Abstract
In angiotensin (Ang) II-dependent hypertension, collecting duct renin synthesis and secretion are stimulated despite suppression of juxtaglomerular (JG) renin. This effect is mediated by Ang II type 1 (AT1) receptor independent of blood pressure. Although the regulation of JG renin is known, the mechanisms by which renin is regulated in the collecting duct are not completely understood. The presence of renin activity in the collecting duct may provide a pathway intratubular AngII formation since angiotensinogen substrate and angiotensin converting enzyme are present in the distal nephron. The recently named new member of the renin angiotensin system (RAS), the (pro)renin receptor ((P)RR) is able to bind renin and the inactive prorenin, thus enhancing renin activity and fully activating prorenin. We have demonstrated that renin and (P)RR, are augmented in renal tissues from rats infused with Ang II and during sodium depletion, suggesting a physiological role in intrarenal RAS activation. Importantly, (P)RR activation also causes activation of intracellular pathways associated with increased cyclooxygenase-2 expression and induction of profibrotic genes. In addition, renin and the (P)RR are upregulated by Ang II in collecting duct cells. Although the mechanisms involved in their regulation are still under study, they seem to be dependent on the intrarenal RAS activation. The complexities of the mechanisms of stimulation also depend on cyclooxygenase-2 and sodium depletion. Our data suggest that renin and (P)RR can interact to increase intratubular Ang II formation and the activation of profibrotic genes in renal collecting duct cells. Both pathways may have a critical role in the development of hypertension and renal disease.
Keywords: Angiotensin II dependent hypertension, renin angiotensin system, signalling pathways
Introduction
Although the renin-angiotensin system (RAS) plays a major role in the physiological control of blood pressure and fluid volume, it also potentially contributes to the development and progression of hypertension and fibrotic and hypertrophic diseases. Beside the systemic RAS, which is mainly controlled by the production and release of renin from the juxtaglomerular (JG) cells in the kidneys, local RAS present in a variety of organs are also important particularly along the nephron. Renin is primarily synthesized in the JG cells where is stimulated by a number of signals that increase intracellular cyclic adenyl mono-phosphate (cAMP) levels and activation of protein kinase A (PKA) (Castrop et al. 2010). The 5′-flanking non-coding region of the renin gene (Borensztein et al. 1994; Castrop et al. 2010) plays a central role in regulating renin expression in all species. This region is considered the classic renin gene promoter. The presence of a functional cAMP response element (CRE) is a characteristic feature of the renin promoter in all species; cAMP binds to the two regulatory subunits of protein kinase A (PKA) to release two catalytic subunits from the inactive PKA tetramer complex. The free catalytic subunits (referred to as activated PKA) translocate to the nucleus and phosphorylate transcription factors of the cAMP response element binding protein/activating transcription factor CREB.
In contrast to the stimulatory effect on cAMP, angiotensin (Ang) II inhibits renin gene expression and secretion from JG cells by increasing the cytosolic calcium and activating protein kinase C (PKC) (Muller et al. 2002). The presence of prorenin and renin has been demonstrated in renal collecting ducts (Seikaly et al. 1990; Prieto-Carrasquero et al. 2004; Prieto-Carrasquero et al. 2005; Prieto-Carrasquero et al. 2008; Prieto-Carrasquero et al. 2009; Prieto et al. 2013; Rohrwasser et al. 1999; Rohrwasser et al. 2003). Furthermore, it has been reported that Ang II increases renin expression in the collecting duct cells in vitro and in vivo (Gonzalez et al. 2011b) which is opposite to what has been observed in JG cells (Muller et al. 2002). These findings are of great relevance in the view that angiotensinogen (AGT) and angiotensin converting enzyme (ACE) are also present along the nephron and are also upregulated by chronic Ang II-infusions (Kobori et al. 2001; Gonzalez-Villalobos et al. 2010), indicating that augmented collecting duct renin may contribute to further intratubular Ang II formation in the distal nephron segments.
With the discovery and characterization of the new member of the RAS, the (pro)renin receptor ((P)RR), a new spectrum of possibilities and pathways with potential roles in the pathogenesis of hypertension and kidney disease have been proposed. The (P)RR is an ATPase H(+)-transporting lysosomal accessory protein (ATP6AP2), but also acts a membrane receptor of renin and prorenin. The binding of the (P)RR to renin and prorenin enhances renin activity and fully activating the biologically inactive prorenin (Nguyen & Contrepas 2008; Nguyen & Muller 2010), thus contributing to a further Ang I formation inside the kidneys (Nguyen et al. 2002). Additionally, binding of prorenin and renin to the membrane bound (P)RR triggers intracellular pathways which have been related to tissue damage (Nguyen et al. 1996; Nguyen & Danser 2006). In this review we will discuss the evidence demonstrating that the principal cells of the collecting duct synthesize and secrete renin/prorenin in response to the physiological activation of the RAS with low sodium diet, as well as to Ang II treatment. We will also deliberate about the presence of the (P)RR in the intercalated cells and its interaction with renin/prorenin in the collecting duct and their possible role in regulating intrarenal Ang II levels during intrarenal RAS activation.
Intrarenal renin angiotensin system: evidence of the augmented expression of AGT and ACE during hypertension
Angiotensin I and Ang II concentrations in the proximal tubule fluid are in the range of 5–10 pmol/ml (Navar & Harrison-Bernard 2000; Navar et al. 2001; Navar et al. 2002), which are similar to renal interstitial fluid concentrations (Nishiyama et al. 2001) and remain elevated in infused hypertensive rats (Wang et al. 2003), suggesting actions on proximal reabsorption rate. The presence of AT1 receptors on luminal membranes of proximal and distal nephron segments suggested that Ang II concentrations are able to activate AT1 receptors (Peti-Peterdi et al. 2002; Komlosi et al. 2003). In mice, AT1a receptors are essential for normal blood pressure regulation and for mediating the hypertensive response to Ang II infusions (Crowley et al. 2006). These studies indicate that distal nephron Ang II is formed locally in the tubules at concentrations that are sufficiently high to influence distal nephron transport function (Peti-Peterdi et al. 2002; Komlosi et al. 2003).
