Abstract
Context:
Goniometric assessment of hip-extension range of motion is a standard practice in clinical rehabilitation settings. A weakness of goniometric measures is that small errors in landmarking may result in substantial measurement error. A less commonly used protocol for measuring hip range of motion involves applying trigonometric principles to the length and vertical displacement of the upper part of the lower extremity to determine hip angle; however, the reliability of this measure has never been assessed using the modified Thomas test.
Objective:
To compare the intrarater and interrater reliability of goniometric (GON) and trigonometric (TRIG) techniques for assessing hip-extension range of motion during the modified Thomas test.
Design:
Controlled laboratory study.
Setting:
Institutional athletic therapy facility.
Patients or Other Participants:
A total of 22 individuals (12 men, 10 women; age range, 18–36 years) with no pathologic knee or back conditions.
Main Outcome Measure(s):
Hip-extension range of motion of each participant during a modified Thomas test was assessed by 2 examiners with both GON and TRIG techniques in a randomly selected order on 2 separate days.
Results:
The intraclass correlation coefficient (ICC) revealed that the reliability of the GON technique was low for both the intrarater (ICC = 0.51, 0.54) and interrater (ICC = 0.30, 0.65) comparisons, but the reliability of the TRIG technique was high for both intrarater (ICC = 0.90, 0.95) and interrater (ICC = 0.91, 0.94) comparisons. Single-factorial repeated-measures analyses of variance revealed no mean differences in scoring within or between examiners for either measurement protocol, whereas a difference was observed when comparing the TRIG and GON tests due to the differences in procedures used to identify landmarks.
Conclusions:
Using the TRIG technique to measure hip-extension range of motion during the modified Thomas test results in superior intrarater and interrater reliability when compared with the GON technique.
Key Words: assessment, musculoskeletal testing, flexibility
Key Points
For measuring hip-extension range of motion, reliability of the trigonometric technique was high, but reliability of the goniometric technique was poor to moderate.
Both intrarater and interrater reliability were higher when examiners used the trigonometric technique than when they used the goniometric technique to assess hip-extension range of motion during the modified Thomas test.
In a clinical setting, joint range-of-motion (ROM) measurements are an integral part of a physical assessment, allowing clinicians to quantify the severity of ROM loss or assess the efficacy of a treatment and the subsequent progress of the patient. Given that clinics report joint ROM to insurance agencies and use it as a return-to-play criterion for athletes, any ROM measurement instrument must be verified as both valid and reliable. A variety of ROM measurement instruments and techniques are available to clinicians; the most commonly applied is the universal goniometer.1 The consistency of the universal goniometer for assessing joint ROM has been reviewed extensively,2,3 and this instrument has shown both intrarater and interrater reliability when hinge joints, such as the elbow and knee, are assessed.4–7 The reliability of the goniometric (GON) technique may be reduced when measuring hip, shoulder, and ankle ROM and varies greatly depending on the movement assessed.2,3 These results suggest that limitations are associated with the GON techniques, specifically when assessing the hip joint.
Linear measurement tools, such as the tape measure, have been assessed in clinical settings and, in some cases, have been combined with trigonometric (TRIG) principles to provide reliable measures of joint angle.8–10 To date, the reliability of TRIG techniques for measuring hip-extension ROM during the modified Thomas test has not been assessed. If this method of measurement can be established as having both intrarater and interrater reliability, it could be an easily learned and practical approach to assessing hip-extension ROM. Therefore, the purpose of our study was to compare the intrarater (within-examiner) and interrater (between-examiners) reliability of GON and TRIG techniques for measuring hip-extension ROM during the modified Thomas test. Given that it is technically easier to identify landmarks and to administer the TRIG technique during the modified Thomas test, we hypothesized that this technique would have superior reliability when compared with GON measures.
METHODS
Participants
A total of 22 college students (12 men, 10 women; age range, 18–36 years) were recruited and completed all testing protocols. Participants answered the Physical Activity Readiness Questionnaire before the study began. They also completed an activity-history questionnaire and were excluded from the study if they had a history of knee, hip, or lower back pathologic conditions or fractures within the preceding 3 years or if they experienced pain in these regions that would inhibit performance of the modified Thomas test. All participants provided written informed consent, and the study was approved by the Sheridan College Research Ethics Board.
