Abstract
Objective:
To present 3 cases of plantar-plate rupture and turf-toe injury in contact athletes at 1 university and to discuss appropriate diagnosis and treatment algorithms for each case.
Background:
Turf toe is a common injury in athletes participating in outdoor cutting sports. However, it has been used as an umbrella term to describe many different injuries of the great toe. In some cases, the injury can be so severe that the plantar plate and sesamoid apparatus may be ruptured. These patients may be better managed with surgery than with traditional nonoperative interventions.
Differential Diagnosis:
Turf toe, plantar-plate disruption, sesamoid fracture.
Treatment:
For stable injuries in which the plantar plate is not completely disrupted, nonoperative treatment with casting or a stiff-soled shoe, gradual weight bearing, and rehabilitation is the best practice. Unstable injuries require surgical intervention and plantar-plate repair.
Uniqueness:
Turf toe and injury to the first metatarsophalangeal joint are relatively common injuries in athletes, but few researchers have detailed the operative and nonoperative treatments of plantar-plate disruption in these patients. We examine 3 cases that occurred over 4 seasons on a collegiate football team.
Conclusions:
Turf toe represents a wide array of pathologic conditions involving the first metatarsophalangeal joint. Stress and instability testing are key components to assess in determining whether surgical intervention is warranted to restore optimal function. Stiffer-soled shoes or shoes with steel-plate insertions may help to prevent these injuries and are useful tools for protection during the rehabilitation period.
Key Words: metatarsophalangeal joint, great toe, football players
Turf toe is a common injury in athletes participating in outdoor cutting sports. Clanton and Ford1 reported that injury to the foot was the third leading cause of missed athletic participation. Damage to the metatarsophalangeal joint (MTPJ) represents a large percentage of those injuries. However, since Bowers and Martin2 coined the term turf toe, it has been a poorly studied topic of substantial controversy. They originally described turf toe as a sprain to the first MTPJ, but in many instances, the injury has been attributed incorrectly to various pathologic conditions involving the first ray.2 Turf toe historically has been managed nonoperatively with a stiff-soled shoe or short walking boot. Yet in severe cases, the plantar plate may be ruptured and disrupted. These injuries are easy to overlook on physical examination. Therefore, the purpose of our study was to review 3 cases of injury to the plantar plate of the first MTPJ in contact athletes and to focus on diagnosis and treatment of the more severe toe injuries.
CASE REPORTS
Case 1
A 21-year-old running back participating in National Collegiate Athletic Association (NCAA) Division I football injured his left great toe during his first carry of the game. He was cutting on a FieldTurf (FieldTurf, Calhoun, GA) playing surface when he planted his left foot and heard a “pop.” He had immediate pain and swelling. The toe was taped, and he attempted to return to play. However, he had continued pain and was unable to run effectively. On physical examination, he had a slight flexion contracture of the first MTPJ, which was passively correctable; instability with drawer testing; plantar ecchymosis; and complete loss of plantar-flexion strength when the flexor hallucis brevis (FHB) was isolated. Radiographs showed proximal retraction of the sesamoids (Figure 1). This retraction was amplified when stress radiographs were performed (Figure 2). Magnetic resonance imaging confirmed the diagnosis as a complete plantar-plate injury.
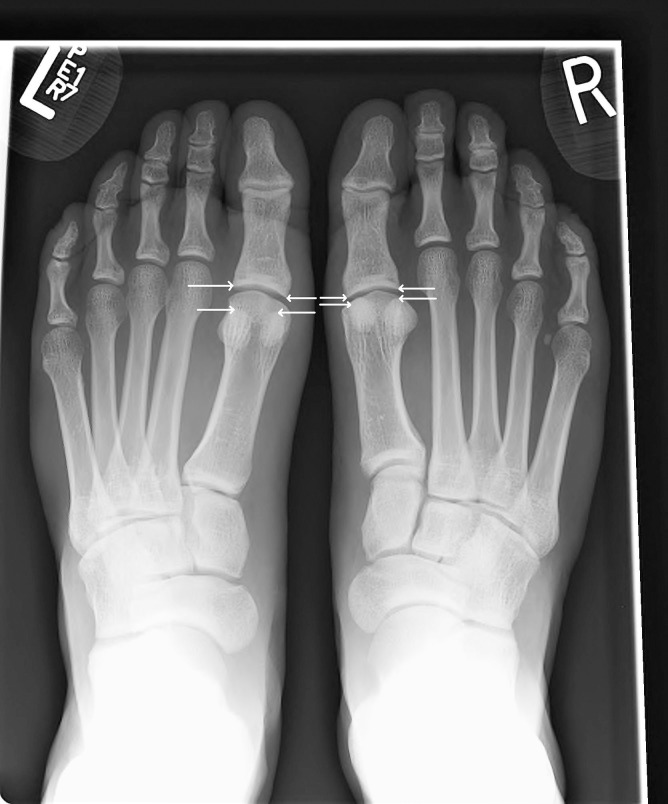
Figure 1.
