Abstract
Background
In the United States, Korean immigrants experience a disproportionately high burden of chronic hepatitis B (HBV) viral infection and associated liver cancer compared to the general population. However, despite clear clinical guidelines, HBV serologic testing among Koreans remains persistently sub-optimal.
Methods
We conducted a cluster-randomized trial to evaluate a church-based small group intervention to improve HBV testing among Koreans in Los Angeles. Fifty-two Korean churches, stratified by size (small, medium, large) and location (Koreatown versus other), were randomized to intervention or control conditions. Intervention church participants attended a single-session small-group discussion on liver cancer and HBV testing and control church participants attended a similar session on physical activity and nutrition. Outcome data consisted of self-reported HBV testing obtained via 6-month telephone follow-up interviews.
Results
We recruited 1123 individuals, 18-64 years of age, across the 52 churches. Ninety-two percent of the sample attended the assigned intervention session and 86% completed the 6-month follow-up. Sample characteristics included: mean age 46 years, 65% female, 97% born in Korea, 69% completed some college, and 43% insured. In an intent-to-treat analysis, the intervention produced a statistically significant effect (OR = 4.9, p < .001), with 19% of intervention and 6% of control group participants reporting a HBV test.
Conclusion
Our intervention was successful in achieving a large and robust effect in a population at high risk of HBV infection and sequelae.
Impact
The intervention was fairly resource efficient and thus has high potential for replication in other high-risk Asian groups.
Keywords: HBV Testing, Koreans, Randomized Trial
Introduction
Chronic hepatitis B viral (HBV) infection is a serious public health challenge with over 400 million individuals worldwide and over 2 million in the United States chronically infected with this virus (1, 2). HBV infection has serious medical sequelae including chronic liver disease, cirrhosis, and hepatocellular carcinoma (3-5). In the United States hepatocellular carcinoma, the primary form of liver cancer, disproportionately affects Asian Americans, reflected in incidence and mortality rates that are eight times higher than those among non-Hispanic Whites (6). Among Asians, over 80% of liver cancer is etiologically related to chronic HBV infection, which is endemic in Asia (7-9) and therefore also very highly prevalent among Asian immigrants to the United States (10, 11). It is estimated that approximately 10% of foreign-born Asian adults in the U.S. are living with chronic HBV infection (12).
Current guidelines recommend hepatitis B serologic testing of adolescents and adults who were born in Asia and the Pacific Islands, and U.S.-born persons not vaccinated as infants whose parents were immigrants from highly endemic areas such as Asia as the first step in the control of HBV and associated morbidities (13, 14). Serologic testing will identify the vulnerable (uninfected) who will need vaccination, allow triage of the infected to appropriate treatment or surveillance, and provide opportunities for counseling infected individuals to reduce vertical and horizontal transmission to close contacts (13, 14). Vaccination of Asian immigrant adults without testing is not considered an adequate public health strategy (13, 15), because of the potential for unnecessary vaccination of immune individuals and missed opportunities for treatment and prevention among those with undiagnosed infection. Despite their elevated disease risk, HBV testing rates among Asians in the U.S. are sub-optimal with estimates ranging from 11% to 67% (16-26) in different Asian sub-populations.
Koreans are a rapidly growing population in the U.S., with the largest concentration of Koreans outside of Korea residing in the Los Angeles region. Approximately 78% of Korean adults in the U.S. are foreign born (27), and therefore at particularly elevated risk for HBV and liver cancer. Liver cancer incidence among Koreans was 34.9 cases per 100,000 people between 2004-2008 compared to 3.6 cases per 100,000 people in non-Latino whites over the same time period (28). We were able to locate only three studies that examined hepatitis B testing rates among Koreans (16, 20, 29) which reported rates of 32% to 56%, indicating much room for improvement.
A high proportion of Korean Americans attend a Christian church on a regular basis with estimates ranging from 67% to over 80% (30-32). Korean churches incorporate and host many organized activities relevant to their congregations such as social services, legal services, and health ministries (30, 33, 34). Thus, churches are hospitable environments in which to deliver health related programming to Koreans (35, 36). The literature also contains numerous examples of successful church-based interventions among other ethnic groups (37-39).
We report outcomes of a cluster-randomized trial to evaluate the effectiveness of a church-based small group intervention to improve HBV testing among Koreans in Los Angeles. This is one of the first HBV testing controlled intervention trials specifically focused on Koreans.
Materials and Methods
Overview of Research Design
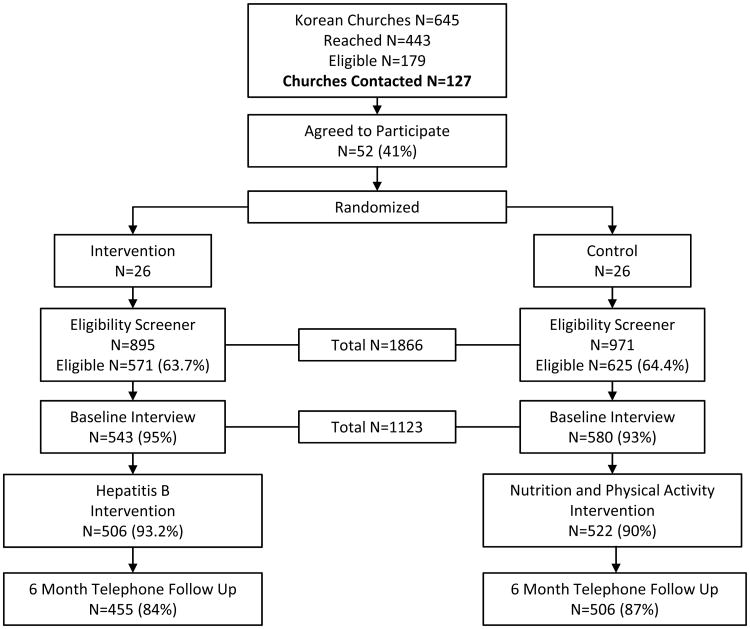
The study utilized a 2-group design with randomization at the level of the church (Figure 1). Eligible churches were classified into six strata defined by size (small, medium, large) and geographic location (Koreatown versus other). Within each stratum, a pair of churches was randomly selected and members of the pair were randomly assigned to either the intervention or control condition.