Examiners
Two examiners (A.H., N.D.) investigated the interrater reliability of the measurement techniques. Both examiners were certified athletic therapists in good standing with 5 and 3 years of clinical experience, respectively. The examiners were responsible for administering the modified Thomas test, positioning the measurement instruments, and reading the measurements to the research assistant who recorded the results.
Study Design and Procedures
We used a crossover, repeated-measures design in which participants executed all protocols. The order in which they completed the protocols was randomized and counterbalanced using a coin toss at the start of each testing day to determine examiner and testing order. This design was used to examine the intrarater and interrater reliability of the GON and TRIG techniques of hip-extension ROM during the modified Thomas test.
Participants were required to report to the human performance laboratory on 3 occasions wearing loose-fitting clothing, such as shorts and a T-shirt. During the first visit, they were provided an oral description of the study and were informed of the time commitment necessary to complete all testing days. After completing the consent form, Physical Activity Readiness Questionnaire, and injury questionnaire, they were familiarized with the modified Thomas test procedure and informed of the protocols associated with both measurement techniques.
Next, they reported on 2 days to complete the testing protocols. On each day, they were assessed by both examiners using the TRIG and GON measurement techniques. Right hip-extension ROM was assessed in randomized order, with each examiner blinded to the results of the other examiner. The right hip-extension ROM of each participant, therefore, was assessed 4 times on each testing day. Testing sessions were separated by a minimum of 24 hours and a maximum of 48 hours. Participants were instructed to continue their activities of daily living without being involved in vigorous exercise 24 hours before test days and without starting any new lower body stretching routines.
Modified Thomas Test
For the modified Thomas test, participants were instructed to sit on the edge of the treatment table, allowing the ischial tuberosity to clear the edge of the bed (resting the gluteal fold on the edge of the bed) while keeping their feet flat on the ground. Next, they flexed the left lower extremity at the hip and knee, bringing the knee to the chest. While grabbing the elevated knee with both hands, participants slowly rolled back onto the table with assistance from the examiner. The left lower extremity was supported externally in 90° of flexion at the hip and knee to allow the participants to completely relax during the test and to standardize the pelvic tilt and lumbar lordotic curve of the spine. The right hip could extend freely and unsupported off the table to allow full extension without infringement by the examination table (Figure 1). The examiner asked the participants if they felt any restriction in hip extension due to the