Abstract
BACKGROUND
In 2005, the Centers for Disease Control and Prevention (CDC) funded 5 sites as part of the Colorectal Cancer Screening Demonstration Program (CRCSDP) to provide colorectal cancer screening to low-income, uninsured, and underinsured individuals. Funded sites experienced unexpected challenges in recruiting patients for services.
METHODS
The authors conducted a longitudinal, qualitative case study of all 5 sites to document program implementation, including recruitment. Data were collected during 3 periods over the 4-year program and included interviews, document review, and observations. After coding and analyzing the data, themes were identified and triangulated across the research team. Patterns were confirmed through member checking, further validating the analytic interpretation.
RESULTS
During early implementation, patient enrollment was low at 4 of the 5 CRCSDP sites. Evaluators found 3 primary challenges to patient recruitment: overreliance on in-reach to National Breast and Cervical Cancer Early Detection Program patients, difficulty keeping colorectal cancer screening and the program a priority among staff at partnering primary care clinics responsible for patient recruitment, and a lack of public knowledge about the need for colorectal cancer screening among patients. To address these challenges, site staff expanded partnerships with additional primary care networks for greater reach, enhanced technical support to primary care providers to ensure more consistent patient enrollment, and developed tailored outreach and education.
CONCLUSIONS
Removing financial barriers to colorectal cancer screening was necessary but not sufficient to reach the priority population. To optimize colorectal cancer screening, public health practitioners must work closely with the health care sector to implement evidence-based, comprehensive strategies across individual, environmental, and systems levels of society.
Keywords: colorectal cancer screening, program evaluation, qualitative evaluation, program implementation, patient recruitment
INTRODUCTION
Colorectal cancer is the second most common type of cancer diagnosed in the United States and the second most deadly among both men and women.1,2 Despite the methods available to detect and prevent colorectal cancer in its early stages, many Americans remain unscreened.2 In 2010, US screening prevalence was just over 65%, with large variations across states.2 These data suggest significant disparities in screening prevalence among those without health insurance and those with lower household incomes.2–5 Racial and ethnic minorities and those with lower levels of education also report lower rates of colorectal cancer screening.6
Fortunately, routine screening has been found effective in reducing colorectal cancer incidence and mortality.7,8 When colorectal cancer is detected at the earliest stage, the 5-year survival rate is greater than 90%, compared with a 12% survival rate for those diagnosed with metastatic disease.9 These outcomes make colorectal cancer screening a critical component in the prevention and early detection of colorectal cancer, especially because endoscopy screening methods may prevent disease entirely if precancerous lesions are found and removed.
To assess the feasibility of providing community-based colorectal cancer screening to the US public, in 2005 the Centers for Disease Control and Prevention (CDC) initiated a pilot service delivery program, the Colorectal Cancer Screening Demonstration Program (CRCSDP).10 Over the course of 4 years, the CDC provided more than $8 million in funding to 5 sites across the country to support the development and implementation of the first federally funded and organized public health colorectal cancer screening program. This was modeled to some extent after the CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEPD)11 referred throughout this paper as the Breast and Cervical Program; funded sites were charged with developing service delivery programs to offer high-quality colorectal cancer screening at no cost to patients. Sites were required to offer screening using the modalities and intervals recommended by the US Preventive Services Task Force.12 The overall priority population for the program included low-income, uninsured, and underinsured men and women ages 50 to 64 years at average risk for colorectal cancer. Sites were permitted to fine-tune selection based on community composition and burden. A more detailed description of the CRCSDP can be found elsewhere in this Supplement to Cancer.13
The catchment areas for the CRCSDP were the city of Baltimore, Maryland; greater Seattle, Washington; St. Louis, Missouri; Suffolk County, New York; and the state of Nebraska. Along with funding screening tests and procedures, programs conducted activities to support high-quality screening and facilitate patient adherence. Working closely with their contracted provider sites, staff collected data from patients to add to the larger evaluation of the 5 CRCSDP sites. Patient recruitment was essential to ensuring success of the program and effective use of federal funds. Details of the program implementation models used by each of the 5 sites have been published elsewhere.14
As part of a broad evaluation of the CRCSDP, we conducted a longitudinal, multiple-case study to assess program implementation.15 Use of qualitative methods facilitated documentation of the program implementation processes, including related challenges and strategies used to address them, over the course of the demonstration project. Given that qualitative data are both experiential and empirical, this study served our purpose of exploring why and how events occurred during program implementation and interpreted outcomes-focused quantitative data presented both within this article (Figures 1 and 2), and across articles within this supplement to Cancer.13,16 What the qualitative data provide are systematic accounts of what occurred at the sites from the perspectives of those running the program. In this report, we discuss an unanticipated challenge that emerged for the CRCSDP sites: recruiting eligible men and women for colorectal cancer screening.
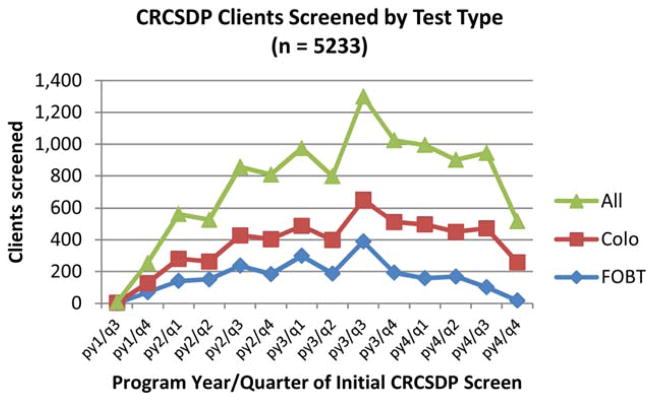
Figure 1.
Number of Colorectal Cancer Screening Demonstration Program (CRCSDP) participants screened by test type and program year (py), 2006–2009.* *The decline in screening within the last 2 quarters is attributed to closing out the program. Data are shown on initial screens only, excluding any repeat procedures. Colo indicates colorectal screening; FOBT, fecal occult blood test.
Figure 2.
