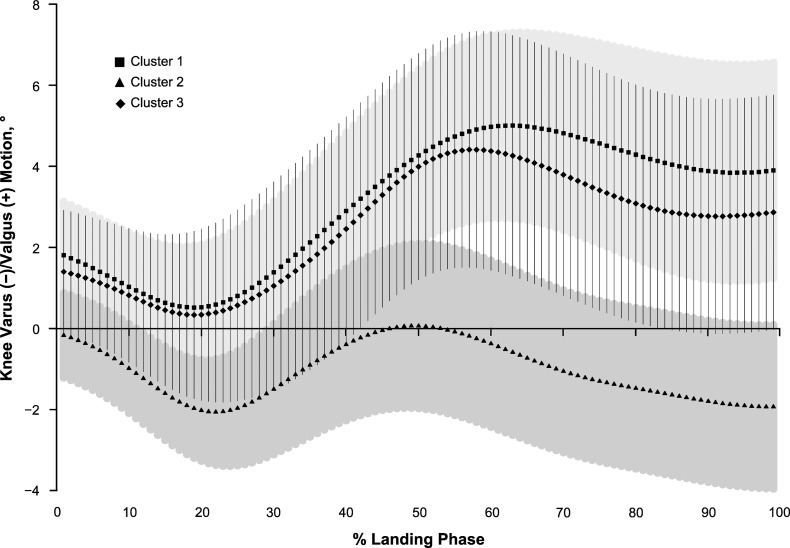
Graphic representation of the data with 95% CIs (Figure 1) and trend analyses for the cluster × percentage landing-phase interaction revealed a linear trend in the data (linear term; F2,135 = 5.18, P = .007). The rate of increase in valgus motion was less in the NEUT cluster than in the HIR-KVAL (F1,104 = 8.83, P = .004) and KER-KVAL (F1,87 = 4.78, P = .03) clusters, resulting in greater knee valgus for participants in the HIR-KVAL cluster during the last 50% of the landing phase than the NEUT cluster. We found no differences in knee varus or valgus motion patterns between the 2 clusters characterized with rotational-valgus alignment (HIR-KVAL versus KER-KVAL; P value range = .55–.89). No other kinematic group main effects or interactions were observed for LEA clusters at the hip or knee (P value range = .09–.76).
Figure 1.
Knee varus (−) and valgus (+) motion (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture.
Kinetic Differences During Landing
Multivariate tests comparing LEA groups on hip and knee external moments ([Nm · BW−1 · Ht−1] × 10−2) across the entire landing phase identified a main effect for group (P < .001) and a group × percentage landing-phase interaction (P < .001). Follow-up univariate tests revealed cluster main effects for hip-flexion (F2,135 = 5.19, P = .007) and knee external-rotation (F2,135 = 5.31, P = .006) moments and cluster × percentage landing-phase interactions for hip-flexion (P = .006), hip internal-rotation (P = .01), and knee external-rotation (P = .01) moments.