examination table. If they felt restriction by the examination table, they repeated the test procedure to modify the setup. If they felt no external restriction by the examination table, the examiner orally instructed them to take a deep breath in and out and then relax. When the participants had relaxed fully, the examiner measured the hip angle using the selected measurement protocol. Body placement was standardized to ensure that any measurement error observed between protocols was actually due to the instrument or technique itself and not to variations in the positioning of participants during the modified Thomas test.
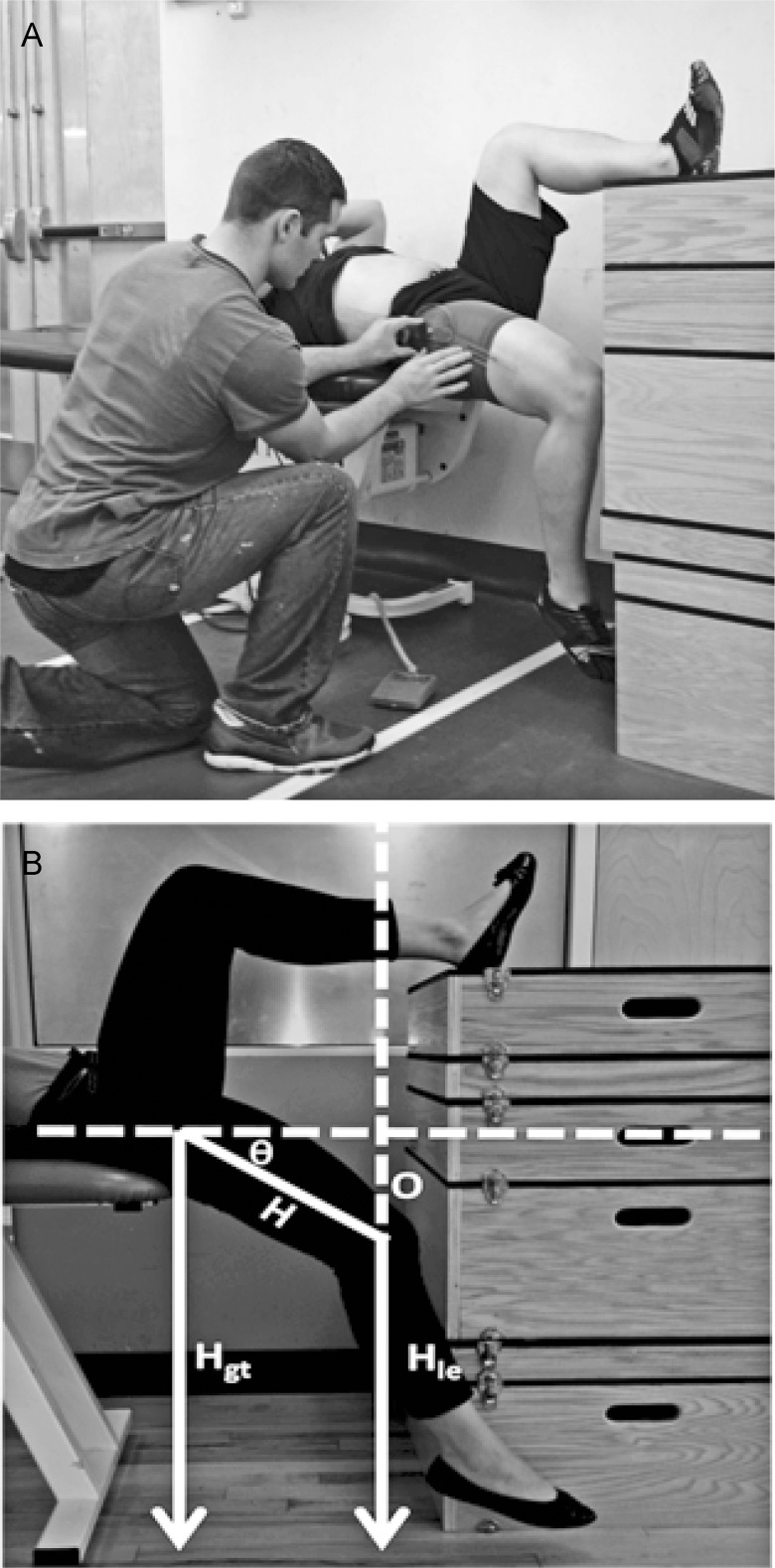
Figure 1.
Measurement of hip-extension range of motion. A, Goniometric method. The goniometer upper arm was placed along the midline of the torso, the fulcrum was placed over the greater trochanter, and the lower arm was placed along the lateral side of the femur, using the lateral epicondyle as a landmark. B, Trigonometric method. The investigator used a marker to identify the greater trochanter and the most posterior palpable aspect of the lateral epicondyle of the femur. The investigator then measured the length between these landmarks with a standard tape measure and the height of the 2 landmarks from the ground using a stadiometer. The hip angle was calculated using the equation, θ = sin−1(O / H), where θ is the hip-extension angle, opposite (O) is the height of the greater trochanter minus the height of the lateral epicondyle, and hypotenuse (H) is the distance from the greater trochanter to the lateral epicondyle.
Goniometric Measurement Procedure
The GON measurement protocol was similar to that reported by Clapis et al.11 Once a participant was positioned correctly in the modified Thomas test, the fulcrum of the goniometer (Jamar, Hatfield, PA) was placed over the lateral aspect of the greater trochanter. The proximal arm was aligned with the lateral midline of the pelvis, and the distal arm was aligned with the lateral midline of the femur using the lateral epicondyle as a reference point (Figure 1A).
Trigonometric Measurement Procedure
Once a participant was positioned correctly in the modified Thomas test, the investigator used a washable marker to identify the greater trochanter and the most posterior palpable aspect of the lateral epicondyle of the femur. The investigator then measured the length between these landmarks with a standard anthropometric tape measure (model J00305; Lafayette Instrument, Lafayette, IN) and the height of the 2 landmarks from the ground using a stadiometer (model 213; seca, Birmingham, UK) (Figure 1B). The joint angle was calculated using the equation θ = sin−1(O / H), where θ is the hip-extension angle, opposite (O) is the height of greater trochanter minus the height of the lateral epicondyle, and hypotenuse (H) is the distance from the greater trochanter to the lateral epicondyle. After each TRIG measurement was taken, the marker was completely cleaned off the skin with alcohol wipes before the next examiner performed the assessment.