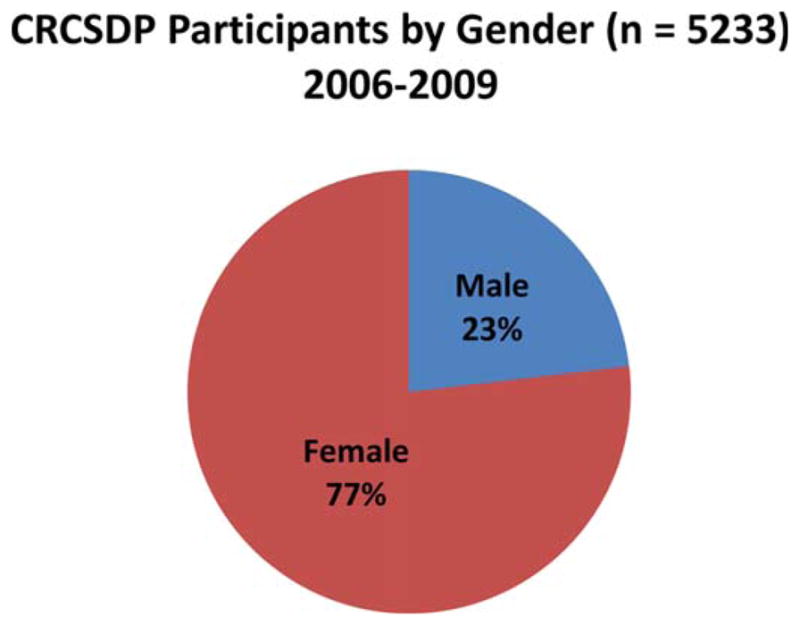
Distribution of Colorectal Cancer Screening Demonstration Program (CRCSDP) participants by sex, 2006–2009.
Patient data collected as part of our overall evaluation indicate that patient recruitment for the program was slow during early screening implementation.13 In general, program staff found recruiting patients for the CRCSDP was difficult. Consequently, sites made programmatic adjustments, adding new strategies or revising existing ones, to boost enrollment. We describe the initial recruitment strategies employed by sites, subsequent recruitment challenges, and programmatic adjustments made to improve patient recruitment for colorectal cancer screening. We divide the remainder of the article into sections describing the relevant literature and research methods, results from the 5 sites, and discussion and conclusions.
In addition to cost and health insurance status, other researchers have identified other significant barriers to colorectal cancer screening.2–5 At the individual level, barriers to screening include lack of knowledge and awareness of the need for screening, fear of the procedure or unfavorable results, lack of trust in the medical system, and fatalistic beliefs about cancer in general.10,17–21 Results from qualitative studies, in particular, have revealed barriers that are rooted in misconceptions about the need for screening.17,18,22 For instance, patients are often confused about risk factors for colorectal cancer and unaware that both men and women are susceptible.17,18 In addition, many people lack the knowledge that, if identified early, colorectal cancer treatment is highly effective in reducing morbidity and mortality.
Other barriers to colorectal cancer screening were identified throughout the literature as occurring at the environmental and systems levels.17,20 Among environmental barriers for patients are securing transportation, receiving adequate time off from work to complete screening, and identifying an available friend or family member to escort the patient to and from the procedure.19,20,23 Systems-level barriers exist within the larger health care system and are related to patients’ interactions with providers.20 The most commonly cited systems-level barrier is the absence of providers’ recommendations for screening to patients.17,18,20,24–26 Even if a provider does make a recommendation for screening, the patient may still not have an adequate understanding of how to complete the process.17,19,20 Multiple factors contribute to these systems-level barriers, such as high patient volume, competing comorbidities of patients, and provider beliefs that patient compliance with the recommendation is unlikely.17,18,20,24–26
Complementary to research identifying patient barriers to screening, intervention studies have been conducted to test strategies aimed specifically at improving colorectal cancer screening adherence. In these studies, several groups have looked at the effectiveness of media campaigns, client and provider reminders, group education, and patient navigation.23,27–31 Much of the intervention research on colorectal cancer screening adherence is summarized in the Guide to Community Preventive Service (Community Guide), developed by the independent, non-federal Task Force on Community Preventive Services.32 In the Community Guide, systematic literature reviews are published on health topics to identify effective public health interventions that will improve health and prevent disease. Based on the most recent reviews, the Community Guide recommends several strategies with a robust evidence base including patient reminders, provider reminders, and the use of small media materials such as brochures and letters. Currently, recommendations of the Community Guide for colorectal cancer screening are almost entirely based on studies of fecal occult blood testing (FOBT) screening. Insufficient evidence exists to make similar recommendations for other screening modalities such as colonoscopy.
Unlike the research we report, studies such as those reviewed for the Community Guide, emphasize outcomes and impact only, and often neglect program processes and the experiences of staff that might help to explain the outcomes. We turn next to our approach to examining patient recruitment for colorectal cancer screening.
MATERIALS AND METHODS
We conducted a longitudinal, multiple-case study of the CRCSDP over the 4-year program as part of an evaluation of program implementation. Each of the 5 CRCSDP sites was included in the analysis, each site representing a unique case.15,33 Qualitative methods included semi-structured interviews with 100 program stakeholders, 125 participant observations, and reviews of 19 documents. The selection of interview participants was based on purposeful sampling.34 Data were analyzed within and across cases using systematic coding and the constant comparative method.35 The first author developed and applied an initial codebook to the data using the software program Atlas.ti.36 The team cross-checked the codes and developed patterns using inductive reasoning.37 These patterns were confirmed by member checking with study participants. A more detailed summary of the qualitative case study methods is included elsewhere in this Supplement to Cancer.38
RESULTS
Results from this multiple-case study reflect the process learning by sites about patient recruitment for screening through the CRCSDP. We begin by describing the initial recruitment strategies sites used and follow with 3 primary recruitment challenges we identified during analysis. Finally, we describe the programmatic adjustments sites made to improve patient recruitment.
