Summary:
Flap prelamination is the process whereby a complex 3- dimensional construct is fashioned in a staged manner. We present a case whereby the tissues of the anterolateral thigh, nourished by perforators of the descending branch of the lateral circumflex femoral artery, were prelaminated with a fibula in the setting of salvage head and neck reconstruction. With a paucity of recipient vessels in the neck and a previous failed free fibula transfer secondary to osteoradionecrosis, a fibula was implanted into a suprafascial pocket created in the anterolateral thigh. This was allowed to pick up a blood supply from this rich vascular bed and mature over a period of 3 weeks before being transferred with the anterolateral thigh tissues as a prelaminated osteocutaneous composite free flap. A bone scan performed both before and after transfer confirmed uptake of radionucleotide by the fibula suggesting neovascularization. The composite mandibular defect was successfully reconstructed using this technique, and we believe this could represent a new strategy in the setting of salvage head and neck surgery.
Flap prelamination was first described in 1994 by Pribaz and Fine.1 It refers to the process by which layers are added to a well-vascularized bed and allowed time to mature. Then, in a second stage, the composite block of tissue is transferred to a recipient site based on its native axial blood supply. This has the advantage of allowing the reconstruction to commence in an anatomical site remote from the area to be reconstructed. In the setting of salvage head and neck surgery, this is essential due to the irradiated and scarred nature of the local tissues. Prelamination is commonly used when reconstructing complex defects of the central face, for instance when prelaminating the tissues of the radial forearm with cartilage grafts prior to 3-dimensional nasal reconstruction.2 With regard to composite defects of the mandible free fibula reconstruction to maintain osseous integrity is established practice,3 but in salvage situations this may not be a feasible reconstructive option. By prelaminating the suprafascial soft tissues nourished by perforators of the descending branch of the lateral circumflex femoral artery, we were able to construct a novel composite vascularized osteocutaneous structure remote from the irradiated tissues of the neck. In a second stage, this was transferred as a composite free flap to successfully reconstruct both the mandible and the soft tissues in a single sitting.
CASE PRESENTATION
A 62-year-old man presented to our service with a locally advanced squamous cell carcinoma of the buccal mucosa. Oncological resection with wide margins was carried out leaving a composite centrolateral mandibular defect measuring 5 cm in length and a soft-tissue defect of the buccal mucosa and overlying skin. A free fibula osteoseptocutaneous flap was used to reconstruct the mandible and buccal mucosa, and a free anterolateral thigh flap (ALT) was used to reconstruct the skin defect. The free fibula was anastomosed to the superior thyroid artery and a branch of the internal jugular vein, and the ALT was anastomosed to the superficial temporal vessels. No complications were encountered, and the patient was discharged 5 days postoperatively. A course of adjuvant radiotherapy was followed, which unfortunately precipitated osteoradionecrosis of the reconstructed segment of the mandible. At the time of the initial reconstruction, the portion of fibula that was not included in the free flap was preserved in a refrigerated tissue bank, for potential future use. After counseling the patient with regard to his reconstructive options, he refused to undergo a second free fibula reconstruction using the contralateral leg as he felt that it might impair his mobility. He agreed to undergo a second free ALT, however, and given the paucity of recipient neck vessels secondary to irradiation and previous surgery, a single flap reconstruction was indeed preferable. It was decided to prelaminate the ALT with the segment of preserved fibula in order to attempt a composite osteocutaneous reconstruction.
The fibula was inserted into a suprafascial pocket created just lateral to the cutaneous perforators of the lateral circumflex femoral artery that had been marked preoperatively with a hand-held Doppler (Fig. 1). A period of 3 weeks was allowed for the fibula to mature in its vascular bed, and a bone scan performed before transfer confirmed radionucleotide uptake of the implanted fibula (Fig. 2). A composite prelaminated osteocutaneous ALT flap was then raised (Fig. 3) and transferred to the recipient site where the vessels were anastomosed to the superficial temporal system. The fibula was osteotomized to the required length at a position within the flap (Fig. 4) to allow for its insertion into the mandibular defect. It was secured in situ with miniplates. Cortical bleeding was noted when performing the osteotomies. The skin flap was inset to reconstruct the cutaneous defect. The patient made an unremarkable recovery, and no postoperative complications were encountered. A bone scan performed 2 weeks later confirmed radionucleotide uptake within the fibula.
Fig. 1.