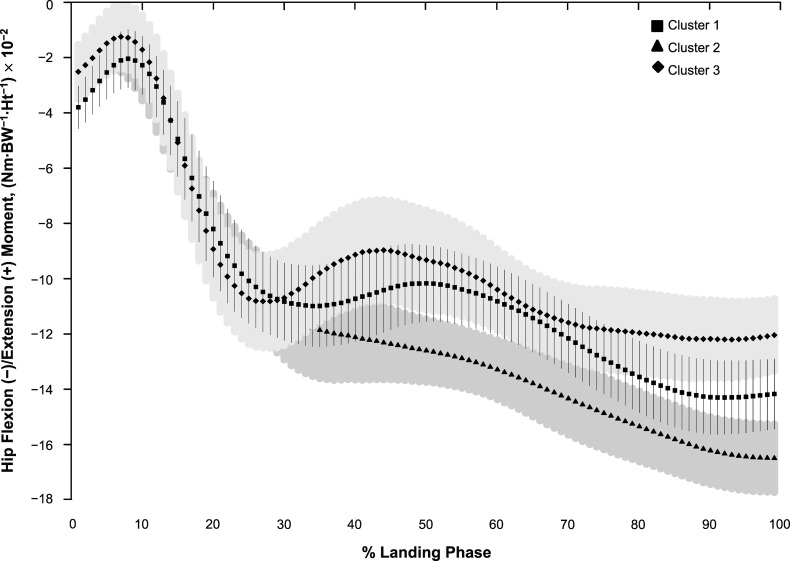
Hip-flexion moments were generally greater across the entire landing phase in the NEUT cluster (−11.5 ± 3.4) than in the HIR-KVAL (−10.2 ± 3.3; P = .04) and KER-KVAL (−9.3 ± 2.8; P = .03) clusters. Graphic representation of the data with 95% CIs (Figure 2) and trend analyses for the cluster × percentage landing-phase interaction revealed a linear trend in the data (linear term; F2,135 = 8.72, P < .001). The rate of increase in hip-flexion moment was greater in the NEUT cluster than in the HIR-KVAL (F1,104 = 8.83, P = .008) and KER-KVAL (F1,87 = 16.99, P < .001) clusters, resulting in greater hip-flexion moments for participants in the NEUT cluster during midlanding and throughout the last 30% of the landing than in the KER-KVAL cluster.
Figure 2.
Hip flexion (−) and extension (+) external moment (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture. Abbreviations: BW, body weight; Ht, height.
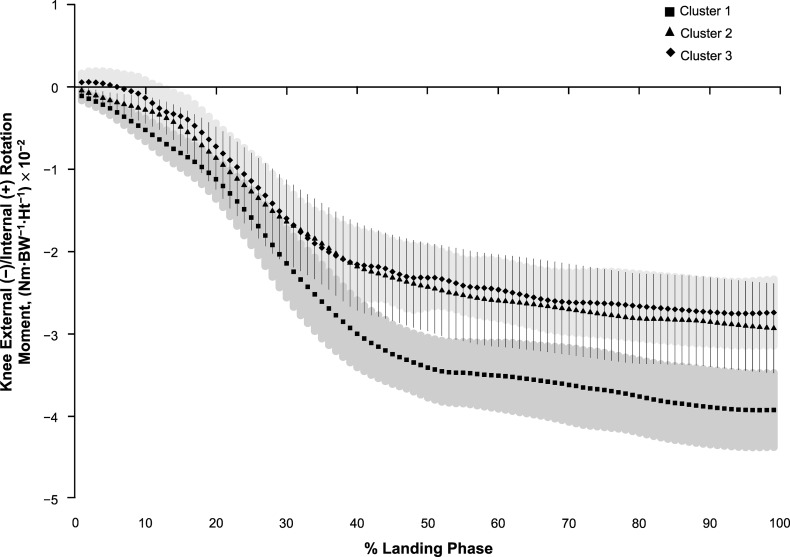
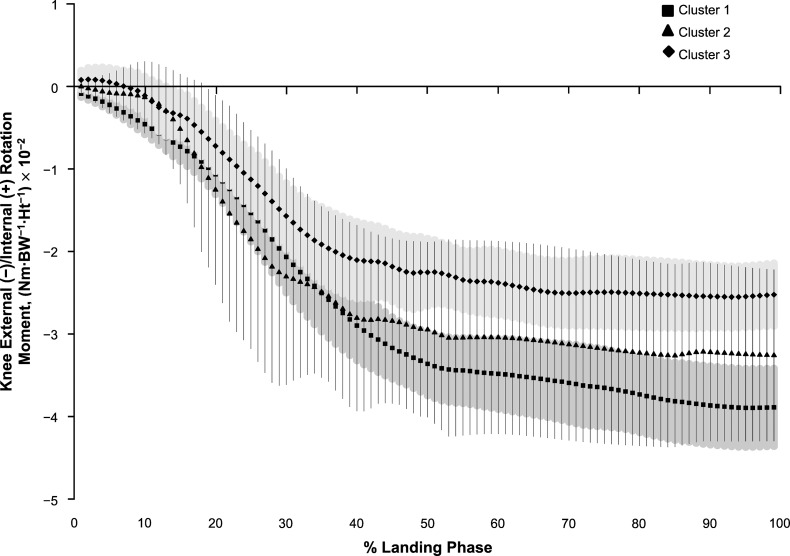
Knee external-rotation moments were generally greater in the HIR-KVAL cluster (−2.7 ± 1.1) than in the NEUT (−2.0 ± 1.6; P = .006) and KER-KVAL (−1.9 ± 0.8; P = .006) clusters. Graphic representation of the data with 95% CIs (Figure 3) and trend analyses revealed a linear trend in the data (linear