Data Analysis
We performed statistical analysis using SPSS (version 22; IBM Corporation, Armonk, NY) and Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA) software programs. Interrater intraclass correlation coefficients (ICCs) (2,1) and intrarater ICCs (3,1) were calculated for the GON and TRIG techniques. Intraclass correlation coefficient values of greater than 0.75 generally are considered to have a high level of reliability; between 0.40 and 0.75, fair to moderate reliability; and less than 0.40, poor reliability.12,13 Standard error of measurement was calculated using the equation, SD × √(1 − ICC), where SD is the standard deviation of all measurements, and the ICC value was obtained from the intrarater and interrater analyses. Coefficient of variance was calculated using the equation, 100 × SD / mean. We conducted single-factorial repeated-measures analyses of variance (ANOVAs) to determine whether a difference existed within and between examiners and testing protocols. Bland-Altman plots were used to provide a visual representation of the scoring range for within-examiner and between-examiners results. These plots allow 2 measurements or measurement techniques to be compared for agreement. The graph was constructed to plot the difference between the measurements against their mean. Bland and Altman14 indicated that a correlation of 2 measurement techniques was not enough to suggest that one is superior to the other and that the device also must show good agreement between measurement trials. A power analysis of 22 participants using r2 values of 0.3 to 0.95 at a P value of .05 indicated a strong power of 0.72 to 1.0, respectively.
RESULTS
The participants' mean hip-joint angles were 14° ± 6° for examiner 1 and 17° ± 5° for examiner 2 using the GON technique and 31° ± 8° for examiner 1 and 33° ± 9° for examiner 2 using the TRIG technique (Table 1).
Table 1.
Goniometric and Trigonometric Technique Measurements of Hip-Joint Angle
| Technique, ° |
||||||
| Goniometric |
Trigonometric |
|||||
| Mean ± SD (95% Confidence Interval) |
Range |
Mean ± SD (95% Confidence Interval) |
Range |
|||
| Examiner |
Test |
Retest |
Test |
Retest |
||
| 1 | 14 ± 6 (12, 17) | 16 ± 5 (13, 18) | 20.0 | 31 ± 8 (28, 35) | 33 ± 8 (28, 35) | 33.0 |
| 2 | 17 ± 5 (15, 19) | 15 ± 6 (13, 17) | 23.0 | 33 ± 8 (30, 37) | 33 ± 9 (29, 36) | 33.7 |
The ICC values for intrarater (between-days) reliability of the GON technique were 0.51 and 0.54 and of the TRIG technique were 0.90 and 0.95 for examiners 1 and 2, respectively (Table 2). Interrater (between-examiners) ICCs for the GON technique were 0.65 and 0.30 and for the TRIG technique were 0.91 and 0.94 for days 1 and 2, respectively (Table 3). Standard error of measurement was consistently smaller for the TRIG technique than for the GON technique between days and between examiners (Tables 2 and 3).
Table 2.
Intrarater Intraclass Correlation Coefficients and Measurement Error Scores for the Goniometric and Trigonometric Techniques of Hip-Joint Angle
| Intrarater, Day 1 Versus Day 2 |
Intraclass Correlation Coefficient (3,1) (95% Confidence Interval) |
Standard Error of Measurement |
Coefficient of Variance, % |
| Examiner 1 | |||
| Goniometric technique | 0.51 (−0.19, 0.80) | 4 | 37 |
| Trigonometric technique | 0.90 (0.76, 0.96) | 2 | 25 |
| Examiner 2 | |||
| Goniometric technique | 0.54 (−0.05, 0.80) | 4 | 34 |
| Trigonometric technique | 0.95 (0.88, 0.98) | 2 | 25 |
Table 3.