Angiotensinogen mRNA is present in the proximal tubule cells (Kobori et al. 2001; Kobori et al. 2002; Kobori et al. 2003). This observation generated interest about its function. A breakthrough was the publication of several reports describing the augmentation of mRNA and urinary excretion in chronic Ang II infusion model(Kobori et al. 2002; Kobori et al. 2003). This effect is mediated via activation of AT1R, since AT1R blockers prevented AGT upregulation (Kobori et al. 2004). Similarly, in vitro studies using proximal tubule cell cultures show that Ang II stimulates AGT mRNA and protein by a mechanism that involves the interactions with inflammatory factors including interleukin (Satou et al. 2009) and oxidative stress (Satou et al. 2008; Satou et al. 2012). The role of AGT in hypertension has been established using genetic models that lead to overexpression of AGT. Angiotensinogen may be used as a marker, reflecting the intratubular RAS status that is correlated with kidney Ang II levels in Ang II-dependent hypertensive rats (Kobori et al. 2003; Kobori et al. 2002). Recently, direct quantitative methods to measure urinary AGT using human/mouse/rat AGT ELISA have been developed (Kobori et al. 2008). Using this system, urinary excretion rates of AGT have been used as an index of intrarenal RAS status in patients with chronic kidney disease (Yamamoto et al. 2007), diabetes mellitus (Ogawa et al. 2009), and hypertension (Lantelme et al. 2005; Kobori et al. 2010). Importantly, patients treated with RAS blockers showed reduced urinary AGT levels (Kobori et al. 2003).
Angiotensin converting enzyme is another key enzyme of the RAS that is also present in collecting duct (Vio & Jeanneret 2003)This enzyme allows the conversion of most of the Ang I into Ang II and there are evidence demonstrating that ACE is augmented in Ang II-dependent hypertension (Harrison-Bernard et al. 2002; Gonzalez-Villalobos et al. 2009; Gonzalez-Villalobos et al. 2010) and other models of kidney injuries (Vio & Jeanneret 2003). These findings, along with the demonstration that proximal tubule cells express AGT and that ACE activity is also present in the collecting ducts (Redublo Quinto et al. 2008; Casarini et al. 1997) support an important physiological role of tubular renin.
Prorenin and renin synthesis in the collecting duct cells is augmented by Ang II in vitro and during physiological RAS activation
Besides its primary localization in the JG cells, renin mRNA and protein expression is also present in renal tubules (Rohrwasser et al. 1999; Rohrwasser et al. 2003; Prieto-Carrasquero et al. 2004; Prieto-Carrasquero et al. 2005; Prieto-Carrasquero et al. 2008). Renin synthesis is augmented in the principal cells of connecting tubules and cortical and medullary collecting ducts of chronic Ang II-infused rats and mice, Cyp1a1Ren2 transgenic rats, and in both kidneys of two-kidney one clip Goldblatt hypertensive rats. (Rohrwasser et al. 1999; Rohrwasser et al. 2003; Prieto-Carrasquero et al. 2004; Prieto-Carrasquero et al. 2005; Prieto-Carrasquero et al. 2008).
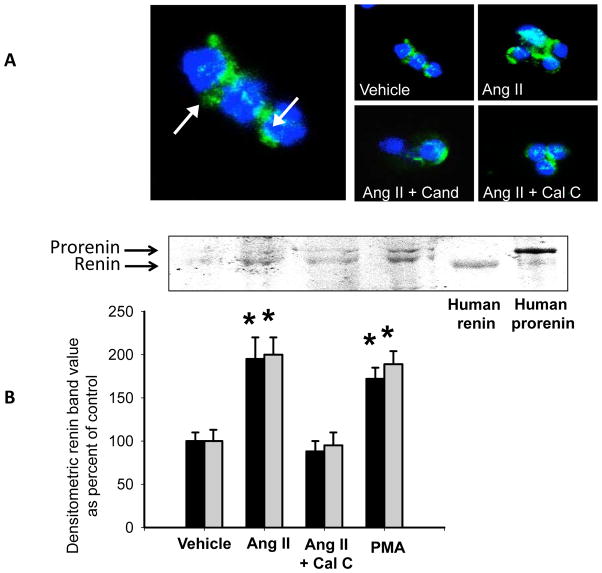
In contrast to the inhibitory effect that Ang II exerts on JG renin, Ang II stimulates renin in the principal collecting duct cells via a mechanism mediated by the Ang II type 1 receptor (AT1R) independent of changes in blood pressure (Prieto-Carrasquero et al. 2004; Prieto-Carrasquero et al. 2005; Prieto-Carrasquero et al. 2008). Activation of AT1R suppresses renin synthesis in JG cells via protein kinase C (PKC) and Ca+2 (Kurtz & Wagner 1999); however, we demonstrated that augmentation of renin synthesis in rat inner medullary collecting duct cells is mediated directly by AT1R via a PKC pathway (Gonzalez et al. 2011b). Figure 1A shows renin immunostaining in a typical scattered pattern in isolated inner medullary collecting ducts (IMCD) cells (arrows). In IMCD cultured cells, renin immunostaining is augmented after Ang II treatment (10−7 M) during 6 h. As shown in Figure 1B, prorenin-renin bands can be identified in cell lysates of IMCD cells. Treatment with Ang II increases prorenin (195 ± 25%, P<0.05) and renin (200 ± 20%, P<0.05) abundance compared to controls. Treatment with PKC inhibitor, calphostin C prevented the stimulatory effect of Ang II on prorenin (88 ± 12%, P=0.56) and renin (95 ± 15%, P=0.23). The phorbol ester PMA, a PKC activator, greatly increases prorenin (172 ± 13%, P<0.05) and renin (189 ± 15%, P<0.05) as compared to controls.
Figure 1.
Immunocytochemical evidence of prorenin-renin expression in freshly isolated renal inner medullary collecting duct cells. A. Prorenin-renin immunostaining was detected as a punctuated pattern (arrows). Treatment with Ang II 10-7 mol/L increased immunostaining signal and prorenin and renin protein levels analysed by western blot (B). Candesartan (an AT1 receptor blocker) and calphostin c (a PKC inhibitor) supressed the Ang II-mediated increases in prorenin-renin. Cell identity was confirmed by using recombinant prorenin and renin standards as described in Liu et al., 2011.