Standing anteroposterior radiographic view of the feet. Note the increased distance between the first metatarsophalangeal joint and the sesamoids on the injured left foot versus the right foot.
Figure 2.
Stress anteroposterior radiographic view of the feet. Note the increase in distance between the first metatarsophalangeal joint space and the sesamoids on the injured left foot versus the right foot.
Surgery was recommended to restore the MTPJ anatomy. Repair of the plantar plate was performed using nonabsorbable 2-0 sutures through a medial approach. We found that the patient had a complete avulsion of the sesamoid apparatus, including both slips of the FHB. Therefore, we used a second plantar incision to repair the lateral aspect of the FHB tendon. The repair was carried out through drill holes in the sesamoid in 15° of plantar flexion. In addition, the patient had a small chondral impaction injury to the dorsum of the metatarsal head, so we performed a chondroplasty. We used an intraoperative stress test to assess stability.
Postoperatively, the patient was placed in a splint and then a cast, for a total of 4 weeks. Next, he was placed in a boot for 4 weeks and started a resisted–range-of-motion (ROM) program. He began plyometrics at 16 weeks. He returned to full participation in football at 6 months. The complete postoperative regimen is diagrammed in Table 1. At final follow-up, his dorsiflexion ROM was 63° in the involved toe and 70° in the contralateral toe.
Table 1.
Plantar-Plate Postoperative Rehabilitation Protocol for Cases 1 and 2
| Phase 1: 0–2 wk |
Phase 2: 2–4 wk |
Phase 3: 4–8 wk |
Phase 4: 8–12 wk |
Phase 5: 12–16 wk |
Phase 6: 16–24 wk |
|
| Special instructions | Bed rest. | Passive range-of-motion movements are gentle. Go slowly. | None | Discontinue walking boot. Use athletic shoe with carbon or steel insert to limit dorsiflexion. | Begin resisted plantar-flexion and dorsiflexion strengthening of metatarsophalangeal joint. | Full return to contact sports without restriction 2–6 mo after surgery. |
| Immobilization in 5°–15° of plantar flexion for 7–10 d to encourage scarring and discourage damage to sutures and reconstructed soft tissue. | ||||||
| Passive range of motion | None | In extension to neutral only. | Increase range of motion. | None | More aggressive passive metatarsophalangeal-joint plantar flexion and dorsiflexion. | None |
| Metatarsophalangeal and interphalangeal joints in flexion only. | Passive flexion and extension guided by tolerance to pain. | |||||
| Active range of motion | None | No active movements. | Gentle active extension to neutral only. | Active flexion and extension without resistance. | None | None |
| No active flexion until 8 wk. | ||||||
| Weight bearing | Non–weight bearing with crutches. | Non–weight bearing with crutches and walking boot for protection for 4 wk. | Partial weight bearing in walking boot. | Continue progression to full weight bearing. | Begin running by initiating a walk/jog program. | Continue running program. |
| Begin with 25 lb (11.25 kg) and increase. | ||||||
| 25 lb/wk (11.25 kg/wk) to full weight bearing. | Case 1: 12 wk | Full running and agility program 18–19 wk after surgery. | ||||
| Discontinue crutches at 6–7 wk after surgery. | Case 2: 16 wk | |||||
| Exercises | None | None | Weight shifts. | Single-legged balancing, core strengthening, stationary bicycling, and swimming without push off. | Continue previous exercises. | Continue previous exercises. |
| Core and hip strengthening. | Increase proprioception exercises. | Begin gradual plyometrics. | ||||
| Single-legged balancing exercises in boot 6–7 wk after surgery. | Add unstable surfaces (eg, Airex balance pad, mini-trampoline).a | |||||
| Avoid | None | None | All resistance at metatarsophalangeal and interphalangeal joints of great toe. | All eccentric contractions at metatarsophalangeal joint. | None | None |
| Running. | ||||||
| Active flexion of metatarsophalangeal and interphalangeal joints of great toe. | Extremes of great toe metatarsophalangeal-joint dorsiflexion. | |||||
| Additional concerns and instructions | Edema control. | Edema control. | Soft tissue mobilization for foot and ankle edema control. | Continue soft tissue mobilization. | Continue soft tissue mobilization. | Wear shoe modified with carbon or steel insert for 6 mo after full return. |
Airex AG, Sins, Switzerland.