Figure 1. Overview of Final Study Design.
Participants were recruited on-site by study staff to participate in a “Korean Health Study,” screened for eligibility, and after completing an interviewer-administered baseline survey, were invited to attend an education session on Korean health. Participants at intervention churches attended a single-session small group discussion on liver cancer and HBV testing and control church participants attended a similar discussion session on physical activity and nutrition (the latter was based on community preferences and feedback). Six-month telephone follow-up interviews assessed the effect of the intervention on self-reported HBV testing rates. Study activities were conducted between 2006 and 2012, in collaboration with partners from the Korean community. The study was approved by the Institutional Review Board of UCLA.
Recruitment of Churches
Information from available church directories was compiled to create a list of 645 unique Korean churches in Los Angeles County. We attempted mail and telephone contact with all 645 churches to obtain information about church size and interest in study participation. Of the 443 churches reached (69%), 146 (33%) were ineligible due to small size (<51 members) and 118 (27%) declined participation. The 179 remaining churches comprised the sampling frame for the study.
Churches in the sampling frame were assigned to one of the six cells created by the two stratification variables. The two location categories were: inside or outside the boundaries of the Koreatown neighborhood of Los Angeles. The three size categories were: “small” (51-200 members), “medium” (201-900 members) or “large” (over 900 members). Based on the distribution of church membership among the location and church size categories our recruitment goals for number of participants per stratum were: 40% within Koreatown and 60% outside of Koreatown; 33% small, 33% medium and 33% large (see Table 1). The justification for the location stratum was potential acculturation differences among members attending churches inside versus outside Koreatown. The justification for the size stratum was the potential for competing activities available at larger churches as well as resource differences for supporting the intervention. First, pairs of churches were randomly selected within each cell. Next, both churches in each pair were re-contacted to confirm eligibility and willingness to participate in the study. If needed, replacements were randomly selected from the affected cell. Finally, members of each pair were randomly assigned to the intervention or control condition.
Table 1. Stratified Random Assignment of Churches and Distribution of Participants by Church Size and Location.
| Koreatown | Outside Koreatown | Total | % of participants | |
|---|---|---|---|---|
| Small (51-200 members) | N = 10 (n = 163) | N = 16 (n = 261) | N = 26 (n = 424) | 38% |
| Medium (201-900 members) | N = 6 (n = 142) | N = 10 (n = 210) | N = 16 (n = 352) | 31% |
| Large (>900 members) | N = 4 (n = 155) | N = 6 (n = 192) | N = 10 (n = 347) | 31% |
| Total | N = 20 (n =460) | N =32 (n = 663) | N = 52 (n = 1123) | |
| % of participants | 41% | 59% |
Note: N = number of churches, n = number of participants within churches
Recruitment of Participants
All participants were recruited in-person at church sites. One week prior to the start of recruitment, an announcement was placed in the church bulletin describing the study and the opportunity for study participation the following weekend. On the day of recruitment, typically Sunday, multiple study staff members were present at the church before and after scheduled church services to enroll participants. The study was described as a “Korean Health Study” at both intervention and control churches to avoid bias that may be introduced by self-selection of individuals based on interest in HBV or Nutrition-Physical Activity topics. After completion of the eligibility screener and baseline survey (interviewer administered), participants attended the applicable intervention session, and it was only there that the topic of the session was revealed. At medium and large churches, typically more than one session was needed to accommodate all study participants (number of sessions per church ranged from 1-5).
Theoretical Model
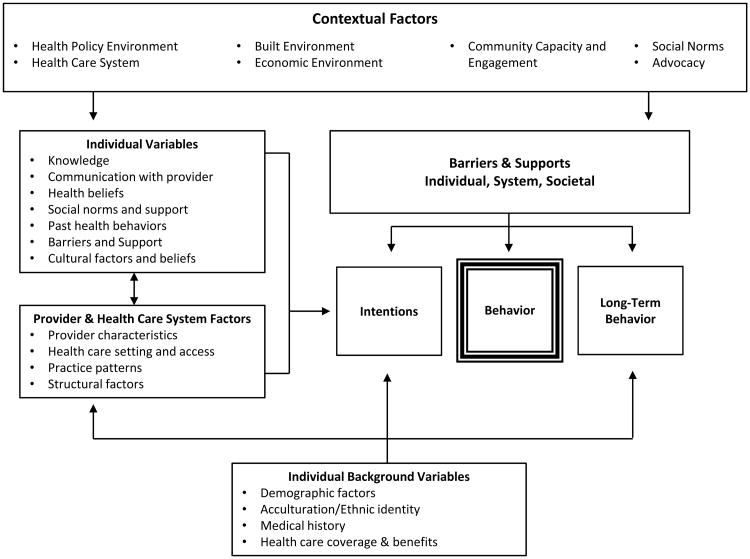
The Health Behavior Framework (HBF; Figure 2) was used to guide the data collection instruments and the intervention (40). The HBF is a comprehensive conceptual framework that posits that individual health behavior is influenced by a complex myriad of individual, health system, community, and societal level factors. The HBF considers cultural context and also provides guidance in selecting an intervention setting and modality that is appropriate for the intended audience. The focus of this trial was primarily on modifying individual (e.g., knowledge, health beliefs) and group/community level (e.g., social norms within group and church) mutable factors in an attempt to influence uptake of HBV testing.