Initial Recruitment Strategies
Before screening implementation, many site staffs anticipated being overwhelmed by the demand for free colorectal cancer screening services offered by their programs, particularly because screening resources were limited and their programmatic infrastructure was new. In attempting to align supply and demand, many site staff believed that relying on the participation of women in the existing Breast and Cervical Program (ie, in-reach) and using small media materials from national public awareness campaigns would be sufficient to recruit patients for screening. Hindsight revealed the need for planning more aggressive recruitment activities. Table 1 identifies the initial recruitment strategies used at sites to elicit interest in colorectal cancer screening and recruit patients into the program.
TABLE 1.
Original Recruitment Strategies by Site for CDC’s Colorectal Cancer Screening Demonstration Program (CRCSDP)
| Site—Test Type | Original Recruitment Strategies |
|---|---|
| Baltimore city, Maryland—colonoscopy |
|
| St. Louis, Missouri—switched from fecal occult blood test (FOBT) to colonoscopy |
|
| Nebraska—FOBT |
|
| Suffolk County, New York—colonoscopy |
|
| Greater Seattle—FOBT and colonoscopy based on shared decision-making process |
|
Recruitment Challenges
Once recruitment strategies were implemented and screening was initiated, patient enrollment was significantly lower than anticipated at sites. Figure 1 illustrates screening trends by quarter over the course of program implementation, indicating a gradual incline, but slow start to patient recruitment. (Screening rates necessarily declined during the last year of funding, as programs approached conclusion.) A site staff member from the Baltimore city site described the slow start succinctly: “We thought we would open an endoscopy suite, and the people would come running down the hallway…and that simply didn’t happen.” Provider staff across sites indicated they had difficulty eliciting patients’ interest in the program. Furthermore, enrollment forms sent by sites to Breast and Cervical Program patients and their male counterparts were not returned in the volume anticipated, prompting site staff to express concern about the sex imbalance (Fig. 2) among patients recruited into the CRCSDP. A site staff member from Nebraska summarized the overall situation: “Just because you build it, doesn’t mean people will come.”
Consistent with problems and inefficiencies identified by program staff, our analysis revealed 3 major factors accounting for sites’ initial recruiting challenges: primary dependence by sites on in-reach to Breast and Cervical Program patients; difficulty integrating the CRCSDP among provider site staff responsible for patient enrollment; and patients’ knowledge, attitudes, and beliefs about colorectal cancer screening.
Primary dependence on in-reach to Breast and Cervical Program patients
Staff at 4 of the 5 sites initially relied on in-reach to a large volume of patients already participating in other screening programs with similar age, income, and insurance eligibility requirements, particularly the Breast and Cervical Program. Launched in 1990, the Breast and Cervical Program offers free or reduced-cost primary care office visits including mammograms and Pap smears to women with low income and lacking adequate insurance.11 The 4 CRCSDP sites that participated in the Breast and Cervical Program viewed the large number of screening-adherent, Breast and Cervical Program-enrolled patients as a readily available “natural audience” for colorectal cancer screening. Strategies to recruit Breast and Cervical Program patients for the CRCSDP in Nebraska and St. Louis included sending postcards with information about the program, along with program enrollment forms, to women, including extra forms for their male counterparts. Baltimore city and greater Seattle engaged provider site staff, including case managers, to identify and contact their Breast and Cervical Program patients for enrollment in the CRCSDP.
Although some Breast and Cervical Program patients were successfully recruited for screening during early implementation, many more did not respond to efforts to enroll them. A staff member from Baltimore city expressed disappointment with the results of early recruitment efforts that relied on Breast and Cervical Program patients for enrollment in the CRCSDP.
Everybody thought we’re going to have plenty of Breast and Cervical Program clients and we didn’t need to do anything…then no one came to the party, you know. They [Breast and Cervical Program patients] are neither all over 50, nor are they all interested or eligible for some reason.…So, I don’t think that was as successful as we had hoped. For every nine people we talked to, one person was interested in the program.
This disappointment was echoed across the 4 sites that participated in the Breast and Cervical Program. CRCSDP site staff found themselves in a delicate position—to advertise the program to enough patients to continuously meet program screening goals while limiting interest to avoid overwhelming systems and resources.39 Overall, site staff believed that relying on the large pool of Breast and Cervical Program patients would provide a sufficient number of patients for colorectal cancer screening, given available screening resources. In addition, staff expressed concern that more aggressive recruitment efforts would lead to screening demand that sites would be unable to meet. Although in-reach to Breast and Cervical Program patients was an initial strategy that resulted in modest recruitment success, most sites quickly realized that relying on this pool of patients alone was inadequate to reach screening capacity.
Difficulty integrating the CRCSDP at provider sites
Difficulty integrating the CRCSDP at provider sites was also a major contributing factor to low recruitment for several programs. Program sites contracted with health care networks such as primary and specialty care clinics and community health centers to recruit patients into their programs. Interviewees suggested that provider site staff did not always remember to enroll eligible patients into the CRCSDP. One clinic staff person said, “A lot of people were being missed. I would get [medical] charts and check, and I’d be, like, this [patient] would have been the perfect candidate; they had no insurance [meaning that the patient was not enrolled in the program].” Three factors seemed to contribute to provider sites’ difficulties in integrating the new program: heavy demand on primary care providers and support staff, especially in indigent-care facilities, such as those participating in the CRCSDP; patients with acute health issues requiring immediate attention, leaving little time to discuss preventive care; and provider site staff discomfort with discussing colorectal cancer screening with patients.
In regard to demands on health care staff, interviewees suggested that colorectal cancer screening messages can quickly lose priority given the hectic environment of a community health center, resulting in haphazard and inconsistent recruitment. A staff member at the greater Seattle site said, “Providers get slammed by schedules and add-ons and walk-ins and, you know, it’s hard to keep everything present if that’s not the issue or complaint that the patient is coming in for.” Consequently, without a systematic approach to ensure recruitment of eligible patients, many potential participants were missed.