Case 2
A 21-year-old NCAA offensive lineman was pass blocking on FieldTurf when he felt as if the sole of his shoe gave out. He had immediate difficulty with ambulation and was unable to continue playing. On physical examination, his foot was well aligned. He pointed directly to the undersurface of the MTPJ as the site of his pain. He had a completely deficient FHB on the left foot with tenderness through the extremes of FHB motion. Radiographs with the toe in dorsiflexion demonstrated that his sesamoids did not migrate distally as they did on the contralateral side (Figure 3). Magnetic resonance imaging showed abnormal signal of the plantar plate consistent with a complete disruption (Figure 4).
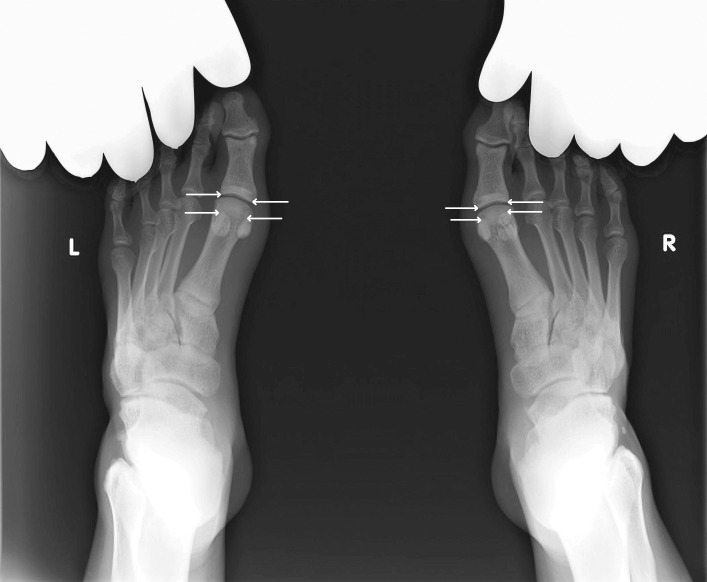
Figure 3.

Stress anteroposterior radiographic view of the feet. Note the increase in distance between the first metatarsophalangeal joint space and the sesamoids on the injured left foot versus the right foot.
Figure 4.
Magnetic resonance image of the toe demonstrating a complete tear of the plantar plate.
Given the positive findings on stress radiographs and his desire to continue participating in sports at a high level, we performed surgery. A medial incision revealed a complete disruption of the plantar plate and proximal retraction of the sesamoids (Figure 5). Scar tissue was debrided. We placed drill holes through the sesamoids and then sutured them to the distal plantar-plate tissue, which had remained intact. A Kirschner wire was used to hold the toe in approximately 10° of plantar flexion to relax the soft tissue repair. The pin was removed 2 weeks after surgery, and the athlete was placed in a cast. He began a progressive rehabilitation program at 6 weeks and a full running and agility program at 18 weeks. He returned to full participation in football at 6 months. The complete postoperative rehabilitation regimen is outlined in Table 1. At his last follow-up, his dorsiflexion ROM was 62° in the involved toe and 63° in the contralateral toe.