Interrater Intraclass Correlation Coefficients and Measurement Error Scores for the Goniometric and Trigonometric Techniques
| Interrater, Examiner 1 Versus Examiner 2 |
Intraclass Correlation Coefficient (2,1) (95% Confidence Interval) |
Standard Error of Measurement |
Coefficient of Variance, % |
| Day 1 | |||
| Goniometric technique | 0.65 (0.20, 0.85) | 3 | 34 |
| Trigonometric technique | 0.91 (0.76, 0.97) | 2 | 24 |
| Day 2 | |||
| Goniometric technique | 0.30 (−0.75, 0.71) | 5 | 36 |
| Trigonometric technique | 0.94 (0.85, 0.97) | 2 | 26 |
The Bland-Altman plots with accompanying 95% limits of agreement illustrated the wide range of measurement scores for intrarater comparison using the GON technique over the 2 testing sessions (upper limit = 12.70°, lower limit = −11.79°; Figure 2A). Interrater comparisons also indicated a wide range of measurement scores for the GON technique between examiners (upper limit = 11.59°, lower limit = −13.23°; Figure 2B). For the TRIG technique, noticeably more agreement existed between testing sessions for intrarater comparisons (upper limit = 7.36°, lower limit = −6.56°; Figure 2C) and similarly for interrater comparisons (upper limit = 6.10°, lower limit = −9.53°; Figure 2D).
Figure 2.
A, Bland-Altman plot depicts differences in test-retest measurement scores on separate days for the goniometric technique plotted against mean scores for each participant. The difference in scores between day 1 and day 2 for the goniometric technique was 0.45° ± 6.25° (upper limit = 12.70°, lower limit = −11.79°). B, Bland-Altman plot depicts differences in test-retest measurement scores for each examiner for the goniometric technique plotted against mean scores for each participant. The difference in scores between examiner 1 and examiner 2 for the goniometric technique was −0.82° ± 6.33° (upper limit = 11.59°, lower limit = −13.23°). The difference in scores between examiner 1 and examiner 2 for the trigonometric technique was −1.72° ± 3.99° (upper limit = 11.59°, lower limit = −13.23°). C, Bland-Altman plot on separate days for the trigonometric technique plotted against mean scores for each participant. The difference in scores between day 1 and day 2 for the trigonometric method was 0.40° ± 3.55° (upper limit = 7.36°, lower limit = −6.56°). D, Bland-Altman plot depicts differences in test-retest measurement scores for each examiner for the goniometric technique plotted against mean scores for each participant. The difference in scores between examiner 1 and examiner 2 for the trigonometric technique was −1.72° ± 3.99° (upper limit = 6.10°, lower limit = −9.53°). a Indicates the 95% confidence interval upper limit (2 SDs). b Indicates the mean difference score. c Indicates the 95% confidence interval lower limit (2 SDs).
Single-factorial repeated-measures ANOVAs revealed no difference between days or examiners for either the GON protocol (F23 = 2.534, P > .05) or TRIG protocol (F23 = 1.184, P > .05). However, a repeated-measures ANOVA revealed a difference when we compared measurement scores between the GON and TRIG techniques (F23 = 91.408, P < .001).
DISCUSSION
The purpose of our study was to assess the intrarater and interrater reliability of the GON technique and compare it with the application of TRIG principles for assessing hip-extension ROM during the modified Thomas test. Our results indicated that the GON technique had poor to moderate reliability, whereas the TRIG technique had high intrarater and interrater reliability. This observation brings into question the use of goniometers and supports the use of TRIG principles to accurately assess hip-extension ROM during the modified Thomas test. The Bland-Altman plots indicated that the examiners were unbiased in scoring over the 2 testing sessions; however, a small bias existed whereby examiner 2 tended to score higher using the TRIG technique (Figure 2C). One key aspect of the Bland-Altman analysis is to establish the magnitude of the limits of agreement and determine whether they fit into acceptable error rates for the measurement being analyzed. The TRIG technique demonstrated smaller-magnitude limits of agreement, indicating less error; however, the level of acceptable error for either measurement technique has not been established.
In the clinical setting, a clinician sometimes must provide a quantitative measure of joint ROM to document patient progress. This reporting necessitates the accurate and reliable measurement of joint ROM so that any changes identified are true changes and not the result of measurement error. Often multiple clinicians are measuring joint ROM of a patient at different periods in a treatment protocol. This requires that the techniques used have evidence not only of intrarater but also of interrater reliability. Our results suggest that the use of linear measurement with TRIG principles would result in higher intrarater and interrater reliability in these settings.