Figure 2. Health Behavior Framework.
Description of Intervention and Control Conditions
The intervention consisted of a single-session small-group discussion supplemented by print materials. Small group interventions have been found to be effective in changing health behavior in a number of studies (38, 41). Group interventions capitalize on social norms and peer modeling and provide participants an opportunity to interact with others to process the information they receive. This type of interaction may enhance learning and execution of the health behavior being promoted compared to more passive formats such as print or audiovisual media. Delivering health programming in a group session capitalizes on a familiar format used for other church activities and is therefore often more acceptable in church settings compared to individually-focused approaches (36, 38, 42-44). The content and format of the intervention and control sessions and the accompanying print materials were developed based on extensive input and pilot testing with Korean churchgoers and were designed to be culturally appropriate and interesting and appealing to the intended audience (40, 45).
Groups consisted of 8-12 participants led by trained, bilingual (Korean/English) lay health workers/facilitators. Facilitators (N=14; mostly female) were recruited from the Korean community and received a 2-day study specific training focused on ethics and confidentiality, IRB certification, overview of hepatitis B/ liver cancer or physical activity/nutrition, intervention materials, and the nuts and bolts and theoretical underpinnings of leading interactive group discussions. The second day involved practicing intervention delivery with focused feedback. Material on liver cancer and HBV testing was presented utilizing an interactive multimedia format. The group sessions were embedded with questions to stimulate and facilitate active discussion and information processing of the topic by participants. Topics covered included prevalence of the virus, transmission routes, the need for testing to identify carriers of the virus, the meaning of test results, necessary follow-up after an abnormal test result, the link between hepatitis B and liver cancer, and common misconceptions about the virus and transmission routes. In addition to providing information to enhance knowledge, the intervention was also designed to influence other mutable HBF factors such as perceived risk for HBV and liver cancer (e.g., providing facts about increased risk for HBV for Korean immigrants), counter barriers to testing (e.g., referral to local clinic for low-cost/free testing), create a social norm within the group supportive of testing (e.g., use of small group format, buy in of church leaders), and encourage participants to discuss HBV with a health care provider and request testing. After the session, participants were given a bilingual informational booklet reinforcing the topics discussed during the session, a handout for their health care provider explaining the rationale for testing to encourage patient-provider discussions, and a resource guide to local clinics where testing and any needed follow-up could be received at low or no cost in order to reduce perceived barriers.
Control group discussion sessions followed a parallel format, delivered by similarly trained facilitators, but focused on nutrition and physical activity. Participants were also led through a 10-minute, low-impact physical activity session guided by the facilitator in conjunction with a culturally targeted video that depicted Korean dancers and music. After the session, participants were given the video and ACS-developed nutrition and physical activity print materials in English and Korean. Upon completion of the follow-up interview, control group participants received the HBV print intervention materials, including information on clinics where low/no cost screening and follow-up care could be received.
Data Collection
Eligibility Screener
Eligibility criteria included being 18-64 years of age, of Korean ethnicity, Korean or English speaking, and never having had an HBV serologic test in the past.
Baseline and Follow-up Data
Survey items were drawn from the published literature and our own prior work (16)and translated from English into Korean by bilingual translators using the forward – back translation method (45). The items were pilot tested in 6 focus groups with 45 participants to ensure applicability to the target audience. Constructs measured at baseline included demographics (age, marital status, education, income), acculturation (short Marin Acculturation Scale translated into Korean (46), country of birth, years in the U.S., English fluency), health care access (insurance, usual source of care, recent health care utilization), and perceived health. Although not the focus of this paper, additional survey items assessed knowledge and beliefs related to hepatitis B and liver cancer (47)as well as a number of other health behaviors (physical activity, diet, tobacco use) to mask the primary focus of the study on HBV testing.
Study Outcome
All participants were re-contacted by telephone six months after baseline. The primary outcome measure was self-reported receipt of HBV testing at 6 month follow-up. Prior to asking about HBV test receipt, participants were informed that routine blood testing does not include screening for HBV. Participants were then asked, “Have you had a blood test specifically for HBV since we spoke with you at your church approximately 6 months ago?”
During the study period, dates and locations of free hepatitis B testing events in the community were tracked and recorded by study staff in an effort to monitor potential sources of contamination.
Data Analysis
Power calculations determined that 21 churches per group with a mean of 20 participants per church would provide 80% power to detect a 10 percentage point group difference in test rates at follow-up (5% versus 15%) assuming an intraclass correlation (ICC) of 0.05. The effect size estimate was based on intervention studies to promote other cancer screening (48, 49) given the paucity of intervention research on HBV testing. The ICC was a conservative value selected based on our experience with small-group interventions and prior studies indicating that ICCs in similar settings are unlikely to exceed 0.05 (50).
We compared the intervention and control groups on baseline sociodemographics and access to health care using mixed effects models accounting for clustering on church. We compared participants lost to follow-up to those retained in the same manner.