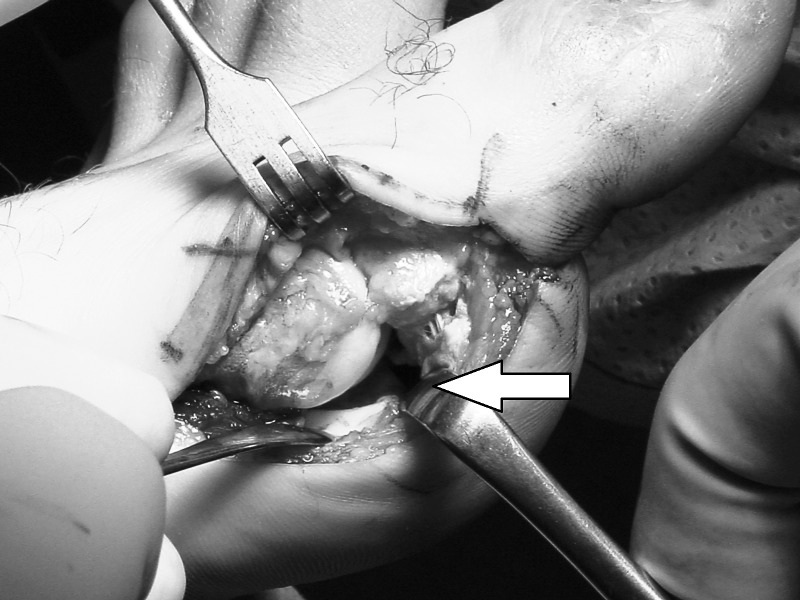
Figure 5.
Intraoperative photograph demonstrates complete tear of the plantar-plate apparatus.
Case 3
A 19-year-old NCAA linebacker injured his left great toe at practice. The patient reported that he felt as if his foot “stepped in a hole” while he was backpedaling during drills. He finished the next few repetitions but was unable to continue practicing. He had immediate pain, swelling, and weakness in the great toe. On physical examination, he pointed to the medial and plantar portions of the first MTPJ as the major sites of pain. His alignment was normal. The patient had some MTPJ flexor weakness, particularly when the FHB was isolated. A Lachman test was negative. He had substantial pain with resisted plantar flexion. Radiographs showed no sesamoid fractures, but he did have a slight 1- to 2-mm retraction of the sesamoids compared with the contralateral side (Figure 6). Magnetic resonance imaging showed 80% of the plantar plate was ruptured, with only a few fibers intact laterally. However, only 1 mm of retraction was present.
Figure 6.
Dorsiflexion stress anteroposterior radiographic view of the feet showing only minimal retraction of the sesamoids on the injured left foot.
Given the minimal retraction, we treated this injury nonoperatively. The patient was placed in a cast with the great toe in maximal plantar flexion to remove pressure from the plantar-plate apparatus and prevent further retraction of the sesamoids (Figure 7). We took serial radiographs to be certain that the sesamoids did not continue to retract. After 6 weeks, the patient was placed in a controlled–ankle-movement walking boot and began a gradual weight-bearing physical therapy program to regain motion and strength of the hallux. The prescribed postoperative rehabilitation is outlined in Table 2. Five months after the injury, his MTPJ extension and flexion ROM were 67° and 35°, respectively, on the injured side and 67° and 42°, respectively, on the uninjured side. His MTPJ flexion strength was 5/5, and he self-rated his flexion strength as excellent. At his last follow-up, the patient had achieved full functional status. He returned to participation in full-contact football with a carbon shoe insert.
Figure 7.
Cast with the great toe in plantar flexion.
Table 2.
