Abstract
Jorge Lobo's Disease is a rare, chronic granulomatous cutaneous mycosis, which is typical of tropical and subtropical regions. It is caused by the traumatic implantation of the fungus Lacazia loboi into the skin and subcutaneous tissue. The disease was first described in 1931 by Jorge Lobo, in Recife (PE), Brazil. It is common in Central and South America, and predominates in the Amazon region. We report a case of Jorge Lobo's Disease, which had been initially referred as being paracoccidioidomycosis. We emphasize clinical and diagnostic features of the disease.
Keywords: Blastomycosis, Lacazia, Lobomycosis
A 47-year-old male patient, who had been living in Macapa (AP) for 10 years presented with a lesion of four years' duration in the right malar region. Physical examination revealed a keloidiform node (Figure 1). Histopathological examination evidenced a granulomatous inflammation with fungal proliferation in the dermis, which was suggestive of Lacazia loboi compatible with Jorge Lobo's disease (Figures 2, 3 and 4).
FIGURE 1.

Keloidiform nodes in the malar region of the patient’s face
FIGURE 2.
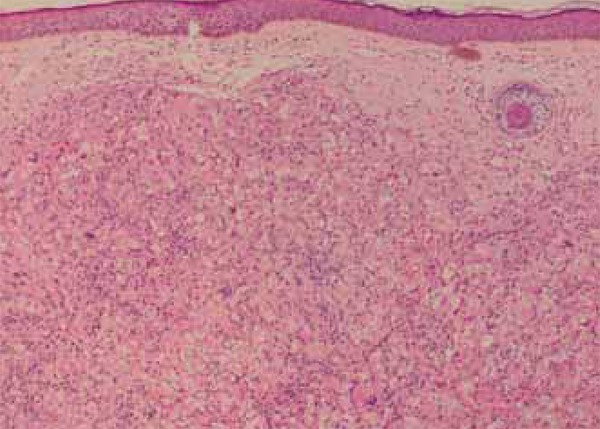
Presence of granulomatous inflammation with intense and diffuse proliferation of fungi in the papillary dermis and superficial reticular dermis, engulfed or not by histiocytes, suggesting Jorge Lobo’s disease - HE 100x
FIGURE 3.
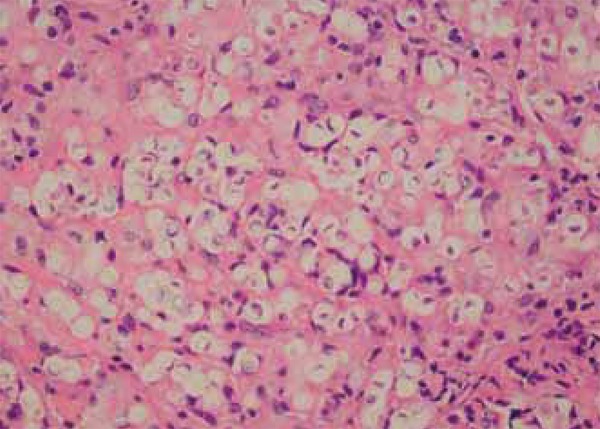
Fungi and granulomatous infi ltrate in detail - HE 400x
FIGURE 4.