The intervention effect was estimated as a comparison between groups at follow-up given that no participants had been tested for HBV at baseline. We conducted intent-to-treat analyses of all randomized participants. Participants who did not provide data at follow-up were assumed to be not tested. The analyses were conducted using mixed effects logistic regression with random intercepts for church and session to account for the hierarchical structure of the data. As sensitivity analyses, the analysis was repeated with missing outcomes multiply imputed using the MICE system of chained equations in Stata 11 (51) with a set of 24 auxiliary variables (details available from authors). Thirty multiply imputed data sets were generated and analyzed. Final estimates were obtained using Rubin's rules (52). Secondary analysis examined the intervention effect within size and location strata. We specified a two-sided significance level of 0.05.
Results
Church Recruitment
Contact was attempted with 127 churches (out of the sampling frame of 179), of which 52 (41%) agreed to participate and were randomized to the intervention (n = 26) or control condition (n = 26). The remaining 75 (59%) churches were not included for the following reasons: no longer in operation or had 50 or less members (n=19), could not be reached (n=5), conflicts with other church events (n = 18), inadequate space for research activities (n=9), not interested in participating in research (n=12), and other (n=12). Table 1 shows the distribution of the 52 enrolled churches among the size and location strata. Each cell included an equal number of intervention and control churches.
Participant Recruitment
A total of 1866 participants were screened for eligibility at the 52 churches (Figure 1). Of these, 1196 (64%) met study eligibility criteria and 1123 (94%) were enrolled and completed the baseline survey, n=543 from intervention churches and n=580 from control churches. Ninety-two percent of enrolled participants attended the discussion group as assigned (93% intervention; 90% control). Six month follow-up interviews were completed with 86% of enrolled participants. The most common reason for study ineligibility in both groups was having had a HBV test in the past (96% of ineligible). Thus, the base rate of HBV testing in our Korean churchgoing population was 34.6% (n=646/1866).
Participant Characteristics
Participant characteristics at baseline, stratified by group assignment, are presented in Table 2. More than half the sample was female (65%), and the mean age was 46 years. The overwhelming majority (97%) of the sample was born in Korea, with an average length of stay in the United States of over 16 years among the foreign born. Education and income levels were fairly high with 69% having completed at least some college and 38% reporting a household income of over $50,000 per year. Thirty seven percent of the sample reported having private health insurance and 6% reported having Medicaid/MediCal. The most common type of private insurance reported was HMO or PPO(80%). Half the sample reported having a usual source of care which was most commonly a clinic/health center (79%), or a traditional practitioner (14%). About half the sample (56%) reported having a regular doctor, and 81% reported that their doctor was of Korean ethnicity.
Table 2. Demographic Characteristics of the Sample.
| Demographic Characteristic | Intervention (N=543) | Control (N=580) | Total (N=1123) |
|---|---|---|---|
|
| |||
| % (N) | % (N) | % (N) | |
| Age | |||
| Mean (sd) | 46 (12) | 45 (13) | 46 (12) |
|
| |||
| 18-29 | 12 (66) | 15 (88) | 14 (154) |
| 30-49 | 43 (233) | 41 (236) | 42 (469) |
| 50-65 | 45 (244) | 44 (256) | 45 (500) |
|
| |||
| Gender | |||
|
| |||
| Male | 33 (178) | 37 (212) | 35 (390) |
| Female | 67 (365) | 63 (368) | 65 (733) |
|
| |||
| Marital Status | |||
|
| |||
| Currently married/living as married | 75 (407) | 75 (433) | 75 (840) |
|
| |||
| Education | |||
|
| |||
| ≤High School graduate | 30 (165) | 31 (177) | 30 (342) |
| Some College | 16 (87) | 16 (91) | 16 (178) |
| ≥College Graduate | 53 (289) | 53 (310) | 53 (599) |
|
| |||
| English Language Ability | |||
|
| |||
| Well/Fluent | 20 (110) | 21 (124) | 21 (234) |
| So so | 52 (280) | 48 (278) | 50 (558) |
| Poorly/Not at all | 28 (153) | 31 (177) | 29 (330) |
|
| |||
| Country of Birth | |||
|
| |||
| Korea | 97 (527) | 97 (560) | 97 (1087) |
| United States | 1 (6) | 3 (17) | 2 (23) |
|
| |||
| Years in the U.S. | |||
|
| |||
| Mean (sd) | 17 (11) | 16 (11) | 17 (11) |
|
| |||
| Household Income | |||
|
| |||
| >$80,000 | 17 (93) | 20 (116) | 19 (209) |
| $50,000-80,000 | 21 (113) | 19 (109) | 20 (222) |
| $30,000-50,000 | 23 (124) | 22 (125) | 22 (249) |
| <$30,000 | 21 (112) | 19 (110) | 20 (222) |
| DON'T KNOW/REFUSED | 19 (101) | 21 (120) | 20 (221) |
|
| |||
| Health Insurance | |||
|
| |||
| None | 59 (319) | 58 (334) | 58 (653) |
| Public Only | 4 (24) | 5 (29) | 5 (53) |
| Private Only | 36 (193) | 37 (213) | 36 (406) |
|
| |||
| Plan Type (for private) | |||
|
| |||
| HMO/PPO | 79 (157) | 81 (176) | 80 (333) |
| Catastrophic/Emergency/Surgery | 7 (13) | 3 (7) | 5 (20) |
| DON'T KNOW | 12 (24) | 14 (31) | 13 (55) |
|
| |||
| Have Usual Source of Care | |||
|
| |||
| Yes | 50 (143) | 48 (130) | 49 (273) |
|
| |||
| Type of Usual Source | |||
|
| |||
| Clinic or health center | 83 (118) | 75 (97) | 79 (215) |
| Traditional practitioner | 12 (17) | 17 (22) | 14 (39) |
| Other | 6 (8) | 8 (11) | 7 (19) |
There were no statistically significant differences between intervention and control participants at baseline. Compared to participants lost to follow-up, those completing the 6-month interview tended to be older (mean 46 vs. 42 years, p<.002) and have longer length of stay in the US (mean 17 vs. 14 years, p<.001). However, the outcome analysis was conducted using the intent-to-treat principle of including all participants in order to maintain the covariate balance created by randomization.