term; F2,135 = 4.30, P < .001). The rate of increase in knee external-rotation moment was greater for participants in the HIR-KVAL cluster than for those in the NEUT (F1,104 = 6.25, P = .01) and KER-KVAL (F1,79 = 6.74, P = .01) clusters, resulting in greater knee external-rotation moments for those in the HIR-KVAL cluster than for those in the KER-KVAL cluster throughout the last 60% of the landing.
Figure 3.
Knee external (−) and internal (+) rotation external moment (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture. Abbreviations: BW, body weight; Ht, height.
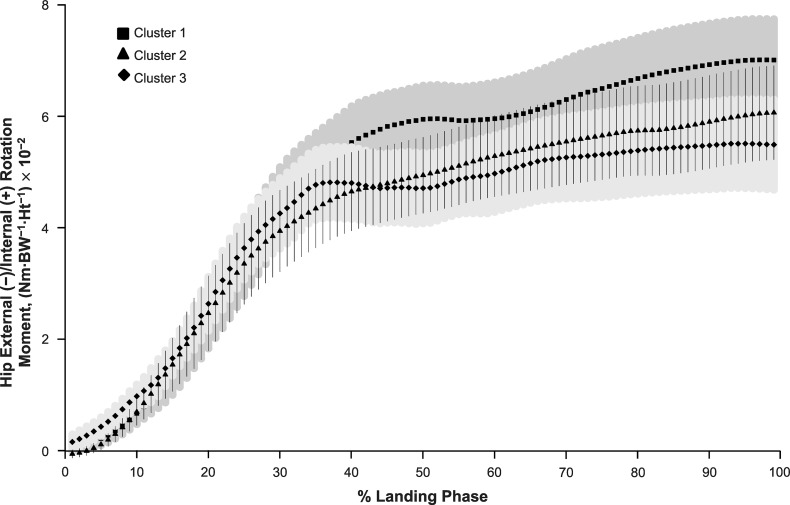
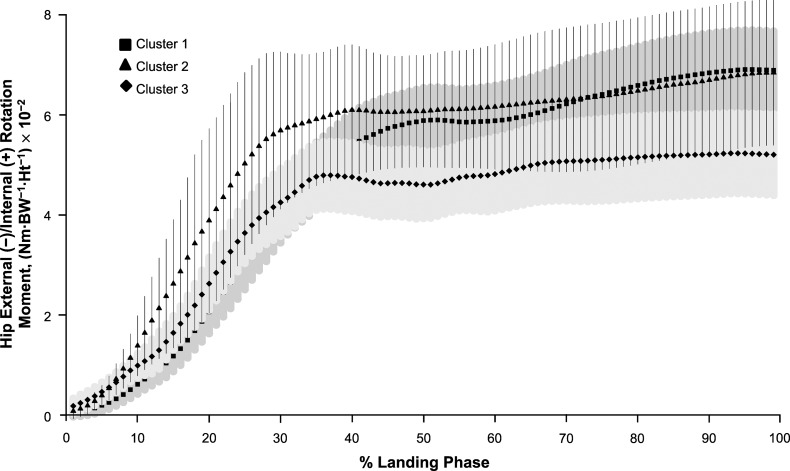
Graphic representation of the data with 95% CIs (Figure 4) and trend analyses for the cluster by percentage of landing interaction for hip internal-rotation moment revealed a linear trend in the data (linear term; F2,135 = 4.52, P = .01). The rate of increase of hip internal-rotation moments was greater in the HIR-KVAL than in the KER-KVAL cluster (F1,79 = 9.08, P = .003), which resulted in greater hip internal-rotation moments during the last 10% of landing in the HIR-KVAL cluster. We found no other group main effects for cluster (P value range = .06–.27) or clusters by percentage of landing (P value range for interactions = .07–.86) for the remaining joint moments.