The augmented levels of renin in the collecting duct in Ang II-dependent hypertensive rats may explain why newly Ang II is formed intratubularly in this animal model of hypertension (Shao et al. 2009; Shao et al. 2010). Recently, our group also showed that during low salt conditions (14 days), a physiological status of RAS activation, renin was augmented in medullary tissues (Shao et al. 2013). In a recent publication we also demonstrated that a short period of 7 days of sodium depletion can also induce the expression of renin mRNA and protein in medullary renal tissues (Gonzalez et al. 2014b), suggesting that renin synthesis is stimulated during low sodium diet. These observations suggest that the induction of intrarenal RAS may promote further Ang II acting directly to enhance sodium reabsorption (Peti-Peterdi et al. 2002; Komlosi et al. 2003).
Recently Ramkumar et al., generated mice with overexpression of renin in the collecting duct (Ramkumar et al. 2013a). They demonstrated a 5-fold in collecting duct renin mRNA levels in renal medulla and higher blood pressure in transgenic mice compared to control animals, suggesting that renin in the collecting duct modulate blood pressure (Ramkumar et al. 2013b; Ramkumar et al. 2013a; Ramkumar & Kohan 2013). Further studies are necessary to establish the mechanisms by which Ang II enhances renin and (P)RR synthesis and the postranscriptional events involved.
The (Pro)renin receptor, cyclooxygenase-2 and RAS activation
The discovery of a receptor for renin and prorenin, the (P)RR, has brought new perspectives about the possible roles of the (P)RR in settings of activated intrarenal RAS. The (P)RR is expressed in the kidneys particularly in mesangial cells, podocytes, and intercalated type A cells of collecting ducts (Ichihara et al. 2007; Ichihara et al. 2008; Ichihara 2012; Gonzalez et al. 2011a). The (P)RR was described as an associated protein with the V-ATPase (vacuolar H+-ATPase), giving the name to the gene ATP6AP2 (ATPase 6 accessory protein 2/(P)RR). The (P)RR binds renin and prorenin with an affinity in the nanomolar range and their binding triggers a range of cellular events like mitogen activated kinases (MAPKs) extracellular-signal-regulated kinases (ERK 1/2). Importantly, the actions of the (P)RR has been linked to diabetes nephropathy (Satofuka et al. 2009; Matavelli et al. 2010). Despite the low levels of plasma renin in patients with diabetic nephropathy, high levels of plasma prorenin detected in these patients are associated with occurrence of microvascular complications, microalbuminuria and retinopathy (Deinum et al. 1999). The (P)RR can activate inflammatory responses in diabetic kidneys. For example, the overexpression of (P)RR leads to augmentation of cycloocygenase-2 (COX-2) (Kaneshiro et al. 2006). Blockade of prorenin binding to the (P)RR is able to prevent and even reverse diabetic nephropathy (Ichihara et al. 2004). Synthesis of prorenin is also augmented in the collecting ducts in diabetic nephropathy (Kang et al. 2008), which may contribute to the activation of (P)RR and signalling pathways that promote tubular damage. Preliminary data from our group suggested that activation of (P)RR using recombinant prorenin is able to increase the expression of profibrotic genes (data not shown). However, it has been shown that intratubular Ang II can also promotes tubular fibrosis (Ishidoya et al. 1995) and that collecting duct cells have the predisposition to epithelial-mesenchymal transition (Ivanova et al. 2008; Butt et al. 2007). We demonstrated in vitro evidence that Ang II treatment of collecting duct cells stimulates fibronectin and collagen I, both markers of fibrosis, via β-catenin pathway (Cuevas et al. 2014). Further studies are necessary to fully elucidate whether the stimulation of tubular fibrosis during intrarenal RAS activation is dependent or independent of an Ang II-mediated mechanism, i.e., the direct activation of the (P)RR by prorenin in the collecting duct.
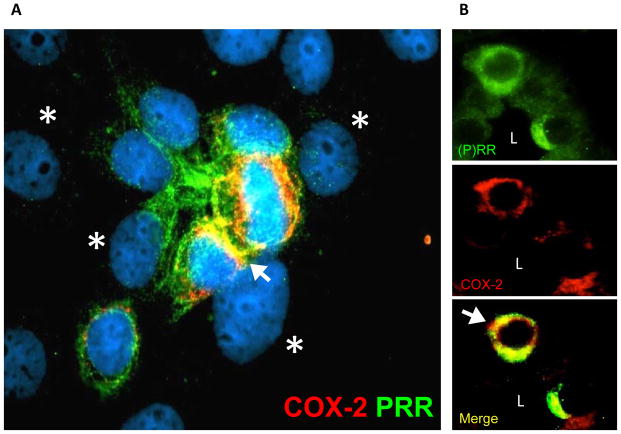
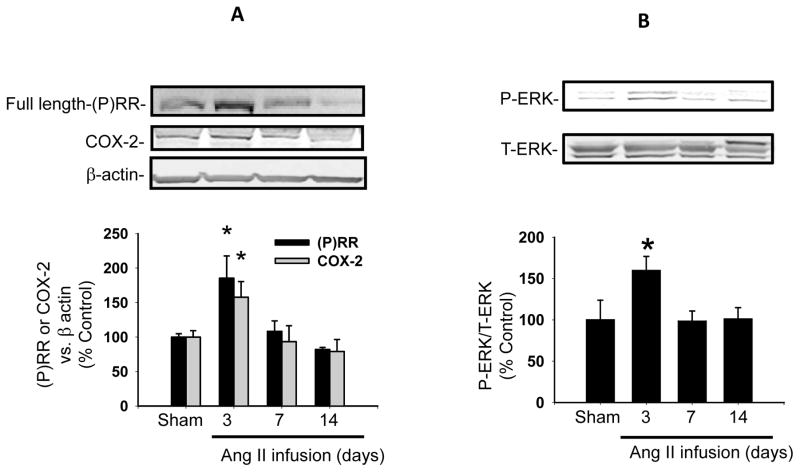
Due to the demonstrations that (P)RR activation upregulates COX-2 via ERK 1/2 pathways (Kaneshiro et al. 2006) contributing to inflammatory process in renal cortex, is it also important to evaluate what are the effects of (P)RR stimulation and overexpression in distal nephron segments and interstitial cells. We have recently reported that (P)RR and COX-2 are co-expressed in intercalated cells of the inner medullary collecting ducts (Gonzalez et al. 2013) In Figure 2A, a co-localization of COX-2 and (P)RR in freshly isolated IMCDs showed that both proteins co-exists in the same cell type (for further characterization of specific markers please see reference Gonzalez et al 2013). This co-localization was also observed in vivo (Figure 2B). We have also shown that activation of the (P)RR) using a recombinant prorenin is able to increase ERK 1/2 phosphorylation in cultured IMCD cells (Figure 3A, modified from (Gonzalez et al. 2013). As shown in Figure 3B, (P)RR activation also increases COX-2 expression (modified from Gonzalez et al. 2013). This is important in the view that the inner medulla COX-2 metabolites play a crucial role in the maintenance of sodium/water balance and appropriate vascular tone responses during RAS activations, thus, activation of COX-2 and synthesis of COX-2 metabolites may have a role not only in inflammatory responses but also in the maintenance of the buffer mechanism against the anti-natriuretic effects of RAS activation.