Plantar-Plate Nonoperative Rehabilitation Protocol for Case 3
| Phase 1: 0–1 wk |
Phase 2: 1–5 wk |
Phase 3: 5–13 wk |
Phase 4: 13–18 wk |
Phase 5: 18–20 wk |
Phase 6: 20–22 wk |
|
| Special instructions | Diagnostic testing walking boot. | Cast immobilization with great toe in maximal plantar flexion to encourage scarring (see Figure 7). | Short walking boot. | None | None | Full return to contact sports without restriction 5 mo postinjury. |
| Discontinue walking boot at 8 wk. | ||||||
| Use athletic shoe with carbon or steel insert to limit dorsiflexion at 8 wk. | ||||||
| Passive range of motion | None | None | Plantar-flexion passive range of motion to metatarsophalangeal and interphalangeal joints. | None | None | None |
| Active range of motion | None | None | Plantar flexion without resistance from neutral. | None | None | None |
| Active flexion and extension of metatarsophalangeal joint without resistance at 12 wk. | ||||||
| Weight bearing | Non–weight bearing with crutches. | Non–weight bearing with crutches. | Partial weight bearing progressing to full weight bearing. | Begin running by initiating a walk/jog program with carbon-fiber shoe insert. | Continue running program. | None |
| Plantar-flexion and dorsiflexion strengthening of great toe using elastic resistance band and manual resistance. | Begin agility program. | |||||
| Exercises | None | None | Single-legged balancing in boot at 6–7 wk. | Stationary bicycling. | None | None |
| Swimming without push off. | ||||||
| Weight shifts at 8 wk. | Increase proprioception exercises. | |||||
| Core and hip strengthening. | Add unstable surfaces (eg, Airex balance pad, mini-trampoline).a | |||||
| Avoid | None | None | None | Toe raises. | None | None |
| Running that is not straight ahead only. | ||||||
| Cutting. | ||||||
| Additional concerns or instructions | Edema control. | None | Neuromuscular electrical stimulation to flexor hallucis brevis. | Continue soft tissue mobilization. | None | Wear shoe modified with carbon or steel insert for 12 mo after full return to participation. |
| Soft tissue mobilization to foot and ankle. |
Airex AG, Sins, Switzerland.
DISCUSSION
Anatomy
The first MTPJ is formed by the articulation of the curved head of the first metatarsal and the concave base of the proximal phalanx. The integrity of the first MTPJ is established primarily by the joint capsule, collateral capsular ligaments, and flexor-tendon complexes coursing medially and laterally.3,4 The medial and lateral collateral capsular ligaments provide varus and valgus stability. The medial flexor-tendon complex comprises the medial head of the FHB and the abductor hallucis tendon as they envelop the medial sesamoid to attach to the medial proximal phalanx. The lateral flexor-tendon complex comprises the lateral head of the FHB and the adductor hallucis tendon as they envelop the lateral sesamoid to attach to the lateral proximal phalanx. The sesamoids serve as a fulcrum to increase the lever arm of the FHB tendons and augment the plantar-flexion strength of the first MTPJ.5 The flexor hallucis longus (FHL) tendon courses in a separate sheath between the sesamoids and attaches to the distal phalanx. The plantar plate is a fibrocartilaginous structure formed by the thickened plantar-joint capsule and medial and lateral flexor-tendon complexes that courses from the first metatarsal head and attaches to the proximal phalanx. These soft tissue stabilizers allow for approximately 50° of dorsiflexion and 30° of plantar flexion.4
Injury
Classic turf toe represents a sprain of the MTPJ due to a hyperextension injury. Usually, a plantar-flexed foot with an extended or dorsiflexed hallux against a ground surface sustains an axial load, often due to someone falling on the back of the foot in the vulnerable position. The plantar-plate complex is designed to resist dorsiflexion of the first MTPJ, but these tissues can be torn, with the degree of damage dependent on the overall severity of the injury and forces to the joint. A first-degree sprain represents only a microtear of the ligament; the first MTPJ is still competent and can resist dorsiflexion. However, a frank dorsal dislocation typically results in complete disruption of many of these important plantar structures, including, but not limited to, the plantar plate.