Figure 4.
Hip external (−) and internal (+) rotation external moment (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture. Abbreviations: BW, body weight; Ht, height.
DISCUSSION
Evidence has suggested that static alignment variables are not independent of one another but rather interact along the lower extremity kinetic chain.21 To our knowledge, we are the first to cluster participants based on a collection of LEA characteristics to better examine the effects of overall lower extremity posture on lower extremity biomechanics during a functional activity. Our primary findings were that the HIR-KVAL and KER-KVAL clusters exhibited a greater absolute magnitude and rate of knee-valgus motion and less hip-flexion moment during landing than participants in the NEUT cluster. The HIR-KVAL cluster also exhibited a greater rate of hip internal-rotation moment than the KER-KVAL cluster and a greater knee external-rotation moment than the NEUT and KER-KVAL clusters. These differences in lower extremity motion, along with the differences in external moments at the hip and knee, suggest that persons who tend to have above-average frontal-plane static knee-valgus angles (quadriceps angle and tibiofemoral angle) and torsional alignment of either the femur (femoral anteversion) or the tibia (outward torsion of the tibia) may be more prone to demonstrate dynamic joint motions or forces associated with an increased risk of ACL injury. However, researchers28 have shown that sex differences are present in static measures of LEA and may directly influence the differences observed in frontal-plane knee kinematics and sagittal-plane hip moments. In the following discussion, we will explore the potential relationships between static LEA and landing biomechanics and the influence of sex on the observed differences.
Kinematic Differences
The only observed difference between LEA groups for kinematic variables was for frontal-plane knee motion. When examining the kinematic curves for knee valgus, we found that the pattern and magnitude of motion were very similar between the HIR-KVAL and KER-KVAL clusters and greater than in the NEUT cluster (Figure 1). Closer examination of the pattern and magnitude of dynamic knee valgus across the landing phase showed that participants in the 2 clusters with greater static rotational-valgus alignments (HIR-KVAL and KER-KVAL) landed in approximately 1.5° to 2° of knee valgus at initial contact, moved briefly toward a neutral knee position before progressing toward more knee-valgus motion during landing (maximal valgus angle was approximately 5°), and ended the landing in approximately 3° to 4° of knee valgus. In contrast, participants in the NEUT cluster landed in a neutral frontal-plane knee angle at initial contact, maintained a more neutral knee throughout the landing (maximal valgus angle was approximately 0.05°), and ended the landing in approximately 2° of varus. Taken together, participants in clusters with more rotational-valgus alignment were in approximately 5° to 6° greater relative valgus than those in the NEUT cluster toward the end of the landing.
These differences in frontal-plane knee motions suggest that persons who have greater static knee valgus, particularly those with a corresponding proximal rotational malalignment (femoral anteversion and anterior pelvic tilt), consistently land in more knee valgus, which has been associated with ACL injury.2 Furthermore, based on a recent study in which the authors35 examined joint kinematics during ACL injury, an increase in knee-valgus motion after initial contact was a mechanism consistently observed in participants who sustained ACL injury. Greater knee valgus at initial contact and peak angles were also reported in a group of female athletes who sustained ACL injuries6 and were found to increase ACL strain.36 Less clear are the clinical implications of landing in more knee valgus, as ACL injury is thought to occur early in landing. Given the conflicting findings to date,1,6,37–40 further work is needed to confirm whether the landing patterns during a double-legged landing task predict future ACL injury.