Similarly, given the limited time for patient-provider interaction, colorectal cancer screening messages often became low priority when providers and support staff were faced with patients experiencing acute medical needs, including existing comorbidities such as diabetes and heart disease. Another site staff member referred to this, saying, “Our clients have so much going on: undercontrolled diabetes, they are homeless, they have hypertension. They just have so much going on that it’s hard to wrap this issue [colorectal cancer screening] into a visit with them.”
Finally, some provider site staff members were uncomfortable broaching the subject of colorectal cancer screening with patients, and this hindered recruitment efforts. In particular, provider site staff lacked the appropriate vocabulary to engage patients in a discussion about screening and participation in the program. For instance, some interviewees reported that provider site staff felt embarrassed or uncomfortable talking with patients about colorectal screening, given the need to discuss the bowel and feces. A staff member from the greater Seattle site described the difficulty medical assistants (MAs), in particular, had with recruiting patients for the CRCSDP: “They [MAs] are not comfortable with the topic; they don’t know how to talk about it.”
Patient knowledge, attitudes, and beliefs
To provide patients with an understanding of colorectal cancer and why screening is vital for prevention, site staff distributed existing brochures and posters created by the CDC and the American Cancer Society. The CDC encouraged the use of these materials, particularly from its Screen for Life campaign, to help sites conserve resources and unify messaging about colorectal cancer prevention.40 To promote their own programs, site staffs customized these materials by adding local program contact information and displayed them in clinic waiting areas or mailed them with enrollment forms.
Although site staff members viewed the CRCSDP as an enormous opportunity to increase the reach of preventive care, they soon realized patients lacked a basic understanding of the need for colorectal screening or had negative attitudes and beliefs associated with screening that prevented them from seeking program services. Site staff indicated that, in general, community members seemed uninformed about colorectal cancer, its risk factors, and how to prevent it. Also, sites found that small media alone were insufficient to stimulate interest or alter existing attitudes and beliefs about screening. Even Breast and Cervical Program patients, familiar with receiving regular breast and cervical cancer screening, appeared unaware of the importance of colorectal cancer screening. A St. Louis staff member speculated that Breast and Cervical Program patients, adherent to breast and cervical cancer screening, did not seem to understand the importance of colorectal cancer, saying: “It isn’t necessarily that they didn’t remember reading about it [colorectal screening through the CRCSDP], because they did; they just didn’t think it was necessary or important enough.”
Site staff members said that, in their efforts to initiate screening as soon as possible, they underestimated the priority population’s need for education on colorectal cancer screening, as this statement from a site staff member in Nebraska demonstrates:
I think one of the biggest issues is education. I think we expected to go to some of these places and just enroll [patients]. Well, I don’t know that everyone’s ready to just enroll. They need to be educated first. If they don’t understand the point of colorectal cancer screening, why on earth would they enroll? So, I think that that education piece, we kind of forgot about. We thought we should jump ahead to hurry up and just get people enrolled. And I think that’s wrong. If the population’s not quite there yet, it’s much more difficult to get them to fill out the paperwork.
Site staff indicated that lack of awareness of or interest in colorectal cancer seemed especially problematic for men, who participated in the CRCSDP in fewer numbers than women. Program staff attributed this lack of uptake to several factors. First, sites noted men’s overall tendency to avoid preventive services, as the following quote exemplifies: “I think that the literature supports that women seek preventive care more than men, in general…[men are] a little less likely to fix something that’s not broken.”41–43 Second, some interviewees proposed that men may harbor fears about colonoscopy that are related to homophobia. That possibility is discussed at length elsewhere in this Supplement to Cancer.38
Efforts to Improve Recruitment
As staff members across the program sites recognized recruitment as a problem, they promptly revised in-reach strategies and introduced new activities in an effort to increase the number of people enrolled. Programmatic adjustments were based on recruitment challenges specific to each site. Overall, 3 strategies were implemented to address sites’ recruitment challenges: expanding partnerships with additional primary care networks for greater reach; enhancing support to providers to address organizational and systemic barriers to encourage more consistent patient enrollment; and developing tailored outreach and education.
Expanding partnerships to additional primary care networks
Because relying primarily on in-reach to Breast and Cervical Program patients’ yielded disappointing enrollment results, sites expanded recruitment efforts by building partnerships with primary care networks not previously contracted with the CRCSDP. This strategy extended the reach of the program to medically underserved patients in new institutions. For example, a staff member from the city of Baltimore site described how they built a new partnership with a large local health care organization to recruit more patients for the CRCSDP:
We paid [a large health care organization] to basically make phone calls to their clients. They have electronic medical records, and within 20 seconds, they could pull up every single client in their system that met our eligibility criteria as far as insurance, income, geographic location, and lapse in screening.
This interviewee indicated that health care systems serving program-eligible populations benefit from the partnership with public health because they are able to refer their patients to free cancer screening services that would otherwise be inaccessible: “It extends their [patients’] care.”
Other sites took similar actions to increase recruitment and expand geographic coverage, working more closely with primary care networks such as Federally Qualified Health Centers (FQHCs) in their catchment area or by adding other community health centers to their program. A St. Louis staff member recounted concerted efforts they took to follow up with FQHC staff members to encourage them to actively enroll patients in the program:
Program staff followed up with phone calls [to FQHCs], you know, “You’ve heard a little bit about our program…we’d really like to get this program rolling and we’d like you to make some referrals. If you’re interested, let’s work on that.”
Changes in recruitment strategies to counter low turnout from Breast and Cervical Program patients involved broadening the base of potential patients by expanding the number of provider sites and then working with their staff to cultivate and strengthen those partnerships in ways that encouraged greater enrollment.
Increasing support to existing provider sites
After seeing lower-than-expected recruitment results based on referrals from original partnering primary care clinics, staff from several CRCSDP sites identified the need for increased support to provider sites. Site staff worked to increase the visibility of the program through facilitating group problem solving among provider site staff members, providing additional training, and implementing provider assessment and feedback mechanisms. Together, these strategies aimed to establish systems to ensure consistent recruitment and ensure that provider sites remained energized about and committed to the CRCSDP.