The adductor or abductor attachments or collateral ligaments may be torn if a lateral load has been placed on the toe, as often happens during cutting movements. This can result in a traumatic bunion or hallux valgus or varus, depending on the direction of the force.6
In lieu of or in addition to an isolated soft tissue injury, the sesamoids can be injured.7–10 They can sustain fractures that may be displaced or injuries to the synchondrosis if the sesamoids are bipartite or tripartite. Given that the sesamoids are intra-articular bones, they may sustain injuries to their articular surfaces as well. These first MTPJ injuries also can include die-punch injuries, shear injuries, or even bone marrow edema analogous to what can occur in the knee with an anterior cruciate ligament tear. Such damage can produce a loose body within the joint itself. Any of these exacerbating factors (eg, bone marrow edema, loose body) may lead to chronic sequelae, such as stiffness, early MTPJ arthrosis, and pain. Furthermore, injury to the plantar plate and FHB tendons may decrease first MTPJ competence and push-off strength, which can affect performance, particularly in sprinters and elite-level athletes participating in cutting sports.11–14
Diagnosis
Diagnostic tools are described in Table 3. Patients with first MTPJ hyperextension injuries almost always report pain focused at the joint. This injury frequently inhibits further participation in athletics. Typically, the athlete describes a mechanism of injury that includes an acute first MTPJ hyperextension event or recalls sustaining a compressive axial load while the foot was plantar flexed and the hallux was dorsiflexed. The patient presents with swelling and later with ecchymosis about the first MTPJ. On physical examination, both passive and active ROM must be assessed. Frank dislocation of the first MTPJ is possible and is not always reducible. Strength also should be assessed with a focus on the FHL and FHB. The FHL tendon is responsible for flexing the MTPJ but attaches to the distal phalanx and also flexes the interphalangeal joint. Isolated FHB strength assessment should be attempted by stabilizing the interphalangeal joint in neutral position and then instructing the patient to flex the MTPJ against resistance applied to the proximal phalanx (Figure 8). Minimal strength of the FHB and pain with this maneuver suggest instability and a more substantial injury. Stability testing should be performed by examining anteroposterior translation and varus-valgus stability. The Lachman test for the first MTPJ is conducted by stabilizing the first metatarsal superiorly and inferiorly with 1 hand while applying an anterior and posterior translational force to the proximal phalanx to feel for dorsal or plantar subluxation. A positive Lachman test demonstrates anteroposterior instability.
Table 3.
Diagnostic Tools
| Tool |
Use |
| History | Mechanism of injury |
| Ability to return to play | |
| Level of pain | |
| Chronicity | |
| Physical examination | Swelling and pain |
| Lachman test for anteroposterior instability | |
| Varus/valgus instability | |
| Passive and active range of motion | |
| Flexor hallucis longus strength | |
| Isolated flexor hallucis brevis strength | |
| Imaging | |
| Bilateral standing radiograph | Compare sesamoid retraction |
| Bilateral standing stress radiograph | Compare sesamoid retraction |
| Computed tomography scan | Evaluate sesamoid fracture |
| Magnetic resonance imaging | Evaluate soft tissue integrity and articular cartilage damage |
Figure 8.
Isolated strength testing of the flexor hallucis brevis by stabilizing the hallux interphalangeal joint.
If the patient develops persistent pain and swelling accompanied by decreased strength or restricted or crepitant ROM, then further evaluation is warranted. Weight-bearing radiographs should be taken to look for fracture and at overall alignment. Contralateral views should be obtained for comparison when proximal sesamoid retraction, a possible sesamoid fracture, or a bipartite sesamoid is present. The total volume of fracture fragments should equal that of an intact sesamoid versus a bipartite sesamoid; the latter may have a larger total volume.15,16 A stress test is recommended to confirm instability. Rodeo et al7 advocated stress radiography with the proximal phalanx dorsiflexed.
McCormick and Anderson13 recommended using fluoroscopy to assess real-time motion of the toe to determine whether the sesamoid apparatus is intact. If the sesamoids do not move the same distance when compared with the contralateral side, a disruption of the plantar plate is possible. A computed tomography scan may be obtained to further evaluate the size and comminution of the fragments. Magnetic resonance imaging is usually more helpful because it can delineate injuries to the collateral ligaments and plantar plate and demonstrate injuries to the articular surface if present.
Treatment
To appropriately manage these injuries, we divide them into 2 groups: stable and unstable. For our purposes, stable injuries are defined by a change of less than 2 mm on dorsiflexion stress radiographs in proximal retraction of the sesamoids of the affected first MTPJ compared with the contralateral first MTPJ. Although other injuries, such as fractures and articular cartilage injuries, may occur, we use the aforementioned guide to determine whether an injury to the plantar plate should be managed aggressively. For stable injuries, symptomatic treatment is warranted and may include a walking boot and protected weight bearing. If the capsule has a substantial injury as seen on magnetic resonance imaging but no instability on provocative testing, then casting for 4 to 6 weeks with the MTPJ in plantar flexion may be prudent. This casting will allow the tissues to heal without undue strain on the plantar-ligament complex, and it ultimately may allow the injury to heal in a more anatomic position and decrease the risk of long-term morbidity.