Comparisons of our findings with previous findings are limited. Authors20 of only 1 study have reported that select static LEA variables predicted greater rotational knee motions during a controlled single-legged squat. However, the observed relationships were relatively weak, which may be attributed to examining each static alignment characteristic independently or simply to the single-legged squat not sufficiently reflecting the more demanding tasks (eg, landing from a jump) commonly observed during sport activity when ACL injuries are more likely to occur. Our study, which builds on previous findings by accounting for the potential interactions among LEA characteristics by clustering participants based on similarities in their LEA profiles, may have allowed us to better identify potential links between posture and high-risk knee motions.
Kinetic Differences
The patterns of transverse-plane moments observed about the hip and knee during landing illustrate a consistent internal-rotation moment at the hip with a concomitant external-rotation moment at the knee (Figures 3 and 4). We observed greater knee external-rotation moment (approximately the first 40% of landing) coupled with greater hip internal-rotation moment throughout the landing (approximately 10%–100% of the landing phase) in the HIR-KVAL cluster than in the NEUT and KER-KVAL clusters. One reason for these differences in the joint moments experienced at the hip and knee may be that persons with increased internal rotation of the proximal structures (ie, increased femoral anteversion and pelvic angle) anatomically position the lower extremity in a more inwardly rotated and valgus position. Researchers have reported an association between increased pelvic tilt with increased internal rotation at the hip41 and increased frontal-plane knee angles (quadriceps and tibiofemoral angles),21 whereas external rotation of the tibia on the femur has been observed as a postural compensation to increased femoral anteversion.42 Collectively, this static alignment, in which the hip is internally rotated with the knee in valgus and external rotation, may anatomically perpetuate the increased internal-rotation moments about the hip and external-rotation moments about the knee during landing. In addition, such positions may lead to a decreased ability to control the external moments acting on the hip during landing, because differences in the structural alignment specific to femoral anteversion have been shown to decrease the internal-moment arms of the hip musculature responsible for controlling rotation at the hip43–45 and have been related to decreased force and activation of the hip musculature.46,47 The tendency for participants in our investigation with rotational-valgus alignments versus neutral alignment to minimize sagittal-plane loads about the hip, coupled with greater internal-rotation load at the hip and external-rotation load at the knee experienced during landing, may place these participants at greater risk of ACL injury.
In addition, participants in the HIR-KVAL and KER-KVAL clusters had, on average, less external hip-flexion moment during landing than participants in the NEUT cluster, with differences occurring during the middle and later parts of the landing phase. Shimokochi et al48 suggested that a landing strategy that allows the hip to produce greater extension moments is associated with a more anteriorly positioned center of mass. This type of landing strategy would also decrease the demand on the quadriceps and increase the demand on hip-extensor contraction, which includes the gluteal and hamstrings muscles, thereby potentially reducing the loads on the ACL.48 In addition, a more flexed trunk position has been shown to reduce ground reaction forces and quadriceps muscle activity during landing, potentially decreasing ACL loading.49 The lesser hip-flexion moment during landing in the rotational-valgus clusters may be attributed to the sagittal-plane position of the pelvis, in which anterior pelvic tilt was approximately 4° greater than in the NEUT cluster. Based on clinical observations, a standing posture characterized by an increased anterior pelvic tilt is associated with elongated and weak hip extensors that include the gluteal and hamstrings muscles.50,51 To decrease the demand on these muscles during landing, participants in the rotational-valgus clusters may have developed a landing strategy with the trunk in a more upright position as an “avoidance strategy” to compensate for weakened hip-extensor muscles (ie, gluteals and hamstrings). Landing in a more upright position, however, might increase the risk of ACL injury,52 and persons with rotational-valgus alignments may not be able to handle greater peak loads about the hip that protect the ACL. Whereas we found no differences in hip-flexion motion during landing, future examinations of trunk motion during landing may help to clarify the relationship between static alignment and landing kinetics.