Researchers have suggested that hip-flexor musculature extensibility or hip-extension ROM is a clinical indication of postural dysfunction and may affect human performance.15–17 The classic Thomas test is a common clinical-assessment protocol used to determine gross hip-flexor musculature extensibility and involves the patient lying supine on the treatment table with the upper part of the lower extremity on the table, such that the popliteal fossa contacts the edge of the plinth. The modified Thomas test involves the patient lying supine with the entire lower limb hanging off the plinth and is used specifically to measure rectus femoris musculature extensibility. Investigators have discussed the limitations of accurately marking GON measures of both the classic and modified Thomas tests. Peeler and Anderson18 assessed the intrarater and interrater reliability of the goniometer for measuring knee-flexion ROM during the Thomas test and noted only moderate reliability (ICCs = 0.67 and 0.50, respectively). These findings were similar to those of Gabbe et al19 and Sutlive et al,20 who observed moderate interrater reliability values of 0.69 and 0.66, respectively. Similar studies appear to have conflicting outcomes. Currier et al21 found poor interrater reliability when measuring hip-extension ROM using the goniometer (ICC = 0.20); whereas Clapis et al,11 Harvey,22 and Winters et al23 reported ICC values between 0.91 and 0.98. Given a lack of methodologic description in some of these studies, rationalizing the discrepancy between these results is difficult. The variability in outcomes, however, may shed light on the need to standardize the classic and modified versions of the Thomas test.
Our results conflict with those of researchers investigating the reliability of the GON technique when assessing hip-extension ROM using the modified Thomas test.11,19,22,23 Winters et al23 found that the universal goniometer showed high intrarater and interrater reliability (r = 0.86–0.95). Similarly, Clapis et al11 demonstrated that the GON technique had high interrater reliability (ICC = 0.92). One explanation for these conflicting outcomes may be examiner experience; Clapis et al11 reported that their examiners had an average of 18.5 years of clinical experience, but Winters et al23 did not identify examiner experience. In our study, the examiners had, on average, 4 years of professional experience in the clinical setting. The different experience levels of the examiners possibly explain the variation in the data between our study and other studies. If this assumption is correct, the reliability of the GON technique may be highly dependent on the examiner's experience level, and a long learning curve may be associated with mastery of the instrument.
Lea and Gerhardt1 noted limitations of the GON technique in assessing joint ROM. They discussed the ambiguities inherent in visually estimating the horizontal position of the long arm on the torso, aligning the distal goniometer arm with the long axis of the limb, and stabilizing the axis of rotation over the greater trochanter while stabilizing both arms of the goniometer. We identified similar limitations in our study, specifically related to ensuring the exact placement of the instrument arms while maintaining the landmark for the center fulcrum. Multiple sources of potential measurement error can occur with GON measurement of hip-extension ROM.
Our results further support those of previous researchers,8–10 who showed that the use of a tape measure or TRIG principles can produce reliable results when assessing ROM about the hip joint. Frost et al8 investigated the intrarater and interrater reliability of tape-measure measurements of trunk and pelvis ROM and found mixed results depending on the ROM measured. Hsieh et al9 observed the reliability of 3 measurement techniques, including a tape-measure method involving TRIG calculations, to assess hip-flexion ROM during the straight-leg–raise test. The tape-measure method produced an intrasessional α coefficient of .99 and intersessional α coefficient of .74. From this, they concluded that the lower intersessional reliability scores may have been due to the lack of standardization of landmarks in their methods. Frost et al8 incorporated a similar protocol to assess the straight-leg–raise test, measuring only the height of the lateral malleolus, and demonstrated low interrater reliability (r = 0.44). The authors acknowledged that their measurement protocol was difficult to perform due to the need to stabilize the pelvis, support the opposite lower extremity, and take the measurement to the floor. The high reliability scores in our study were likely due to the standardized identification of landmarks, whereby the examiners were instructed to mark the most posterior palpable aspect of the lateral epicondyle and not merely the lateral epicondyle itself. Furthermore, the opposite lower extremity was supported, and we used a stadiometer device to measure vertical displacement, requiring less manual contact with the participant and improving stabilization of the measurement apparatus.
Hsieh et al9 criticized the application of TRIG principles due to the possibility that a clinician would not have the time or the inclination to solve mathematical equations in a busy clinical setting. However, this research was conducted when personal computers and electronic medical records were not as available as they are today in many clinics. Data spreadsheets can be configured easily and automatically to perform TRIG calculations from the input of linear measurements. Anecdotally, our examiners believed that the TRIG technique was easier to perform, and they were more comfortable and confident in the results they were producing with it. It is fair to assume that, if clinicians require a quantitative measure of joint ROM and a method exists that is both reliable and less cumbersome, they will choose such a measure if the computation can be automated.