For unstable injuries, the treatments are less well defined. Fractures have been treated in a variety of ways, including nonoperatively. For displaced fractures in which the plantar-plate apparatus has been rendered incompetent, some authors3,13,14 have proposed excising the smaller fragment and repairing the plantar plate, which can be accomplished with or without augmentation. McCormick and Anderson3,12 proposed augmentation using the abductor hallucis tendon. However, it is important to balance the forces across the MTPJ so that a hallux valgus is not created. Thus, they also suggested a modified McBride tenotomy of the adductor to account for this. Some authors17 have excised the sesamoid completely. Other authors3 have proposed open reduction and internal fixation, but given the small size of the sesamoid, many have avoided this practice.18,19 However, with current instrumentation, internal fixation can be attained. Specifically, small (1.3-mm) screws, which usually are found in modular hand surgery sets, have been used with or without bone grafting to address this problem.20 In the chronic setting (ie, sesamoid nonunions), a bone graft should be used.21 This technique has been reported with and without the use of instrumentation.
If the plantar plate has been ruptured and stress testing shows that the sesamoid apparatus does not move symmetrically with the contralateral side, operative management should be considered. Unfortunately, we could not find published prospective studies in which the researchers examined plantar-plate rupture injuries in athletes. Conventional wisdom suggests that patients with instability will have worse long-term outcomes and difficulty with return to sport if treated nonoperatively. Long-term disability manifested by MTPJ stiffness, arthrosis, and pain has been reported. However, the definitive criteria for surgical intervention based on objective radiographic findings and physical examination testing are still being investigated. Waldrop et al22 found that an increase of 3 mm or more in the distance from the sesamoid to the proximal phalanx on a lateral-dorsiflexion stress radiograph predicted a severe injury to the plantar plate in cadaveric models that would require surgical intervention in a patient. McCormick and Anderson13 constructed a list of surgical indications for treating a turf-toe injury, but these indications have not been studied in a controlled trial setting. The topic of operative versus nonoperative treatment for plantar-plate injuries requires more thorough research to establish definitive guidelines for intervention.
In cases of instability, some authors3 have proposed primary repair of the plantar plate. When the injuries are addressed late, delayed surgical repair can be difficult because the plantar plate is attached to the FHB tendons, which retract it proximally.13 These forces can prevent the plate from healing in an anatomic position. Furthermore, this area can scar and make it difficult to determine normal tissue planes. In these cases, suture anchors frequently are needed to properly affix the tissue back to the proximal phalanx.
CONCLUSIONS
Injuries to the first MTPJ flexor apparatus are common and can be quite disabling. As demonstrated in our patients, they represent a wide array of pathologic conditions. Simply labeling these injuries as turf toe is neither accurate nor predictive of the appropriate treatment that should be pursued. As with any injury, paying close attention to the history and the mechanism of injury provides important clues to the diagnosis. These injuries frequently occur on artificial playing surfaces due to the increased traction at the shoe-surface interface. Moreover, stiffer-soled shoes or shoes with steel-plate insertions may help prevent these injuries and are useful tools for protection during the rehabilitation period.
Diagnostically, special consideration should be given to the strength, ROM, and stability examinations, as well as to the ability to return to play (Table 3). Athletes with more extensive injuries typically have more difficulty returning to play and need further examination of their symptoms, which may include functional disability and difficulty with pushing off and running. Furthermore, patients should be referred to physicians with experience treating these injuries. Even after radiographic imaging, fractures may be mistaken for bipartite sesamoids and therefore need to be evaluated. Stress and instability testing are key components to assess when determining whether surgical intervention is warranted to restore optimal function. Accurate and timely diagnosis and treatment can allow for full return to activity for many of these athletes.