We acknowledge that most participants in the HIR-KVAL and KER-KVAL clusters were women, most participants in the NEUT cluster were men, and sex differences in knee-valgus angles and joint moments during landing tasks are well documented.3–7 However, factors that contribute to these sex differences in lower extremity biomechanics have not been identified clearly. To better understand the influence of sex on the observed kinematic and kinetic differences, we examined separately the graphical representation of the data with 95% CIs for women. The differences observed in frontal-plane knee kinematics and sagittal-plane hip moments between the clusters were no longer present when women were examined separately. This finding suggests that sex is a modifier in these specific biomechanical variables and that the differences in frontal-plane knee kinematics and sagittal-plane hip moments are less likely to be related to differences in static LEA clusters and more likely to be related to sex. However, we still observed differences in knee and hip rotational moments, in which the rate of increase in knee external-rotation and hip internal-rotation moments were greater in the HIR-KVAL than in the KER-KVAL cluster (Figures 5 and 6). This observation suggests that, regardless of sex, persons with increased internal rotation of the proximal structures (ie, increased femoral anteversion and pelvic angle) may have anatomical or neuromuscular differences that result in their landing with greater internal-rotation moments about the hip and external-rotation moments about the knee than persons with increased external-rotation alignment of the distal structures. Given that women have greater angles in the LEA variables (pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, genu recurvatum) 28 that we used to define the specific clusters in our study, our findings provide empirical data that differences in static LEA, in part, may contribute to the differences in hip- and knee- rotation moments during landing between men and women.
Figure 5.
Knee external (−) and internal (+) rotation external moment in women (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture. Abbreviations: BW, body weight; Ht, height.
Figure 6.
Hip external (−) and internal (+) rotation external moment in women (mean ± 95% confidence interval). Cluster 1 indicates an internally rotated hip and valgus knee posture. Cluster 2 indicates a neutral posture. Cluster 3 indicates an externally rotated knee and valgus knee posture. Abbreviations: BW, body weight; Ht, height.
CONCLUSIONS
The direction and magnitude of frontal-plane hip and knee biomechanics during landing were different among participants who were clustered based on their lower extremity postures. These observed differences suggest that persons with lower extremity postures that include some degree of knee valgus tend to demonstrate joint kinematic and kinetic patterns that are commonly thought to increase the risk of ACL injury. Whereas frontal- and sagittal-plane biomechanical differences in landing can be attributed to sex, differences in the static alignment of proximal structures of the hip and pelvis appear to influence the rotational moments about the hip and knee, regardless of sex. Researchers should continue to examine whether the biomechanical differences observed among static LEA clusters are associated with neuromuscular function during activity and whether their interactions contribute to an increased risk of sustaining ACL injury.
ACKNOWLEDGMENTS
This project was supported by award number R01AR053172 from the National Institutes of Health (NIH) National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) to the University of North Carolina at Greensboro (S.J.S.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the NIAMS.