Intervention Effect
Table 3 presents the results of intent-to-treat analyses in which individuals lost to follow-up were assumed not tested for HBV. Overall, the intervention produced a statistically significant intervention effect (OR = 4.9, p < .001, 95% CI = 2.4 – 9.9), with 19% of intervention and 6% of control group participants reporting receipt of a HBV serologic test at the 6 month follow up. Sensitivity analysis using multiple imputation of missing outcomes also showed a significant intervention advantage, with estimated rates of 22.8% and 6.7% (OR = 4.8, p<.001, 95% CI = 2.5 – 9.2).
Table 3. Effect of the Intervention on Hepatitis B Testing Rates at 6 Month Follow-up.
| All Randomized Participants (n = 1123) | Randomized Participants Excluding those from Large, Koreatown Churches with Documented Contamination (n = 968) | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | OR (95% CI) | P | Intervention Group | Control Group | OR (95% CI) | P | |
| All Participants | 19% (104/543) | 6% (33/580) | 4.9 (2.4-9.9) | <.001 | 18% (77/440) | 4% (20/528) | 5.7 (3.1-10.3) | <.001 |
| By Size | ||||||||
| Small churches (51-200) | 17% (36/206) | 4% (9/218) | 5.3 (1.7-16.5) | .004 | 17% (36/206) | 4% (9/218) | 5.3 (1.7-16.5) | .004 |
| Medium churches (201-900) | 19% (30/161) | 4% (7/191) | 6.4 (2.5-16.3) | <.001 | 19% (30/161) | 4% (7/191) | 6.4 (2.5-16.3) | <.001 |
| Large churches (901+) | 22% (38/176) | 10% (17/171) | 3.1 (0.7-14.9) | .152 | 15% (11/73) | 3% (4/119) | 5.1 (1.2-21.3) | .026 |
| By Geographic Location | ||||||||
| Koreatown churches | 20% (50/247) | 11% (23/213) | 2.4 (0.8-7.0) | .105 | 16% (23/144) | 6% (10/161) | 2.9 (1.1-7.2) | .025 |
| Non-Koreatown churches | 18% (54/296) | 3% (10/367) | 8.6 (3.9-19.4) | <.001 | 18% (54/296) | 3% (10/367) | 8.6 (3.9-19.4) | <.001 |
Intent-to-treat analysis in which participants with missing outcome data were assumed not tested for HBV. Odds ratios and p-values are from mixed effects logistic regression accounting for clustering on church and session.
In stratified secondary analyses, statistically significant intervention effects were observed within small, medium and non-Koreatown churches (Table 3). Process data collected over the course of the study documented that three large Koreatown churches (1 control and 1 intervention church in the same pair and 1 additional intervention church) hosted free hepatitis B testing events during the follow-up period. For exploratory purposes, analyses were repeated after omitting the two church pairs in which one or both were contaminated (also in Table 3). In this restricted sample the overall effect of the intervention remained significant (OR=5.7, p<.001)and statistically significant intervention effects were also observed among large and Koreatown churches.
Discussion
Our theoretically informed and culturally tailored intervention was successful in increasing HBV testing in a large community sample of Koreans who are at high risk for HBV infection and associated risks for liver disease and liver cancer. The effect was large, with the odds of HBV testing in the intervention group nearly five times higher than in the control group. These findings are similar to those observed in controlled community trials targeting other Asian groups such as Cambodians (53), the Hmong (17) as well as a trial that included multiple Asian sub-groups (54).
Due to our large sample and our stratified design, we were also able to assess intervention effects by church size and location. This more nuanced analysis revealed interesting findings. Strong intervention effects were observed in small and medium churches and in non-Koreatown churches. In large churches and Koreatown churches the intervention failed to produce statistically significant effects although the data indicated trends favoring the intervention group. Process data collected during the course of the trial indicated that a community group had hosted free HBV testing events at three churches in our sample, between the baseline and follow-up data points of the affected churches. All three contaminated churches were large and located in Koreatown. Analyses omitting the two pairs of churches in which one or both members were contaminated resulted in consistent and robust intervention effects across all six strata in our design including large and Koreatown churches. These findings support the need for systematically attending to and cataloging events in community settings that are not within the control of the research team that could potentially affect the research design and/or the study findings. This is particularly important when employing cluster randomized designs with a small to medium number of randomized clusters as was the case in this study. If the effect of the external event is large, even a small number or proportion of contaminated clusters could lead to compromised findings.
Although the intervention had a large effect size, only 19% of intervention participants reported HBV testing at the 6-month follow-up, leaving the majority of the group untested. While these findings are similar to those obtained in other studies (17, 53, 54) they nevertheless raise questions regarding the efficiency of community-based interventions delivered in non-healthcare settings. Our intervention was guided by the HBF which is a broad conceptual framework that includes a complex mix of individual, healthcare system and community factors that could influence uptake of health behaviors. Not all of the factors are amenable to change via health interventions, and most programs do not have the resources to intervene on all possible mutable factors. Thus, our intervention focused primarily on individual level factors which may explain the modest uptake of HBV testing observed in the intervention group. Physician and/or healthcare system directed interventions, either alone or in combination with individual directed interventions, may produce larger effects (55). However, for immigrant groups with low health insurance coverage such as our Korean population, it is unlikely that health care system-based approaches would reach substantial proportions of the population. Also, more intensive community interventions (e.g., patient navigation, transportation assistance, free on-site testing, multiple contacts/reminders over time) might produce larger effects but would likely face resource challenges for dissemination and sustainability.