Establishing normative values of hip-extension ROM for specific populations is required to make diagnostic decisions regarding the functional ROM of a patient relative to the corresponding population. Harvey22 proposed that, in a population of athletes, mean hip-extension ROM during the modified Thomas test was 11.9°. Clapis et al11 presented mean values of −1.7° to −2.8° in young adults. In our study, the mean value observed for the GON technique when assessing hip-extension ROM was 15.4°. The variation in hip ROM values observed in these studies could be associated with various factors, such as the population from which the sample was taken, slight differences in the landmarks used for device placement, and positioning of the participant during the test. The variation among studies demonstrates the need to develop greater standardization of the GON protocol and the modified Thomas test procedure itself. The mean differences observed between the 2 measures applied in our study most likely are related to the differences in identifying landmarks between the 2 techniques. For example, the TRIG technique used the most posterior palpable aspect of the lateral epicondyle, whereas the standard GON technique involves aligning the arm of the goniometer with the midline of the thigh while using the lateral epicondyle as a visual landmark. The GON technique then will naturally produce smaller angles than the TRIG technique.
Some questions exist as to whether the population we chose may have affected the outcomes. We accepted only participants who were healthy, had no history of lower limb or back pathologic conditions, and were pain free. The reliability of the TRIG technique to assess individuals with orthopaedic or neurologic impairments or the elderly may not be similar to our findings. Error may be created in identifying landmarks due to excessive adipose tissue, bony pannus formation, or joint malformation. The relatively small sample of college-aged students also may limit its applicability to a larger, more heterogeneous population. Whereas the size of the sample could limit the application of our findings to other populations, the high correlation and good agreement shown with the TRIG technique implies that the correlation is quite strong and likely would be strengthened further with a larger test pool. A concern with studies using the Thomas test or modified Thomas test is that day-to-day variation can occur in the positioning of the participants.18 The level of control of the participant's body position in our study appears to be more rigorous than previously reported11,18,22,23; therefore, we do not believe this was a major limitation of our study.
To help in the stabilization of measurement, we used a portable stadiometer to measure displacement between the floor and the hip and knee landmarks. This piece of equipment may not be readily available at many clinics, so clinicians may have to use a tape measure instead. We believed that the stadiometer would provide the most accurate measure of height, resulting in less equipment-related measurement error. We recommend, therefore, that clinicians applying the TRIG technique invest in portable stadiometer devices because they are easy to use and more stable for measuring a variety of vertical displacements. In addition, we recommend externally supporting the untested lower extremity to improve the participant's relaxation and consistent placement; however, this may not always be practical in a clinical setting.
CONCLUSIONS
We investigated the reliability of the GON technique and a method using TRIG principles to assess hip-extension passive ROM. The low variation in measures supports use of the TRIG technique and provides evidence that applying TRIG principles to assess joint angles is reliable. The higher variation in measurements found with the GON technique suggests that this protocol has limitations that may be affected by clinical experience and the joint being measured. In future studies, researchers should consider investigating the application of TRIG techniques to other joints of the body, such as assessing ankle dorsiflexion and plantar flexion and shoulder ROM. Furthermore, researchers should investigate the reliability of these measures in individuals with orthopaedic or neurologic impairments.
ACKNOWLEDGMENTS
We thank all the participants who volunteered for this study and Richard Wakefield for his technical advice.