Interviewees from several sites said they believed that conducting visits to clinics reminded providers and their staff of the program. This was especially true for the greater Seattle site, where an interviewee mentioned that site staff had started conducting regular clinic visits to keep provider site staff mindful of the program or, in their words, to “keep the program present.” One interviewee said, “Our site staff went out and basically met with everybody [all provider sites] again and did retraining to get people refocused.” Another site staff member from the greater Seattle site suggested that these visits had a noticeable effect on improving recruitment: “Whenever we go to a health center, the number of referrals coming from that health center always jumps right after our visit.” Site staff also convened clinic staff members across multiple provider sites to discuss common challenges and to brainstorm potential solutions.
More specific training provided to provider sites emphasized how to discuss screening with patients. Staff members from the greater Seattle site mentioned that making sure clinic staff members such as medical assistants were comfortable with discussing screening with patients led to greater referrals and increased screening utilization. An interviewee explained,
What we decided was to set up training specifically for medical assistants to explain to them how FOBT kits work and teach them how to talk to their clients about FOBT tests.
This particular site also encouraged provider sites to adopt system-based strategies to improve recruitment such as provider-reminder systems and chart flagging. In addition, provider sites were encouraged to identify a designated clinic program “champion”, a staff member who consistently prompts physicians and nurses to discuss colorectal cancer screening with their patients. A provider site staff “champion” from greater Seattle described the implementation of this recruitment strategy: “We started just automatically putting packets [FOBT kits] in the folders for those [patients] who do not have insurance and are over the age of 50 [and] that has been working so far.”
Although the Suffolk County, New York, site did not report difficulties recruiting patients for the program, program staff developed strategies to boost recruitment among community health centers that were lagging behind others in patient enrollment. Unlike the other four sites, Suffolk County had conducted previous formative research related to colorectal cancer screening in primary care facilities.44 Specifically, results of this research suggested that direct referral from the primary care clinics to a point of contact at an endoscopy suite would be the least burdensome and most effective approach. The Suffolk County program incorporated the role of a physician, who received the referrals from the primary care centers, completed medical history reviews, and educated patients on screening processes before scheduling colonoscopy appointments.
Staff members with the Suffolk County site suggested that their use of a provider assessment and feedback tool was particularly effective for patient recruitment. The site developed a provider report card comparing the number of patient referrals across the community health centers, engendering a spirit of friendly competition among participating clinics. A staff member from Suffolk County described the report card:
When we went to the health centers to give the 1-year talk, I generated a report card to bring up some friendly competition, and we gave the health centers a list of where all the health centers stood with regard to number of referrals and how many of their referrals were actually eligible and how many were actually screened. So this generates some “Oh gosh, we should be better than this”-type thinking and hopefully gets them to screen more.
Tailored outreach and education
Finally, to combat a general lack of public knowledge about the importance and necessity of colorectal cancer screening, sites incorporated tailored educational messages and materials. Rather than relying solely on national colorectal cancer educational campaigns, program staffs developed locally relevant plans for their specific priority populations, including those who were especially difficult to recruit, such as men.
The Nebraska program represents a clear example of this more tailored approach to outreach and recruitment. Nebraska program staff members developed an aggressive education and awareness approach, which included a large-scale, sports-themed media campaign called “Stay in the Game.” The campaign engaged well-known college sports coaches and former University of Nebraska athletes to promote colorectal cancer screening among Nebraskans aged 50 and older. Men were a primary target for this campaign. A staff member described the impetus for creating “Stay in the Game”:
What led us to this [campaign] is we started enrolling people into the program and we were lacking men. We thought, men are associated with sports and Nebraskans are real big sports fanatics, so we’d try it out and see.
Agricultural events were an important venue for program staff to provide colorectal cancer education to Nebraskans. Site staff used creative educational tools, such as the game described below, at booths stationed at events:
Do you know the Operation Game? We actually made a colonoscopy game. So we have the picture of the colon, and then we cut out circles along the colon that are the polyps. Then they try to take out the polyp without it buzzing on them. I am amazed at how many people are drawn to that and not even necessarily to do the game, but just like, “Oh, this is my colon? Oh, this is what it looks like. Oh, this is what you mean when you reach the cecum.”
Site staff members in Nebraska suggested that adding these tailored educational activities to their recruitment strategy led to an increase in screening not only for the uninsured patients participating in the program but also for the insured population accessing care outside the program throughout the state.
Other program sites also developed tailored screening promotion approaches to bolster recruitment including staff appearances on local television programs and articles about colorectal cancer screening published in non-English-language newspapers, reaching culturally diverse communities. For example, to promote colorectal cancer screening and their program, Baltimore city staff members joined a television morning show that highlights local programs and events in the city. A site staff member described her participation: “In March, a local television station offered time slots to organizations, so we did a TV spot for Colorectal Cancer Awareness Month, and that generated more referrals than you can ever imagine.” An example of tailored outreach to diverse communities is the greater Seattle site’s publication of an article describing colorectal cancer prevention and program contact information in a citywide Vietnamese newspaper.
In summary, most site staff from across the program, except for that of Suffolk County, experienced challenges enrolling patients during early program implementation. They described this situation as a difficulty with recruitment and made changes to their original strategies to bring more patients into the program for colorectal cancer screening. The primary challenges faced in recruiting patients were a lack of public knowledge about the need for colorectal cancer screening, overreliance on in-reach to Breast and Cervical Program patients, and difficulty keeping colorectal cancer screening and the program a priority among staff members at partnering primary care clinics responsible for patient recruitment. To address these challenges, programs took action by developing tailored educational messages to pair with their promotional activities. They also broadened the pool of potential patients by expanding recruitment to additional health care networks. Finally, to ensure the program was a priority at clinics, site staff increased the amount of support for provider site staff and encouraged the use of systematic approaches to identify patients for the CRCSDP.