We recruited an immigrant sample of Koreans who experience what is considered the most significant health disparity affecting Asians in the U.S. (6), namely, a disproportionately high burden of HBV infection and liver cancer compared to the general U.S. population. Despite their elevated disease risk, only about 35% of Koreans in our study reported prior HBV serologic testing on our screener, further supporting the need for intervention research in this area. Similar underutilization of HBV testing has been reported in the literature for Koreans and other Asian groups in the U.S. (16, 17, 20, 23, 24, 26).
It is important to note that the demographic profile of Koreans in the U.S. (27), well reflected in our sample, does not fit neatly into common notions regarding immigrants experiencing health disparities; the latter group generally characterized as having a confluence of low income, low education, low healthcare access, and limited English proficiency. In our community sample of Koreans, 97% were immigrants, 80% had limited English fluency and only 40% had any type of health insurance. However, the insurance was mostly private and 50% reported having a usual source of care that was not an emergency room. Seventy percent of our sample had some college education, 53% had at least a college degree and 40% reported household incomes of over $50,000. The relatively low levels of insurance coverage are likely related to a very high proportion of the sample being employed in self or family owned small businesses (27). A thorough understanding of these and other characteristics of our target population (16) led us to select a community-based intervention, delivered at churches in a small group discussion format, and also informed our decision to provide a comparable intervention in the control condition as opposed to utilizing a usual care control group. Church leaders were strongly opposed to a delayed intervention design; thus, this option was considered unfeasible. Also, given the relatively high income level of our target group it was not unrealistic to expect participants to bear potential out-of-pocket costs of a HBV test, although we did provide a listing of clinics at which a test could be obtained free or at low cost.
There are several limitations to this study. First is the reliance on self-reports for measuring the main outcome of HBV testing. Positive response bias is likely to have inflated self-reports of testing. However, validation of self-reports through medical record review is impractical and costly in community settings in which participants are not recruited from a small number of clinical practices or an integrated health system, resulting in the need to contact numerous individual providers (56). Also, among populations without regular providers it is not clear which provider should be contacted for validation among those not reporting test receipt (17, 53, 56). Future studies conducted in settings more conducive to medical record verification may help shed light on the validity of self-reported HBV testing.
Another limitation is that the 52 participating churches may not be representative of the 127 churches invited to join the study or of Korean churches in other parts of the country. Also, participants were self-selected within churches and may have been particularly interested in health related topics. Still, the fact that our intervention was effective in churches of differing sizes and in those located in an ethnic enclave as well as those widely dispersed across a large county provides reasonable confidence in the generalizability of our findings.
In conclusion, we successfully implemented a cluster-randomized trial in a population at high risk of HBV infection and sequelae. Our intervention conducted at Korean churches achieved a large and robust intervention effect. However, the actual proportion of individuals in the intervention group that received HBV testing was modest suggesting that more intensive interventions and interventions conducted in settings other than churches may be needed to achieve higher population level coverage rates.
Acknowledgments
We would like to acknowledge the significant contributions of Mr. Hosung Kim, Ms. Min Jung Sung, and Dr. Jennifer Cha in implementing study activities in the community. We also want to thank the many additional community members that provided assistance with the project, the participating churches, and the Asian Pacific Liver Center that served as a community resource for low cost hepatitis B testing services.
Financial Support: This publication was supported by Grants P01 CA109091-01A1 (P01 PI: M.S. Chen, Component Project PI: R. Bastani), U54CA153499 (PI: M.S. Chen), U01CA114640 (PI: M.S. Chen) and P30 CA16042 from the NIH, National Cancer Institute.
Footnotes
Conflict of interest statement: No financial disclosures were reported by any of the authors.