REFERENCES
- 1.Lea R, Gerhardt J. Range-of-motion measurements. J Bone Joint Surg Am. 1995;77(5):784–798. doi: 10.2106/00004623-199505000-00017. [DOI] [PubMed] [Google Scholar]
- 2.van de Pol RJ, van Trijffel E, Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother. 2010;56(1):7–17. doi: 10.1016/s1836-9553(10)70049-7. [DOI] [PubMed] [Google Scholar]
- 3.van Trijffel E, van de Pol RJ, Oostendorp RA, Lucas C. Inter-rater reliability for measurement of passive physiological movements in lower extremity joints is generally low: a systematic review. J Physiother. 2010;56(4):223–235. doi: 10.1016/s1836-9553(10)70005-9. [DOI] [PubMed] [Google Scholar]
- 4.Bierma-Zeinstra SM, Bohnen AM, Ramlal R, Ridderikhoff J, Verhaar JA, Prins A. Comparison between two devices for measuring hip joint motions. Clin Rehabil. 1998;12(6):497–505. doi: 10.1191/026921598677459668. [DOI] [PubMed] [Google Scholar]
- 5.Chapleau J, Canet F, Petit Y, Laflamme GY, Rouleau DM. Validity of goniometric elbow measurements: comparative study with a radiographic method. Clin Orthop Relat Res. 2011;469(11):3134–3140. doi: 10.1007/s11999-011-1986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters PG, Herbenick MA, Anloague PA, Markert RJ, Rubino LJ., III Knee range of motion: reliability and agreement of 3 measurement methods. Am J Orthop (Belle Mead NJ) 2011;40(12):E249–E252. [PubMed] [Google Scholar]
- 7.Rothstein JM, Miller PJ, Roettger RF. Goniometer reliability in a clinical setting: elbow and knee. Phys Ther. 1983;63(10):1611–1615. doi: 10.1093/ptj/63.10.1611. [DOI] [PubMed] [Google Scholar]
- 8.Frost M, Stuckey S, Smalley LA, Dorman G. Reliability of measuring trunk motions in centimeters. Phys Ther. 1982;62(10):1431–1437. doi: 10.1093/ptj/62.10.1431. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh CY, Walker JM, Gillis K. Straight-leg-raising test: comparison of three instruments. Phys Ther. 1983;63(9):1429–1433. doi: 10.1093/ptj/63.9.1429. [DOI] [PubMed] [Google Scholar]
- 10.Tanigawa MC. Comparison of the hold-relax procedure and passive mobilization on increasing muscle length. Phys Ther. 1972;52(7):725–735. doi: 10.1093/ptj/52.7.725. [DOI] [PubMed] [Google Scholar]
- 11.Clapis PA, Davis SM, Davis RO. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother Theory Pract. 2008;24(2):135–141. doi: 10.1080/09593980701378256. [DOI] [PubMed] [Google Scholar]
- 12.Atkinson G, Nevill AM. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26(4):217–238. doi: 10.2165/00007256-199826040-00002. [DOI] [PubMed] [Google Scholar]
- 13.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. [Google Scholar]
- 14.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 15.Glard Y, Launay F, Viehweger E, Guillaume JM, Jouve JL, Bollini G. Hip flexion contracture and lumbar spine lordosis in myelomeningocele. J Pediatr Orthop. 2005;25(4):476–478. doi: 10.1097/01.bpo.0000161099.46339.eb. [DOI] [PubMed] [Google Scholar]
- 16.Godges JJ, MacRae H, Longdon C, Tinberg C, MacRae PG. The effects of two stretching procedures on hip range of motion and gait economy. J Orthop Sports Phys Ther. 1989;10(9):350–357. doi: 10.2519/jospt.1989.10.9.350. [DOI] [PubMed] [Google Scholar]
- 17.Ingber RS. Iliopsoas myofascial dysfunction: a treatable cause of “failed” low back syndrome. Arch Phys Med Rehabil. 1989;70(5):382–386. [PubMed] [Google Scholar]
- 18.Peeler JD, Anderson JE. Reliability limits of the modified Thomas test for assessing rectus femoris muscle flexibility about the knee joint. J Athl Train. 2008;43(5):470–476. doi: 10.4085/1062-6050-43.5.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gabbe BJ, Bennell KL, Wajswelner H, Finch CF. Relability of common lower extremity musculoskeletal screening tests. Phys Ther Sport. 2004;5(2):90–97. [Google Scholar]
- 20.Sutlive TG, Lopez HP, Schnitker DE, et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. J Orthop Sports Phys Ther. 2008;38(9):542–550. doi: 10.2519/jospt.2008.2753. [DOI] [PubMed] [Google Scholar]
- 21.Currier LL, Froehlich PJ, Carow SD, et al. Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short-term response to hip mobilization. Phys Ther. 2007;87(9):1106–1119. doi: 10.2522/ptj.20060066. [DOI] [PubMed] [Google Scholar]
- 22.Harvey D. Assessment of the flexibility of elite athletes using the modified Thomas test. Br J Sports Med. 1998;32(1):68–70. doi: 10.1136/bjsm.32.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winters MV, Blake CG, Trost JS, et al. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: a randomized clinical trial. Phys Ther. 2004;84(9):800–807. [PubMed] [Google Scholar]