Figure 2.
Evidence for (P)RR and COX-2 expression in intercalated cells of the collecting duct. A. Primary cultured renal inner medullary collecting duct cells stained with anti-(P)RR (green signal) and anti-COX-2 (red signal) antibodies. Yellow color (Merge) indicates co-localization in intercalated cells (arrows). Asterisks indicate principal cells which are non stained with (P)RR antibodies. B. co-localization of (P)RR and COX-2 in rat kidney sections demonstrating the expression of COX-2 and (P)RR in intercalated cells (arrow). L; lumen.
Figure 3.
Recombinant prorenin increases ERK 1/2 phosphorylation and COX-2 expression in primary cultured rat renal inner medullary collecting duct cells. A. Time dependent ERK1/2 phosphorylation levels reached maximal levels at 15 min. B. COX-2 protein levels was induced after 3 hours of recombinant prorenin incubations and was still significant after 16 hours. *P<0.05 versus control group. Modified from Gonzalez et al., 2013.
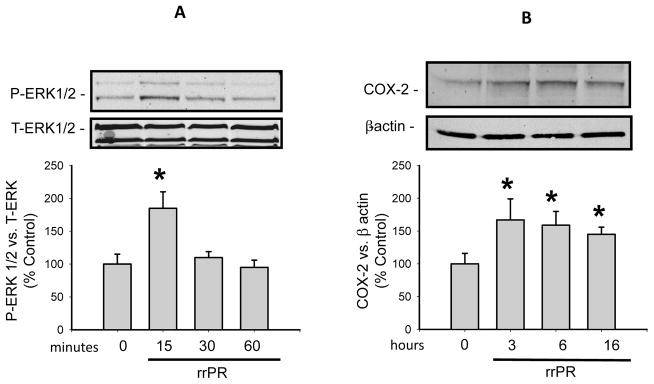
Common pathways in the regulations of the (P)RR and COX-2 seems to be shared by these two proteins in renal medulla (Gonzalez et al. 2014a; Gonzalez et al. 2013; Wang et al. 2014a; Wang et al. 2014b). We examined the time dependent pattern of the expression of COX-2 and (P)RR in Ang II-dependent hypertensive rats, since both are augmented in response to chronic Ang II infusions during 3, 7 and 24 days (Gonzalez et al. 2014a). Our data showed that in the early phase of Ang II-dependent hypertension, COX-2 and (P)RR are upregulated in the inner medulla (Figure 4A), this response was associated with increased ERK 1/2 phosphorylation levels (Figure 4B). We did not observe this pattern at 14 days; COX-2 was not different from non infused normotensive rats, and interestingly full length (P)RR was reduced, but s(PRR) was increased (Gonzalez et al. 2011a; Gonzalez et al. 2014a). Furthermore, in immunoprecipitation studies, we shown that renin – (P)RR interaction in hypertensive animals. Taken together, this line of evidence suggests that the (P)RR activation increases COX-2 in the renal medulla. Thus, the interaction between the (P)RR and renin or prorenin in plasma, interstitial space or in tubular fluids may play a physiological role. The and prorenin levels in the plasma are not correlated with plasma renin activity in some diseases (Deinum et al. 1999), suggesting that the final effect of the interaction between prorenin and (P)RR may depend on tissue specific expression levels of them. Also, further studies are needed to elucidate the real contribution of the full length and the soluble form of the (P)RR to the increases of intrarenal Ang II generation and intracellular pathways involved with tissue damage.
Figure 4.
Time dependent expression of (P)RR and COX-2 in renal medullary tissues of Ang II infused rats. A. Medullary protein levels of the full length form of (P)RR and COX-2 in 3, 7 and 14 days of Ang II infusions. B. ERK 1/2 phosphorylation levels in renal medullary tissues in rats Ang II infused by 3, 7 and 14 days. *P<0.05 versus control group. Modified from Gonzalez et al., 2013.
Conclusions and Perspectives
Evidence over the past 10 years of studies in this field indicates that in hypertensive models of Ang II-dependent hypertension, increased renal (P)RR transcript levels (Gonzalez et al. 2011a), as well as renin synthesis and secretion in the distal nephron segments (Prieto-Carrasquero et al. 2004; Prieto-Carrasquero et al. 2005; Prieto-Carrasquero et al. 2008; Liu et al. 2012) provide a pathway for enhanced tubular Ang II formation and the activation of intracellular pathways via (P)RR. Nguyen and associates originally reported the presence of (P)RR predominantly in glomerular mesangial cells and in vascular smooth muscle cells of renal arteries using immunofluorescence on frozen kidney tissues (Nguyen et al. 2003). The same group described the immunoexpression of the (P)RR on the basolateral side of distal tubular cells as well as in macula densa cells (Nguyen et al. 2002). This particular cell-side localization of the (P)RR might be also important for regulating Ang II levels in the renal interstitium. The increases in collecting duct renin, (P)RR gene expression and s(P)RR activity may have a key role in mediating local augmentation of intrarenal angiotensin peptides content, since there is plenty ACE activity in the distal nephron segments (Casarini et al. 1997; Komlosi et al. 2003; Quinto et al. 2002). Augmented intrarenal Ang II content contributes to the pathogenesis of hypertension through sustained stimulation of Na+ reabsorption, renal vasoconstriction, and to the development of renal injury (Navar LG., et al 2011). The demonstrations showing that mice infused chronically with Ang II enhance distal sodium reabsorption (Zhao & Navar 2008; Zhao et al. 2009) emphasize further the importance that renin and (P)RR interaction may have in the distal nephron segments.