REFERENCES
- 1.Olsen O, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 2.Ireland ML. Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train. 1999;34(2):150–154. [PMC free article] [PubMed] [Google Scholar]
- 3.Shultz SJ, Schmitz RJ. Effects of transverse and frontal plane knee laxity on hip and knee neuromechanics during drop landings. Am J Sports Med. 2009;37(9):1821–1830. doi: 10.1177/0363546509334225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 5.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 6.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 7.Lephart SM, Ferris CM, Riemann BL, Myers JB, Fu FH. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop Relat Res. 2002;401:162–169. doi: 10.1097/00003086-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 8.McLean SG, Fellin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 9.McLean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon) 2005;20(8):863–870. doi: 10.1016/j.clinbiomech.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Sigward SM, Powers CM. The influence of gender on knee kinematics, kinetics and muscle activation patterns during side-step cutting. Clin Biomech (Bristol, Avon) 2006;21(1):41–48. doi: 10.1016/j.clinbiomech.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Hutchinson MR, Ireland ML. Knee injuries in female athletes. Sports Med. 1995;19(4):288–302. doi: 10.2165/00007256-199519040-00006. [DOI] [PubMed] [Google Scholar]
- 13.Ireland ML, Gaudette M, Crook S. ACL injuries in the female athlete. J Sport Rehabil. 1997;6(2):97–110. [Google Scholar]
- 14.McClay Davis I, Ireland ML. ACL injuries: the gender bias. J Orthop Sports Phys Ther. 2003;33(8):A2–A8. [PubMed] [Google Scholar]
- 15.Shultz SJ, Schmitz RJ, Nguyen AD, et al. ACL Research Retreat V: An Update on ACL Injury Risk and Prevention, March 25–27, 2010, Greensboro, NC. J Athl Train. 2010;45(5):499–508. doi: 10.4085/1062-6050-45.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beckett ME, Massie DL, Bowers KD, Stoll DA. Incidence of hyperpronation in the ACL injured knee: a clinical perspective. J Athl Train. 1992;27(1):58–62. [PMC free article] [PubMed] [Google Scholar]
- 17.Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91–97. doi: 10.2519/jospt.1996.24.2.91. [DOI] [PubMed] [Google Scholar]
- 18.Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29(4):343–346. [PMC free article] [PubMed] [Google Scholar]
- 19.Hertel J, Dorfman JH, Braham RA. Lower extremity malalignments and anterior cruciate ligament injury history. J Sports Sci Med. 2004;3(4):220–225. [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen A, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH. A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. J Athl Train. 2011;46(3):246–256. doi: 10.4085/1062-6050-46.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen A, Shultz SJ. Identifying relationships among lower extremity alignment characteristics. J Athl Train. 2009;44(5):511–518. doi: 10.4085/1062-6050-44.5.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther. 1996;23(2):164–170. doi: 10.2519/jospt.1996.23.2.164. [DOI] [PubMed] [Google Scholar]
- 23.Shultz SJ, Schmitz RJ, Kong Y, et al. Cyclic variations in multiplanar knee laxity influence landing biomechanics. Med Sci Sports Exerc. 2012;44(5):900–909. doi: 10.1249/MSS.0b013e31823bfb25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shultz SJ, Dudley WN, Kong Y. Identifying multiplanar knee laxity profiles and associated physical characteristics. J Athl Train. 2012;47(2):159–169. doi: 10.4085/1062-6050-47.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shultz SJ, Nguyen AD, Beynnon BD. Anatomical factors in ACL injury risk. In: TE Hewett, Shultz SJ, Griffin LY., editors. Understanding and Preventing Noncontact ACL Injury. Champaign, IL: Human Kinetics;; 2007. pp. 239–258. In. eds. [Google Scholar]
- 26.Shultz SJ, Nguyen A, Windley TC, Kulas AS, Botic TL, Beynnon BD. Intratester and intertester reliability of clinical measures of lower extremity anatomical characteristics: implications for multi-center studies. Clin J Sport Med. 2006;16(2):155–161. doi: 10.1097/00042752-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Shultz SJ, Nguyen AD, Levine B. The relationship among lower extremity alignment characteristics and anterior knee joint laxity. Sports Health. 2009;1(1):54–60. doi: 10.1177/1941738108326702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389–398. doi: 10.2519/jospt.2007.2487. [DOI] [PubMed] [Google Scholar]