DISCUSSION
Results from national surveys including the National Health Interview Survey and the Behavioral Risk Factor Surveillance System indicate that financial barriers for the uninsured are a major factor in poor adherence to colorectal cancer screening.2,45 Accordingly, a primary function of the program was to provide colorectal cancer screening and, if indicated, diagnostic tests at no cost to those who were otherwise unable to afford screening based on similar models of the Breast and Cervical Program. The CRCSDP, as a pilot program, was a kind of test market for translating current research regarding barriers into practice by addressing these barriers within a service delivery setting. Since then, evidence-based strategies to systematically increase colorectal cancer screening have been identified by the Community Guide.32
Program planners for the CRCSDP anticipated a high demand for these services and were concerned this demand would overwhelm limited resources. However, the experience of 4 of the 5 program sites suggests that removing financial barriers to colorectal cancer screening was insufficient in creating interest and a demand among the majority of their priority populations. Several factors impeded patient recruitment: a primary dependence by sites on in-reach to Breast and Cervical Program patients, difficulty prioritizing the program among provider site staff responsible for patient enrollment, and patients’ knowledge, attitudes, and beliefs about colorectal cancer screening.
Our research is limited by conditions discussed by Rohan et al elsewhere in this Supplement to Cancer.38 Limitations pertaining to this particular report include the description of broader issues of patient recruitment for colorectal cancer screening, rather than an outline of the challenges by individual test type offered by each program. With only 5 cases and 3 variations of test choices offered (FOBT, colonoscopy, choice between either), we did not examine recruitment patterns by test type. Another important limitation of this report relates to our inability to quantify the success of any recruitment strategy used in the program, although this is not to say they were unsuccessful. Here we only review what happened, rather than comment on the effectiveness of recruitment activities. As issues of recruitment emerged over the course of the case study, we were able to incorporate related questions into our data collection instruments; however, an assessment of each strategy was never a component of this evaluation.
Our findings are consistent with other US studies demonstrating that even individuals with insurance coverage for screening do not always routinely seek it, if at all.44,46,47 Similarly, in countries like the United Kingdom, where all age-eligible citizens have access to colorectal cancer screening, studies have shown that non-financial barriers, such as a patient’s lack of knowledge and negative associations with colorectal cancer, hinder screening adherence.48–50
Among patient recruitment challenges we identified were a lower-than-expected screening adherence by women participating in the Breast and Cervical Program. Other research supports this finding, suggesting that public health practitioners should not assume that patients adherent to 1 type of cancer screening will be amenable to similar testing.51–53 In 1 study, only 24% of 2616 eligible women approached during mammogram visits agreed to participate in colorectal cancer screening.53 Similarly, Hay et al noted disappointingly low screening adherence for colorectal cancer among a group of mammography-adherent women.51 The authors conclude that to effectively recruit women during breast health visits, provider recommendations for colorectal screening must be delivered along with education about its benefits.
When faced with limited recruitment among Breast and Cervical Program women, some program sites expanded their network of providers to include new partnerships with safety-net health systems serving low-income, uninsured patients. These relationships proved mutually beneficial, suggesting that public health programs can offer health care organizations valuable assistance in designing and implementing systems to increase the number of patients screened and the quality of screening services. For instance, public health programs can strengthen existing partnerships with health care organizations by supporting systems to improve the quality of interventions, such as those that educate patients about the need for screening and recommend routine screening to age-appropriate patients.54
It is well recognized that staff in primary care clinics, especially those treating underserved populations, face substantial demands.55 Not surprisingly, several of our sites found that their provider staff responsible for program enrollment had difficulty prioritizing colorectal cancer screening. Research has shown that patients’ acute care needs can be a barrier to provider recommendation of preventive health measures.56 Other studies suggest that limited time for providers to discuss prevention during patient visits may lead to inconsistency in recommending colorectal cancer screening.55,56
Our data show that providing ongoing support to clinic staff, assessing clinic recruitment performance and offering feedback, and encouraging the use of clinic champions and systematic reminders all played an important role in ensuring patients receive information about colorectal cancer and maintaining adequate patient referrals for screening. These finding are preceded by studies, such as those reviewed by the Community Guide, reporting the effectiveness of system-level interventions, such as patient and provider reminder systems (i.e., educational, targeted postcard mailers and patient chart flagging or electronic medical records reminders) and provider assessment and feedback, in increasing colorectal cancer screening within health care systems.12,32,56,57 In addition, the Suffolk County program’s emphasis on reducing the burden on primary care for colorectal cancer screening facilitated referrals to colonoscopy screening.44 The previous research that had been conducted by Suffolk County staff on barriers specifically for their local clinics allowed the site to translate findings into a program that directly tested identified impediments to screening.
Finally, our finding that patients’ knowledge, attitudes, and beliefs about colorectal cancer screening were a barrier to recruitment is supported in the literature.18,58–60 As noted elsewhere in this Supplement to Cancer, social taboos regarding bowels and bowel movements inhibit the widespread acceptance of colorectal cancer screening.38 The program responded by developing10 tailored educational messages, materials, and large-scale public media campaigns. Further promotional efforts must continue to normalize colorectal cancer screening within the general public.
In summary, the experiences of program and provider staff of the program illustrate the complexities of recruiting patients into an organized colorectal cancer screening program despite the removal of financial barriers. Our results indicate that a multipronged approach to patient recruitment is crucial. Program sites implemented interventions at the individual, interpersonal, and systems levels, suggesting that approaches such as the social ecological model49,50 provide useful frameworks for planning public health efforts for colorectal cancer screening. To optimize colorectal cancer screening, public health practitioners must work closely with the health care sector to implement evidence-based, comprehensive strategies across these multiple levels. With the passage of the Affordable Care Act, which extends coverage for colorectal cancer screening, public health professionals will soon have a unique opportunity to significantly increase population-level cancer screening prevalence.61
Acknowledgments
FUNDING SOURCES
The Colorectal Cancer Screening Demonstration Program evaluated in this supplement was funded by the Centers for Disease Control and Prevention Funding Opportunity Number: RFA AA030.
Footnotes
The opinions or views expressed in this supplement are those of the authors and do not necessarily reflect the opinions or recommendations of the journal editors, the American Cancer Society, John Wiley & Sons, Inc., or the Centers for Disease Control and Prevention.