References
- 1.Kowdley KV, Wang CC, Welch S, Roberts H, Brosgart CL. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology. 2012;56:422–33. doi: 10.1002/hep.24804. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Hepatitis B Factsheet World Health Organization. 2014 [Google Scholar]
- 3.Mitchell T, Armstrong GL, Hu DJ, Wasley A, Painter JA. The increasing burden of imported chronic hepatitis B--United States, 1974-2008. PloS one. 2011;6:e27717. doi: 10.1371/journal.pone.0027717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen TT, Taylor VM, Maxwell AE, Chen MS, Jr, Bastani R, Stewart SL. In: Handbook of Asian American Health. Yoo GJ, Le MN, Oda AY, editors. New York: Springer-Verlag; 2012. pp. 251–65. [Google Scholar]
- 5.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports /Centers for Disease Control. 2008;57:1–20. [PubMed] [Google Scholar]
- 6.McCracken M, Olsen M, Chen MS, Jr, Jemal A, Thun M, Cokkinides V, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA: a cancer journal for clinicians. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 7.Beasley RP. Hepatitis B virus. The major etiology of hepatocellular carcinoma. Cancer. 1988;61:1942–56. doi: 10.1002/1097-0142(19880515)61:10<1942::aid-cncr2820611003>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 8.Blumberg BS, London WT. Hepatitis B virus: pathogenesis and prevention of primary cancer of the liver. Cancer. 1982;50:2657–65. [PubMed] [Google Scholar]
- 9.Chen CJ, Yu MW, Liaw YF. Epidemiological characteristics and risk factors of hepatocellular carcinoma. Journal of gastroenterology and hepatology. 1997;12:S294–308. doi: 10.1111/j.1440-1746.1997.tb00513.x. [DOI] [PubMed] [Google Scholar]
- 10.Misra R, Jiobu K, Zhang J, Liu Q, Li F, Kirkpatrick R, et al. Racial disparities in hepatitis B infection in Ohio: screening and immunization are critical for early clinical management. Journal of investigative medicine : the official publication of the American Federation for Clinical Research. 2013;61:1121–8. doi: 10.2310/JIM.0b013e3182a70f10. [DOI] [PubMed] [Google Scholar]
- 11.Pollack HJ, Kwon SC, Wang SH, Wyatt LC, Trinh-Shevrin C, Coalition A. Chronic Hepatitis B and Liver Cancer Risks among Asian Immigrants in New York City: Results from a Large, Community-Based Screening, Evaluation, and Treatment Program. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2014;23:2229–39. doi: 10.1158/1055-9965.EPI-14-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hutton DW, Brandeau ML, So SK. Doing Good with Good OR: Supporting Cost-effective Hepatitis B Interventions. Interfaces. 2011;41:289–300. doi: 10.1287/inte.1100.0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chou R, Dana T, Bougatsos C, Blazina I, Khangura J, Zakher B. Screening for hepatitis B virus infection in adolescents and adults: a systematic review to update the U.S. Preventive Services Task Force recommendation. Annals of internal medicine. 2014;161:31–45. doi: 10.7326/M13-2837. [DOI] [PubMed] [Google Scholar]
- 14.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 15.Kim WR. Epidemiology of hepatitis B in the United States. Hepatology. 2009;49:S28–34. doi: 10.1002/hep.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bastani R, Glenn BA, Maxwell AE, Jo AM. Hepatitis B testing for liver cancer control among Korean Americans. Ethnicity & disease. 2007;17:365–73. [PubMed] [Google Scholar]
- 17.Chen MS, Jr, Fang DM, Stewart SL, Ly MY, Lee S, Dang JH, et al. Increasing hepatitis B screening for hmong adults: results from a randomized controlled community-based study. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22:782–91. doi: 10.1158/1055-9965.EPI-12-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu DJ, Xing J, Tohme RA, Liao Y, Pollack H, Ward JW, et al. Hepatitis B testing and access to care among racial and ethnic minorities in selected communities across the United States, 2009-2010. Hepatology. 2013;58:856–62. doi: 10.1002/hep.26286. [DOI] [PubMed] [Google Scholar]
- 19.Pollack H, Wang S, Wyatt L, Peng CH, Wan K, Trinh-Shevrin C, et al. A comprehensive screening and treatment model for reducing disparities in hepatitis B. Health affairs. 2011;30:1974–83. doi: 10.1377/hlthaff.2011.0700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. Journal of community health. 2012;37:1071–80. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanaka M, Gehan E, Chen MY, Wang JH. Hepatitis B screening practice among older Chinese in the Greater Washington, DC, area. Southern medical journal. 2014;107:655–60. doi: 10.14423/SMJ.0000000000000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pacific journal of cancer prevention : APJCP. 2007;8:127–34. [PubMed] [Google Scholar]
- 23.Nguyen TT, McPhee SJ, Stewart S, Gildengorin G, Zhang L, Wong C, et al. Factors associated with hepatitis B testing among Vietnamese Americans. Journal of general internal medicine. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor VM, Talbot J, Do HH, Liu Q, Yasui Y, Jackson JC, et al. Hepatitis B knowledge and practices among Cambodian Americans. Asian Pacific journal of cancer prevention : APJCP. 2011;12:957–61. [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor VM, Tu SP, Woodall E, Acorda E, Chen H, Choe J, et al. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pacific journal of cancer prevention : APJCP. 2006;7:313–7. [PubMed] [Google Scholar]
- 26.Ma G, Tan Y, Wang M, Yuan Y, Chae W. Hepatitis B Screening Compliance and Non Compliance among Chinese, Koreans, Vietnamese and Cambodians. Clinical Medicine: Gastroenterology. 2010;3:1–10. doi: 10.4137/CGast.S3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pew Research Center. The Rise of Asian Americans. Washington, D.C.: Pew Research Center; 2012. [Google Scholar]
- 28.Altekruse SF, Henley SJ, Cucinelli JE, McGlynn KA. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. The American journal of gastroenterology. 2014;109:542–53. doi: 10.1038/ajg.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma GX, Gao W, Tan Y, Chae WG, Rhee J. A community-based participatory approach to a hepatitis B intervention for Korean Americans. Progress in community health partnerships : research, education, and action. 2012;6:7–16. doi: 10.1353/cpr.2012.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jo AM, Maxwell AE, Choi S, Bastani R. Interest in health promotion among Korean American Seventh-day Adventists attending a religious retreat. Asian Pacific journal of cancer prevention : APJCP. 2012;13:2923–30. doi: 10.7314/apjcp.2012.13.6.2923. [DOI] [PubMed] [Google Scholar]