Siragy and associates showed the effects of low sodium diet on (P)RR expression (Matavelli et al. 2012; Huang & Siragy 2012) in the proximal tubule. Data from our group and others, also suggest that (P)RR expression is augmented during low sodium diet (Matavelli et al. 2012; Huang & Siragy 2012; Gonzalez et al. 2014b). Coincidently with the augmented (P)RR expression in renal medulla from rats fed a low salt diet (0.03% NaCl), renin activity in inner medulla, as well as mRNA and protein expression are increased as compared to normal salt diet (0.4% NaCl). These data is concurrent with findings in freshly isolated rat IMCDs grown in natural hyperosmotic conditions with preferential selectivity for IMCD principal and intercalated cells, which also exhibit increased (P)RR mRNA levels after sodium reduction (from ~280 mmol/L NaCl to ~140 mmol/L). Both proteins, (P)RR and renin, respond to Ang II by increasing their expressions in isolated medullary collecting duct cells, indicating that Ang II regulates renin and (P)RR in the collecting duct during physiological and pathophysiological conditions.
Acknowledgments
The authors thank Nancy Busija, M.A., for the help with editing of this manuscript
Source of funding
Fondecyt 11121217, Chile provided support for A.A.G, the National Institutes of Health-NIDDK (DK104375-01) for M.C.P and the Institutional Developmental Award Program of the National Center for Research Resources (P20RR-017659) for A.A.G., and M.C.P.
Reference List
- Borensztein P, Germain S, Fuchs S, Philippe J, Corvol P, Pinet F. cis-Regulatory elements and trans-acting factors directing basal and cAMP-stimulated human renin gene expression in chorionic cells. Circulation Research. 1994;74:764–773. doi: 10.1161/01.res.74.5.764. [DOI] [PubMed] [Google Scholar]
- Butt MJ, Tarantal AF, Jimenez DF, Matsell DG. Collecting duct epithelial-mesenchymal transition in fetal urinary tract obstruction. Kidney Int. 2007;72:936–944. doi: 10.1038/sj.ki.5002457. [DOI] [PubMed] [Google Scholar]
- Casarini DE, Boim MA, Stella RCR, Krieger-Azzolini MH, Krieger JE, Schor N. Angiotensin I-converting enzyme activity in tubular fluid along the rat nephron. American Journal of Physiology-Renal Physiology. 1997;272:F405–F409. doi: 10.1152/ajprenal.1997.272.3.F405. [DOI] [PubMed] [Google Scholar]
- Castrop H, Hocherl K, Kurtz A, Schweda F, Todorov V, Wagner C. Physiology of kidney renin. Physiol Rev. 2010;90:607–673. doi: 10.1152/physrev.00011.2009. [DOI] [PubMed] [Google Scholar]
- Crowley SD, Gurley SB, Herrera MJ, Ruiz P, Griffiths R, Kumar AP, Kim HS, Smithies O, Le TH, Coffman TM. Angiotensin II causes hypertension and cardiac hypertrophy through its receptors in the kidney. Proc Natl Acad Sci USA. 2006;103:17985–17990. doi: 10.1073/pnas.0605545103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuevas CA, Gonzalez AA, Inestrosa NC, Vio CP, Prieto MC. Angiotensin II increases fibronectin and collagen I through the beta-catenin dependent signaling in mouse collecting duct cells. Am J Physiol Renal Physiol. 2014 doi: 10.1152/ajprenal.00429.2014. ajprenal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deinum J, Ronn B, Mathiesen E, Derkx FH, Hop WC, Schalekamp MA. Increase in serum prorenin precedes onset of microalbuminuria in patients with insulin-dependent diabetes mellitus. Diabetologia. 1999;42:1006–1010. doi: 10.1007/s001250051260. [DOI] [PubMed] [Google Scholar]
- Gonzalez AA, Green T, Luffman C, Bourgeois CR, Gabriel NL, Prieto MC. Renal medullary cyclooxygenase-2 and (pro)renin receptor expression during angiotensin II-dependent hypertension. Am J Physiol Renal Physiol. 2014a;307:F962–F970. doi: 10.1152/ajprenal.00267.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez AA, Lara LS, Luffman C, Seth DM, Prieto MC. Soluble Form of the (Pro) Renin Receptor Is Augmented in the Collecting Duct and Urine of Chronic Angiotensin II-Dependent Hypertensive Rats. Hypertension. 2011a;57:859–864. doi: 10.1161/HYPERTENSIONAHA.110.167957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez AA, Liu L, Lara LS, Seth DM, Navar LG, Prieto MC. Angiotensin II Stimulates Renin in Inner Medullary Collecting Duct Cells via Protein Kinase C and Independent of Epithelial Sodium Channel and Mineralocorticoid Receptor Activity. Hypertension. 2011b;57:594–599. doi: 10.1161/HYPERTENSIONAHA.110.165902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez AA, Luffman C, Bourgeois CR, Vio CP, Prieto MC. Angiotensin II-Independent Upregulation of Cyclooxygenase-2 by Activation of the (Pro)Renin Receptor in Rat Renal Inner Medullary Cells. Hypertension. 2013;61:443–449. doi: 10.1161/HYPERTENSIONAHA.112.196303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez AA, Womack JP, Liu L, Seth DM, Prieto MC. Angiotensin II Increases the Expression of (Pro)Renin Receptor During Low-Salt Conditions. American Journal of the Medical Sciences. 2014b;348:416–422. doi: 10.1097/MAJ.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Villalobos RA, Satou R, Ohashi N, Semprun-Prieto LC, Katsurada A, Kim C, Upchurch GM, Prieto MC, Kobori H, Navar LG. Intrarenal mouse renin-angiotensin system during ANG II-induced hypertension and ACE inhibition. Am J Physiol Renal Physiol. 2010;298:F150–F157. doi: 10.1152/ajprenal.00477.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Villalobos RA, Satou R, Seth DM, Semprun-Prieto LC, Katsurada A, Kobori H, Navar LG. Angiotensin-converting enzyme-derived angiotensin II formation during angiotensin II-induced hypertension. Hypertension. 2009;53:351–355. doi: 10.1161/HYPERTENSIONAHA.108.124511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison-Bernard LM, Zhuo J, Kobori H, Ohishi M, Navar LG. Intrarenal AT(1) receptor and ACE binding in ANG II-induced hypertensive rats. Am J Physiol Renal Physiol. 2002;282:F19–F25. doi: 10.1152/ajprenal.00335.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Siragy HM. Sodium depletion enhances renal expression of (pro)renin receptor via cyclic GMP-protein kinase G signaling pathway. Hypertension. 2012;59:317–323. doi: 10.1161/HYPERTENSIONAHA.111.186056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichihara A. (Pro)renin receptor and autophagy in podocytes. Autophagy. 2012;8:271–272. doi: 10.4161/auto.8.2.18846. [DOI] [PubMed] [Google Scholar]