Participants in the case study evaluation provided verbal, informed consent for participation in interviews.
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
The articles in this supplement were commissioned based on participation in evaluating the Centers for Disease Control and Prevention-funded Colorectal Cancer Screening Demonstration Program.
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2007 Incidence and Mortality Web-based Report. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2010. http://www.cdc.gov/uscs. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Vital signs: colorectal cancer screening, incidence, and mortality—United States, 2002–2010. [Accessed December 13, 2011];MMWR Morb Mortal Wkly Rep. 2011 60:884–889. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6026a4.htm?s_cid=mm6026a4_w. [PubMed] [Google Scholar]
- 3.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 4.Rim SH, Joseph DA, Steele CB, Thompson TD, Seeff LC. Colorectal cancer screening - United States, 2002, 2004, 2006, and 2008. MMWR Surveill Summ. 2011;60(Suppl):42–46. [PubMed] [Google Scholar]
- 5.Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008;17:1623–1630. doi: 10.1158/1055-9965.EPI-07-2838. [DOI] [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality. Enhancing the Use and Quality of Colorectal Cancer Screening. Rockville, MD: U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 7.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–1607. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 8.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 9.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2008. National Cancer Institute; 2011. [Google Scholar]
- 10.Seeff LC, DeGroff A, Tangka F, et al. Development of a federally funded demonstration colorectal cancer screening program. Prev Chronic Dis. 2008;5:A64. [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention DoCPaC. [Accessed April 28, 2011];National Breast and Cervical Cancer Early Detection Program (Breast and Cervical Program) 2011 http://www.cdc.gov/cancer/nbccedp.
- 12.U. S. Preventive Services Task Force. [Accessed February 24, 2011];Screening for colorectal cancer: clinical summary of US Preventive Services Task Force Recommendation. 2008 http://www.uspreventiveservicestaskforce.org/uspstf08/colocancer/colosum.htm.
- 13.Seeff LC, Royalty J, Helsel WE, et al. Clinical outcomes from the CDC’s Colorectal Cancer Screening Demonstration Program. Cancer. 2013;119(suppl 15):2820–2833. doi: 10.1002/cncr.28163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeGroff A, Holden D, Goode Green S, Boehm J, Seeff LC, Tangka F. Start-up of the colorectal cancer screening demonstration program. Prev Chronic Dis. 2008;5:A38. [PMC free article] [PubMed] [Google Scholar]
- 15.Stake RE. Multiple Case Study Analysis. New York: The Guilford Press; 2006. [Google Scholar]
- 16.Subramanian S, Tangka FKL, Hoover S, et al. Costs of planning and implementing the CDC’s Colorectal Cancer Screening Demonstration Program. Cancer. 2013;119(suppl 15):2855–2862. doi: 10.1002/cncr.28158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Malley AS, Beaton E, Yabroff KR, Abramson R, Mandelblatt J. Patient and provider barriers to colorectal cancer screening in the primary care safety-net. Prev Med. 2004;39:56–63. doi: 10.1016/j.ypmed.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 18.Beeker C, Kraft JM, Southwell BG, Jorgensen CM. Colorectal cancer screening in older men and women: Qualitative research findings and implications for intervention. J Community Health. 2000;25:263–278. doi: 10.1023/a:1005104406934. [DOI] [PubMed] [Google Scholar]
- 19.Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–995. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wender RC. Barriers to screening for colorectal cancer. Gastrointest Endosc Clin N Am. 2002;12:145–170. doi: 10.1016/s1052-5157(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 21.Glasgow RE, Marcus AC, Bull SS, Wilson KM. Disseminating effective cancer screening interventions. Cancer. 2004;101:1239–1250. doi: 10.1002/cncr.20509. [DOI] [PubMed] [Google Scholar]
- 22.Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998. Reliability is consistency of judgment; pp. 144–159. [Google Scholar]
- 23.Lane DS, Cavanagh MF, Messina CR, Anderson JC. An academic medical center model for community colorectal cancer screening: the Centers for Disease Control and Prevention demonstration program experience. Acad Med. 2010;85:1354–1361. doi: 10.1097/ACM.0b013e3181df05e7. [DOI] [PubMed] [Google Scholar]
- 24.Hendren S, Griggs JJ, Epstein RM, et al. Study protocol: a randomized controlled trial of patient navigation-activation to reduce cancer health disparities. BMC Cancer. 2010;10:551. doi: 10.1186/1471-2407-10-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Percac-Lima S, Grant RW, Green A, et al. A patient-tailored navigator program for colorectal cancer screening in a community health center: a randomized controlled trial. J Gen Intern Med. 2008;23:237–238. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cult Anthropol Method. 1998;10:31–36. [Google Scholar]
- 27.Miller MF, Wong JG. Reducing financial barriers enhances the return rate of stool Hemoccult packets. Am J Med Sci. 1993;306:98–100. doi: 10.1097/00000441-199308000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Harris MA, Byles JE, Cockburn J, D’Este C. A general practice-based recruitment strategy for colorectal cancer screening. Aust N Z J Public Health. 2000;24:441–443. doi: 10.1111/j.1467-842x.2000.tb01609.x. [DOI] [PubMed] [Google Scholar]
- 29.Freedman JD, Mitchell CK. A simple strategy to improve patient adherence to outpatient fecal occult blood testing. J Gen Intern Med. 1994;9:462–464. doi: 10.1007/BF02599066. [DOI] [PubMed] [Google Scholar]
- 30.Fiscella K, Yosha A, Hendren SK, et al. Get screened: a pragmatic randomized controlled trial to increase mammography and colorectal cancer screening in a large, safety net practice. BMC Health Serv Res. 2010;10:280. doi: 10.1186/1472-6963-10-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baron RC, Rimer BK, Breslow RA, et al. Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening a systematic review. Am J Prev Med. 2008;35(1 Suppl):S34–S55. doi: 10.1016/j.amepre.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 32.Community Preventive Services Task Force. [Accessed October 2011];What is the Community Guide? 2011 http://www.thecommunityguide.org/index.html.