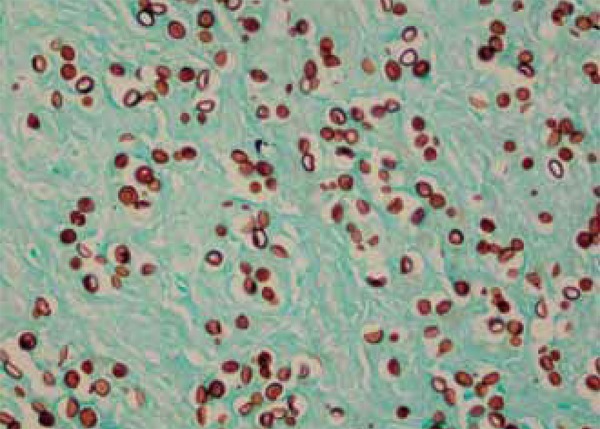
Grocott’s method to show the distribution of fungi in the dermis - 400x
Jorge Lobo's Disease is a rare, chronic granulomatous cutaneous infection caused by the traumatic implantation of the fungus Lacazia loboi into the skin and subcutaneous tissue. The disease was first described in 1931 by the dermatologist Jorge Lobo, in Recife (PE), Brazil.1 It is common in Central and South America, and predominates in the Amazon region.2,3 There are about 550 cases reported in the literature. Of these, 322 occurred in Brazil. About 90% of cases have occurred in forest workers.4,5
Clinically, it is characterized by a large polymorphism of cutaneous lesions. Keloidiform nodes usually predominate. It primarily affects exposed areas of the skin, tending to spare mucous membranes. Local symptoms are bloating, itching and pain on palpation. It may affect the lymph nodes, but not internal organs.6,7
The diagnosis is made based on anatomicopathological evidence and presence of the fungus in the skin lesion; culture is negative. Pathology shows nodular and diffuse granulomatous inflammatory infiltrate in the dermis, consisting of macrophages and numerous multinucleated Langerhans'-type cells and foreign body cells filled wih fungi. Fungus examination shows globoid structures with thick, double-contour walls, which reproduce by simple budding. They are usually rosary-shaped or dumbbell-shaped.7,8,9
Surgery is the usual conduct of choice for isolated lesions. Some studies have described the use of cryotherapy. There are no effective drugs for disseminated forms of the disease.
Footnotes
Conflict of Interest: None.
Financial Support: None.
How to cite this article: Carvalho KA, Floriano MC, Enokihara MMSS, Mascarenhas MRM. Jorge Lobo’s Disease. An Bras Dermatol. 2015;90(4):586-8.
Study conducted at the Department of Dermatology, Universidade Federal de São Paulo (Unifesp) - São Paulo (SP), Brazil.
REFERENCES
- 1.Lobo J. Um caso de blastomicose produzido por uma espécie nova, encontrada em Recife. Rev Med Pernambuco. 1931;1:763–765. [Google Scholar]
- 2.Rodríguez-Toro G. Lobomycosis. Int J Dermatol. 1993;32:324–332. doi: 10.1111/j.1365-4362.1993.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 3.Haubold EM, Cooper CR, Jr, Wen JW, McGinnis MR, Cowan DF. Comparative morphology of Lacazia loboi (syn. Loboa loboi) in dolphins and humans. Med Mycol. 2000;38:9–14. doi: 10.1080/mmy.38.1.9.14. [DOI] [PubMed] [Google Scholar]
- 4.Papadavid E, Dalamaga M, Kapniari I, Pantelidaki E, Papageorgiou S, Pappa V, et al. Lobomycosis: A case from Southeastern Europe and review of the literature. J Dermatol Case Rep. 2012;6:65–69. doi: 10.3315/jdcr.2012.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baruzzi RG, Lacaz CS, Souza FAA. História natural da doença de Jorge Lobo. Ocorrência entre os índios Caiabi (Brasil Central) Rev Inst Med Trop São Paulo. 1979;21:302–338. [PubMed] [Google Scholar]
- 6.Queiroz-Telles F, Nucci M, Colombo AL, Tobón A, Restrepo A. Mycosis of implantation in Latin America: an overview of epidemiology, clinical manifestations, diagnosis and treatment. Med Mycol. 2011;49:225–236. doi: 10.3109/13693786.2010.539631. [DOI] [PubMed] [Google Scholar]
- 7.Brito AC, Quaresma JAS. Lacaziosis (Jorge Lobo`s disease): review and update. An Bras Dermatol. 2007;82:461–474. [Google Scholar]
- 8.Reif JS, Schaefer AM, Bossart GD. Lobomycosis: risk of zoonotic transmission from dolphins to humans. Vector Borne Zoonotic Dis. 2013;13:689–693. doi: 10.1089/vbz.2012.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baruzzi RG, Rodrigues DA, Michalany NS, Salomão R. Squamous-cell carcinoma and lobomycosis (Jorge Lobo's disease) Int J Dermatol. 1989;28:183–185. doi: 10.1111/j.1365-4362.1989.tb02459.x. [DOI] [PubMed] [Google Scholar]
- 10.Bustamante B, Seas C, Salomon M, Bravo F. Case report: Lobomycosis successfully treated with posaconazole. Am J Trop Med Hyg. 2013;88:1207–1208. doi: 10.4269/ajtmh.12-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]