- 29.Shultz SJ, Nguyen AD, Schmitz RJ. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137–149. doi: 10.2519/jospt.2008.2645. [DOI] [PubMed] [Google Scholar]
- 30.Gilliam J, Brunt D, MacMillan M, Kinard RE, Montgomery WJ. Relationship of the pelvic angle to the sacral angle: measurement of clinical reliability and validity. J Orthop Sports Phys Ther. 1994;20(4):193–199. doi: 10.2519/jospt.1994.20.4.193. [DOI] [PubMed] [Google Scholar]
- 31.Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anterversion: a comparison with established techniques. J Bone Joint Surg Am. 1992;74(6):820–830. [PubMed] [Google Scholar]
- 32.Leardini A, Cappozzo A, Cantani F, et al. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32(1):99–103. doi: 10.1016/s0021-9290(98)00148-1. [DOI] [PubMed] [Google Scholar]
- 33.Kadaba MP, Ramakrishnan HK, Wootten ME, Gainey J, Gorton G, Cochran GV. Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. J Orthop Res. 1989;7(6):849–860. doi: 10.1002/jor.1100070611. [DOI] [PubMed] [Google Scholar]
- 34.Everitt B, Landau S, Leese M. Cluster Analysis. 4th ed. New York, NY: Oxford University Press;; 2001. p. 330. [Google Scholar]
- 35.Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218–2225. doi: 10.1177/0363546510373570. [DOI] [PubMed] [Google Scholar]
- 36.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 37.Utturkar GM, Irribarra LA, Taylor KA, et al. The effects of a valgus collapse knee position on in vivo ACL elongation. Ann Biomed Eng. 2013;41(1):123–130. doi: 10.1007/s10439-012-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 39.Boden B, Torg J, Knowles S, Hewett T. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252–259. doi: 10.1177/0363546508328107. [DOI] [PubMed] [Google Scholar]
- 40.Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34(2):163–170. doi: 10.1016/s0021-9290(00)00154-8. [DOI] [PubMed] [Google Scholar]
- 41.Khamis S, Yizhar Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture. 2007;25(1):127–134. doi: 10.1016/j.gaitpost.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 42.Hvid I, Andersen LI. The quadriceps angle and its relation to femoral torsion. Acta Orthop Scand. 1982;53(4):577–579. doi: 10.3109/17453678208992261. [DOI] [PubMed] [Google Scholar]
- 43.Dostal WF, Andrews JG. A three-dimensional biomechanical model of hip musculature. J Biomech. 1981;14(11):803–812. doi: 10.1016/0021-9290(81)90036-1. [DOI] [PubMed] [Google Scholar]
- 44.Dostal WF, Soderberg GL, Andrews JG. Actions of hip muscles. Phys Ther. 1986;66(3):351–361. doi: 10.1093/ptj/66.3.351. [DOI] [PubMed] [Google Scholar]
- 45.Delp SL, Hess WE, Hungerford D, Jones LC. Variation of rotation moment arms with hip flexion. J Biomech. 1999;32(5):493–501. doi: 10.1016/s0021-9290(99)00032-9. [DOI] [PubMed] [Google Scholar]
- 46.Merchant AC. Hip abductor muscle force: an experimental study of the influence of hip position with particular reference to rotation. J Bone Joint Surg Am. 1965;47(3):462–476. [PubMed] [Google Scholar]
- 47.Nyland J, Kuzemchek S, Parks M, Caborn DN. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. J Electromyogr Kinesiol. 2004;14(2):255–261. doi: 10.1016/S1050-6411(03)00078-6. [DOI] [PubMed] [Google Scholar]
- 48.Shimokochi Y, Lee SY, Shultz SJ, Schmitz RJ. The relationships among sagittal-plane lower extremity moments: implications for landing strategy in anterior cruciate ligament injury prevention. J Athl Train. 2009;44(1):33–38. doi: 10.4085/1062-6050-44.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009;44(2):174–179. doi: 10.4085/1062-6050-44.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles: Testing and Function, with Posture and Pain. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins;; 2005. pp. 82–83. [Google Scholar]
- 51.Janda V, Schmid HJA. Muscles as a pathogenic factor in back pain. Paper presented at: 4th Conference of the International Federation of Orthopaedic Manipulative Therapists; February 18–22, 1980. Christchurch, New Zealand: [Google Scholar]
- 52.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Vally II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]