- 33.Yin RK. Case Study Research: Designs and Methods. 4. Thousand Oaks CA: Sage; 2009. [Google Scholar]
- 34.Patton MQ. Qualitative Research and Evaluation Methods. 3. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 35.Glaser B, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. New York: Aldine de Gruyter; 1967. [Google Scholar]
- 36.ATLAS. ti [computer program] Berlin, Germany: Atlas.ti Scientific Software Development GmbH; 2010. [Google Scholar]
- 37.Thomas DR. A General Inductive Approach for Analyzing Qualitative Evaluation Data. American Journal of Evaluation. 2006;27:237–246. [Google Scholar]
- 38.Rohan EA, Boehm J, DeGroff A, Glover-Kudon R, Preissle J. Implementing the CDC’s Colorectal Cancer Screening Demonstration Program: wisdom from the field. Cancer. 2013;119(suppl 15):2870–2883. doi: 10.1002/cncr.28162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glover-Kudon R, DeGroff A, Rohan E, Preissle J, Boehm J. Developmental milestones across the programmatic life cycle: implementing the CDC’s Colorectal Cancer Screening Demonstration Program. Cancer. 2013;119(suppl 15):2926–2939. doi: 10.1002/cncr.28166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Screen for Life: National Colorectal Cancer Action Campaign. [Accessed May 2011];Colorectal (Colon) Cancer. 2011 http://www.cdc.gov/cancer/colorectal/sfl/
- 41.Corney RH. Sex differences in general practice attendance and help seeking for minor illness. J Psychosom Res. 1990;34:525–534. doi: 10.1016/0022-3999(90)90027-2. [DOI] [PubMed] [Google Scholar]
- 42.Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 43.Rafuse J. Men’s attitudes about seeking health care may put them at risk, conference told. CMAJ. 1993;149:329–330. [PMC free article] [PubMed] [Google Scholar]
- 44.Lane DS, Messina CR, Cavanagh MF, Chen JJ. A provider intervention to improve colorectal cancer screening in county health centers. Med Care. 2008;46(9 Suppl 1):S109–S116. doi: 10.1097/MLR.0b013e31817d3fcf. [DOI] [PubMed] [Google Scholar]
- 45.Klabunde CN, Cronin KA, Breen N, Waldron WR, Ambs AH, Nadel MR. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20:1611–1621. doi: 10.1158/1055-9965.EPI-11-0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shires DA, Divine G, Schum M, et al. Colorectal cancer screening use among insured primary care patients. Am J Manag Care. 2011;17:480–488. [PubMed] [Google Scholar]
- 47.Klabunde CN, Schenck AP, Davis WW. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med. 2006;30:313–319. doi: 10.1016/j.amepre.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 48.Domati F, Travlos E, Cirilli C, et al. Attitude of the Italian general population towards prevention and screening of the most common tumors, with special emphasis on colorectal malignancies. Intern Emerg Med. 2009;4:213–220. doi: 10.1007/s11739-008-0184-5. [DOI] [PubMed] [Google Scholar]
- 49.McCaffery K, Wardle J, Waller J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev Med. 2003;36:525–535. doi: 10.1016/s0091-7435(03)00016-1. [DOI] [PubMed] [Google Scholar]
- 50.Calazel-Benque A, Viguier J, Roussel C, et al. Organized colorectal cancer screening programmes: how to optimize efficiency in the general population. Eur J Cancer Prev. 2011;20(Suppl 1):S20–S25. doi: 10.1097/01.cej.0000391566.41383.61. [DOI] [PubMed] [Google Scholar]
- 51.Hay JL, Ford JS, Klein D, et al. Adherence to colorectal cancer screening in mammography-adherent older women. J Behav Med. 2003;26:553–576. doi: 10.1023/a:1026253802962. [DOI] [PubMed] [Google Scholar]
- 52.McQueen A, Vernon SW, Meissner HI, Klabunde CN, Rakowski W. Are there gender differences in colorectal cancer test use prevalence and correlates? Cancer Epidemiol Biomarkers Prev. 2006;15:782–791. doi: 10.1158/1055-9965.EPI-05-0629. [DOI] [PubMed] [Google Scholar]
- 53.Shike M, Schattner M, Genao A, et al. Expanding colorectal cancer screening among minority women. Cancer. 2011;117:70–76. doi: 10.1002/cncr.25566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mays GP, Scutchfield FD. Improving public health system performance through multiorganizational partnerships. Prev Chronic Dis. 2010;7:A116. [PMC free article] [PubMed] [Google Scholar]
- 55.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guerra CE, Schwartz JS, Armstrong K, Brown JS, Halbert CH, Shea JA. Barriers of and facilitators to physician recommendation of colorectal cancer screening. J Gen Intern Med. 2007;22:1681–1688. doi: 10.1007/s11606-007-0396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sabatino SA, Habarta N, Baron RC, et al. Interventions to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers systematic reviews of provider assessment and feedback and provider incentives. Am J Prev Med. 2008;35(1 Suppl):S67–S74. doi: 10.1016/j.amepre.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 58.Bass SB, Gordon TF, Ruzek SB, et al. Perceptions of colorectal cancer screening in urban African American clinic patients: differences by gender and screening status. J Cancer Educ. 2011;26:121–128. doi: 10.1007/s13187-010-0123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Geiger TM, Miedema BW, Geana MV, Thaler K, Rangneka NJ, Cameron GT. Improving rates for screening colonoscopy: analysis of the health information national trends (HINTS I) data. Surg Endosc. 2008;22:527–533. doi: 10.1007/s00464-007-9673-2. [DOI] [PubMed] [Google Scholar]
- 60.DeBourcy AC, Lichtenberger S, Felton S, Butterfield KT, Ahnen DJ, Denberg TD. Community-based preferences for stool cards versus colonoscopy in colorectal cancer screening. J Gen Intern Med. 2007;23:169–174. doi: 10.1007/s11606-007-0480-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Read the Law: The Affordable Care Act, Section by Section. Health-Care.gov. 2012 http://www.healthcare.gov/law/full/