- Ichihara A, Hayashi M, Kaneshiro Y, Suzuki F, Nakagawa T, Tada Y, Koura Y, Nishiyama A, Okada H, Uddin MN, Nabi AH, Ishida Y, Inagami T, Saruta T. Inhibition of diabetic nephropathy by a decoy peptide corresponding to the "handle" region for nonproteolytic activation of prorenin. Journal of Clinical Investigation. 2004;114:1128–1135. doi: 10.1172/JCI21398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichihara A, Kaneshiro Y, Takemitsu T, Sakoda M, Itoh H. The (pro)renin receptor and the kidney. Semin Nephrol. 2007;27:524–528. doi: 10.1016/j.semnephrol.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Ichihara A, Sakoda M, Kurauchi-Mito A, Kaneshiro Y, Itoh H. Involvement of (pro)renin receptor in the glomerular filtration barrier. J Mol Med(Berl) 2008;86:629–635. doi: 10.1007/s00109-008-0327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingelfinger JR, Jung F, Diamant D, Haveran L, Lee E, Brem A, Tang SS. Rat proximal tubule cell line transformed with origin-defective SV40 DNA: autocrine ANG II feedback. American Journal of Physiology-Renal Physiology. 1999;276:F218–F227. doi: 10.1152/ajprenal.1999.276.2.F218. [DOI] [PubMed] [Google Scholar]
- Ishidoya S, Morrissey J, McCracken R, Reyes A, Klahr S. Angiotensin II receptor antagonist ameliorates renal tubulointerstitial fibrosis caused by unilateral ureteral obstruction. Kidney Int. 1995;47:1285–1294. doi: 10.1038/ki.1995.183. [DOI] [PubMed] [Google Scholar]
- Ivanova L, Butt MJ, Matsell DG. Mesenchymal transition in kidney collecting duct epithelial cells. Am J Physiol Renal Physiol. 2008;294:F1238–F1248. doi: 10.1152/ajprenal.00326.2007. [DOI] [PubMed] [Google Scholar]
- Kaneshiro Y, Ichihara A, Takemitsu T, Sakoda M, Suzuki F, Nakagawa T, Hayashi M, Inagami T. Increased expression of cyclooxygenase-2 in the renal cortex of human prorenin receptor gene-transgenic rats. Kidney Int. 2006;70:641–646. doi: 10.1038/sj.ki.5001627. [DOI] [PubMed] [Google Scholar]
- Kang JJ, Toma I, Sipos A, Meer EJ, Vargas SL, Peti-Peterdi J. The collecting duct is the major source of prorenin in diabetes. Hypertension. 2008;51:1597–1604. doi: 10.1161/HYPERTENSIONAHA.107.107268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Harrison-Bernard LM, Navar LG. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney International. 2002;61:579–585. doi: 10.1046/j.1523-1755.2002.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Harrison-Bernard LM, Navar LG. Enhancement of angiotensinogen expression in angiotensin II-dependent hypertension. Hypertension. 2001;37:1329–1335. doi: 10.1161/01.hyp.37.5.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Katsurada A, Miyata K, Ohashi N, Satou R, Saito T, Hagiwara Y, Miyashita K, Navar LG. Determination of plasma and urinary angiotensinogen levels in rodents by newly developed ELISA. Am J Physiol Renal Physiol. 2008;294:F1257–F1263. doi: 10.1152/ajprenal.00588.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Nishiyama A, Harrison-Bernard LM, Navar LG. Urinary angiotensinogen as an indicator of intrarenal Angiotensin status in hypertension. Hypertension. 2003;41:42–49. doi: 10.1161/01.hyp.0000050102.90932.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Prieto-Carrasquero MC, Ozawa Y, Navar LG. AT1 receptor mediated augmentation of intrarenal angiotensinogen in angiotensin II-dependent hypertension. Hypertension. 2004;43:1126–1132. doi: 10.1161/01.HYP.0000122875.91100.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobori H, Urushihara M, Xu JH, Berenson GS, Navar LG. Urinary angiotensinogen is correlated with blood pressure in men (Bogalusa Heart Study) Journal of Hypertension. 2010;28:1422–1428. doi: 10.1097/HJH.0b013e3283392673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komlosi P, Fuson AL, Fintha A, Peti-Peterdi J, Rosivall L, Warnock DG, Bell PD. Angiotensin I conversion to angiotensin II stimulates cortical collecting duct sodium transport. Hypertension. 2003;42:195–199. doi: 10.1161/01.HYP.0000081221.36703.01. [DOI] [PubMed] [Google Scholar]
- Kurtz A, Wagner C. Cellular control of renin secretion. Journal of Experimental Biology. 1999;202:219–225. doi: 10.1242/jeb.202.3.219. [DOI] [PubMed] [Google Scholar]
- Lantelme P, Rohrwasser A, Vincent M, Cheng T, Gardier S, Legedz L, Bricca G, Lalouel JM, Milon H. Significance of urinary angiotensinogen in essential hypertension as a function of plasma renin and aldosterone status. J Hypertens. 2005;23:785–792. doi: 10.1097/01.hjh.0000163147.20330.f5. [DOI] [PubMed] [Google Scholar]
- Liu L, Lara LS, Gonzalez AA, Bourgeois CR, Seth DM, Prieto MC. Angiotensin Ii Stimulates Renin Synthesis and Secretion Via Protein Kinase C Activation and Camp Accumulation in Collecting Duct M-1 Cells. Journal of Investigative Medicine. 2012;60:456–457. [Google Scholar]