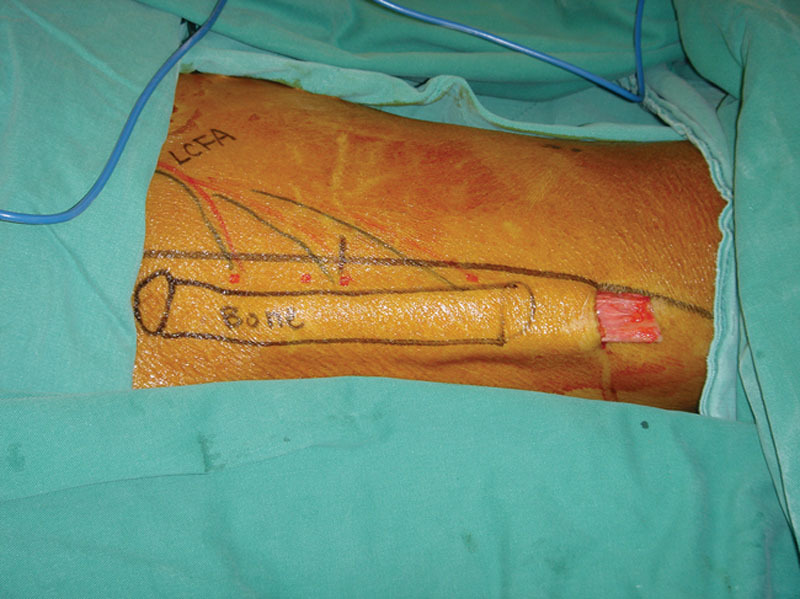
Insertion of long segment of fibula into suprafascial pocket created in the anterolateral thigh lateral to the premarked perforators of the descending branch of the lateral circumflex femoral artery.
Fig. 2.
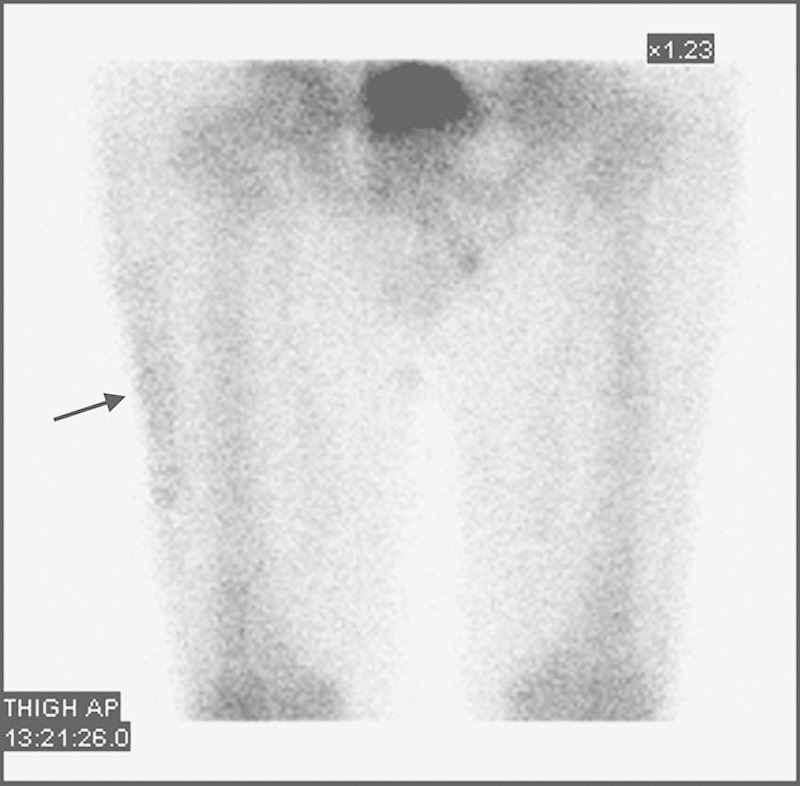
Bone-scan performed 3 weeks post insertion of the fibula. Black arrow denotes position of the fibula within the soft tissues of the thigh.
Fig. 3.
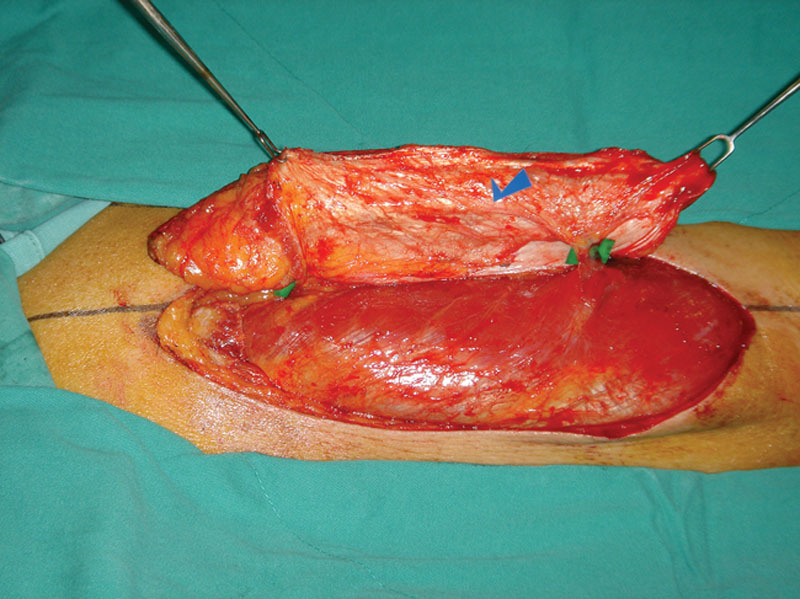
Prelaminated ALT flap raised with green denoting the position of the perforators and the blue arrow denoting the position of the fibula.