- 31.Juon HS, Choi Y, Kim MT. Cancer screening behaviors among Korean-American women. Cancer detection and prevention. 2000;24:589–601. [PubMed] [Google Scholar]
- 32.Min PG, Kim JH. Religions in Asian America : building faith communities Critical perspectives on Asian Pacific Americans series. Walnut Creek, CA: AltaMira Press; 2002. pp. 185–213. [Google Scholar]
- 33.Jo AM, Maxwell AE, Yang B, Bastani R. Conducting health research in Korean American churches: perspectives from church leaders. Journal of community health. 2010;35:156–64. doi: 10.1007/s10900-009-9213-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee HB, Hanner JA, Cho SJ, Han HR, Kim MT. Improving access to mental health services for korean american immigrants: moving toward a community partnership between religious and mental health services. Psychiatry investigation. 2008;5:14–20. doi: 10.4306/pi.2008.5.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Juon HS, Strong C, Oh TH, Castillo T, Tsai G, Oh LD. Public health model for prevention of liver cancer among Asian Americans. Journal of community health. 2008;33:199–205. doi: 10.1007/s10900-008-9091-y. [DOI] [PubMed] [Google Scholar]
- 36.Ma GX, Shive S, Tan Y, Gao W, Rhee J, Park M, et al. Community-based colorectal cancer intervention in underserved Korean Americans. Cancer epidemiology. 2009;33:381–6. doi: 10.1016/j.canep.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 37.Allicock M, Johnson LS, Leone L, Carr C, Walsh J, Ni A, et al. Promoting fruit and vegetable consumption among members of black churches, Michigan and North Carolina, 2008-2010. Preventing chronic disease. 2013;10:E33. doi: 10.5888/pcd10.120161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maxwell AE, Bastani R, Danao LL, Antonio C, Garcia GM, Crespi CM. Results of a community-based randomized trial to increase colorectal cancer screening among Filipino Americans. American journal of public health. 2010;100:2228–34. doi: 10.2105/AJPH.2009.176230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sauaia A, Min SJ, Lack D, Apodaca C, Osuna D, Stowe A, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Preventing chronic disease. 2007;4:A99. [PMC free article] [PubMed] [Google Scholar]
- 40.Bastani R, Glenn BA, Taylor VM, Chen MS, Jr, Nguyen TT, Stewart SL, et al. Integrating theory into community interventions to reduce liver cancer disparities: The Health Behavior Framework. Preventive medicine. 2010;50:63–7. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diallo DD, Moore TW, Ngalame PM, White LD, Herbst JH, Painter TM. Efficacy of a single-session HIV prevention intervention for black women: a group randomized controlled trial. AIDS and behavior. 2010;14:518–29. doi: 10.1007/s10461-010-9672-5. [DOI] [PubMed] [Google Scholar]
- 42.Drake BF, Shelton RC, Gilligan T, Allen JD. A church-based intervention to promote informed decision making for prostate cancer screening among African American men. Journal of the National Medical Association. 2010;102:164–71. doi: 10.1016/s0027-9684(15)30521-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paskett ED, Tatum CM, D'Agostino R, Jr, Rushing J, Velez R, Michielutte R, et al. Community-based interventions to improve breast and cervical cancer screening: results of the Forsyth County Cancer Screening (FoCaS) Project. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 1999;8:453–9. [PubMed] [Google Scholar]
- 44.Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public health reports. 2001;116(Suppl 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maxwell AE, Bastani R, Glenn BA, Taylor VM, Nguyen TT, Stewart SL, et al. Developing theoretically based and culturally appropriate interventions to promote hepatitis B testing in 4 Asian American populations, 2006-2011. Preventing chronic disease. 2014;11:E72. doi: 10.5888/pcd11.130245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marin G, Sabogal F, Vanoss Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a Short Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- 47.Maxwell AE, Bastani R, Chen MS, Jr, Nguyen TT, Stewart SL, Taylor VM. Constructing a theoretically based set of measures for liver cancer control research studies. Preventive medicine. 2010;50:68–73. doi: 10.1016/j.ypmed.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Earp JA, Eng E, O'Malley MS, Altpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: results from a community trial. American journal of public health. 2002;92:646–54. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Slater JS, Ha CN, Malone ME, McGovern P, Madigan SD, Finnegan JR, et al. A randomized community trial to increase mammography utilization among low-income women living in public housing. Preventive medicine. 1998;27:862–70. doi: 10.1006/pmed.1998.0370. [DOI] [PubMed] [Google Scholar]
- 50.Feng Z, Diehr P, Yasui Y, Evans B, Beresford S, Koepsell TD. Explaining community-level variance in group randomized trials. Statistics in medicine. 1999;18:539–56. doi: 10.1002/(sici)1097-0258(19990315)18:5<539::aid-sim50>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 51.Royston P. Multiple imputation of missing values: update. Stata Journal. 2005;5:1–14. [Google Scholar]
- 52.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- 53.Taylor VM, Bastani R, Burke N, Talbot J, Sos C, Liu Q, et al. Evaluation of a hepatitis B lay health worker intervention for Cambodian Americans. Journal of community health. 2013;38:546–53. doi: 10.1007/s10900-012-9649-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Juon HS, Lee S, Strong C, Rimal R, Kirk GD, Bowie J. Effect of a liver cancer education program on hepatitis B screening among Asian Americans in the Baltimore-Washington metropolitan area, 2009-2010. Preventing chronic disease. 2014;11:130258. doi: 10.5888/pcd11.130258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsu L, Bowlus CL, Stewart SL, Nguyen TT, Dang J, Chan B, et al. Electronic messages increase hepatitis B screening in at-risk Asian American patients: a randomized, controlled trial. Digestive diseases and sciences. 2013;58:807–14. doi: 10.1007/s10620-012-2396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bastani R, Glenn BA, Maxwell AE, Ganz PA, Mojica CM, Chang LC. Validation of self-reported colorectal cancer (CRC) screening in a study of ethnically diverse first-degree relatives of CRC cases. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2008;17:791–8. doi: 10.1158/1055-9965.EPI-07-2625. [DOI] [PubMed] [Google Scholar]