- Matavelli LC, Huang J, Siragy HM. (Pro)renin receptor contributes to diabetic nephropathy by enhancing renal inflammation. Clin Exp Pharmacol Physiol. 2010;37:277–282. doi: 10.1111/j.1440-1681.2009.05292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matavelli LC, Huang J, Siragy HM. In vivo regulation of renal expression of (pro)renin receptor by a low-sodium diet. Am J Physiol Renal Physiol. 2012;303:F1652–F1657. doi: 10.1152/ajprenal.00204.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller MW, Todorov V, Kramer BK, Kurtz A. Angiotensin II inhibits renin gene transcription via the protein kinase C pathway. Pflugers Archiv European Journal of Physiology. 2002;444:499–505. doi: 10.1007/s00424-002-0835-8. [DOI] [PubMed] [Google Scholar]
- Navar LG, Harrison-Bernard LM. Intrarenal angiotensin II augmentation in angiotensin II dependent hypertension. Hypertens Res. 2000;23:291–301. doi: 10.1291/hypres.23.291. [DOI] [PubMed] [Google Scholar]
- Navar LG, Harrison-Bernard LM, Nishiyama A, Kobori H. Regulation of intrarenal angiotensin II in hypertension. Hypertension. 2002;39:316–322. doi: 10.1161/hy0202.103821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navar LG, Mitchell KD, Harrison-Bernard LM, Kobori H, Nishiyama A. Intrarenal angiotensin II levels in normal and hypertensive states. JRAAS. 2001;2:S176–S184. doi: 10.1177/14703203010020013001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen G, Burckle C, Sraer JD. The renin receptor: the facts, the promise and the hope. Curr Opin Nephrol Hypertens. 2003;12:51–55. doi: 10.1097/00041552-200301000-00009. [DOI] [PubMed] [Google Scholar]
- Nguyen G, Contrepas A. Physiology and pharmacology of the (pro)renin receptor. Curr Opin Pharmacol. 2008;8:127–132. doi: 10.1016/j.coph.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Nguyen G, Danser AH. The (pro)renin receptor: therapeutic consequences. Expert Opin Investig Drugs. 2006;15:1131–1135. doi: 10.1517/13543784.15.10.1131. [DOI] [PubMed] [Google Scholar]
- Nguyen G, Delarue F, Berrou J, Rondeau E, Sraer JD. Specific receptor binding of renin on human mesangial cells in culture increases plasminogen activator inhibitor-1 antigen. Kidney Int. 1996;50:1897–1903. doi: 10.1038/ki.1996.511. [DOI] [PubMed] [Google Scholar]
- Nguyen G, Delarue F, Burckle C, Bouzhir L, Giller T, Sraer JD. Pivotal role of the renin/prorenin receptor in angiotensin II production and cellular responses to renin. J Clin Invest. 2002;109:1417–1427. doi: 10.1172/JCI14276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen G, Muller DN. The biology of the (pro)renin receptor. J Am Soc Nephrol. 2010;21:18–23. doi: 10.1681/ASN.2009030300. [DOI] [PubMed] [Google Scholar]
- Nishiyama A, Seth DE, Navar LG. Renal interstitial concentrations of angiotensin I and angiotensin II in angiotensin II-infused hypertensive rats. Journal of the American Society of Nephrology. 2001;12:574A. Ref Type: Abstract. [Google Scholar]
- Ogawa S, Kobori H, Ohashi N, Urushihara M, Nishiyama A, Mori T, Ishizuka T, Nako K, Ito S. Angiotensin II Type 1 Receptor Blockers Reduce Urinary Angiotensinogen Excretion and the Levels of Urinary Markers of Oxidative Stress and Inflammation in Patients with Type 2 Diabetic Nephropathy. Biomark Insights. 2009;4:97–102. doi: 10.4137/bmi.s2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peti-Peterdi J, Warnock DG, Bell PD. Angiotensin II directly stimulates ENaC activity in the cortical collecting duct via AT(1) receptors. Journal of the American Society of Nephrology. 2002;13:1131–1135. doi: 10.1097/01.asn.0000013292.78621.fd. [DOI] [PubMed] [Google Scholar]
- Prieto MC, Gonzalez AA, Navar LG. Evolving concepts on regulation and function of renin in distal nephron. Pflugers Archiv European Journal of Physiology. 2013;465:121–132. doi: 10.1007/s00424-012-1151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto-Carrasquero MC, Botros FT, Kobori H, Navar LG. Collecting Duct Renin: A major player in Angiotensin II-dependent Hypertension. J Am Soc Hypertens. 2009;3:96–104. doi: 10.1016/j.jash.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto-Carrasquero MC, Botros FT, Pagan J, Kobori H, Seth DM, Casarini DE, Navar LG. Collecting duct renin is upregulated in both kidneys of 2-kidney, 1-clip goldblatt hypertensive rats. Hypertension. 2008;51:1590–1596. doi: 10.1161/HYPERTENSIONAHA.108.110916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto-Carrasquero MC, Harrison-Bernard LM, Kobori H, Ozawa Y, Hering-Smith KS, Hamm LL, Navar LG. Enhancement of collecting duct renin in angiotensin II-dependent hypertensive rats. Hypertension. 2004;44:223–229. doi: 10.1161/01.HYP.0000135678.20725.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto-Carrasquero MC, Kobori H, Ozawa Y, Gutierrez A, Seth D, Navar LG. AT1 receptor-mediated enhancement of collecting duct renin in angiotensin II-dependent hypertensive rats. Am J Physiol Renal Physiol. 2005;289:F632–F637. doi: 10.1152/ajprenal.00462.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinto BM, Pesquero JB, Casarini DE. Identification of a new site of angiotensin I-converting enzyme (ACE) production in IMCD cells and study of interaction between the bradykinin receptor B2 and ACE using ACE inhibitor. J Hypertens. 2002;20:S195. Ref Type: Abstract. [Google Scholar]
- Ramkumar N, Kohan DE. Role of collecting duct renin in blood pressure regulation. American Journal of Physiology-Regulatory Integrative and Comparative Physiology. 2013;305:R92–R94. doi: 10.1152/ajpregu.00191.2013. [DOI] [PubMed] [Google Scholar]
- Ramkumar N, Ying J, Stuart D, Kohan DE. Overexpression of renin in the collecting duct causes hypertension. FASEB Journal. 2013b;27 doi: 10.1093/ajh/hpt071. [DOI] [PubMed] [Google Scholar]