Fig. 4.

Free prelaminated osteocutaneous ALT flap with position of fibula marked in purple in distal aspect of flap.
DISCUSSION
Prelamination is a recognized technique that has many applications in the field of reconstructive surgery. Indeed, many different tissue types, including cartilage, bone, mucosa, and nerve, have successfully been used as graft materials in the prelamination of tissues.4–6 In addition, the ability of cancellous bone graft to undergo neovascularization in a heterotopic “carrier” location has been reported.7 However, when bone is required in the reconstruction, the fibula is more commonly preferred as a donor site that can be prelaminated, as this avoids the need to graft bone into heterotopic sites. This can be seen with the prelaminated fibula used in both penile and maxillary reconstruction.6,8
When a free fibula is harvested for mandibular reconstruction, a relatively large section of the bone is often discarded after it has been osteotomized to the required size. At our institution, we have preserved the remaining portion of fibula in a refrigerated tissue bank for potential future use in complex cases. In situations where a second free osteocutaneous flap is not feasible, such as in our case, the potential exists to insert the fibula bone graft into a well-vascularized heterotopic site, thus prelaminating those soft tissues with bone for later transfer. In our case, we were able to demonstrate neovascularization of the fibula by means of a bone scan both before and after transfer. No complications were encountered, and a complex 3-dimensional salvage reconstruction was achieved using a novel approach to an established technique.
CONCLUSIONS
Prelamination of the soft tissues of the anterolateral thigh with a large segment of fibula could represent a novel salvage technique in complex cases of head and neck reconstruction. It combines the established principles of prelamination with the basic plastic surgical principle of never throwing anything away that you may later need.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Pribaz JJ, Fine NA. Prelamination: defining the prefabricated flap–a case report and review. Microsurgery. 1994;15:618–623. doi: 10.1002/micr.1920150903. [DOI] [PubMed] [Google Scholar]
- 2.Pribaz JJ, Weiss DD, Mulliken JB, et al. Prelaminated free flap reconstruction of complex central facial defects. Plast Reconstr Surg. 1999;104:357–365. doi: 10.1097/00006534-199908000-00005. discussion 366. [DOI] [PubMed] [Google Scholar]
- 3.Wei FC, Seah CS, Tsai YC, et al. Fibula osteoseptocutaneous flap for reconstruction of composite mandibular defects. Plast Reconstr Surg. 1994;93:294–304. discussion 305. [PubMed] [Google Scholar]
- 4.Miyawaki T, Degner D, Jackson IT, et al. Easy tissue expansion of prelaminated mucosa-lined flaps for cheek reconstruction in a canine model. Plast Reconstr Surg. 2002;109:1978–1985. doi: 10.1097/00006534-200205000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Rath T, Tairych GV, Frey M, et al. Neuromucosal prelaminated flaps for reconstruction of intraoral lining defects after radical tumor resection. Plast Reconstr Surg. 1999;103:821–828. doi: 10.1097/00006534-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Santamaria E, Correa S, Bluebond-Langner R, et al. A shift from the osteocutaneous fibula flap to the prelaminated osteomucosal fibula flap for maxillary reconstruction. Plast Reconstr Surg. 2012;130:1023–1030. doi: 10.1097/PRS.0b013e31826864aa. [DOI] [PubMed] [Google Scholar]
- 7.Orringer JS, Shaw WW, Borud LJ, et al. Total mandibular and lower lip reconstruction with a prefabricated osteocutaneous free flap. Plast Reconstr Surg. 1999;104:793–797. doi: 10.1097/00006534-199909030-00028. [DOI] [PubMed] [Google Scholar]
- 8.Schaff J, Papadopulos NA. A new protocol for complete phalloplasty with free sensate and prelaminated osteofasciocutaneous flaps: experience in 37 patients. Microsurgery. 2009;29:413–419. doi: 10.1002/micr.20647. [DOI] [PubMed] [Google Scholar]