REFERENCES
- 1.Clanton TO, Ford JJ. Turf toe injury. Clin Sports Med. 1994;13(4):731–741. [PubMed] [Google Scholar]
- 2.Bowers KD, Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8(2):81–83. [PubMed] [Google Scholar]
- 3.McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health. 2010;2(6):487–494. doi: 10.1177/1941738110386681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodeo SA, O'Brien S, Warren RF, Barnes R, Wickiewicz TL, Dillingham MF. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med. 1990;18(3):280–285. doi: 10.1177/036354659001800311. [DOI] [PubMed] [Google Scholar]
- 5.Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop Relat Res. 1996;325:209–217. doi: 10.1097/00003086-199604000-00025. [DOI] [PubMed] [Google Scholar]
- 6.Fabeck LG, Zekhnini C, Farrokh D, Descamps PY, Delince PE. Traumatic hallux valgus following rupture of the medial collateral ligament of the first metatarsophalangeal joint: a case report. J Foot Ankle Surg. 2002;41(2):125–128. doi: 10.1016/s1067-2516(02)80037-0. [DOI] [PubMed] [Google Scholar]
- 7.Rodeo SA, Warren RF, O'Brien SJ, Pavlov H, Barnes R, Hanks GA. Diastasis of bipartite sesamoids of the first metatarsophalangeal joint. Foot Ankle. 1993;14(8):425–434. doi: 10.1177/107110079301400801. [DOI] [PubMed] [Google Scholar]
- 8.Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003;24(2):137–141. doi: 10.1177/107110070302400207. [DOI] [PubMed] [Google Scholar]
- 9.Mouhsine E, Leyvraz PF, Borens O, Ribordy M, Arlettaz Y, Garofalo R. Acute fractures of medial and lateral great toe sesamoids in an athlete. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):463–464. doi: 10.1007/s00167-003-0472-6. [DOI] [PubMed] [Google Scholar]
- 10.Pagenstert GI, Valderrabano V, Hintermann B. Medial sesamoid nonunion combined with hallux valgus in athletes: a report of two cases. Foot Ankle Int. 2006;27(2):135–140. doi: 10.1177/107110070602700212. [DOI] [PubMed] [Google Scholar]
- 11.Coughlin MJ, Kemp TJ, Hirose CB. Turf toe: soft tissue and osteocartilaginous injury to the first metatarsophalangeal joint. Phys Sportsmed. 2010;38(1):91–100. doi: 10.3810/psm.2010.04.1766. [DOI] [PubMed] [Google Scholar]
- 12.McCormick JJ, Anderson RB. Rehabilitation following turf toe injury and plantar plate repair. Clin Sports Med. 2010;29(2):313–323. doi: 10.1016/j.csm.2009.12.010. ix. [DOI] [PubMed] [Google Scholar]
- 13.McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin. 2009;14(2):135–150. doi: 10.1016/j.fcl.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Watson TS, Anderson RB, Davis WH. Periarticular injuries to the hallux metatarsophalangeal joint in athletes. Foot Ankle Clin. 2000;5(3):687–713. [PubMed] [Google Scholar]
- 15.Anwar R, Anjum SN, Nicholl JE. Sesamoids of the foot. Curr Orthop. 2005;19(1):40–48. [Google Scholar]
- 16.Munuera PV, Dominguez G, Reina M, Trujillo P. Bipartite hallucal sesamoid bones: relationship with hallux valgus and metatarsal index. Skeletal Radiol. 2007;36(11):1043–1050. doi: 10.1007/s00256-007-0359-6. [DOI] [PubMed] [Google Scholar]
- 17.Richardson EG. Injuries to the hallucal sesamoids in the athlete. Foot Ankle. 1987;7(4):229–244. doi: 10.1177/107110078700700405. [DOI] [PubMed] [Google Scholar]
- 18.Bichara DA, Henn RF, III, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int. 2012;33(9):704–706. doi: 10.3113/FAI.2012.0704. [DOI] [PubMed] [Google Scholar]
- 19.Blundell CM, Nicholson P, Blackney MW. Percutaneous screw fixation for fractures of the sesamoid bones of the hallux. J Bone Joint Surg Br. 2002;84(8):1138–1141. doi: 10.1302/0301-620x.84b8.13064. [DOI] [PubMed] [Google Scholar]
- 20.McCormick JJ, Anderson RB. Surgical correction of the recalcitrant turf toe. Tech Foot Ankle Surg. 2013;12(1):29–38. [Google Scholar]
- 21.Anderson RB, McBryde AM., Jr Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18(5):293–296. doi: 10.1177/107110079701800509. [DOI] [PubMed] [Google Scholar]
- 22.Waldrop NE, III, Zirker CA, Wijdicks CA, Laprade RF, Clanton TO. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot Ankle Int. 2013;34(3):403–408. doi: 10.1177/1071100712464953. [DOI] [PubMed] [Google Scholar]