- Ramkumar N, Ying J, Stuart D, Kohan DE. Overexpression of Renin in the Collecting Duct Causes Elevated Blood Pressure. American Journal of Hypertension. 2013a;26:965–972. doi: 10.1093/ajh/hpt071. [DOI] [PubMed] [Google Scholar]
- Redublo Quinto BM, Camargo de Andrade MC, Ronchi FA, Santos EL, ves Correa SA, Shimuta SI, Pesquero JB, Mortara RA, Casarini DE. Expression of angiotensin I-converting enzymes and bradykinin B-2 receptors in mouse inner medullary-collecting duct cells. International Immunopharmacology. 2008;8:254–260. doi: 10.1016/j.intimp.2007.09.013. [DOI] [PubMed] [Google Scholar]
- Rohrwasser A, Ishigami T, Gociman B, Lantelme P, Morgan T, Cheng T, Hillas E, Zhang S, Ward K, Bloch-Faure M, Meneton P, Lalouel JM. Renin and kallikrein in connecting tubule of mouse. Kidney Int. 2003;64:2155–2162. doi: 10.1046/j.1523-1755.2003.00302.x. [DOI] [PubMed] [Google Scholar]
- Rohrwasser A, Morgan T, Dillon HF, Zhao L, Callaway CW, Hillas E, Zhang S, Cheng T, Inagami T, Ward K, Terreros DA, Lalouel JM. Elements of a paracrine tubular renin-angiotensin system along the entire nephron. Hypertension. 1999;34:1265–1274. doi: 10.1161/01.hyp.34.6.1265. [DOI] [PubMed] [Google Scholar]
- Satofuka S, Ichihara A, Nagai N, Noda K, Ozawa Y, Fukamizu A, Tsubota K, Itoh H, Oike Y, Ishida S. (Pro)renin receptor-mediated signal transduction and tissue renin-angiotensin system contribute to diabetes-induced retinal inflammation. Diabetes. 2009;58:1625–1633. doi: 10.2337/db08-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satou R, Gonzalez-Villalobos RA, Miyata K, Ohashi N, Katsurada A, Navar LG, Kobori H. Costimulation with angiotensin II and interleukin 6 augments angiotensinogen expression in cultured human renal proximal tubular cells. Am J Physiol Renal Physiol. 2008;295:F283–F289. doi: 10.1152/ajprenal.00047.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satou R, Gonzalez-Villalobos RA, Miyata K, Ohashi N, Urushihara M, Acres OW, Navar LG, Kobori H. IL-6 augments angiotensinogen in primary cultured renal proximal tubular cells. Mol Cell Endocrinol. 2009;311:24–31. doi: 10.1016/j.mce.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satou R, Miyata K, Gonzalez-Villalobos RA, Ingelfinger JR, Navar LG, Kobori H. Interferon-gamma biphasically regulates angiotensinogen expression via a JAK-STAT pathway and suppressor of cytokine signaling 1 (SOCS1) in renal proximal tubular cells. FASEB J. 2012;26:1821–1830. doi: 10.1096/fj.11-195198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seikaly MG, Arant BS, Jr, Seney FD., Jr Endogenous angiotensin concentrations in specific intrarenal fluid compartments of the rat. Journal of Clinical Investigation. 1990;86:1352–1357. doi: 10.1172/JCI114846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao W, Seth DM, Navar LG. Augmentation of endogenous intrarenal angiotensin II levels in Val5-ANG II-infused rats. Am J Physiol Renal Physiol. 2009;296:F1067–F1071. doi: 10.1152/ajprenal.90596.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao W, Seth DM, Navar LG. Angiotensin II type 1 receptor-mediated augmentation of urinary excretion of endogenous angiotensin II in Val5-angiotensin II-infused rats. Hypertension. 2010;56:378–383. doi: 10.1161/HYPERTENSIONAHA.110.153106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao W, Seth DM, Prieto MC, Kobori H, Navar LG. Activation of the Renin-Angiotensin System by a Low Salt Diet Does Not Augment Intratubular Angiotensinogen and Angiotensin II in Rats. Am J Physiol Renal Physiol. 2013 doi: 10.1152/ajprenal.00587.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vio CP, Jeanneret VA. Local induction of angiotensin-converting enzyme in the kidney as a mechanism of progressive renal diseases. Kidney Int Suppl. 2003:57–63. doi: 10.1046/j.1523-1755.64.s86.11.x. [DOI] [PubMed] [Google Scholar]
- Wang CT, Navar LG, Mitchell KD. Proximal tubular fluid angiotensin II levels in angiotensin II-induced hypertensive rats. J Hypertens. 2003;21:353–360. doi: 10.1097/00004872-200302000-00027. [DOI] [PubMed] [Google Scholar]
- Wang F, Lu X, Peng K, Zhou L, Li C, Wang W, Yu X, Kohan DE, Zhou SF, Yang T. COX-2 Mediates Angiotensin II-Induced (Pro)Renin Receptor Expression in the Rat Renal Medulla. Am J Physiol Renal Physiol. 2014a doi: 10.1152/ajprenal.00548.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Lu XH, Peng KX, Du YM, Zhou SF, Zhang AH, Yang TX. Prostaglandin E-Prostanoid(4) Receptor Mediates Angiotensin II-Induced (Pro) Renin Receptor Expression in the Rat Renal Medulla. Hypertension. 2014b;64:369–377. doi: 10.1161/HYPERTENSIONAHA.114.03654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto T, Nakagawa T, Suzuki H, Ohashi N, Fukasawa H, Fujigaki Y, Kato A, Nakamura Y, Suzuki F, Hishida A. Urinary angiotensinogen as a marker of intrarenal angiotensin II activity associated with deterioration of renal function in patients with chronic kidney disease. J Am Soc Nephrol. 2007;18:1558–1565. doi: 10.1681/ASN.2006060554. [DOI] [PubMed] [Google Scholar]
- Zhao D, Navar LG. Acute angiotensin II infusions elicit pressure natriuresis in mice and reduce distal fractional sodium reabsorption. Hypertension. 2008;52:137–142. doi: 10.1161/HYPERTENSIONAHA.108.111435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao D, Seth DM, Navar LG. Enhanced distal nephron sodium reabsorption in chronic angiotensin II-infused mice. Hypertension. 2009;54:120–126. doi: 10.1161/HYPERTENSIONAHA.109.133785. [DOI] [PMC free article] [PubMed] [Google Scholar]